
Initial Report on Public Health
August 2009
Public Health Division
Ministry of Health and Long-Term Care

Initial Report on Public Health Contacts
Public Health Practice Branch:

iii
We are very pleased to provide you with the Ministry of Health and Long-Term Care’s (MOHLTC)
Initial Report on Public Health in Ontario.
The Public Health Division, in partnership with the Ministry of Health Promotion (MHP) and
the Ministry of Children and Youth Services (MCYS), has made significant strides to renew
public health in Ontario and build a public health sector with a greater focus on performance,
accountability and sustainability. Some of our recent achievements towards this goal include
delivering the new Ontario Public Health Standards, producing the Ontario Health Plan for
an Influenza Pandemic, and now, releasing a public report that reflects the state of public
health in Ontario. This report demonstrates our commitment to a public health sector that
is accountable to the people of Ontario.
The indicators provided in this report are intended to contribute to our understanding of
public health in Ontario as a system, at both the provincial and local levels. As we move
towards implementing a performance management system in public health, we have an
increased need for information that can be used to ensure the public’s health is protected, to
inform decisions on where improvements are required, to ensure that appropriate governance
is in place and to help promote organizational excellence.
This initial report is intended to provide a snapshot of the current state of public health in
Ontario. Over time, with the continued involvement of public health professionals in the
sector, different indicators will need to be identified and developed. There is significant
expertise related to performance management already available within our sector, and within
the health care sector, and we will be relying on these resources to assist in developing
the tools and processes required to operate a useful, efficient and effective performance
management system at the provincial level.
Foreword

iv
The work of the Capacity Review Committee (2006) gave us an important conceptual framework for
performance management. The work to implement this vision is now well underway, and this report is
the first tangible product that begins to articulate that vision.
We hope you find the report informative and, most importantly, useful. We would like to take this opportunity
to thank the members of the Performance Management Working Group who provided advice that shaped the
development of this report. Their knowledge and wisdom have contributed substantially to the quality of this
product.
Allison J. Stuart Arlene S. King, MD, MHSc, FRCPC
Assistant Deputy Minister (A) Chief Medical Officer of Health (effective June 15, 2009)
Public Health Division
Ministry of Health and Long-Term Care
David C. Williams MD, MHSc, FRCPC
Chief Medical Officer of Health (A) (until June 15, 2009)
Associate Chief Medical Officer of Health,
Health Protection

v
Initial Report on Public Health 2009
Producing this report involved the commitment of a diverse group of individuals, each of whom contributed
their time and advice to ensure that the final product was representative of public health in Ontario at both
the local and provincial levels. The ministry acknowledges and thanks the many individuals who contributed
to this report including:
• ThemembersofthePerformanceManagementWorkingGroup(PMWG)in2007-2008
i
who advised on the
development of this report:
– Dr. Kathleen Dooling, Community Medicine Resident, University of Toronto
– Dr. Vera Etches, Medical Officer of Health (A), Sudbury & District Health Unit
– Dr. Charles Gardner, Medical Officer of Health,
Simcoe-MuskokaDistrictHealthUnit/2007-08COMOHChair
– Ms. Dawne Kamino, Director, Controllership & Resources Management Branch,
Ministry of Health and Long-Term Care
– Dr. Jeff Kwong, Scientist, Institute for Clinical Evaluative Sciences
– Dr. Robert Kyle, Commissioner & Medical Officer of Health, Durham Region Health Department
– Dr. Jack Lee, Senior Strategic Advisor, Ministry of Health Promotion
– Dr. Doug Manuel, Senior Scientist, Institute for Clinical Evaluative Sciences
(co-chairDecember,2007–May,2008)
– Dr. Rosana Pellizzari, Associate Medical Officer of Health, Toronto Public Health
(co-chairfromMay,2008)
– Ms. Katharine Robertson-Palmer, Coordinator, Education and Research, Ottawa Public Health
– Ms. Julie Stratton, Manager, Epidemiology, Peel Regional Health Unit/APHEO
– Ms. Brenda Tipper, Health System Strategy Division, Ministry of Health and Long-Term Care
– Ms. Monika Turner, Director, Public Health Standards Branch,
Ministry of Health and Long-Term Care (co-chair)
– Dr. Erica Weir, Associate Medical Officer of Health, York Regional Health Unit
– Ms. Jackie Wood, Manager, Corporate Services, Ministry of Health Promotion
• Staffinpublichealthunitsacrosstheprovince,whocontributedbycompletingthesurveyofboards
of health on governance and management issues, providing case studies, and verifying the indicator
methodology and data that appear in the report.
• MembersoftheAssociationofPublicHealthBusinessAdministratorswhoassistedindevelopingthe
survey tool that was used to gather governance, organizational practices and financial data.
Acknowledgements
i
It should be noted that some members changed positions during the course of the production of the report. However this list accurately
reflects the PMWG membership and roles during the period of the report’s development.

vi
• TheInstituteforClinicalEvaluativeSciences(ICES)andPeelPublicHealth,whichprovideddataanalysis
and advice.
• MembersoftheAssociationofPublicHealthEpidemiologistsinOntario(APHEO)whoprovidedtechnical
advice on indicator methodology and development:
– Ms. Deborah Carr
– Ms. Sherri Deamond
– Mr. Foyez Haque
– Ms. Joanna Oliver
– Ms. Suzanne Sinclair
• StaffwithintheMinistryofHealthPromotionandtheMinistryofChildrenandYouthServices,
who contributed to the indicator narratives and conducted data analysis.
• StaffwithintheMinistryofHealthandLong-TermCare,whoadvisedonthedevelopmentofthisreport
throughout2008-09withinthefollowingbranches:
ii
– Communications and Information Branch
– Controllership and Resources Management Branch
– Emergency Management Branch
– Environmental Health Branch
– Health Analytics Branch
– Infectious Diseases Branch
– Legal Services Branch
– Strategic Alignment Branch
• StaffoftheStrategicPolicyandImplementationBranch,
ii
who provided research and editorial support in
the development of this report:
– Ms. Allison McArthur
– Ms. Beata Pach
• StaffofthePublicHealthStandardsBranch,
ii
who acted as secretariat to the PMWG and guided this
document through the development process, including:
– Mr. David Moore
– Mr. Hassan Parvin
– Ms. Paulina Salamo
– Ms. Sylvia Shedden
– Ms. Joanne Thanos
– Ms. Lisa Vankay
– Ms. Tricia Willis
ii
Note that the Public Health Division underwent a restructuring that coincided with the publication of this report. The branch names
shown here reflect the branches as they were known during the period of the report’s development.
Acknowledgements

vii
Initial Report on Public Health 2009
Table of Contents
Foreword .............................................................................................................. iii
Acknowledgements ................................................................................................ v
Section I: Introduction ..........................................................................................1
Section II: Overview of the Public Health Sector ............................................... 3
Scope of Public Health ...................................................................................................... 3
Legislative Framework for Public Health ....................................................................... 4
Determinants of Health...................................................................................................... 5
Public Health Programs and Services in Ontario ........................................................... 6
Health Unit Profiles ............................................................................................................ 6
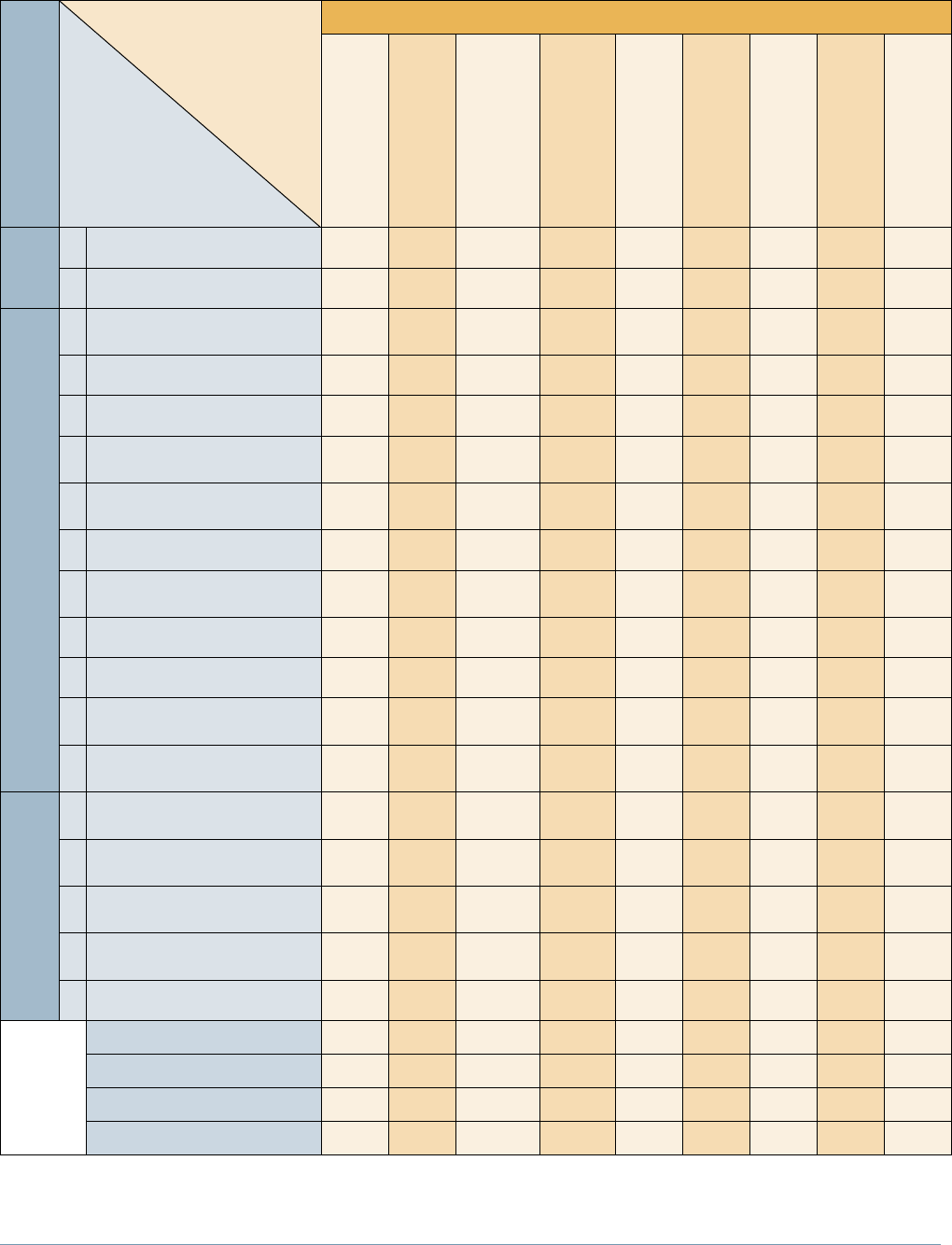
Table 1: Health Unit Profiles ............................................................................................. 8
Section III: Performance of the Public Health Sector ...................................... 13
Report Development ........................................................................................................ 13
Development of Indicators .............................................................................................. 15
Case Studies ...................................................................................................................... 16
Section IV: Indicators ..........................................................................................17
Table 2: Indicators by Public Health Unit ...................................................................... 20
Group A – Population Health Indicators............................................................29
1. Teen Pregnancy .......................................................................................................... 29
2. Low Birth Weight ........................................................................................................ 31
3. Breastfeeding Duration ............................................................................................. 32
4. Postpartum Contact ................................................................................................... 33
5. Smoking Prevalence .................................................................................................. 34
6. Youth Lifetime Smoking Abstinence ........................................................................ 34
7. Adult Heavy Drinking ................................................................................................ 37
8.YouthHeavyDrinking ................................................................................................ 39
9. Physical Activity Index .............................................................................................. 40
10. Healthy Body Mass Index .......................................................................................... 41
11. Fruit and Vegetable Consumption............................................................................ 42
12. Fall-Related Hospitalizations among Seniors ......................................................... 43
13. Enteric Illnesses Incidence ....................................................................................... 46
14. Respiratory Infection Outbreaks in Long-Term Care Homes ............................... 46

viii
15. Chlamydia Incidence ................................................................................................. 48
16. Immunization Coverage for Hepatitis B .................................................................. 48
17. Immunization Coverage for Measles, Mumps and Rubella ................................... 50
18.AdverseWaterQualityIncidents .............................................................................. 51
Group B – Governance and Accountability Indicators .....................................53
19. Total Board of Health Expenditures ........................................................................ 53
20. Board of Health Expenditure Variance ................................................................... 54
21. Expenditures on Training and Professional Development ................................... 56
22. Numbers of FTEs by Job Category .......................................................................... 56
23. Number of Vacant Positions by Job Category ........................................................ 58
24. Employment Status of Medical Officers of Health ................................................ 59
25. Staff Length of Service .............................................................................................. 61
26. Familiarity with Public Health Unit Programs and Services ................................ 62
27. Issuance of a Health Status Report .......................................................................... 63
28.StrategicPlan .............................................................................................................. 65
29. Emergency Response Plan Tested ........................................................................... 65
30. Accreditation Status .................................................................................................. 66
31. Medical Officer of Health Performance Evaluation .............................................. 67
32. Medical Officer of Health Reporting Relationships ............................................... 67
33. Board Member Orientation ....................................................................................... 68
34. Board Self-Evaluation ................................................................................................ 68
Section V: Moving Towards Performance Reporting ......................................... 71
Context for Performance Management in Public Health ........................................... 71
Developing a Performance Management Culture ........................................................ 73
Future Indicators .............................................................................................................. 73
Requirements for a Performance Management System ............................................. 74
Implementation Challenges ............................................................................................ 74
Implementation Opportunities ....................................................................................... 75
Conclusion ......................................................................................................................... 75
Appendices ........................................................................................................... 77
Appendix 1: Peer Groups ................................................................................................ 77
Appendix 2: Health Unit Profile Variable Definitions ................................................. 83
Appendix 3: Indicator Definitions ................................................................................. 89
References .......................................................................................................... 125
Table of Contents

1
Initial Report on Public Health 2009
Introduction
Section I:
In A Dictionary of Public Health, John Last
1
defines public health as:
“an organized activity of society to promote, protect, improve, and when necessary, restore the health of
individuals, specified groups, or the entire population ...The term “public health” can describe a concept,
a social institution, a set of scientific and professional disciplines and technologies, and a form of
practice ... It is a way of thinking, a set of disciplines, an institution of society, and a manner of practice”.
On a daily basis, Ontario’s public health sector contributes to keeping Ontarians healthy and safe through
health protection, disease prevention and management, and health promotion activities. The essential day-to-
day work of the public health sector often goes unnoticed as many potential health threats or conditions are
contained or averted by routine prevention, health protection, health promotion, as well as surveillance and
management activities carried out by public health organizations across Ontario.
Some of the great accomplishments of public health in the twentieth century include the virtual elimination
of polio in Canada, the pasteurization of milk, the disinfection and fluoridation of drinking water, and the
identification and prevention of tobacco-related illness. These examples demonstrate the contribution that
public health has made to protect the health of the population.
A strong public health sector is vital to a healthy and safe Ontario population and yet we tend not to think
about it except in times of crisis. The anonymity of the public health sector disappeared quickly with the
gastroenteritis outbreaks in Walkerton in 2000 and the Severe Acute Respiratory Syndrome (SARS) crisis
in 2003. These two events revealed serious weaknesses in the province’s public health sector at the time.
Key reports that resulted from the Walkerton incident (the O’Connor Reports
2,3
) and SARS (the Walker,
4,5
Naylor,
6
and Campbell
7,8,9
reports) provided a range of recommendations for renewal of public health in
Canada and specifically in Ontario. In response, the government of Ontario announced Operation Health
Protection
10
in 2004. The Operation Health Protection (OHP) action plan focused on revitalizing the public
health sector, preventing future health threats, and promoting a healthy Ontario. The plan also included a
commitment to produce an annual Ontario public health performance report.
Ontario has made significant progress delivering on the commitments made in the OHP. Ontario’s continued
commitment to build a strong, flexible, and responsive public health sector has been demonstrated through
initiatives such as:
• amendingtheHealth Protection and Promotion Act (HPPA)
11
to modernize the legislation
• creatingtheOntarioAgencyforHealthProtectionandPromotion
• increasingprovincialfundingtopublichealthunits
• developingnewstandardsforpublichealth,whichstrengthenpublichealthsectoraccountability
Another outcome of OHP was the establishment of the Capacity Review Committee (CRC). The committee
was tasked with making recommendations to government on long-term strategies to revitalize public health
in Ontario. The committee delivered its final report in 2006, which included a recommendation to adopt a
comprehensive public health performance management system.
12
Public reporting was seen as an important
tool within this system to demonstrate accountability and measure performance.

2
Ontario has responded to the need to improve performance management in public health by initiating work
on the development of a public health performance management system. This system is intended to enable
the public health sector to demonstrate its achievements in terms of improvements in both outcomes and
services over time.
The introduction of the new performance management system is intended to move Ontario away from
focusing primarily on compliance with processes, towards an emphasis on tracking outcomes. As the
performance management system continues to be developed, improved measures of outcomes will follow.
This initial report provides a snapshot of Ontario’s public health sector. It provides an overview of the scope
of public health and profiles the local operational context of public health program and service delivery. It is a
first step in understanding the current work of public health and will inform the discussion as Ontario moves
towards a performance management system for public health.
This report also serves an important purpose in raising awareness of the vital role public health plays in
protecting the health of Ontarians and in contributing to the provincial health system as a whole.
Towards Performance Management
Ontario’s efforts to introduce a performance management framework for public health are being
informed by the Performance Management Working Group (PMWG).
Formed in 2007, PMWG members come from diverse backgrounds and include members of
the Council of Ontario Medical Officers of Health (COMOH), the Association of Public Health
Epidemiologists in Ontario (APHEO), Public Health Research, Education and Development (PHRED)
Program, the Association of Local Public Health Agencies (alPHa), and local public health units.
The group also includes representatives from the Ministry of Health and Long-Term Care, the Ministry
of Health Promotion and the Ministry of Children and Youth Services – the three ministries that share
responsibility for providing funding and policy direction to public health units. The group’s advice
has informed the development of this report as well as continuing to address the larger performance
management framework for public health.
Introduction

3
Initial Report on Public Health 2009
Overview of the Public Health Sector
Section II:
Scope of Public Health
The World Health Organization (WHO) defines public health as “a social and political concept aimed at
improving health, prolonging life and improving the quality of life among whole populations through health
promotion, disease prevention and other forms of health intervention.”
13
The WHO notes a distinction
between the traditional model of public health and an emerging concept of public health, which emphasizes:
• asignificantlydifferentunderstandingofhowlifestylesandlivingconditions(social,economicand
physical environments) determine health status
• theneedtomobilizeresourcesandmakesoundinvestmentsinpolicies,programsandserviceswhich
create, maintain and protect health
The public health sector has contributed to improving the health of Ontarians through initiatives such
as childhood immunizations, the control of infectious diseases, supporting parenting/early childhood
development, addressing oral health, ensuring safe water, education and inspections related to safe food
handling, the promotion of healthy sexuality, reproductive and child health, the prevention of injury, and the
prevention of chronic diseases through initiatives such as tobacco control and promotion of healthy eating.
Public health also contributes to the health of Ontarians by complementing the work of other parts of the
health care system. Through its work in addressing the determinants of health and reducing health risks to
the population, public health contributes to reducing the need for other health care services and limiting the
consequences of poor health including:
• theneedforacutemedicalcare
• long-termconsequencesofillnessandinjury,includingtheseverityandincidenceofdiseasesanddisability
• reducedincomeorlossofemployment
• prematuremortality
The public health system consists of governmental, non-governmental, and community organizations operating
at the local, provincial, and federal levels. However, the prime responsibility for program delivery in Ontario lies
with local boards of health, which comprise the public health sector. Provincial and federal level organizations
play an important role in setting policy, providing funding, issuing directives about specific programs, services
and situations, as well as coordination across jurisdictions.
There are exceptions to this indirect support of the provincial and federal governments, such as the work
of the Canadian Food Inspection Agency, which has the authority to take direct action at the community
level when necessary to protect the food supply. In addition, First Nations Band Councils and the federal
government have the responsibility for much of the delivery of public health programs on reserves.

4
In Ontario, the role of the provincial government is to:
• establishoverallstrategicdirectionandprovincialprioritiesforpublichealth
• developlegislation,regulations,standards,policies,anddirectivestosupportthosestrategicdirections
• monitorandreportontheperformanceofthepublichealthsectorandthehealthofOntarianswithregard
to public health issues
• establishfundingmodelsandlevelsoffundingforpublichealthservicedelivery
• ensurethatministry,publichealthsectorandhealthcaresystemstrategicdirectionsandexpectations
are met
Ontarians are served by 36 local boards of health that collectively cover the entire province and are individually
responsible for serving the population within their geographic borders. Approximately two-thirds of Ontario’s
boards of health are autonomous bodies created to provide public health services in their jurisdictions. For the
remainder, municipal or regional councils act as the board of health.
All boards of health in Ontario and their staff:
• havethesamestatutoryresponsibilitiesundertheHPPAfordeliveringpublichealthprogramsand
services within their communities
• mustcomplywithoverfiftyactsandregulations
• mustdeliverthesamecoresetofservicesaccordingtotheOntarioPublicHealthStandards
14
(OPHS);
local service delivery models vary based on community need, geography and other local factors
• deliverotheroptionalprogramming,withfundingfromavarietyofsources,toaddresslocalcommunity
needs and priorities
Within this document, the term “board of health” has the meaning assigned to it in Section 1 of the HPPA, and
refers to either the legal entities that provide public health programs and services within a specific geographic
region or to the governing body of the organization, depending on the context. The term “public health unit”
is used to refer to the staff complement of the organization who deliver the programs and services, which is
usually headed by a medical officer of health or by a shared leadership model of a medical officer of health
and a chief executive officer.
Legislative Framework for Public Health
Ontario’s HPPA provides the legislative mandate for boards of health. The guiding purpose of the HPPA is
to “provide for the organization and delivery of public health programs and services, the prevention of the
spread of disease and the promotion and protection of the health of the people of Ontario.”
11
Part II, Section 5 of the HPPA specifies that boards of health must provide or ensure the provision of specific
public health programs and services. The OPHS are published by the Minister of Health and Long-Term Care
under his/her authority in Section 7 of the HPPA and specify the minimum mandatory programs and services
with which all boards of health must comply.
Overview of the Public Health Sector

5
Initial Report on Public Health 2009
Determinants of Health
The health of individuals and communities is significantly influenced by complex interactions between social
and economic factors, the physical environment, and individual behaviours and living conditions. These factors
are referred to as the determinants of health, and together they play a key role in determining the health status
of the population as a whole. Determinants of health include the following:
• incomeandsocialstatus
• socialsupportnetworks
• educationandliteracy
• employment/workingconditions
• socialandphysicalenvironments
• personalhealthpracticesandcopingskills
• healthychilddevelopment
• biologyandgeneticendowment
• healthservices
• gender
• culture
• language
Public health works to address the determinants of health as the underlying causes of health inequities. This
approach is reinforced in the OPHS, which require the following types of activities by public health units:
• identificationofprioritypopulations
• adaptingprogramsandservicedeliverytomeetlocallyidentifiedpriorityneeds
• assessmentandsharinginformationofhealthinequities
• raisingawarenesswithcommunitydecisionmakersandpartners
These actions will foster more comprehensive solutions that will help improve the immediate and long-term
health of Ontarians. The OPHS incorporate and address the determinants of health, and identify a broad
range of population-based activities designed to promote health and reduce health inequities by working
with community partners.

6
Public Health Programs and Services in Ontario
In addition to delivering programs and services to meet local contexts and situations, the scope of public
health programs and services, as articulated in the OPHS, encompasses:
Chronic Diseases and Injuries: Chronic Disease Prevention
Prevention of Injury and Substance Misuse
Family Health: Reproductive Health
Child Health
Infectious Diseases: Infectious Diseases Prevention and Control
Rabies Prevention and Control
Tuberculosis Prevention and Control
Sexual Health, Sexually Transmitted Infections,
and Blood-borne infections (including HIV)
Vaccine Preventable Diseases
Environmental Health: Food Safety
Safe Water
Health Hazard Prevention and Management
Emergency Preparedness: Public Health Emergency Preparedness
Health Unit Profiles
Each of Ontario’s 36 public health units must respond to unique demographics, social conditions and
health needs within their community. The health unit profile information shown in Table 1: Health Unit
Profiles describes the local service delivery environment for each public health unit in Ontario. The table
provides context for the indicator data included in Section IV of the report. Each of the variables in the table
underscores the fact that the delivery of public health programs and services in Ontario occurs in significantly
different, multi-faceted and complex physical, cultural, social and economic environments.
For each variable, the provincial totals or averages, the minimum value, and the maximum value are shown.
The Table is organized to show the public health units according to their peer groups. A peer group is a
cluster of public health units, identified by Statistics Canada
15
as having similar social, demographic and
economic characteristics. Appendix 1 provides additional information on the definitions of peer groups.
Appendix 2 provides information on the variable definitions and data sources.
Overview of the Public Health Sector

7
Initial Report on Public Health 2009

8
% Francophone
Population
2.3%
48.2%
42.0%
1.1%
1.0%
1.2%
1.3%
0.8%
3.7%
1.2%
0.6%
5.6%
2.7%
7.4%
18.4%
26.8%
4.2%
25.2%
4.4%
0.6%
48.2%
Size of Birth Cohort
(2007)
973
1,063
2,015
1,091
1,356
1,008
1,369
569
1,434
1,214
862
1,020
4,910
1,028
1,058
1,849
1,530
297
151,304
297
31,581
% with Post Secondary
Education
49.2%
51.8%
51.1%
50.0%
53.4%
52.2%
53.1%
48.7%
57.5%
49.5%
49.4%
51.7%
55.9%
56.1%
56.3%
58.1%
57.2%
52.5%
61.4%
48.7%
71.6%
%Personsunder18years
of age in Low Income
Households (after tax)
6.5%
10.8%
9.1%
7.4%
7.0%
7.4%
8.8%
5.8%
6.8%
5.8%
5.7%
7.6%
7.4%
13.1%
11.6%
11.0%
11.3%
8.6%
13.7%
5.7%
25.4%
Housing Affordability
16.9%
19.7%
23.7%
22.2%
22.8%
21.9%
22.9%
19.4%
22.5%
20.4%
20.2%
19.4%
26.1%
19.7%
25.3%
20.9%
19.9%
19.6%
27.7%
16.9%
36.5%
Employment Rate
60%
57%
61%
64%
61%
62%
57%
65%
60%
66%
70%
58%
64%
52%
55%
57%
58%
54%
63%
52%
70%
# First Nations
39
10
1
0
2
0
1
0
0
0
0
1
4
8
6
13
25
2
127
0
39
% Immigrants
5.5%
3.2%
6.0%
13.2%
8.4%
11.1%
9.6%
8.0%
7.6%
10.9%
9.4%
6.2%
11.8%
9.7%
5.8%
6.2%
9.3%
4.1%
28.3%
3.2%
50.0%
Population Density (km
2
)
(2007)
0.5
0.3
37.5
48.3
18.9
39.1
19.5
18.1
26.9
52.3
34.8
6.7
56.6
2.7
7.5
4.3
0.7
2.4
14.1
0.3
4,207.9
Population Growth Rate
(2002-2007)
-3.2%
-4.5%
1.5%
6.2%
1.2%
2.2%
3.4%
-1.0%
2.1%
2.9%
0.3%
0.2%
8.0%
-1.8%
0.1%
0.4%
-3.5%
-4.4%
5.8%
-4.5%
20.8%
Population (2007)
80,042
87,305
199,227
90,758
161,896
111,684
175,187
61,373
170,205
106,574
77,156
100,468
494,081
119,121
125,383
198,265
155,079
34,564
12,803,861
34,564
2,651,717
Size of Region (km
2
)
171,288
266,291
5,308
1,881
8,586
2,858
8,988
3,397
6,329
2,039
2,218
14,980
8,731
44,308
16,802
46,475
235,531
14,125
907,574
630
266,291
Variable
Public Health Unit
Northwestern Health Unit
Porcupine Health Unit
The Eastern Ontario
Health Unit
Elgin-St. Thomas Health Unit
Grey Bruce Health Unit
Haldimand-Norfolk
Health Unit
Haliburton, Kawartha, Pine
Ridge District Health Unit
Huron County Health Unit
Leeds, Grenville and
Lanark District Health Unit
Oxford County Health Unit
Perth District Health Unit
Renfrew County and District
Health Unit
Simcoe Muskoka District
Health Unit
The District of Algoma
Health Unit
North Bay Parry Sound
District Health Unit
Sudbury and District
Health Unit
Thunder Bay District
Health Unit
Timiskaming Health Unit
Ontario
Ontario Total
Ontario Minimum
Ontario Maximum
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
Peer Group
Rural
Northern
Regions
Mainly Rural
Sparsely Populated
Urban-Rural Mix
Table 1: Health Unit Profiles
Overview of the Public Health Sector

9
Initial Report on Public Health 2009
Board of Health
Governance Model
Autonomous
Autonomous
Autonomous
Autonomous
Autonomous
Single-Tier
Autonomous
Autonomous/
Integrated
Autonomous
Regional
Autonomous
Autonomous
Autonomous
Autonomous
Autonomous
Autonomous
Autonomous
Autonomous
# Municipalities
19
13
15
8
17
2
12
9
22
8
6
18
24
22
31
19
15
24
413
1
31
# Small Drinking Water
Systems(2008)
1,196
369
660
110
1,304
344
924
256
825
216
398
719
1,483
649
999
790
791
225
17,879
0
1,483
# School Boards
4
9
4
2
3
2
4
2
3
3
2
7
6
4
5
10
6
4
154
2
10
# Schools
48
75
136
36
69
55
77
34
84
53
37
61
209
86
79
129
86
29
4,927
29
808
# Personal Service
Settings (estimated)
95
186
343
82
281
148
256
103
227
121
104
137
610
374
178
350
223
54
18,560
54
3,469
# Licenced Day Nurseries
53
28
61
12
71
24
71
12
69
33
25
25
142
53
57
98
45
21
4,620
12
924
# Hospital Sites
8
11
4
1
11
3
5
5
9
3
3
5
7
6
5
8
6
3
209
1
21
# Long-term Care Homes
12
13
18
8
30
10
20
9
14
19
10
14
29
12
11
11
15
8
777
7
86
# Food Premises (2006)
512
641
973
552
1,567
954
1,636
443
1,253
603
450
798
3,782
880
968
1,286
1,737
404
76,163
404
13,367
Cost of Nutritious Food
Basket for a Family of
Four(2008)
$176
$157
$144
$140
$145
$134
$141
$139
$138
$136
$137
$141
$134
$144
*
$141
$157
$143
$141
$130
$176
% Speaking neither
English nor French
0.7%
0.3%
0.2%
0.9%
0.3%
0.5%
0.1%
0.7%
0.1%
0.4%
0.7%
0.1%
0.3%
0.4%
0.1%
0.2%
0.6%
0.0%
2.2%
0.0%
5.3%
Variable
Public Health Unit
Northwestern Health Unit
Porcupine Health Unit
The Eastern Ontario
Health Unit
Elgin-St. Thomas Health Unit
Grey Bruce Health Unit
Haldimand-Norfolk
Health Unit
Haliburton, Kawartha, Pine
Ridge District Health Unit
Huron County Health Unit
Leeds, Grenville and
Lanark District Health Unit
Oxford County Health Unit
Perth District Health Unit
Renfrew County and District
Health Unit
Simcoe Muskoka District
Health Unit
The District of Algoma
Health Unit
North Bay Parry Sound
District Health Unit
Sudbury and District
Health Unit
Thunder Bay District
Health Unit
Timiskaming Health Unit
Ontario
Ontario Total
Ontario Minimum
Ontario Maximum
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
Peer Group
Rural
Northern
Regions
Mainly Rural
Sparsely Populated
Urban-Rural Mix
Table 1: Health Unit Profiles (cont’d)
* Health Unit did not have a Registered Dietitian in 2008 and therefore data is unavailable. The 2007 amount was $130.65.

10
% Francophone
Population
1.2%
3.0%
1.5%
2.4%
2.9%
2.5%
1.6%
3.6%
1.3%
2.0%
2.1%
18.6%
1.3%
1.5%
1.3%
3.6%
1.1%
1.5%
4.4%
0.6%
48.2%
Size of Birth Cohort
(2007)
1,444
1,165
5,416
1,582
1,763
1,191
4,858
3,906
1,188
6,352
5,645
9,245
16,345
6,077
2,891
4,370
10,837
31,581
151,304
297
31,581
% with Post Secondary
Education
52.1%
49.0%
58.1%
52.5%
61.8%
58.1%
61.5%
56.1%
58.3%
60.1%
69.3%
71.6%
62.9%
58.1%
57.4%
55.4%
67.1%
66.4%
61.4%
48.7%
71.6%
%Personsunder18years
of age in Low Income
Households (after tax)
12.1%
10.1%
18.6%
10.2%
9.5%
7.8%
12.5%
10.5%
9.7%
8.9%
7.8%
15.2%
14.5%
9.1%
6.7%
12.2%
11.5%
25.4%
13.7%
5.7%
25.4%
Housing Affordability
23.4%
22.3%
27.4%
24.2%
26.3%
19.1%
25.8%
25.4%
26.8%
25.9%
23.3%
24.4%
32.0%
23.1%
24.1%
23.7%
29.7%
36.5%
27.7%
16.9%
36.5%
Employment Rate
64%
61%
60%
58%
60%
60%
63%
61%
58%
67%
69%
65%
67%
68%
69%
60%
67%
60%
63%
52%
70%
# First Nations
2
2
0
1
0
3
3
0
2
1
0
0
0
0
0
0
1
0
127
0
39
% Immigrants
12.9%
10.1%
25.4%
8.2%
11.4%
11.6%
20.0%
18.0%
9.5%
20.3%
24.8%
22.3%
48.6%
22.3%
16.1%
22.4%
42.9%
50.0%
28.3%
3.2%
50.0%
Population Density (km
2
)
(2007)
121.3
44.4
465.2
23.2
29.1
44.1
132.2
234.0
35.1
236.0
484.9
304.6
1,043.9
362.7
64.1
218.1
553.9
4,207.9
14.1
0.3
4,207.9
Population Growth Rate
(2002-2007)
4.6%
-1.3%
1.0%
2.2%
0.4%
0.0%
2.9%
1.2%
1.4%
10.7%
16.5%
3.5%
19.7%
7.0%
5.6%
1.8%
20.8%
1.3%
5.8%
-4.5%
20.8%
Population (2007)
136,865
109,612
519,741
163,120
187,843
132,228
438,438
433,946
133,583
595,354
468,980
846,169
1,296,505
496,370
265,319
403,797
975,906
2,651,717
12,803,861
34,564
2,651,717
Size of Region (km
2
)
1,129
2,471
1,117
7,028
6,449
3,002
3,317
1,854
3,806
2,523
967
2,778
1,242
1,369
4,142
1,851
1,762
630
907,574
630
266,291
Variable
Public Health Unit
Brant County Health Unit
Chatham-Kent Health Unit
City of Hamilton Health Unit
Hastings and Prince Edward
Counties Health Unit
Kingston, Frontenac and
Lennox and Addington
Health Unit
Lambton Health Unit
Middlesex-London
Health Unit
Niagara Regional Area
Health Unit
Peterborough County-City
Health Unit
Durham Regional Health Unit
Halton Regional Health Unit
City of Ottawa Health Unit
Peel Regional Health Unit
Waterloo Health Unit
Wellington-Dufferin-Guelph
Health Unit
Windsor-Essex County
Health Unit
York Regional Health Unit
City of Toronto Health Unit
Ontario
Ontario Total
Ontario Minimum
Ontario Maximum
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
Peer Group
Urban/Rural MixUrban Centres
Metro
Centre
Table 1: Health Unit Profiles (cont’d)
Overview of the Public Health Sector

11
Initial Report on Public Health 2009
Table 1: Health Unit Profiles (cont’d)
Board of Health
Governance Model
Autonomous
Autonomous/
Integrated
Single-Tier
Autonomous
Autonomous
Autonomous/
Integrated
Autonomous
Regional
Autonomous
Regional
Regional
Single-Tier
Regional
Regional
Autonomous
Autonomous
Regional
Semi-
Autonomous
# Municipalities
2
1
1
17
9
11
9
12
9
8
4
1
3
7
16
9
9
1
413
1
31
# Small Drinking Water
Systems(2008)
114
94
246
580
805
64
507
294
494
395
261
476
130
148
393
61
559
0
17,879
0
1,483
# School Boards
3
3
4
5
4
4
4
4
4
6
4
4
4
4
5
4
4
4
154
2
10
# Schools
64
50
184
78
92
60
164
196
55
214
147
306
386
173
97
171
299
808
4,927
29
808
# Personal Service
Settings (estimated)
200
189
717
204
286
140
550
700
287
646
516
1,100
1,200
707
327
500
2,950
3,469
18,560
54
3,469
# Licenced Day Nurseries
30
48
204
65
95
51
133
154
50
169
250
326
433
123
77
163
425
924
4,620
12
924
# Hospital Sites
2
3
8
5
4
3
8
10
1
6
4
10
3
3
8
3
4
21
209
1
21
# Long-term Care Homes
7
8
29
26
11
10
18
46
17
26
18
40
36
33
30
24
49
86
777
7
86
# Food Premises (2006)
786
808
2,988
1,265
1,100
640
2,714
2,655
704
3,349
2,655
5,723
5,013
2,175
1,460
2,455
6,867
13,367
76,163
404
13,367
Cost of Nutritious Food
Basket for a Family of
Four(2008)
$149
$138
$136
$137
$142
$135
$139
$135
$145
$141
$133
$140
$130
$141
$149
$135
$143
$136
$141
$130
$176
% Speaking neither
English nor French
0.4%
0.5%
1.7%
0.2%
0.3%
0.2%
1.1%
0.6%
0.1%
0.5%
0.8%
1.3%
3.7%
1.5%
0.8%
1.7%
4.0%
5.3%
2.2%
0.0%
5.3%
Variable
Public Health Unit
Brant County Health Unit
Chatham-Kent Health Unit
City of Hamilton Health Unit
Hastings and Prince Edward
Counties Health Unit
Kingston, Frontenac and
Lennox and Addington
Health Unit
Lambton Health Unit
Middlesex-London
Health Unit
Niagara Regional Area
Health Unit
Peterborough County-City
Health Unit
Durham Regional Health Unit
Halton Regional Health Unit
City of Ottawa Health Unit
Peel Regional Health Unit
Waterloo Health Unit
Wellington-Dufferin-Guelph
Health Unit
Windsor-Essex County
Health Unit
York Regional Health Unit
City of Toronto Health Unit
Ontario
Ontario Total
Ontario Minimum
Ontario Maximum
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
Peer Group
Urban/Rural MixUrban Centres
Metro
Centre

12

13
Initial Report on Public Health 2009
Report Development
The process of developing this report began with careful consideration of how public reporting contributes
to performance management. Meeting the longer term objective of publishing provincial performance reports
reflective of the public health mandate will require time and resources to develop new measures of program
outcomes and to address data collection issues.
While this report is not intended as a performance report, it does provide a status update on a range of
indicators related to public health practice. Over time, as new data sources and indicators are developed,
these basic indicators may be replaced by more appropriate measures. The development of this report was
informed by the decision to avoid trying to directly link the indicators to the standards in the OPHS, which
were released during the report’s development. This decision was made because it was seen as inappropriate
to begin to publicly report on local public health performance until public health units have had time to adapt
to the new standards and begin measuring their impact at the outcome level. These outcome level measures
will need to be identified and developed as this public health performance management work continues.
In presenting the scope of public health in Ontario at both the provincial and local levels, an important
consideration was to use reliable data that could be presented at the health unit level. The selection of
indicators, therefore, was contingent upon the availability of reliable and comprehensive data. During the
indicator selection process a wide range of indicators, other than those presented, were considered for
inclusion but were not selected for a variety of reasons, including unavailability of consistent and reliable data.
To guide the selection of indicators for the report, several different frameworks, or approaches to
performance management indicator reporting were evaluated by the PMWG, including:
• balancedscorecardapproach
• strategymappingapproach
• attributesofahighperformingsystem
Through discussion and research on the use of these frameworks in other sectors and other jurisdictions, it
was determined that each of these approaches has merits and limitations when applied to the public health
sector in Ontario.
Balanced Scorecard Approach
The Balanced Scorecard, as developed by ICES for public health, identifies four quadrants:
1) Health Determinants and Status, 2) Community Engagement, 3) Resources and Services,
4) Integration and Responsiveness for the reporting of information on a system or organization.
16
Several public health units have used the Balanced Scorecard approach for local public reporting in the recent
past. However, the lack of consistent and available data for all health units for two of the four quadrants
(Community Engagement, and Integration and Responsiveness) would compromise the usefulness of this tool
for provincial reporting at this time.
Performance of the Public Health Sector
Section III:

14
Strategy Mapping Approach
A strategy mapping approach was explored as a framework to guide measurement of performance in public
health. This approach was helpful in understanding the strategic components of public health, but was found
to be too high level for use as a framework for this report.
Attributes of a High Performing System
Determining the “attributes of a high performing system” that could be used in relation to the public health
sector was approached by first researching the performance dimensions used in other jurisdictions and in
other health care sector reports. Through discussion with the PMWG, the following five key dimensions were
identified as appropriate for capturing the key aspects of Ontario’s public health sector.
1) Effectiveness
2) Capacity
3) Equitable
4) Community Partnership
5) Effectively Governed and Managed
Each of these approaches provides an organized way of presenting performance information. The PMWG
determined that any one of these performance reporting approaches could be used as part of the process for
selecting potential indicators. In fact, an exercise was completed which showed that the indicators that were
available for use at this time could be mapped into all of the above frameworks. This shows that the different
frameworks have significant conceptual overlap, and any one of them could be used to assess public health
performance.
As the report development process continued, it was determined that focussing on performance reporting
at this time was inappropriate, due mainly to the lack of performance related indicators and consistent
data to support them, and because of the early stage of development of the new approach to performance
management within the public health sector.
While the work of developing the report and the selection of indicators was informed by the earlier work on
performance reporting frameworks, a decision was made to not use any specific reporting framework for this
report.
Performance of the Public Health Sector

15
Initial Report on Public Health 2009
Development of Indicators
Indicators used in existing reports on public health and population health were considered as part of the
context for informing Ontario’s public health reporting. These existing reports included:
• Q Monitor: 2008 Report on Ontario’s Health System(OntarioHealthQualityCouncil)
17
• Ontario Health System Scorecard 2007/08 (Ministry of Health and Long-Term Care)
18
• Healthy Canadians: A Federal Report on Comparable Health Indicators 2006 (Health Canada)
19
• Report on the State of Public Health in Canada 2008 (Public Health Agency of Canada)
20
• Developing a Balanced Scorecard for Public Health (Institute for Clinical Evaluative Sciences)
16
• Towards Outcome Measurement (Public Health Research Education and Development Program)
21
Many public health units have also produced and will continue to produce, local health status reports or
performance reports, which may contain similar or related indicators with more analysis and interpretation
on the impact of these measures within their communities.
The indicators presented in this report are intended to complement and enhance our understanding of the
scope and impact of public health across Ontario, whereas many other health reports focus on information
about the impact of the health care system or the health of the general population.
A modified Delphi process was employed to select indicators for this report, using a number of rationales,
including:
• strategicpriorityforpublichealth
• providessector-levelinformation
• provideslocal-levelinformation
• theabilityofpublichealthtoinfluenceoutcomesinthisarea
• whethertheindicatorrelatestomultipleprogramareas
Selection criteria that were used to determine the final set of indicators required that each indicator be:
• relevant,feasible,andscientificallysound
• supportedbycurrentlyavailabledatathatcouldbereportedatthehealthunitlevel
• partofasetwhichreflectsthescopeofpublichealthpractice
• meaningfulindescribingthescopeofpublichealthatboththeprovincialandlocallevels
This report will allow local public health officials and other stakeholders to consider how a board of health is
currently providing programs and services alongside of its peers. But this is only a starting point which also
requires an understanding of local context and conditions, which must be taken into account. It is expected
that public reporting will evolve as performance management in public health develops, consistent with the
OPHS and Protocols, and that this will drive the development of better indicators and new data sources.

16
Case Studies
Throughout the report, examples of public health initiatives that are currently in place at the local level have
been included as case studies. The case studies provide additional context to the work of the public health
sector in Ontario.
Case study submissions were requested from public health units to showcase innovative or exciting local
practices. The case studies included in the report are drawn from among the large number of submissions
received from public health units. A full list of submissions can be found in the report’s webpage, at
www.health.gov.on.ca/english/public/pub/pubhealth/init_report/index.html.
While examples of local practice are attributed to specific public health units, please note that this does not
necessarily represent exclusive practice as other public health units may also deliver similar programs.
The case studies were selected to reflect a range of program areas, populations served, levels of interaction
and types of local practice. While the case studies are intended to complement the information in the report,
they do not relate directly to any specific indicators, particularly because they were selected as examples of
the work of public health that is not currently well represented in the available data. There is no association
between the indicators and the placement of the case studies.
i
i
The names of the public health units used in this section reflect locally used health unit names, and may differ from the legal names
used by the ministry, as shown in the data tables.
Performance of the Public Health Sector

17
Initial Report on Public Health 2009
Indicators
Section IV:
This section contains narratives for each of the 34 selected indicators. The narratives provide background and
contextual information on the importance of the indicator in public health practice and give specific examples
of the role of public health in relation to that indicator. There is some duplication of text for those indicators
which are closely related, particularly in terms of describing public health interventions. This structure was
chosen so that each indicator narrative would provide the same level of information when read independently.
The corresponding data for each indicator can be found in Table 2: Indicators by Public Health Unit and
information on indicator definitions, including sources and data limitations, can be found in Appendix 3.
The data were compiled from existing data sources, such as Statistics Canada or the ministry’s Integrated
Public Health Information System (iPHIS) system, with the exception of the governance and accountability
data, which were collected directly from public health units via a survey.
For each indicator, the provincial totals or averages, the minimum value, and the maximum value are shown.
The table is organized to show the public health units according to their peer groups, as described earlier in
the health unit profile section.
Group A – Population Health Indicators
1. Teen Pregnancy
2. Low Birth Weight
3. Breastfeeding Duration
4. Postpartum Contact
5. Smoking Prevalence
6. Youth Lifetime Smoking Abstinence
7. Adult Heavy Drinking
8. YouthHeavyDrinking
9. Physical Activity Index
10. Healthy Body Mass Index
11. Fruit and Vegetable Consumption
12. Fall-Related Hospitalizations among Seniors
13. Enteric Illnesses Incidence
14. Respiratory Infection Outbreaks in Long-Term Care Homes
15. Chlamydia Incidence
16. Immunization Coverage for Hepatitis B
17. Immunization Coverage for Measles, Mumps and Rubella
18. AdverseWaterQualityIncidents

18
Group B – Governance and Accountability Indicators
19. Total Board of Health Expenditures
20. Board of Health Expenditure Variance
21. Expenditures on Training and Professional Development
22. Number of FTEs by Job Category
23. Number of Vacant Positions by Job Category
24. Employment Status of Medical Officers of Health
25. Staff Length of Service
26. Familiarity with Public Health Unit Programs and Services
27. Issuance of a Health Status Report
28. StrategicPlan
29. Emergency Response Plan Tested
30. Accreditation Status
31. Medical Officer of Health Performance Evaluation
32. Medical Officer of Health Reporting Relationships
33. Board Member Orientation
34. Board Self-Evaluation
Indicators

19
Initial Report on Public Health 2009
20
Notes:
* Ontario value is not provided
†
Note that an amalgamation occurred in these health units during the period for which data is shown
E
Warning of high variability associated with estimates
F
Estimates of unreliable quality and could not be reported
Table 2: Indicators by Public Health Unit
Population Health Indicators
Physical activity index
(percent)
56%
51%
57%
53%
52%
49%
55%
52%
58%
44%
48%
51%
57%
52%
54%
55%
52%
49%
50%
43%
64%
Youth heavy drinking
(percent)
34%
E
51%
34%
E
45%
27%
E
46%
E
33%
E
F
35%
E
45%
E
F
25%
E
34%
E
34%
65%
44%
18%
E
F
25%
12%
E
65%
Adult heavy drinking
(percent)
48%
49%
45%
36%
54%
48%
46%
43%
50%
42%
41%
43%
49%
48%
43%
47%
51%
50%
37%
24%
54%
Youth lifetime smoking
abstinence (percent)
69%
48%
E
75%
67%
E
77%
74%
56%
E
81%
70%
70%
91%
80%
80%
79%
62%
E
62%
85%
81%
E
81%
48%
E
92%
Smoking prevalence
(percent)
25%
E
28%
24%
29%
26%
28%
27%
23%
29%
34%
18%
30%
24%
29%
30%
29%
29%
25%
*
16%
34%
Postpartum contact
(percent)
94.2%
86.8%
88.4%
89.4%
83.6%
73.8%
83.4%
77.2%
92.0%
93.7%
80.2%
85.3%
92.7%
89.3%
90.3%
95.0%
87.5%
75.4%
80.8%
58.2%
95.8%
Breastfeeding duration
(percent)
48%
E
33%
E
35%
44%
E
53%
49%
E
43%
45%
E
54%
53%
39%
E
31%
E
50%
†
46%
E
45%
†E
38%
44%
F
50%
31%
E
65%
Low birth weight (rate)
20.9
33.9
36.7
49.0
39.2
40.7
36.3
46.6
36.2
42.2
35.8
41.2
41.0
51.8
30.9
41.1
41.5
41.8
47.9
20.9
67.5
Teen pregnancy (rate)
60.8
53.1
32.5
28.2
26.4
22.8
30.6
22.1
25.3
33.5
23.8
29.0
26.8
42.5
31.4
32.6
44.6
42.6
25.7
9.5
60.8
Indicator
Public Health Unit
Northwestern Health Unit
Porcupine Health Unit
The Eastern Ontario
Health Unit
Elgin-St. Thomas Health Unit
Grey Bruce Health Unit
Haldimand-Norfolk
Health Unit
Haliburton, Kawartha, Pine
Ridge District Health Unit
Huron County Health Unit
Leeds, Grenville and
Lanark District Health Unit
Oxford County Health Unit
Perth District Health Unit
Renfrew County and District
Health Unit
Simcoe Muskoka District
Health Unit
The District of Algoma
Health Unit
North Bay Parry Sound
District Health Unit
Sudbury and District
Health Unit
Thunder Bay District
Health Unit
Timiskaming Health Unit
Ontario
Ontario Total
Ontario Minimum
Ontario Maximum
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
Peer Group
Rural
Northern
Regions
Mainly Rural
Sparsely Populated
Urban-Rural Mix
Indicators

21
Initial Report on Public Health 2009
Notes:
* Ontario value is not provided
†
Note that an amalgamation occurred in these health units during the period for which data is shown
E
Warning of high variability associated with estimates
F
Estimates of unreliable quality and could not be reported
Table 2: Indicators by Public Health Unit (cont’d)
Population Health Indicators
Adverse water quality
incidents (number)
207
86
172
35
234
101
202
165
153
81
30
179
446
138
210
217
157
43
4,458
13
446
Immunization coverage
for Measles, Mumps and
Rubella (percent)
95.7%
97.8%
82.4%
97.2%
95.6%
20.7%
95.6%
95.4%
52.2%
89.3%
96.0%
86.4%
44.2%
94.6%
67.8%
93.8%
97.4%
96.8%
84.9%
20.7%
97.8%
Immunization coverage
for Hepatitis B (percent)
88.3%
86.8%
78.6%
67.9%
90.7%
78.3%
75.1%
87.1%
74.0%
81.2%
85.3%
76.9%
70.9%
89.0%
79.6%
77.7%
88.4%
73.6%
79.8%
65.2%
95.2%
Chlamydia incidence
(rate)
678.9
303.2
99.7
101.6
159.1
102.3
159.6
78.9
122.8
126.4
138.9
149.0
169.9
276.9
238.3
292.6
388.3
203.5
219.8
78.9
678.9
Respiratory infection
outbreaks in LTC homes
(number)
0
3
23
8
14
1
10
8
8
9
13
4
17
0
16
9
0
8
602
0
113
Enteric illnesses
incidence (rate)
47.3
41.3
78.3
51.9
119.7
89.7
84.5
164.1
56.2
72.6
150.5
75.8
64.4
46.1
48.4
40.0
44.1
64.1
88.7
40.0
164.1
Fall-related
hospitalizations among
seniors (rate)
2,053.8
1,619.6
1,596.1
1,335.7
1,792.5
1,641.2
1,445.7
2,030.7
1,618.9
1,850.3
1,493.1
2,371.5
1,581.6
1,576.8
1,741.6
1,571.9
1,663.4
2,022.3
1,309.5
942.6
2,371.5
Fruit and vegetable
consumption (percent)
36%
41%
44%
42%
47%
41%
38%
48%
40%
39%
46%
36%
41%
34%
45%
45%
38%
45%
42%
29%
50%
Healthy body mass
index (percent)
33%
E
39%
38%
51%
39%
42%
38%
38%
48%
42%
38%
35%
42%
38%
44%
43%
45%
36%
47%
33%
E
55%
Indicator
Public Health Unit
Northwestern Health Unit
Porcupine Health Unit
The Eastern Ontario
Health Unit
Elgin-St. Thomas Health Unit
Grey Bruce Health Unit
Haldimand-Norfolk
Health Unit
Haliburton, Kawartha, Pine
Ridge District Health Unit
Huron County Health Unit
Leeds, Grenville and
Lanark District Health Unit
Oxford County Health Unit
Perth District Health Unit
Renfrew County and District
Health Unit
Simcoe Muskoka District
Health Unit
The District of Algoma
Health Unit
North Bay Parry Sound
District Health Unit
Sudbury and District
Health Unit
Thunder Bay District
Health Unit
Timiskaming Health Unit
Ontario
Ontario Total
Ontario Minimum
Ontario Maximum
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
Peer Group
Rural
Northern
Regions
Mainly Rural
Sparsely Populated
Urban-Rural Mix
Initial Report on Public Health 2009

22
Table 2: Indicators by Public Health Unit (cont’d)
Governance and Accountability Indicators
Number of FTEs by job category
Librarian
1.0
0.0
1.0
0.0
0.0
0.0
0.0
0.0
0.0
0.0
0.0
0.0
0.6
0.0
0.0
1.0
1.0
0.0
20.1
0.0
4.0
Heart Health Coordinator
1.0
1.0
1.0
0.0
0.0
1.0
1.0
1.0
1.0
1.0
1.0
0.0
2.0
1.0
1.0
1.0
1.0
1.0
29.0
0.0
2.0
Epidemiologist
2.0
1.0
1.5
1.0
1.5
1.0
1.0
1.0
1.0
1.0
1.0
0.8
2.0
0.3
1.0
2.0
1.0
1.0
72.6
0.0
11.0
Speech – Language
Pathologist
4.0
6.0
9.6
0.0
0.0
3.7
0.0
0.0
5.0
0.0
0.0
0.0
0.0
2.8
0.0
0.0
6.2
2.0
64.3
0.0
15.2
Dietitian/Nutritionist
2.0
4.0
7.0
2.0
1.0
2.5
5.0
0.5
3.0
1.4
2.6
1.0
6.0
2.0
2.8
7.9
2.5
1.0
203.1
0.5
64.5
Health Promoter
5.0
2.0
21.7
3.0
1.3
6.5
14.0
3.0
0.0
1.0
6.2
3.0
7.0
1.0
6.0
8.0
3.0
6.4
416.7
0.0
123.4
Dental Hygienist/
Dental Assistant
6.0
4.0
0.9
1.4
3.0
1.3
5.0
0.7
3.7
2.7
2.0
1.3
13.9
6.7
5.4
6.0
2.4
1.5
286.4
0.7
86.7
Dentist
0.3
0.0
0.1
0.2
0.0
0.3
0.0
0.0
0.1
0.3
0.0
0.3
0.4
0.3
0.0
0.0
0.0
0.1
54.9
0.0
32.0
Public Health Inspector
5.0
12.0
7.0
8.0
16.0
10.5
23.0
7.0
18.1
10.5
7.2
8.2
33.5
10.6
15.0
25.0
13.0
4.2
900.5
4.2
202.8
Nurse Practitioner
0.0
2.0
0.0
0.0
0.0
2.0
0.0
1.0
0.0
1.0
0.0
0.0
2.0
2.2
0.0
2.5
1.0
1.0
28.5
0.0
4.0
Registered Practical Nurse
1.0
0.0
1.4
0.0
2.0
0.0
1.0
0.0
1.0
0.0
0.0
2.0
8.9
2.6
0.0
0.0
2.0
0.0
100.3
0.0
41.4
Registered Nurse
0.0
9.0
0.0
0.5
2.0
1.9
5.0
2.8
1.0
1.0
0.8
1.0
4.5
2.5
3.8
1.1
6.9
2.0
180.1
0.0
36.0
Public Health Nurse
33.3
38.0
47.7
25.0
39.3
18.8
25.0
14.0
43.4
37.2
31.3
23.1
82.9
48.0
41.8
86.4
47.5
16.4
2,717.2
14.0
536.9
Expenditures on training and
professional development
(percent)
0.7%
0.8%
0.6%
0.6%
0.3%
0.9%
0.5%
0.9%
0.3%
0.5%
0.7%
0.7%
0.4%
0.8%
0.3%
1.6%
0.9%
1.3%
0.7%
0.1%
1.7%
BoH expenditure variance
(percent)
4.0%
-6.2%
-1.7%
-6.4%
-1.2%
-7.5%
-1.6%
-2.8%
-2.0%
-10.9%
-2.3%
-20.8%
-1.2%
0.0%
-4.5%
-1.9%
-2.5%
-1.8%
-3.3%
-20.8%
6.3%
Total BoH expenditures ($M)
13.0
10.7
14.1
6.4
10.8
7.0
15.1
6.2
10.5
6.8
6.6
6.2
28.8
16.6
14.3
15.8
15.7
5.7
837.7
5.7
193.6
Indicator
Public Health Unit
Northwestern Health Unit
Porcupine Health Unit
The Eastern Ontario
Health Unit
Elgin-St. Thomas Health Unit
Grey Bruce Health Unit
Haldimand-Norfolk
Health Unit
Haliburton, Kawartha, Pine
Ridge District Health Unit
Huron County Health Unit
Leeds, Grenville and
Lanark District Health Unit
Oxford County Health Unit
Perth District Health Unit
Renfrew County and District
Health Unit
Simcoe Muskoka District
Health Unit
The District of Algoma
Health Unit
North Bay Parry Sound
District Health Unit
Sudbury and District
Health Unit
Thunder Bay District
Health Unit
Timiskaming Health Unit
Ontario
Ontario Total
Ontario Minimum
Ontario Maximum
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
Peer Group
Rural
Northern
Regions
Mainly Rural
Sparsely Populated
Urban-Rural Mix
Indicators

23
Initial Report on Public Health 2009
Table 2: Indicators by Public Health Unit (cont’d)
Governance and Accountability Indicators
Board self-evaluation (year)
2003
n/a
2008
n/a
2006
n/a
n/a
n/a
n/a
n/a
n/a
n/a
n/a
n/a
n/a
2005
2008
n/a
12/36
=Yes
2003
2008
Board member orientation
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes
35/36
=Yes
MOH reporting
relationships
MOH reporting to standing
committee (proportion)
5/8
6/8
–
–
–
4/8
–
–
–
–
2/2
–
3/3
–
16/16
–
–
–
MOH reporting to the BoH
(proportion)
13/14
7/9
13/13
9/9
13/13
4/11
10/10
12/12
9/10
16/16
10/12
7/7
10/10
10/10
8/8
9/9
10/10
9/9
MOH performance evaluation
Yes
Yes
Yes
Yes
Yes
–
No
Yes
Yes
No
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes
32/36
=Yes
Accreditation status
Yes
No
Yes
No
No
Yes
No
Yes
Yes
No
No
No
Yes
Yes
No
Yes
No
Yes
21/36
=Yes
Emergency response plan tested
Yes
Yes
Yes
No
Yes
Yes
Yes
Yes
Yes
No
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes
29/36
=Yes
Strategicplan(2008)
Yes
No
Yes
No
Yes
Yes
No
Yes
Yes
No
Yes
No
Yes
Yes
No
Yes
Yes
No
24/36
=Yes
Issuance of a health status report
(year)
2007
2006
2007
2006
2008
2008
2006
2007
2008
2008
2007
2007
2008
2006
2008
2008
2007
2008
2000
2008
Familiarity with public health unit
programs and services (year)
1998
2005
2007
2003
2005
No
2007
2008
2006
2008
2007
No
2007
2008
No
2006
2003
No
1998
2008
Proportion of staff
by length of service
>20 years
10%
16%
12%
9%
11%
19%
12%
5%
13%
19%
14%
18%
16%
16%
10%
11%
15%
17%
14%
5%
21%
>10 years <20 years
18%
10%
16%
24%
14%
11%
28%
7%
22%
9%
16%
31%
18%
22%
15%
15%
16%
18%
18%
7%
31%
>5 years <10 years
21%
27%
25%
20%
22%
23%
22%
25%
24%
36%
28%
16%
31%
28%
29%
28%
35%
29%
28%
16%
38%
>1 year <5 years
41%
43%
39%
35%
43%
37%
26%
43%
28%
19%
30%
19%
29%
29%
40%
34%
20%
34%
31%
19%
43%
Up to 1 year
9%
4%
8%
12%
10%
10%
11%
21%
13%
17%
12%
15%
6%
5%
6%
13%
14%
2%
9%
0%
21%
Employment status of MOH (FTE)
1.0
1.0
1.0
1.0
1.0
1.0
‡
1.0
1.0
1.0
0.5
0.3
1.0
1.0
1.0
1.0
1.0
1.0
1.0
34.2
0.3
1.0
Total number of vacant positions
2.0
5.0
3.2
0.0
2.0
3.0
3.0
3.0
1.0
1.5
0.0
4.0
0.0
1.0
3.0
3.4
0.0
2.5
103.4
0.0
27.0
Indicator
Public Health Unit
Northwestern Health Unit
Porcupine Health Unit
The Eastern Ontario
Health Unit
Elgin-St. Thomas Health Unit
Grey Bruce Health Unit
Haldimand-Norfolk
Health Unit
Haliburton, Kawartha, Pine
Ridge District Health Unit
Huron County Health Unit
Leeds, Grenville and
Lanark District Health Unit
Oxford County Health Unit
Perth District Health Unit
Renfrew County and District
Health Unit
Simcoe Muskoka District
Health Unit
The District of Algoma
Health Unit
North Bay Parry Sound
District Health Unit
Sudbury and District
Health Unit
Thunder Bay District
Health Unit
Timiskaming Health Unit
Ontario
Ontario Total
Ontario Minimum
Ontario Maximum
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
Peer Group
Rural
Northern
Regions
Mainly Rural
Sparsely Populated
Urban-Rural Mix

24
Table 2: Indicators by Public Health Unit (cont’d)
Population Health Indicators
Physical activity index
(percent)
50%
47%
52%
58%
55%
51%
52%
58%
64%
52%
56%
59%
47%
48%
62%
50%
46%
43%
50%
43%
64%
Youth heavy drinking
(percent)
35%
36%
E
30%
E
F
34%
E
38%
E
12%
33%
E
39%
E
22%
45%
31%
13%
E
21%
E
19%
E
35%
E
19%
E
17%
E
25%
12%
E
65%
Adult heavy drinking
(percent)
37%
24%
43%
39%
42%
47%
40%
44%
48%
41%
45%
42%
27%
40%
42%
40%
26%
28%
37%
24%
54%
Youth lifetime smoking
abstinence (percent)
69%
83%
77%
91%
87%
68%
89%
79%
62%
E
84%
80%
80%
92%
79%
82%
82%
79%
82%
81%
48%
E
92%
Smoking prevalence
(percent)
26%
30%
27%
26%
26%
31%
20%
31%
23%
23%
19%
17%
17%
22%
22%
20%
16%
18%
*
16%
34%
Postpartum contact
(percent)
65.9%
87.5%
60.2%
84.1%
88.5%
90.1%
87.6%
95.4%
82.2%
89.1%
86.4%
94.9%
58.2%
95.8%
83.9%
90.0%
82.4%
72.8%
80.8%
58.2%
95.8%
Breastfeeding duration
(percent)
35%
E
40%
E
43%
38%
E
56%
53%
55%
42%
65%
52%
50%
63%
49%
51%
58%
34%
54%
53%
50%
31%
E
65%
Low birth weight (rate)
53.7
44.5
52.8
49.4
59.4
44.3
48.8
50.0
67.5
44.0
32.6
44.8
58.3
42.3
39.5
48.8
42.2
54.0
47.9
20.9
67.5
Teen pregnancy (rate)
41.5
34.1
34.4
35.0
33.0
32.9
34.5
32.4
41.8
24.9
9.5
22.2
12.8
30.8
18.8
26.4
12.1
27.4
25.7
9.5
60.8
Indicator
Public Health Unit
Brant County Health Unit
Chatham-Kent Health Unit
City of Hamilton Health Unit
Hastings and Prince Edward
Counties Health Unit
Kingston, Frontenac and
Lennox and Addington
Health Unit
Lambton Health Unit
Middlesex-London Health
Unit
Niagara Regional Area
Health Unit
Peterborough County-City
Health Unit
Durham Regional Health Unit
Halton Regional Health Unit
City of Ottawa Health Unit
Peel Regional Health Unit
Waterloo Health Unit
Wellington-Dufferin-Guelph
Health Unit
Windsor-Essex County
Health Unit
York Regional Health Unit
City of Toronto Health Unit
Ontario
Ontario Total
Ontario Minimum
Ontario Maximum
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
Peer Group
Urban/Rural MixUrban Centres
Metro
Centre
Indicators
Notes:
* Ontario value is not provided
†
Note that an amalgamation occurred in these health units during the period for which data is shown
E
Warning of high variability associated with estimates
F
Estimates of unreliable quality and could not be reported

25
Initial Report on Public Health 2009
Population Health Indicators
Adverse water quality
incidents (number)
67
35
88
164
107
13
64
86
99
133
82
121
36
154
82
69
121
81
4,458
13
446
Immunization coverage
for Measles, Mumps and
Rubella (percent)
70.5%
95.9%
94.2%
92.2%
83.3%
85.6%
97.1%
95.5%
92.3%
88.2%
89.0%
96.3%
45.5%
92.1%
85.9%
87.0%
77.0%
89.9%
84.9%
20.7%
97.8%
Immunization coverage
for Hepatitis B (percent)
74.8%
79.6%
75.9%
82.9%
67.1%
67.5%
–
88.3%
81.6%
86.2%
95.2%
65.2%
89.8%
84.6%
83.2%
69.5%
79.1%
79.0%
79.8%
65.2%
95.2%
Chlamydia incidence
(rate)
184.6
149.6
236.1
179.1
276.5
163.0
249.9
186.1
233.0
199.4
106.3
208.4
181.6
192.8
160.4
148.7
134.9
280.2
219.8
78.9
678.9
Respiratory infection
outbreaks in LTC homes
(number)
19
22
14
18
10
0
36
33
10
7
25
52
8
26
13
8
37
113
602
0
113
Enteric illnesses
incidence (rate)
60.4
44.8
63.2
53.2
54.0
47.5
84.9
87.2
83.3
70.7
86.8
91.5
93.2
99.3
98.2
69.1
94.4
119.9
88.7
40.0
164.1
Fall-related
hospitalizations among
seniors (rate)
1,571.2
1,669.4
1,287.7
1,422.8
1,034.6
1,372.4
1,230.7
1,210.1
1,444.3
1,291.8
1,425.3
1,196.7
950.9
1,165.5
1,682.3
1,431.5
942.6
1,087.5
1,309.5
942.6
2,371.5
Fruit and vegetable
consumption (percent)
43%
29%
45%
46%
43%
37%
38%
44%
45%
42%
48%
50%
42%
41%
50%
34%
37%
40%
42%
29%
50%
Healthy body mass
index (percent)
50%
49%
41%
40%
45%
45%
48%
47%
49%
39%
52%
48%
46%
43%
48%
41%
52%
55%
47%
33%
E
55%
Indicator
Public Health Unit
Brant County Health Unit
Chatham-Kent Health Unit
City of Hamilton Health Unit
Hastings and Prince Edward
Counties Health Unit
Kingston, Frontenac and
Lennox and Addington
Health Unit
Lambton Health Unit
Middlesex-London Health
Unit
Niagara Regional Area
Health Unit
Peterborough County-City
Health Unit
Durham Regional Health Unit
Halton Regional Health Unit
City of Ottawa Health Unit
Peel Regional Health Unit
Waterloo Health Unit
Wellington-Dufferin-Guelph
Health Unit
Windsor-Essex County
Health Unit
York Regional Health Unit
City of Toronto Health Unit
Ontario
Ontario Total
Ontario Minimum
Ontario Maximum
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
Peer Group
Urban/Rural MixUrban Centres
Metro
Centre
Table 2: Indicators by Public Health Unit (cont’d)
Notes:
* Ontario value is not provided
†
Note that an amalgamation occurred in these health units during the period for which data is shown
E
Warning of high variability associated with estimates
F
Estimates of unreliable quality and could not be reported

26
Table 2: Indicators by Public Health Unit (cont’d)
Governance and Accountability Indicators
Number of FTEs by job category
Librarian
0.0
0.0
2.0
0.5
1.0
1.0
1.0
0.0
0.0
1.0
0.0
1.0
1.0
1.0
1.0
0.0
1.0
4.0
20.1
0.0
4.0
Heart Health Coordinator
1.0
1.0
1.0
1.0
1.0
1.0
0.0
1.0
0.0
0.0
1.0
1.0
1.0
1.0
1.0
1.0
0.0
0.0
29.0
0.0
2.0
Epidemiologist
1.0
1.0
2.5
0.0
1.5
1.0
2.0
3.0
1.0
4.6
2.0
4.0
4.9
3.0
2.0
1.0
6.0
11.0
72.6
0.0
11.0
Speech – Language
Pathologist
0.0
0.0
0.0
0.0
4.8
0.0
15.2
0.0
0.0
0.0
0.0
0.0
0.0
0.0
3.0
0.0
0.0
2.0
64.3
0.0
15.2
Dietitian/Nutritionist
3.0
3.0
4.5
4.8
6.0
2.0
4.0
4.9
2.9
4.8
3.8
3.0
12.0
4.7
4.0
4.0
13.0
64.5
203.1
0.5
64.5
Health Promoter
6.0
3.0
13.0
6.0
6.0
8.3
3.0
17.1
11.3
0.0
7.3
0.0
65.0
26.5
2.8
8.0
12.0
123.4
416.7
0.0
123.4
Dental Hygienist/
Dental Assistant
7.2
1.0
3.8
4.8
4.0
1.7
8.6
12.0
1.7
13.0
6.8
14.0
14.8
7.5
3.9
5.0
22.0
86.7
286.4
0.7
86.7
Dentist
1.0
0.0
1.6
0.5
0.2
0.2
1.0
0.0
0.1
1.0
1.0
11.0
1.0
0.5
0.4
0.0
1.0
32.0
54.9
0.0
32.0
Public Health Inspector
8.0
9.0
41.1
13.0
11.0
9.7
26.5
33.0
10.1
45.0
29.1
39.0
60.0
26.0
18.5
20.0
65.0
202.8
900.5
4.2
202.8
Nurse Practitioner
1.5
1.0
0.4
0.0
0.0
0.0
1.1
1.6
0.0
1.0
1.7
4.0
0.0
0.5
1.0
0.0
0.0
0.0
28.5
0.0
4.0
Registered Practical Nurse
0.0
0.0
2.0
3.0
4.8
2.2
0.0
1.0
1.0
0.0
5.0
7.0
0.0
0.0
0.0
0.0
11.0
41.4
100.3
0.0
41.4
Registered Nurse
0.0
3.7
9.0
1.8
1.6
0.0
2.0
0.0
4.3
36.0
13.5
1.0
*
11.2
7.5
0.0
7.0
35.8
180.1
0.0
36.0
Public Health Nurse
37.2
33.1
128.0
35.0
49.6
26.0
99.8
99.7
15.9
118.0
73.5
190.0
229.8
80.0
59.8
67.0
139.0
536.9
2,717.2
14.0
536.9
Expenditures on training and
professional development
(percent)
1.7%
0.4%
1.1%
0.7%
0.5%
0.7%
0.8%
0.7%
0.4%
0.6%
0.6%
0.3%
0.6%
0.5%
0.8%
0.1%
0.4%
0.2%
0.7%
0.1%
1.7%
BoH expenditure variance
(percent)
-0.2%
1.6%
1.0%
-0.8%
-10.2%
6.3%
-7.0%
-0.2%
0.4%
-3.4%
-3.0%
-4.9%
-6.6%
-2.5%
0.0%
-8.2%
-4.7%
-4.9%
-3.3%
-20.8%
6.3%
Total BoH expenditures ($M)
10.0
8.9
35.7
11.3
15.6
8.6
28.2
28.9
10.3
33.8
24.1
46.0
61.7
28.8
17.0
17.0
47.7
193.6
837.7
5.7
193.6
Indicator
Public Health Unit
Brant County Health Unit
Chatham-Kent Health Unit
City of Hamilton Health Unit
Hastings and Prince Edward
Counties Health Unit
Kingston, Frontenac and
Lennox and Addington
Health Unit
Lambton Health Unit
Middlesex-London Health
Unit
Niagara Regional Area
Health Unit
Peterborough County-City
Health Unit
Durham Regional Health Unit
Halton Regional Health Unit
City of Ottawa Health Unit
Peel Regional Health Unit
Waterloo Health Unit
Wellington-Dufferin-Guelph
Health Unit
Windsor-Essex County
Health Unit
York Regional Health Unit
City of Toronto Health Unit
Ontario
Ontario Total
Ontario Minimum
Ontario Maximum
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
Peer Group
Urban/Rural MixUrban Centres
Metro
Centre
Indicators
* Ontario value is not provided

27
Initial Report on Public Health 2009
Table 2: Indicators by Public Health Unit (cont’d)
Governance and Accountability Indicators
Board self-evaluation (year)
n/a
2007
n/a
n/a
2007
2008
n/a
2007
n/a
n/a
n/a
n/a
n/a
n/a
2008
2007
2008
n/a
12/36
=Yes
2003
2008
Board member orientation
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes
No
Yes
Yes
Yes
Yes
Yes
Yes
35/36
=Yes
MOH reporting
relationships
MOH reporting to standing
committee (proportion)
–
–
–
–
–
–
–
16/16
–
14/14
12/13
10/18
–
14/14
9/11
5/5
7/7
–
MOH reporting to the BoH
(proportion)
10/11
9/10
11/12
9/10
9/9
0/11
10/10
16/16
10/10
13/13
12/13
–
12/13
–
9/10
10/10
9/10
10/10
MOH performance evaluation
Yes
Yes
Yes
Yes
Yes
No
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes
32/36
=Yes
Accreditation status
Yes
Yes
Yes
Yes
Yes
No
Yes
Yes
No
Yes
No
Yes
Yes
Yes
Yes
No
No
No
21/36
=Yes
Emergency response plan tested
Yes
Yes
Yes
No
Yes
Yes
Yes
Yes
No
Yes
Yes
Yes
No
No
Yes
No
Yes
Yes
29/36
=Yes
Strategicplan(2008)
Yes
No
Yes
Yes
Yes
No
Yes
Yes
Yes
No
Yes
No
Yes
Yes
Yes
No
Yes
Yes
24/36
=Yes
Issuance of a health status report
(year)
2008
2007
2007
2006
2008
2008
2008
2008
2008
2008
2008
2006
2007
2008
2006
2000
2007
2008
2000
2008
Familiarity with public health unit
programs and services (year)
2007
2008
2008
2008
2005
2008
2002
2008
2005
2008
2004
2007
2007
2008
2008
2002
2008
2008
1998
2008
Proportion of staff
by length of service
>20 years
10%
9%
18%
19%
14%
17%
16%
21%
14%
10%
11%
17%
8%
9%
10%
18%
9%
17%
14%
5%
21%
>10 years <20 years
16%
19%
20%
15%
20%
21%
13%
20%
27%
17%
18%
25%
19%
19%
16%
16%
13%
23%
18%
7%
31%
>5 years <10 years
31%
27%
31%
28%
28%
27%
22%
34%
22%
37%
30%
33%
27%
26%
31%
29%
38%
31%
28%
16%
38%
>1 year <5 years
38%
40%
21%
27%
27%
36%
36%
21%
25%
30%
26%
20%
36%
41%
28%
31%
30%
23%
31%
19%
43%
Up to 1 year
5%
6%
10%
10%
11%
0%
14%
5%
12%
6%
14%
4%
9%
6%
16%
6%
10%
6%
9%
0%
21%
Employment status of MOH (FTE)
1.0
‡
1.0
1.0
1.0
1.0
0.4
1.0
1.0
1.0
1.0
1.0
1.0
1.0
1.0
1.0
1.0
1.0
1.0
34.2
0.3
1.0
Total number of vacant positions
0.0
1.0
9.7
1.4
1.0
0.0
0.0
3.0
0.4
2.8
0.0
11.0
1.0
0.0
2.0
0.5
27.0
5.0
103.4
0.0
27.0
Indicator
Public Health Unit
Brant County Health Unit
Chatham-Kent Health Unit
City of Hamilton Health Unit
Hastings and Prince Edward
Counties Health Unit
Kingston, Frontenac and
Lennox and Addington
Health Unit
Lambton Health Unit
Middlesex-London Health
Unit
Niagara Regional Area
Health Unit
Peterborough County-City
Health Unit
Durham Regional Health Unit
Halton Regional Health Unit
City of Ottawa Health Unit
Peel Regional Health Unit
Waterloo Health Unit
Wellington-Dufferin-Guelph
Health Unit
Windsor-Essex County
Health Unit
York Regional Health Unit
City of Toronto Health Unit
Ontario
Ontario Total
Ontario Minimum
Ontario Maximum
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
Peer Group
Urban/Rural MixUrban Centres
Metro
Centre
‡
Shared MOH 1 FTE between two health units

28

29
Initial Report on Public Health 2009
1. Teen Pregnancy
The teen pregnancy rate indicator estimates the number of pregnancies (resulting in live births, stillbirths,
and therapeutic abortions) per 1,000 females age 15-19 years.
Teen pregnancy poses increased health risks to both the mother and the child, including the following:
• pregnantteenshaveagreaterriskofdevelopinghealthproblemssuchasanaemia,hypertension,
eclampsia and depressive disorders
22,23
• childrenofteenmothersaremorelikelytohavelowbirthweights,pretermbirthsand,asaresult,
are more likely to experience increased mortality and childhood morbidities including developmental
problems, learning difficulties, hearing and visual impairments, and chronic respiratory problems
24,25
The rate of teen pregnancy is significant from a public health and determinants of health perspective because:
• teenpregnancyismorecommonamongdisadvantagedteens
26,27
• pregnancyintheteenyearscanbeasignificantpredictorofothersocial,educationalandemployment
barriers in later life
26,27
• childrenofteenmothershavehigherratesofbecomingteenparentsthemselves,thusperpetuatingthe
cycle of teen pregnancy
28,29
Ontario’s public health units play a role in reducing the rate of teen pregnancy and promoting healthy
pregnancies for those teens who do become pregnant. Public health units provide a comprehensive
range of sexual health education and counselling services that aim to support young mothers to have
positive health outcomes for themselves and their babies.
Specific public health initiatives include:
• healthysexualityeducationandcounselling
• theprovisionoflowcostbirthcontrolsupplies
• confidentialandfreesexualhealthclinicservices
• buildingcommunitypartnershipswithschools,hospitals,andcommunity-basedorganizationstodeliver
healthy sexuality and reproductive health programs and services
Public health units may face specific challenges with community receptivity to sexual health education and
clinic services – it is important to acknowledge that the acceptance of these services may vary across Ontario.
In 2007, the pregnancy rate in Ontario for women aged 15-19 was 25.7 per 1,000. Based on 36 public health
unitsinOntario,thehighestratewas60.8,andthelowestratewas9.5per1,000womenaged15-19.
Teen pregnancy rates have been on the decline in Canada in the last 25 years, with significant variation across
provinces and territories. However, teen pregnancy has continued to be of significant concern in specific
populations including socio-economically disadvantaged teens.
Population Health Indicators
Group A

30
Population Health Indicators
Food Security Case Studies
Case Study 1
Having
access to affordable healthy foods is an issue of public health concern, and
Peterborough County-City Health Unit has been working to address this
issue with its Food Security Community Partnership Project.
For more than a decade, the annual Nutritious Food Basket survey has identified that low-income
residents in Peterborough City and County cannot afford an adequate diet once they have paid
for housing and other basic needs. In response, the Peterborough County-City Health Unit rallied
community partners to provide the Food Security Community Partnership Project (FSCPP), with a
focus on community-based food programs and food skill development.
The FSCPP involves 5,000 adults and children living on low incomes in Peterborough City and County.
The program targets priority populations, including those from: rural and First Nation communities,
youth living independently, parents of young children, homeless and under-housed community members,
and seniors living in isolated situations. The new partnerships allowed the program to expand its reach
within these priority populations.
The project components include:
• Advocacy for improved incomes for people receiving social assistance and low wages.
• Come Cook with Us – Cooking sessions in which participants cook, enjoy a meal together, share
healthy eating and food safety tips, and take home meals and a food voucher. Graduates are invited
to join a monthly collective kitchen.
• Food Box Programs – Monthly boxes of staples and/or produce with a subsidy for low income
clients.
• Cooking up Employment – Two community members work with the “Open Table Chef” to
provide a free, nourishing meal to community members five days a week.
• Frozen Meal Program – The provision of nutritious meals, delivered to isolated rural community
members in Peterborough County.
Evaluations of this initiative indicate that participants are making healthier food choices. Community
response to the program has been remarkable, in both the numbers reached and in the stories from
individuals whose lives have been impacted.
Another local example of work on food security is occurring in the Huron County Health Unit, with
their Farm to Table Project. This network of community organizations, concerned about access to
local, healthy food and the overall decline in agriculture in Huron and Perth Counties, aims to educate
consumers about food, nutrition, and agricultural issues, and create new markets for local farmers.
Farm to Table’s central initiative is the monthly Huron Good Food Box program, which provides Huron
County residents with a regular, affordable supply of local fresh fruits and vegetables. The program
relies on volunteers, and annual sales volumes have grown since its inception in 2001, to more than
2,500 Good Food Boxes in 2007, to a customer base that included 25% of buyers with annual household
incomes of less than $20,000. More than 60% of users of the Huron Good Food Box program report they
have increased their consumption of fruits and vegetables.

31
Initial Report on Public Health 2009
2. Low Birth Weight
The low birth weight rate indicator estimates the rate of singleton live births weighing 500-2499 grams
immediately upon birth, based on the mother’s usual place of residence per the total for singleton live
births weighing at least 500 grams per 1,000 births.
Low birth weight is considered one of the most important indicators of a newborn’s chances of survival, with
low birth weight being a major risk factor for perinatal and infant mortality.
30
Low birth weight babies are
more likely to have health and developmental problems including learning difficulties, hearing and visual
impairments, chronic respiratory problems such as asthma and chronic diseases later in life.
31,32
Low birth weight is also an important population health indicator as it occurs with greater prevalence in
disadvantaged populations. Risk factors associated with low birth weight include:
• socio-economicdisadvantage
• poorhealthandnutritionofwomenduringpregnancy
• smokingwhilepregnant
• consumptionofdrugsandalcoholwhilepregnant
• experiencingabusewhilepregnant
33,34
It has been demonstrated that maternal smoking is one of the most modifiable risk factors to prevent low
birth weight babies in developed countries.
35,36
This underscores the importance of programs and policies to
prevent women from becoming smokers and encouraging those who do smoke to quit.
Public health programs and services provide education and resources to women of child bearing age to promote
healthy nutrition prior to conception and during pregnancy, provide prenatal education, encourage pregnant
women to access prenatal support services, and provide assessments to at-risk pregnant women to help ensure
that they receive appropriate medical attention.
Public health interventions also address factors that influence health outcomes such as access to nutritious
foods, smoking, substance misuse, and alcohol consumption during pregnancy.
In 2007, the rate of singleton live births in Ontario with a birth weight of less than 2500 grams was 47.9 per
1,000 births. Based on 36 public health units in Ontario, the highest rate of live births weighing under 2500
grams was 67.5 and the lowest rate was 20.9 per 1,000 births.

32
Population Health Indicators
3. Breastfeeding Duration
The breastfeeding duration rate indicator estimates the proportion of mothers age 15-55 years who breastfed
(not exclusively) their last baby (born within the past five years) for a duration of six months or more.
According to the WHO, “breastfeeding is the ideal way of providing young infants with the nutrients they
need for healthy growth and development.”
37
Breast milk contains the ideal nutritional elements for proper
digestion, brain development, and growth. Breast milk transmits a mother’s antibodies to her baby, helping to
protect the baby against infections and illnesses. Studies also suggest that breastfeeding may protect infants
against allergies and respiratory infections,
38
and may lower rates of type 2 diabetes later in the child’s life.
39
Additionally, breastfeeding forms a bond between a mother and her child that is thought to contribute to the
healthy psychological development of the child.
40
Breastfeeding is not only beneficial for infants. Research suggests that breastfeeding may lower rates of certain
types of ovarian and breast cancer and reduce the risk of osteoporosis in women who have breastfed.
41
Most new mothers have the potential to breastfeed, giving their newborns breast milk which contains
everything they need for a healthy start in life. The public health sector in Ontario helps to promote
breastfeeding through:
• providingprenatalandparentingprograms,servicesandsupports
• distributinginformationregardingthebenefitsofbreastfeedingthroughmassmedia
• offeringbreastfeedingsupportandcounsellingthroughphonelines,homevisits,groups,andclinics
• providingreferralstoprofessionalsandcommunityprogrammingandservicesforbreastfeedingsupport
and information
• advocatingandassistinginthedevelopmentofpoliciestosupportbreastfeedingintheworkplace,
restaurants, shopping malls and other public places
The data presented in Table 2: Indicators by Public Health Unit for the proportion of mothers in Ontario who
breastfed their last baby for a duration of six months or more uses a combination of three sets of Canadian
Community Health Survey data, collected over a span of 5 years. Because sample sizes of breastfeeding rates
at the public health unit level can be quite small, it was necessary to combine these three sets of data in order
to arrive at a stable figure for each public health unit.
Approximately 50% of mothers in Ontario breastfed their last baby for a duration of six months or more
(over 3 cycles of the survey). Based on 36 public health units in Ontario, the highest estimated proportion
of breastfeeding for six months or more was 65% and the lowest estimate was 31% for mothers who had given
birth in the last five years at the time of the surveys.
In Ontario, the proportion of mothers breastfeeding for six months or more for each of the survey periods
was as follows:
Canadian Community Health Survey Cycle 2.1 (2003) – 46.7%
42
CanadianCommunityHealthSurveyCycle3.1(2005)–50.8%
43
Canadian Community Health Survey 2007 – 53.1%
44
The indicator results demonstrate that improvements are being made in breastfeeding uptake and that there
is more opportunity to encourage and support breastfeeding initiation and duration in Ontario, particularly at
a time when hospital based supports for breastfeeding are limited.

33
Initial Report on Public Health 2009
4. Postpartum Contact
The postpartum contact indicator is defined as the percentage of families who consented to a post-partum
phone call under the Healthy Babies Healthy Children (HBHC) program and who received a post-partum
phone call or contact from the health unit within 48 hours of release from hospital after giving birth.
The postpartum contact by a public health nurse is a universal component of the HBHC program where
newmotherswhoconsentarecontactedwithin48hoursofdischargefromhospitalorafterahomebirth,
and offered a home visit, counselling, support and information about community services on parenting and
healthy child development.
ThedatainTable2:IndicatorsbyPublicHealthUnitshowthepercentageofmotherscontactedwithin48
hours of hospital discharge. This definition is consistent with the target used by the HBHC program, and
the HBHC Protocol
45
under the Child Health standard of the OPHS. It is important to note, however, that
the method of contact under this definition includes all types of contact including person to person contact,
phone messages, and letters; there is no way of ensuring that a message or letter was received by the new
mother. This indicator therefore does not measure the effectiveness or success of the HBHC program. Rather,
it gives an indication of the extent of work and resources expended by public health units attempting to make
contact with every new mother in their community.
Addressing Poverty Case Study
Case Study 2
Grey
Bruce Health Unit’s Moving Forward program focuses on breaking the
cycle of poverty by addressing systemic barriers that prevent marginalized
individuals from obtaining adequate education and employment. Targeting high-risk young
families, the program uses motivational interviewing to help clients recognize their readiness
to change and to develop an action plan to achieve specific goals. Set-backs and relapses
are common throughout the change process. Public health professionals support clients to
evaluate their goals and reaffirm their action plans.
Grey Bruce Health Unit also provides tangible support through the provision of
transportation, access to adequate childcare and by helping clients purchase affordable,
appropriate interview clothing. All these elements increase the client’s opportunities for
employment and education.
Moving Forward works on many levels to address and improve determinants of health
associated with poverty and access to education and employment opportunities.

34
5. Smoking Prevalence
The smoking prevalence indicator estimates the age-standardized proportion of people age 12 years and
older who are current smokers (daily or occasional cigarette smokers).
Tobacco use is the number one preventable cause of premature death and illness in Ontario. Smoking accounts
for approximately 13,000 deaths annually and results in a substantial burden on the health care system.
46
Public health units are key partners in the implementation of the Smoke-Free Ontario Strategy (SFOS).
The SFOS is focused on:
1. Prevention – preventing children and youth from starting to use tobacco products
2. Protection – eliminating involuntary exposure to second-hand smoke
3. Cessation – motivating and supporting people to quit tobacco use
Locally, public health units lead the delivery of several programs involving youth engagement, local tobacco
control coordination and enforcement of the Smoke-Free Ontario Act (SFOA).
47
The goal of these public health programs and services is to reduce the burden of preventable chronic diseases
of public health importance. Public health units are responsible for:
• increasingpublicawarenessoftheimportanceofcomprehensivetobaccocontrol
• workingwithprioritypopulationstoadopttobacco-freeliving
• ensuringtobaccovendorsareincompliancewiththeSFOA
• reducingyouthaccesstotobaccoproducts
Based on 36 public health units in Ontario, in 2007 the highest proportion of current smokers among people
age 12 years and older was 34% and the lowest was 16%.
6. Youth Lifetime Smoking Abstinence
The youth lifetime smoking abstinence indicator estimates the proportion of young people age 12-19 years
who have never smoked a whole cigarette.
Tobacco use is the number one preventable cause of premature death and illness in Ontario. Smoking accounts
for approximately 13,000 deaths annually and results in a substantial burden on the health care system.
46
Preventing children and youth from starting to use tobacco products is a key pillar of the Smoke-Free Ontario
Strategy(SFOS).Researchhasshownthatmorethan80%ofcurrentandformersmokersinCanadastarted
smoking before the age of 20.
48
Thus, preventing adolescents from experimenting with tobacco products
during adolescence is a key intervention to prevent them from smoking as adults – and to prevent morbidity
and mortality from chronic disease.
Youth tobacco use is associated with a variety of personal, behavioural, environmental, and socio-demographic
factors, including:
• lowerselfesteem
49
• loweracademicachievement
50
• lowersocio-economicstatus
51
Population Health Indicators

35
Initial Report on Public Health 2009
• peerandparentalsmoking
48
• useofalcohol,andmarijuana
50
The goal of public health policies, programs and services is to reduce the burden of preventable chronic
diseases of public health importance. Public health units are responsible for:
• increasingpublicawarenessoftheimportanceofcomprehensivetobaccocontrol
• workingwithyouthtoadopttobacco-freeliving
• workingwithschoolstoeducatestudentsaboutthedangersofsmoking
• ensuringtobaccovendorsareincompliancewiththeSFOA
• reducingyouthaccesstotobaccoproducts
In2007,81%ofyouthage12-19yearsinOntariohadneversmokedawholecigarette.Basedon36public
healthunitsinOntario,thehighestproportionwas92%andthelowestwas48%ofyouthage12-19years
who have never smoked a whole cigarette.
The Low-Wage Worker Project Case Study
Case Study 3
Public
health programming that directly addresses the underlying social factors
associated with poor health outcomes is an important practice area for
public health units. As an example, in 2003, the Sudbury & District Health Unit (SDHU)
staff and its university partners launched a major project to understand the health and
wellness issues facing low-wage worker populations in the City of Greater Sudbury and to
identify interventions that could be taken to improve their health, safety, and well-being.
A literature review revealed that research on public health interventions to improve the
lives and working conditions of working poor people is limited. This made a series of needs
assessment interviews fundamental to understanding the challenges faced by low-income
workers and the possible interventions to address those challenges. As a result, nine focus
groups were conducted with 23 key informants and 65 low-wage workers. Recommendations
from the interviews included calls for:
• enhancementofexistinghealthpromotion,protection,andsafetyprogramsfocusedon
the low-wage worker population
• developmentofcommunitypartnershipstoadvocateforandimplementpolicychanges
• conductingmoreresearchontheneedsoflow-wageworkersandtheidentificationof
interventions at the individual, workplace, community, and social policy levels.
These recommendations have implications for public health planners across Ontario.
Full reports are available on the Sudbury & District Health Unit’s website at
http://www.sdhu.com.

36
Population Health Indicators
Crystal Meth Task Force Case Study
Case Study 4
As
new health concerns emerge in a community, public health units use their know-
ledge and skills to respond with creative community engagement strategies. For
example, in 2005, The Toronto Star labelled Perth County the “Crystal Meth Capital” of
Ontario. A series of methamphetamine lab discoveries and rising substance misuse rates
had leaders scrambling to deal with this problem.
In response, the Perth District Health Unit became involved with the formation of
the Perth County Task Force on Crystal Meth, which formed in 2005. By 2008, it had
grown to a 40-member committee, including public health, police, politicians, fire, EMS,
health-care providers, addiction counsellors, social services, pharmacies, and agriculture
associations. The Director of Health Protection from the Perth District Health Unit and
the Mayor of Stratford co-chair the committee.
The Task Force is tackling the crystal meth problem on four fronts:
• enforcement
• healthprotection
• preventionandeducation
• treatment
Through its leadership on the Task Force, the Perth District Health Unit is able to ensure
that crystal meth use is addressed using a comprehensive, best-practices approach. In
2008,theTaskForceimplementednineprogramsacrossthefourareasoffocus.Public
health unit programs have focused on youth development and engagement to prevent
substance misuse, and health protection measures related to drug labs.
To date, the program has experienced successes resulting in:
• adecreaseinmethlabdiscoveries
• majorenforcementsuccesses
• improvedaddictiontreatmentservices
• betterinformedyouththroughtheimpactof
widespread, multifaceted education measures

37
Initial Report on Public Health 2009
7. Adult Heavy Drinking
The adult heavy drinking episode indicator estimates the age-standardized proportion of people age
20 years and older who reported consuming five or more drinks on at least one occasion during the
previous 12 months.
Alcohol use is a significant risk factor for both injury and chronic disease. Heavy drinking puts a person at
much higher risk of death or injuries from motor vehicle collisions; alcohol associated illness, falls, drowning
and other hazards of poor judgement and reduced coordination.
52,53
Longer term, heavy drinking can result in
high blood pressure, stroke, liver disease, and neurological damage.
54
It is estimated that 10% of all deaths in Ontario directly or indirectly result from alcohol misuse.
55
Alcohol
misuse is involved in about 40% of all traffic collisions,
56
which result in a large number of potential years of
life lost because of the relatively young age of those killed in traffic collisions.
57
Alcohol misuse is associated with significant economic impacts including:
• lostproductivityduetomorbidity
• prematuremortality
• socialservicescosts
• lawenforcementcosts
• directhealthcarecosts
58
Heavy drinking also increases the risk of violence,
59
vandalism,
60
sexual assault, and unprotected sexual
encounters with the potential for unplanned pregnancy or infection from sexually transmitted diseases.
61
Public health programs and services aim to increase public awareness of the dangers of substance misuse and
promote healthy public policy to reduce the risks. Programs and services include:
• promotingtheLow-RiskDrinkingGuidelinesdesignedtominimizethehealthrisksofalcoholuse
• promotingresponsibledrivingincludingnotdrivingundertheinfluenceofalcohol
• advisingwomenwhoknowtheyarepregnantorareplanningonbecomingpregnantoftheharmfuleffects
of alcohol on their unborn child
• promotingadoptionofmunicipalalcoholpolicies
• providingServerInterventionTrainingandSafeBarPolicy
• promotingresponsiblehosting
In addition, there are provincially funded initiatives such as the FOCUS Community Project which operates in
21 communities with the aim of reducing the abuse of alcohol and other drugs and preventing their associated
problems, injuries, and chronic diseases.
In 2007, 37% of people in Ontario age 20 years and older reported consuming at least five or more drinks on at
least one occasion in the last 12 months. Based on 36 public health units in Ontario, the highest proportion of
heavy drinkers,that is those who reported consuming five or more drinks on at least one occasion in the last
12 months, was 54% and the lowest was 24% of adults age 20 years and older.

38
Population Health Indicators
Teen Sexual Health Case Studies
Case Study 5
Many
health units are addressing teens’ sexual health needs by providing
services in ways that are relevant to this client group.
For example, Kingston, Frontenac and Lennox & Addington Public Health offers
its comprehensive school-based teen sexual health clinic program in partnership with the
Limestone District School Board. A public health nurse visits various local high schools
to increase the access local teens have to free, confidential sexual health services. Public
health nurses work closely with the adolescent care worker at each school and facilitate
physician referrals as required.
The teen sexual health clinic program is designed to decrease the rate of teen pregnancy
and prevent the spread of sexually transmitted infections. The program is currently available
at five secondary schools within the public health unit’s catchment area. One Teen Clinic
occurs at an alternate education centre where many of the students are homeless or
involved in prostitution. A Teen Clinic database is currently being developed to capture all
relevant demographic information and sexual health services provided in order to evaluate
the program’s success.
Another approach is being used by the Middlesex-London Health Unit, which runs a
one-day, interactive high school outreach program designed to enhance knowledge and
engage youth. The Having a Baby Day program operates in conjunction with St. Joseph’s
Health Care, London, the Regional Sexual Assault and Domestic Violence Treatment Centre
(RSADVTC), and the Thames Valley and London District Catholic school boards.
The program is offered quarterly and brings high school students and their teachers into
St. Joseph’s Health Care to learn about preparing for parenthood, achieving optimal pre-
conception health, experiencing a healthy pregnancy, and having the healthiest newborn
possible.
Students rotate through small-group discussion sessions on and site visits to:
• theFamilyBirthingCentre(FBC)
• theNeonatalIntensiveCareUnit
• HealthyRelationships
• theRegionalSexualAssaultandDomesticViolenceTreatmentCentre
• Post-PartumIssues
The sessions include discussions by health care staff on topics such as antenatal, intra-
partum, and post-partum care, implications of having a pre-term or ill infant, decisions about
safer sex, resources on preventing abuse, and changes facing families with newborns.

39
Initial Report on Public Health 2009
8. Youth Heavy Drinking
The youth heavy drinking episode indicator identifies the proportion of people age 12-19 years who reported
consuming five or more drinks on at least one occasion during the previous 12 months.
Research shows that young people, whose brains are still developing, may be at greater risk than mature
adults of lasting brain damage from heavy alcohol consumption.
62
Alcohol is the most commonly used drug
among Canada’s youth.
63
Alcohol-related trauma is a significant and preventable cause of death among young
Canadians.
64,65,66
Research indicates that youth view heavy drinking as a social norm and that the consequences of excessive
alcohol consumption are a ‘rite of passage’. This view is highlighted by the fact that while illicit drug use
has generally been declining, the prevalence of heavy drinking has been holding steady and even increasing,
particularly among youth aged 15 to 25.
67,68
Moreover, new studies show that some youth start drinking at age
13 or younger.
69
Heavy drinking is associated with risk taking behaviour. Risks and consequences associated with heavy
drinking include death, injury, violence, alcohol poisoning, unplanned and unwanted sexual experiences
including sexual assault and sexually transmitted infections.
70
Prolonged heavy drinking may result in brain
damage, liver disease, cancer or heart disease.
71
Although most health consequences of alcohol and drug use typically appear later in life, early initiation of
heavy drinking can lead to earlier problems and the development of life-long habits.
Public health programs and services aim to increase public awareness of the dangers of substance misuse and
promote healthy public policy to reduce these risks. Programs and services include:
• promotingtheLow-RiskDrinkingGuidelinesdesignedtominimizethehealthrisksofalcoholuse
• promotingresponsibledrivingincludingnotdrivingundertheinfluenceofalcohol
• advisingwomenwhoknowtheyarepregnantorareplanningonbecomingpregnantoftheharmfuleffects
of alcohol on their unborn child
• promotingadoptionofmunicipalalcoholpolicies
• providingServerInterventionTrainingandpromotingSafeBarPolicy
• promotingresponsiblehosting
Interventions to address youth heavy drinking are given additional prominence before and during events such
as high school proms where a single episode of binge drinking can have severe health effects. More broadly
though, interventions with youth promote adoption of behaviours to minimize health risks and reduce under-
age drinking.
In 2007, 25% of people in Ontario age 12-19 years reported consuming at least five or more drinks on at least
one occasion in the previous 12 months. Based on 36 public health units in Ontario, the highest proportion of
heavy drinkers was 65% and the lowest was 12% for people age 12-19 years who reported consuming five or
more drinks on at least one occasion.

40
Population Health Indicators
9. Physical Activity Index
The physical activity index indicator estimates the age-standardized proportion of the population age 12
years and older by level of energy expenditure in the categories active and moderately active in their
leisure time physical activity.
Physical activity directly benefits a person’s physical and mental health. People who exercise regularly are less
susceptible to a number of chronic health conditions. Evidence also suggests that regular physical activity can
contribute to improved mental health.
72
Physical inactivity is among the leading contributors to a wide range of illnesses and conditions including:
• coronaryheartdiseaseandstroke
• type2diabetes
• certaintypesofcancer
• osteoporosis
73
A physically active lifestyle among the population will substantially reduce the burden of disease, death, and
disability in Ontario.
74,75
Childhood obesity is a serious concern in Canada and internationally. Over the past 25 years, obesity rates
among children and youth have nearly tripled. Not only are children eating too much high-energy, high-fat
food, but they also are more sedentary. Childhood obesity can result in serious medical problems, including
type 2 diabetes, high blood pressure, and liver disease as well psychological difficulties. Most children do not
outgrow their weight problem and many continue to gain weight as they age.
76
The increased prevalence of overweight/obese young people and adults, combined with only moderate levels
of physical activity, is a public health issue. To address these issues, the Ministry of Health Promotion launched
ACTIVE2010 Ontario’s Sport and Physical Activity Strategy in October 2004.
77
Public health programs and services use a population health approach to promote healthy behaviours that
improve the quality of life and help reduce the number of Ontarians seeking diagnostic services and medical
care. Public health initiatives promote a healthier Ontario by:
• Promotinghealthateachageandstageoflife,focusingfirstonchildrenandyouth
• Influencingthesocialdeterminantsofhealth–thesocialandeconomicfactorsthatshapeourhealth
• EngagingpartnerstosharetheresponsibilityforahealthierOntario
• Improvingthehealthofthosemostatrisk
• Removingbarrierstohealthy,activelivingsoOntarianshavemoreopportunitiestoenjoygoodhealth
(i.e., bicycle/walking trails)
In 2007, 50% of people in Ontario age 12 years and older reported participating in physical activities in which
they were active or moderately active. Based on 36 public health units in Ontario, the highest proportion was
64% and the lowest was 43% of people age 12 years and older who reported participating in physical activities
in which they were active or moderately active.

41
Initial Report on Public Health 2009
10. Healthy Body Mass Index
The healthy body mass index indicator estimates the age-standardized proportion of people age 18 years
and older whose self reported height and weight denote a healthy body mass index (BMI). BMI is calculated
using the person’s weight in kilograms divided by their height in squared metres. The World Health Organization
considersaBMIintherangeof18.5-24.9tobehealthyformostadults.
78
A healthy body weight is associated with good health. Excess weight can lead to:
• coronaryarterydisease
• stroke
• hypertension
• coloncancer
• postmenopausalbreastcancer
• type2diabetes
• gallbladderdisease
• osteoarthritis
79
Chronic diseases such as the above are the leading causes of death in Ontario.
80
Best Start’s Primary Care Strategy Case Study
Case Study 6
Healthy
development during a child’s first years significantly impacts the
health and well being of that individual later in life. The Best Start
initiative, funded through the Ministry of Children and Youth Services, is designed to improve
early identification and resource networking at the community level throughout Ontario,
and public health units have been active participants in these projects.
As an example, City of Hamilton Public Health Services worked with primary care, public
health and Ontario Early Years Centre (OEYC) representatives to form a sub-committee
under Hamilton’s Best Start Network. A team that included a physician opinion leader,
public health nurse and OEYC facilitator delivered presentations on early identification
and the availability of community resources to primary care practitioners. Where possible,
practitioners were invited to the neighbourhood OEYC, which reinforced the availability of
local Early Years services. Other presentations were held in group practices, and physician
rounds.
Attendees received an information package that included multiple copies of the Nipissing
District Developmental Screen
TM
(NDDS),RourkeWellBabyRecord,anarticleonthe18-
month visit, and a flowchart of local early years services with contact information. In addition,
a continuing medical education accreditation event provided more in-depth understanding of
child development. Project evaluation demonstrated an increase in referrals to community
services.

42
Obesity is strongly linked with type 2 diabetes, which itself is associated with other health problems such as
heart disease, stroke, blindness and kidney failure. Type 2 diabetes is a major cost driver of Ontario’s health
care system.
81
Diabetes is the single most significant contributor to renal disease and vision loss and a leading
cause of heart disease, stroke, and non-traumatic limb amputations.
82
There are many contributing factors to obesity, including:
• overeating
• lowactivitylevels
• genetics
• bodymetabolism
• socio-economicstatus
• psychological/emotionalfactors
Unhealthy weights – both overweight and obesity – are a global public health priority. Overweight and obesity
now are such a serious public health concern that they are known as ‘the new tobacco’.
83,84,85
The increased prevalence of overweight and obese young people is of concern because overweight and
obesity may persist into adulthood.
86,87,88,89
To address these issues, and in response to the Chief Medical
Officer of Health’s report, Healthy Weights, Healthy Lives,
90
the Ministry of Health Promotion launched the
Healthy Eating Active Living (HEAL) Action Plan in 2006.
91
Public health units play a significant role in chronic disease prevention and health promotion related to
healthy weights, proper nutrition and physical activity.
Public health works with individuals to build food skills and promote healthy behaviours, and with communities
to promote food security and awareness of healthy eating. Efforts also are made to influence policy makers
and community partners to address issues related to the existing community infrastructure, environment, and
community spaces so that people have options that support them to be active and to access healthy foods.
In2007,47%ofindividualsage18yearsandolderhadahealthyBMI.Basedon36publichealthunitsinOntario,
thehighestproportionofindividualsage18yearsandolderwithahealthyBMIwas55%andthelowestwas33%.
11. Fruit and Vegetable Consumption
The fruit and vegetable consumption indicator estimates the age-standardized proportion of the population
age 12 years and older that reported consuming fruits and vegetables five or more times per day.
Research has shown that diets containing substantial and varied amounts of vegetables and fruit:
• maypreventcertaintypesofcancer
92
• areassociatedwithreducedriskofcardiovasculardisease
93
• areassociatedwithhealthyweightsanddecreasedriskofobesity
94
Lack of adequate fruit and vegetable consumption has become an important public health issue. According to
the Canadian Community Health Survey (2.2) 59% of Canadian children 2-17 years of age consume fruit and
vegetables less than five times a day.
95
These children are significantly more likely to be overweight or obese
compared to those who consume fruit and vegetables more frequently.
Population Health Indicators

43
Initial Report on Public Health 2009
Fruit and vegetable consumption is influenced by many factors, including:
• physicalaccesswithinacommunity
• foodaffordability
• knowledgeofhealthyfoodchoices
• foodskillssuchasshopping,budgeting,preparation,andstorage
Public health programs and services related to healthy eating and food security issues target both individuals,
to build food skills and promote healthy behaviours, and communities to promote food security and awareness
of healthy eating. Programs and services that support healthy eating and food security include:
• communitygardens
• schoolnutritionprograms
• awarenesscampaignsincludingcomparisonsofthecostofanutritiousfoodbaskettothecostofliving
The annual tracking of a cost of the Nutritious Food Basket for an Ontario family is used to monitor food
affordability across Ontario and to advocate for food access and security for specific populations. Data for
the2008costoftheNutritiousFoodBasketacrossOntarioareshownwithintheHealthUnitProfiletable.
The Northern Fruit and Vegetable Program is a provincial initiative that aims to increase fruit and vegetable
consumption and increase awareness of the importance of fruits and vegetables among elementary school
children in select communities in Northern Ontario, and to educate elementary school-aged children and their
families about the importance of eating fruit and vegetables, and the associated benefits of healthy eating and
physical activity to overall health. The project provides fresh Ontario produce twice a week in conjunction
with a curriculum-based resource that outlines the benefits of eating fruits and vegetables. Northern Ontario
was selected for the project because of the higher proportion of overweight children, the higher cost of the
Nutritious Food Basket in Northern Ontario, and because 62% of children in the region aged 12-19 do not eat
five or more servings of fruits and vegetables daily.
In 2007, 42% of individuals age 12 years and older reported consuming fruits and vegetables five or more times
per day. Based on 36 public health units in Ontario, the highest proportion of people age 12 years and older that
consumed fruits and vegetables five or more times per day was 50% and the lowest was 29%.
12. Fall-Related Hospitalizations among Seniors
The fall-related hospitalization rate indicator estimates the age-standardized number of injury-related
hospital separations that are due to falls in seniors age 65 years and older per 100,000 population.
Persons over age 65 have the highest mortality rate from injuries. In the elderly, injuries from falls cause
about one-half of deaths due to injury – more than either pneumonia or diabetes.
96,97
Injury prevention is a cost-effective strategy for reducing the indirect and direct health care costs associated
with falls.
98,99
Effective injury prevention interventions can reduce injury-associated demand for care, including
reducing hospitalizations, the demand for rehabilitation and assistive devices, as well as for residential care
and home care.
100,101
Injury prevention can also help seniors preserve their independence and quality of life –
avoiding clinical complications and increased dependency on support services.
102,103

44
Most falls are predictable and therefore, preventable. Public health injury prevention interventions focus on
eliminating or reducing known risk factors associated with falling.
Public health programs and services focus on reducing the frequency, severity, and impact of preventable
injury. Public health units and their community partners promote:
• thesafeuseofprescriptionandover-the-countermedication
• theimportanceofnutritionandcalciumandVitaminDrichfoodscombinedwithexercisetopreventfalls
and/or delay the onset of osteoporosis
• awarenessofthebuiltenvironmentandtheidentificationofhazardstoreducetheriskoffallingbothin
the home and in the community
The risk of being injured and the incidence of injury are not equal throughout Ontario; each age group is at
risk for different types of injuries. Seniors are most at risk for serious injuries resulting from changes that
occur during the aging process (e.g. decreased vision, diminished reflexes, reduced muscular strength and
mass, and decreased bone density).
In 2007, the rate of injury-related hospital separations due to falls in seniors age 65 years and older was 1,309.5
per 100,000 seniors in Ontario. Based on 36 public health units in Ontario, the highest rate was 2,371.5 and the
lowest rate was 942.6 injury-related hospital separations due to falls in seniors age 65 years and older, per
100,000 population.
Population Health Indicators
Guelph Inclusiveness Alliance Case Study
Case Study 7
The
Guelph Inclusiveness Alliance (GIA) is a multicultural coalition of more than 30
service provider organizations and persons focusing on making Guelph a more
welcoming place for immigrants in need of support. The Wellington-Dufferin-Guelph Public
Health (WDGPH) provides GIA with epidemiological expertise and brings a determinants-of-
health perspective to the coalition’s work.
The 2006 Census found that immigrants represent 21% of Guelph’s population. In 2009, the Guelph
Inclusiveness Alliance will buy customized, demographic information from Statistics Canada
to provide more detailed immigrant profiles as a basis for identifying inequities and improving
accuracy.
WDGPH uses census and postal code information to examine the spatial and temporal distribution
of immigrants, mortality rates, emergency room visits, and hospitalizations, across 12 Guelph
neighbourhoods. This work supports a powerful Geographic Information System (GIS) that
includes advanced statistical analysis tools to help interpret health patterns within Guelph.
Through the GIA, Wellington-Dufferin-Guelph Public Health is attempting to identify and
reduce health inequities among Guelph’s diverse populations, tailor its programs and services
to better meet local needs, and share its knowledge and expertise with community partners.

45
Initial Report on Public Health 2009
Case Study 8
Developing
methods of promoting and supporting knowledge exchange is an
important aspect of ensuring that new knowledge is translated into
practice and that current thinking on best practices is continually updated.
Peel Public Health has embarked on a ten year strategic direction setting process to enhance
evidence informed decision making throughout the health unit. This multi-faceted strategy currently
includes a review of library services, staff skill development, particularly in critical appraisal of
the literature, a department wide communication plan, a project by one of the Associate Medical
Officers of Health who has a fellowship through the CHSRF Executive Training for Research
Application (EXTRA) program, and a post doctoral study on the change management process by
a researcher at McMaster University. Additional activities include piloting the use of a knowledge
broker role, contracting academics for selected literature reviews, a 12 month pilot of RefWorks
(an online research management tool that manages on line information and generates citations and
bibliographies) and formation of a critical appraisal club where staff can develop new skills and
learn from each other.
Region of Waterloo Public Health approached this task by organizing a Research Pathways
to Healthy Public Policy forum as a way to advance population health assessment, research, and
evaluation activities. The forum is part of a program through which the health unit developed
specific goals and objectives to guide its work with key stakeholder groups, including community
organizations, the community at large and in particular vulnerable populations, professional partners
and colleagues, decision makers and members of academia.
TheResearchPathwaystoHealthyPublicPolicyonedayforumattractedmorethan80
participants from local academic institutions and key community groups. The event focused on
three themes:
• healthandthebuiltenvironment(communitydesign)
• environmentalconditionsaffectinghealth(drinkingwater,airquality)
• localhealthyfoodsystemdevelopment
The day was organized into three sections:
1. a general overview of the public health context, which outlined the Region of Waterloo Public
Health’s mandate and what Research Pathways had to offer researchers
2. a large-group plenary section, which addressed expectations and concerns in partnering with
Public Health and brainstormed how to overcome barriers to working together
3. small-group break-out sessions covering the three themes
Each small-group session identified key issues for both academia and public health by theme area,
discussed ways to continue communications on the issues, and identified the key contact people
for each theme area. Since the session, public health staff have followed up on at least 10 potential
research ideas, proposals, or discussions for projects with the academic attendees.
Knowledge Exchange Case Studies

46
13. Enteric Illnesses Incidence
The enteric illnesses age-standardized incidence rate estimates the total number of reported cases of selected
enteric illnesses
ii
per 100,000 population.
Enteric illnesses are frequently characterized by diarrhea, nausea, vomiting, abdominal cramps, fever, and
other symptoms. They can be transmitted via ingestion of contaminated food or water, exposure to infected
vomit or feces, direct or indirect contact with infected persons or animals, or contaminated objects. Enteric
illnesses are typically caused by pathogens such as Campylobacter, Salmonella, and E. coli. Young children,
the elderly, and those with weakened immune systems, are at greater risk for complications from these
pathogens, which can result in significant morbidity and mortality.
Enteric diseases are generally under-reported. Many individuals who acquire an enteric disease do no seek
medical attention, or do not submit a laboratory specimen to confirm the existence of the disease. Studies
estimate that for each reported case of enteric illness, there are at least several hundred undiagnosed or
unreported cases in the community.
104
An important role of public health is to increase public awareness of the importance of hand hygiene, food
safety and safe food handling practices, and the safe use of drinking and recreational water to reduce the
spread of enteric diseases in the community. Public health programs and services aimed at reducing enteric
illnesses include:
• inspectingregulatedestablishments,suchasfoodpremisesandrecreationalwaters,forcompliancewith
the HPPA
• conductinglocalandprovincialsurveillanceofentericdiseases
• investigatingentericillnessesandoutbreaks
• educatingthepublicregardingentericdiseaseprevention
• providingfood-safetytrainingprogramsforfood-handlers
• educatingdrinkingwatersystemoperators
In2007,thereportedincidencerateofcasesofselectedentericillnessesinOntariowas88.7per100,000
population. Based on 36 public health units in Ontario, the highest incidence rate was 164.1 and the lowest
was 40.0 cases of selected enteric illnesses, per 100,000 population.
14. Respiratory Infection Outbreaks in Long-Term Care Homes
The respiratory infection outbreak indicator estimates the number of confirmed respiratory infection
outbreaks in long-term care homes between September 1, 2006 and August 31, 2007.
Respiratory tract infections such as the common cold (Rhinovirus), adenovirus, and influenza, along with
other respiratory pathogens, are spread through contact with an infected person via droplets from coughs,
sneezes, and tissues or surfaces contaminated with the virus. Although symptoms vary depending on the
Iii
Selected enteric illnesses reporting fields include: Amebiasis; Botulism; Campylobacter Enteritis; Cholera; Cryptosporidiosis;
Cyclosporariasis; Food Poisoning, All Causes; Gastroenteritis, Institutional Outbreaks; Giardiasis; Hepatitis A; Listeriosis; Paratyphoid fever;
Typhoid Fever; Salmonellosis; Shigellosis; Trichinosis; Verotoxin producing E.coli including Hemolytic Uremic syndrome (HUS); Yersiniosis
Population Health Indicators

47
Initial Report on Public Health 2009
causative agent, they generally include nasal congestion, cough, running nose, sore throat, fever, sneezing,
and fatigue.
A confirmed respiratory infection outbreak in a long-term care home is defined as:
• Twocasesofacuterespiratorytractillness,atleastoneofwhichmustbelaboratoryconfirmed;or
• Threecasesofacuterespiratorytractillnessoccurringwithin48hoursinageographicarea
(e.g. unit, floor); or
• Morethantwounitshavingacaseofacuterespiratorytractillnesswithin48hours.
105
Respiratory tract infections are one of the most commonly diagnosed infections of long-term care home
residents. Long term care residents are predisposed to such infections in part because they may:
• beelderly
• havechronicillnesseswhichweakentheirimmunesystem
• havechroniclungorneurologicaldiseasewhichimpairstheirabilitytoclearsecretionsfromtheirlungs
and airways
Residents are also at risk because they are often already medically compromised and many viral and bacterial
respiratory pathogens are easily transmitted in an institutional environment. Thus, respiratory infections can
result in substantial morbidity and mortality in residents of long-term care homes.
106,107
Public health units provide support to long-term care homes to prevent and reduce the spread of infectious
diseases. This includes:
• promotinginfluenzaimmunizationtostaffandresidents
• providingeducationtostaffoninfectiousdiseaseprevention
• workinginpartnershipwithstaffto:
– develop infection prevention and control policies and procedures
– develop an outbreak contingency plan surveillance system
– assist in the prevention, investigation, confirmation and management of cases and outbreaks
The number of outbreaks provides an indication of the workload and resources required of public health units
to carry out appropriate response and investigations, to prevent the further spread of illness, and to prevent
death. A high number of outbreaks should not be considered a sign of poor performance by a health unit, but
may indicate an effective surveillance strategy and strong working relationships between long term care homes
and a local public health unit staff. The data presented reflect the number of outbreaks and not closures due to
outbreaks.
Through long-term care home reporting of respiratory infection outbreaks to public health units, early detection
and investigation of outbreaks and implementation of appropriate infection control measures can be put in
place to limit further transmission, illness and death.
Between September 1, 2006 and August 31, 2007 there were a total of 602 respiratory infection outbreaks in
Ontario long-term care homes. Based on 36 public health units, the highest number of respiratory infection
outbreaks in long-term care homes was 113 and the lowest number was zero.

48
15. Chlamydia Incidence
The age-standardized chlamydia incidence rate indicator estimates the total number of reported chlamydia
cases per 100,000 population.
Chlamydia is the most common bacterial sexually transmitted bacterial infection (STI) in Canada.
108
If left
untreated in women, it can cause complications such as pelvic inflammatory disease which can lead to ectopic
pregnancies, infertility, and septicaemia. In men, untreated infections can cause inflammation of the testicles
and prostate which can also lead to infertility.
109
Public health units play a significant role in the prevention and management of STIs through the programs
and services they provide. These programs and services include:
• promotinghealthysexuality
• providingsexualhealthclinicalservices
• providingtestingandcounsellingforSTIs
• providingcaseandcontactmanagementofSTIcases
• providingtreatmentforChlamydiaatnocosttotheclient
Individuals infected with one STI are at a higher risk of contracting another STI, including HIV. By improving
counselling, screening, diagnosis and treatment of chlamydia, public health units can help decrease new cases
of other STIs.
The highest incidence rate of chlamydia infections is found in young adults aged 15-24.
108
In recent years,
the number of reported cases has been increasing. While this reflects a real increase in infection rates, it
is also believed to reflect an increase in partner notification, expanded screening efforts and improved
diagnostic testing.
In2007,theincidencerateofreportedchlamydiacasesinOntariowas219.8per100,000population.Based
on36publichealthunitsinOntario,thehighestincidencerateofreportedchlamydiacaseswas678.9andthe
lowestincidencerateofreportedofchlamydiacaseswas78.9,per100,000population.
16. Immunization Coverage for Hepatitis B
The immunization coverage for hepatitis B indicator estimates the proportion of grade 7 students who have
completed the immunization series against hepatitis B by the end of grade 7.
Hepatitis B is caused by a virus that attacks, and can permanently damage, the liver. It is the leading cause of
liver cancer worldwide.
110
The highly contagious virus is spread through close contact with infected bodily
fluids including blood. Unprotected sexual contact is the most common risk factor for hepatitis B infection in
Ontario.
111
Sharing needles with an infected person is another risk factor for infection.
112
In Ontario, publicly funded hepatitis B vaccines are provided for specific populations including those at higher
risk due to lifestyle, or due to being a contact, being a carrier, or having been diagnosed with an acute liver
Population Health Indicators

49
Initial Report on Public Health 2009
disease. In addition, a universal vaccination program is administered by public health units through a school-
basedprogramtostudentsingrade7.Thereisalsoacatch-upprogramforstudentsingrade8whomayhave
missed some or all of the vaccine series in grade 7.
Hepatitis B coverage among students is a unique indicator in that it speaks to the efficacy of a program over
which public health units have direct control at the local level.
Public health units plan and deliver school-based hepatitis B immunization clinics. This indicator reflects the
appropriate planning and delivery of school-based hepatitis B immunization clinics, public health unit efforts
to educate parents and children and promote uptake of hepatitis B immunization, and public health unit data
gathering with respect to hepatitis B immunization.
Attheendofthe2007-2008schoolyear79.8%ofgrade7studentsinOntariocompletedtheimmunizationseries
against hepatitis B. Based on 36 public health units in Ontario, the highest coverage was 95.2% and the lowest
coverage was 65.2% of grade 7 students who completed the two-dose series against hepatitis B.
Toronto Cancer Prevention Coalition Case Study
Case Study 9
The
TorontoCancerPreventionCoalitionwascreatedin1998byToronto Public
Health and community partners and is North America’s largest municipal
cancer prevention coalition. In November 2002, City Council endorsed the Coalition Action
Plan as the cornerstone of cancer prevention in the City of Toronto.
The strength of the coalition lies in its dedicated membership. For the first time in history,
governments, universities, unions, health and environmental agencies, school boards,
grassroots groups, activists and survivors have brought their individual expertise to the
coalition and its comprehensive agenda for cancer prevention. The coalition’s work has
accomplished or influenced prevention work being done throughout Canada today.
In 2007, the Toronto Board of Health endorsed a policy statement for shade for the City of
Toronto which was forwarded to City Managers for implementation and has since been a
catalyst for additional pilot projects, activities and advocacy work in effectively reducing
overexposure to ultraviolet radiation within the city’s facilities.

50
17. Immunization Coverage for Measles, Mumps and Rubella
The immunization coverage for measles, mumps and rubella indicator estimates the proportion of school
children age 7 years who are known to be complete for age for vaccination against measles, mumps and
rubella.
Several vaccines are currently provided through the publicly funded immunization program to reduce the
incidence of vaccine preventable diseases.
113
Publicly funded vaccines are provided for routine immunization,
the immunization of high-risk persons, and the control of disease outbreaks. The measles virus is highly
contagious and can result in respiratory complications and death in extreme cases;
114
mumps can cause
sterility and subfertility in adult males;
115
and the rubella virus is a respiratory disease that causes rash
and fever. If contracted by a pregnant woman, the rubella virus can have devastating consequences on the
developing fetus.
116
The combined measles, mumps and rubella (MMR) vaccine became available in 1975. It is administered to
Ontariochildrenonoraftertheirfirstbirthdayandagainatage18monthsaspartofthePubliclyFunded
Immunization Schedules. Under the Immunization of School Pupils Act (ISPA), all school pupils must have
documented receipt of two doses of measles and one dose each of mumps and rubella by 7 years of age for
school attendance, unless a valid exemption is provided.
117
Children receive this immunization primarily
through primary care physicians or through public health unit clinics.
Public health units are required to assess the immunization status of all school pupils and attendees of
licensed day nurseries on a yearly basis to determine their immunization status and in the case of school
pupils, the medical officer of health may issue suspension orders to school principals, where required, to
remove non-immunized children from school. The process also provides important information to public
health units regarding vulnerable children and populations in order to target these groups for immunization
and to plan for potential outbreaks of disease. Public health units also provide recommendations to parents
to immunize infants and children whose immunization is not up to date to ensure that both day nursery
attendees and school pupils are appropriately immunized.
Having up to date MMR immunization at age 7 contributes to the timely and effective detection and
identification of children and priority populations facing barriers to immunization who may be susceptible
to vaccine preventable diseases, and their associated risk factors, as well as to any emerging immunization
trends. It relates to the public’s awareness of the importance of immunization across the lifespan and the
achievement of target coverage rates for provincially-funded immunizations.
Attheendofthe2007-2008schoolyear84.9%ofschoolchildreninOntarioage7yearswereknowntobe
complete for age for vaccination against measles, mumps and rubella. Based on 36 public health units in
Ontario,thehighestcoveragewas97.8%andthelowestcoveragewas20.7%ofschoolchildrenage7years
known to be complete for age for vaccination against measles, mumps and rubella.
Population Health Indicators

51
Initial Report on Public Health 2009
18. Adverse Water Quality Incidents
The adverse water quality incidents indicator identifies the number of adverse water quality incidents from
drinking water systems subject to O.Reg 170/03/O.Reg 252/05 and unregistered drinking water systems. An
adverse drinking water incident occurs when a water sample test result exceeds the Ontario Drinking Water
QualityStandards
118
or an operator observes that the system may not be providing safe water.
Contaminated drinking water can lead to serious health concerns. Most water-related health problems are
caused by microbial or chemical contamination and can result in illnesses ranging from mild gastroenteritis,
to disease outbreaks including E. coli infections, giardiasis and cryptosporidiosis.
Public health programs and services, together with programs through the Ministry of the Environment, aim to
prevent or reduce the occurance of water-borne illness:
• throughtimelyandeffectivedetectionandidentificationofwatercontaminantsandillnesses,
their associated risk factors and emerging trends
• mitigatingwater-borneillness
• usingevidencetoinfluencethedevelopmentofhealthypublicpolicytoreducetheburdenofwater-borne
illnesses of public health importance
• ensuringpublicawarenessofdrinkingwatersafetyandtheimportanceofsourceprotection
Boards of health must ensure that the medical officer of health, or designate, is available 24 hours a day, 7 days a
week to receive and respond to reports of adverse water quality incidents. Public health units are also involved
in providing input into the development of legislation and regulations in order to ensure that the minimum
standards for public water systems reflect evidence informed best practices.
The safety of drinking water is a major concern throughout Ontario, especially since the Walkerton
contaminated drinking water incident in 2000.
Thereareabout2,855drinkingwatersystemsinOntarioasofFebruary2008governedundertheSafe Drinking
Water Act
119
Regulation 170/03.
120
These include year-round residential systems as well as those that supply
watertodesignatedfacilitiessuchasschools,daycaresandnursinghomes.Anadditional18,000smalldrinking
watersystemsfallunderOntarioRegulation318/08
121
(Transitional- Small Drinking Water Systems) and Ontario
Regulation319/08,
122
(Small Drinking Water Systems).
There are wide variations in the size and complexity of the drinking water systems that fall under the various
regulations. These variations have a direct bearing on the water sampling and testing frequency and, ultimately,
the number of adverse water quality incidents which may occur.
In2007therewereatotalof4,458adversedrinkingwaterincidentsinOntarioforallsystemtypes.Basedon
36 public health units in Ontario the highest number of adverse drinking water incidents was 446 and the lowest
number was 13 for the calendar year of 2007. The wide variation of reported adverse water quality incidents
among public health units reflects the number of regulated drinking water systems within each health unit
as well as the size of the population served by the systems. Systems serving larger populations have greater
sampling frequency requirements.

52
SPARK Youth Website Case Study
Case Study 10
Substance
misuse prevention initiatives need to match both the
community characteristics and the needs of the population
being served. Huron County Health Unit, which is located in a rural region, has developed
a web based intervention that is designed to reduce barriers that rural youth face in accessing
health information such as distance, transportation, lack of anonymity, and a general lack of
youth health and social services.
Since local rates of youth alcohol abuse are significantly higher than the provincial average,
the website content focuses on alcohol and drug abuse, but also contains information on a
variety of health topics, including healthy sexuality, relationships, and mental health. There
is a strong evaluation component to this project to ensure this interactive, youth-led site is
continually evolving to meet the needs of local youth.
By providing employment for 6 youth in the initial stages of the design and maintenance of
the website itself and currently employing 1 SPARK youth ambassador, the SPARK youth
website is designed to give at-risk youth in Huron County the opportunity to develop the
skills to:
• designandmaintainahealth-promotionwebsiteand
• buildthewebsiteintoareliablesourceofpublichealthinformationfor
Huron County youth
The website, found at www.youthspark.ca includes personal stories, local information and
announcements of events. It also has open forums for youth to find answers together, and to
connect with health professionals who can answer questions anonymously.
Population Health Indicators

53
Initial Report on Public Health 2009
Governing bodies are responsible for the general oversight and direction of an organization. Effective
governance is required for efficient program management, fiscal accountability, and the achievement of
organizational objectives. Good governance is achieved through the implementation of guidelines and
mechanisms which ensure that appropriate actions are taken when needed, and that the public is protected.
Governance is a multi-faceted subject. A well governed organization will feature:
• anabilitytofocusonstrategicmatters
• aclearunderstandingofthepurposeoftheorganization
• cleardelineationbetweenboardandadministrativeroles,responsibilities,andaccountabilities
• anabilityfortheboardtomanageitselfeffectively
• boardtimeusedtofocusonthemostimportantissues
• administrativestaffhavethefreedomtooperatewithintheconfinesofstatedpolicies
• alignmentofresourceswithgoalsoftheorganization
107
Being able to demonstrate effective governance is a key component of any performance management system.
Strengthened and consistent governance is the foundation for all other reforms to revitalize public health in
Ontario.
In this report, three key aspects of organizational effectiveness are presented. They are 1) board of health
finances, 2) human resource issues and 3) board operations.
ThedataforthissectionofthereportwerecollectedviaasurveyofboardsofhealthinNovember2008.
The survey tool is available on the report website at: www.health.gov.on.ca/english/public/pub/pubhealth/init_
report/index.html. A summary of the survey data can be found in Table 2: Indicators by Public Health Unit.
This information builds on the previous work of the CRC, which also conducted a survey of boards of health
in June 2005. To support the CRC, MOHLTC sent all health units in Ontario an extensive, online survey about
issues such as governance, funding, accountability, human resources and their research and knowledge
transfer capacity. Health units were asked to describe their management and reporting structures, as well
as the strategies they use to recruit and support their boards, and to assess performance. These results were
presented in the CRC Interim Report.
123
19. Total Board of Health Expenditures
The indicator for total board of health expenditures is defined as the total board of health expenditures
for “core and related public health programs and services”, from all sources, including all government
funding, user fees, one time funding, fee for service contracts, and donations.
Expenditure data are one of the most basic pieces of baseline information used to describe an organization.
They provide context to other information that describes the size, scope, diversity and complexity of an
organization’s operations.
Governance and Accountability Indicators
Group B

54
Boards of health were asked to report on revenues from all sources, and to categorize their funding by whether
it was for a core public health program, a program related to public health, or for a program that is outside the
traditional public health functions. Note that these categories do not align with those used by the ministry in
its Program Based Grant funding package, where “related” programs has a specific meaning; further details are
available within the data definition for this indicator.
This report marks the first time that this level of information has been presented on board of health budgets in a
way that allows for comparisons across the province. It is important to note that because this was the first time
that this information was collected, the completeness and consistency of reporting within the funding categories
limits the validity of comparisons between boards using this data.
Because boards self defined which of their programs fit within each of the expenditure categories, there was
some inconsistency in the reporting. Based on the information gathered from this first effort to collect board
of health expenditure data, future iterations of this question will be able to support more consistent data
collection and reporting. Despite this limitation, the reported expenditure data give an overall sense of the
relative range and scope of program spending across Ontario.
The expenditure data also begin to provide a picture of the complexity of managing the delivery of public
health in Ontario, as evidenced by the variation in the number of separate programs that boards of health are
administering. While some boards of health focus primarily on delivering core public health programs, others
are providing a large number of different programs, most with separate funding streams.
Expenditures for public health programs and services from all revenue sources for all boards of health were
reportedtobe$837.7Min2007.Programfundingisprovidedprimarilybythethreeministrieswithresponsibility
for public health: Ministry of Health and Long-Term Care, Ministry of Health Promotion and Ministry of Children
and Youth Services. In addition, some boards of health receive funding from the federal government (e.g., for the
Canada Prenatal Nutrition Program) and collect fee for service revenues related to septic inspections.
20. Board of Health Expenditure Variance
The indicator board of health expenditure variance is defined as the percentage variance between a board of
health’s projected annual budget for “core and related public health programs and services” and year-end
actual expenditures with revenue from all sources.
Expenditure variance measures the effectiveness of internal fiscal management. A small amount of variance
is expected, unless there are unforeseen events that result in one time financial anomalies.
Of the 36 boards of health, a total of 30 reported overall underspending totaling $34.6M in 2007, which
represents approximately 4.0% of board of health budgets for core and related programs.
The most commonly cited reasons for underspending were staff vacancies due to difficulty in recruiting
(citedby21boardsofhealth),delaysinrecruitingduetodelayinbudgetapprovals(citedby18boardsof
health) and cost containment initiatives or planned gapping to actively manage expenditures.
The presence of surpluses is partly due to the timing of provincial government decisions on funding levels.
While some municipalities will provide cash flow early in the calendar year in anticipation of government
Governance and Accountability Indicators

55
Initial Report on Public Health 2009
announcements of funding increases, others wait until the approval letters are received before allowing
boards of health to spend at the new level.
Because of the lack of alignment between the fiscal years used by boards of health (January to December)
and the provincial government (April to March), provincial funding approvals are not provided until well
into the operational year for public health programs and services. Some municipalities delay their approvals
to avoid financial risks, but this leaves little time for public health units to adjust their spending or program
service levels either up or down to accommodate the provincial funding adjustment.
Overspending totaled $1.6M in 2007, which accounts for less than one percent of reported planned
expendituresof$870.7M.Outofthetotalofsixboardsofhealththatreportedoverspending,three
accountedfor88%ofthetotal.
The commonly cited reasons for overspending were unexpected demand for programs (cited by 5 boards of
health), funding shortfalls (cited by 4 boards of health) and unanticipated in-year costs (e.g., training, one
time purchases of office equipment).
First Nations Children’s Oral Health Initiative Case Study
Many
health units are working in innovative ways with First Nations communities
to address local health needs and build collaborative partnerships that will
support improved communication and planning.
For example, in September 2004 the Northwestern Health Unit (NWHU) partnered with
Health Canada to enrol five new First Nations communities in the Children’s Oral Health
Initiative (COHI), pilot program, and to date 19 communities are involved. The initiative
addresses the high rates of preventable dental disease in First Nations and Inuit communities
in Canada.
Under the program the NWHU provides diversified oral health promotion activities, such
as: education, oral health assessments, screenings, fluoride varnish, sealants, scaling, and
oral hygiene instruction. Yearly baseline epidemiological data are collected and used to
implement and evaluate the program and determine trends in oral disease.
This strategy has broken down the federal/provincial/First Nations jurisdictional barriers
and ties in nicely with other tripartite initiatives across Canada, enabling health unit staff to
provide desperately needed services to children under federal jurisdiction.
The ultimate goal is to empower communities to provide these services themselves.
Case Study 11

56
21. Expenditures on Training and Professional Development
The indicator for expenditures on training and professional development is defined as the percentage of board
of health total actual expenditures for “core and related public health programs and services” used to support
staff training and professional development costs.
Spending on training and professional development is a measure of a board of health’s investment to support
staff in their ongoing skill enhancement and maintenance for effective public health practice. Given the
emphasis on the need to use evidence informed approaches, it is essential that staff have opportunities
to enhance their knowledge. Access to current information on new methods of practice contributes to
improvements in the delivery of public health programs and services.
Boards of health report that their expenditures on training and development in 2007 ranged from 0.15% to
1.65% of their total budgets, with most under 1% (32 out of 36).
The CRC recognized that professional development is a key to increasing staff satisfaction, improving staff
retention and improving the quality of public health service delivery. Their report comments that public
health units need deliberate strategies to provide professional development to address both program and
discipline needs, and that innovative strategies need to be considered, such as subsidized refresher courses,
scholarship programs, training networks and activities related to developing core competencies. The CRC
recommended that public health units support training and staff development with expenditures in the range
of 1% - 2% of their overall budgets.
124
22. Numbers of FTEs by Job Category
The indicator number of FTEs by job category is defined as the number of FTE positions in 2007 in each of
the following professional job categories: public health nurse, registered nurse, registered practical nurse,
nurse practitioner, public health inspector, dentist, dental hygienist/dental assistant, health promoter,
dietitian/public health nutritionist, speech-language pathologist, epidemiologist, heart health coordinator
and librarian.
Information on the number of staff positions in specific job categories provides context for understanding
current human resource capacities in terms of the range and size of staff complements of boards of health.
Information was collected on the number of FTE positions in these selected job categories because of the
persistent concerns within the sector regarding the potential for gaps in human resource capacity in these
professional job categories, and the need to establish context for consideration of this issue.
The table below indicates that the single most common job category in public health units is public health
nurse. All 36 public health units also have public health inspectors, dental hygienists/dental assistants and
dietitians/public health nutritionists, and almost all have health promoters (33 public health units) and
epidemiologists (35 public health units).
Less than half of public health units employ librarians (17 public health units) and speech-language pathologists
(12 public health units). Information on the remaining job categories that were included in the board of health
survey but not shown in the table below is available in Table 2: Indicators by Public Health Unit.
Governance and Accountability Indicators

57
Initial Report on Public Health 2009
Numbers of FTEs by Specific Job Categories
Number of public health
units reporting FTEs
Total FTEs across
all health units
Median across
all health units
Public health nurses 36 2,717.2 45.5
Public health inspectors 36 900.5 14.0
Dental hygienists/dental assistants 36 286.1 4.4
Dietitian/nutritionists 36 203.1 3.4
Health promoters 33 416.7 6.2
Epidemiologists 35 72.6 1.0
Nurse practitioners 19 28.5 1.1
Librarians 17 20.1 1.0
Speech-language pathologists 12 64.3 4.4
First Nations, Métis and Inuit Diabetes Network Case Study
An
example of current work taking place with First Nations is Ottawa Public Health’s
work with the First Nations, Métis and Inuit Diabetes Network. With diabetes
among Ontario Aboriginals three times higher than that in non-Aboriginal populations, the
Ottawa Aboriginal community recognized the need for a more coordinated approach to
diabetes education. Ottawa Public Health, working with Ottawa Aboriginal organizations,
initiated the formation of a network that includes the Canadian Diabetes Association, Heart
and Stroke Foundation, and the Diabetes Education Program of Ottawa.
The strength of the First Nations, Métis and Inuit Diabetes Network is its Aboriginal
membership and its commitment to collectively engage, discuss, and arrive at a shared
understanding on planning diabetes education while ensuring the efforts reflect the three
distinct populations. As a result, the network has been able to move toward developing
and sharing culturally relevant resources, training, and service approaches to diabetes
prevention, as well as bring a focus to the prevention of other chronic diseases.
The First Nations, Métis and Inuit Diabetes Network is building on its interdisciplinary
and intersectoral membership to attract new service, research, and academic partners to
work together to reduce the burden of this preventable chronic disease among Ottawa’s
approximately 60,000 Aboriginals.
Case Study 12

58
23. Number of Vacant Positions by Job Category
The number of vacant positions by job category is defined as the number of job vacancies for staff positions
in the following job categories for which there had been a job posting and that had remained vacant
between May 1, 2008 and date of survey in November, 2008. The job categories are: associate medical
officer of health, public health nurse, registered nurse, registered practical nurse, nurse practitioner,
public health inspector, dentist, dental hygienist/dental assistant, health promoter, dietitian/public health
nutritionist, speech-language pathologist, epidemiologist, heart health coordinator and librarian.
Information on the number of vacancies in specific job categories is important because it identifies areas
of potential gaps in public health unit human resource capacity that may have both local and system wide
implications.
Boards of health were asked to report the number of positions that had been advertised and had remained
vacant over the last six months in specific job categories. This indicator measures persistent vacancies that
boards of health are trying to fill but where they have been unable to attract suitable candidates.
Boards of health reported minimal persistent vacancies in positions for registered nurses, registered practical
nurses, dentists, and librarians. In each of these categories, the number of job vacancies that had remained
unfilled after a six month posting was less than 1 FTE across all public health units.
The largest proportion of ongoing vacancies in public health units are for associate medical officer of
health positions, with almost 25% of the total reported FTE positions sitting vacant for the last six months,
and for nurse practitioners with approximately 15% of the total reported FTE positions vacant over the
last six months. The other job categories where concern about the inability to fill positions has been noted
(epidemiologist, registered practical nurse, speech-language pathologist) show province wide vacancy rates
of between 4.7% and 9.1%.
Numbers of Vacant Positions by Job Categories
Associate MOH
Nurse
practitioner
Epidemiologist
Registered
practical nurse
Speech-language
pathologist
Total number of vacant
positions (for the last
6 months)
6.3 4.4 6.5 5.5 3.0
Total FTE staff positions 25.6 28.5 71.6 100.3 64.3
Total number of vacant
positions as a % of Total
FTE staff positions
24.6% 15.3% 9.1% 5.5% 4.7%
Boards of health also reported that these numbers may underrepresent the impact of persistent vacancies
because of the lateral movement of staff into vacant positions to backfill for a maternity leave, or as part
of a vacancy management plan that delays recruitment for a part of a year. These types of situations were
specifically excluded from this measure, in order to get a picture of long term vacancies in certain job
categories.
Governance and Accountability Indicators

59
Initial Report on Public Health 2009
24. Employment Status of Medical Officers of Health
The indicator employment status of medical officers of health is defined as a situation where the medical
officer of health is employed on a permanent full time basis with the board of health.
Strong medical officer of health (MOH) leadership is essential in public health to protect the community’s health,
and assume overall responsibility for management of the delivery of public health programs and services.
Under the HPPA, each board of health is responsible for recruiting a qualified MOH to fill the position on a
permanent, full time basis. In the event that the MOH office becomes vacant, the Act requires that the board
of health appoint an Acting MOH while it works expeditiously to fill the position. Boards may also appoint
one or more Associate MOHs.
The appointment of both MOHs and AMOHs requires approval by the Minister of Health and Long-Term Care
and the qualifications for these positions are specified in regulation.
Healthy Menus for Arenas Case Study
In
developing strategies to encourage healthy eating, health units are exploring ways to
get beyond the use of broadcast messages to a whole population and are looking at
strategies that address the specific locations where people eat meals away from home.
An innovative local approach led by the Durham Region Health Department is occurring
whereby a Healthy Menus for Arenas program is currently operating in five Durham arenas.
This program was based on the positive results of a 2007 pilot study, which found that arena
users will make healthy food choices if options are available at arena concession stands.
Healthy menu options were developed by Public Health Nurses and Nutritionists in
collaboration with the Heart and Stroke Foundation of Ontario, Canadian Cancer Society,
Canadian Diabetes Association, Canadian Liver Foundation, FoodSense Vending Services,
and local Municipal Recreation Facilities.
Further initiatives have also been introduced in support of healthy eating in other recreational
facilities, including a communication campaign and a coaches’ incentive program. Along with
Health Department funding, financial support has also been received from the local Heart
Health Coalition (Durham Lives!), the Public Health Agency of Canada’s Diabetes Strategy,
and the Canadian Cancer Society, Ontario Division.
Case Study 13

60
Public health units with acting MOHs (as of December 31st, 2008)
Type of Public Health Unit Public Health Unit
Length of time MOH position has
been filled on an acting basis
Rural Northern Regions
Northwestern > 2 years
Porcupine > 7 years
Mainly Rural
Eastern Ontario > 2 years
Elgin-St. Thomas > 12 years
Haldimand-Norfolk > 12 years
Oxford County > 11 years
Perth District > 2 years
Urban/Rural Mix
Chatham-Kent > 6 years
Lambton > 10 years
Sparsely Populated Urban-Rural Mix
Timiskaming > 12 years
Urban Centres Wellington-Dufferin-Guelph > 3 years
In terms of full time status, three public health units reported that they have MOHs who are working less than
a full time equivalent, and two public health units share one FTE.
Governance and Accountability Indicators
Building Internal Evaluation Capacity Case Study
The
Leeds, Grenville and Lanark District Health Unit has developed a plan to
build organizational capacity for program evaluation and evidence-based public
health practice. The goal is to integrate the planning and evaluation function into all public
health professional job functions within the health unit and thus build an organizational
culture of continuous quality improvement.
The plan involves implementing a comprehensive strategy of policies, supportive
environments, infrastructure development, and staff education and training. The goal of the
plan is to enhance the skills of public health professionals in the foundations of effective,
evidence-based public health practice. The strategy includes the launch of a learning
series to enhance knowledge and skills, and the creation of an Evaluation Community of
Practice, which is an informal network supporting the exchange of ideas and experiences
in program evaluation.
Ultimately, building organizational capacity for program evaluation will enhance
accountability to stakeholders and the quality of public health programs delivered to the
community.
Case Study 14

61
Initial Report on Public Health 2009
25. Staff Length of Service
The indicator staff length of service is defined as the percent of current full and part time public health unit
staff who have been employed continuously by the public health unit, by length of service.
Length of staff service is a commonly used measure of staff retention and turnover. High staff turnover rates
affect organizational stability and capacity, since it is recognized that an organization needs to retain staff in
order to maintain stability in operations, transfer corporate knowledge, and support the orientation of new
staff. On the other hand, an organization where the majority of staff have over 20 years of service may have
less change in their organizational culture.
Board of health reporting on the length of service of their staff is summarized in the table below. The figures
represent the percentage of the staff in a board of health that were reported to have been with the board of
health for the designated period of time.
Across the province, about 9% of staff have been with their board of health for less than one year. In this
category, the majority of boards (27) reported rates between 5% and 15%, with one board having double the
average, with just over 20% of their staff in this category.
Data collected through the survey of public health units found that:
• inthe“morethan1yearbutlessthan5years”category,20boardsreportedthisastheirpeakinstaff
length of service, with ranges from 19.2% to 43.0% of all staff.
• inthecategory“morethan5butlessthan10years”,13boardsreportedthatthemajorityoftheirstaffhad
alengthofservicethatfitwithinthiscategory,withratesrangingfrom16.4%to38.0%.
For the majority of public health units, the highest proportion of staff were in these two specific categories.
This suggests that staff may be near the beginning of their careers or are moving between public health units
every few years.
Staff Length of Service
Rates across
all public
health units
Up to 1 year
More than 1 year,
but less than
5 years
More than 5,
but less than
10 years
More than 10,
but less than
20 years
More than
20 years
Lowest % 0.0% 19.2% 16.4% 6.6% 4.6%
Highest % 20.5% 43.0% 38.0% 31.3% 21.0%
Average length
of service – all
health units
9.3% 31.3% 27.8% 18.0% 13.6%

62
In a few cases, boards of health were unable to confirm whether all their staff had worked continuously for
the public health unit or had spent some time working in other departments within the municipal or regional
government. This will primarily impact the reporting on administrative and corporate support staff (such
as IT, communications, HR), who have transferable skills. Given that these staff positions are a minority of
all public health positions, the effect will be minor but it may have skewed the length of service upward for
boards of health that are part of municipal or regional governments, since the reporting was on staff length of
service with the same employer.
26. Familiarity with Public Health Unit Programs and Services
The indicator familiarity with public health unit programs and services is defined as whether a board of
health has assessed local community members’ familiarity with any of the public health unit’s programs
and services.
Although it is an important component of public health practice, indicators that measure community engagement
and awareness of public health are not yet well developed or validated. For this report, data were collected from
boards of health on whether they had assessed local community members’ familiarity with their programs and
services. Of the 36 boards of health, 26 reported that they had most recently conducted an assessment on this
issuebetween2005and2008,andafurther6hadlastconductedanassessmentbetween1998and2004.
In other jurisdictions, the leading edge practice is to collect information on community partners’ awareness of
a public health organization directly from the partner organizations and stakeholders. Survey tools are used
to question staff in settings such as other health care services, schools, housing organizations and outreach
programs about their knowledge and opinions of the availability and delivery of public health services in their
community.
Building community awareness is a necessary first step towards building community engagement. But this is
a challenge for public health because interventions are often invisible to the community. Public health does
not usually receive credit for news stories that do not happen, such as preventing disease outbreaks or long
term health outcomes that are improved for a whole population over a generation.
Because of this paradox, members of the general public are often unaware of the role and mandate of public
health. Community organizations that public health works with every day may also under estimate the role
that public health plays in influencing public policy and contributing to new knowledge about what works to
create and sustain change in communities.
The foundational principles guiding public health service delivery in Ontario speak directly to the issue of
partnership and collaboration. The OPHS describe partnership and collaboration as involving partnerships
within the health sector (e.g., Local Health Integration Networks and primary health care) and other sectors
(e.g., education, social services, housing, workplace health and safety system, and environment).
Community collaborations and citizen engagement can occur in the areas of assessment, planning, delivery,
management, and evaluation of programs and services. Boards of health need to use their influence to achieve
and maintain the leadership role required to create the conditions necessary for effective program outcomes.
Governance and Accountability Indicators

63
Initial Report on Public Health 2009
27. Issuance of a Health Status Report
The indicator issuance of a health status report is defined as situations where a board of health has issued a
health status report or other health intelligence or information product that considered inequities in health
outcomes and health determinants.
A health status report or other health intelligence or information product includes any publication designed
for distribution to the public and partners that used health status statistics and provided analysis of these
statistics to describe the inequity of health outcomes or health determinants among various populations in
the public health unit’s catchment area.
The Health Bus Case Study
Case Study 15
The
Health Bus began as a vision of the Niagara-based Wise Guys charity, which provided
funding to allow Niagara Region Public Health to purchase a bus and convert it
into a mobile health care facility for the homeless. The Health Bus is permanently staffed by a
team leader and a public health nurse. In addition, staff from the sexual health program, the dental
program and the mental health program provide services on a rotating or occasional basis.
The initial homeless target population has been expanded to include vulnerable, marginalized,
and isolated populations. Niagara Region Public Health undertook extensive collaboration and
consultation with community partners to determine the services required and the best locations
at which to reach the target population, and works to keep community agencies abreast of Health
Bus services and service locations.
The Health Bus provides a wide range of health services, including:
• treatmentforminormedicalconditions
• general,mental,andsexualhealthcounselling
• footcare
• immunizations
• sexuallytransmitteddiseasetestingandtreatment
• needleexchange
• dentalassessmentsand
• referralstoappropriatemedicalanddentalserviceproviders
Despite demands to expand the coverage area, the Health Bus has been able to maintain its focus
on providing access to the target population. One of the Health Bus’s strengths is its visibility
and the trust it has developed with the target population. The Health Bus has been successful
in increasing client, community, and staff satisfaction in providing health care to a traditionally
poorly served population.

64
Issuing a health status report provides information about the community which the public health unit serves
that can be used to guide programming and resource decisions. It also works to educate the community about
the role of public health programs in keeping a community healthy.
Health status reports are usually customized to highlight local issues. They can be about a single issue or a
specific population or age group, or they can provide an overview of the general health of a community, often
in comparison to provincial or national averages.
Allboardsofhealthissuedalocalhealthstatusreportbetween2006and2008,withoneexception,which
issued a report in 2000.
Governance and Accountability Indicators
Collaboration with First Nations Case Study
As
an example of inclusion at the governance level, the Peterborough County-
City Board of Health (PCCHU) has signed an agreement with Curve Lake First
Nation and Hiawatha First Nation for comprehensive public health services.
Both communities contribute their share of the 25% local funding, and the council of each
band appoints one of its members to the board of health for one, two, or three years. Curve
Lake First Nation and Hiawatha First Nation also may jointly appoint a representative. In
Peterborough, Curve Lake First Nation Chief Keith Knott has served as a Board Member
since 2002, including a term as Chair in 2004. The relationship with these two communities
continues to evolve and PCCHU continues to act as a resource, a facilitator, an educator,
a trainer, and an advocate as needs arise.
PCCHU has partnered with staff at the Curve Lake First Nation Health Centre on a youth
tobacco-prevention strategy. Curve Lake First Nation and Hiawatha First Nation are part-
ners in the Health Canada funded smoking cessation project and also have partnered with
PCCHU on a proposal to the Canadian Tobacco Control Research Initiative.
Services offered by the health unit, such as HBHC home-visiting, food handler training and
certification, parenting groups (such as Nobody’s Perfect), and food security initiatives,
such as “Come Cook with Me” enhance the programs that already exist within the First
Nation. Child care is provided, so parents can have some time for themselves, forge new
friendships, and learn new skills.
Case Study 16

65
Initial Report on Public Health 2009
28. Strategic Plan
The indicator for strategic plan is defined as whether a board of health reports having a strategic plan in
place that covers the current period (2008).
A strategic plan is an organizational document that generally covers a period of three to five years, presents
the organization’s mission and vision, describes the relationship of programs to community needs and
establishes priorities for action within a specific timeframe and with specific resources.
The existence of a strategic plan is an indicator of good governance because it signals a purposeful approach
to planning and priority setting for the organization. Such plans are also a key element in capacity building
because they provide an opportunity for an organization to consider its strengths and weaknesses, and to
make plans to address these.
Strategic plans are commonly used among boards of health, with 24 of the 36 boards of health reporting
havingastrategicplancurrentasof2008.Threeboardsofhealthhadstrategicplansthatexpiredpriorto
2008,twoboardsofhealthhaveastrategicplanthatbeganin2009,andsevenreportedthattheydonothave
a strategic plan in place.
29. Emergency Response Plan Tested
The indicator emergency response plan tested is defined as whether a board of health has an internal
emergency response plan and whether it was tested between January 1, 2007 and the date of the survey
in November, 2008. Testing an emergency response plan would include activities such as running a table top
exercise, testing a telephone contact list of all staff, and staging a mock emergency scenario.
All boards of health reported that they had an internal emergency response plan in place, and the majority (29)
had tested their plans since January 1, 2007. Seven boards of health reported they had not tested their plans
since this date.
Of the 29 boards of health that reported they had tested their plans, most used more than one method to assess
thestrengthsandweaknessesoftheirplans.Themostcommonmethodsweretabletopexercises(18boardsof
health) and scenarios or simulations (17 boards of health). The third most common method, used by 15 boards
of health, was to conduct a call out or fan out exercise, which tests the ability to contact all staff or designated
people by telephone and other electronic means.
More than seventy percent of boards of health that had tested their plans (21 of 29 boards of health) used at
least two of these methods and 10 boards of health had completed multiple versions of a testing exercise over
this time period.
In addition, eight of the boards of health that had tested their plans have also faced real emergency situations
during this period, and reported that they have been able to identify ways to improve their emergency response
plans based on these experiences.

66
30. Accreditation Status
The accreditation status indicator is defined as whether the board of health participates in an accreditation
process, and if so, indicates the accrediting organization and current accreditation status.
Accreditation sets benchmarks of consistent standards for public health services that should be met by boards
of health. It also provides a process for quality improvement by identifying areas for improvement in efficiency
and performance. In doing so, accreditation acts as a continuous quality improvement mechanism and embeds
this as a feature of the public health culture.
Fourteen boards of health were accredited at the time of the survey. A further seven boards of health are
preparing to undertake, or are currently undertaking the accreditation process.
Of the 21 boards of health involved in accreditation, 19 are accredited with or working towards accreditation
with the Ontario Council on Community Health Accreditation (OCCHA), one is accredited with Accreditation
Canada,andoneisaccreditedwiththeNationalQualityInstitute.
Governance and Accountability Indicators
Operation Hairspray Case Study
Ottawa
Public Health has developed a health protection initiative that
works with community members to provide health information to
populations at risk. Operation Hairspray trains African and Caribbean hairdressers and
barbers to deliver culturally appropriate information about HIV/AIDS prevention strategies
to their customers and to members of local African and Caribbean communities.
Volunteers in Operation Hairspray are trained as peer educators and acquire the knowledge
and skills needed to impart STI and HIV/AIDS prevention information while they are
interacting with their clients. Over the course of 12 months, 19 peer volunteers were recruited
and trained across Ottawa. In total, they made more than 14,000 contacts with clients and
community members, sharing information and a variety of different written publications on
basic HIV/AIDS prevention, and distributing more than 24,000 condoms. South East Ottawa
Centre Healthy Communities created a database to house information collected by the peer
volunteers.
In 2008, Ottawa Public Health developed a successful partnership with Somerset West
Community Health Centre to expand the reach of the project by recruiting and training an
additional 20 peer volunteers. The AIDS Community Action Programme (ACAP) provided
time-limited funding for Operation Hairspray, Phase 2: Spray the Word. To date, an additional
seven peer volunteers have been recruited and trained.
Case Study 17

67
Initial Report on Public Health 2009
31. Medical Officer of Health Performance Evaluation
The indicator medical officer of health performance evaluation is defined as the completion of a regularly
scheduled performance evaluation of the medical officer of health, by type of evaluator and by year of the
most recent evaluation.
The majority of boards of health (32) report that their medical officer of health receives a regularly scheduled
performance evaluation, and three report that MOH performance evaluation does not occur within their boards
of health. One board of health did not respond to this question.
In terms of frequency, about two thirds of those that have regular performance evaluations (21 of 32) report
that reviews are done annually. An additional four boards of health conduct MOH performance evaluations
every 2 years and the remaining boards of health use varying schedules.
In terms of who conducts the performance evaluations, 23 boards of health use a committee of board members,
and two use a self evaluation method. Among the remaining boards of health that conduct performance
evaluations, the performance evaluation was conducted by the Chief Administrative Officer (3), the City
Manager or Deputy City Manager (2) or the Commissioner of Health (2). In two of these cases, the senior
manager also received input from members of the board of health. Two boards of health did not report on their
method of evaluation.
32. Medical Officer of Health Reporting Relationships
The indicator medical officer of health (MOH) reporting relationships is defined as situations where the
Medical Officer of Health attends board of health meetings and/or standing committee meetings, and
whether he or she participated in the meetings. Participation includes attending meetings and providing
reports, advice or presentations to the board.
The MOH is entrusted with statutory responsibilities to guard and protect the community’s health. In order to
fulfill these responsibilities, the HPPA specifies that the MOH “report directly to the board of health on issues
related to public health concerns and to public health programs and services”.
125
Boards of health were asked to describe how their MOHs reported to their boards of health in 2007, with
participation including activities such as providing written or verbal reports, presenting items, or participating
in the meeting to address issues under discussion.
In the majority of cases (23), MOHs reported directly to the board of health while 10 others have the MOH
report to both a standing committee of the board and to the board of health itself. In two cases, the MOH
reports only to a standing committee of the board.

68
33. Board Member Orientation
The indicator board member orientation is defined as situations where new board of health members are
provided with an orientation to the roles and responsibilities of the board of health, the duties of members
and public health functions and issues.
In order to effectively carry out their responsibilities, new members of any board of directors require a
thorough understanding of their service sector. An orientation program for new members to a board of health
should include information on public health in Ontario; the board’s roles and responsibilities, as well as the
individual’s role and responsibilities; the board’s vision and objectives; existing provincial legislation related
to boards of health; the roles and responsibilities of the board of health in relation to the medical officer of
health; the Ontario Public Health Standards; and information about relevant organizations.
Orientation of board members is supported by the Association of Local Public Health Agencies through
training programs and resources.
Of the 36 boards of health, 35 reported that they routinely orient new board members and that this orientation
includes training or information on the core functions of public health and the board of health’s governance
responsibilities.
34. Board Self-Evaluation
The indicator board self-evaluation is defined as situations where a board of health has engaged in a process
to evaluate its governance processes and organizational effectiveness.
Board self-evaluation is usually a requirement for the accreditation of an organization.
Of the 36 boards of health, 13 reported that they regularly evaluate their performance to improve systems and
processes, including an assessment of the governing body’s own structures, processes and team functioning.
Themostrecentreviewtimeframesrangedfrom2003to2008,with9occurringin2007or2008.
The remaining 23 boards of health reported that their boards do not undertake a self evaluation process.
Governance and Accountability Indicators

69
Initial Report on Public Health 2009
Working with Correctional Facilities Case Study
The
Halton Region Health Department’s Communicable Disease Control
team has launched a program to assist and support health in the two “Super
Jails” (Maplehurst and the Vanier Centre) within its jurisdiction. Maplehurst Correctional
Complex,withapopulationof1,182andaturnoverrateof30inmatesperday,isthelargest
male correctional facility in Canada. The Vanier Centre for Women is a 333-bed medium- and
maximum-securityfacilitywithanalmost100%turnoverrateevery18to21daysandan80%
recidivism rate.
The Communicable Disease Control team provides program support to both facilities and
works closely with the jail’s health services and administration to ensure routine admission
testing, including testing for tuberculosis, and prompt reporting of communicable disease
issues for appropriate follow-up and treatment. At both facilities, 95% of the workload is
TB related, including latent TB infections (LTBIs), active disease follow-up, treatment and
contact management.
In addition, the Food Safety team conducts regular compliance inspections of the kitchen
facilities at both locations. One is a commercial-grade food-production facility that provides
more than 9,000 meals daily to five other provincial institutions. The other provides the
meals for inmates at both Maplehurst and Vanier. In both kitchens, inmates assist in the
production and assembly of meals.
In this role, Halton Region Public Health has been involved in both investigating food-
safety-related complaints and outbreaks, including those resulting from contaminated food
products and intentional adulteration. As well, staff respond to environmental health issues,
including mould and indoor air quality issues.
The health unit also runs a Sexual Health and Needle Exchange Program that provides
Maplehurst and Vanier inmates with education and case management for those diagnosed
with a sexually transmitted infection (STI), and general education on STIs, including HIV/
AIDS and hepatitis A, B, and C.
Case Study 18

70

71
Initial Report on Public Health 2009
Context for Performance Management in Public Health
Public health interventions contribute to the effectiveness and outcomes of the health care system in a number
of ways, including:
• reducingtheneedforemergencyroomandacuteservicesthroughpreventionefforts,sothatfewerpeople
develop conditions that require hospitalization
• providinginformationonpopulationhealthstatusandneedsthroughsurveillance,toassistwithhealth
care planning and demand analysis
• improvinghealthoutcomesforbroadpopulationsthroughcommunitybasedpartnershipsand
collaboration with other health care providers.
Around the world, governments and communities are implementing performance measurement and management
strategies in order to better address increasingly complex health issues and growing demand for services. The
need to demonstrate program effectiveness and cost efficiency is driving the development of performance
measures in all parts of the health care system.
Ontario’s work in implementing performance management within public health is congruent with this global
trend within the health sector. It is also consistent with the performance reporting that is emerging on Ontario’s
healthcaresystem,suchastheMOHLTCHealthSystemScorecardandfromtheOntarioHealthQualityCouncil.
The development of this report has benefited from some of the lessons learned in other jurisdictions. Every
jurisdiction faces the lack of reliable, meaningful performance indicators and corresponding data. As with
other jurisdictions, data on process measures or need for services tend to be more readily available than data
on the outcomes of population based interventions or how these outcomes are achieved.
All parts of the system, including acute care, primary care, public health, and long-term care, as well as Local
Health Integrated Networks (LHINs), government, provincial associations, and provincial and regional service
networks need to champion the changes required to shift from reactive, episodic acute care to proactive health
protection, health promotion and chronic disease prevention and management. Leadership, skills development,
incentives, and quality improvement across the health system and within individual organizations are pre-
requisite to successful implementation of sustainable change.
This report represents the ministry’s first steps towards developing a product to inform the development
of the public health performance management system based on the conceptual approach presented in the
Capacity Review Committee’s (CRC) 2006 final report.
12
Moving Towards Performance Reporting
Section V:

72
CRC Vision for Performance Management in Public Health
Source: Capacity Review Committee. Revitalizing Ontario’s public health capacity: the final report of the Capacity Review Committee.
Toronto, ON: Queen’s Printer for Ontario; 2006, p.25. Reproduced with permission.
As the CRC’s diagram illustrates, a performance management system requires the development of tools and
business processes focused on:
• settingclearperformancegoalsandexpectationsthatspanmultipledimensionsoftheorganization
• measuringprogress
• reportingonperformanceandassessingtheriskstoachievinggoalsandexpectations
• evaluatinghoweffectivethesystemisinachievinggoalsandbuildingknowledge
• ongoingadjustmentstoincorporatenewknowledgeandcircumstances
Some framework components, such as the release of the Ontario Public Health Standards and amendments to
the HPPA to permit the use of accountability agreements, have been developed. Others, however, still are in
early stages of development or redesign. Creating the tools and processes to properly support this framework
is a long-term project that will align with, and build on, existing systems and processes.
Moving Towards Performance Reporting

73
Initial Report on Public Health 2009
Developing a Performance Management Culture
As a first product of the new approach to performance management in public health, it is hoped that this
report will serve as a catalyst for a cultural shift within the sector. Such a shift involves moving away from
an exclusive focus on measuring compliance and reporting on processes, and moving towards measuring
outcomes and looking for ways to improve practices.
This shift in focus does not diminish the importance of tracking processes or delivering on program requirements.
Performance management is far more than simply meeting minimum standards. Under the new performance
management system, organizations within the public health system will need to work together to:
• identifycurrentachievementlevels
• explorewaystoachievemorewiththesameresources
• useacontinuousqualityimprovementapproachtosupportchange
As the performance management system matures, it is assumed that provincial level public reporting on
all requirements and outcomes would be inappropriate and unmanageable. However, boards of health are
responsible for ensuring that they are fulfilling and managing all requirements as a necessary part of their
responsibilities for effective governance and management.
Moving forward, it will be necessary to balance provincial reporting on key high-level outcomes of primary
importance to protecting and improving the public’s health and the need to have enough information available
to identify sectoral pressure points in order to be able to intervene when it is in the public’s interest to do so.
Future Indicators
Through the process of developing this initial report it became clear that the kinds of indicators that directly
measure performance of public health programs and services are not currently available. While Ontario’s
work in this area is building on the work of other jurisdictions, a review of the literature shows that it takes
time; there are no ready made answers or systems that can be adopted quickly or without customization.
Developing these future indicators will be an iterative process as information needs are clarified and defined over
time. The consensus-building phase of indicator selection and the more technical phases of indicator definition
and development will require a significant investment of time and effort to properly consider the issues, the
implications, and possible alternatives. It will also require engagement with public health professionals to
develop a consensus that the right things are being measured, in the right ways, for the right purpose.
Once appropriate measures are identified as priorities for development, it will also be necessary to develop or
modify data collection mechanisms and procedures for ensuring consistency in data collection.
Over time, it is anticipated that the indicators included in this report may be amended, or replaced in order to
include a focus on sector-level risk assessment measures. Currently, measures that assess the strengths and
weaknesses of public health have not been agreed upon, have not been clearly developed and defined and
therefore are not likely to be supported by existing data sources.

74
Requirements for a Performance Management System
Developing an effective public health performance management system will require substantial infrastructure
which will take time to design and implement. It is anticipated that much of this change will happen within
the context of existing local and provincial resources.
The infrastructure required to support a performance management approach features:
• validandreliableindicators
• accurateandreliablebaselinedataforeachindicator
• arobustdata-collectionsystem
• policyontheuseoftargets
• knowledgeabouthowprogramactivitieschangeoutcomes
• considerationoflocalconditions,constraints,andprogram/organizationalcapacitytochangeoutcomes
• organizationalcapacitytomanagedata,interpretresults,andundertakeactionstosupportoperational
changes
Some of the tasks required to support implementation of this vision include:
• reachingconsensusonwhichindicatorstodevelopthatwillreportonprogramoutcomesandallowthe
assessment of risks to the public
• designingandvalidatingtheidentifiedindicators
• developingandimplementingcorrespondingdata-collectiontools
• developingandimplementingnewaccountabilitymechanismsthatclarifyroles,responsibilities,and
reporting requirements
• developingandimplementingsupportsandincentivesforimprovingpractices
The ministry, with its sister ministries (MHP and MCYS) and the advice of the Performance Management
Working Group, is currently planning how best to accomplish these important tasks.
Implementation Challenges
Experience with performance management in other systems and jurisdictions has highlighted certain
common implementation challenges. In Ontario, these challenges include the following:
• Theindividualsandorganizationswithinthesectoralreadyhaveanexistingsetofrelationships,areasof
expertise, and ownership for data systems, processes, and tools, all of which are likely to be impacted by
the implementation process.
• Successultimatelyrequireschangesinattitudesandbehaviours.Thiswillrequiretheuseofchange-
management strategies at all levels of the sector.
• Currentparticipantshavedifferentlevelsofexperienceandexpertiseinunderstandingandusing
performance management approaches. Some public health units are farther ahead than the ministry;
others are newer to the ideas and process changes required for performance management. To fully engage
staff at all levels, implementation will have to be concrete and practical. If the individuals within the
sector do not share an understanding of accountability or performance management, the system will face
strategy dilution which will undermine the implementation’s effectiveness.
Moving Towards Performance Reporting

75
Initial Report on Public Health 2009
• ThisnewapproachtoperformancemanagementisoccurringatthesametimeastheOntarioAgencyfor
Health Protection and Promotion is becoming active and all parties are in the process of establishing new
relationships and determining appropriate linkages and roles.
• Thesignificanceoftheissuesfacedindevelopingtheday-to-dayprocessesforworkingwithdataand
ensuring data quality and integrity cannot be underestimated. The importance of using data to drive
program delivery is emphasized in the Foundational Standard of the OPHS, and public health units are
already working on ways to integrate these requirements into their processes.
Implementation Opportunities
Along with the challenges, there are opportunities to be leveraged, including:
• ThesubstantialcapacityandperformancemanagementexpertisealreadyatworkwithintheOntario
public health sector. This can be marshalled to support the implementation of performance management
at the sector level.
• Thefactthatmanypublichealthunitsandotherstakeholdersalreadyareimplementingcompatible
performance management practices at the local level. This presents the opportunity to learn from each
other and benefit from our collective experience.
• AstheOntarioAgencyforHealthProtectionandPromotionbecomesmoreoperational,newcapacityin
such areas as assessing evidence, exchanging knowledge, collecting and analyzing data, and carrying out
professional development activities will become available just as that additional capacity is needed.
• Performancemanagementisaboutworkingsmarter,notharder.Theprinciplesofperformance
management support working smarter by collecting data once for multiple uses and restricting collection
to only the data that will be used to inform decisions. These principles will need to inform our work in
order for everyone in the sector to see the benefits.
Conclusion
The ministry, in collaboration with MHP and MCYS, is pleased to be offering this report on public health in
Ontario as an initial step towards implementing a new approach to performance management.
In the process of developing this report, with the advice of the Performance Management Working Group and
others, experience has been gained as to the iterative decision making processes that are a vital and necessary
part of developing this new performance management approach. Moving from a compliance framework to a
performance management framework does not necessarily require new resources; what is most fundamental is
a shift in thinking and in organizational culture to support continuous quality improvement.
The intended outcome of the performance management framework is to emphasize improvements through
informed decision making, appropriate accountability, and sustainability of the Ontario public health system.
Reaching this outcome will require that the ministries involved in public health continue to engage with
organizations in Ontario’s public health sector as well as those in the broader health care sector. Partnerships
and collaborative efforts are a vital aspect of supporting a strong, flexible, and responsive public health
system that is able to demonstrate improvements and achievements over time.

76

77
Initial Report on Public Health 2009
Appendices
Appendix 1: Peer Groups
A peer group is a cluster of health units with similar social and economic factors. From a practical perspective,
the impact of social and economic factors on health outcomes can be seen more clearly by clustering the health
units and comparing results within peer groups.
The peer groups used in this report are drawn from Statistics Canada’s 2007 peer groups, which use 2007
health region boundaries and 2001 Census data. Across Canada there are nine peer groups identified by
letters A through I. Ontario health units fall into six of these peer groups. The following tables provide a
breakdown of Ontario health units by peer groups, the principal characteristics of each of the peer groups,
and the variables used in the cluster analysis to determine the peer groups.
The method used to determine the peer groups is described on the Statistics Canada website.
126
“Statistics
Canada uses a statistical method to achieve maximum statistical differentiation between health regions.
Twenty–four variables were chosen to cover as many of the social and economic determinants of health as
possible, using data collected at the health region level mostly from the Census of Canada. Concepts covered
include:
• basicdemographics(forexample,populationchangeanddemographicstructure),
• livingconditions(forexample,socio-economiccharacteristics,housing,andincomeinequality),and
• workingconditions(forexample,labourmarketconditions).”
For additional information please refer to the website at the following address:
http://www.statcan.gc.ca/pub/82-221-x/2008001/5202322-eng.htm

78
Table A: Ontario health units by peer group
2007 Peer Groups Health Unit
Peer Group A:
Urban/Rural Mix Brant County Health Unit
City of Hamilton Health Unit
Hastings and Prince Edward Counties Health Unit
Chatham-Kent Health Unit
Kingston, Frontenac and Lennox and Addington Health Unit
Lambton Health Unit
Middlesex-London Health Unit
Niagara Regional Area Health Unit
Peterborough County-City Health Unit
Peer Group B:
Urban Centre Durham Regional Health Unit
Halton Regional Health Unit
City of Ottawa Health Unit
Peel Regional Health Unit
Waterloo Health Unit
Wellington-Dufferin-Guelph Health Unit
Windsor-Essex County Health Unit
York Regional Health Unit
Peer Group C:
Sparsely Populated
Urban-Rural Mix
The District of Algoma Health Unit
North Bay Parry Sound District Health Unit
Sudbury and District Health Unit
Thunder Bay District Health Unit
Timiskaming Health Unit
Peer Group E:
Mainly Rural Elgin-St. Thomas Health Unit
Grey Bruce Health Unit
Haldimand-Norfolk Health Unit
Haliburton, Kawartha, Pine Ridge District Health Unit
Huron County Health Unit
Leeds, Grenville and Lanark District Health Unit
Oxford County Health Unit
Perth District Health Unit
Renfrew County and District Health Unit
The Eastern Ontario Health Unit
Simcoe Muskoka District Health Unit
Peer Group G:
Metro Centre
City of Toronto Health Unit
Peer Group H:
Rural Northern Regions Northwestern Health Unit
Porcupine Health Unit
Appendices

79
Initial Report on Public Health 2009
Table B: Principal characteristics of peer groups
127
Peer group Principal characteristics
A
Urban-rural mix from coast to coast
Average percentage of Aboriginal population
Low male population
Slow population growth from 1996 to 2001
B
Mainly urban centres with moderately high population density
Low percentage of government transfer income
Rapid population growth from 1996 to 2001
C
Sparsely populated urban-rural mix from coast to coast
Average percentage of Aboriginal population
Negative population growth
D
Rural regions mainly in the central Prairies
Moderate Aboriginal population
Moderately high percentage of government transfer income
Almost equal numbers of men and women
Negative population growth
E
MainlyruralregionsinQuebec,OntarioandthePrairies
High proportion of people recently moved to or within these regions since 1996
Average percentage of Aboriginal population
Moderate population growth
F
Northern and remote regions
Very high Aboriginal population
Moderately high percentage of government transfer income
Slightly higher male population
Moderate population growth
G
Largest metro centres with an average population density of 3,934 people per
square kilometre
Low Aboriginal population
Moderate percentage of government transfer income
High female population
H
Rural northern regions
High Aboriginal population
High male population
Negative population growth
I
Mainly rural Eastern regions
Very high percentage of government transfer income
Negative population growth
Low percentage of people having moved to or within these regions since 1996
Source: Statistics Canada. Health Indicators. 82-221-X., no. 1. Health regions and peer groups. Ottawa, Ont.: Minister of Industry; 2008.
Adapted with permission.

80
Appendices
Table C: Variables used in cluster analysis to define peer groups
128
Variable Definitions Source
2001 Population Estimate of the total number of individuals
living in a region.
Statistics Canada,
Census 2001 (unadjusted)
Aboriginal Percentage Proportion of a regions' total population self-
identifying with an Aboriginal group.
Statistics Canada, 2001
Census, 2001 Census
Coverage Studies, and
Demography Division
(population estimates)
Average Dwelling Value Average expected value of an owner-occupied,
non-farm, non-reserve dwelling (including the
value of the land the dwelling is on) at the time
of the Census.
Statistics Canada,
2001 Census
Average Income Average family income for persons aged 15
and over, from all sources.
Statistics Canada,
2001 Census
Post-secondary
graduates
Population aged 25 to 54 who have obtained a
post-secondary certificate, diploma, or degree
Statistics Canada, 2001
Census (special tabulations)
Employment Rate
(25 to 54)
Number of employed persons aged 25 to 54
divided by the total number of individuals
between the ages of 25 and 54 in a given
region.
Statistics Canada, 2001
Census (special tabulations)
Health Region Peer Groups
2003, June 2004, Page 17
Growth Rate Percent change in a regions population
estimate from 1996 to 2001.
Statistics Canada, 1996 and
2001 Census (unadjusted)
Government
Transfer Income
Proportion of all income that came from
governmenttransfers(e.g.,GIS/OAS,C/QPP,
EI, etc.) for the population 15 years of age and
older. EI, etc.) for the population 15 years of
age and older.
Statistics Canada,
2001 Census
Housing Affordability Proportion of total households spending 30%
or more of total household income on shelter.
Statistics Canada,
2001 Census
Immigrant Percentage Those immigrants who came to Canada from
1991 to 2001 as a proportion of the total
population.
Statistics Canada,
2001 Census
Median share of income Proportion of income (from all sources) held
by the bottom half of all households, based
on the median household income for that
specific community.
Statistics Canada, 2001
Census (special tabulations)

81
Initial Report on Public Health 2009
Variable Definitions Source
Internal Migrant
Mobility
Proportion of people that lived in a different
Canadian municipality at the time of the
previous Census (5-year internal migrants).
This excludes Canadians in households
outside Canada (military and government
personnel).
Statistics Canada,
2001 Census Health Region
Peer Groups 2003, June 2004,
Page18
Lone-Parent Families Proportion of lone-parent families among all
census families living in private households. A
census family refers to a married or common-
law couple or lone parent with at least one
never-married son or daughter living in the
same household.
Statistics Canada,
2001 Census
Long Term
Unemployment Rate
Proportion of the labour force aged 15 and
over who did not have a job any time during
the current or previous year.
Statistics Canada,
2001 Census
Low Income 15+ Proportion of persons in economic families
and unattached individuals with 2000 incomes
below the Statistics Canada low-income cut-
off (LICO). The cut-offs represent levels of
income where people spend disproportionate
amounts of money for food, shelter, and
clothing. LICOs are based on family size and
degree of urbanization; cut-offs are updated
to account for changes in the consumer price
index. Data were not derived for economic
families or unattached individuals in the
Territories or on Indian Reserves.
Statistics Canada,
2001 Census
Low Income Children Proportionofchildrenunderage18livingin
economic families with 2000 incomes below
Statistics Canada's low-income cut-offs
(LICO). Data were not derived for economic
families or unattached individuals in the
Territories or on Indian Reserves.
Statistics Canada,
2001 Census
Male-Female Ratio Total number of males in a given region in
2001 divided by the total number of females.
Statistics Canada,
2001 Census
Table C: Variables used in cluster analysis to define peer groups (cont’d)

82
Variable Definitions Source
Owner-Occupied
Dwellings
Proportion of dwellings in which the owner
also lives. Band housing and collective
dwellings (i.e. rooming houses, nursing
homes, military camps etc.) are excluded
from both numerator and denominator.
Statistics Canada,
2001 Census, Health Region
Peer Groups 2003, June 2004,
Page 19
Population Density Number of people per square kilometre. Statistics Canada, 2001
Census and Geography
Division (special tabulations)
Population under 15 Proportion of the population in a given region
under the age of 15 (2001 population).
Statistics Canada, 2001
Census (unadjusted)
Population 65 Years
and Older
Proportion of the population in a given region
aged 65 years and older (2001 population).
Statistics Canada, 2001
Census (unadjusted)
Strong MIZ Census Metropolitan and Census
Agglomeration Influenced Zones represents
the proportion of the population living in
Census Metropolitan Areas (CMAs), Census
Agglomerations (CAs) and communities that
fall outside CMAs/CAs that have at least 30%
of the employed labour force commuting to
CMAs/CAs. The larger the proportion, the
stronger the relationship between the specific
community and a nearby CMA/CA.
Statistics Canada, 2001
Census (special tabulations)
Unemployment Rate Total number of unemployed individuals
15 and older divided by the total number of
individuals 15 and older participating in the
labour force.
Statistics Canada,
2001 Census
Visible Minority Proportion of the population belonging
to a visible minority group. As defined by
theEmploymentEquityAct(1986),visible
minorities are persons (other than Aboriginal
people) who are non-Caucasian in race or
non-white in colour.
Statistics Canada,
2001 Census
Table C: Variables used in cluster analysis to define peer groups (cont’d)
Appendices

83
Initial Report on Public Health 2009
Appendix 2: Health Unit Profile Variable Definitions
# Variable Definition Data Source
1 Size of Region (km
2
) Land area of health unit in square kilometres. Statistics Canada, 2006
Census of Population
2 Population (2007) Number of individuals residing in the health
unit based on population estimates.
Provincial
Health Planning
Database (PHPDB),
December2008
3 Population Growth Rate
(2002-2007)
The difference between the population at
the end of the period and the population at
the beginning of the period relative to the
population at the beginning of the period; 2002
to 2007 Population Estimates Change (%).
Provincial
Health Planning
Database (PHPDB),
December2008
4 Population Density (km
2
)
(2007)
Number of individuals residing in the health
unit (2007 Estimates) divided by the land area
of the health unit in square kilometres.
Size of region:
Statistics Canada, 2006
Census of Population;
Population Estimates:
Provincial Health
Planning Database,
December2008
5 % Immigrants Immigrants are persons who are, or have ever
been, landed immigrants in Canada. A landed
immigrant is a person who has been granted
the right to live in Canada permanently by
immigration authorities. Some immigrants
have resided in Canada for a number of years,
while others are more recent arrivals. Most
immigrants are born outside Canada, but a
small number were born in Canada. Includes
immigrants who landed in Canada prior to
Census Day, May 16, 2006 relative to the non-
institutionalized population.
Statistics Canada,
2006 Census of
Population
6 First Nations A First Nation, or Band, is a group of people
for whom lands have been set aside or
declared to be a band for the purposes of the
Indian Act.
First Nations Profiles,
Indian and Northern
AffairsCanada,2008

84
# Variable Definition Data Source
7 Employment Rate Number of persons employed in the week
(Sunday to Saturday) prior to Census Day
(May 16, 2006), expressed as a percentage
of the total population 15 years and over
excluding institutional residents.
Statistics Canada, 2006
Census of Population
8 Housing Affordability Households (total renters and owners)
spending 30% or more of total household
income on shelter expenses. Shelter expenses
include payments for electricity, oil, gas,
coal, wood or other fuels, water and other
municipal services, monthly mortgage
payments, property taxes, condominium fees
and rent. This excludes band housing on First
Nation reserves.
Statistics Canada,
2006 Census of
Population
9 % of Persons under
18yearsofagein
Low Income Households
(after tax)
Proportionofpersons<18yearsinlow-income
households relative to the total number of
children<18yearsinprivatehouseholds.
Proportionofchildren<18yearslivingunder
LICOs after tax. After tax income refers to
total income from all sources minus federal,
provincial and territorial income taxes paid
for 2005. Refers to the position of an economic
family or a person 15 years and over not in
an economic family in relation to Statistics
Canada's low income before-tax or after-tax
cut-offs. Since each family member shares the
income status of that family, percentages in
low income can be derived for all persons in
private households.
Statistics Canada,
2006 Census of
Population
10 % with Post Secondary
Education
Proportion of population ages 25-64 years
completing a post-secondary education
relative to the total non-institutional
population 25-64 years of age. Post-secondary
education includes: Apprenticeship or trades
certificate or diploma; College, CEGEP or
other non-university certificate or diploma;
University certificate or diploma below the
bachelor level; and University certificate,
diploma or degree.
Statistics Canada,
2006 Census of
Population
Appendices
Appendix 2: Health Unit Profile Variable Definitions
(cont’d)

85
Initial Report on Public Health 2009
# Variable Definition Data Source
11 Size of Birth Cohort
(2007)
Number of live births for the 2007 calendar
year based on hospital newborn admissions
weighing 500 grams or more. Note that the
provincial total includes unknown but not out
of province births as analyzed by residence of
mother.
Provincial Health
Planning Database
(PHPDB), Inpatient
Discharges,
February 2009
12 % Francophone
Population
Number of people with French as their mother
tongue. Mother tongue refers to the first
language learned at home in childhood and
still understood by the individual at the time
of the census. Definition of Francophone
status includes a response of French as a first
language including: French (single response);
English and French (multiple); French and
non-official language (multiple) + English and
French and non-official language(s) (multiple).
Statistics Canada, 2006
Census of Population
13 % Speaking neither
English nor French
Proportion of individuals who cannot conduct
a conversation in either of the official
languages of Canada (in English only, in
French only, in both English and French).
Statistics Canada, 2006
Census of Population
14 Cost of Nutritious Food
Basket for a Family of
Four(2008)
The nutritious food basket is a food costing
tool that is a measure of the cost of healthy
eating based on Canada’s current nutrition
recommendations. It consists of a weekly cost
of a fixed basket of food items for various age/
sex groups, expressed for a reference family
of four (a man and woman, each aged 25-49
years; a boy, 13-15 years of age; and a girl 7-9
years old).
Submitted by Public
Health Units to Ministry
of Health Promotion,
Chronic Disease
Prevention & Health
PromotionBranch,2008
Appendix 2: Health Unit Profile Variable Definitions
(cont’d)

86
# Variable Definition Data Source
15 # Food Premises (2006) Encompass premises where food or milk is
manufactured, processed, prepared, stored,
handled, displayed, distributed, transported,
sold or offered for sale, but does not include a
private residence as defined under the Health
Promotion and Protection Act. Included are
the total number of high, moderate and low
risk permanent (year round) food premises.
Ministry of Health and
Long-Term Care, Food
Safety Audit 2006.
16 # Long-term Care Homes Number of Long-Term Care Homes in the
health unit. A long-term care (LTC) home
provides care and services for people who
no longer are able to live independently or
who require onsite nursing care, 24-hour
supervision or personal support. Nursing
homes under the Nursing Homes Act,
approved charitable homes for the aged under
the Charitable Institutions Act and homes
under the Homes for the Aged and Rest
Homes Act are all LTC homes. This definition
includes all Nursing Homes and Homes for
Aged. It does not include temporary and
interim facilities. It excludes retirement homes
and supportive housing.
Provincial Health
Planning Database
(PHPDB), Institution
Data[2008].Updated
on advice of individual
public health units.
17 # Hospital Sites Number of hospital sites in the health unit. Ministry of Health and
Long-TermCare,2008.
Updated on advice of
individual public health
units.
18 # Licensed Day Nurseries Number of licensed child care centres under
section 1 of the Day Nurseries Act in the
health unit.
Based on data from
Ministry of Children and
YouthServices,2008.
Updated on advice of
individual public health
units.
Appendices
Appendix 2: Health Unit Profile Variable Definitions
(cont’d)

87
Initial Report on Public Health 2009
# Variable Definition Data Source
19 # Personal Service
Settings (estimated)
Estimated number of personal service settings
as defined in the Infection Control in Personal
ServicesSettingsProtocol(1998)includeany
facility where there is a risk of exposure to
blood, such as but not limited to, hairdressing
and barber shops, tattoo and body piercing
studios, electrolysis, and aesthetic clinics.
Board of Health Survey,
2008
20 # Schools Number of public and separate schools in a
health unit. Excludes private schools. Schools
that share facilities are counted individually.
Based on data from
Ministry of Education,
2008.Updatedonadvice
of individual public
health units.
21 # School Boards Number of school boards in a health unit.
Includes both English and French language
school boards for public and separate schools.
Does not include boards of private schools.
The Ontario total reflects the number of
unique school boards in Ontario. Because
some school boards cross over into multiple
health units the sum total of the column is
different from the Ontario total.
Based on data from
Ministry of Education,
2008.Updatedonadvice
of individual public
health units.
22 # Small Drinking
Water Systems
Number of small drinking water systems
within each health unit as per the inventories
submitted by health units and their review
by the Environmental Health Branch. Small
drinking water systems are defined as per
O.Reg318/08andO.Reg319/08underthe
Health Protection and Promotion Act.
Ministry of Health and
Long-TermCare,2008.
Appendix 2: Health Unit Profile Variable Definitions
(cont’d)

88
Appendices
Appendix 2: Health Unit Profile Variable Definitions
(cont’d)
# Variable Definition Data Source
23 # Municipalities Number of Ontario single and lower tier
municipalities within each health unit.
Based on data from
Ministry of Municipal
Affairs and Housing,
2008.Updatedonadvice
of individual public
health units.
24 Board of Health
Governance Model
There are five types of governance models as
follows:
Autonomous: Separate from any
municipal organization but with multi-
municipal representation (including citizen
representatives appointed by municipalities);
potential for provincial appointees.
Autonomous/Integrated: Only one municipality
appoints representatives (including citizen
representatives); potential for provincial
appointees. Operate within municipal
administrative structure.
Regional: Boards are Councils of
Regional Government (federations of local
municipalities); no citizen representatives; no
provincial appointees.
Single-Tier: Boards are Councils of Single
Tier Municipalities (area with only one
level of municipal government); no citizen
representatives; no provincial appointees.
Semi-Autonomous: Single-tier Council
appoints members to a separate “board of
health” (including citizen representatives);
Council approves budget and staffing;
no provincial appointees.
Ministry of Health and
Long-TermCare,2008.

89
Initial Report on Public Health 2009
Appendix 3: Indicator Definitions
1. Teen Pregnancy
Definition:
The teen pregnancy rate estimates the number of pregnancies (resulting in live births, still births and
therapeutic abortions) per 1,000 females age 15 -19 years.
Data Source(s):
Numerator: Number of deliveries (live birth and still births): Inpatient Discharges, Provincial
Health Planning Database, Ministry of Health and Long-Term Care
Therapeutic abortions: Therapeutic Abortions Summary,
Provincial Health Planning Database, Ministry of Health and Long-Term Care
Denominator: Population Estimates, Provincial Health Planning Database,
Ministry of Health and Long-Term Care
Formula:
{
Total number of deliveries (live births and stillbirths) and therapeutic
abortions for females age 15-19 years (2007 calendar year)
}
X 1,000
Total number of females age 15-19 years (2007 calendar year)
Notes:
• Intellihealththerapeuticabortionssummaryreportwasusedtoderivethenumberoftherapeutic
abortions for females ages 15-19 years
• IntelliHealth\20-OntarioSpecialReports\TherapeuticAbortionSummary.Report#20-0001wasused
to derive the number of therapeutic abortions
• Intellihealth\05InpatientDischarges\HospitalBirths\Deliveries-OntarioxMother’sAge:Report#:
05-0004 was used to derive the number of deliveries
• Analyzedbymother’susualplaceofresidence,notplaceofbirth
• AnalyzedbyICD10-CAcodescontainingZ37forlivebirthsandstillbirthsbymother’sdateof
discharge, and mother’s age at time of delivery
• Excludesbirthsandtherapeuticabortionstofemalesresidingout-of-province;excludesestimatesof
fetal loss; excludes abortions conducted with females residing out of province

90
Appendices
2. Low Birth Weight
Definition:
The low birth weight rate indicator estimates the rate of singleton live births weighing 500-2499 grams
immediately upon birth, based on the mother’s usual place of residence per the total for singleton live
births weighing at least 500 grams per 1,000 births.
Data Source(s):
Numerator: Inpatient Services Provincial Health Planning Database,
Ministry of Health and Long-Term Care
Denominator: Inpatient Services (Hospital Data), Provincial Health Planning Database,
Ministry of Health and Long-Term Care
Formula:
Total number of singleton live births weighing between
500 and 2499 grams (2007 calendar year)
{
Total number of singleton live births weighing
}
X 1,000
at least 500 grams (2007 calendar year)
Notes:
• Excludesbirthswithweightsrecordedunder500gramsduetopossibleentryerrorswith
still born births
• Excludesmultiplebirths
• PHPDBQualifications:Newborns(entrycode=N)atdateofadmission;PatientDiagnosisCodes
(beginningwithZ380,Z381,Z382)fortheCalendarYear(2007).Weightsforsingletonlivebirths
(greater than or equal to 500); Weights for low births weights (greater than or equal to 500 grams
and less than 2500 grams)
• Intellihealth\05InpatientDischarges\HospitalBirths\LowBirthWeight,SingletonBirths:Report#
05−0004 was used to derive both the numerator and denominator
• Theindicatorisnotlimitedtofull-termbirthsandalsoincludespre-termbirths
• Analyzedbymother’susualplaceofresidence,notplaceofbirth
• Excludesbirthstomotherswhoresideoutofprovince

91
Initial Report on Public Health 2009
3. Breastfeeding Duration
Definition:
The breastfeeding duration rate indicator estimates the proportion of mothers age 15-55 years who breastfed
(not exclusively) their last baby (born within the past five years) for a duration of six months or more.
Data Source(s):
Numerator: Canadian Community Health Survey Cycles 2.1, 3.1 and Canadian Community Health
Survey 2007, Statistics Canada, Ontario Share Files distributed by the Ministry of
Health and Long-Term Care
Denominator: Canadian Community Health Survey Cycles 2.1, 3.1 and Canadian Community Health
Survey 2007, Statistics Canada, Ontario Share Files distributed by the Ministry of
Health and Long-Term Care
Formula:
Total weighted number of female respondents age 15-55 years
who gave birth in the past five years and who
{
breastfed (non-exclusively) their child for at least six months
}
X 100
Total weighted number of female respondents age 15-55 years
who gave birth in the past five years
Notes:
• ThisindicatorwasderivedbycombiningthreecyclesoftheCanadianCommunityHealthSurvey
(CCHS) in order to obtain reportable and stable data for breastfeeding duration estimates at the
public health unit level in Ontario. Simply using one survey to estimate for breastfeeding duration
resulted in unstable estimates for the majority of public health units in Ontario, and in many cases
the data was unreportable
• Numerator:MEX_06=SixMonths(9),SeventoNineMonths(10),TentoTwelveMonths(11),
One year or more (12)
• Denominator:MEX_01=Hasgivenbirthinthelastfiveyears(1)
• Excludednotapplicable(96)andnotstated(99)responsestoMEX_01.Exclusionofwomen
who are currently breastfeeding (MEXC_05=2)
• PHU3545wasdropped,3547=NorthBay,and3560=SimcoeinCCHS2.1duetoamalgamations
of public health units
• TherewasinsufficientsamplesizetostratifythedataforeachpublichealthunitforCCHS2007,and
therefore cycles 2.1, 3.1, and CCHS 2007 of the CCHS were combined according to methods outlined
by Thomas and Wannell.
129
Both the separate and pooled approaches to combining cycles of the
CCHS were considered. The separate approach to combining cycles of CCHS was used in the report
• Astherewerenotconsistenttrendsovertimeoverthe3individualestimatesforbreastfeeding
duration, combining the 3 cycles of the CCHS did not diminish the data output in any way
92
Appendices
4. Postpartum Contact
Definition:
The postpartum contact indicator is defined as the percentage of families who consented to a post-partum
phone call under the Healthy Babies Healthy Children (HBHC) program and who received a post-partum
phonecallorcontactfromthehealthunitwithin48hoursofreleasefromhospitalaftergivingbirth.
Data Source(s):
Numerator: Integrated Services for Children Information System, Ministry of Children
and Youth Services
Denominator: Integrated Services for Children Information System, Ministry of Children
and Youth Services
Formula:
# of families who were contacted by the health unit within
{
48hoursofhospitaldischarge(2007calendaryear)
}
X 100
# of families (with or without a Parkyn) who consented to be
contacted by the health unit (2007 calendar year)
Notes:
• DataextractedonJuly27,2008
• Notbasedonalllivebirths.FamiliesmusthaveconsentedtoreceivinganHBHCphonecall
• Items21.1/21.0ontheISCISextractreportwereused

93
Initial Report on Public Health 2009
5. Smoking Prevalence
Definition:
The smoking prevalence indicator estimates the age-standardized proportion of people age 12 years and
older who are current smokers (daily or occasional cigarette smokers).
• Currentsmoker–dailysmokeroroccasionalsmoker
• Dailysmoker–smokingatleastonecigaretteperday
• Occasionalsmoker–doesnothaveatleastonecigaretteperday
Data Source(s):
Numerator: Canadian Community Health Survey 2007, Statistics Canada, Ontario Share File
distributed by the Ministry of Health and Long-Term Care
Denominator: Canadian Community Health Survey 2007, Statistics Canada, Ontario Share File
distributed by the Ministry of Health and Long-Term Care
Formula:
Weighted number of respondents age 12+ years who
{
are current (daily + occasional) cigarette smokers
}
X 100
Weighted total number of respondents age 12+ years
Notes:
• Numerator:SMK_DSTY=DailySmoker(1)orOccasionalSmoker(formerdailysmoker)(2)and
Occasional Smoker (3)
• Denominator:SMK_DSTY=Daily(1),Occasional(2)Occasional(3)FormerDailySmoker(4)Former
Occasional Smoker (5) and Never Smoker (6)
• NotAnswered((99),basedonDon’tKnow,Refusals,andNotStatedtoatleastoneofthequestions)
responses were excluded
• Agegroupsinyearsusedfordirectage-standardization:12-19,20-34,35-49,50-64,65-74,75+
• Directage-standardizationtothe1991Canadianpopulation

94
Appendices
6. Youth Lifetime Smoking Abstinence
Definition:
The youth lifetime smoking abstinence indicator estimates the proportion of young people age 12-19 years
who have never smoked a whole cigarette.
Data Source(s):
Numerator: Canadian Community Health Survey 2007, Statistics Canada, Ontario Share File
distributed by the Ministry of Health and Long-Term Care
Denominator: Canadian Community Health Survey 2007, Statistics Canada, Ontario Share File
distributed by the Ministry of Health and Long-Term Care
Formula:
Weighted number of respondents age 12-19 years
{
who have never smoked at least one whole cigarette
}
X 100
Weighted total number of respondents age 12-19 years
Notes:
• BasedonCCHSQuestionSMK_01B“Haveyoueversmokedawholecigarette?”
• Numerator:SMK_01=No(2)
• Denominator:SMK_01=Yes(1),No(2)orNotApplicable(6)
• Refusals(8)andNotStated(9)responseswereexcluded

95
Initial Report on Public Health 2009
7. Adult Heavy Drinking
Definition:
The adult heavy drinking episode indicator estimates the age-standardized proportion of people age
20 years and older who reported consuming five or more drinks on at least one occasion during the
previous 12 months.
Data Source(s):
Numerator: Canadian Community Health Survey 2007, Statistics Canada, Ontario Share File
distributed by the Ministry of Health and Long-Term Care
Denominator: Canadian Community Health Survey 2007, Statistics Canada, Ontario Share File
distributed by the Ministry of Health and Long-Term Care
Formula:
Weighted number of respondents who are age 20+ years
who reported consuming 5 or more drinks, on at least one
{
occasion during the previous 12 months
}
X 100
Weighted number of respondents age 20+ years who did or did not drink
Notes:
• NumeratorALC_3=Lessthanoncepermonth(2),Oncepermonth(3),2-3timespermonth(4),
Once per week(5), More than once per week (6)
• Denominator:ALC_1=Yes(1),No(2)
• Don’tKnow(97),Refusal(98),NotStated(99)responseswereexcluded
• Agegroupsinyearsusedfordirectage-standardization:20-34,35-49,50-64,65-74,75+
• Directage-standardizationtothe1991Canadianpopulation

96
Appendices
8. Youth Heavy Drinking
Definition:
The youth heavy drinking episode indicator identifies the proportion of people age 12-19 years who
reported consuming five or more drinks on at least one occasion during the previous 12 months.
Data Source(s):
Numerator: Canadian Community Health Survey 2007, Statistics Canada, Ontario Share
File distributed by the Ministry of Health and Long-Term Care
Denominator: Canadian Community Health Survey 2007, Statistics Canada, Ontario Share
File distributed by the Ministry of Health and Long-Term Care
Formula:
Weighted number of respondents age 12-19 years who reported consuming
{
5 or more drinks on at least one occasion during the previous 12 months
}
X 100
Weighted number of respondents age 12-19 years who did or did not drink
Notes:
• Numerator:ALC_3=Lessthanoncepermonth(2),Oncepermonth(3),2-3timespermonth(4),
Once per week(5), More than once per week (6)
• Denominator:ALC_1=Yes(1)No(2)
• Don’tKnow(97),Refusal(98),NotStated(99)responseswereexcluded

97
Initial Report on Public Health 2009
9. Physical Activity Index
Definition:
The physical activity index indicator estimates the age-standardized proportion of the population age
12 years and older by level of energy expenditure in the categories active and moderately active in their
leisure time physical activity.
• Active=respondentswhoaverage3.0+kcal/kg/dayofenergyexpenditure
• Moderatelyactive=respondentswhoaverage1.5-2.9kcal/kg/day
• Inactive=respondentswithenergyexpenditurelevelslessthan1.5kcal/kg/day
Data Source(s):
Numerator: Canadian Community Health Survey 2007, Statistics Canada, Ontario Share File
distributed by the Ministry of Health and Long-Term Care
Denominator: Canadian Community Health Survey 2007, Statistics Canada, Ontario Share File
distributed by the Ministry of Health and Long-Term Care
Formula:
Weighted number of respondents age 12+ years by
{
physical activity index categories active and moderately active
}
X 100
Weighted number of respondents age 12+ years
Notes:
• Numerator:PACDPAI=active(1)ormoderatelyactive(2)
• Denominator:PACDPAI=active(1)andmoderatelyactive(2)andinactive(3)
• Excludednotstatedresponses(9)fromdenominator
• Agegroupsinyearsusedfordirectage-standardization:12-19,20-34,35-49,50-64,65-74,75+
• Directage-standardizationtothe1991Canadianpopulation
• Respondentswereaskedabouttheirparticipationinvarioustypesofphysicalactivitiesinthe
previous three-month period, as well as the frequency and duration of each activity

98
Appendices
10. Healthy Body Mass Index
Definition:
Thehealthybodymassindexindicatorestimatestheage-standardizedproportionofpeopleage18yearsand
older whose self reported height and weight denote a healthy body mass index (BMI). BMI is calculated using
the person’s weight in kilograms divided by their height in metres squared. The International Standard for
BMIis:<18.5(underweight),18.5-24.9(acceptableweight),25-29.9(overweight),and30orhigher(obese).
TheWorldHealthOrganizationconsidersaBMIintherangeof18.5-24.9tobehealthyformostadults.
Classification BMI Category Risk of developing health problems
Underweight <18.5 Increased
“Normal or Healthy” Weight,
Acceptable Weight Range
18.5–24.9 Least
Overweight 25.0 – 29.9 Increased
Obese
Class I 30.0 – 34.9 High
Class II 35.0 – 39.9 Very high
Class III ≥ 40.0 Extremely high
Data Source(s):
Numerator: Canadian Community Health Survey 2007, Statistics Canada, Ontario Share File
distributed by the Ministry of Health and Long-Term Care
Denominator: Canadian Community Health Survey 2007, Statistics Canada, Ontario Share File
distributed by the Ministry of Health and Long-Term Care
Formula:
Weightednumberofrespondentsage18+years(excluding
{
pregnantwomenandbreastfeedingwomen)withBMIof18.5-24.9
}
X 100
Weightednumberofrespondentsage18+years
(excluding pregnant women and breastfeeding women)
Notes:
• CCHSexcludespregnantwomen,aswellaswomenage18-49yearswhodidnotanswerthe
pregnancyquestion.Theindexiscalculatedforthoseage18yearsandover,excludingpregnantand
lactating women, as well as persons less than 3 feet tall or greater than 6 feet 11 inches.
130
There was
an additional exclusion of women who were currently breastfeeding (MEX_05=1), and respondents
who chose ‘Not applicable’ (96) or Not Stated (99) responses in the indicator calculation
• Numerator:HWTDISW=Normalorhealthyweight(2)
• Denominator:HWTDISW=Underweight(1),Normalorhealthyweight(2),Overweight(3),and
Obese (4-6)
• Agegroupsinyearsusedfordirectage-standardization:18-34,35-49,50-64,65-74,75+
• Directage-standardizationtothe1991Canadianpopulation

99
Initial Report on Public Health 2009
11. Fruit and Vegetable Consumption
Definition:
The fruit and vegetable consumption indicator estimates the age-standardized proportion of the population
age 12 years and older that reported consuming fruits and vegetables five or more times per day.
Data Source(s):
Numerator: Canadian Community Health Survey 2007, Statistics Canada, Ontario Share File
distributed by the Ministry of Health and Long-Term Care
Denominator: Canadian Community Health Survey 2007, Statistics Canada, Ontario Share File
distributed by the Ministry of Health and Long-Term Care
Formula:
Weighted number of respondents age 12+ years who
{
Consumed fruit and vegetables five or more times per day
}
X 100
Weighted number of respondents age 12+ years
Notes:
• Numerator:FVCGTOT=5to10“servings”offruitandvegetables(2)andmorethan10“servings”of
vegetables (3)
• Denominator:FVCGTOT=lessthan5“servings”(1),5to10“servings”offruitandvegetables(2)and
more than 10 “servings” of vegetables (3)
• Excludedifanswerwasnotstated
• Agegroupsinyearsusedfordirectage-standardization:12-19,20-34,35-49,50-64,65-74,75+
• Directage-standardizationtothe1991Canadianpopulation

100
Appendices
12. Fall-Related Hospitalizations among Seniors
Definition:
The fall-related hospitalization rate indicator estimates the age-standardized number of injury-related
hospital separations that are due to falls in seniors age 65 years and older per 100,000 population.
Data Source(s):
Numerator: Discharge Abstract Database, Canadian Institute for Health Information
Distributed by Population Health Planning Database, Ministry of Health and Long-
Term Care
Denominator: Population Estimates, Population Health Planning Database, Ministry of Health and
Long-Term Care
Formula:
Number of hospital separations due to falls
{
In those age 65+ years (2007 calendar year)
}
X 100,000
Total population age 65+ years (2007 calendar year)
Notes:
• Agegroupsinyearsfordirectage-standardization:65-74,75-85,and85+
• Directage-standardizationtothe1991Canadianpopulation
• IncludesAccidentalFalls(ICD-10-CA:W00-W19)withexternalcauses
• PHPDBQualifications:CalendarYear(2007);Ages(greaterthanorequalto65);Patientdiagnosis
beginning with W0 or W1 in ICD-10-CA Block Codes including diagnosis with external cause
diagnoses
• IntelliHealth\SharedReports\PHU\FallRelatedHospitalizations65120

101
Initial Report on Public Health 2009
13. Enteric Illnesses Incidence
Definition:
The enteric illnesses age-standardized incidence rate estimates the total number of reported cases of
selected enteric illnesses per 100,000 population.
Selected reporting fields include:
• Amebiasis
• Botulism
• CampylobacterEnteritis
• Cholera
• Cryptosporidiosis
• Cyclosporariasis
• FoodPoisoning,AllCauses
• Gastroenteritis,InstitutionalOutbreaks
• Giardiasis
• HepatitisA
• Listeriosis
• Paratyphoidfever
• TyphoidFever
• Salmonellosis
• Shigellosis
• Trichinosis
• VerotoxinproducingE.coliincludingHemolyticUremicsyndrome(HUS)
• Yersiniosis
Data Source(s):
Numerator: Integrated Public Health Information System, Ministry of Health and Long-Term Care
Denominator: Population Estimates, Provincial Health Planning Database, Ministry of Health and
Long-Term Care
Formula:
{
Total number of new reported cases of selected enteric illnesses (2007 Calendar year)
}
X 100,000
Total population (2007 Calendar year)
Notes:
• DatawasextractedonFebruary3,2009fromtheIntegratedPublicHealthInformationSystem
• Includesbothsporadicandoutbreakreportableentericcasesthatmettheprovincialsurveillance
case definition
• Agegroupsinyearsusedfordirectage-standardization:0-4,5-9,10-14,15-19,20-24,25-29,30-34,
35-39,40-44,45-49,50-54,55-59,60-64,65-69,70-74,75-79,80-84,85-89,90+
• Directage-standardizationtothe1991Canadianpopulation

102
14. Respiratory Infection Outbreaks in Long-Term Care Homes
Definition:
The respiratory infection outbreak indicator estimates the number of confirmed respiratory infection
outbreaks in long-term care homes between September 1, 2006 and August 31, 2007.
Data Source(s):
Integrated Public Health Information System, Ministry of Health and Long-Term Care
Formula:
Number of confirmed respiratory infection outbreaks in Long-Term Care homes for the 2006/2007
respiratory virus surveillance season.
Notes:
• DatawasextractedonFebruary2,2009fromtheIntegratedPublicHealthInformationSystem.
• IndicatedbyselectingLong-TermCareHomeoptionintheExposureSettingTypeFieldforoutbreaks
in iPHIS
• Outbreaksthatdonotmeetthecasedefinitionforaconfirmedrespiratoryinfectionoutbreakina
long-term care home were removed
• Thereportiscalled:ListofcreatedOutbreaks-ChildCareFacilitiesHighlighted-forHUuse
• CognosReportNetpath:PublicFolders>CRN1.0>SharedCommunicableDiseasesReports>
ManagementReports>QAReports
Appendices

103
Initial Report on Public Health 2009
15. Chlamydia Incidence
Definition:
The age-standardized chlamydia incidence rate indicator estimates the total number of reported
chlamydia cases per 100,000 population.
Data Source(s):
Numerator: Integrated Public Health Information System, Ministry of Health and Long-Term Care
Denominator: Provincial Health Planning Database, Ministry of Health and Long-Term Care
Formula:
{
Total number of new reported cases of chlamydia (2007 calendar year)
}
X 100,000
Total population (2007 calendar year)
Notes:
• DatawasextractedonFebruary3,2009fromiPHIS.
• Agegroupsinyearsusedfordirectage-standardization:<10,10-14,15-19,20-24,25-29,30-34,35-39,
40-44, 45-49, 50-54, 55-59, 60-64, 65+
• Directage-standardizationtothe1991Canadianpopulation

104
16. Immunization Coverage for Hepatitis B
Definition:
The immunization coverage for hepatitis B indicator estimates the proportion of grade 7 students who
have completed the immunization series against hepatitis B by the end of grade 7.
Data Source(s):
Numerator: As reported by public health units to Public Health Division, Ministry of Health and
Long-Term Care
Denominator: As reported by public health units to Public Health Division, Ministry of Health and
Long-Term Care
Formula:
# of grade 7 students who have completed the immunization
series against hepatitis B by the end of grade 7 (vaccinated before or
{
duringgrade7byphysicianorpublichealth)(2007/2008schoolyear)
}
X 100
TotalnumberofGrade7students(2007/2008schoolyear)
Notes:
• DataascompleteasofJune30,2008(2007/2008schoolyear)forgrade7students(birthyear1995)
• HepatitisBimmunizationisnotadesignateddiseaseundertheISPA(Immunization of School Pupils
Act) and therefore health units are not required to report Hepatitis B immunization rates; reporting is
voluntary
• AllpublichealthunitsarerequiredtoreportHepatitisBcoverageratestotheMinistryofHealthand
Long-Term Care. Some public health units also record Hepatitis B coverage rates in the IRIS reporting
data system; use of this system is voluntary
• Thisindicatorisspecifictotheschool-basedimmunizationprogram,anddoesnotincludeall
immunizations against Hepatitis B as administered by the public health unit (e.g. doses administered
in other setting or populations/age groups, such as sexual health clinics)
Appendices

105
Initial Report on Public Health 2009
17. Immunization Coverage for Measles, Mumps, and Rubella
Definition:
The immunization coverage for measles, mumps and rubella indicator estimates the proportion of school
children age 7 years who are known to be complete for age for vaccination against measles, mumps and
rubella.
Data Source(s):
Numerator: Immunization Record Information System, 36 locally maintained databases shared
with the Public Health Division, Ministry of Health and Long-Term Care
Denominator: Immunization Record Information System, 36 locally maintained databases shared
with the Public Health Division, Ministry of Health and Long-Term Care
Formula:
Number of school children age seven years who are known by the
health unit to be complete for age for vaccination against measles,
{
mumpsandrubella(2007/2008schoolyear)
}
X 100
Numberofchildrenenrolledinschool(2007/2008schoolyear)
Notes:
• DataascompleteonJune30,2008(2007/2008schoolyear)for7yearolds(birthyear2000)
• DatawasextractedfromIRIS,August2008toJanuary2009
• Vaccinationinformationiscollectedonlyforchildrenattendingschoolsthatpublichealthunits
have screened
• Somechildren/studentsmaynotbeeligibleforavaccineduetomedicalcontraindication.This
information may be collected and recorded in IRIS. However, ineligible children are not excluded
from the denominator of vaccine coverage calculations since not all IRIS vaccine coverage reports
summarize this information
• Children/studentswithexemptions(medical,philosophical,conscienceorreligious)orwithno
information are treated as incomplete

106
18. Adverse Water Quality Incidents
Definition:
Number of adverse water quality incidents from drinking water systems subject to O.Reg 170/03/O.Reg
252/05 and unregistered drinking water systems.
Data Source(s):
Drinking Water Programs Branch, Ministry of the Environment
Formula:
Number of adverse water quality incidents from drinking water systems subject to O.Reg 170/03/O.Reg
252/05 and unregistered drinking water systems for the 2007 calendar year
Notes:
• ExceedancesfromschoolsanddaycaressubjecttoO.Reg243/07notincludedinthissummary
• O.Reg170/03,a.k.a.DrinkingWaterSystemsincludedyearroundresidentialsystemsaswellas
designated facilities including schools, daycares and nursing homes
• O.Reg252/05a.k.a.Non-ResidentialandNon-MunicipalSeasonalResidentialSystemsThatDoNot
Serve Designated Facilities
Appendices

107
Initial Report on Public Health 2009
Standard Population
The following 1991 Canadian population is the referent
population used in the age-standardized indicators in this
report.
131
Standard Population
1991 Canadian Population
Age (years) Total population by age
<1 403,061
1- 4 1,550,285
5-9 1,953,045
10-14 1,913,115
15-19 1,926,090
20-24 2,109,452
25-29 2,529,239
30-34 2,598,289
35-39 2,344,872
40-44 2,138,891
45-49 1,674,153
50-54 1,339,902
55-59 1,238,441
60-64 1,190,217
65-69 1,084,588
70-74 834,024
75-79 622,221
80-84 382,303
85-89 192,410
90 + 95,467
Total 28,120,065
Additional Age Groups Used
Age (years) Total population by age
10-11 777,691
12-15 1,135,424
15-17 1,149,377

108
19. Total Board of Health Expenditures
Definition:
Total board of health expenditures in 2007 for “core and related public health programs and services”,
including spending based on revenue from all sources including all government funding (federal, provincial
andmunicipal),userfees(suchasPart8inspectionfees),onetimefunding,feeforservicecontracts,
research funding, and all other grants and donations. Excludes projected expenditures for EMS and animal
control services, which are not part of the public health mandate.
Data Source(s):
Surveyofboardsofhealth,2008
Formula:
Total board of health actual expenditures from all sources
Notes:
• Consolidatesreportingonexistingboardofhealthfundinglevels
• Inthisreportandsurvey“relatedprograms”referstoagroupofprogramsthataredefinedbypublic
health units as ancillary to their core public health programs and services. This definition was used
in the data collection for this indicator in order to allow public health units to provide information on
all current programs regardless of funding source. However, when used in the context of the Program
Based Grants (PBG) funding agreement “Related Programs” refers to a specific group of programs
that are funded through the PBG grant and these are: Infectious Diseases Control, West Nile Virus/
VBD, PHRED, Unorganized Territories, AIDS Hotline, SIECCAN, Infection Prevention and Control
Nurses(newin2008/09),SmallDrinkingWaterSystems,andonetimefundingreceivedthroughPBG.
• Theinclusionofonetimeortimelimitedfundingmayskewthereportingforsomeboardsofhealth
• Lackofcleardefinitionofcategoriesoffundingby“corepublichealth”,“publichealthrelated”and
“other services delivered by public health” resulted in some lack of congruence in categorization
across all boards of health
• Datawerecollectedonexpendituresbyprogram,butdidnotincludeinformationonfundingsources
or cost sharing arrangements
Appendices

109
Initial Report on Public Health 2009
20. Board of Health Expenditure Variance
Definition:
Percent variance between a board of health’s projected annual budget for “core and related public health
programs and services”, and year-end actual expenditures in with revenue from all sources in 2007.
Data Source(s):
Surveyofboardsofhealth,2008
Numerator: Board of health year-end total expenditures and projected annual expenditures on
core and related public health programs and services with revenues from all sources
Denominator: Board of health projected annual expenditures on core and related public health
programs and services reflecting revenue from all sources
Formula:
{
(year-end actual expenditures – projected annual expenditures)
}
X 100
projected annual expenditures
Notes:
• NotethatthesecategoriesdonotalignwiththoseusedbytheministryinitsProgramBasedGrant
funding package, where “Related Programs” has a specific meaning; see notes under Total Board of
Health Expenditures for further detail.
• Boardsreportthatvariancesareusuallyprogramorfundingsourcespecific
• Therehashistoricallybeenunderspendinginboardofhealthbudgetsduetothelocalmunicipal
council control on the overall budget and the timing of ministry budget approvals. In some places,
councils insist that program spending cannot exceed the prior year amount until ministry final budget
approval is received
• Unexpectedinyearactivitieswillimpactactualexpendituresofsomeboardsofhealth,andtherefore
skew their variances

110
21. Expenditures on Training and Professional Development
Definition:
Percent of board of health total actual expenditures for “core and related public health programs and
services” used to support staff training and professional development in 2007.
Staff training and professional development costs include training and educational services for vocational,
technical training, professional courses and seminars; may include payments to external trainers, conference
registration fees, tuition fees and payments for associated textbooks, registration and course delivery costs
such as library access fees, costs associated with conferences, seminars and internally developed courses,
as well as associated event costs such as payments to guest speakers, trainers, catering and space rental
fees. Excludes any associated travel costs and any fees paid to register with a professional regulatory body.
Data Source(s):
Surveyofboardsofhealth,2008
Numerator: Actual board of health expenditures on staff training and professional development
Denominator: Total board of health actual expenditures (core and related)
Formula:
{
Board of health actual expenditures on staff training and professional development
}
X 100
Total board of health actual expendttitures
Notes:
• Largerpublichealthunitsmaybeabletoachieveeconomiesofscalethatwouldlowertheirperstaff
cost for training and development
• Surveydidnotcollectinformationonthenumberofstafftrainedornumberofdaysoftraining
purchased
• Reportedexpendituresmaybeestimatesduetocomplexityofaccessingtraininganddevelopment
expenses that meet the proposed definition within the timeframe
• Excludingtravelcostsmaylimittheabilitytointerprettheoverallimpactoftrainingcostsonthe
budgets of health units with high travel costs (i.e. northern health units)
Appendices

111
Initial Report on Public Health 2009
22. Number of FTEs by Job Category
Definition:
Indicates the number of full time equivalent (FTE) positions in 2007 in each of the following specified
professional job categories. FTE is defined by local board of health HR policies.
a) Public Health Nurse
b) Registered Nurse
c) Registered Practical Nurse
d) Nurse Practitioner
e) Public Health Inspector
f) Dentist
g) Dental Hygienist/Dental Assistant
h) Health Promoter
i) Dietitian/Public Health Nutritionist
j) Speech-Language Pathologist
k) Epidemiologist
l) Heart Health Coordinator
m) Librarian
Data Source(s):
Surveyofboardsofhealth,2008
Formula:
Number of FTEs per professional job category
Notes:
• Indicatordoesnotcoveralljobcategorieswithinaboardofhealth;adecisionwasmadetocollect
data on direct service job categories of interest in relation to assessing local service capacity
• ThenumberofFTEsdoesnotnecessarilyreflectthenumberofstaffworkinginthesepositionsdue
to job sharing or part-time work
• Differencesinlocaluseofjobtitlesmayresultinunder-reportingorinconsistenciesbetween
categories
• Managerswereexcludedfromthisreporting,whichmayaffectreportingoncapacitywheremanagers
also work directly in programs

112
23. Number of Vacant Positions by Job Category
Definition:
The number of job vacancies for staff positions in the following job categories for which there had been a
jobpostingandthathadremainedvacantbetweenMay1,2008anddateofsurveyinNovember,2008.
a) Associate Medical Officer of Health
b) Public Health Nurse
c) Registered Nurse
d) Registered Practical Nurse
e) Nurse Practitioner
f) Public Health Inspector
g) Dentist
h) Dental Hygienist/Dental Assistant
i) Health Promoter
j) Dietitian/Public Health Nutritionist
k) Speech-Language Pathologist
l) Epidemiologist
m) Heart Health Coordinator
n) Librarian
Data Source(s):
Surveyofboardsofhealth,2008
Formula:
Number of vacant positions by job category
Notes:
• Indicatordoesnotcoveralljobcategorieswithinaboardofhealth;adecisionwasmadetocollect
data on direct service job categories of interest in relation to assessing local service capacity
• DoesnotcapturefulllengthofvacanciesthatbeganbeforeMay1,2008
• Doesnotshowfullextentoflackoflocalcapacitywherevacanciesarebeingmanagedby
reassignment and backfilling by existing staff
Appendices

113
Initial Report on Public Health 2009
24. Employment Status of Medical Officers of Health
Definition:
Indicates where a medical officer of health is employed on a permanent, full time basis with a board of
health. FTE is defined by local board of health HR policies.
Data Source(s):
Surveyofboardsofhealth,2008
Formula:
Number of positions by full time status, with values to not exceed 1.0 FTE
Notes:
• SomeboardsofhealthconsiderMOHtimespentprovidingoncallservicetocontributetoorexceed
the requirement for full time status
• Thereisnostandardizeddefinitionof“fulltime”acrossallboardsofhealth

114
25. Staff Length of Service
Definition:
Indicates the percentage of current full and part time public health unit staff who have been employed
continuously by the public health unit by length of service in years.
Periods of time for employment include: up to 1 year; more than 1 year but less than 5 years; more than
5 years but less than 10 years; more than 10 years but less than 20 years; and more than 20 years.
Data Source(s):
Surveyofboardsofhealth,2008
Numerator: Number of public health unit staff employed for specific periods of time
Denominator: Total number of full and part time public health unit staff
Formula:
{
Number of public health unit staff employed for specific periods of time
}
X 100
Total number of public health unit staff
Notes:
• Stafflengthofservicemaybeinfluencedbyoveralldemographicsofthelocalworkforceorthe
presence of training programs (influenced by recruitment through placements)
• Regionallyandmunicipallybasedboardsofhealthwillnotbeabletodisaggregatethedataon
employment length of service for staff that have worked for the organization in different departments
throughout their careers. This will affect primarily administrative and information management staff,
however, the overall effect on total employee length of service will be small
Appendices

115
Initial Report on Public Health 2009
26. Familiarity with Public Health Unit Programs and Services
Definition:
Indicates whether a board of health has assessed local community members’ familiarity with any of the
public health unit’s programs and services.
Data Source(s):
Surveyofboardsofhealth,2008
Formula:
Yes, with year and method of most recent assessment; no
Notes:
• Originalintentwastoreportondegreeofcommunitymembers’familiaritywithpublichealthunit
programs and services based on local surveys
– Although data was collected by most health units (through Rapid Risk Factor Surveillance System
(RRFSS) or local survey), consent to share this data was not included in the instructions of the
original surveys, and therefore local results are not available
– RRFSS module includes seeking information on community members’ basic familiarity with the
existence of public health services, use of health unit service, how respondent has heard about
health unit program and service, and satisfaction with use of health unit program and service
• Lackofaconsistentdefinitionof“assessingcommunitymembers’familiaritywithpublichealthunit
programs and services” may contribute to inconsistency in reporting

116
27. Issuance of a Health Status Report
Definition:
Indicates whether a board of health has issued a health status report or other health intelligence or
information product that considered inequities in health outcomes and health determinants at any
time in the past.
A health status report or other health intelligence or information product is defined as including any
publication that was designed for distribution to the public that used health status statistics and provided
analysis of these statistics to describe the equity of health outcomes or health determinants.
Data Source(s):
Surveyofboardsofhealth,2008
Formula:
Yes and year; no
Notes:
• Manypublichealthunitspublishhighqualitylocalhealthstatusreportsthatareavailableon
their websites
• Thereisnostandardizeddefinitionofinequitiesinhealthoutcomesinordertocompareresults
between health units
• Assessingonlytheexistenceofareportwithoutassessmentofthescopeofthepublication
• Relevanceofthedatainlocalreportsistimesensitive;olderreportsmaynotbereflectiveof
current situations
• Reportingincludesbothfocusedhealthissuereportsandcomprehensivecommunitywidehealth
status reports
Appendices

117
Initial Report on Public Health 2009
28. Strategic Plan
Definition:
Indicates whether a board of health reports having a strategic plan in place that covers the current
period(2008).
Data Source(s):
Surveyofboardsofhealth,2008
Formula:
Yes, with years of strategic plan; no
Notes:
• Havingastrategicplanwillimproveorganizationalperformanceonlywhereitiswellimplemented
and amended over time in response to emerging situations
• Assessesonlytheexistenceofastrategicplanwithoutassessmentofthescopeoftheplan
• Lackofconsistencyinthecontentandrigorofstrategicplanningmakescompilationofresults
difficult to interpret
• Doesnotprovideinformationonhowthestrategicplanisusedtoinfluenceoperationsandachieve
strategic goals

118
29. Emergency Response Plan Tested
Definition:
Indicates whether a board of health has an internal board of health emergency response plan and whether
theplanwastestedbetweenJanuary1,2007andthedateofthesurveyinNovember,2008.Testingan
emergency response plan includes activities such as running a table top exercise, testing a telephone call
out list of all staff, and holding a mock emergency scenario.
Data Source(s):
Surveyofboardsofhealth,2008
Formula:
Yes, with description of testing method; no
Notes:
• Includedasameasureofpublichealthunitemergencypreparedness;providesastartingpointfor
the development of possible future indicators, which may relate to community awareness of public
health’s role in emergency preparedness or effectiveness of staff training in emergency preparedness
• Becausemunicipalitiesarerequiredtohaveanorganizationalemergencyresponseplan,nilresponses
were not anticipated
• Criteriafortestingtheplanwereself-definedanddescribedbyboardsofhealth
• Lackofathresholdforadequacyoftestinganemergencyresponseplanwilllimitinterpretation
of results
Appendices

119
Initial Report on Public Health 2009
30. Accreditation Status
Definition:
Indicates whether a board of health participates in an accreditation process by accrediting body and
current accreditation status.
Data Source(s):
Surveyofboardsofhealth,2008
Formula:
Yes, by specific accrediting body, by accreditation status; no
Notes:
• Boardsofhealthmayhavebeenaccreditedinthepast,butnotcurrentlyaccredited
• Therearedifferencesinscopeofaccreditationstandardsacrossdifferentorganizations
• Numbersincludeboardsofhealththatarebothaccreditedandcurrentlyintheprocessofbecoming
accredited

120
31. Medical Officer of Health Performance Evaluation
Definition:
Indicates completion of a regularly scheduled performance evaluation of the medical officer of health, by
type of evaluator, and year of the most recent evaluation.
Data Source(s):
Surveyofboardsofhealth,2008
Formula:
Yes, with date of most recent evaluation and type of evaluator; no
Notes:
• CapacityReviewCommittee(CRC)surveyofboardofhealthmanagementgovernancepractices
found wide variations in depth and scope of MOH performance evaluation practices
• Themethodsofstaffevaluationsusedandtherigoroftheprocessesisinfluencedbydifferent
governance models across boards of health
• Doesnotcaptureperformanceevaluationpracticesrelatingtootherexecutiveofficers,suchasCAOs
and CEOs
Appendices

121
Initial Report on Public Health 2009
32. Medical Officer of Health Reporting Relationships
Definition:
Indicates medical officer of health attendance at board of health meetings and/or standing committee
meetings, and whether he of she participated in the meetings. Participation includes attending meetings
and providing reports, advice or presentations to the board.
Data Source(s):
Surveyofboardsofhealth,2008
Formula:
Yes on reporting to board of health, standing committee or both; no
Yes on attending specific meetings; no
Notes:
• Surveydataindicatethatsomemedicalofficersofhealthparticipateinmeetingsofastanding
committee as well as meetings of the board of health
• Doesnotdescribethequalityofthemedicalofficerofhealth’sinteractionwiththeboard

122
33. Board Member Orientation
Definition:
Indicates situations where new board of health members are provided with an orientation to the roles and
responsibilities of the board of health, the duties of members and information to understand public health
functions and issues.
Data Source(s):
Surveyofboardsofhealth,2008
Formula:
Yes; no
Notes:
• Presenceofboardorientationdoesnotindicatewhetherorientationsareinfluencinggovernance
capacity or effectiveness
• Lackofconsistencyinthecontentandrigoroforientationofboardmembersmakesresultsdifficult
to interpret
Appendices

123
Initial Report on Public Health 2009
34. Board Self-Evaluation
Definition:
Indicates whether a board of health has engaged in a process to evaluate its governance processes and
organizational effectiveness.
Data Source(s):
Surveyofboardsofhealth,2008
Formula:
Yes; no
Notes:
• Presenceofboardselfevaluationdoesnotindicatewhetherboardselfevaluationsinfluence
governance practices or effectiveness
• Lackofconsistencyinthecontentandrigorofboardselfevaluationmakesresultsdifficultto
interpret

124

125
1
Last JM, editor. A dictionary of public health. New York: Oxford University Press; 2006.
2
O’Connor DR. Part one: report of the Walkerton Inquiry: the events of May 2000 and related issues.
Toronto,ON:Queen’sPrinterforOntario;2002.RetrievedApril23,2009from:
http://www.attorneygeneral.jus.gov.on.ca/english/about/pubs/walkerton/part1/.
3
O’Connor DR. Part two: report of the Walkerton Inquiry: a strategy for safe drinking water. Toronto, ON:
Queen’sPrinterforOntario;2003.RetrievedApril23,2009from:
http://www.attorneygeneral.jus.gov.on.ca/english/about/pubs/walkerton/part2/.
4
Expert Panel on SARS and Infectious Disease Control, Walker D. For the public’s health: a plan of action.
Final report of the Ontario Expert Panel on SARS and Infectious Disease Control. Toronto, ON:
Queen’sPrinterforOntario;2004.RetrievedApril23,2009from:
http://www.health.gov.on.ca/english/public/pub/ministry_reports/walker04/walker04_mn.html.
5
Expert Panel on SARS and Infectious Disease Control, Walker D. For the public’s health:
initial report of the Ontario Expert Panel on SARS and Infectious Disease Control. Toronto,
ON:Queen’sPrinterforOntario;2003.RetrievedApril23,2009from:
http://www.health.gov.on.ca/english/public/pub/ministry_reports/walker_panel_2003/walker_panel.html.
6
National Advisory Committee on SARS and Public Health, Naylor D. Learning from SARS: the renewal of
public health in Canada. Ottawa, ON: Health Canada; 2003. Retrieved April 23, 2009 from:
http://www.phac-aspc.gc.ca/publicat/sars-sras/pdf/sars-e.pdf.
7
SARSCommission,CampbellA.Springoffear:finalreport.Toronto,ON:Queen’sPrinterforOntario;
2006. Retrieved April 23, 2009 from:
http://www.health.gov.on.ca/english/public/pub/ministry_reports/campbell06/online_rep/index.html.
8
SARS Commission, Campbell A. The SARS Commission second interim report: SARS and public health
legislation.Toronto,ON:Queen’sPrinterforOntario;2005.RetrievedApril23,2009from:
http://www.health.gov.on.ca/english/public/pub/ministry_reports/campbell05/campbell05.pdf.
9
SARS Commission, Campbell A. The SARS Commission interim report: SARS and public health in Ontario.
Toronto,ON:Queen’sPrinterforOntario;2004.RetrievedApril23,2009from:
http://www.health.gov.on.ca/english/public/pub/ministry_reports/campbell04/campbell04.pdf.
10
Ministry of Health and Long-Term Care, Public Health Division. Operation health protection: an action
plantopreventthreatstoourhealthandtopromoteahealthyOntario.Toronto,ON:Queen’sPrinterfor
Ontario; 2004. Retrieved April 23, 2009 from: http://www.health.gov.on.ca/english/public/pub/ministry_
reports/consumer_04/oper_healthprotection04.pdf.
11
Health Protection and Promotion Act, R.S.O. 1990, c. H7. Retrieved April 14, 2009 from:
http://www.e-laws.gov.on.ca/html/statutes/english/elaws_statutes_90h07_e.htm.
References

126
12
Capacity Review Committee. Revitalizing Ontario’s public health capacity: the final report of the Capacity
ReviewCommittee.Toronto,ON:Queen’sPrinterforOntario;2006.RetrievedApril23,2009from:http://
www.health.gov.on.ca/english/public/pub/ministry_reports/capacity_review06/capacity_review06.pdf.
13
Nutbeam,D.Healthpromotionglossary.Geneva,Switzerland:WorldHealthOrganization;1998.Retrieved
April 14, 2009 from: http://www.who.int/hpr/NPH/docs/hp_glossary_en.pdf.
14
Ministry of Health and Long-Term Care, Public Health Division. Ontario public health standards. Toronto,
ON:Queen’sPrinterforOntario;2008.RetrievedApril8,2009from:http://www.health.gov.on.ca/english/
providers/program/pubhealth/oph_standards/ophs/progstds/pdfs/ophs_2008.pdf.
15
StatisticsCanada.HealthIndicators.82-221-X.,no.1.Healthregionsandpeergroups.Ottawa,On.
MinisterofIndustry;2008.RetrievedApril15,2009from:
http://www.statcan.gc.ca/pub/82-221-x/2008001/5202322-eng.htm
16
Woodward G, Manuel D, Goel V. Developing a balanced scorecard for public health. Toronto, ON:
Institute for Clinical Evaluative Sciences; 2004. Retrieved April 14, 2009 from:
http://www.ices.on.ca/file/Scorecard_report_final.pdf.
17
OntarioHealthQualityCouncil.Qmonitor:2008reportonOntario’sHealthSystem.Toronto,ON:
Queen’sPrinterforOntario;2008.RetrievedApril14,2009from:
http://www.ohqc.ca/pdfs/ohqc_2008_report_-_english.pdf.
18
MinistryofHealthandLong-TermCare.OntarioHealthSystemScorecard2007/08.Toronto,ON:
Queen’sPrinterforOntario;2008.
19
Health Canada. Healthy Canadians: a federal report on comparable health indicators 2006. Ottawa, ON:
HerMajestytheQueeninRightofCanada;2006.RetrievedApril14,2009from:http://www.hc-sc.gc.ca/hcs-
sss/alt_formats/hpb-dgps/pdf/pubs/2006-fed-comp-indicat/2006-fed-comp-indicat-eng.pdf.
20
TheChiefPublicHealthOfficer’sreportonthestateofpublichealthinCanada2008:addressinghealth
inequalities.Ottawa,ON:HerMajestytheQueeninRightofCanada;2008.RetrievedApril14,2009from:
http://www.phac-aspc.gc.ca/publicat/2008/cpho-aspc/pdf/cpho-report-eng.pdf.
21
Dunkley G, Ciliska D, Michelin L, et al. Towards outcome measurement for Ontario boards of health: a
planning and evaluation model via an analysis of the Ontario mandatory health programs and services
guidelines. Hamilton, ON: Public Health Research, Education, and Development Program: 2002. Retrieved
April 14, 2009 from: http://www.phred-redsp.on.ca/Docs/Reports/Ottawa/PlanEvaluationModelJan02.PDF.
22
ParanjothyS,BroughtonH,AdappaR,FoneD.Teenagepregnancy:whosuffers?ArchDisChild.
2009;94(3):239-45.
23
Dryburgh, H. Teenage pregnancy. Health Reports. 2000;12(1): 9-19. Retrieved April 14, 2009 from:
http://www.statcan.gc.ca/studies-etudes/82-003/archive/2000/5299-eng.pdf.
24
Federal, Provincial, and Territorial Advisory Committee on Population Health. Statistical report on the
health of Canadians. Ottawa, ON: Statistics Canada; 1999. Retrieved April 14, 2009 from:
http://www.statcan.gc.ca/pub/82-570-x/82-570-x1997001-eng.pdf.
References

127
Initial Report on Public Health 2009
25
Chen XK, Wen SW, Fleming N, Demissie K, Rhoads GG, Walker M. Teenage pregnancy and adverse birth
outcomes:alargepopulationbasedretrospectivecohortstudy.IntJEpidemiol.2007Apr;36(2):368-73.
26
Kearney MS, Levine PB. Socioeconomic disadvantage and early childbearing. Cambridge, MA: National
Bureau of Economic Research; 2007. Retrieved April 14, 2009 from: http://www.nber.org/papers/w13436.pdf.
27
Luong,M.Lifeafterteenagemotherhood.PerspectivesonLabourandIncome.2008;6-13.
RetrievedApril15,2009from:http://www.statcan.gc.ca/pub/75-001-x/2008105/pdf/10577-eng.pdf.
28
East PL, Reyes BT, Horn EJ. Association between adolescent pregnancy and a family history of teenage
births.PerspectSexReprodHealth.2007Jun;39(2):108-15.
29
Wellings, K. Causes and consequences of teenage pregnancy. In: Baker P, Guthrie K, Hutchinson C, Kane
R, Wellings K, eds. Teenage pregnancy and reproductive health. London: Royal College of Obstetricians
and Gynaecologists; 2007. p.70.
30
Core Health Indicators Work Group. Perinatal mortality. In: Core indicators for public health in Ontario.
Toronto, ON: Association of Public Health Epidemiologists in Ontario; 2005. Retrieved April 15, 2009 from:
http://www.apheo.ca/index.php?pid=145#comments.
31
Cole C, Hagadorn J, Kim C, et al. Criteria for determining disability in infants and children: low birth
weight. Evidence report/technology assessment no. 70. Rockville, MD: Agency for Healthcare Research
andQuality;2002.RetrievedApril15,2009from:
http://www.ahrq.gov/downloads/pub/evidence/pdf/lbw/lbw.pdf.
32
Matsuo, H. The health consequences of low birth weight: literature review and critique. UCL working
paper no. 23. Louvain-la-Neuvem, Belgium: l’Université catholique de Louvain; 2005.
Retrieved April 14, 2009 from: http://www.uclouvain.be/cps/ucl/doc/sped/documents/dt23.pdf.
33
Canadian Institute of Child Health. Fact sheet: low birth weight. In: The health of Canada’s children:
a CICH profile. Ottawa, ON: Canadian Institute of Child Health; 2000. Retrieved April 15, 2009 from:
http://www.cich.ca/PDFFiles/ProfileFactSheets/English/LBWEng.pdf.
34
Perinatal Education Program of Eastern Ontario. Factors and interventions associated with low birth
weight. In: Prevention of low birth weight in Canada: literature review and strategies. 2nd ed.
Toronto,ON:BestStart;1998.RetrievedApril15,2009from:
http://www.beststart.org/resources/lbw_aware/pdf/lbw_aware/lbw_rpt/lbw98TOC.html.
35
AlmondD,ChayKY,LeeDS.Thecostsoflowbirthweight.QuarterlyJournalofEconomics.2005.
120(3):1031–1083.RetrievedApril14,2009from:http://www.nber.org/~almond/qje_bw_final.pdf.
36
KramerMS.Intrauterinegrowthandgestationaldurationdeterminants.Pediatrics.1987;80:502-511.
37
WorldHealthOrganization.Breastfeeding[Internet].Geneva:WorldHealthOrganization;2009.Retrieved
April 15, 2009 from: ; 2009. Retrieved April 15, 2009 from: http://www.who.int/topics/breastfeeding/en/.

128
38
Canadian Paediatric Society; Dietitians of Canada; Health Canada. Benefits of breastfeeding to infants
in Canada. In: Nutrition for healthy term infants. Ottawa, ON: Minister of Public Works and Government
Services Canada; 2005. Retrieved April 15, 2009 from:
http://www.hc-sc.gc.ca/fn-an/pubs/infant-nourrisson/nut_infant_nourrisson_term_3-eng.php#benefits.
39
Owen CG, Martin RM, Whincup PH, Smith GD, Cook DG. Does breastfeeding influence risk of type 2
diabetesinlaterlife?Aquantitativeanalysisofpublishedevidence.AmericanJournalofClinicalNutrition.
2006;84(5):1043-1054.RetrievedApril15,2009from:http://www.ajcn.org/cgi/reprint/84/5/1043.pdf.
40
College of Family Physicians of Canada. Infant feeding policy statement 2004. Toronto, ON: College
of Family Physicians of Canada; 2004. Retrieved April 15, 2009 from: http://www.cfpc.ca/local/files/
Communications/Health%20Policy/Final_04Infant_Feeding_Policy_Statement.pdf.
41
Breastfeeding Committee for Canada. Breastfeeding statement of the Breastfeeding Committee for
Canada. Toronto, ON: The Committee; 2002. Retrieved April 15, 2009 from:
http://breastfeedingcanada.ca/pdf/webdoc5.pdf.
42
StatisticsCanada.Canadiancommunityhealthsurvey—cycle2.1[datafile].Ottawa,ON:Statistics
Canada; 2003.
43
StatisticsCanada.Canadiancommunityhealthsurvey[datafile].Ottawa,ON:StatisticsCanada;2005.
44
StatisticsCanada.CanadianCommunityHealthSurvey2007[datafile].Ottawa,ON:StatisticsCanada;
2008.
45
MinistryofHealthandLong-TermCare.Healthybabieshealthychildrenprotocol.Toronto,ON:Queen’s
PrinterforOntario;2008.RetrievedApril15,2009from:http://www.health.gov.on.ca/english/providers/
program/pubhealth/oph_standards/ophs/progstds/protocols/hbhc.pdf.
46
MinistryofHealthPromotion.Smoke-freeOntarioStrategy[Internet].RetrievedAugust7,2009from:
http://intra.mhp.gov.on.ca/what_we_do/smoke_free_ontario/strategy.asp
47
Smoke-Free Ontario Act, S.O. 1994, c. 10. Retrieved April 15, 2009 from:
http://www.e-laws.gov.on.ca/html/statutes/english/elaws_statutes_94t10_e.htm.
48
Health Canada. Youth smoking in Canada. CTUMS: Canadian Tobacco Use Monitoring Survey. Annual.
2000;Feb-Dec: 3. Retrieved April 17, 2009 from: http://www.hc-sc.gc.ca/hc-ps/tobac-tabac/research-
recherche/stat/_ctums-esutc_fs-if/2000-youth-eng.php.
49
Kaufman AR, Augustson EM. Predictors of regular cigarette smoking among adolescent females: does
bodyimagematter?NicotineTobRes.2008;10(8):1301-9.
50
Leatherdale ST, Hammond D, Ahmed R. Alcohol, marijuana, and tobacco use patterns among youth in
Canada.CancerCausesControl.2008;19(4):361-9.
51
Shields, M. Youth smoking. Health Reports. 2005;16(3):53-57. Retrieved April 17, 2009 from:
http://www.statcan.gc.ca/pub/82-003-x/82-003-x2004003-eng.pdf.
References

129
Initial Report on Public Health 2009
52
Roerecke M, Haydon E, Giesbrecht N. Alcohol and chronic disease: an Ontario perspective. Toronto, ON:
Alcohol Policy Network, Ontario Public Health Association; 2007. Retrieved April 17, 2009 from:
http://www.apolnet.ca/resources/pubs/rpt_ChronicDisease.pdf.
53
APOLNET.Statisticaloverviewofalcoholuse.Toronto,ON:AlcoholPolicyNetwork;2008.
Retrieved April 20, 2009 from: http://www.apolnet.ca/AboutUsHome.html.
54
Mukamal KJ. Patient information: risks and benefits of alcohol. Waltham, MA: UpToDate; 2007. Retrieved
April20,2009from:http://www.uptodate.com/patients/content/topic.do?topicKey=~6WTzKjHnjBtd1.
55
MinistryofHealthandLong-TermCare.Alcoholandsubstanceabuseprevention[Internet].
Toronto,ON:Queen’sPrinterforOntario;2006.RetrievedApril15,2009from:
http://www.health.gov.on.ca/english/public/pub/hpromo/hpromo.html#1.
56
Mercer GW (Applied Research and Evaluation Services, University of British Columbia). Estimating the
presence of alcohol and drug impairment in traffic crashes and their costs to Canadians: 1999 to 2006.
Oakville, ON: Mothers Against Drunk Driving Canada; 2009. Retrieved April 20, 2009 from:
http://www.madd.ca/english/research/estimating_presence.pdf.
57
Core Health Indicators Work Group. Heavy drinking episodes. In: Core indicators for public health in
Ontario. Toronto, ON: Association of Public Health Epidemiologists in Ontario; 2009.
RetrievedApril15,2009from:http://www.apheo.ca/index.php?pid=123.
58
SMARTRISK. The economic burden of injury in Ontario.
Toronto,ON:Queen’sPrinterforOntario;2006.RetrievedApril17,2009from:
http://www.mhp.gov.on.ca/english/injury_prevention/Smartrisk-EBI-Ont-2006.pdf.
59
BrewerRD,SwahnMH.Bingedrinkingandviolence.JAMA.2005;294(5):616-8.
60
Kuo M, Adlaf EM, Lee H, Gliksman L, Demers A, Wechsler H. More Canadian students drink but American
studentsdrinkmore:comparingcollegealcoholuseintwocountries.Addiction.2002Dec;97(12):1583-92.
Retrieved April 20, 2009 from: http://www.hsph.harvard.edu/cas/Documents/Canadian1/CanadaPaper.pdf.
61
Centers for Disease Control and Prevention Women and alcohol. Atlanta, GA: Centers for Disease Control
and Prevention; 2007. Retrieved April 20, 2009 from: http://www.cdc.gov/Features/WomenAndAlcohol/.
62
Tapert SF, Caldwell L, Burke C. Alcohol and the adolescent brain: human studies.
AlcoholResHealth.2004-2005;28(4):205-212.
RetrievedApril20,2009from:http://pubs.niaaa.nih.gov/publications/arh284/205-212.pdf.
63
LeslieK.Alcoholanddruguseamongteenagers.CMAJ.2008Jan15;178(2):149.RetrievedApril20,2009
from:http://www.cmaj.ca/cgi/reprint/178/2/149.pdf.
64
Chamberlain EA, Solomon RM. Minimizing impairment-related youth traffic deaths: the need for
comprehensiveprovincialaction.CanJPublicHealth.2008;99(4):267-70.RetrievedApril20,2009from:
http://journal.cpha.ca/index.php/cjph/article/view/1657/1841.pdf.

130
65
Rehm J, Giesbrecht N, Patra J, Roerecke M. Estimating chronic disease deaths and hospitalizations
due to alcohol use in Canada in 2002: Implications for policy and prevention strategies.
Prev Chronic Dis. 2006;3(4):A121.
66
Rehm J, Patra J, Popova S. Alcohol-attributable mortality and potential years of life lost in Canada 2001:
Implicationsforpreventionandpolicy.Addiction.2006;101(3):373-84.
67
Beck KH, Treiman KA. The relationship of social context of drinking, perceived social norms, and parental
influence to various drinking patterns of adolescents. Addict Behav. 1996;21(5):633-44.
68
Pedersen ER, LaBrie JW. Normative misperceptions of drinking among college students: a look at the
specificcontextsofprepartyinganddrinkinggames.JStudAlcoholDrugs.2008;69(3):406-11.
69
Simons-Morton B. Prospective association of peer influence, school engagement, drinking expectancies,
and parent expectations with drinking initiation among sixth graders. Addict Behav. 2004;29(2):299-309.
70
Miller JW, Naimi TS, Brewer RD, Jones SE. Binge drinking and associated health risk behaviors among
highschoolstudents.Pediatrics.2007;119(1):76-85.
71
World Helath Organization. Global status report on alcohol 2004.
Geneva:WorldHealthOrganization;2004.pp.35-58.RetrievedApril23,2009from:
http://www.who.int/substance_abuse/publications/globalstatusreportalcohol2004_healtheffects.pdf.
72
Jones M, O’Beney, C. Promoting mental health through physical activity: examples from practice. J Ment
Health Prom. 2004;3(1):39-47.
73
Warburton DE, Katzmarzyk PT, Rhodes RE, Shephard RJ. Evidence-informed physical activity guidelines
forCanadianadults.CanJPublicHealth.2007;98Suppl2:S16-68.
74
Katzmarzyk PT, Gledhill N, Shephard RJ. The economic burden of physical inactivity in Canada. CMAJ.
2000Nov28;163(11):1435-40.
75
Janssen I, Lam M, Katzmarzyk PT. Influence of overweight and obesity on physician costs in adolescents
and adults in Ontario, Canada. Obes Rev. 2009;10(1):51-7.
76
Herman KM, Craig CL, Gauvin L, Katzmarzyk PT. Tracking of obesity and physical activity from childhood
toadulthood:ThePhysicalActivityLongitudinalStudy.IntJPediatrObes.2008Dec15:1-8.
77
Ministry of Health Promotion. ACTIVE 2010: Ontario’s sport and physical activity strategy.
Toronto,ON.Queen’sPrinterforOntario;2005.Availablefrom:
http://www.mhp.gov.on.ca/English/sportandrec/physical_activity/active2010-strategy-e.pdf.
78
World Health Organization. Obesity: preventing and managing the global epidemic: report of a
WHOconsultation.WHOTechnicalReportSeries#894.Geneva:WorldHealthOrganization;2000.
Table 2.1: Classification of adults according to BMI, p. 9. Retrieved August 11, 2009 from:
http://whqlibdoc.who.int/trs/WHO_TRS_894_(part1).pdf.
79
Luo W, Morrison H, de Groh M, et al. The burden of adult obesity in Canada. Chronic Dis Can.
2007;27(4):135-44.
References

131
Initial Report on Public Health 2009
80
StatisticsCanada.LeadingcausesofdeathinCanada–2005[Internet].84-215-X.Ottawa,ON:Statistics
Canada, 2009. Table 3-6: Ten leading causes of death, by sex and geography, 2005 – Ontario. Retrieved
April20,2009from:http://www.statcan.gc.ca/pub/84-215-x/2009000/tbl/t019-eng.pdf.
81
Ontario.MinistryofHealthandLong-TermCare.OntariolaunchesDiabetesStrategy[pressrelease].
July22,2008.RetrievedApril20,2009from:
http://www.newswire.ca/en/releases/archive/July2008/22/c6499.html.
82
Public Health Agency of Canada. Living with diabetes. National diabetes fact sheet.
Ottawa:PublicHealthAgencyofCanada;2008.RetrievedAugust6,2009from:
http://www.phac-aspc.gc.ca/publicat/2008/ndfs-fnrd-08/ndfs_lwd-fnrd_vad-eng.php.
83
Heart and Stroke Foundation of Canada. 2004 Annual Report Card on Canadians’ Health.
Ottawa: Heart and Stroke Foundation of Canada; 2004.
84
Nathan SA, Develin E, Grove N, Zwi AB. An Australian childhood obesity summit: the role of data and
evidence in ‘public’ policy making. Aust New Zealand Health Policy. 2005 Jul 20;2:17. Retrieved April 20,
2009from:http://www.anzhealthpolicy.com/content/pdf/1743-8462-2-17.pdf.
85
JillingsC,SamisS.Isfatthenewtobacco?StrategiesforaddressingtheobesityepidemicinCanada.
12th EUPHA conference: urbanisation and health: new challenges in health promotion and prevention.
Eur J Public Health. 2004; 14(Suppl 1): 35.
86
Lobstein T, Baur L, Uauy R; IASO International Obesity TaskForce. Obesity in children and young people:
a crisis in public health. Obes Rev. 2004;5 Suppl 1:4-104.
87
Guo SS, Wu W, Chumlea WC, Roche AF. Predicting overweight and obesity in adulthood from body mass
indexvaluesinchildhoodandadolescence.AmJClinNutr.2002;76(3):653-8.RetrievedAugust6,2009
from: http://www.ajcn.org/cgi/reprint/76/3/653.pdf.
88
Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from
childhoodandparentalobesity.NEnglJMed.1997;337(13):869-73.RetrievedAugust6,2009from:
http://content.nejm.org/cgi/reprint/337/13/869.pdf.
89
Koplan JP, Liverman CT, Kraak VI. Preventing childhood obesity: health in the balance.
Washington, DC: National Academies Press; 2005.
90
Basrur SV. 2004 Chief Medical Officer of Health report: healthy weights, healthy lives. Toronto, ON:
Queen’sPrinterforOntario;2004.Availablefrom:http://www.health.gov.on.ca/english/public/pub/
ministry_reports/cmoh04_report/healthy_weights_112404.pdf.
91
Ministry of Health Promotion. Ontario’s action plan for healthy eating and active living. Toronto, ON:
Queen’sPrinterforOntario;2006.RetrievedApril20,2009from:http://www.mhp.gov.on.ca/english/health/
HEAL/actionplan-EN.pdf.
92
World Cancer Research Fund and American Institute for Cancer Research. Food, nutrition, physical
activity, and the prevention of cancer: a global perspective. Washington, DC: AIRC; 2007.

132
93
Hung HC, Joshipura KJ, Jiang R, et al. Fruit and vegetable intake and risk of major chronic disease.
JNatlCancerInst.2004;96(21):1577-84.
94
Hall JN, Moore S, Harper SB, Lynch JW. Global variability in fruit and vegetable consumption.
Am J Prev Med. 2009;36(5):402-409, e5.
95
Shields M. Nutrition: findings from the Canadian Community Health Survey. Measured obesity:
overweightCanadianchildrenandadolescents[Internet].Ottawa,ON:StatisticsCanada;2005.
Chart 9: Overweight and obesity rates, by fruit and vegetable consumption, household population
aged 2 to 17, Canada excluding territories, 2004.Retrieved April 23, 2009 from:
http://www.statcan.gc.ca/pub/82-620-m/2005001/c-g/child-enfant/4053588-eng.htm.
96
NationalSafetyCouncil.Fallsleadingcauseofinjurydeathforpeople65andolder[pressrelease].
May7,2008.RetrievedApril23,2009from:http://www.nsc.org/news/nr050708.aspx.
97
Public Health Agency of Canada, Division of Aging and Seniors. Report on seniors’ falls in Canada.
Ottawa, ON: Minister of Public Works and Government Services Canada; 2005. Retrieved April 23, 2009
from: http://www.phac-aspc.gc.ca/seniors-aines/pubs/seniors_falls/pdf/seniors-falls_e.pdf.
98
Stevens JA, Corso PS, Finkelstein EA, Miller TR. The costs of fatal and non-fatal falls
among older adults. Inj Prev. 2006 Oct;12(5):290-5. Retrieved August 5, 2009 from:
http://injuryprevention.bmj.com/cgi/reprint/12/5/290.pdf.
99
Tiedemann AC, Murray SM, Munro B, Lord SR. Hospital and non-hospital costs for fall-related injury in
community-dwellingolderpeople.NSWPublicHealthBull.2008Sep-Oct;19(9-10):161-5.
100
SMARTRISK. The economic burden of injury in Ontario.
Toronto:Smartrisk;2006.p.47-48.RetrievedAugust5,2009
from: http://www.oninjuryresources.ca/downloads/Ontario_Economic_Burden_of_Injury.pdf.
101
Beard J, Rowell D, Scott D, van Beurden E, Barnett L, Hughes K, Newman B. Economic analysis of a
community-basedfallspreventionprogram.PublicHealth.2006Aug;120(8):742-51.Epub2006Jul5.
102
Ontario Injury Prevention Resource Centre. Falls across the lifespan: evidence-based
practicesynthesisdocument.Toronto:Smartrisk;2008.RetrievedAugust5,2009from:
http://www.oninjuryresources.ca/downloads/misc/FallsReview-D8.pdf.
103
Public Health Agency of Canada. Report on seniors’ falls in Canada.
Ottawa: Public Health Agency of Canada; 2005. Retrieved August 5, 2009 from:
http://www.phac-aspc.gc.ca/seniors-aines/pubs/seniors_falls/pdf/seniors-falls_e.pdf.
104
Majowicz SE, Edge VL, Fazil A, et al. Estimating the under-reporting rate for infectious gastrointestinal
illnessinOntario.CanJPublicHealth.2005;96(3):178-81.
105
Ministry of Health and Long-Term Care, Public Health Division and Long-Term Care Homes Branch.
A guide to the control of respiratory infection outbreaks in long-term care homes.
Toronto,ON:Queen’sPrinterforOntario;2004.p.19.RetrievedApril23,2009from:
http://www.health.gov.on.ca/english/providers/pub/pubhealth/ltc_respoutbreak/ltc_respoutbreak.pdf.
References

133
Initial Report on Public Health 2009
106
Chong CP, Street PR. Pneumonia in the elderly: a review of the epidemiology, pathogenesis, microbiology,
andclinicalfeatures.SouthMedJ.2008;101(11):1141-5.
107
Chan Carusone SB, Walter SD, Brazil K, Loeb MB. Pneumonia and lower respiratory infections in nursing
home residents: predictors of hospitalization and mortality. J Am Geriatr Soc. 2007 ;55(3):414-9.
108
Public Health Agency of Canada. 2002 Canadian sexually transmitted infections surveillance report.
Can Commun Dis Rep. 2005;31(Suppl 2):1-39. Retrieved April 23, 2009 from:
http://www.phac-aspc.gc.ca/publicat/ccdr-rmtc/05pdf/31s2_e.pdf.
109
Wong T, Singh A, Mann J, Hansen L, McMahon, S. Gender differences in bacterial STIs in
Canada. BMC Women’s Health. 2004;4(Suppl 1):S26. Retrieved April 23, 2009 from:
http://www.pubmedcentral.nih.gov/picrender.fcgi?artid=2096668&blobtype=pdf.
110
Zuckerman J, van Hattum J, Cafferkey M, et al. Should hepatitis B vaccination be introduced into
childhoodimmunisationprogrammesinnorthernEurope?LancetInfectDis.2007;7(6):410-9.
111
Tepper ML, Gully PR. Lovers and livers: Hepatitis B as an STD. Can J Hum Sexuality. 1997; 6(2): 135-142.
112
Piot P, Goilav C, Kegels E. Hepatitis B: transmission by sexual contact and needle sharing.
Vaccine.1990Mar;8Suppl:S37-40.
113
Ministry of Health and Long-Term Care. Publicly funded immunization schedules for Ontario –
January2009[Internet].Toronto,ON:Queen’sPrinterforOntario;2009.RetrievedApril23,2009from:
http://www.health.gov.on.ca/english/providers/program/immun/pdf/schedule.pdf.
114
PerryRT,HalseyNA.Theclinicalsignificanceofmeasles:areview.JInfectDis.2004;189(Suppl1):S4-16.
115
Masarani M, Wazait H, Dinneen M. Mumps orchitis. J R Soc Med. 2006;99(11):573-5.
116
Anonymous.Rubella(Germanmeasles)inpregnancy.PaediatrChildHealth.2007Nov;12(9):798-802.
117
Immunization of School Pupils Act, R.S.O. 1990, c. I.1. Retrieved April 23, 2009 from:
http://www.e-laws.gov.on.ca/html/statutes/english/elaws_statutes_90i01_e.htm.
118
O. Reg. 169/03. Retrieved April 23, 2009 from:
http://www.e-laws.gov.on.ca/html/regs/english/elaws_regs_030169_e.htm.
119
Safe Drinking Water Act, S.O. 2002, c.32. Retrieved April 23, 2009 from:
http://www.e-laws.gov.on.ca/html/statutes/english/elaws_statutes_02s32_e.htm.
120
O. Reg. 170/03. Retrieved April 23, 2009 from:
http://www.e-laws.gov.on.ca/html/regs/english/elaws_regs_030170_e.htm.
121
O.Reg.318/08.RetrievedApril23,2009from:
http://www.e-laws.gov.on.ca/html/regs/english/elaws_regs_080318_e.htm.
122
O.Reg.319/08.RetrievedApril23,2009from:
http://www.e-laws.gov.on.ca/html/regs/english/elaws_regs_080319_e.htm.

134
123
Capacity Review Committee. Revitalizing Ontario’s public health capacity: a discussion of issues and
options.Toronto,ON:Queen’sPrinterforOntario;2005.RetrievedApril15,2009from:http://www.health.
gov.on.ca/english/public/pub/ministry_reports/capacity_review05/capacity_review05.pdf.
124
Capacity Review Committee. Revitalizing Ontario’s public health capacity: a discussion of issues and
options.Toronto,ON:Queen’sPrinterforOntario;2005.RetrievedApril15,2009from:http://www.health.
gov.on.ca/english/public/pub/ministry_reports/capacity_review05/capacity_review05.pdf.
125
Health Protection and Promotion Act, R.S.O. 1990, c. H7, s. 67(1). Retrieved April 14, 2009 from:
http://www.e-laws.gov.on.ca/html/statutes/english/elaws_statutes_90h07_e.htm.
126
StatisticsCanada.HealthIndicators.82-221-X.,no.1.Healthregionsandpeergroups.
Ottawa,Ont.:MinisterofIndustry;2008.RetrievedApril15,2009from:
http://www.statcan.gc.ca/pub/82-221-x/2008001/5202322-eng.htm
127
StatisticsCanada.HealthIndicators.82-221-X.,no.1.Healthregionsandpeergroups.
Ottawa,Ont.:MinisterofIndustry;2008.RetrievedApril15,2009from:
http://www.statcan.gc.ca/pub/82-221-x/2008001/hregions-regionss/5202306-eng.htm
128
StatisticsCanada.HealthIndicators.82-221-X.,no.1.Healthregionsandpeergroups.
Ottawa,Ont.:MinisterofIndustry;2008.RetrievedApril15,2009from:
http://www.statcan.gc.ca/pub/82-221-x/2008001/hregions-regionss/5215169-eng.pdf
129
Thomas S, Wannell B. Combining cycles of the Canadian Community Health Survey.
HealthReports.2009;20(1):53-60.RetrievedJune18,2009from
http://www.statcan.gc.ca/pub/82-003-x/2009001/article/10795-eng.pdf.
130
StatisticsCanada.Healthindicators[Internet].82-221-X.,no.1.Ottawa,ON:MinisterofIndustry;2008.
p.21.RetrievedApril20,2009from:http://www.statcan.gc.ca/pub/82-221-x/82-221-x2008001-eng.pdf.
131
Bains N. Standardization of rates. Toronto: Association of Public Health Epidemiologists in Ontario;
2009. Retrieved July 2, 2009 from: http://www.apheo.ca/resources/indicators/Standardization%20report_
NamBains_FINALMarch16.pdf.
ISBN: 978-1-4249-9794-7 August 2009 © 2009 Queen’s Printer for Ontario
