Advances in cervical cancer
prevention
Dr Margaret Sage
NCSP Clinical Lead, Pathology

Major advances are occurring in cervical
cancer prevention: four topics
1. Reducing health inequities between different population
groups in New Zealand
2. HPV immunisation (primary prevention): prevents HPV
infection so less abnormal cytology and histology
3. Primary screening with HPV testing (secondary
prevention): more sensitive than cytology so more
detection
4. Self-testing (self-collection) for HPV tests: increases
coverage i.e. more people screened so more detection
2

3
2021 Stats NZ Estimates
Total NZ Population
5,122,600
European/Pakeha 69.4%
Maori 17.1%
Asian 17.1%
Pacific 8.6%
Treaty of Waitangi (Te Tiriti o Waitangi) signed 1840
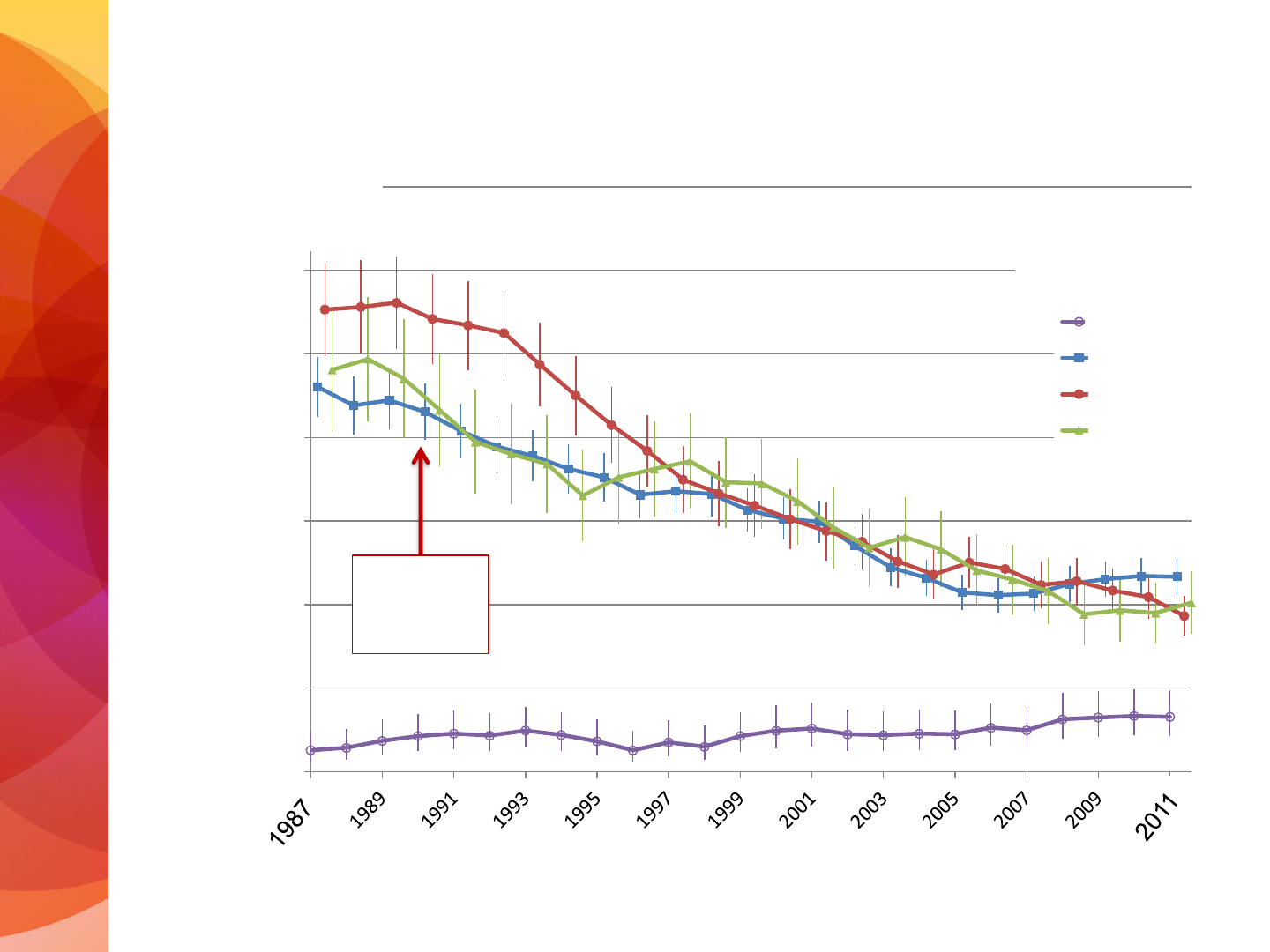
Topic 1: Inequities in cervical screening
New Zealand has a high quality cervical screening programme…
• In 2012 our cervical cancer incidence and mortality rates were the third
lowest in the world (after Finland and Switzerland)
• Since: our coverage has dropped, other countries have moved ahead
with HPV primary screening and have better HPV immunisation rates
…BUT we have significant ethnic disparities in cervical cancer rates
• The NCSP has been trying hard to close the gap between Maori and
European/Pakeha cervical cancer rates for years, with limited success
• major initiatives now being introduced to reduce inequalities

NCSP Annual Report 2017
Age-standardised (WHO) cervical cancer
incidence rates 1985-2017
4
Incidence per 100,000
9.7 Maori
6.1 All women
(5.7 Euro/
Pakeha)
168 new cases in 2017

Is the gap closing?
Cervical Cancer incidence 2011-2017
5
Rates Maori vs All women: 2011: 12.0/6.8 = 1.7 x higher for Maori
2017: 9.7/6.1 = 1.6 x higher for Maori
Rates Maori vs Euro/Pakeha women: 2011: 12.0/6.2 = 1.8 x higher for Maori
2017: 9.7/5.7 = 1.7 x higher for Maori

3-year screening coverage, 25-69 years
over 15 years, to July 2021
6

7
3-year screening coverage, 25-69 years over 15
years, to July 2021, by ethnicity
Coverage is the major reason why cancer rates vary across
different ethnic groups
Delays in follow-up e.g. time to get to colposcopy also contributes
Smoking rates may also play a role

Age-standardised (WHO) cervical cancer incidence
rates in 5–year periods by age: 2013-17
8
NCSP Annual Report 2017
Incidence per 100,000 women

9
Cervical Cancer Incidence Rates in 5 year periods, by
age and ethnicity
NCSP Annual Report 2017

10
Cervical Cancer Incidence Rates in 5 year periods, by age
NCSP Annual Reports 2012 and 2017

11
Trends in 3-year coverage by age (women screened in the
previous three years, as a proportion of the hysterectomy-
adjusted population)
NCSP Monitoring Report 52

12
NCSP Annual Report 2017
Age-standardised (WHO) cervical cancer mortality rates
2.9 Maori
1.7 All women
(1.3 = Other)
Maori death rate is 1.7 times All women rate, and 2.2 times Euro/Pak women

NCSP Annual Report 2017
Five-year average cervical cancer mortality rates
(2011-2015) by age
13

NCSP Annual Report
Five-year average cervical cancer mortality rates,
2012-16, by age and ethnicity
14

Topic 2. HPV Immunisation in NZ
HPV immunisation programme using Gardasil-4 commenced in
2008, was free for women up to 20 years of age
The school–based programme for girls began in 2011 and was
much more successful in achieving coverage.
Since 1 Jan 2017:
Gardasil-9 is funded for both boys and girls aged 9-26 years
(inclusive) with two-doses @9-14 years and three doses@15+
years of age
• Vaccination sometimes used after treatment of a high-grade
lesion because it can still protect against other HPV types
In 2017, approximately 70% of both boys and girls aged 10-11
years were immunised against HPV

Effect of immunisation to date
16

High rates of CIN2/3 occur in women <35 years
17
Rate of women with CIN2/3 per 1,000 women screened, by age and ethnicity
for July-Dec 2019

HPV type No. of
infections
HPV-16 116
HPV-18 47
HPV-31 9
HPV-45 7
HPV-52 7
HPV-59 5
HPV-33 4
HPV-35 3
HPV-39 3
HPV-51 2
HPV-56 3
HPV-66 1
HPV-68 3
Un
-
identified
2
Low
-risk HPV
-
11, 70
2 (1)
Red HPV types: Gardasil-9 (191/212 infections)
Type distribution of HPV among adult
women diagnosed with invasive cervical
cancer (stage 1b or higher) in New
Zealand
Peter Sykes, Kusuma Gopala, Ai Ling Tan,
Diane Kenwright, Simone Petrich, Arico
Molijn, and Jing Chen
BMC Infectious Diseases 2014,14:374
HPV genotyping was performed on cervical
tissue for 227 cases of cervical cancer
diagnosed 2004 - 2010
HPV was detected in 201 cases (88.5%) with
multiple infections present in 11 cases
(5.5%).

Topic 3: Primary screening with HPV tests
NCSP in NZ: what we do now
Cytology-based screening from 25-69 years of age with
a 3-yearly screening interval
• hrHPV testing is used as a second test for
1. Triage of low-grade cytology for women 30+years
with no cyto/histo abnormality in the last 5 years
2. Test of cure after treatment of high-grade
squamous lesions
3. Specialist-ordered testing for managing women
with discordant histo/cyto/colposcopy results
19

March 2016: Minister of Health announced that
the NCSP will move to HPV primary screening with
partial genotyping and cytology triage, with
screening commencing at 25 years of age
June 2018
1. Implementation of HPV primary screening was
delayed until 2021 (later delayed again to 2023)
2. The recommenced age to commence screening
would still rise to 25 years in 2019 (which it did)
Changing cervical screening in NZ

The NCSP raised the recommended age to
commence cervical screening to 25 years of
age in November 2019
• This remained cytology-based screening
• Women commencing screening continue to have two
screens 12 months apart before moving to regular three-
yearly screening
Recommendations are:
1. Women who have not commenced screening: Start at 25
2. Women who have already been screened and have had an
abnormality: Continue with current management pathway
3. Women who have commenced screening and have normal
results: Continue with the current screening pathway
Five-year average cervical cancer incidence in New
Zealand, by age (age-standardised, per 100,000)
0
5
10
15
20
25
30
35
Age-standardised
incidence
20-24 years
25-49 years
50-69 years
70 + years
NCSP
starts
Cancer Council of NSW
A/Prof Karen Canfell, Dr Megan Smith
20-24
25-49
50-69
70+
AGE (years)

Invasive cervical cancers under 25 years: 2009-18
New Zealand Cancer Registry data
0
1
2
3
4
5
6
7
8
2009 2010 2011 2012 2013 2014 2015 2016 2017 2018
Number of cases
2009-2013: 25 cases
2014-2018: 9 cases (excluding one sarcoma in 2015)

NCSP: what we will do from mid-2023
HPV-based screening from 25-69 years of age
with a 5-yearly screening interval
• Cytology will be used as a second test for those
who are HPV positive
24

Colposcopy
hrHPV Testing (ST or CTS)

Predicted reductions in cervical cancer rates
by using HPV testing for primary screening
(vaccinated-unvaccinated scenarios)
Incidence reduction: 11.7 – 15.7%
Mortality reduction: 11.9 – 16.5%
If 170 new cases annually, HPV screening strategy
prevents 20 - 27 cases
If 60 deaths annually, HPV screening strategy prevents
7 – 10 deaths
These predictions to not include the impact of self-
testing to increase coverage so the gains are likely to
be quite a bit higher than this
HPV type No. of
infections
HPV-16 116
HPV-18 47
HPV-31 9
HPV-45 7
HPV-52 7
HPV-59 5
HPV-33 4
HPV-35 3
HPV-39 3
HPV-51 2
HPV-56 3
HPV-66 1
HPV-68 3
Un
-
identified
2
Low
-risk HPV
-
11, 70
2 (1)
Red HPV types: Gardasil-9 (191/212 infections)
Green types: HPV Testing covers the red HPV types
plus the green HPV types
Type distribution of HPV among adult
women diagnosed with invasive cervical
cancer (stage 1b or higher) in New
Zealand
Peter Sykes, Kusuma Gopala, Ai Ling Tan,
Diane Kenwright, Simone Petrich, Arico
Molijn, and Jing Chen
BMC Infectious Diseases 2014,14:374
HPV genotyping was performed on
cervical tissue for 227 cases of cervical
cancer diagnosed 2004 - 2010
HPV was detected in 201 cases (88.5%)
with multiple infections present in 11
cases (5.5%).

4. Self-Testing (= self-sampling or self-collection)
Self-testing can assist women who are reluctant or unable to be
screened currently, to have a cervical screening test. This could
result in a significant reduction in cervical cancer rates.
Trials in New Zealand have shown significant acceptability and
impact on improving coverage rates particularly for Maori
women and underscreened women
Robust evidence has established that HPV testing on a self-
collected sample is as accurate as a clinician-taken sample as
long PCR DNA-based HPV test technology is used. All NZ HPV
test technologies comply with this
• Sampling will still be based in primary health care, with
a variety of outreach initiatives to improve coverage.

The future is bright for cervical cancer
prevention
29
