
California Hospital
Mental Health Law Manual
Mental Health
2019
MentalHealth_Manual_2019_TitlePg_ATP.indd 1 5/17/2019 1:09:20 PM
Limited Use License:
In purchasing this electronic publication (Publication), the individual who purchased it
(Purchaser) agrees to abide by the terms of this Limited Use License. This Limited Use
License: (1) gives Purchaser a non-exclusive, non-assignable, royalty free, perpetual, limited
right to use this electronic publication only for his/her personal use; and (2) prohibits
Purchaser from posting, reproducing, distributing, disseminating, transmitting, or otherwise
allowing anyone else to access or use this Publication. CHA is and will be the sole and
exclusive owner of all right, title, and interest, including intellectual property rights, in this
Publication and its contents. CHA will strictly enforce the terms of this Limited Use License.

September 2019
13th Edition
Mental Health Law
Manual
A handbook on laws governing mental health treatment

Ordering Information
For more information, visit CHA online at www.calhospital.org/publications
This publication is designed to produce accurate and authoritative information with regard to the subject matter covered.
It is sold with the understanding that CHA is not engaged in rendering legal service. If legal or other expert assistance is
required, the services of a competent professional person should be sought.
© 2005, 2009, 2011, 2012, 2013, 2014, 2015, 2016, 2017, 2018, 2019 by the California Hospital Association
© 2003, 2004 by the California Healthcare Association
All rights reserved. First edition 2003.
Thirteenth edition 2019.
No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means,
electronic, mechanical, photocopying, recording, or otherwise, without the prior written approval of:
California Hospital Association
ATTN: Publishing
1215 K Street, Suite 800
Sacramento, CA 95814
However, hospitals that are members of the California Hospital Association may use the model forms, signs and handouts
as templates in developing their own forms, signs and handouts.
It is the intent of CHA to strictly enforce this copyright.
Published by the California Hospital Association.
Printed in the United States of America.
Liz Mekjavich, Vice President, Publishing and Education
Lois J. Richardson, Esq., Vice President and Legal Counsel
Bob Mion, Director, Publishing and Marketing
Emily Stone, Publishing Manager
CHA Publications
Several helpful publications are available through CHA including:
• California Health Information
Privacy Manual
• California Hospital Compliance Manual
• California Hospital Survey Manual —
A Guide to the Licensing & Certification
Survey Process
• Consent Manual
• Discharge Planning for Homeless Patients
• EMTALA — A Guide to
Patient Anti-Dumping Laws
• Guide to Release of Patient Information
• Healthcare Workplace Violence Prevention
Hospital Financial Assistance Policies
and Community Benefit Laws
• Mental Health Law Manual
• Managing High Profile and Patient Care
Conflict Situations
• Minors and Health Care Law Manual
• Model Medical Staff Bylaws & Rules
• Record and Data Retention Schedule
• The Cal/OSHA Safe Patient Handling
Regulation
Plus numerous human resource and volunteer publications.

Preface
Welcome to the thirteenth edition of the Mental Health Law Manual — a handbook on laws
governing mental health treatment. The California Hospital Association has published this manual
to help health care professionals understand the laws governing mental health treatment as well
as the rights and protections of the patients they serve.
This manual is comprised of information taken from two other CHA publications: the Consent
Manual and the California Health Information Privacy Manual. It also contains a chapter on the
state and federal laws governing the use of seclusions and restraint. This edition reflects all state
and federal legislation, regulations, and judicial decisions through January 2019.
We are pleased to publish this manual as a service to our members and others. We hope you will
find it useful.
Lois J. Richardson, Esq.
Vice President and Legal Counsel
Editor, Mental Health Law Manual, Thirteenth Edition
California Hospital Association
(916) 552-7611
Information contained in the Mental Health Law Manual should not be construed as legal advice or used to resolve legal problems
by health care facilities or practitioners without consulting legal counsel. A health care facility may want to accept all or some of the
Mental Health Law Manual as part of its standard operating policy. If so, the hospital or health facility’s legal counsel and its board of
trustees should review such policies.

Quick Reference
INTRODUCTION
WHERE TO FIND LAWS REFERENCED IN THE MANUAL
LIST OF FORMS AND APPENDICES BY CHAPTER
CHAPTERS
Chapter 1
Overview of Mental Health Laws
Chapter 2
Principles of Consent for Mental Health Patients
Chapter 3
Voluntary Admission and Involuntary Detainment for Mental Health
Treatment
Chapter 4
Rights of Mental Health Patients
Chapter 5
Restraints and Seclusion
Chapter 6
Health Information Privacy Basics
Chapter 7
Reporting Assaults, Potentially Dangerous Patients and Firearms
Prohibitions
Chapter 8
Adverse Events and Incident Reports
Chapter 9
Payment for Medi-Cal Emergency and Post-Stabilization Mental
Health Services
LIST OF FORMS AND APPENDICES
INDEX

Introduction
Providing care to patients with mental health issues is complicated. Knowing what is in the best
interest of the patient — and what is legal — isn’t always easy.
Special protections are afforded to individuals with mental health issues who may be unable to
make rational decisions regarding their care. These individuals have the right to be treated by a
provider who protects their interests and preserves their basic rights.
Medical information about mental health treatment is particularly sensitive and therefore add
another layer of complexity to the treatment process. This information must be handled with the
utmost of care. At the same time, disclosure of information to patient advocacy groups, clinical
reviewers, county behavioral health directors and others is sometimes required. And, there are
unique reporting requirements for facilities and individuals that treat mental health patients.
Sorting through the maze of laws governing mental health treatment is particularly difficult
because there are multiple bodies of law. In this manual, all laws governing mental health
treatment and medical privacy are discussed — the Lanterman-Petris-Short (LPS) Act,
the Confidentiality of Medical Information Act (CMIA), the Health Insurance Portability and
Accountability Act (HIPAA), the Health Information Technology for Economic and Clinical Health
(HITECH) Act, and other state and federal laws.
At the back of the manual you will find sample forms and appendices that can be adapted
to fit your specific operations. (These forms can also be found online for CHA members at
www.calhospital.org/free-resources, along with Spanish versions where available.)

All of the laws discussed in the Mental Health Law Manual
can be found on the Internet.
I. FEDERAL LAW
A federal statute is written by a United States Senator or
Representative. It is voted on by the United States Senate
and the House of Representatives, and then signed by the
President. A federal statute is referenced like this: 42 U.S.C.
Section 1395. “U.S.C.” stands for “United States Code.”
Federal statutes may be found at www.gpo.gov/fdsys or at
www.law.cornell.edu.
A federal regulation is written by a federal agency such
as the U.S. Department of Health and Human Services
or the U.S. Food and Drug Administration. The proposed
regulation is published in the Federal Register, along with
an explanation (called the “preamble”) of the regulation,
so that the general public and lobbyists may comment on
it. The federal agency must summarize and respond to
each comment it receives on the proposed regulation. The
agency may or may not make changes to the proposed
regulation based on the comments. The final regulation is
also published in the Federal Register. A federal regulation
is referenced like this: 42 C.F.R. Section 482.1 or 42 C.F.R.
Part 2. “C.F.R.” stands for “Code of Federal Regulations.”
Federal regulations may be found at www.gpo.gov/fdsys or
at www.ecfr.gov. The preamble, however, is only published
in the Federal Register and not in the Code of Federal
Regulations. The Federal Register may be found at www.
gpo.gov/fdsys or at www.federalregister.gov.
The Centers for Medicare & Medicaid Services (CMS)
publishes its Interpretive Guidelines on the internet. The
Interpretive Guidelines include information for surveyors
on how CMS interprets the Conditions of Participation,
and instructions for surveyors on how to assess hospitals’
compliance with the Conditions of Participation. They may
be found at www.cms.gov/Regulations-and-Guidance/
Guidance/Manuals/Internet-Only-Manuals-IOMs.html
(click on Publication 100-07, “State Operations Manual,
then “Appendices Table of Contents”). There are several
appendices that hospitals will find useful, for example, A
(hospitals), AA (psychiatric hospitals), V (EMTALA), and W
(critical access hospitals).
A federal law must be obeyed throughout the United
States, including in California, unless the federal law
expressly states otherwise. As a general rule, if a federal
law conflicts with a state law, the federal law prevails,
unless the federal law expressly states otherwise.
If there is no conflict, such as when one law is stricter
but they don’t actually conflict with each other, both laws
generally must be followed. For example, under the Health
Insurance Portability and Accountability Act of 1996
(HIPAA), the federal law states that providers must conform
to whichever provision of federal or state law provides
patients with greater privacy protection or gives them
greater access to their medical information.
II. STATE LAW
A state statute is written by a California Senator or
Assembly Member. It is voted on by the California Senate
and Assembly, and then signed by the Governor. A state
statute is referenced like this: Civil Code Section 56 or
Health and Safety Code Section 819. State statutes may
be found at www.leginfo.legislature.ca.gov. Proposed laws
(Assembly Bills and Senate Bills) may also be found at
this website.
A state regulation is written by a state agency such as the
California Department of Public Health or the California
Department of Managed Health Care. A short description
of the proposed regulation is published in the California
Regulatory Notice Register, more commonly called the
Z Register, so that the general public and lobbyists may
request a copy of the exact text of the proposed regulation
and comment on it. The state agency must summarize
and respond to each comment it receives on the proposed
regulation. The agency may or may not make changes to
Where to Find Laws Referenced
in the Manual

CHA Where to Find Laws Referenced in the Manual
the proposed regulation based on the comments. A notice
that the final regulation has been officially adopted is also
published in the Z Register. The Z Register may be found at
www.oal.ca.gov/notice_register.htm.
A state regulation is referenced like this: Title 22, C.C.R.,
Section 70707. “C.C.R.” stands for “California Code of
Regulations.” State regulations may be found at www.
calregs.com.
A state law must be obeyed in California only. As a general
rule, if a California law conflicts with a federal law, the
federal law prevails, unless the federal law expressly states
otherwise. (If there is no conflict, such as when one law is
stricter but they don’t actually conflict with each other, both
laws generally must be followed.)

2. PRINCIPLES OF CONSENT FOR MENTAL
HEALTH PATIENTS
1-1
S
Consent to Surgery or Special Procedure*
1-2
S
Informed Consent to Surgery or Special
Procedure*
2-1
S
Self-Sufficient Minor Information
2-2
S
Caregiver’s Authorization Affidavit
2-3
S
Authorization for Third Party to Consent to
Treatment of Minor Lacking Capacity to Consent
2-A Decision Makers for Medical Treatment of Adults
2-B Consent Requirements for Medical Treatment of
Minors*
2-D Health Care Decisions for Unrepresented Patients
2-E Considerations for Revising the Hospital’s Policy
and Procedure Regarding Decision Making for
Unrepresented Patients
4-7
S
Consent to Receive Antipsychotic Medications
8-1
S
Conditions of Admission
23-1
S
Consent for the HIV Test
3. VOLUNTARY ADMISSION AND
INVOLUNTARY DETAINMENT FOR MENTAL
HEALTH TREATMENT
12-1
S
Request for Voluntary Admission and Authorization
for Treatment
12-2 Statement of Professional Person Responsible for
Minor’s Admission
12-3
S
Notice to Minors
12-4 Certification of Admitting Physician
12-5 Application for Involuntary Admission — Inebriates
12-6
S
Notice of Certification for Intensive Treatment
12-7
S
Advisement of Rights — Involuntary Patient
12-8
S
Leave of Absence from Psychiatric Service
12-9
S
Request for Release From Involuntary Treatment
12-10
S
Notice of Certification for Second Involuntary
14-Day Period for Intensive Treatment — Suicidal
Patient
12-11 Petition for Postcertification Treatment of
Imminently Dangerous Person
12-12 Detention of Patient With Psychiatric Emergency in
a Nondesignated Health Facility
(Health and Safety Code Section 1799.111)
12-A Summary of Lanterman-Petris-Short Act’s
Provision for Involuntary Evaluation and Treatment
and Right of Review
4. RIGHTS OF MENTAL HEALTH PATIENTS
13-3
S
Aftercare Plan
5. RESTRAINTS AND SECLUSION
25-A Report of a Hospital Death Associated With
Restraint or Seclusion
6. HEALTH INFORMATION PRIVACY BASICS
16-1
S
Authorization for Use or Disclosure of Health
Information*
16-2
S
Request to Withhold Public Release of
Information
7. REPORTING ASSAULTS, POTENTIALLY
DANGEROUS PATIENTS AND FIREARMS
PROHIBITIONS
13-4 Notice to Law Enforcement Agency: Release of
Person From Hospital From Whom a Firearm or
Other Deadly Weapon Was Confiscated
13-5
S
Notice to Patient: Procedure for Return of
Confiscated Weapon(s)
19-2 Employee Acknowledgment of Child Abuse and
Neglect Reporting Obligations
19-4 Employee Acknowledgment of Elder and
Dependent Adult Abuse Reporting Obligations
19-A Table 19-A Assault and Abuse Reporting
Requirements
These documents are provided in English in the back of the manual. All forms can be found online for CHA members at
www.calhospital.org/free-resources, including Spanish versions, when available. “S” denotes that the form is provided in
English and Spanish.
List of Forms and Appendices by
Chapter
* Indicates forms that are new or revised in this edition.

CHA List of Forms and Appendices by Chapter
8. ADVERSE EVENTS AND INCIDENT
REPORTS
20-1 Adverse Event Report Form — Sample
21-1 Incident Report
21-2 Report to Attorney
9. PAYMENT FOR MEDI-CAL EMERGENCY AND
POST-STABILIZATION MENTAL HEALTH
SERVICES
MH 9-A Medical Necessity for MHP Coverage
MH 9-B Types of MCPs and MHPs
MH 9-C Pertinent DHCS Plan Letters
MH 9-D DHCS Chart: Medi-Cal Mental Health Services
MH 9-E Pertinent Legal Definitions of Emergency
Psychiatric Conditions
* Indicates forms that are new or revised in this edition.

Chapter 1 — Contents
1 Overview of Mental Health Laws
©CALIFORNIA HOSPITAL ASSOCIATION
I. INTRODUCTION ....................................... 1.1
II. THE LANTERMAN-PETRIS-SHORT ACT:
INVOLUNTARY EVALUATION AND
PATIENT RIGHTS
..................................... 1.1
III. LAWS REGARDING RESTRAINT AND
SECLUSION ............................................. 1.1
IV. PATIENT ADVOCACY PROGRAMS ............. 1.1
V. PRIVACY RIGHTS OF MENTAL HEALTH
PATIENTS ................................................ 1.1
A. State Law .......................................................1.2
Mental Health Treatment Information
Protected by LPS
.............................................1.2
Mental Health Treatment Information
Not Protected by LPS
....................................... 1.3
Psychotherapist-Patient Privilege
......................1.3
HIV Test Results
................................................1.3
B. Federal Law ....................................................1.3
HIPAA ...............................................................1.3
Federally-Assisted Substance Use Disorder
Programs
..........................................................1.4

1 Overview of Mental Health Laws
1.1
©CALIFORNIA HOSPITAL ASSOCIATION
I. INTRODUCTION
State and federal law recognize that every adult with
the capacity to make health care decisions has the
fundamental right of self-determination over his or her body
and property. A patient’s right to determine the course of
his or her own medical or mental health treatment may
be limited by the government in only the narrowest of
circumstances; for example, to protect the public health
(in the instance of communicable diseases), and to protect
vulnerable persons who may not be able to protect or care
for themselves. In many cases, the latter category includes
persons who may be seriously mentally ill.
Persons who are mentally ill may not recognize their
need for medical or mental health treatment. Indeed, the
very nature of their illness may cause them to resist the
treatment they desperately need.
State and federal laws seek to balance the conflicting
interests of seriously mentally ill persons. In limited
circumstances, the liberty of a person who may be a
danger to self or others or gravely disabled may be
curtailed while that person undergoes mental health
evaluation and/or treatment. Because our system of
government recognizes the seriousness of curtailing a
person’s liberty for even a short time, laws permitting
involuntary hospitalization include strong procedural and
substantive protections to ensure that these citizens do not
become the victims of abuse.
State and federal laws have also been enacted to provide
protections for mental health patients who have not been
involuntarily hospitalized, in recognition of the fact that even
less seriously mentally ill patients may not be completely
able to protect and advocate for themselves.
This manual describes the laws regulating mental health
evaluation and treatment, whether voluntarily or involuntarily
accessed by the patient. This manual also describes the
rights and responsibilities of health care providers who
evaluate and treat mental health patients.
II. THE LANTERMAN-PETRIS-SHORT ACT:
INVOLUNTARY EVALUATION AND PATIENT
RIGHTS
In California, the main law governing mental health
evaluation and treatment is the Lanterman-Petris-Short
(LPS) Act [Welfare and Institutions Code Section 5000
et seq.]. This law, enacted in 1967 (and amended many
times since then), sets forth the procedures that law
enforcement and health care providers must follow prior to
involuntarily detaining a person for mental health evaluation
and treatment. LPS also sets forth the rights of mental
health patients, whether voluntarily or involuntarily admitted,
and contains procedural requirements that must be
followed prior to providing specified types of treatment to
mental health patients. (See chapters 3 and 4 for detailed
information.)
III. LAWS REGARDING RESTRAINT AND
SECLUSION
Both state and federal law protect patients from the
inappropriate use of seclusion and restraint, and establish
requirements to be followed when the use of either
intervention is necessary. A complete discussion of these
requirements is found in chapter 5.
IV. PATIENT ADVOCACY PROGRAMS
Both state and federal law have appointed independent
parties to safeguard the rights of mental health patients.
The laws regarding patient advocates are found in
chapter 4.
V. PRIVACY RIGHTS OF MENTAL HEALTH
PATIENTS
Both the state and federal constitutions recognize the
privacy rights of all individuals. Due to the sensitive nature
of mental health information, many statutes and regulations
have been enacted to provide confidentiality protections.
A brief overview of these laws follows, with more detailed
information in chapter 6.

CHA Mental Health Law Manual 2019
1.2
©CALIFORNIA HOSPITAL ASSOCIATION
The privacy of a patient’s medical information, including the
use of such information and its disclosure to third parties,
is governed by both California and federal law. Specific
state protections for medical information are provided in the
Confidentiality of Medical Information Act (CMIA) [Civil Code
Section 56 et seq.] and, for specified mental health patients,
in LPS [Welfare and Institutions Code Section 5328 et seq.].
Both the CMIA and LPS govern the disclosure to third
parties of patient-identifiable information by hospitals and
other health care providers. These laws generally specify
that health care providers may not disclose information
relating to patients, their care and treatment, unless
the disclosure is specifically authorized by law or by the
patient. In addition, the federal Health Insurance Portability
and Accountability Act (HIPAA) of 1996 protects medical
information, including mental health information, held by
hospitals, physicians, health plans and others.
A. State Law
California law provides heightened protection to information
relating to mental health treatment delivered in institutional
and other specified outpatient settings under LPS. In
addition, the California legislature has seen fit to protect
mental health treatment information through the creation of
a psychotherapist-patient privilege instead of relying on the
physician-patient privilege that applies to routine medical
information but which has numerous exceptions.
MENTAL HEALTH TREATMENT INFORMATION
PROTECTED BY LPS
Since 1969, LPS [Welfare and Institutions Code sections
5328-5328.9] has provided strict confidentiality protection
to information and records obtained in the course of
providing services to:
1. Patients who are treated or evaluated under Welfare
and Institutions Code Sections 5150-5344. These
code sections include involuntary evaluation and
treatment in a designated facility for patients who are
a danger to self or others or gravely disabled. These
patients do not include patients who may be detained
involuntarily for up to 24 hours in a non-designated
hospital on an emergency basis (usually, but not
always, in the emergency department) under Health
and Safety Code Section 1799.111 (chapter 3 contains
a thorough description of all of these patients); and
2. Patients who are receiving voluntary or involuntary
mental health treatment in a:
a. State mental hospital;
b. County psychiatric ward, facility or hospital;
c. University of California psychiatric facility:
Langley Porter Psychiatric Institute and the
Neuropsychiatric Institute at UCLA. Other
University of California mental health services
providers should consult University of California
counsel regarding their status under LPS;
d. Federal hospital, psychiatric hospital or unit;
e. Private institution, hospital, clinic or sanitarium
which is conducted for, or that includes a
department or ward conducted for, the care and
treatment of persons who are mentally disordered;
f. Psychiatric health facility as described in Health
and Safety Code Section 1250.2;
g. Mental health rehabilitation center as defined in
Welfare and Institutions Code Section 5675;
h. Skilled nursing facility with a special treatment
program service unit for patients with chronic
psychiatric impairments (see Title 22, California
Code of Regulations, Sections 51335 and
72443-72475 regarding such special treatment
programs);
i. Community program funded by the
Bronzan-McCorquodale Act. Because it is often
difficult to determine which patients received
services funded under the Bronzan-McCorquodale
Act, each program and its legal counsel
should review any funds received under the
Bronzan-McCorquodale Act to determine
the applicability, if any, of those confidentiality
provisions as a result of such funding [Welfare and
Institutions Code Sections 5600-5778]; and
j. Community program specified in the Welfare and
Institutions Code Sections 4000-4390 and Welfare
and Institutions Code Sections 6000-6008.
LPS also protects information and records obtained
in the course of providing services to persons with
developmental disabilities. In some instances, overlapping
protection is provided to records of such individuals under
the Lanterman Developmental Disabilities Services Act
[Welfare and Institutions Code Sections 4514-4518], whose
provisions are substantially the same as the provisions
of LPS and apply only to persons with developmental
disabilities, primarily in settings other than private hospitals.
Although LPS became law in 1969, its confidentiality
provisions apply to records and information obtained in
the course of providing similar services to patients prior to
1969.

Chapter 1 — Overview of Mental Health Laws CHA
1.3
©CALIFORNIA HOSPITAL ASSOCIATION
More information about the LPS confidentiality protections
is found in chapter 6.
MENTAL HEALTH TREATMENT INFORMATION NOT
PROTECTED BY LPS
Absent some tie-in to one of the above described
programs, LPS does not apply to other mental health
patients or their records, even though those records
may describe mental health treatment similar to what is
protected under LPS. These records are instead subject
to the Confidentiality of Medical Information Act (CMIA)
(see chapter 6). For example, mental health services
provided to a voluntary patient in a private general acute
care hospital that has no psychiatric unit are subject to the
CMIA rather than LPS. Mental health services provided
to an involuntary patient in a private, non-designated
hospital emergency department are subject to the CMIA
rather than LPS. Mental health services provided by a
consulting psychotherapist to a medical patient (who is not
on a psychiatric hold) are subject to the CMIA rather than
LPS. Also, mental health services provided by a private
psychotherapist in the community are subject to the CMIA.
The information generated by these psychotherapists does
not fall under LPS.
More information about CMIA confidentiality protections is
found in chapter 6.
PSYCHOTHERAPIST-PATIENT PRIVILEGE
The psychotherapist-patient privilege applies to patients
covered by both LPS and CMIA. This privilege is relevant
to health care providers only when patient information is
requested for court proceedings, such as in response to a
subpoena or court order, or for a deposition or testimony
in court. Providers don’t need to consider this privilege
when using or disclosing information for treatment or
payment purposes.
Under the psychotherapist-patient privilege [Evidence Code
Section 1010 et seq.], a patient may refuse to disclose,
and prevent other persons (such as the psychotherapist)
from disclosing, the patient’s confidential communication
with a psychotherapist in the context of legal proceedings.
“Confidential communication” refers to information,
including information obtained by an examination of the
patient, transmitted between a patient and his or her
psychotherapist in the course of that relationship and
in confidence by a means which, so far as the patient
is aware, discloses the information to no third persons
other than those who are present to further the interest
of the patient in the consultation, or those to whom
disclosure is reasonably necessary for the transmission
of the information or the accomplishment of the purpose
for which the psychotherapist is consulted. Confidential
communication also includes a diagnosis made and the
advice given by the psychotherapist in the course of that
relationship. [Evidence Code Section 1012]
The term psychotherapist includes psychiatrists,
psychologists, licensed clinical social workers, school
psychologists, marriage and family therapists, professional
clinical counselors, psychological assistants, and various
interns and trainees for such categories. Interestingly,
the definition of psychotherapist also includes persons
authorized, or reasonably believed by the patient to be
authorized, to practice the professions listed above. Thus,
California law seeks to protect the confidentiality of mental
health information disclosed by patients so long as the
patient reasonably believes that the professional receiving
it is a psychotherapist, regardless of whether the person
actually is a psychotherapist or not.
HIV TEST RESULTS
AIDS became recognized as a specific disease in the
United States in 1981. Because of the stigma associated
with the disease then, the California legislature gave
HIV test results extra confidentiality protection in 1985.
These strict laws are still on the books. The confidentiality
protections afforded to HIV test results are discussed in
chapter 6.
B. Federal Law
HIPAA
The state laws described above are augmented by federal
privacy protections pursuant to HIPAA. HIPAA provides
federal protection to all medical information, including
mental health information, held by hospitals, physicians,
health plans and other “covered entities.” With the
exception of a narrow category relating to psychotherapy
notes, HIPAA does not distinguish between mental health
and other forms of medical information. State provisions
that are more stringent than HIPAA continue in effect; as a
result, many of the California protections specific to mental
health information continue to provide additional protection.
HIPAA calls for providers to conform to whichever federal or
state law provides patients with greater privacy protection
or with greater access to their own health information.
Specifically, providers must comply with whichever
provision of each law is more strict. Thus if HIPAA is
more stringent than California law, with the exception of
one provision, providers must comply with HIPAA and

CHA Mental Health Law Manual 2019
1.4
©CALIFORNIA HOSPITAL ASSOCIATION
the provision in state law that gives the individual greater
protection.
HIPAA contains patient privacy rights including the right to
a Notice of Privacy Practices, the right to access medical
information, the right to request amendments, and the
right to an accounting of disclosures, among others. These
rights are discussed in chapter 6.
HIPAA also restricts the use and disclosure of medical
information. These restrictions are described in chapter 6.
Psychotherapy Notes
HIPAA introduced the concept of “psychotherapy notes.”
There is no such concept in California law. “Psychotherapy
notes” means:
notes recorded (in any medium) by a health care provider
who is a mental health professional documenting or
analyzing the contents of conversation during a private
counseling session or a group, joint, or family counseling
session and that are separated from the rest of the
individual’s medical record. (emphasis added)
Most hospitals, skilled nursing facilities, and other
institutional providers will not have psychotherapy notes, as
defined in HIPAA, because the definition requires the notes
to be separate from the rest of the medical record.
The special provisions in HIPAA regarding the use and
disclosure of psychotherapy notes must be complied
with for all patient types in California — patients whose
records are covered by the CMIA, patients whose records
are covered by LPS, and patients receiving services in a
federally-assisted drug or alcohol abuse program.
More information about psychotherapy notes is found in
chapter 6.
FEDERALLY-ASSISTED SUBSTANCE USE DISORDER
PROGRAMS
The federal government has promulgated confidentiality
rules that apply to drug and alcohol abuse treatment
programs. These rules do not apply to all substance
abuse patients; they apply only to patients served by
“federally-assisted programs.” These rules are described in
detail in CHA’s California Health Information Privacy Manual,
available online at www.calhospital.org/privacy.

Chapter 2 — Contents
©CALIFORNIA HOSPITAL ASSOCIATION
2 Principles of Consent for Mental
Health Patients
I. INTRODUCTION ....................................... 2.1
II. WHY CONSENT IS NECESSARY ................ 2.1
A. The Patient’s Right to Consent to, or
Refuse, Medical Treatment
..........................2.1
Failure to Obtain Consent: Battery .....................2.1
Failure to Obtain Informed Consent:
Malpractice
.......................................................2.2
Informed Refusal
...............................................2.2
B. The Patient’s Right to Consent to
Hospital Services
...........................................2.2
III. WHEN CONSENT IS NECESSARY .............. 2.2
A. General Rule ..................................................2.2
B. Emergency Treatment Exception ................2.3
Statement of Principle .......................................2.3
Limitations
........................................................ 2.3
Recommended Procedure for Providing
Care Pursuant to the Emergency Medical
Treatment Exception
.........................................2.3
Immunity From Liability
......................................2.4
C. Other Circumstances in Which a
Physician is Not Required to Obtain
Informed Consent
..........................................2.4
Circumstances ..................................................2.4
Procedure
.........................................................2.5
D. Exceptions for Minors ...................................2.5
IV. INFORMED CONSENT .............................. 2.5
A. Elements of Informed Consent ....................2.5
B. Identifying Procedures That Require
Informed Consent
..........................................2.6
C. The Role of the Physician in Obtaining
Informed Consent ..........................................2.6
Process by Which Physician Informs Patient......2.6
Informed Consent Forms That Contain
Medical Information
..........................................2.7
Physician Documentation
..................................2.7
D. The Role of the Hospital in the
Informed Consent Process
...........................2.8
Verification That Informed Consent Has
Been Obtained
.................................................2.8
Obtaining Verification
........................................2.8
Recommended Procedure for Completing
the Hospital’s Form
........................................... 2.8
Procedure When Physician Uses Informed
Consent Forms That Contain Medical
Information
.......................................................2.9
E. Two-Doctor Consent .....................................2.9
F. Duration of Informed Consent ...................... 2.9
G. Patient Doubt or Confusion Concerning
Informed Consent ..........................................2.9
V. HOW CONSENT SHOULD BE OBTAINED .... 2.9
A. Capacity to Consent ....................................2.10
B. Consent Must Be Knowingly Made and
Freely Given
.................................................2.10
C. The Nature of Consent ................................2.10
D. Consent Evidenced in Writing ....................2.10
Recommended Forms ....................................2.10
Principles Guiding Completion of Forms
.......... 2.10
E. Securing Consent When
Communication Barriers Exist
...................2.11
VI. WHO MAY GIVE CONSENT: ADULTS ...... 2.12
A. Adults With Capacity to Make Health
Care Decisions
.............................................2.12
“Adult” Defined ...............................................2.12
“Capacity” Defined
..........................................2.12
Determination of Capacity
............................... 2.12
Documentation
...............................................2.13
Special Circumstances Involving Adults
With Capacity
.................................................2.13
B. Adults Who Have Appointed an
Agent or Surrogate
......................................2.14
Psychiatric Advance Directives ........................ 2.14

Chapter 2 — Contents
CHA Mental Health Law Manual 2019
©CALIFORNIA HOSPITAL ASSOCIATION
C. Adults Under Conservatorship ...................2.15
Caution: Type of Conservatorship .................... 2.15
LPS Conservatorship
......................................2.15
Probate Code Conservatorship
.......................2.15
D. Adults Lacking Capacity and Not
Under a Conservatorship
............................2.17
General Rule ...................................................2.17
Unrepresented Patients in Skilled Nursing
Facilities
.........................................................2.18
Unrepresented Patients in Acute Care
Facilities
..........................................................2.19
Court Order Authorizing Medical Treatment
.....2.20
Temporary or Permanent Conservatorship
.......2.22
Petition for Appointment of Public Guardian
....2.22
Family Members
.............................................2.22
E. Summary of Consent Requirements
Regarding Adults .........................................2.24
VII. WHO MAY GIVE CONSENT: MINORS ........ 2.24
A. Introduction..................................................2.24
B. The Evolution of the Rights of Minors .......2.24
C. Financial Responsibility for Treatment
of Minors
......................................................2.25
D. Privacy Rights of Minors ............................. 2.25
E. Minor’s Disagreement with Parent or
Other Legal Representative Regarding
Treatment
.....................................................2.25
Minor’s Age, Maturity, and Experience With
the Treatment in Question
..............................2.26
Disagreement Regarding the Treatment
Decision
........................................................2.26
F. Where Refusal of Treatment May
Cause Serious Harm to the Minor
..............2.26
Refusal for Religious Reasons .........................2.26
Court Intervention
...........................................2.27
VIII. MINORS LACKING LEGAL AUTHORITY
TO CONSENT ...................................... 2.27
A. Parental Consent for Treatment of
Minors
...........................................................2.27
Minors with Married Parents ............................2.27
Minors with Divorced Parents
..........................2.27
Minors with Stepparents
.................................2.28
Adopted Minors
.............................................. 2.28
Minors Born out of Wedlock
............................2.28
Minors with a Registered Domestic Partner
Parent(s)
......................................................... 2.28
Other Situations Involving Nonbiological
Parents or Multiple Parents
.............................2.29
B. Guardian Consent for Treatment of
Minors
...........................................................2.29
Nonsurgical Treatment ....................................2.29
Surgical Treatment
.......................................... 2.29
Limitations on a Guardian’s Consent
...............2.29
C. Third-Party Consent for Treatment of
Minors
...........................................................2.30
The Caregiver’s Authorization Affidavit .............2.30
Other Third-Party Consent
..............................2.30
D. Special Situations Involving Minors
Lacking Legal Authority to Consent
..........2.32
Minors Placed for Adoption .............................2.32
Children of Minor Parents
................................2.32
Minors Who Are Also Parents
..........................2.32
Minors Who Are Ill or Injured During School
Hours
.............................................................2.32
Nonabandoned Minors Whose Parents Are
Unavailable
..................................................... 2.32
Court Authorization: Minors 16 Years of Age
or Older
......................................................... 2.33
Abandoned Minors
.........................................2.33
Dependents and Wards of the Juvenile Court
.. 2.33
Minors in Custody of a Social Worker or
Probation Officer
.............................................2.34
Minors in Custody of Foster Parents
................2.34
Minors Who Are Suspected Victims of Child
Abuse
.............................................................2.35
Minors Receiving Medication Assisted
Treatment for Opioid Use Disorders
.................2.35
E. Minor’s Disagreement with Parent or
Other Legal Representative Regarding
Treatment
.....................................................2.36
Minor’s Age, Maturity, and Experience
With the Treatment in Question
......................2.36
Disagreement Regarding the Treatment
Decision
........................................................2.36
IX. MINORS WITH LEGAL AUTHORITY TO
CONSENT .............................................. 2.36
A. Introduction..................................................2.36
B. Capacity to Consent .................................... 2.37
C. Emancipation Pursuant to Court Order ..... 2.37
D. Self-Sufficient Minors .................................2.38
Definitions ...................................................... 2.38
Documentation
...............................................2.38
Notifying Parent/Guardian
...............................2.38
E. Minors on Active Duty with U.S. Armed
Forces ...........................................................2.38
F. Married or Previously Married Minors .......2.39

Chapter 2 — Contents
Chapter 2 — Principles of Consent for Mental Health Patients CHA
©CALIFORNIA HOSPITAL ASSOCIATION
FORMS & APPENDICES
1-1
S
Consent to Surgery or Special Procedure
1-2
S
Informed Consent to Surgery or Special Procedure
2-1
S
Self-Sufficient Minor Information
2-2
S
Caregiver’s Authorization Affidavit
2-3
S
Authorization for Third Party to Consent to
Treatment of Minor Lacking Capacity to Consent
2-A Consent Requirements for Medical Treatment
of Adults
2-B Consent Requirements for Medical Treatment
of Minors
2-D Health Care Decisions for Unrepresented Patients
2-E Considerations for Revising the Hospital’s
Policy & Procedure Regarding Decision Making
for Unrepresented Patients
4-7
S
Consent to Receive Antipsychotic Medications
8-1
S
Conditions of Admission
23-1
S
Consent for the HIV Test
Forms and Appendices can be found at the back of the manual and
online for CHA members at www.calhospital.org/free-resources.
“S” denotes that the form is provided in English and Spanish.
G. Minors in Need of Outpatient Mental
Health Treatment or Residential Shelter
Services
........................................................2.39
Definitions .......................................................2.39
Parental Involvement/Liability
..........................2.39
Privacy Implications
........................................2.40
Limitations
...................................................... 2.40
H. Minors with Drug- or Alcohol-Related
Problems ......................................................2.40
I. Minors Consenting to Other Procedures ..2.41
Minors Receiving Pregnancy or
Contraceptive Care
......................................... 2.41
Communicable Reportable Diseases
............... 2.41
Minor Rape Victims
.........................................2.41
Minor Victims of Sexual Assault
.......................2.41
Minor Victims of Intimate Partner Violence
.......2.42
J. Summary of Consent Requirements
Regarding Minors ........................................2.42
X. TREATMENTS THAT REQUIRE SPECIAL
CONSENT .............................................. 2.42
A. Background ..................................................2.42
B. Antipsychotic Medications .........................2.42
Voluntary Patients ........................................... 2.43
Involuntary Patients
.........................................2.44
Minors in Custody of the Juvenile
Court/Foster Children
......................................2.47
C. Psychosurgery .............................................2.47
Conditions Under Which Psychosurgery
May Be Performed
..........................................2.47
Documentation of Refusal of Psychosurgery
...2.49
Reports of Psychosurgery
...............................2.49
D. Convulsive Therapy and Insulin Coma
Treatment .....................................................2.49
Definitions .......................................................2.49
Involuntary Adult Patients
................................2.49
Voluntary Adult Patients
..................................2.51
Minors Under the Age of 12
............................2.52
Minors Between 12 and 16 Years of Age
.........2.52
Minors 16 and 17 Years of Age
.......................2.52
Committee Review of Treatment
......................2.52
Reports to Local Behavioral Health Director
....2.52
Excessive Use of Convulsive Treatment
........... 2.53
Local Regulation of Convulsive Treatment
Void
................................................................2.53
E. Mandatory Consultation — Outpatient
and Discharge Medications
........................2.53
Discharge Medications ....................................2.53
Outpatient Medications
................................... 2.53
Patient Declines or is Unavailable
....................2.54
Drug Substitutions
..........................................2.54
F. Telemedicine/Telehealth .............................2.54
Consent Required ........................................... 2.54
Additional Requirements for Medi-Cal
Patients
..........................................................2.54
Definitions
.......................................................2.54
G. Consent for HIV Testing ..............................2.55
Required Information .......................................2.55
Informed Consent
........................................... 2.55
Documenting Refusals
....................................2.56
Minors 12 and Older
.......................................2.56
Adults Lacking Capacity and Minors
Under 12
........................................................2.56
Foster Child/Dependent Child of the
Court/Infant in Temporary Custody
..................2.57
Deceased Patient
...........................................2.57
Occupational Exposures
.................................2.57
Criminal Defendants and Inmates of
Correctional Institutions
...................................2.57
Exceptions: When Informed Consent is
Not Required
..................................................2.58
Informing the Patient of Test Results
...............2.59

2 Principles of Consent for Mental
Health Patients
2.1
©CALIFORNIA HOSPITAL ASSOCIATION
I. INTRODUCTION
State and federal laws grant patients certain rights.
Foremost among these is the right for a competent adult
to make his or her health care decisions. A patient does
not lose this right solely because he or she has been
diagnosed with a psychiatric disorder. (See “Required
Statement of California Law,” page4.3.) This chapter
discusses the basic principles of consent, including when
consent is necessary, the difference between “simple”
consent and informed consent, how consent may be
obtained, who may give consent and procedures that
require special consent. (See CHA’s Consent Manual for a
more detailed discussion of these topics with respect to
nonmental health patients.)
II. WHY CONSENT IS NECESSARY
Every competent adult has the fundamental right of
self-determination over his or her body and property.
Individuals who are unable to exercise their rights, such
as minors and incapacitated adults, have the right to
be represented by another person who will protect their
interests and preserve their basic rights. In some cases,
such as involuntary mental health treatment, the law
determines when and how a person will be treated rather
than requiring or permitting a surrogate decision maker to
do so. However, involuntarily hospitalized mental health
patients retain the right to consent to (or refuse) other types
of medical care, unless a judge orders otherwise.
A. The Patient’s Right to Consent to, or Refuse,
Medical Treatment
A person does not give up the right to control what is done
with his or her body and property when seeking care at a
hospital or from a doctor or therapist. Indeed, a physician
has both a legal and an ethical duty to obtain the patient’s
consent, or the consent of the patient’s legal representative,
to medical treatment.
Failure to obtain the proper consent to treatment in
accordance with applicable legal standards may result in
a charge of battery, professional negligence (malpractice),
and/or unprofessional conduct against the physician,
nurses or other health care providers, for even the simplest
of procedures.
If the nature of the treatment involved is complicated, such
that the average layperson would not understand it, or its
risks and benefits (for example, ECT), the recognition of
the patient’s right to self-determination may require that
“informed” consent be obtained. [Cobbs v. Grant, 8 Cal.3d
229 (1972)] The distinction between “simple” consent
and “informed” consent is described in IV.“Informed
Consent,” page2.5. In such a case, the physician must
explain the nature of the treatment, the risks, possible
complications, and expected benefits or effects of the
treatment, as well as the alternatives to the treatment and
their risks and benefits. The physician must also inform
the patient of any potentially conflicting interests he or
she may have, such as research or financial interests.
Informed consent is not required for the performance
of “simple and common” procedures, where the related
risks are commonly understood — for example, typical
outpatient psychotherapy.
FAILURE TO OBTAIN CONSENT: BATTERY
“Battery” is defined legally as an intentional touching of a
person in a harmful or offensive manner without his or her
consent. Consequently, a claim of battery may be made
against a physician or other health care provider who
performs a medical procedure on a patient without the
patient’s consent. A battery may also arise if the patient
consents to a particular procedure and the provider either
exceeds the scope of the consent or performs a different
procedure for which consent was not obtained. It is
important to note that no wrongful intent need be present;
a physician may sincerely intend to aid the patient, but still
be liable for committing a battery. A medical procedure may
be considered to be a “harmful touching” (a battery) even if
it is performed competently with no adverse outcome.

CHA Mental Health Law Manual 2019
2.2
©CALIFORNIA HOSPITAL ASSOCIATION
FAILURE TO OBTAIN INFORMED CONSENT:
MALPRACTICE
A patient’s right to decide whether or not to submit
to medical treatment establishes the physician’s
corresponding duty to inform the patient about the
recommended care so that the patient’s decision is
meaningful. The physician’s duty of disclosure arises from
the fiduciary quality of the physician-patient relationship,
which is based upon the patient’s dependence on the
physician’s specialized knowledge. [Cobbs v. Grant, supra,
at 242]
A physician who fails to adequately disclose the nature
of the procedure and its risks and alternatives may be
liable for negligence (malpractice). In Cobbs v. Grant, the
California Supreme Court established guidelines regarding
the physician’s duty of disclosure that are explained
at length in IV.“Informed Consent,” page2.5. If the
recommended treatment involves the performance of
a “complicated” procedure, a physician must explain the
nature of the treatment, the risks, possible complications,
and expected benefits or effects of the treatment, as well
as the alternatives to the treatment and their risks and
benefits. The physician must also inform the patient of any
potentially conflicting interests he or she may have, such
as research or financial interests. Informed consent is not
required for the performance of “simple and common”
procedures, where the related risks are commonly
understood. Examples of simple and common procedures
include routine blood tests or chest X-rays.
INFORMED REFUSAL
The California Supreme Court has specifically ruled
that the physician’s duty of disclosure includes the
responsibility to inform the patient of the risks of refusing to
undergo a simple and common procedure that has been
recommended [Truman v. Thomas, 27 Cal.3d 285 (1980)].
In the Truman case, the court held that the defendant
doctor breached his duty to his patient by failing to inform
her of the risks resulting from her failure to authorize and
undergo a Pap smear test. The court stated:
If a patient indicates that he or she is going to decline
a risk free test or treatment, then the doctor has
the additional duty of advising of all material risks of
which a reasonable person would want to be informed
before deciding not to undergo the procedure … If
the recommended test or treatment is itself risky,
the physician should always explain the potential
consequences of declining to follow the recommended
course of action. [Id. at 292]
Consequently, depending upon the type of procedure
involved, a physician may be liable for professional
negligence (malpractice) if he or she fails to obtain the
patient’s “informed refusal.”
B. The Patient’s Right to Consent to Hospital
Services
The patient’s personal and property rights may also be
affected by certain activities conducted by the hospital
and its personnel (as distinct from activities conducted by
the physician). Although a hospital is not subject to the
physician’s fiduciary duty to the patient and is not directly
responsible for obtaining the patient’s informed consent
to medical treatment, the hospital is responsible for the
care of its patients and for obtaining their consent, or the
consent of their legal representatives, to those hospital
activities which, without such consent, would impinge on
patients’ rights. Examples of hospital activities that require
consent (although not necessarily informed consent)
include routine blood tests, chest X-rays and nursing
services. Consent to these activities is included in the
model “Conditions of Admission” form (CHA Form 8-1).
A hospital’s failure to obtain a patient’s consent may raise
allegations of battery, false imprisonment, and possibly
other charges.
In summary, the patient’s consent to medical treatment and
hospital services is necessary because, as a general rule,
without such consent, the physician and the hospital have
no authority to subject the patient to medical treatment
or hospitalization and related services. One notable
exception to this general rule involves patients who are a
danger to themselves or others or gravely disabled. The
laws applicable to such persons are discussed in detail in
chapter 3.
III. WHEN CONSENT IS NECESSARY
The general rules for determining when consent is required
are presented below. Subsequent chapters address
the requirements that apply in specific situations. The
exceptions to the general rule are described below.
(See also chapter 3 regarding involuntary mental health
evaluation and treatment.)
A. General Rule
The hospital may not permit any treatment, without the
risk of liability, unless the patient, or a person legally
authorized to act on the patient’s behalf, has consented to

Chapter 2 — Principles of Consent for Mental Health Patients CHA
2.3
©CALIFORNIA HOSPITAL ASSOCIATION
the treatment. The consent may be simple or informed (see
B.“Identifying Procedures That Require Informed Consent,”
page2.6). The exceptions to this general rule are
described below. (See also chapter 3 regarding involuntary
mental health evaluation and treatment.)
B. Emergency Treatment Exception
STATEMENT OF PRINCIPLE
Treatment of a medical emergency may be provided without
consent where the provider reasonably believes that a
medical procedure should be undertaken immediately, and
that there is insufficient time to obtain the consent of the
patient or of a person authorized to consent for the patient.
The law implies consent in these circumstances on the
theory that if the patient were able, or if a qualified legal
representative were present, the consent would be given.
This exception applies to minors as well as to adult patients.
The location of the patient is not relevant to the
determination of whether the patient has a medical
emergency. A patient may be in the emergency department,
yet may not have a medical emergency that obviates the
necessity to obtain consent. Similarly, the patient may be
located in a medical/surgical unit or outpatient department
and develop a medical emergency that requires treatment
to be provided without consent.
California law defines a medical emergency for certain
purposes, such as the provision of immunity to physicians
who provide treatment in emergency situations, the
rendering of care to incompetent adults without court
authorization, and the rendering of care to minors in
custody of the juvenile court. According to these laws, a
medical emergency exists when:
1. Immediate services are required for the alleviation of
severe pain; or
2. Immediate diagnosis and treatment of unforeseeable
medical conditions are required, if such conditions
would lead to serious disability or death if not
immediately diagnosed and treated.
[Business and Professions Code Section 2397(c)(2) and
(3); Probate Code Section 3210(b); Welfare and Institutions
Code Sections 369(d)]
LIMITATIONS
It is important to note that only the emergency condition
may be treated. Treatment that exceeds the necessary
response to the emergency condition may not be rendered
without consent from someone authorized to consent to
treatment on a nonemergency basis.
As a general rule, if a patient or the patient’s legal
representative has validly exercised his or her right to
refuse particular medical treatment, the treatment may not
be provided. Since the emergency treatment exception is
based on the theory of implied consent, it does not apply
when a patient has validly refused medical treatment, and
the emergency arises from the fact that treatment was
not given. However, if the medical emergency is the result
of a condition or injury that is not specifically related to
the condition or injury for which the patient previously
refused treatment, the emergency treatment exception
generally applies.
If evidence exists to indicate that the patient (or the
patient’s legal representative) would refuse the treatment —
such as a wallet card stating that the patient is a Jehovah’s
Witness and refuses blood products — legal counsel
should be consulted.
RECOMMENDED PROCEDURE FOR PROVIDING
CARE PURSUANT TO THE EMERGENCY MEDICAL
TREATMENT EXCEPTION
Determination of Existence and Nature of Emergency
The physician must initially determine whether the patient
has the capacity to give consent, since the emergency
exception applies only when consent cannot be given. In
addition, the scope of the emergency must be determined,
and any treatment provided must be limited to that
necessary to alleviate the severe pain, or to prevent the
patient’s severe disability or death. The treatment provided
may be a matter of first aid, temporary medical care in lieu
of surgery, or actual surgical procedures. However, only
the emergency medical condition may be treated under
this exception.
Consultation
There is no legal requirement that the physician consult a
second physician to confirm the existence of an emergency.
However, such consultation may be required by hospital
or medical staff policy, if desired. Otherwise, the treating
physician has discretion to determine if consultation is
advisable to confirm the existence of the emergency.
Otherwise Obtaining Consent
The possibility of obtaining consent from the patient, if he
or she is able to give consent (e.g., a conscious adult with
capacity), or another person legally capable of consenting,

CHA Mental Health Law Manual 2019
2.4
©CALIFORNIA HOSPITAL ASSOCIATION
should be assessed and weighed against the possibility
that a delay in treatment to obtain consent would result in
the patient’s severe disability, death or continuing severe
pain. If a delay in treatment for purposes of obtaining
consent would not jeopardize the condition of the patient,
treatment must be delayed and consent obtained pursuant
to the guidelines contained in this manual.
Documentation in the Medical Record
The physician should document his or her determination
that an emergency exists (e.g., “The immediate
treatment of the patient is necessary because ...”). The
physician does not sign a consent form on behalf of the
patient. Consent is implied by law from the existence of
the emergency.
If the physician has obtained a consultation, the consulting
physician should similarly document his or her findings and
opinion in the patient’s medical record.
IMMUNITY FROM LIABILITY
The emergency treatment exception has been recognized
in several statutes that provide immunity to a physician who
does not inform a patient and obtain his or her consent
to treatment under certain emergency circumstances.
Business and Professions Code Section 2397 provides
that a physician is not liable for civil damages for injury
or death caused in an emergency situation occurring in
his or her office or in a hospital on account of a failure to
inform a patient of the possible consequences of a medical
procedure where the failure to inform is caused by any of
the following:
1. The patient was unconscious.
2. The medical procedure was undertaken without
the consent of the patient because the physician
reasonably believed that a medical procedure should
be undertaken immediately and that there was
insufficient time to fully inform the patient.
3. A medical procedure was performed on a person
legally incapable of giving consent, and the physician
reasonably believed that a medical procedure should
be undertaken immediately and that there was
insufficient time to obtain the informed consent of a
person authorized to give such consent for the patient.
This law applies only to lawsuits for injuries arising because
of a physician’s failure to inform, not to actions for a
physician’s negligence in rendering or failing to render
treatment. Business and Professions Code Section 1627.7
provides similar protections for dentists.
In addition, Health and Safety Code Section 1317 provides
immunity from liability for an act or omission (which
includes the failure to obtain consent) that occurs while
a rescue team established by a licensed health facility or
government entity attempts to resuscitate a person who is
in immediate danger of death or serious injury or illness, if
the rescue team acts in good faith. This immunity extends
to the facility, its officers, staff, and employees.
C. Other Circumstances in Which a Physician is
Not Required to Obtain Informed Consent
CIRCUMSTANCES
In Cobbs v. Grant, the court noted two special
circumstances in which a physician is not required to
disclose all of the information that is required to obtain the
patient’s informed consent.
First, the court indicated that a physician need not disclose
the risks of the recommended treatment when the patient
has requested that he or she not be so informed.
Second, a physician is not required to disclose information
to the patient if such disclosure would seriously harm,
rather than benefit, the patient. In this regard, the
court explained:
A disclosure need not be made beyond that required
within the medical community when a doctor can
prove by a preponderance of the evidence [that the
doctor] relied upon facts which would demonstrate to
a reasonable [person that] the disclosure would have
so seriously upset the patient that the patient would
not have been able to dispassionately weigh the risks
of refusing to undergo the recommended treatment.
[Cobbs v. Grant, 8 Cal.3d at 245-246]
This second exception to the physician’s duty of disclosure
is commonly known as the “therapeutic privilege.”
Neither exception should be relied upon by the physician
unless it is extremely clear that the facts and circumstances
of the case justify invoking it. The court stated that these
two exceptions constitute situations in which a physician
who fails to make the disclosure required by law may
defend his or her actions, and specified that any such
defense “must be consistent with what has been termed
the ‘fiducial qualities’ of the physician-patient relationship.”
The physician’s decision to not disclose information will
be measured in terms of what “a reasonable person”
would have done, not what another physician would have
done. Also, the court’s discussion about the exceptions
generally referred to the disclosure of information about
the potential risks of the recommended procedure and did

Chapter 2 — Principles of Consent for Mental Health Patients CHA
2.5
©CALIFORNIA HOSPITAL ASSOCIATION
not specifically state that a physician may be justified in not
disclosing other information, such as that pertaining to the
diagnosis, the nature of the recommended treatment, its
expected benefits or effects, alternatives and any potentially
conflicting interests of the physician (such as research or
financial interests).
The use of these two exceptions should be very rare in
the case of adult patients who have the capacity to make
health care decisions. It is not clear that either exception
is available in the case of a patient who lacks the legal
authority to consent to his/her own care or the capacity
to make a health care decision. If the parent, guardian, or
other legal representative who ordinarily would make health
care decisions for a minor or patient who lacks capacity
requests not to be given certain information, or is not able
to emotionally handle the information, legal counsel should
be consulted. In such situations, it should be determined
whether a different decision maker would be appropriate.
PROCEDURE
If the physician determines that the patient specifically
asked to not receive information about the proposed
procedure or treatment, or that the “therapeutic privilege”
applies, the physician should fully document in the
patient’s medical record the facts that resulted in this
conclusion. The physician should also document what, if
any, information was disclosed to the patient. It may be
appropriate for the physician to discuss the information that
was not disclosed to the patient with the patient’s closest
available relative (if the patient consents to the release
of medical information to, and the involvement of, the
relative) and secure that person’s approval for proceeding
with the procedure in view of this full disclosure. The
physician should document in the patient’s medical record
the nature and results of any such consultation with the
patient’s family.
The hospital’s role is to verify, by checking the
documentation in the medical record, that the physician’s
failure to disclose information resulted from a determination
that one of the two exceptions applied. The hospital may
wish to refer such cases to hospital administration or risk
management for review prior to beginning the procedure.
D. Exceptions for Minors
Consent is not required in very limited situations involving
minors who are suspected victims of child abuse or
who become sick or injured at school. (See D.“Special
Situations Involving Minors Lacking Legal Authority to
Consent,” page2.32 for further information.)
IV. INFORMED CONSENT
A. Elements of Informed Consent
As discussed above, the California Supreme Court held in
Cobbs v. Grant, that a patient must give “informed consent”
prior to certain medical treatment. The court stated that
in order to give informed consent, the patient must be
informed of:
1. The nature of the procedure;
2. The risks, complications, and expected benefits or
effects of the procedure;
3. Any alternatives to the treatment and their risks
and benefits.
In addition, a later court held that the patient must also be
informed of any potentially conflicting interest the physician
may have (such as research or financial interests).
The Cobbs court explained that:
The scope of the physician’s communications to the
patient, then, must be measured by the patient’s need,
and that need is whatever information is material to
the decision. Thus the test for determining whether a
potential peril must be divulged is its materiality to the
patient’s decision. [Cobbs v. Grant, supra, 8 Cal.3d
229, 245]
In a subsequent case, the court clarified its definition of
“material information” as follows:
[T]hat which the physician knows or should know would
be regarded as significant by a reasonable person in the
patient’s position when deciding to accept or reject the
recommended procedure…To be material, a fact must
also be one that is not commonly appreciated. . . . If the
physician knows or should know of a patient’s unique
concern or lack of familiarity with medical procedures,
this may expand the scope of required disclosure.
[Truman v. Thomas, 27 Cal.3d 285, 291 (1980)]
The Centers for Medicare & Medicaid Services (CMS)
Conditions of Participation (CoP) Interpretive Guidelines
(Tag A-0466) state that material risks could include risks
with a high degree of likelihood but a low degree of severity,
as well as those with a very low degree of likelihood but
high degree of severity. The Interpretive Guidelines also
state that hospitals are free to delegate to the responsible
practitioner (the physician, podiatrist or dentist) who
uses the available clinical evidence as informed by the
practitioner’s professional judgment, the determination
of which material risks, benefits and alternatives will be
discussed with the patient. The Interpretive Guidelines can
be found at www.cms.gov/Regulations-and-Guidance/
Guidance/Manuals/Internet-Only-Manuals-IOMs.html,

CHA Mental Health Law Manual 2019
2.6
©CALIFORNIA HOSPITAL ASSOCIATION
then Publication 100-07 State Operations Manual, then
“Appendices Table of Contents.” The State Operations
Manual has several appendices that apply to hospitals,
for example, A (hospitals), AA (psychiatric hospitals), V
(EMTALA), and W (critical access hospitals).
For some procedures and treatments, the California
legislature has passed laws requiring the physician to give
specified additional information. Some of these treatments
include electroconvulsive therapy, psychosurgery, and
antipsychotic medications. (See X.“Treatments That
Require Special Consent,” page2.42.)
A physician is not required to inform a patient about
treatment that cannot legally be administered in California
[Schiff v. Prados, 92 Cal.App.4th 692 (2001)]. A physician
must inform a patient about alternative treatments only
to the extent required for competent practice within the
medical community. [Vandi v. Permanente Medical Group,
7 Cal.App.4th 1064 (1992)] For example, a physician need
not discuss coffee enemas with patients.
In certain circumstances the patient’s physician is not
required to disclose all information that would otherwise be
required to be given to the patient to obtain the patient’s
informed consent. (See C.“Other Circumstances in Which
a Physician is Not Required to Obtain Informed Consent,”
page2.4.)
B. Identifying Procedures That Require Informed
Consent
“Informed” consent, as distinguished from “simple”
consent, is not required for all medical treatments. The
Cobbs court held that treatments or procedures that are
“complicated” require that informed consent (as described
above) be obtained. Procedures that are “simple and
common” do not require informed consent (although they
still require consent, usually obtained in the “Conditions
of Admission” form (CHA Form 8-1)). The court stated
that a physician is not expected to explain risks that are
commonly understood to be remote. The performance of
a blood count was cited as an example of a simple and
common procedure.
The determination of which procedures are “complicated”
and, therefore, require informed consent, is medical in
nature. It is the position of CMS that medical staff policies
should address which procedures and treatments require
written informed consent. (See Hospital Interpretive
Guidelines, Tag A-0466.) The medical staff bylaws
themselves would not seem to be the best place for this
information. The rules and regulations or a policy and
procedure would seem to be better choices. However it is
done, it should be appropriately documented and approved
by the medical staff executive committee. Procedures for
which the law specifically requires informed consent should
also be included (see X.“Treatments That Require Special
Consent,” page2.42). To determine whether a procedure
is “simple and common” or “complicated,” the medical
staff should consider whether the average layperson would
understand the nature of the procedure and its risks and
benefits.
C. The Role of the Physician in Obtaining
Informed Consent
It is the physician’s responsibility to determine the patient’s
capacity and to obtain informed consent. Generally, the
physician who performs the procedure is responsible
for obtaining the patient’s consent. If a nonphysician will
perform the procedure, then the ordering physician is
responsible for obtaining consent. If more than one doctor
is involved, they can determine together which one will
obtain consent, or hospital policy may determine which
physician will obtain consent. Hospital personnel should
not be involved in providing the information necessary to
secure the patient’s informed consent or responding to the
patient’s questions concerning the procedure. The duty
to provide this information and obtain informed consent
is the exclusive duty of the physician. Nurses and other
hospital personnel may provide general patient or family
education, however.
PROCESS BY WHICH PHYSICIAN INFORMS PATIENT
Physicians may use verbal discussion, written information,
audio and video recordings to give the patient the
information to the patient or legal representative necessary
to obtain informed consent.
The physician should also always give the patient a
personal explanation of the procedure or treatment, its
possible complications, risks and alternatives. This verbal
discussion gives the patient the opportunity (as required
by the legal doctrine of informed consent) to ask questions
about the information presented by the physician. A
patient’s consent given after a discussion with the physician
and the opportunity for inquiry is more likely to be truly
“informed.”
Written or Recorded Patient Information
Written handouts and audiovisual recordings may play
an important part in the informed consent process since
they give the patient the information in a form that may be
reviewed later. However, the use of the hospital’s name or

Chapter 2 — Principles of Consent for Mental Health Patients CHA
2.7
©CALIFORNIA HOSPITAL ASSOCIATION
the distribution of information by hospital personnel might
cause a patient to conclude that the hospital employs
the physician and/or is responsible for the physician’s
provision of medical services, including the physician’s
duty to provide the patient with information about the
procedure. Thus, any written information sheets, audio or
video recordings, etc. that contain medical information that
a physician is responsible for giving to a patient to obtain
informed consent should be designated as the physician’s
information. If the information contains the hospital’s
name, or hospital personnel are involved in distributing the
information, describing the procedure to the patient, or
responding to the patient’s questions about the procedure
or the information, this could suggest that the physician is
a hospital agent or otherwise confuse a patient regarding
the legal responsibility for obtaining informed consent. For
these reasons, involvement by the hospital or its staff is
discouraged.
If a hospital chooses to distribute such information or put
the hospital’s name on information sheets, etc., it should be
clearly noted that the form or information is being provided
by the hospital as a courtesy and that the patient should
review the information with his or her physician. It should
also clearly state that the physician is not the employee or
agent of the hospital (if that is the case).
INFORMED CONSENT FORMS THAT CONTAIN MEDICAL
INFORMATION
Some physicians prefer to give patients an “informed
consent” form that contains within it the medical
information the patient must be provided. This procedure
promotes complete disclosure and allows patients to
study the information. While such forms should not be
prepared or distributed by hospital personnel for the
reasons discussed above, forms may be used by hospitals
to verify and document that informed consent was given by
each patient.
A physician who prepares an informed consent form
that contains the medical information which must be
provided to the patient may use as a guide the “Informed
Consent to Surgery or Special Procedure” form (CHA
Form 1-2). The physician should include the name of the
procedure(s), nature of the treatment, its expected benefits
or effects, its possible risks and complications, and any
alternatives to the proposed treatment and their possible
risks and complications. The physician should also include
any potentially conflicting interests, such as research or
financial interests.
It is often not possible to include all information relevant
to a particular patient’s condition on a written form.
Accordingly, the form must either be supplemented through
verbal discussions with the patient and/or by written
additions containing the information. For example, the
risks of a treatment will differ depending upon whether the
patient is a young, healthy person; a pregnant woman; or
an elderly, brittle diabetic. A standardized list of risks may
be used, but must be supplemented with any additional
information pertinent to the particular patient.
Written forms are helpful only if they are understood by
the patient. Therefore, it is important that the medical
information included in the forms be written in clear,
simple, and easily understood terms. In addition, the forms
should clearly state that the patient should ask any and all
questions he or she may have concerning the proposed
treatment.
Also, some forms may ask patients to respond to
questions such as: “Have you been given all the
information you desire about the proposed treatment?”
or “Do you understand the nature of the proposed
treatment, its expected benefits and the possible risks
and complications?” However, if this type of question is
included in a consent form, the physician must verify it has
been answered affirmatively on the form; otherwise, the
patient will have established in the document that he or
she did not give informed consent. The format provided
in CHA Form 1-2 does not include such questions; rather,
it requires the patient to acknowledge receipt of the
relevant information.
PHYSICIAN DOCUMENTATION
It is recommended that the physician carefully document
in the hospital medical record that a discussion was held
with the patient and that informed consent was obtained.
This documentation can be accomplished in a variety of
ways — through a certification on the consent form itself
(see the certifications on the“Consent to Surgery or Special
Procedure” form (CHA Form 1-1)), through a progress
note in the patient’s record, through a note in the patient’s
history and physical, or through documentation provided
from the physician’s office (e.g., an informed consent
form signed by both the patient and the physician). The
physician should also place in the medical record a copy
of any written material provided to the patient. Any special
circumstances should also be documented.

CHA Mental Health Law Manual 2019
2.8
©CALIFORNIA HOSPITAL ASSOCIATION
D. The Role of the Hospital in the Informed
Consent Process
VERIFICATION THAT INFORMED CONSENT HAS BEEN
OBTAINED
The hospital’s role in the consent process should be
limited to verifying that the physician obtained and properly
documented the patient’s informed consent before the
physician is permitted to perform the medical procedure.
The physician, not the hospital, has the duty to disclose all
information relevant to the patient’s decision and to obtain
the patient’s informed consent.
Obtaining informed consent involves the practice of
medicine, in which the hospital and its employees should
not intervene. Hospital employees are not licensed
or qualified to adequately explain the various types of
medical procedures to the patient, why the physician has
recommended a particular procedure over another, and
to respond to the patient’s potential questions. Only the
physician has both the technical medical knowledge and
the knowledge of the particular patient’s history and current
condition necessary to assure that an adequate disclosure
of information, including information about the risks of
treatment, has been given to the patient and that proper
responses have been given to the patient’s questions.
Although hospital personnel should not be responsible for
securing the patient’s informed consent (or for providing
the information required to secure the patient’s informed
consent), it is foreseeable that a patient may ask questions
of hospital employees who perform a procedure pursuant
to the doctor’s orders. Hospital personnel generally may
answer such questions. However, if it appears that the
patient has significant questions about the nature of the
procedure, its benefits or risks which indicate that the
patient may not have been given sufficient information
about the procedure or did not understand the information,
hospital personnel should contact the patient’s physician
to allow him or her to assure that the patient indeed gave
informed consent to the procedure.
OBTAINING VERIFICATION
The form “Consent to Surgery or Special Procedure” (CHA
Form 1-1) or a similar form should be used after informed
consent is given by the patient to the physician. This form
serves the dual purposes of:
1. Assuring that the physician obtained informed consent
from the patient for the contemplated procedure, and
2. Documenting that the patient is aware of the right
to give informed consent or refusal to the procedure
recommended by the physician.
By signing this form, the patient acknowledges that the
physician adequately explained the procedure to the
patient and gave the patient all the information he or she
desired. This form does not list the risks of the procedure
nor alternative therapies; thus, if this form is used by the
hospital, an additional form, prepared by the physician,
which lists the risks and alternatives (signed by the
patient and the physician) must also be included in the
medical record.
NOTE: The form itself is not informed consent; it is
evidence for both the hospital and the physician that
informed consent was obtained. The form is not a
substitute for the critical role of the attending physician in
the informed consent process.
RECOMMENDED PROCEDURE FOR COMPLETING THE
HOSPITAL’S FORM
The consent form should include the name of the patient,
and when appropriate, the patient’s legal representative.
Identification of the Procedure or Treatment
The medical terminology for the procedure and the type
of anesthesia to be used (if applicable) should be entered
into the space provided on the form. In addition, it is
recommended that a description of the procedure or
treatment in lay terminology be entered in the space along
with the medical terminology to provide a more meaningful
description of the procedure.
If lay terminology is used, there should be consistency
within an institution in describing such procedures. The
medical staff and nursing staff may want to establish
a glossary of lay terms corresponding to the medical
terminology for procedures performed in the facility.
Identification of the Practitioner(s)
In the Hospital Interpretive Guidelines, CMS states that
the consent form include the name of the practitioner
performing the procedure or administering the treatment.
The Guidelines also recommend, but do not require, that
the form state, if applicable, that:
1. Physicians other than the operating practitioner,
including but not limited to residents, will perform
important tasks related to the surgery, in accordance
with the hospital’s policies (and, in the case of
residents, based on their skill set and under the
supervision of the responsible practitioner); and
2. Qualified medical practitioners who are not physicians
will perform important parts of the surgery or
administration of anesthesia within their scope of

Chapter 2 — Principles of Consent for Mental Health Patients CHA
2.9
©CALIFORNIA HOSPITAL ASSOCIATION
practice, as determined under state law and regulation,
and for which they have been granted privileges by the
hospital. (See Hospital Interpretive Guidelines, Tags
A-0466 and A-0955.)
This supersedes CMS’ previous position that informed
consent forms must state the names of practitioners other
than the primary surgeon who will perform important
aspects of the surgical procedure.
Medical Information
The Hospital Interpretive Guidelines require that informed
consent forms include a statement that the procedure or
treatment, including the anticipated benefits, material risks,
and alternative therapies, was explained to the patient
or the patient’s legal representative. The Guidelines also
recommend, but do not require, that the form include
an indication or list of the material risks of the procedure
or treatment that were discussed with the patient or the
patient’s legal representative. (See Hospital Interpretive
Guidelines, Tag A-0466.) This reverses CMS’ previous
position that the form itself must include all information
about the procedure or treatment and its alternatives.
PROCEDURE WHEN PHYSICIAN USES INFORMED
CONSENT FORMS THAT CONTAIN MEDICAL
INFORMATION
Review and Approval of Forms
Before a form is relied upon by the hospital as evidence
that the physician secured the patient’s informed consent,
the hospital may wish to review it to see that it contains all
the information that must be provided to the patient.
When the physician uses an informed consent form that
contains medical information that has been approved by
the hospital and appropriate medical staff committees, the
hospital may verify that the patient gave informed consent
by relying on this form. The hospital should check the
original form signed by the patient to ensure it is complete
and that the patient or the patient’s legal representative
properly completed the document. The original consent
form should be placed in the patient’s medical record. The
patient should be given a copy of the consent form if this
has not already been done.
E. Two-Doctor Consent
A common misconception related to consent law is that
if two doctors agree that a patient would benefit from a
particular procedure or treatment, the two doctors may
consent on behalf of the patient. This is a myth.
There is no provision in California or federal law that permits
two doctors to consent on behalf of a patient. This is true
whether the patient has the capacity to make health care
decisions or not. The patient or a legal representative
must provide consent to medical treatment, except in
an emergency or as otherwise permitted by law. In an
emergency, patient consent is implied by law (see III.“When
Consent is Necessary,” page2.2).
F. Duration of Informed Consent
A patient’s consent to treatment remains effective until the
patient revokes it or until circumstances change so as to
materially affect the nature of, or the risks of, the procedure
and/or the alternatives to the procedure to which the
patient consented.
For example, if a patient has been admitted to a hospital
for a specific course of treatment, or a specific operation,
but in the course of studying the patient several days
elapse and the anticipated treatment or operation changes
considerably, the physician should obtain a new informed
consent. Similarly, if the patient’s condition changes or
new information is learned about the patient’s condition,
resulting in increased or different risks to the patient from
the contemplated procedure or treatment, a new consent
should be obtained.
G. Patient Doubt or Confusion Concerning
Informed Consent
If, when the verification of consent form is presented to the
patient, he or she voluntarily indicates doubt or confusion
about the procedure and consequently the question is
raised whether an informed consent was obtained, the
physician should be contacted immediately. The physician
should obtain the patient’s informed consent (again, if
necessary). Under no circumstances should an employee
of the hospital attempt to obtain the patient’s informed
consent in such a situation.
V. HOW CONSENT SHOULD BE OBTAINED
Obtaining informed consent is a communication process,
not a signature on a paper form. Getting patients to
sign consent forms does not mean they have read them
or that they understand them. While documentation is
important, and often required, the ultimate goal of patient
understanding must also be met.
All requirements regarding translation and interpreter
services must be followed (see E.“Securing Consent When
Communication Barriers Exist,” page2.11).

CHA Mental Health Law Manual 2019
2.10
©CALIFORNIA HOSPITAL ASSOCIATION
A. Capacity to Consent
The patient or legal representative must be conscious and
have the capacity to understand the purpose and effect of
the decision to be made and the form to be signed. It is
the treating physician’s responsibility to determine whether
the patient has this capacity. (See ““Capacity” Defined,”
page2.12.)
B. Consent Must Be Knowingly Made and Freely
Given
To be effective, consent must be made knowingly and given
freely. Consent must not be obtained through the exercise
of duress or coercion.
C. The Nature of Consent
Consent may be express (oral or written statement) or
implied (for example, by voluntary submission to the
procedure or by the existence of a medical emergency).
Express consent should be obtained whenever possible.
D. Consent Evidenced in Writing
The “Conditions of Admission” form contains a clause
that documents the patient’s consent to noncomplicated
procedures such as routine blood tests, X-rays, nursing
and other services that may be performed during the
patient’s hospitalization, outpatient visit, or emergency
room treatment. (See CHA Form 8-1 “Conditions of
Admission.”)
In certain instances, particularly when the patient is
authorizing complicated medical treatment or refusing
recommended care, it is recommended that the patient’s
consent (or refusal) be evidenced in writing. If a dispute
arises as to whether consent was given, proof of consent is
more readily established when it is in writing.
California law requires that consent for some procedures
be documented in writing. These laws are discussed in
X.“Treatments That Require Special Consent,” page2.42.
In addition, Title 22, California Code of Regulations, Section
70223(d)(3) requires that, prior to nonemergency surgery,
the person responsible for administering anesthesia, or
the general surgeon if a general anesthetic will not be
administered, must ascertain that a written informed
consent form for the contemplated surgical procedure
is in the medical record. All necessary consent forms
must be made a part of the medical record. [Title 22,
California Code of Regulations, Sections 70749, 70527(d)
and 71549]
CMS requires each medical staff to review those
procedures that are performed at the facility and identify
which require informed consent. For those procedures
that are identified as requiring informed consent, written
verification that informed consent was given should be
obtained and placed in the patient’s medical record.
[Hospital Interpretive Guidelines, Tag A-0466] The CoP
Interpretive Guidelines state that a properly executed
informed consent form contains the signature of the patient
or the patient’s legal representative [Hospital Interpretive
Guidelines, Tag A-0466].
The Hospital Interpretive Guidelines state that a properly
executed informed consent form contains the signature of
the patient or the patient’s legal representative [Hospital
Interpretive Guidelines, Tag A-0466].
In addition, Title 22, California Code of Regulations, Section
70223(d)(3) requires that, prior to nonemergency surgery,
the person responsible for administering anesthesia, or
the general surgeon if a general anesthetic will not be
administered, must ascertain that a written informed
consent form for the contemplated surgical procedure
is in the medical record. Title 22, California Code of
Regulations, Sections 70749, 70527(d) and 71549 require
that all necessary consent forms be made a part of the
medical record.
RECOMMENDED FORMS
In order to provide written evidence of consent, various
forms have been developed for use by hospitals and
physicians. These forms are included and discussed in this
manual. In addition, as discussed in subsequent chapters,
several statutes and regulations require specific information
to be included in consent forms or require the use of
prescribed forms under certain circumstances. The forms
included in this manual fulfill these requirements.
PRINCIPLES GUIDING COMPLETION OF FORMS
Signature of Person Consenting
The hospital should accept the name given by the patient
unless there are legitimate business reasons to demand a
specific name or a name in a specific form (for example, the
name required by third-party payers).
When a person other than the patient signs a form, the
relationship to the patient (for example, parent, guardian,
conservator) should be noted below the signature, and
a brief statement included as to why the patient cannot
personally sign the form. Hospitals should consider asking
the patient to also sign when able, if the inability to sign
was due to a temporary condition.

Chapter 2 — Principles of Consent for Mental Health Patients CHA
2.11
©CALIFORNIA HOSPITAL ASSOCIATION
If the person who is required to sign is physically unable
to write his or her name, but has mental capacity to make
the decision, the person’s mark should be obtained. This
is done by the hospital representative first writing the
person’s name in full and then having the person place an
“X” beneath it. Two people should witness the signer place
his or her mark on the consent form, and they should sign
the consent form as witnesses.
Patient Declines to Sign Due to Religious Beliefs
Some patients may decline to sign forms on certain days
with religious significance. For example, the Orthodox
Jewish faith proscribes any writing on the Jewish Sabbath
(sundown Friday to sundown Saturday) and recognized
Jewish holidays. The wishes of such patients should
be respected.
In these instances it is important to remember that oral
consent to treatment is, in most cases, as valid as written
consent. Consent forms and acknowledging signatures
merely document consent. However, when a surgical
procedure is involved, California law requires that the
anesthesiologist or surgeon assure that the patient’s
medical record contains informed consent, in writing,
prior to commencing surgery [Title 22, California Code
of Regulations, Section 70223(d)]. When it is possible to
accept the patient’s oral consent, the informed consent
process is the same as when written consent is obtained.
In such cases, the patient should read the relevant
documents and acknowledge the information given.
The patient should then orally consent to or refuse the
recommended treatment. The oral consent should
be documented in the patient’s medical record and
appropriate written documentation obtained from the
patient later, with an appropriate explanation for the date
of the patient’s signature. The following note should be
entered and dated at an appropriate place on each form:
This patient read this document on this date, but
declined to sign it today for religious reasons. The
patient agreed to sign this document tomorrow or as
soon thereafter as his/her religious faith will allow.
This statement should be initialed by a second hospital
employee who witnessed the consent discussion.
Time and Date of Signature
The time and date on the form should be the time and
date the form is signed by the patient or the patient’s legal
representative, not the time and date of the procedure
or operation.
Witnesses
Consent forms need not be notarized. It is recommended
(but not required) that one hospital employee serve as
a witness to the signature by the patient. (However, an
advance health care directive requires two witnesses.)
Unless otherwise indicated, admitting personnel, registered
nurses, licensed vocational nurses, ward clerks, or other
hospital employees of similar responsibility may act as
witnesses to hospital forms. All witnesses should be
18 years of age or over.
Each witness should be present when the form is signed
by the patient or the patient’s legal representative. The
witness need not be present during the discussion between
the patient and the physician about the procedure — the
witness only needs to observe the patient signing the
document. The witness should indicate that he or she
witnessed the signing by placing his or her signature in the
designated space on the form.
Copies of Consent Forms
The original consent form should always be placed in the
patient’s medical record.
In certain circumstances the law requires that a copy of the
consent form be given to the patient. Such requirements
are discussed throughout this manual.
In addition, it is recommended, but not legally required,
that a copy of the facility’s “Conditions of Admission” (CHA
Form 8-1), or other similar document, and a copy of the
“Informed Consent to Surgery or Special Procedure” (CHA
Form 1-2) always be given to the patient.
A copy of any other form signed by the patient should be
given upon request.
E. Securing Consent When Communication
Barriers Exist
If a patient or his or her legal representative cannot
communicate with the physician because of language
or communication barriers, the physician, with the
hospital’s assistance, should arrange for an interpreter.
The interpreter’s responsibilities will include translating the
information regarding the recommended medical treatment
that the patient or the patient’s legal representative needs
to receive before deciding whether to give consent, as well
as instructions regarding medical care.
Similarly, vital documents, including consent forms,
presented by hospital staff to a patient must be written in a
language that the patient can understand or translated into
such a language.

CHA Mental Health Law Manual 2019
2.12
©CALIFORNIA HOSPITAL ASSOCIATION
Both state and federal laws contain detailed requirements
regarding interpreter and translator services. (See CHA’s
Consent Manual, chapter 1, for further information.)
VI. WHO MAY GIVE CONSENT: ADULTS
An adult patient generally has the right to make his or her
own health care decisions. However, in some cases, a
patient’s physical or mental condition may render him
or her unable to consent to medical treatment, either
temporarily or permanently. If the patient lacks “capacity,”
someone else must consent to the treatment on his or her
behalf, except in emergency situations (see B.“Emergency
Treatment Exception,” page2.3).
For purposes of consent for medical treatment, an adult
patient may be in one of the following categories:
1. Adult with capacity.
2. Adult who has appointed an agent or surrogate to
make health care decisions (see chapter 3 of CHA’s
Consent Manual regarding agents and surrogates).
An agent or surrogate may be named in an advance
health care directive or other similar document;
surrogates may be appointed verbally by the patient.
3. Conservatee specifically adjudicated to lack the
capacity to make health care decisions.
4. Conservatee not specifically adjudicated to lack the
capacity to make health care decisions.
5. Adult lacking capacity without a conservator, agent, or
surrogate for health care decisions (whether the patient
temporarily or permanently lacks capacity).
The laws applicable to consent for inpatient mental health
admission and treatment for adults, both voluntary and
involuntary, are found in chapter 3. The laws regarding
involuntary outpatient mental health treatment for adults
are also described in chapter 3. There are no special
requirements regarding voluntary outpatient mental health
treatment. Many mental health patients have concurrent
medical conditions and may need medical treatment
requiring informed consent. This part of the manual
addresses those circumstances.
A. Adults With Capacity to Make Health Care
Decisions
An adult patient with capacity has the right to make
his or her own health care decisions [Probate Code
Section 4670]. This includes consenting to medical
treatment and refusing medical treatment, including
life-sustaining treatment.
“ADULT” DEFINED
For the purpose of making health care decisions, an “adult”
is a person who has reached the age of 18, or a minor who
has entered into a valid marriage or domestic partnership
(whether or not it was later terminated by divorce or death
of the spouse/partner), who is on active duty with the
armed forces of the United States of America, or who
has been declared emancipated pursuant to Family Code
Section 7122 et seq. [Family Code Section 7002]. (See
IX.“Minors with Legal Authority to Consent,” page2.36.)
“CAPACITY” DEFINED
A patient is presumed to have the capacity to make a
health care decision, to give or revoke an advance directive,
and to designate or disqualify a surrogate [Probate Code
Section 4657]. However, if there are indications that the
patient lacks the capacity to make health care decisions,
the primary physician should evaluate the patient.
“Capacity” means a person’s ability to understand the
nature and consequences of a decision and to make
and communicate a decision, and includes in the case
of proposed health care, the ability to understand its
significant benefits, risks, and alternatives [Probate Code
Section 4609; see also Probate Code Sections 812 and
813].
The primary physician usually makes the determination
that a patient lacks or has recovered capacity, or that
another condition exists that affects an individual health
care instruction or the authority of an agent or surrogate.
However, the patient may state in the advance directive
that someone else is required to make this determination.
[Probate Code Section 4658]
DETERMINATION OF CAPACITY
The primary physician should determine whether a
patient has the capacity to make health care decisions
[Probate Code Section 4658]. The “primary physician”
is the physician designated by the patient to have
primary responsibility for the patient’s health care, or, in
the absence of such a designation or if the designated
physician is not reasonably available or declines to act as
the primary physician, any physician who undertakes the
responsibility [Probate Code Section 4631]. A psychiatric
consult is not required, although it may be useful in unusual
situations, particularly when the patient has a serious
mental illness or another psychiatric or neurologic condition.
A physician determining a patient’s capacity to give
informed consent may wish to consider the same factors
a judge would be required to consider in the context of

Chapter 2 — Principles of Consent for Mental Health Patients CHA
2.13
©CALIFORNIA HOSPITAL ASSOCIATION
judicial determination of incapacity. A judge would evaluate
whether a patient is able to do all of the following:
1. Respond knowingly and intelligently to queries about
the proposed medical treatment.
2. Participate in the treatment decision by means of a
rational thought process.
3. Understand all of the following items of minimum
basic treatment information with respect to the
proposed treatment:
a. The nature and seriousness of the illness, disorder
or defect that the person has.
b. The nature of the medical treatment that is
being recommended by the person’s health
care providers.
c. The probable degree and duration of any benefits
and risks of any medical intervention that is
being recommended by the person’s health
care providers, and the consequences of lack
of treatment.
d. The nature, risks and benefits of any
reasonable alternatives.
A patient who has the capacity to give informed consent
to a proposed treatment also has the capacity to refuse
consent to that treatment. [Probate Code Section 813]
The mere fact that a patient has a mental health or
neurologic condition, or has recently taken prescription
or recreational drugs, does not determine whether
the patient has the requisite mental ability to make a
treatment decision. The physician must make an individual
assessment, which should be clearly documented.
A patient may lack capacity permanently (for example, a
patient with late-stage Alzheimer’s disease) or temporarily
(for example, a patient with a head injury or under the
influence of illegal drugs). The primary physician should
make the determination of capacity on a case-by-case
basis, reasonably close in time to the performance of the
procedure for which consent is sought.
Generally, it may be assumed that a patient presenting
himself or herself for treatment has the capacity to make
health care decisions unless there is evidence to the
contrary [Probate Code Sections 810 and 4657]. In the
case of mental health patients, it should be noted that
Welfare and Institutions Code Section 5331 provides that:
No person may be presumed to be incompetent
because he or she has been evaluated or treated for
a mental disorder or chronic alcoholism, regardless of
whether such evaluation or treatment was voluntarily or
involuntarily received.
Patients who have been diagnosed with a mental illness
may or may not have the capacity to give informed consent,
depending upon the degree to which their illness affects
their thought processes. The primary physician may make
this determination. A psychiatric consult is not required, but
may be useful.
DOCUMENTATION
A primary physician who determines that a patient lacks
(or has recovered) capacity must promptly record that
determination in the patient’s medical record. The physician
must communicate the determination to the patient, if
possible, and to any person then authorized to make health
care decisions for the patient. [Probate Code Section 4732]
SPECIAL CIRCUMSTANCES INVOLVING ADULTS WITH
CAPACITY
Married Patients
The patient has the right to consent to, or to refuse,
medical treatment. A patient’s spouse does not have
the legal authority to make health care decisions for the
patient simply because they are married. However, in some
circumstances a spouse may make health care decisions
on the basis of another legal relationship (for example, the
spouse is the patient’s conservator or agent appointed
pursuant to a power of attorney for health care) or on the
basis that the patient lacks capacity and the spouse is the
closest available relative.
Adults in Custody of Law Enforcement Officers
A person in the custody of law enforcement officers must
still consent to a nonemergency medical examination,
treatment, or operation before such procedures may be
performed. If the person in custody lacks the capacity
to make health care decisions, an appropriate legal
representative should be found, if possible. Although
law enforcement officers may not consent for the patient,
in narrowly defined circumstances law enforcement
officers may request limited medical examinations and
tests pursuant to their authority to make constitutionally
permissible searches. In addition, specific rules govern
drug and alcohol tests performed pursuant to Vehicle Code
Section 23612. (See CHA’s Consent Manual, chapter 9,
for more information regarding the hospital’s rights and
responsibilities with regard to patients in the custody of law
enforcement officers.)

CHA Mental Health Law Manual 2019
2.14
©CALIFORNIA HOSPITAL ASSOCIATION
Developmentally Disabled Adults
A developmentally disabled adult should not be presumed
incompetent to make his or her medical treatment
decisions. If a developmentally disabled adult is determined
by his or her physician to be mentally incapable of
consenting to treatment, consent can be provided by the
patient’s agent or surrogate, conservator legally authorized
to consent to treatment, the closest available relative, or
by court order (see “Court Order Authorizing Medical
Treatment,” page2.20).
The director of a regional center (an agency that contracts
with the state to provide services to developmentally
disabled persons) or his or her designee may consent to
medical, dental and surgical treatment of a regional center
client in certain circumstances. The hospital should consult
its legal counsel in these cases. [Welfare and Institutions
Code Section 4655]
Potential Exposure of Public Safety Workers and
Medical Personnel to Communicable Diseases
There is a limited ability to test for the presence of
communicable diseases without the patient’s consent when
a public safety worker or medical personnel may have been
exposed. The specific procedures and legal requirements
for these exceptions are described in chapter 5 of CHA’s
Consent Manual.
B. Adults Who Have Appointed an Agent or
Surrogate
An adult having capacity may execute an advance health
care directive or similar document that contains a power
of attorney for health care. The power of attorney for
health care may authorize another person, called an agent,
to make health care decisions on behalf of the patient.
The power of attorney for health care may also include
directions concerning health care decisions for the patient.
[Probate Code Section 4671]
An adult may also designate another adult as a surrogate
to make health care decisions by personally informing
the primary physician (or another health care provider in
specified circumstances) [Probate Code Section 4711].
Generally, an agent or surrogate has the same authority as
a patient to make health care decisions. However, an agent
or surrogate may not consent to the following on behalf of
a patient:
1. Commitment to or placement in a mental health
treatment facility (see chapter 3).
2. Convulsive treatment (see D.“Convulsive Therapy and
Insulin Coma Treatment,” page2.49).
3. Psychosurgery (see C.“Psychosurgery,” page2.47).
4. Sterilization or abortion (see chapter 5 of CHA’s
Consent Manual).
A detailed discussion of the laws regarding the appointment
of an agent or surrogate is found in chapter 3 of CHA’s
Consent Manual.
PSYCHIATRIC ADVANCE DIRECTIVES
A psychiatric advance directive is an instrument that mental
health patients may use to document their preferences
regarding future mental health treatment, in preparation for
the possibility of losing capacity to give or withhold consent
to treatment in the future. The mental health advocacy
community advocates the use of such documents,
particularly with respect to involuntary treatment,
psychiatric medications, restraint and seclusion.
Neither California nor federal law recognizes a special
document called a “psychiatric advance directive.” The
California advance health care directive laws and statutory
form were created with end-of-life issues in mind, not
mental health matters. However, the law does not prohibit a
person who executes an advance health care directive from
including instructions regarding mental health treatment.
Whether such wishes are required to be followed by a
health care provider if the patient loses capacity depends
upon several factors, including:
1. Whether the patient would have the legal ability to
consent or withhold consent to the recommended
treatment if he or she were competent. For example,
a patient who is detained pursuant to Welfare
and Institutions Code Section 5150 et seq. is, by
law, unable to withhold consent to be evaluated
for a mental disorder and may not leave the facility.
Therefore, if such a patient has executed an advance
directive denying consent to such care, a hospital need
not comply with this instruction.
2. Whether the wishes stated in the advance directive are
medically ineffective or contrary to generally accepted
health standards. In such a case, the facility need
not comply with the patient’s instructions. However, a
provider that declines to comply must follow certain
procedures (see Probate Code Sections 4735 and
4736).
There are no statutes, regulations, or judicial decisions
regarding “psychiatric” advance directives in California.
However, California law does contain one reference to
advance directives in the context of mental health care.

Chapter 2 — Principles of Consent for Mental Health Patients CHA
2.15
©CALIFORNIA HOSPITAL ASSOCIATION
Health and Safety Code Section 1180.4(a) requires
psychiatric units of general acute care hospitals, acute
psychiatric hospitals, skilled nursing facilities, and other
specified facilities to conduct an assessment of each
patient prior to a placement decision or upon admission,
or as soon thereafter as possible. This assessment must
include, based on the information available at the time,
the patient’s advance directive regarding de-escalation
or the use of seclusion or behavioral restraints. This law
does not authorize “psychiatric advance directives,” nor
does it require a provider to comply with a patient’s stated
preferences. It merely requires the specified providers to
assess a patient’s advance directive, if any. (See chapter 5
regarding restraint and seclusion.)
A hospital should consult legal counsel if a situation arises
regarding a psychiatric advance directive. (See chapter 3
of CHA’s Consent Manual for a complete discussion of the
law regarding advance directives.)
C. Adults Under Conservatorship
An adult patient under a conservatorship may be able
to make health care decisions. The determination of
who may make health care decisions — the patient (the
conservatee) and/or the conservator — will depend on
whether or not the conservatee has been adjudicated
to lack the capacity to make health care decisions. The
letters of conservatorship should specify whether a patient
has been adjudicated to lack the capacity to make health
care decisions.
The hospital should obtain a copy of the certified letters
of conservatorship, review them carefully and place them
in the patient’s medical record. If the hospital has any
questions about the documents, legal counsel should
be consulted.
[Probate Code Sections 1880-1898 and 2353-2357]
CAUTION: TYPE OF CONSERVATORSHIP
A conservatorship under the Lanterman-Petris-Short Act
(LPS) (which is found in the Welfare and Institutions Code)
is different from a conservatorship under the Probate
Code. If a patient is under a conservatorship, hospitals
should review the conservatorship documents issued by
the court to determine the type of conservatorship and the
conservator’s scope of authority. A patient may be subject
to both an LPS conservatorship and a Probate Code
conservatorship; however, this is not common. Both types
of conservatorship are described below.
LPS CONSERVATORSHIP
An LPS conservatorship is meant for psychiatric patients.
The purpose of an LPS conservatorship is the provision
of individualized psychiatric treatment, supervision, and
placement for a patient who is gravely disabled as a result
of a mental disorder or impairment by chronic alcoholism.
An LPS conservator may authorize the admission of the
conservatee to a mental health facility. (A Probate Code
conservator may not authorize admission to a mental
health facility.)
An LPS conservator may consent to, or refuse, routine
medical treatment (other than psychiatric treatment) of
the conservatee only if the court order establishing the
conservatorship specifically states that the conservator
may consent to routine medical treatment unrelated
to remedying or preventing the recurrence of the
conservatee’s being gravely disabled. An LPS conservator
may not, however, consent for surgery. Surgery may be
performed on an LPS conservatee only if:
1. The conservatee consents;
2. The emergency exception applies (see B.“Emergency
Treatment Exception,” page2.3); or
3. The conservator petitions for and receives a court
order issued under Welfare and Institutions Code
Section 5358.3 authorizing the surgery. [Welfare and
Institutions Code Sections 5357, 5358 and 5358.2]
[Welfare and Institutions Code Section 5350 et seq.] (See
F.“Additional Treatment for Gravely Disabled Person (LPS
Conservatorship),” page3.31. More information about LPS
conservatorships is found in chapter 3.)
PROBATE CODE CONSERVATORSHIP
A conservatorship under the Probate Code is meant
to ensure that the conservatee’s basic needs for food,
clothing, shelter, money management, and health care are
met. Conservatees may be comatose, developmentally
disabled, or have dementia or other medical problems.
Some patients under a Probate Code conservatorship may
have the ability to make their own health care decisions,
while others may not — the letters of conservatorship will
state the authority of the conservator. A Probate Code
conservator may not authorize admission to a mental
health facility.
The remainder of this section of the manual describes the
law governing Probate Code conservatorships.

CHA Mental Health Law Manual 2019
2.16
©CALIFORNIA HOSPITAL ASSOCIATION
Probate Code Conservatees Adjudicated to Lack
Capacity
A petition for a court order that the conservatee does not
have the capacity to make health care decisions may be
filed by the conservator, the conservatee, the spouse, the
registered domestic partner, a relative or a friend of the
conservatee [Probate Code Sections 1880 and 1891].
If the letters of conservatorship state that the patient lacks
the capacity to make health care decisions, then the
conservator has exclusive authority to do so. However, a
conservator may not consent in those situations discussed
under “Limitations on a Guardian’s Consent,” page2.29.
The conservator must make health care decisions for
the conservatee in good faith based on medical advice.
The decisions must be made in accordance with the
conservatee’s individual health care instructions, if any,
and other wishes to the extent known to the conservator.
Otherwise, the conservator must make the decision
in accordance with the conservator’s determination
of the conservatee’s best interest. In determining the
conservatee’s best interest, the conservator must consider
the conservatee’s personal values to the extent known
to the conservator. Provided these requirements are met,
treatment may be legally given even if the patient objects.
[Probate Code Section 2355(a)] Although the conservatee’s
consent need not be secured, the physician may wish
to explain to the conservatee the decision that has been
made for the patient, the nature of the procedure that
will be performed and any possible risks or discomforts
associated with the procedure (see Probate Code Section
4730).
Visitors, Phone Calls and Mail
A court may issue an order that grants a conservator the
power to enforce a conservatee’s right to receive visitors,
telephone calls, and personal mail. The law also allows
the court to issue an order directing a conservator to allow
specific visitors, telephone calls, and personal mail. The
conservator may be required to inform certain persons
of the patient’s death. This law was enacted to address
a situation in which a conservator (wife) refused to allow
the conservatee’s children from a prior marriage to visit
the conservatee (husband) in his home or anywhere else,
despite the conservatee’s desire to have them visit. This
law was not intended to be specific to hospital visitation,
and hospitals may continue to enforce their usual visitation
policy and reasonable visitation restrictions. [Probate
Code Sections 2351 and 2361] Hospitals should always
get a copy of conservatorship orders for conserved
patients and read them to fully understand the authority
of the conservator and any limitations. [Probate Code
Section 2351]
Prayer Healing
If, prior to the establishment of the conservatorship, the
conservatee was an adherent of a religion that calls for
reliance on prayer alone for healing, the law states that
the treatment authorized by the conservator must be
administered by an accredited practitioner of that religion
[Probate Code Section 2355(b)]. A hospital that has a
patient in this category should consult legal counsel to
determine the character of care, if any, that legally may
be provided.
Limitations on Consent by Conservator
Authorization must be obtained pursuant to the specific
statute indicated below if the treatment proposed involves
any of the following (the consent of the conservator is not
sufficient):
1. Placing a patient in a mental health treatment
facility against his or her will [Probate Code Section
2356(a)]. (See chapter 3 regarding establishing a
Lanterman-Petris-Short Act conservatorship and
involuntary detainment for mental health evaluation and
treatment.)
2. Prescribing or administering an experimental drug as
defined in Health and Safety Code Section 111515 et
seq. [Probate Code Section 2356(b)]. (See chapter 10
of CHA’s Consent Manual on the specific situations in
which a conservator may consent to the prescription or
administration of an experimental drug.)
3. Administering convulsive treatment as defined in
Welfare and Institutions Code Section 5325 [Probate
Code Section 2356(c)]. (See D.“Convulsive Therapy
and Insulin Coma Treatment,” page2.49 for more
information on conservator consent to convulsive
treatment.)
4. Sterilizing a minor [Probate Code Section 2356(d)].The
California Supreme Court’s decision in Conservatorship
of Valerie N., 40 Cal.3d 143 (1985), allows a
conservator to obtain a court order authorizing an adult
conservatee’s sterilization. Application should be made
pursuant to Probate Code Section 2357 and strict
criteria must be met.
Further, a conservator may not consent to treatment that
thwarts a valid and effective advance health care directive
and may not authorize the administration of an aid-in-dying
medication [Probate Code Section 2356(e)].
Conservatees with Dementia
Probate Code Section 2356.5 permits a conservator, with
a court order, to authorize the placement of a conservatee

Chapter 2 — Principles of Consent for Mental Health Patients CHA
2.17
©CALIFORNIA HOSPITAL ASSOCIATION
with a major neurocognitive disorder (dementia) in certain
secured perimeter residential care facilities for the elderly
operated pursuant to Health and Safety Code Section
1569.698, or a locked and secured nursing facility that
specializes in the care of people with major neurocognitive
disorders pursuant to Health and Safety Code Section
1569.691(c), and that has a care plan that meets the
requirements of Title 22, California Code of Regulations,
Section 87705. The court must find all of the following:
1. The conservatee has a major neurocognitive disorder,
as defined in the most recently published edition of the
“Diagnostic and Statistical Manual of Mental Disorders.”
2. The conservatee lacks capacity to give informed
consent to this placement and has at least one mental
function deficit pursuant to Probate Code Section
811(a) that significantly impairs the patient’s ability to
understand and appreciate the consequences of the
decision to be made.
3. The conservatee needs or will benefit from a restricted
and secure environment.
4. The proposed placement in a locked facility is the
least restrictive placement appropriate to the needs of
the patient.
The court order may also give the conservator the authority
to consent to the administration of medications appropriate
to the care of major neurocognitive disorders on behalf of
the conservatee, if the court makes findings similar to those
listed above.
If the patient is an adherent of a religion that calls for
reliance on prayer alone for healing, the treatment required
must be provided by an accredited practitioner of that
religion in lieu of administration of medications.
A conservatee may not be placed in a mental health
rehabilitation center or an institution for mental disease
under this law [Probate Code Section 2356.5(e)].
Probate Code Conservatees Not Adjudicated to Lack
Capacity
Consent by Conservatee. If the letters of conservatorship
are silent about the capacity of the patient to consent
to medical treatment, the conservatee may consent to
treatment if the physician finds the conservatee has the
capacity to give consent. The consent of the conservator is
not required, and is not sufficient, in this circumstance. The
conservatee must provide consent. [Probate Code Section
2354(a)]
However, the conservator may consent, even if the
conservatee objects to the treatment, if the conservator
has determined in good faith, on the basis of medical
advice, that there is an emergency and that treatment is
required for the alleviation of severe pain or that the medical
condition of the patient, if not immediately treated, will
lead to serious disability or death [Probate Code Section
2354(c)]. A conservator of a patient who has not been
adjudicated to lack capacity to give informed consent may
also give consent if a court has authorized the conservator
to do so [Probate Code Section 2354(b)].
If the physician has determined that the patient has
capacity to consent, a conservator who wishes to authorize
or prevent treatment that the conservatee has refused or
authorized must seek a court decision under Probate Code
Section 1880 that the patient lacks the capacity to give
informed consent (as discussed above). The conservator
also may seek a court order pursuant to Probate Code
Section 2357 that authorizes the conservator to give
consent for the specific medical treatment that is proposed.
If the physician is unwilling to rely on the consent of the
patient because the physician is uncertain of the patient’s
capacity, the physician may require the conservator to
consent also (see Law Revision Commission comment
to Probate Code Section 2354(a)). If the conservator
refuses to consent, the physician may seek a court order
authorizing the treatment under Probate Code Section
2357(i) (as discussed below).
Court Order Authorizing Treatment of Conservatee. A
conservator or other interested person may file a petition
for a court order authorizing the conservator to consent on
behalf of the conservatee for specified medical treatment.
The court may authorize the recommended medical
procedure pursuant to Probate Code Section 2357(i).
The hospital should obtain a copy of the court order, review
it carefully and place it in the patient’s medical record. The
only procedures that should be performed pursuant to the
court’s authorization are those that are specifically included
in the court order.
D. Adults Lacking Capacity and Not Under a
Conservatorship
GENERAL RULE
If a patient temporarily or permanently lacks capacity to
make health care decisions, and the emergency medical
situation exception does not apply (see B.“Emergency
Treatment Exception,” page2.3), medical treatment
should be withheld until:
1. The patient regains capacity;

CHA Mental Health Law Manual 2019
2.18
©CALIFORNIA HOSPITAL ASSOCIATION
2. An agent appointed in an advance health care directive
or a surrogate is available and gives consent;
3. A court order is issued under Probate Code Section
3200 et seq. authorizing the treatment (as discussed
in “Court Order Authorizing Medical Treatment,”
page2.20);
4. A conservator who may make health care decisions is
appointed (as discussed in “Temporary or Permanent
Conservatorship,” page2.22, and “Petition for
Appointment of Public Guardian,” page2.22);
5. In the circumstances discussed in “Family Members,”
page2.22, the patient’s closest available relative gives
consent; or
6. Consent is obtained from an interdisciplinary team as
described in “Unrepresented Patients in Skilled Nursing
Facilities,” page2.18, or “Unrepresented Patients in
Acute Care Facilities,” page2.19.
UNREPRESENTED PATIENTS IN SKILLED NURSING
FACILITIES
Prior to 1992, if a patient in a skilled nursing or intermediate
care facility lacked capacity and had no family member who
was available and willing to make health care decisions,
no conservator, and no other person with legal authority
to make health care decisions on his or her behalf, the
facility was forced to seek court authorization for treatment
pursuant to Probate Code Section 3200 et seq. (see “Court
Order Authorizing Medical Treatment,” page2.20). Health
and Safety Code Section 1418.8, adopted in 1992 and
amended in 1994, allows the facility’s interdisciplinary
team (IDT) to authorize the initiation of medical intervention
ordered by the attending physician that requires informed
consent. The use of this process has recently been
questioned by a court (see “CANHR v. Chapman,”
page2.19).
This law creates a process for authorizing affirmative
care, not for authorizing the withholding or withdrawal
of life-sustaining treatment. The IDT process is triggered
“if the attending physician ... prescribes or orders a medical
intervention that requires that informed consent be
obtained ...” [Health and Safety Code Section 1418.8(a)].
The IDT process must be undertaken as follows:
1. The attending physician must determine, through direct
patient interview, review of the patient’s medical record,
and consultation with facility staff, family members and
friends, that the patient is unable to understand the
nature and consequences of the proposed treatment,
including its risks and benefits, or is unable to express
a preference regarding the treatment;
2. The attending physician must determine, through direct
patient interview, review of the patient’s medical record,
and consultation with facility staff, family members and
friends, that there is no person with legal authority to
make health care decisions for the patient (that is, no
agent appointed in a valid power of attorney for health
care, guardian, conservator, or next of kin);
3. Except in an emergency (see h. below), the facility
must conduct an IDT review of the medical intervention
prior to its administration. This review must include all
of the following:
a. A review of the physician’s assessment of the
patient’s condition.
b. The reason for the proposed use of the
medical intervention.
c. A discussion of the desires of the patient, where
known. To determine the desires of the patient,
the IDT must interview the patient, review the
patient’s medical records and consult with family
members or friends, if any have been identified.
d. The type of medical intervention to be used in the
patient’s care, including its probable frequency
and duration.
e. The probable impact on the patient’s
condition, with and without the use of the
medical intervention.
f. Reasonable alternative medical interventions
considered or utilized, and reasons for their
discontinuance or inappropriateness.
g. Evaluation by the IDT of the use of the
prescribed medical intervention at least quarterly
or upon a significant change in the patient’s
medical condition.
h. In the case of an emergency, after obtaining a
physician’s order as necessary, a skilled nursing
or intermediate care facility may administer a
medical intervention that requires informed
consent prior to convening an IDT review. If the
emergency results in the application of physical or
chemical restraints, the IDT must meet within one
week of the emergency for an evaluation of the
medical intervention.
4. The IDT must oversee the care of the patient utilizing
a team approach to assessment and care planning
and must include the patient’s attending physician, a
registered nurse with responsibility for the patient, and
other appropriate staff in disciplines as determined by

Chapter 2 — Principles of Consent for Mental Health Patients CHA
2.19
©CALIFORNIA HOSPITAL ASSOCIATION
the patient’s needs. A patient representative must be
included on the IDT, where practicable. The patient
representative may include a family member or friend
of the patient who is unable to take full responsibility for
the health care decisions of the patient, but has agreed
to serve on the IDT, or another person authorized by
state or federal law, such as the public guardian or
the ombudsman.
5. All determinations, and the bases therefore, must be
documented in the patient’s medical record and must
be made available to the patient’s representative for
review.
This interdisciplinary team process was upheld by the
California Court of Appeal in Rains v. Belshé, 32 Cal. App.
4th 157 (1995), as meeting constitutional standards for
the privacy and due process rights of the patient. The
court said the arduous requirements on the physician and
the facility, the inclusion of a patient representative on the
interdisciplinary team and the right of the patient, or the
patient’s representative, to judicial intervention, constituted
a fair process that balanced the privacy and due process
rights of the patient with the patient’s right to medically
necessary care. However, a later court has ruled in CANHR
v. Chapman (discussed below) that this process may be
unconstitutional. This decision has been appealed and is
not in effect at the time of publication of this manual (June
2019).
CANHR v. Chapman
The Alameda County Superior Court on Jan. 27, 2016,
held that Health and Safety Code Section 1418.8 is
unconstitutional because it doesn’t require SNFs to notify
the patient that:
1. He or she has been determined to be incapable of
making medical decisions,
2. There is no substitute decision maker available,
3. The nature of the prescribed medical intervention, and
4. How to seek review.
In addition, the court explicitly stated that interdisciplinary
team consent may not be used to approve the
administration of antipsychotic drugs or end-of-life
care, such as withholding or withdrawing life-sustaining
treatment. The court indicated that judicial review or an
independent physician review would be required for these
decisions. The decision in the case, California Advocates
for Nursing Home Reform (CANHR) v. Chapman, has been
appealed and is not in effect at the time of publication of
this manual (June 2019).
As a strict legal matter, Health and Safety Code Section
1418.8 applies only to SNFs and not acute care hospitals.
Acute care hospitals can expect to be affected, however, if
the court order becomes final, because SNFs may transfer
unrepresented patients who lack capacity to acute care
hospitals if they develop conditions that trigger the need for
an informed consent. SNFs may also decline to admit new
patients who lack capacity and a decision maker. Hospitals
may, therefore, see an increase in unrepresented patients.
In addition, many acute care hospitals have adopted
the California Medical Association/California Hospital
Association/Alliance of Catholic Hospitals model
policy on making decisions for unrepresented patients
(CHA Appendix 2-D), which is based on Health and Safety
Code Section 1418.8. Hospitals that use this policy should
consult legal counsel. They may wish to add appropriate
safeguards to address the Superior Court’s concerns,
or seek conservatorship for unrepresented patients or
court approval for prescribed care under Probate Code
Section 3200 et seq. (see “Court Order Authorizing
Medical Treatment,” page2.20). CHA has developed a
check list of safeguards to consider; see CHA Appendix
2-E, “Considerations for Revising the Hospital’s Policy &
Procedure Regarding Decision Making for Unrepresented
Patients.” In addition, CHA has revised CHA Appendix 2-D
to add appropriate safeguards.
UNREPRESENTED PATIENTS IN ACUTE CARE
FACILITIES
California law has no provisions for consent to treatment on
behalf of patients in general acute care hospitals who lack
the capacity to make health care decisions, and who have
no known family member or other legally authorized person
available and willing to make those decisions.
In such cases, a hospital may wish to contact the public
guardian or conservator in its geographic area, file a
petition seeking a private conservator, or obtain a court
order authorizing medical treatment. However, the
California legislature has recognized that, “[i]n the absence
of controversy, a court is normally not the proper forum in
which to make health care decisions, including decisions
regarding life-sustaining treatment” [Probate Code Section
4650(c)].
The California Hospital Association, California Medical
Association, and Alliance for Catholic Health Care have
developed a model policy for general acute care hospitals
regarding health care decisions for unrepresented patients.
This policy, “Health Care Decisions for Unrepresented
Patients,” is found at the end of this chapter as CHA
Appendix 2-D.

CHA Mental Health Law Manual 2019
2.20
©CALIFORNIA HOSPITAL ASSOCIATION
Because there is no provision in California law for consent
for treatment for unrepresented patients, hospitals are
advised to consult legal counsel and risk management
regarding whether to adopt this policy, and if so, how to
implement it. Each hospital will need to carefully consider
which patients the policy will apply to, the circumstances
under which an independent physician consultation
will be sought, when to seek a court order authorizing
medical treatment, and when to seek the appointment of
a conservator. Hospitals using this policy, or considering
using this policy, should read the discussion under “CANHR
v. Chapman,” page2.19. These are difficult and important
decisions that each hospital will need to make.
COURT ORDER AUTHORIZING MEDICAL TREATMENT
Probate Code Sections 3200 to 3212 provide a procedure
for petitioning a court to:
1. Determine that a patient has the capacity to make a
health care decision; or
2. Determine that a patient lacks the capacity to make
a health care decision and to designate a person to
make a health care decision on behalf of the patient.
[Probate Code Section 3201]
For purposes of this law, a “health care decision” means
a decision regarding the patient’s health care, including:
1. Selection and discharge of health care providers and
institutions;
2. Approval or disapproval of diagnostic tests, surgical
procedures, and programs of medication; and
3. Directions to provide, withhold, or withdraw artificial
nutrition and hydration and all other forms of health
care, including cardiopulmonary resuscitation.
[Probate Code Section 3200(b)]
The law specifically states that it is not necessary to obtain
a court order in an emergency situations in which health
care is required for the alleviation of severe pain or the
patient’s condition, if not immediately diagnosed and
treated, will lead to serious disability or death [Probate
Code Section 3210(b)].
Persons Authorized to Petition for Court Order
A petition for a court order under this law may be filed by:
1. The patient.
2. The patient’s spouse.
3. A relative or friend of the patient or other interested
person, including the patient’s agent under a power of
attorney for health care.
4. The patient’s physician.
5. A person acting on behalf of the health care facility in
which the patient is located.
6. The public guardian or other county officer designated
by the board of supervisors of the county in which the
patient is located or resides or is temporarily living.
[Probate Code Section 3203]
Although the law allows the petition to be filed by a person
acting on behalf of the hospital, it is recommended that
the hospital not assume this responsibility except in
extraordinary situations. The recommended alternative is
to encourage another party authorized by the law to file
a petition.
Contents of the Petition
The petition must state all of the following, so far as is
known to the petitioner at the time the petition is filed:
1. The condition of the patient’s health that
requires treatment.
2. The recommended health care that is considered to be
medically appropriate.
3. The threat to the patient’s condition if authorization for
the recommended health care is delayed or denied by
the court.
4. The predictable or probable outcome of the
recommended health care.
5. The medically available alternatives, if any, to the
recommended health care.
6. The efforts made to obtain consent from the patient.
7. The name of the person to be designated to consent to
the recommended health care on behalf of the patient,
if the petition is filed by a person on behalf of a health
care facility.
8. The deficit(s) in the patient’s mental functions, as listed
in Probate Code Section 811(a), that are impaired,
and identification of a link between the deficit(s)
and the patient’s inability to respond knowingly and
intelligently to queries about the recommended health
care or inability to participate in a decision about the
recommended health care by means of a rational
thought process. The mental functions enumerated
in Probate Code Section 811(a) fall into the following
categories: alertness and attention; information
processing; thought processes; and ability to modulate
mood and affect.

Chapter 2 — Principles of Consent for Mental Health Patients CHA
2.21
©CALIFORNIA HOSPITAL ASSOCIATION
9. The names and addresses, so far as they are known to
the petitioner or proposed conservator, of the spouse
or domestic partner and the relatives of the proposed
conservatee within the second degree. If no spouse or
domestic partner or relatives within the second degree
are known to the petitioner, the names and addresses
of certain other persons must be listed [Probate Code
Section 1821(b)].
[Probate Code Section 3204]
This information may be included in the petition itself or in
an attached affidavit.
The mere diagnosis of a mental or physical disorder is not
sufficient in and of itself to support a determination that a
person is of unsound mind or lacks the capacity to consent
to medical treatment [Probate Code Section 811(d)].
Court Action on Petition
After the petition is filed, the court will determine whether
the patient is represented by legal counsel, whether it will
consider the petition in summary proceedings, and what, if
any, notice of the hearing must be given.
Legal Counsel. If the patient has not retained an attorney
and does not plan to do so, the court will appoint the
public defender or a private attorney to consult with and
represent the patient in the court proceedings [Probate
Code Section 3205].
Summary Proceedings. The petition may be submitted
for the determination of the court, without a hearing, upon
proper and sufficient medical declarations if the attorney for
the petitioner and the attorney for the patient so stipulate,
provided they also stipulate that there remains no issue
of fact to be determined. If, however, the parties do not
stipulate to summary proceedings, a hearing must take
place. [Probate Code Section 3207]
Notice of Hearing. If a hearing is required, notice of the
time and place of the hearing on the petition, and a copy of
the petition, must be:
1. Personally served on the patient, the patient’s attorney,
and the agent under the patient’s power of attorney for
health care, if any, and
2. Mailed to the patient’s spouse, if any, and the patient’s
relatives named in the petition.
The personal service and mail service must take place
not less than 15 days before the hearing. The court may
shorten or waive notice of the hearing for good cause. In
determining the period of notice to be required, the court
must take into account the existing medical facts and
circumstances and the desirability, where the condition
of the patient permits, of giving adequate notice to all
interested persons. [Probate Code Section 3206]
Circumstances in Which the Court May Issue an Order
Except in those situations discussed in “Limitations on
a Guardian’s Consent,” page2.29, the court may issue
an order authorizing the recommended health care for
the patient and designating a person to consent to the
recommended health care on behalf of the patient if it
determines from the evidence all of the following:
1. The existing or continuing condition of the patient’s
health requires the recommended health care.
2. There is a probability that the condition will become
life-endangering or result in a serious threat to the
physical or mental health of the patient, if untreated.
3. The patient is unable to consent to the recommended
health care.
[Probate Code Section 3208(a)]
The court may also order the withholding or withdrawal of
artificial nutrition and hydration and all other forms of health
care, and designate a person to give or withhold consent to
the recommended health care if the court determines that:
1. The recommended health care is in accordance with
the patient’s best interest, taking into consideration the
patient’s personal values to the extent known, and
2. The patient is unable to consent to the recommended
health care.
[Probate Code Section 3208(c)]
Limitations on Court Order
Authorization must be obtained under the specific law
indicated below if the treatment proposed involves any of
the following (the court order obtained pursuant to Probate
Code Section 3200 et seq. is not sufficient):
1. Placing a patient in a mental health treatment
facility against his or her will [Probate Code Section
3211(a)]. (See chapter 3 regarding establishing a
Lanterman-Petris-Short Act conservatorship and
involuntary detainment.)
2. Prescribing or administering an experimental drug as
defined in Health and Safety Code Section 111515 et
seq. [Probate Code Section 3211(b)]. (See chapter 7
of CHA’s Consent Manual on the specific situations in
which a conservator may consent to the prescription or
administration of an experimental drug.)

CHA Mental Health Law Manual 2019
2.22
©CALIFORNIA HOSPITAL ASSOCIATION
3. Administering convulsive treatment as defined in
Welfare and Institutions Code Section 5325 [Probate
Code Section 3211(c)]. (See D.“Convulsive Therapy
and Insulin Coma Treatment,” page2.49 for more
information on conservator consent to convulsive
treatment.)
4. Sterilizing a patient [Probate Code Section
3211(d)]. The California Supreme Court’s decision in
Conservatorship of Valerie N., 40 Cal.3d 143 (1985),
allows a conservator to obtain a court order authorizing
an adult conservatee’s sterilization. Application should
be made pursuant to Probate Code Section 2357 and
strict criteria must be met.
Further, a court may not order treatment that thwarts a
valid and effective advance health care directive [Probate
Code Section 3211(e)].
Finding that Patient has Capacity to Consent
If the court finds that the patient has the capacity to
consent to the recommended health care, the court will so
state in its order [Probate Code Section 3208.5(a)].
If the court has determined that the patient has the
capacity to consent to the recommended health care, the
court must, if requested, determine whether the patient
has accepted or refused the recommended health care,
and whether the patient’s consent to the recommended
health care is an informed consent [Probate Code Section
3208.5(b)].
Where the court finds that the patient has the capacity
to consent to the recommended health care, but refuses
to do so, the court may not make an order authorizing
the treatment or designating a person to give consent to
the treatment. Furthermore, if an order has been made
authorizing the treatment and designating a person to give
consent, the order must be revoked if the court determines
that the patient has recovered the capacity to give
informed consent to the recommended course of medical
treatment. Until revoked or modified, the order is effective
authorization for the course of medical treatment [Probate
Code Section 3208.5(c)].
TEMPORARY OR PERMANENT CONSERVATORSHIP
Any interested party may request a temporary and/or
permanent conservatorship under Probate Code Section
1820. Although this often is the most desirable means of
resolving the situation, it may not be a viable alternative if:
1. The patient needs relatively expedited care that cannot
be postponed while the request for a conservatorship
is being processed; and/or
2. The patient may only temporarily lack capacity (e.g., as
a result of the patient’s immediate medical condition)
and therefore a conservatorship may not be warranted.
Once a petition for conservatorship is filed, a court
investigator must interview the proposed conservatee,
petitioners, proposed conservators, the proposed
conservatee’s spouse or registered domestic partner and
relatives. The investigator will prepare a written report
about the mental capacity of the proposed conservatee,
which will be made available to the proposed conservatee,
petitioners and relatives.
The conservatee has the right to have the matter tried
by jury, be represented by legal counsel, and have legal
counsel appointed by the court if unable to retain legal
counsel.
If a conservatorship is ordered, the court investigator will
interview the conservatee from time to time to determine if
continuation of the conservatorship is warranted.
PETITION FOR APPOINTMENT OF PUBLIC GUARDIAN
Any interested person may initiate a proceeding to have
the county public guardian appointed as the guardian or
conservator of a:
person domiciled in the county who appears to require
a guardian or conservator, if it appears that there is no
one else who is qualified and willing to act, and if that
appointment as guardian or conservator would be in the
best interests of the person.
In fact, the law requires the public guardian to apply for
appointment as guardian or conservator of the person,
the estate, or both, if there is an imminent threat to the
person’s health or safety or the person’s estate.
A hospital that is interested in having the public guardian
appointed as a patient’s guardian or conservator should
consult the public guardian’s office. [Probate Code
Section 2920]
FAMILY MEMBERS
Basis for Relying on Consent
In some circumstances, it may be necessary or desirable
to rely upon the consent given by family members of a
patient lacking capacity to make health care decisions.
The California Supreme Court has indicated that in some
cases it is appropriate for a relative to give consent. The
court said:
[I]f the patient is a minor or incompetent, the authority
to consent is transferred to the patient’s legal guardian
or closest available relative (emphasis added). [Cobbs v.
Grant, 8 Cal.3d 229, 244 (1972)]

Chapter 2 — Principles of Consent for Mental Health Patients CHA
2.23
©CALIFORNIA HOSPITAL ASSOCIATION
Also, a California appellate court, in Barber v. Superior
Court, 147 Cal.App.3d 1006 (1983), held that a hospital
and physicians properly relied upon the decisions regarding
discontinuance of medical treatment that were made by
a patient’s wife and children. The court explained that
California law does not state that only court-appointed
guardians or conservators have the authority to act on
behalf of another person, and that in the absence of such
a statement in the law, an incompetent patient’s immediate
family could make health care decisions for the patient.
The court cautioned, however, that such persons must
be guided first by the patient’s own desires and feelings,
to the extent they were expressed before the patient
became incompetent. If the patient’s desires were not
expressed or cannot be ascertained, the court stated that
surrogate decision makers must be guided by the patient’s
best interests.
The Barber decision adds an important element of
protection for health facilities that rely on the consent of
immediate family members. Accordingly, such reliance
may be considered a reasonable means of dealing with
situations in which an adult patient who does not have an
agent or a conservator is unable to consent to required
treatment. By obtaining the consent or concurrence of
concerned relatives, the risk of liability will be minimized.
Basis for Not Relying on Consent
The hospital should not rely on consent from family
members if any of the following circumstances are present:
1. The relative’s capacity to make health care decisions or
motives are questionable.
2. There is a substantial question as to whether the
patient, if he or she had the capacity to make health
care decisions, would consent to the procedure.
3. Another close relative objects to the medical procedure.
The facility should carefully consider the situation if the
medical procedure required has uncertain or minimal
expected benefits; will result in severe debilitation; and/or
involves a significant risk of a negative outcome, such as
paralysis. Also, if the relative’s refusal to consent appears
to be unreasonable, the refusal should not be relied upon.
In each of these situations, it is probably preferable to
rely upon the use of a Probate Code Section 3200 et seq.
petition. (See “Court Order Authorizing Medical Treatment,”
page2.20.) Legal counsel should be consulted.
Identifying an Appropriate Family Member to Consent
Once it is determined that it is appropriate to rely upon the
consent of a family member, it is necessary to determine
which family member is the most appropriate surrogate
decision maker. The California Medical Association and
the California Hospital Association have developed
guidelines to assist physicians and hospitals in identifying
an appropriate surrogate decision maker for a patient who
lacks capacity and who has no guardian, conservator
or agent appointed in a valid advance directive. These
guidelines are found in CHA’s Consent Manual, chapter 2.
If there is reason to suspect that the patient’s family
members are not acting in the best interests of the patient,
the use of a Probate Code Section 3200 et seq. petition
may be appropriate (see “Court Order Authorizing Medical
Treatment,” page2.20). Legal counsel should be consulted.
Registered Domestic Partners
California law states that a registered domestic partner
has the same authority to make a health care decision
for his or her incapacitated domestic partner as a spouse
would have to make a health care decision for his or her
incapacitated spouse [Family Code Section 297.5 and
Probate Code Section 4716].
The physician must make a determination that the patient
lacks capacity, prior to looking to the registered domestic
partner to provide consent (see ““Capacity” Defined,”
page2.12).
The law permitting persons to register as domestic
partners is found at Family Code Sections 297 and 297.1.
“Domestic partners” are “two adults who have chosen
to share one another’s lives in an intimate and committed
relationship of mutual caring.” The following requirements
must be met in order to register as domestic partners:
1. Neither person is married or a member of another
domestic partnership.
2. The two persons are not related by blood in a way that
would prevent them from being married to each other
in this state.
3. Both persons are at least 18 years of age. Persons
under 18 must obtain parental permission and/or a
court order.
4. Either of the following apply:
a. Both persons are members of the same sex.
b. One or both of the persons meet the eligibility
criteria under Title II of the Social Security Act
for old-age insurance benefits or Title XVI of the
Social Security Act for aged individuals. However,
persons of opposite sexes may not constitute a
domestic partnership unless one or both are over
62 years of age.

CHA Mental Health Law Manual 2019
2.24
©CALIFORNIA HOSPITAL ASSOCIATION
5. Both persons are capable of consenting to the
domestic partnership.
The Secretary of State produces forms entitled “Declaration
of Domestic Partnership” and “Notice of Termination of
Domestic Partnership” to document the beginning and
ending of a domestic partnership. The forms must be
signed by each partner and also by a notary public. The
Secretary of State will register the partnership and return a
copy of the registered form to the domestic partners.
Hospitals are advised to develop and implement policies
regarding proof of marriage and proof of domestic
partnership equally. For example, if a hospital requires a
person to produce a marriage certificate to prove that he
is indeed the spouse of a patient, then the hospital should
require a person to produce a registered “Declaration of
Domestic Partnership” form to prove that he is indeed the
registered domestic partner of a patient.
Under California law, registered domestic partners have
the same rights and responsibilities as spouses. This may
include paying medical and hospital bills.
E. Summary of Consent Requirements Regarding
Adults
CHA has included a table at the end of this manual
titled “Consent Requirements for Medical Treatment of
Adults” (CHA Table 2-A) summarizing consent issues
regarding adults.
VII. WHO MAY GIVE CONSENT: MINORS
A. Introduction
Parents have a legal obligation to provide the necessities
of life for their minor children, including medical care [Penal
Code Section 270]. It is generally accepted that, until their
children reach 18 years of age, parents also have the right
to control that care.
Some exceptions to this general rule exist. Some
exceptions are based on the status of the minor
(emancipated, married, serving in the military, etc.). Other
exceptions are based upon the nature of the treatment
sought (pregnancy-related care, communicable disease,
mental health, etc.). This portion of the manual discusses
who may consent for treatment on behalf of minors.
Additional requirements for inpatient mental health
admissions and treatment for minors, both voluntary and
involuntary, are discussed in chapter 3.
The person who has the legal authority to consent for the
treatment of a minor also has the legal authority to refuse
the treatment. Thus, if a minor is legally authorized to
consent to treatment, the minor also has the legal authority
to refuse the treatment. The minor must also have the
capacity to make health care decisions (see B.“Capacity to
Consent,” page2.37). However, if a parent or other legal
representative refuses treatment for a minor and serious
harm to the minor may result, legal counsel should be
consulted. (See F.“Where Refusal of Treatment May Cause
Serious Harm to the Minor,” page2.26, for additional
information.)
“Minors” are all persons under 18 years of age [Family
Code Section 6500].
B. The Evolution of the Rights of Minors
Minors, because of their legal status, have generally been
recognized as lacking the legal capacity to give consent
for health care services. In recognition of the interests
of minors in health care decisions affecting them, and in
appreciation of their actual capacity to understand and
evaluate the nature of health care decisions confronting
them, state legislatures and courts have determined that
under specific circumstances, minors are to be treated as
adults for purposes of consenting to care.
The early court cases that laid the foundation for this
transformation found minors capable of providing consent
to medical treatment through the doctrine of the “mature
minor.” This doctrine provides that a minor may give
consent to medical care when the treating physician
finds that:
1. The minor is of sufficient age (typically 14 years of age
or over) to appreciate the risks and benefits of the
proposed treatment;
2. The minor understands the risks and benefits of the
treatment, and the consequences of the decision (i.e.,
the minor can give informed consent); and
3. The treatment will benefit the minor, not another person.
California has not adopted the mature minor doctrine.
However, in 1953, the California Legislature gave unmarried
pregnant minors the authority to consent to treatment
related to their reproductive care. In 1961, minors on active
duty in the armed services and those who were married,
divorced, or widowed were given the right to consent to
medical treatment. By 1970, the rights of minors were
broadened to include the ability to consent to treatment if
the minor is 15 years of age or over, living away from home
and managing his or her own finances.

Chapter 2 — Principles of Consent for Mental Health Patients CHA
2.25
©CALIFORNIA HOSPITAL ASSOCIATION
Whether a minor has the legal right to consent to medical
treatment independent of the minor’s parents will depend
on several factors. In California, the law permits a minor
to obtain medical treatment independent of parental
authorization when:
1. The minor has achieved a status of “emancipation” as
established by law;
2. The minor is seeking treatment for a statutorily
specified medical need; or
3. There is some other specialized situation recognized by
the law in which parental consent is not required.
These exceptions to the general rule requiring parental
consent are discussed in this manual.
C. Financial Responsibility for Treatment of
Minors
The person legally responsible for a minor (i.e., the minor’s
parent(s) or guardian) is generally responsible for the
minor’s financial obligations, including payment of medical
bills. However, Welfare and Institutions Code Section
14010 states that the parents of a minor are not financially
responsible for health care or related services to which the
minor may legally consent. There is a limited exception
to this general rule for emancipated minors living in the
home of the parent(s) (see C.“Emancipation Pursuant to
Court Order,” page2.37), or if the parents are participating
in counseling with the minor (see “Parental Involvement/
Liability,” page2.39).
Health care providers should establish a system to ensure
that they do not bill parents for services for which the
parents are not financially responsible, as this may be
considered a breach of the minor’s privacy rights (unless
the minor’s authorization is obtained). Medi-Cal has a
“minor consent” program (also known as “sensitive services”
program) that enrolls minors regardless of parental income
or assets, insurance status, or citizenship status. Parents
will not be contacted. This program covers health care
services for pregnancy, family planning, abortion, sexual
assault, sexually transmitted diseases, mental health
outpatient treatment (with some limitations), and substance
abuse treatment. [Title 22, California Code of Regulations,
Sections 50063.5, 50147.1, 50157, 50167 and 50195(d)]
It is acceptable to bill insurance companies, even if the
parent is the named subscriber on the policy; payers
are required to have a procedure in place to ensure the
minor’s confidentiality.
D. Privacy Rights of Minors
Under state and federal law, a minor has a privacy right
in health information resulting from services to which
the minor is authorized to consent. This is true even if,
as a practical matter, the minor’s parent actually gives
consent. For example, a parent may take his teenager to
a physician for treatment of a reportable communicable
disease. Even though the parent solicits and consents to
the services, privacy laws prevent the health care provider
from disclosing health information to the parent or guardian
without the minor’s authorization because, under state law,
the minor could have obtained those services independent
of the parent.
Both the Confidentiality of Medical Information Act and
HIPAA contain an exception to privacy requirements to
permit disclosure of limited information to a family member
if the information is directly relevant to the family member’s
involvement with the patient’s care. However, there are
limitations on this exception (see I.“Minor’s Medical
Records,” page6.12, and E.“Family and Friends: Patients
Covered by CMIA,” page6.7). In addition, this exception
does not apply to records and information covered by the
Lanterman-Petris-Short (LPS) Act or to substance abuse
information from federally-assisted substance use disorder
treatment programs (see chapter 6). The safest course of
action if a provider wishes to discuss outpatient mental
health treatment with a parent or guardian is to obtain
the minor’s written authorization for disclosure of health
information. [45 C.F.R. Sections 164.502(g) and 164.510(b);
Civil Code Sections 56.11(c) and 56.1007; Health and
Safety Code Sections 123110 and 123115; Welfare and
Institutions Code Section 5328]
Thus, in order to ensure HIPAA compliance and to avoid
privacy breaches, providers must also understand the
instances in which a minor has legal authority to consent
to treatment. (See chapter 6 for more information about
minors’ privacy rights.)
E. Minor’s Disagreement with Parent or Other
Legal Representative Regarding Treatment
Medical providers occasionally encounter situations in
which minors who do not have the legal authority to make
health care decisions indicate a desire to refuse treatment
that their parents or other legal representatives wish
them to have — or conversely, wish to have treatment
that their parents or other legal representatives decline.
Although minors are considered legally incompetent to
make decisions in many areas of medical care by virtue of
their age, nevertheless it is appropriate to discuss medical

CHA Mental Health Law Manual 2019
2.26
©CALIFORNIA HOSPITAL ASSOCIATION
decisions with them in a manner appropriate to their age.
Ascertainment of the child’s preference for treatment was
specifically approved in the case In re Christopher I. (see
“Minors in Custody of the Juvenile Court/Foster Children,”
page2.47).
A minor’s refusal to participate in mental health treatment
presents special challenges for the therapist and may make
treatment unproductive. A therapist is not required to treat
a minor who is voluntarily admitted or who is an outpatient
if the minor declines to cooperate, even if the parent(s) are
insistent. Minors who are involuntarily admitted have a right
to treatment (see E.“Special Requirements for a Minor,”
page3.16).
Providers should proceed cautiously in situations where
the minor disagrees with the parents or other legal
representatives, particularly if the treatment or refusal
involves a significant risk of serious adverse consequences.
Providers faced with such situations may wish to consider
the following.
MINOR’S AGE, MATURITY, AND EXPERIENCE WITH
THE TREATMENT IN QUESTION
Remember that the law permits minors as young as 12
years of age to consent to certain treatments, including
outpatient mental health treatment (see G.“Minors in
Need of Outpatient Mental Health Treatment or Residential
Shelter Services,” page2.39). This suggests that minors
of that age may be in a position to appreciate the risks
and burdens of other treatments as well, and may have
reasonable grounds for wishing to consent to, or refuse,
such treatment.
DISAGREEMENT REGARDING THE TREATMENT
DECISION
The provider may be in a position to discuss the treatment
with the minor, clarify any confusion or misunderstanding,
and bring the matter into perspective. It may be helpful to
involve a social worker, psychologist, or other person with
a positive relationship with the minor to help resolve the
disagreement between the minor and the parents or other
legal representative.
If the provider is uncomfortable in providing treatment over
the minor’s objection, the provider may wish to reconsider
the clinical appropriateness of the treatment, or may
decline to participate in the case after taking appropriate
steps to transfer the care of the patient to another
health care provider. It may be appropriate to consult
legal counsel in such situations. Consultation with legal
counsel is strongly encouraged where refusal of care may
cause serious harm to the minor (see F.“Where Refusal
of Treatment May Cause Serious Harm to the Minor,”
page2.26).
F. Where Refusal of Treatment May Cause
Serious Harm to the Minor
At times a health care provider may encounter a situation in
which the parent, guardian, or other legal representative of
a minor declines medically necessary care, and the refusal
of that care may cause serious harm to the minor. In such
cases, legal counsel should be consulted immediately.
A parent or other legal representative may not decline
treatment where such refusal may cause serious physical
harm or illness to the minor; judicial intervention should
be sought. This portion of the manual provides a very
brief description of basic legal principles regarding such
situations, but it is emphasized that legal counsel should
always be sought in these cases.
If a minor, as a result of a mental disorder, is a danger
to self or others or gravely disabled, the minor may be
involuntarily detained for mental health evaluation and
treatment even if the parent(s) will not authorize voluntary
treatment [Welfare and Institutions Code Section 5585.53].
(See E.“Special Requirements for a Minor,” page3.16.)
REFUSAL FOR RELIGIOUS REASONS
Two of the more common situations involving refusal of care
for religious reasons involve Jehovah’s Witnesses, who
may decline blood products, and Christian Scientists, who
may decline traditional medical care in favor of treatment by
spiritual means. (See CHA’s Consent Manual, chapter 6, for
further information about refusal of blood products.)
California law explicitly permits a parent to provide a minor
with “treatment by spiritual means through prayer alone in
accordance with the tenets and practices of a recognized
church or religious denomination, by a duly accredited
practitioner thereof” [Penal Code Section 270]. (See also
Welfare and Institutions Code Sections 300, 5006, 7104
and 16509.1.) However, provision of prayer alone to a
minor child is permitted only insofar as the child is not
threatened with serious physical harm or illness [Walker
v. Superior Court, 253 Cal.Rptr. 1, 47 Cal.3d 112 (1988),
rehearing denied, cert.den.109 S.Ct. 3186, 491 U.S. 905].
If the refusal of treatment may cause serious harm to the
minor, California courts may order life-saving medical
treatment despite the parents’ refusal to consent to such
treatment on religious grounds. The Walker court stated
that “parents have no right to free exercise of religion at
the price of a child’s life…” The threatened harm does not

Chapter 2 — Principles of Consent for Mental Health Patients CHA
2.27
©CALIFORNIA HOSPITAL ASSOCIATION
need to rise to the level of death for the courts to intervene.
Health care providers should seek court intervention
in such cases, rather than attempting to balance the
competing interests involved and making the decision
themselves whether to treat a minor over the parent’s (or
other legal representative’s) objection.
Thus, the state may intervene in the parent-child
relationship to protect the child.
COURT INTERVENTION
Welfare and Institutions Code Section 300 delineates the
circumstances under which a child can be declared a
dependent of the court. Any child who comes within the
following description is within the jurisdiction of the juvenile
court and may be declared a dependent child of the court:
The child has suffered, or there is a substantial risk that
the child will suffer, serious physical harm or illness, as
a result of the failure or inability of his or her parent or
guardian to … provide the child with adequate food,
clothing, shelter, or medical treatment … Whenever
it is alleged that a child comes within the jurisdiction
of the court on the basis of the parent’s or guardian’s
willful failure to provide adequate medical treatment or
specific decision to provide spiritual treatment through
prayer, the court shall give deference to the parent’s or
guardian’s medical treatment, nontreatment, or spiritual
treatment through prayer alone in accordance with the
tenets and practices of a recognized church or religious
denomination, by an accredited practitioner thereof,
and shall not assume jurisdiction unless necessary to
protect the child from suffering serious physical harm
or illness. In making its determination, the court shall
consider (1) the nature of the treatment proposed by the
parent or guardian, (2) the risks to the child posed by
the course of treatment or nontreatment proposed by
the parent or guardian, (3) the risk, if any, of the course
of treatment being proposed by the petitioning agency,
and (4) the likely success of the courses of treatment or
nontreatment proposed by the parent or guardian and
agency. The child shall continue to be a dependent child
pursuant to this subdivision only so long as is necessary
to protect the child from risk of suffering serious physical
harm or illness. [Welfare and Institutions Code Section
300(b)]
In many counties, particular agencies provide assistance
in securing the court’s authorization to treat a minor
when the parents have refused to consent (e.g., Child
Protective Services). Such agencies are usually a part of
the county’s juvenile court services or department of social
services. Also, assistance for securing court authorization
for juveniles on probation may often be secured from the
county’s probation department.
VIII. MINORS LACKING LEGAL AUTHORITY TO
CONSENT
By statutory definition, a person under the age of 18
is unable to consent to medical treatment except as
otherwise allowed by law (see IX.“Minors with Legal
Authority to Consent,” page2.36). When a minor needs
medical treatment, health care providers usually must look
to a parent, guardian or other person to consent.
However, as with adults, consent to treatment may be
presumed in medical emergencies, i.e., where a minor
requires immediate care for alleviation of severe pain or
immediate diagnosis and treatment of unforeseeable
medical conditions which, if not immediately diagnosed and
treated, would lead to serious disability or death [Business
and Professions Code Section 2397(c)(2) and (3)]. (See
B.“Emergency Treatment Exception,” page2.3, for more
information.)
A. Parental Consent for Treatment of Minors
MINORS WITH MARRIED PARENTS
In the absence of evidence of a disagreement between the
parents of a minor, either parent has the legal authority to
consent [Family Code Section 6903]. Where one parent
consents to treatment but the other parent is opposed,
treatment should not be provided until the conflict
is resolved.
MINORS WITH DIVORCED PARENTS
If both parents agree on the proposed treatment of the
minor, the health care provider should have both parents
sign the applicable consent forms.
If a disagreement exists about the treatment of a minor with
divorced parents, a copy of the custody order should be
obtained to determine which parent has the authority to
make health care decisions for the child. The copy of the
court order should be placed in the minor’s medical record.
If one parent has sole legal custody, then that parent has
the right and responsibility to make health care decisions
for the child [Family Code Sections 3006 and 6903].
Where, as is often the case, the parents have joint legal
custody, either parent has the right and responsibility to
make health care decisions for the child unless the court
has specified, in its custody order, that the consent of both
parents is required [Family Code Sections 3003, 3083 and
6903].

CHA Mental Health Law Manual 2019
2.28
©CALIFORNIA HOSPITAL ASSOCIATION
If the parents having joint legal custody disagree regarding
treatment of the minor, they should be instructed to
obtain a court order resolving the dispute before medical
treatment is provided, if the procedure can be delayed
without jeopardizing the minor’s health. If the delay might
harm the minor, the physician and hospital may decide
that treatment should be provided, notwithstanding one
parent’s objection. The rationale for such a decision should
be carefully documented in the minor’s medical record.
Providers should consult with legal counsel regarding
individual cases, as appropriate.
Access to a minor’s medical records and information, to
which the parent is otherwise entitled, may not be denied
to a parent solely because that parent is not the minor’s
custodial parent [Family Code Section 3025]. (See In re
Daniel C. H., 220 Cal. App.3d 814 (1990).) However, other
reasons may apply to deny a non-custodial parent access
to the record (for example, the minor may consent to his or
her own care and denies the parent access to the related
information, or the parent has abused the child, etc.).
MINORS WITH STEPPARENTS
A stepparent who has not legally adopted a minor does not
have the authority to consent to treatment on the minor’s
behalf without written authorization from the natural parent
or guardian or a valid Caregiver’s Authorization Affidavit
(see C.“Third-Party Consent for Treatment of Minors,”
page2.30).
ADOPTED MINORS
Where a minor has been legally adopted (by order of the
court), the adoptive parents have the same right to consent
to medical care on behalf of the minor as would birth
parents [Family Code Section 8616]. The birth parents have
no rights or responsibilities for the child after adoption and
thus may not consent to, or object to, medical treatment for
the minor [Family Code Section 8617]. (See also “Minors
Placed for Adoption,” page2.32.)
MINORS BORN OUT OF WEDLOCK
The mother has the legal authority to consent to medical
treatment for a minor born out of wedlock.
The father also has the legal authority to consent to medical
treatment for the minor. However, where there is reason to
doubt the status of someone claiming to be a child’s father,
the provider should require a copy of a birth certificate or
court judgment or order determining the existence of the
father-child relationship before accepting the consent of the
alleged father (see California Uniform Parentage Act, Family
Code Section 7600 et seq.).
Where one parent consents to treatment but the other
parent is opposed, treatment should not be provided until
the conflict is resolved, if the procedure can be delayed
without jeopardizing the child’s health. If the delay might
harm the child, the physician and hospital may decide that
treatment should be provided, notwithstanding one parent’s
objection. The rationale for such a decision should be
carefully documented in the minor’s medical record. Legal
counsel should be consulted in such cases.
MINORS WITH A REGISTERED DOMESTIC PARTNER
PARENT(S)
California permits adults to register as domestic
partners [Family Code Section 297] (see “Registered
Domestic Partners,” page2.23, for information about
the requirements for registration as domestic partners).
State law gives registered domestic partners (or former or
surviving registered domestic partners) the same rights
and obligations as are granted spouses in a marriage. This
includes the rights and obligations of registered domestic
partners with respect to a child of their partner. [Family
Code Section 297.5]
However, becoming the spouse of a parent is not the
same as becoming a parent, even for legally married
heterosexual couples. For example, as noted above,
even though a stepmother is legally married to a minor’s
natural father, the stepmother does not have the authority
to consent to treatment on the minor’s behalf without
written authorization from the father or mother, or a valid
Caregiver’s Authorization Affidavit.
These same rules apply to registered domestic partners. In
order for the registered domestic partner of a child’s parent
to consent for medical care for that child, the domestic
partner must do one of the following:
1. The registered domestic partner must have legally
adopted the child;
2. The registered domestic partner must provide a signed
third-party authorization form giving him or her the
ability to consent to medical care for the child (see
“Other Third-Party Consent,” page2.30); or
3. The registered domestic partner must complete a valid
Caregiver’s Authorization Affidavit (see “The Caregiver’s
Authorization Affidavit,” page2.30).
Given the variety of relationships that can arise, if questions
arise, or there is reason to doubt the status of someone
claiming to be a child’s parent, the provider may rely on
the birth certificate or custody order to determine who may
legally provide consent. If a registered domestic partner

Chapter 2 — Principles of Consent for Mental Health Patients CHA
2.29
©CALIFORNIA HOSPITAL ASSOCIATION
is not named on the birth certificate or custody order,
the registered domestic partner should be treated as a
stepparent.
OTHER SITUATIONS INVOLVING NONBIOLOGICAL
PARENTS OR MULTIPLE PARENTS
The courts are continuing to address a variety of situations
in which men and women not biologically related to a
child are being recognized as having parental rights and
obligations, even in the absence of marriage or a registered
domestic partnership. Several cases involving female
same sex couples were decided in 2005. (See Elisa B. v.
Superior Court, 37 Cal.4th 108 (2005) (woman held to have
parental support obligations for children born to former
partner during time that the women were in a committed
relationship); K.M. v. E.G., 37 Cal.4th 130 (2005) (woman
who donated ovum to birth mother and helped raised
children acknowledged to have parental rights following
their separation).) These situations may present challenges
where medical decision making for children is involved.
One difficulty in such instances is that an individual’s legal
relationship to a child may be contested and require judicial
intervention to determine. Hospitals should consult their
legal counsel should they have reason to question the
authority of purported decision makers.
A court may declare that a child has more than two parents
[Family Code Sections 3040 and 7612]. Each parent
should be treated as a natural parent, unless a court order
says otherwise.
B. Guardian Consent for Treatment of Minors
If a guardian has been appointed for a minor, the ability of
the guardian to consent to medical treatment for the minor
depends on the specific authority granted by the court and
the type of treatment.
A copy of the official certified letters of guardianship should
be obtained and placed in the minor’s medical record
before proceeding with treatment. The official letters of
guardianship should be reviewed to determine the scope
of the guardian’s legal authority to consent to medical
treatment and that, if any, of the parents. If a conflict arises
between the guardian and the parent(s), legal counsel
should be contacted.
Except as otherwise specified in the letters of guardianship,
the guardian may consent to medical treatment of the
minor as follows.
NONSURGICAL TREATMENT
The guardian has the same rights as a parent to consent to
nonsurgical treatment for the minor [Probate Code Section
2353(a)].
SURGICAL TREATMENT
The guardian’s consent is necessary for surgical treatment.
However, if the minor is 14 years of age or older, surgery
may not be performed upon the minor without:
1. The consent of both the minor and the guardian; or
2. A court order obtained by the guardian; or
3. The consent of the guardian alone provided that the
guardian determines in good faith, based on medical
advice, that the case involves an emergency in which
the minor faces loss of life or serious bodily injury if
the surgery is not performed. In this situation, there
is immunity from liability for an allegation of lack
of consent.
[Probate Code Section 2353(b) and (c)]
LIMITATIONS ON A GUARDIAN’S CONSENT
The guardian’s consent for certain types of treatment for
the minor is insufficient or must meet additional specific
requirements if the treatment involves:
1. Placing the patient in a mental health treatment
facility [Probate Code Section 2356(a)]. A guardian
may admit a ward to a private psychiatric facility
pursuant to Welfare and Institutions Code Section
6002.15 or to a state hospital pursuant to Welfare
and Institutions Code Section 6000. (See chapter
3 about the admission of minors to psychiatric
facilities, establishing Lanterman-Petris-Short Act
conservatorships, and involuntary detainment.)
2. Prescribing or administering an experimental drug as
defined in Health and Safety Code Section 111515 et
seq. [Probate Code Section 2356(b)]. (See chapter 10
of CHA’s Consent Manual on the specific situations in
which a guardian may consent to the prescription or
administration of an experimental drug.)
3. Administering convulsive treatment as defined in
Welfare and Institutions Code Section 5325 [Probate
Code Section 2356(c)]. (See X.“Treatments That
Require Special Consent,” page2.42, on the protocol
for and restrictions on a guardian’s consent for
administration of convulsive treatment.)
4. Sterilization of the patient [Probate Code Section
2356(d)]. This prohibition applies only to elective

CHA Mental Health Law Manual 2019
2.30
©CALIFORNIA HOSPITAL ASSOCIATION
sterilizations (i.e., procedures performed primarily for
the purpose of rendering the patient sterile), but not
to treatment that is not for the purpose of, but results
in, sterility (i.e., secondary sterilization). (See chapter
5 of CHA’s Consent Manual regarding the prohibition
against elective sterilization of a minor.)
5. Psychosurgery. Under no circumstances may
psychosurgery be performed on a minor [Welfare and
Institutions Code Section 5326.6].
6. Administering aid-in-dying medication. Only a mentally
competent adult may request and self-administer
an aid-in-dying medication [Health and Safety Code
Section 443.2].
C. Third-Party Consent for Treatment of Minors
Children are often under the supervision of a person other
than their parents or guardians for a major part of the day.
Apart from the time minors spend in school, care for minors
is often left in the hands of a babysitter, relative, neighbor,
camp counselor, sports coach, preschool teacher or day
care provider. (See “Minors Who Are Ill or Injured During
School Hours,” page2.32, about medical treatment of a
minor’s injury or illness at school.) These persons are “third
parties” within the context of health care law.
In specified circumstances, a third party (not the minor
and not the parent/guardian) may consent to medical
treatment on behalf of a minor. These circumstances are
discussed below.
THE CAREGIVER’S AUTHORIZATION AFFIDAVIT
A nonparent adult relative with whom a minor is living may
authorize medical and dental care (for which the minor
lacks authority to consent) for the minor by completing
and signing a “Caregiver’s Authorization Affidavit” (CHA
Form 2-2; form also found at ). The relative has the same
rights to authorize medical care as does a guardian (see
B.“Guardian Consent for Treatment of Minors,” page2.29).
It should be noted that this authority is not as extensive as
a parent’s authority when the treatment involved is surgical.
The law specifies that the relative may authorize mental
health treatment, except for involuntary commitment,
experimental treatment and convulsive treatment.
All of the following must apply for the authorization to
be valid:
1. The minor must be living with the adult family member.
“Living with” is not defined in the law, but presumably
would not include a minor who is temporarily visiting
an adult relative.
2. The adult must be a “qualified relative,” which is
defined in the law as a spouse, parent, stepparent,
brother, sister, stepbrother, stepsister, half-brother,
half-sister, uncle, aunt, niece, nephew, first cousin, or
any person denoted by the prefix “grand” or “great,”
or the spouse of any of the persons specified in this
definition, even after the marriage has been terminated
by death or divorce.
3. The adult must advise the parent(s) of the proposed
medical treatment and have received no objection
thereto, or the adult must be unable to contact
the parents.
4. The adult must complete a “Caregiver’s Authorization
Affidavit” (CHA Form 2-2 or similar form) in which he or
she attests that the elements outlined above are true
and correct.
The affidavit becomes invalid when the health care provider
learns that the minor no longer lives with the caregiver.
However, affidavits printed before Jan. 1, 2005, contain
the statement, “This affidavit is valid for only one year after
the date on which it is executed.” If a hospital is presented
with an affidavit containing this statement, and the one-year
time period has expired, the hospital should request that
the caregiver complete a new affidavit.
Health care providers who treat minors in good faith
reliance on the signed affidavit of a qualified relative are not
subject to criminal or civil liability or subject to professional
disciplinary action for such reliance if the applicable
portions of the affidavit are completed. Health care
providers have no obligation to make any further inquiry
or investigation.
Providers should be careful to require that the affidavit is
completed in its entirety, and that an attempt has been
made to reach the minor’s parents, prior to care being
delivered to the minor.
OTHER THIRD-PARTY CONSENT
Family Code Section 6910 permits a parent, guardian
or relative caregiver under the Caregiver’s Authorization
Affidavit to authorize someone else to consent to medical
or dental care for the minor. For purposes of this law, the
following definitions apply.
“Dental care” means X-ray examination, anesthetic, dental
or surgical diagnosis or treatment, and hospital care by a
dentist licensed under the Dental Practice Act [Family Code
Section 6901].

Chapter 2 — Principles of Consent for Mental Health Patients CHA
2.31
©CALIFORNIA HOSPITAL ASSOCIATION
“Medical care” means X-ray examination, anesthetic,
medical or surgical diagnosis or treatment, and hospital
care under the general or special supervision and upon the
advice of or to be rendered by a physician and surgeon
licensed under the Medical Practice Act [Family Code
Section 6902].
“Parent or guardian” means either parent if both parents
have legal custody, or the parent or person having legal
custody, or the guardian, of a minor [Family Code Section
6903].
This procedure should be used only when the minor is not
legally authorized to consent to his or her own treatment
and when the minor’s parents, guardians or caregiver under
the Caregiver’s Authorization Affidavit, are not available.
CHA has developed a form, “Authorization for Third-Party
Consent to Treatment of Minor Lacking Capacity to
Consent” (CHA Form 2-3) for parents to complete when
they wish to authorize another person to consent for health
care for their child.
The “Authorization for Third Party to Consent to
Treatment of Minor Lacking Capacity to Consent” (CHA
Form 2-3) also authorizes the hospital to surrender the
physical custody of a minor to the authorized agent(s)
of the parent(s) upon completion of treatment. Such an
authorization is required before the hospital may surrender
the physical custody of a minor who is not authorized to
give consent and who is under the age of 16 to someone
other than the minor’s parent, guardian, or caregiver
pursuant to the caregiver’s authorization affidavit. In
addition, the law requires the hospital to report such
releases [Health and Safety Code Section 1283].
Content and Form of Authorization
Written Authorization. The authorization must be in
writing. It may be prepared by a parent who has legal
custody or another person who has legal custody (e.g.,
guardian). There is no requirement that the authorization be
completed in the presence of hospital personnel or that it
be dated.
Authorized Third Person. The designated third person
may be any adult into whose care the minor has
been entrusted.
It is permissible to identify the authorized adult person
by title and employer rather than by name (e.g., Athletic
Coach, John F. Kennedy High School, Sacramento). The
treating health care provider should not be authorized as
a third party to consent to the treatment of a minor. (See
“Authorizing the Provider as the Third Party” below.)
Preference for CHA Form. The form “Authorization for
Third Party to Consent to Treatment of Minor Lacking
Capacity to Consent” (CHA Form 2-3) has been developed
to comply with Family Code Section 6910. While it is the
preferred authorization in content and form, a comparable
authorization signed by the parent(s) or guardian can
be used.
Recommended Procedure
Where an adult who is not the parent or guardian seeks
care for a minor with injury or illness which is not an
emergency, the provider should request a copy of the
parent’s authorization and include it in the minor’s medical
record. Even where third party authorization is provided,
it is prudent to attempt to contact the parent to confirm
consent, and to inform the parent of the status of the minor.
If the adult does not have a written authorization and
emergency care is not necessary, the provider should
contact the parent(s) or guardian to obtain consent for
treatment. If it is not possible to contact the parent(s)
or guardian, the provider should apply first aid, where
necessary, and consult with the adult regarding the
necessary steps to be taken for further care.
Neighbors, Sitters and Other Noninstitutional Child
Care Custodians
It is advisable that parents provide neighbors, adult
babysitters and others to whom they entrust their children,
a written authorization for consent to treatment along
with a list of emergency phone numbers. When such an
authorization is presented to a health care provider, an
attempt should be made to contact and confer with the
parents or other responsible person regarding the situation;
however, the minor would still be able to get medically
necessary care pursuant to the authorization.
When no authorization is provided and emergency care
is not necessary, the provider must contact the parent(s)
or guardian to obtain consent prior to treatment. If it is
not possible to contact the parent(s) or guardian, the
provider should apply first aid, if necessary, and consult
with the adult regarding the necessary steps to be taken for
further care.
Authorizing the Provider as the Third Party
Except for special circumstances addressed in the law
(e.g., interdisciplinary teams in long-term care facilities),
the treating health care provider should not be authorized
as a third party to consent to treatment of a minor. The
treating physician should discuss the situation and

CHA Mental Health Law Manual 2019
2.32
©CALIFORNIA HOSPITAL ASSOCIATION
proposed treatment with another person who is authorized
to consent.
Health care providers can best serve their communities by:
1. Educating parents in their service area about the
need to provide written authorizations for specified
third parties to give consent for medical treatment for
their children;
2. Developing model forms for parents to use that meet
the legal requirement for authorization to consent to
treatment of a minor; and
3. Providing local parents with the opportunity to keep a
record of information about their child’s basic health
history, medications, and emergency contacts at
the facility.
D. Special Situations Involving Minors Lacking
Legal Authority to Consent
MINORS PLACED FOR ADOPTION
Where an adoption agency has obtained a relinquishment
from the birth parent but the minor has not yet been legally
adopted, the adoption agency may consent to medically
necessary treatment.
Where the birth parents have not yet formally relinquished
the child for adoption, a continuing consent for
medical treatment should be obtained from the birth
parents. This may be done by completing the “Health
Facility Minor Release Report” (California Department
of Social Services form AD-22). This form may be
downloaded at www.dss.cahwnet.gov/cdssweb/entres/
forms/english/ad22.pdf.
CHILDREN OF MINOR PARENTS
The law requiring parental consent to treat minors makes
no distinction based on the age of the parent [Uniform
Parentage Act, Family Code Section 7600 et seq.]. Thus,
a minor parent may validly consent to medical or surgical
treatment for his or her child. However, the minor parent
must demonstrate the ability to understand the nature of
the treatment, its risks and benefits, and any alternatives
to the treatment, as with any situation requiring informed
consent (see B.“Capacity to Consent,” page2.37).
Therefore, a provider may determine that a minor parent
does not have the requisite maturity to make health care
decisions for his or her child. Typically, the minor parent will
authorize the grandparent to make health care decisions
on behalf of the child. However, where there is conflict
between the minor parent and other responsible adults, the
provider should seek legal advice.
In order to assure financial responsibility if the minor parent
is not emancipated or self-sufficient, the signature of some
responsible adult, such as the mother’s parents, also
should be obtained on the “Conditions of Admission” form
(CHA Form 8-1).
MINORS WHO ARE ALSO PARENTS
Since parenthood is not an emancipating event, an
unmarried minor parent who is living with his or her
parents or other responsible adult is not authorized under
the law to consent to his or her own medical treatment.
Thus, although it does not seem logical, a 14-year-old girl
living with her parents may not legally consent to her own
medical treatment (with those exceptions that apply to all
minors), but she may legally consent to medical treatment
for her baby.
MINORS WHO ARE ILL OR INJURED DURING SCHOOL
HOURS
When a minor is ill or injured during regular school hours,
reasonable medical treatment may be provided without
parental consent if the minor’s parent(s) or guardian cannot
be reached. This does not apply if the parent(s) or guardian
has filed with the school district a written objection to any
medical treatment other than first aid. [Education Code
Section49407] Treatment is limited to medical treatment
that is “reasonable” under the circumstances. This does not
include procedures involving significant risk or invasiveness.
The law provides immunity from liability to a school district,
officer of a school district, school principal, physician or
hospital treating any child in any school in any district. It
is not clear whether this law also applies when minors
attending private schools are treated.
Before relying on this law, however, a provider should
attempt to contact parents and determine whether a
written objection has been filed with the school (or the
school district). Schools typically have on file the name
and telephone number of a student’s parent or guardian
authorized to consent to medical treatment for the student.
NONABANDONED MINORS WHOSE PARENTS ARE
UNAVAILABLE
A minor may have parents who are unavailable. This
situation usually arises when the parents are incarcerated
or on a trip, or when the minor is away from home or in
the care or custody of law enforcement agencies, a camp,
sitter, foster home, foster parents pending adoption, and
the like.

Chapter 2 — Principles of Consent for Mental Health Patients CHA
2.33
©CALIFORNIA HOSPITAL ASSOCIATION
In such cases, the parents, guardian, or a legally authorized
caregiver may authorize a third party to consent to medical
treatment of the minor (see C.“Third-Party Consent for
Treatment of Minors,” page2.30). The third party must be
an adult, and the authorization must be in writing. [Family
Code Section 6910]
Also, as discussed below, Family Code Section 6911
provides that a superior court, upon a petition to the court
by a minor, may summarily grant consent if the parents of
a minor who is 16 years of age or older are unavailable to
provide consent.
COURT AUTHORIZATION: MINORS 16 YEARS OF AGE
OR OLDER
If the parents or guardian of a minor 16 years of age or
older are unavailable to consent to medical treatment that
requires their consent, a superior court may summarily
grant consent upon an application of the minor. The minor
must be a California resident. [Family Code Section 6911]
A copy of the court order should be obtained and placed in
the patient’s medical record before treatment is furnished
pursuant to the order. No fee is charged by the court for
proceedings under this law.
ABANDONED MINORS
It must first be established that the minor has been
abandoned or deserted by the parents. If so, the local
juvenile court or probation department should be contacted
for assistance.
Family Code Section 6911, regarding consent by the
superior court (discussed above), also applies under
these circumstances.
DEPENDENTS AND WARDS OF THE JUVENILE COURT
Under certain circumstances, a minor may be
adjudged either:
1. A dependent child of the juvenile court under Welfare
and Institutions Code Section 300 (a child in danger of
abuse or neglect); or
2. A ward of the juvenile court under Welfare and
Institutions Code Sections 601 (a disobedient or truant
child) or 602 (a child who has committed a crime).
After adjudication, parents are allowed to consent to health
care for the child, unless the court takes away that right.
A copy of the court order should be obtained, reviewed
carefully, and placed in the child’s medical record before
treatment is furnished. In addition, the court may authorize
medical treatment for the child. [Welfare and Institutions
Code Sections 362 (dependent) and 727 (ward)]
Even before a final adjudication is made, the court may
order medical treatment for a minor who is the subject of
a petition for dependent child or ward status if the parent/
guardian or other person who is authorized to consent is
unwilling or unable to consent to treatment and a written
recommendation for treatment has been obtained from a
physician [Welfare and Institutions Code Sections 369(b)
and 739(b)].
Psychotropic Medications
If a child is in the custody of the juvenile court (whether
as a dependent child or a ward) and the child has been
removed from the physical custody of the parent, only a
juvenile court judicial officer has the authority to order the
administration of psychotropic medications for the child.
However, the juvenile court may issue an order delegating
this authority to a parent upon finding that the parent poses
no danger to the child and has the capacity to authorize
the administration of psychotropic medications.
Court authorization for the administration of psychotropic
medication is based on:
1. The child’s overall mental health assessment and
treatment plan,
2. The rationale for the proposed medication (provided in
the context of past and current treatment efforts),
3. Other pharmacological and nonpharmacological
treatments that have been used and the child’s
response to those treatments,
4. A discussion of symptoms not alleviated or ameliorated
by other current or past treatment efforts, and
5. An explanation of how the psychotropic medication
being prescribed is expected to improve the child’s
symptoms.
The court and various state agencies have developed
policies and procedures and forms to implement this
requirement. The process includes periodic oversight by
the court of orders for psychotropic medications, facilitated
by the county social worker, public health nurse, or
other appropriate county staff. This oversight process is
conducted in conjunction with other regularly scheduled
court hearings and reports provided to the court by the
county child welfare agency. The forms to implement this
law are found at www.courts.ca.gov/forms.htm. (See
form JV-217-INFO, for information about the various
Judicial Council forms regarding consent for psychotropic
medications.)
For the purposes of this law, “psychotropic medications”
means medications administered for the purpose of
CHA Mental Health Law Manual 2019
2.34
©CALIFORNIA HOSPITAL ASSOCIATION
affecting the central nervous system to treat psychiatric
disorders or illnesses. These medications include, but are
not limited to, anxiolytic agents, antidepressants, mood
stabilizers, antipsychotic medications, anti-Parkinson
agents, hypnotics, medications for dementia, and
psychostimulants. [Welfare and Institutions Code Section
369.5 and 739.5]. (See B.“Antipsychotic Medications,”
page2.42, regarding consent to antipsychotic
medications.)
A copy of the applicable court order, if any, should be
obtained and placed in the medical record.
MINORS IN CUSTODY OF A SOCIAL WORKER OR
PROBATION OFFICER
Absent special circumstances, social workers and
probation officers do not have the authority to consent to
treatment for minors in their custody. The parents retain
this right. Exceptions to this general rule are described
below. In addition to the exceptions in the law described
below, the juvenile court may order that the social worker or
probation officer be given the power to authorize medical
treatment if the parent or guardian is unwilling or unable to
do so [Welfare and Institutions Code Sections 369(c) and
739(c)]. Many courts have issued “standing orders” that
give social workers and probation officers in the court’s
jurisdiction the right to consent for specified medical
treatment. Hospitals should consult their county juvenile
court for information.
Minor in Temporary Custody
If a minor is in temporary custody, a social worker or
probation officer may, upon recommendation of the
attending physician, authorize necessary medical treatment
if he or she first notifies the parent or guardian. If the parent
or guardian objects, treatment can be provided only upon
order of the court. [Welfare and Institutions Code Sections
369(a) and 739(a)]
Minor in Custody of Probation Officer
If the court has ordered the custody of a minor to be
under the supervision of a probation officer, the officer may
place the minor in the home of a relative. In that case, the
court may authorize the relative to consent for the minor’s
medical, surgical and dental care. [Welfare and Institutions
Code Section 727(a)(1)]
Providers who are caring for these minors must request a
copy of either the parent’s consent or an order from the
court authorizing treatment or specifying that the probation
officer or relative may consent on behalf of the minor.
Emergency
In an emergency situation, emergency medical, surgical
or dental treatment may be provided by a physician or
dentist, as appropriate, without a court order and upon
authorization of a social worker or probation officer. The
consent of a parent, guardian or other legally-authorized
person is not required, but reasonable efforts must be
made by the social worker or probation officer to obtain
such consent or at least to notify the parent(s) or guardian
prior to authorizing the treatment. [Welfare and Institutions
Code Sections 369(d) and 739(d)]
Minor Has Authority to Consent
For those treatments for which a minor can legally
provide his or her own consent, no court order or other
authorization is necessary.
MINORS IN CUSTODY OF FOSTER PARENTS
A child may become a “dependent child of the juvenile
court” (often referred to as a “foster child”) when the parent
is not properly caring for the child. This usually happens
after a complaint to a local child protective services agency
is investigated by a social worker. After investigating, the
social worker will do one of the following:
1. Not take any action, if there is no evidence of abuse or
neglect that requires court involvement.
2. Offer the parent services to help him or her learn how
to parent the child more safely.
3. Leave the child in the parent’s care and file a petition
with the court that asks to the court to open a case to
protect the child.
4. Take custody of the child from the parent and file a
petition with the court that asks the court to open a
case to protect the child. The social worker must file
the petition within two court days of removing the child.
The social worker may place the child with the other
parent (if they are separated), with a relative, or in a
foster home.
The parents retain the legal authority to consent to health
care on behalf of the child, unless a court order says
otherwise. In addition, foster parents may provide consent
in some circumstances.
A foster parent’s right to consent to treatment for a minor
depends upon whether the child has been placed with the
foster parent:
1. By court order or with the consent of the child’s legal
custodians; or

Chapter 2 — Principles of Consent for Mental Health Patients CHA
2.35
©CALIFORNIA HOSPITAL ASSOCIATION
2. On a temporary basis before a detention hearing has
been held.
Licensed foster care providers may consent to “ordinary”
medical and dental treatment for a minor placed with them
pursuant to a court order or with the voluntary consent
of the parent or guardian. “Ordinary” medical and dental
treatment includes, but is not limited to, immunizations,
physical examinations and X-rays [Health and Safety Code
Section 1530.6].
Foster parents who have custody of a child on only a
temporary basis prior to a detention hearing and court
ordered placement do not have this same authority.
Therefore, they do not have the right to consent to medical
treatment for the child under that law.
However, providers should look to the local juvenile court
for guidance in such situations. Many courts have issued
“standing orders” that give all foster parents in the court’s
jurisdiction the right to consent for specified medical
treatment. Hospitals should consult their county juvenile
court for information.
Written evidence of the foster parent’s authority (e.g., a
copy of a court order or the consent of the child’s parent
or guardian) should be obtained and placed in the child’s
medical record before proceeding with treatment. The
provider should consult legal counsel if questions arise
about consent for minors in the custody of foster parents.
MINORS WHO ARE SUSPECTED VICTIMS OF CHILD
ABUSE
Special Law for X-Rays
Health care providers are required to report suspected
cases of child abuse and neglect to law enforcement
officers. Chapter 11 contains detailed information about
child abuse reporting requirements as well as consent
for examination and treatment of suspected child
abuse victims.
A physician or dentist (or their agents at their direction)
may take skeletal X-rays of a child without the consent of
the child’s parent or guardian, but only for the purpose
of diagnosing the case as one of possible child abuse or
neglect and determining the extent of the abuse or neglect
[Penal Code Section 11171.2].
Additionally, if a peace officer in the course of investigation
of child abuse or neglect has reasonable cause to believe
that the child has been physically abused, the officer may
apply to a magistrate for an order directing that the child
be X-rayed without parental consent [Penal Code Section
11171.5]. X-rays performed pursuant to such an order must
be performed by a physician or dentist or their agents.
Reimbursement by the county for administrative costs of
these X-rays will not exceed 5 percent of the cost of the
X-rays.
Other Treatment
If further treatment beyond X-rays is necessary and the
parents object, the hospital should consult legal counsel. It
may be appropriate to seek a petition to declare the minor
a dependent child of the juvenile court under Welfare and
Institutions Code Section 300 for the purposes of assuring
that he or she receives the proper medical care.
If the minor has been raped or sexually assaulted, the minor
may give consent to medical treatment (see “Minor Victims
of Sexual Assault,” page2.41, and “Minor Rape Victims,”
page2.41).
MINORS RECEIVING MEDICATION ASSISTED
TREATMENT FOR OPIOID USE DISORDERS
An opioid treatment program (OTP) must be certified by
the U.S. Substance Abuse and Mental Health Services
Administration (SAMHSA) to dispense opioid drugs to treat
opioid use disorder. In addition, a practitioner who intends
to dispense opioid drugs to treat opioid use disorder must
first obtain from SAMHSA a certification that he or she is
qualified and will comply with SAMHSA rules.
An OTP must ensure that patients are admitted to
maintenance treatment by qualified personnel who have
determined, using accepted medical criteria such as those
listed in the Diagnostic and Statistical Manual for Mental
Disorders, that the person is currently addicted to an
opioid drug, and that the person became addicted at least
one year before admission for treatment. In addition, a
program physician shall ensure that each patient voluntarily
chooses maintenance treatment and that all relevant facts
concerning the use of the opioid drug are clearly and
adequately explained to the patient, and that each patient
provides informed written consent to treatment.
A person under 18 years of age is required to have had
two documented unsuccessful attempts at short-term
detoxification or drug-free treatment within a 12-month
period to be eligible for maintenance treatment. No person
under 18 years of age may be admitted to maintenance
treatment unless a parent, legal guardian, or responsible
adult designated by state law consents in writing to
such treatment.
“Maintenance treatment” means the dispensing of an
opioid agonist treatment medication at stable dosage levels
for a period in excess of 21 days in the treatment of an
individual for opioid use disorder.
[42 C.F.R. Sections 8.2, 8.11 and 8.12]

CHA Mental Health Law Manual 2019
2.36
©CALIFORNIA HOSPITAL ASSOCIATION
E. Minor’s Disagreement with Parent or Other
Legal Representative Regarding Treatment
Medical providers occasionally encounter situations in
which minors who do not have the legal authority to make
health care decisions indicate a desire to refuse treatment
that their parents or other legal representatives wish
them to have — or conversely, wish to have treatment
that their parents or other legal representatives decline.
Although minors are considered legally incompetent to
make decisions in many areas of medical care by virtue of
their age, nevertheless it is appropriate to discuss medical
decisions with them in a manner appropriate to their age.
Ascertainment of the child’s preference for treatment was
specifically approved in the case In re Christopher I. (see
“Dependents and Wards of the Juvenile Court,” page2.33).
A minor’s refusal to participate in mental health treatment
presents special challenges for the therapist and may make
treatment unproductive. A therapist is not required to treat
a minor who is voluntarily admitted or who is an outpatient
if the minor declines to cooperate, even if the parent(s) are
insistent. Minors who are involuntarily admitted have a right
to treatment (see D.“Special Situations Involving Minors
Lacking Legal Authority to Consent,” page2.32).
Providers should proceed cautiously in situations where
the minor disagrees with the parents or other legal
representatives, particularly if the treatment or refusal
involves a significant risk of serious adverse consequences.
Providers faced with such situations may wish to consider
the following.
MINOR’S AGE, MATURITY, AND EXPERIENCE WITH
THE TREATMENT IN QUESTION
Remember that the law permits minors as young as
12 years of age to consent to certain treatments. This
suggests that minors of that age may be in a position to
appreciate the risks and burdens of other treatments as
well, and may have reasonable grounds for wishing to
consent to, or refuse, such treatment.
DISAGREEMENT REGARDING THE TREATMENT
DECISION
The provider may be in a position to discuss the treatment
with the minor, clarify any confusion or misunderstanding,
and bring the matter into perspective. It may be helpful to
involve a social worker, psychologist, or other person with
a positive relationship with the minor to help resolve the
disagreement between the minor and the parents or other
legal representative.
If the provider is uncomfortable in providing treatment over
the minor’s objection, the provider may wish to reconsider
the clinical appropriateness of the treatment, or may
decline to participate in the case after taking appropriate
steps to transfer the care of the patient to another health
care provider. It may be appropriate to consult legal
counsel in such situations. Consultation with legal counsel
is strongly encouraged where refusal of care may cause
serious harm to the minor.
IX. MINORS WITH LEGAL AUTHORITY TO
CONSENT
A. Introduction
The California Legislature has enacted a series of laws,
discussed below, authorizing particular categories of
minors to consent to various medical services. Many of
these laws also include provisions relating to parental
notice and payment for the minor’s medical care. Minors
may be legally authorized to consent to their own medical
care in two different ways:
1. Because of their quasi-adult status (emancipated,
self-sufficient, on active duty in the military, or
married/previously married), or
2. Because of the type of treatment they are seeking
(pregnancy or contraceptive care, communicable
reportable disease, rape or sexual assault treatment,
etc.).
This section of the manual describes those circumstances.
Welfare and Institutions Code Section 14010 states that the
parents of a minor are not financially responsible for health
care or related services to which the minor may legally give
consent. (See C.“Financial Responsibility for Treatment of
Minors,” page2.25, for further information.)
Under state and federal law, a minor has a privacy right
in health information resulting from services to which
the minor is authorized to consent. This is true even
if, as a practical matter, the minor’s parent or guardian
actually gives consent. Thus, in order to ensure HIPAA
compliance and to avoid privacy breaches, providers must
also understand the instances in which a minor has legal
authority to consent to treatment. (See D.“Privacy Rights of
Minors,” page2.25, for additional information.)
A minor who would otherwise have the legal authority to
consent to medical treatment may not do so if he or she
does not understand the nature and consequences of
the proposed health care, including its significant benefits,

Chapter 2 — Principles of Consent for Mental Health Patients CHA
2.37
©CALIFORNIA HOSPITAL ASSOCIATION
risks, and alternatives (see B.“Capacity to Consent”
below). Legal counsel should be consulted if doubt
exists about whether a particular minor may consent to
medical treatment.
B. Capacity to Consent
Even where the law specifies that a minor is legally
authorized to consent to his or her own care, the doctrine
of informed consent requires that a determination be made
that, in fact, the minor has the capacity to make health
care decisions. California law defines capacity for adults in
the context of advance health care directives. “Capacity”
means that the person has the ability to understand the
nature and consequences of a decision and to make
and communicate a decision, and includes, in the case
of proposed health care, the ability to understand its
significant benefits, risks and alternatives [Probate Code
Section 4609]. The primary physician determines the
patient’s capacity to make health care decisions [Probate
Code Sections 4657 and 4658].
“Primary physician” means a physician designated by a
patient or the patient’s agent, conservator, or surrogate, to
have primary responsibility for the patient’s health care or, in
the absence of a designation or if the designated physician
is not reasonably available or declines to act as primary
physician, a physician who undertakes the responsibility
[Probate Code Section 4631].
There is no specific statute defining capacity for a
minor. Providers should consult the adult standard as a
guideline (see “Determination of Capacity,” page2.12). In
addition, providers may look to the mature minor doctrine,
applicable in other states (not in California), that suggests
that a minor who has reached a certain age (typically
14), and demonstrates an understanding of the risks and
benefits of a medical treatment, does not need parental
consent for such treatment, regardless of the minor’s
legal status. Under the mature minor doctrine, some key
considerations when working with minors who are seeking
treatment without the consent of a parent or other legal
representative are:
1. Does the minor understand the nature of the treatment,
its risks, benefits, and alternatives?
2. Does the minor appreciate the potential consequences
of the treatment and of foregoing treatment?
3. Can the minor make a reasoned decision based on the
information provided?
4. Is the proposed treatment for the benefit of the minor,
and not for the benefit of another person?
5. Is the proposed treatment medically necessary?
6. Does the treatment, or its consequences, involve
complex, high-risk medical care?
(See B.“The Evolution of the Rights of Minors,” page2.24,
for more information about the mature minor doctrine.)
If the minor has the legal authority to consent to his or her
own health care, the provider should take extra care to
explain, in terms that are understandable to the minor, the
elements necessary to making an informed decision about
the proposed treatment (see A.“Elements of Informed
Consent,” page2.5).
If a minor lacks the capacity to provide informed consent
to treatment which the law otherwise would allow, the
health care provider does not necessarily have the
authority or responsibility to contact the minor’s parents.
Communications with the minor, as with any adult patient,
are generally confidential and subject to medical privacy
laws. In such circumstances the health care provider
should attempt to obtain the agreement of the minor to
contact the parent or guardian. Legal counsel should be
consulted if the minor refuses and may forego necessary
medical care.
If a parent or other legal representative is providing
consent on behalf of a patient who lacks the capacity to
make a health care decision, the parent or other legal
representative must have the capacity to make health care
decisions.
C. Emancipation Pursuant to Court Order
A minor 14 years of age or older may petition the court
for emancipation. If the court grants the request, the
Department of Motor Vehicles will issue an identification
card that states that the minor is emancipated. The
provider should obtain a copy of the identification card and
place it in the patient’s medical record. A person who, in
good faith, examines a minor’s identification card and relies
on a minor’s representation that he/she is emancipated, will
be protected under the law [Family Code Sections 7120,
7140 and 7141].
An emancipated minor may consent to his or her own
medical, dental or psychiatric care without parental
consent, knowledge, or liability [Family Code Sections 7002
and 7050(e)(1)].
However, the parents of an emancipated minor who is
living in the home of the parent(s) may be responsible
for the minor’s medical expenses, with the exception of

CHA Mental Health Law Manual 2019
2.38
©CALIFORNIA HOSPITAL ASSOCIATION
services described in Family Code Sections 6924 through
6929 (see CHA Appendix 2-B, “Consent Requirements
for Medical Treatment of Minors,” for a description of what
these services are) [Welfare and Institutions Code Section
14010(b)]. Hospitals should be aware of the privacy rights
of such minors and obtain the minor’s consent prior to
sending the parents a bill (see C.“Financial Responsibility
for Treatment of Minors,” page2.25).
If the minor does not have an identification card, the
facility should determine if he or she is self sufficient under
Family Code Section 6922 (see D.“Self-Sufficient Minors,”
page2.38) and, therefore, capable of granting a valid
consent under that law.
D. Self-Sufficient Minors
A self-sufficient minor is legally authorized to consent
to medical or dental care without parental or guardian
consent, knowledge, or financial liability. To be considered a
self-sufficient minor, the minor must:
1. Be 15 years of age or older;
2. Be living separate and apart from his or her parent(s)
or legal guardian, whether with or without the consent
or acquiescence of his or her parent(s) or legal
guardian. The duration of the separate residence is
irrelevant; and
3. Be managing his or her financial affairs, regardless of
the source of income.
[Family Code Section 6922]
A health care provider should make a good faith attempt to
determine whether the above requirements are met. While
a provider may be able to verify the minor’s age (e.g., by
reference to a driver’s license, school identification card, or
birth certificate), the other requirements are more difficult
to verify. A health care provider may ask questions to help
determine whether the minor is living separate and apart
from his parents or is managing his or her financial affairs,
but it may be difficult to verify the truthfulness of the minor’s
answers. Furthermore, the law provides no guidance
whatsoever to making those determinations. For example,
the law does not specify that the minor must have a job or
a bank account to be considered self-sufficient — or that
if the minor has a job or bank account, this demonstrates
that he or she is self-sufficient. Providers are advised to
make a good faith effort to determine whether the minor
meets the requirements listed above, and document the
information obtained from the minor thoroughly.
DEFINITIONS
“Medical care” means “X-ray examination, anesthetic,
medical or surgical diagnosis or treatment, and hospital
care” under the supervision and upon the advice of a
licensed physician [Family Code Section 6902].
“Dental care” means “X-ray examination, anesthetic, dental
or surgical diagnosis or treatment, and hospital care” by a
licensed dentist [Family Code Section 6901].
Psychiatric care is not explicitly included within the
definition of “medical care” to which a self-sufficient minor
may consent. Because the definition of health care to which
an emancipated minor may consent explicitly discusses
psychiatric care, and because there is a statute that
explicitly discusses minor consent to outpatient psychiatric
care, an argument may be made that a self-sufficient minor
may not consent to psychiatric care pursuant to Family
Code Section 6922. A health care facility should consult its
own legal counsel regarding the advisability of permitting a
self-sufficient minor to consent to his or her own inpatient
psychiatric care (or outpatient care if the requirements
of Family Code Section 6924 or Health and Safety Code
Section 124260 do not apply). (See G.“Minors in Need of
Outpatient Mental Health Treatment or Residential Shelter
Services,” page2.39, regarding consent by minors to
outpatient mental health treatment.)
DOCUMENTATION
The minor should affirm that the above conditions are
met and complete the “Self-Sufficient Minor Information”
(CHA Form 2-1). In the absence of evidence to the
contrary, the hospital may reasonably believe that the
affirmations made in CHA Form 2-1 are correct without
independent verification.
NOTIFYING PARENT/GUARDIAN
The treating physician may inform a self-sufficient minor’s
parent(s) or guardian of the treatment given or needed with
or without the minor’s consent, if the minor has told the
physician where the parents or guardian may be contacted.
[Family Code Section 6922(c)] However, this authority
should be exercised with caution and with due respect for
the minor’s privacy rights.
E. Minors on Active Duty with U.S. Armed Forces
A minor, regardless of age, while serving on active duty with
any branch of the U.S. armed services is emancipated and
may consent to medical, dental, or psychiatric care without

Chapter 2 — Principles of Consent for Mental Health Patients CHA
2.39
©CALIFORNIA HOSPITAL ASSOCIATION
parental consent, knowledge, or liability [Family Code
Sections 7002 and 7050(e)(1)]. The hospital may wish to
photocopy the patient’s active duty military identification
card and include it in the medical record.
F. Married or Previously Married Minors
A minor who has entered into a valid marriage or domestic
partnership, whether or not it was later terminated by
dissolution (divorce) or death of the spouse or partner,
is emancipated and may consent to medical, dental or
psychiatric care without parental consent, knowledge, or
liability [Family Code Sections 7002 and 7050(e)(1)].
The provider may wish to require a person under 18 years
of age who claims that he or she is or was married or in a
domestic partnership to present a copy of the marriage or
domestic partnership certificate.
California does not recognize so-called “common
law” marriages.
G. Minors in Need of Outpatient Mental Health
Treatment or Residential Shelter Services
A minor 12 years of age or older may consent to mental
health treatment or counseling on an outpatient basis or to
residential shelter services if:
1. He or she is, in the opinion of the attending
professional person, mature enough to participate
intelligently in the outpatient services or residential
shelter services; and
2. The minor would present a danger of serious physical
or mental harm to self or to others without the mental
health treatment or counseling or residential shelter
services, or the minor is the alleged victim of incest
or child abuse. This requirement need not be met
with respect to mental health treatment or counseling
services (it still applies to residential shelter services);
however, Medi-Cal may not cover these services
unless this requirement is met. (See C.“Financial
Responsibility for Treatment of Minors,” page2.25.)
[Family Code Section 6924; Health and Safety Code
Section 124260]
However, this law does not allow minors to consent to
convulsive therapy, psychosurgery or psychotropic drugs.
Psychotropic drugs include antidepressants, antianxiety
medications, antipsychotics, and other medications
commonly prescribed for mental health patients.
DEFINITIONS
“Mental health treatment or counseling services” means
the provision of such services on an outpatient basis by any
of the following:
1. A governmental agency.
2. A person or agency having a contract with a
governmental agency to provide the services.
3. An agency that receives funding from community
united funds.
4. A runaway house or crisis resolution center.
5. A professional person (as defined below).
A “professional person” includes a psychiatrist, clinical
psychologist, marriage and family therapist, licensed
educational psychologist, credentialed school psychologist,
licensed professional clinical counselor, licensed clinical
social worker, and others [Family Code Section 6924(a)
(2); Health and Safety Code Section 124260(a)(2); Title 9,
California Code of Regulations, Sections 622-626].
“Residential shelter services” means the provision of
residential and other support services to minors on a
temporary or emergency basis in a facility that services
only minors by a governmental agency, a person or agency
having a contract with a governmental agency to provide
these services, an agency that receives funding from
community funds, or a licensed community care facility
or crisis resolution center. Residential shelter services
also include other support services on a temporary or
emergency basis by a professional person.
PARENTAL INVOLVEMENT/LIABILITY
The consent of the parent(s) or guardian for mental health
treatment or counseling is not necessary and they will
not be liable for payment for the minor’s care unless they
participate, and then only for the services rendered with
such participation. The minor’s parent(s) or guardian must
be given the opportunity to participate in the treatment or
counseling unless the professional person who is providing
the treatment or counseling deems it inappropriate. The
professional person must consult with the minor prior to
making this determination. (This law does not require the
professional to cease treating a minor if the parents are
contacted but refuse to participate in and/or object to
the minor’s receiving such treatment.) The professional
responsible for treating the minor must document in the
patient’s record whether and when he or she attempted to
contact the minor’s parent(s) or guardian, whether or not
they were contacted, or the reason why it would not be
appropriate to contact the parent(s) or guardian.

CHA Mental Health Law Manual 2019
2.40
©CALIFORNIA HOSPITAL ASSOCIATION
A professional person offering residential shelter services,
whether as an individual or as a representative of an entity,
must make his or her best efforts to notify the parent or
guardian of the provision of services. The minor’s parents
or guardian are not liable for payment for residential
shelter services unless they consent to the provision of
those services.
PRIVACY IMPLICATIONS
Under state and federal law, a minor has a privacy right
in health information resulting from services to which the
minor is authorized to consent. This is true even if, as a
practical matter, the minor’s parent or guardian actually
gives consent. Thus, a parent may take his adolescent
child to a private therapist for treatment of an eating
disorder. Even though the parent or guardian solicits
and consents to the services, privacy laws prevent the
therapist from disclosing health information to the parent
or guardian (without the minor’s authorization) because,
under state law, the minor could have obtained those
services independent of the parent or guardian, and the
minor has not requested that the parent or guardian be
treated as the minor’s personal representative under
the Health Insurance Portability and Accountability Act
(HIPAA). Both the Confidentiality of Medical Information Act
and HIPAA contain an exception to privacy requirements to
permit disclosure of limited information to a family member
if the information is directly relevant to the family member’s
involvement with the patient’s care. However, there are
limitations on this exception (see I.“Minor’s Medical
Records,” page6.12, and E.“Family and Friends: Patients
Covered by CMIA,” page6.7). In addition, this exception
does not apply to records and information covered by
the Lanterman-Petris-Short Act. [45 C.F.R. Sections
164.502(g) and 164.510(b); Civil Code Sections 56.11(c) and
56.1007; Health and Safety Code Sections 123110 and
123115; Welfare and Institutions Code Section 5328]
LIMITATIONS
This law does not authorize a minor to receive convulsive
therapy, psychosurgery, or psychotropic drugs without
the consent of his parent(s) or guardian according to the
appropriate legal requirements. (See X.“Treatments That
Require Special Consent,” page2.42.)
H. Minors with Drug- or Alcohol-Related
Problems
A minor 12 years of age or older may consent to medical
care and counseling relating to the diagnosis and treatment
of a drug- or alcohol-related problem. “Counseling” is
defined, for the purposes of this law, as the provision of
counseling services by a provider under a contract with
the state or a county to provide alcohol or drug abuse
counseling services. “Medical care” is defined, for the
purposes of this law, as X-ray examination, anesthetic,
medical or surgical diagnosis or treatment, as well as
hospital care under the supervision of a physician. [Family
Code Sections 6902 and 6929]
The consent of the minor’s parent(s) or guardian is not
necessary and they will not be liable for payment of
the minor’s care unless they participate in a counseling
program related to such treatment. The minor’s parent(s)
or guardian must be given the opportunity to participate
in the treatment or counseling unless the professional
who is providing the treatment or counseling deems it
inappropriate. (This law does not require the professional
to cease treating the minor if the parents are contacted but
refuse to participate and/or object to the minor’s receiving
such treatment.) The professional responsible for treating
the minor must document whether and when he or she
tried to contact the minor’s parent(s) or guardian, whether
or not they were contacted, or the reason why it would not
be appropriate to contact the parents or guardian.
“Professional person” means a physician and surgeon,
registered nurse, psychologist, clinical social worker,
marriage and family therapist, marriage and family
therapist registered intern (when appropriately employed
and supervised pursuant to Business and Professions
Code Section 4980.43), psychological assistant (when
appropriately employed and supervised pursuant to
Business and Professions Code Section 2913), associate
clinical social worker (when appropriately employed
and supervised pursuant to Business and Professions
Code Section 4996.18), or associate professional clinical
counselor (when appropriately employed and supervised
pursuant to Business and Professions Code Section
4999.42).
The law explicitly states that a parent or guardian has the
right to seek medical care and counseling for the drug-
or alcohol-related problem of a minor, even if the minor
does not consent to the medical care and counseling
[Family Code Section 6929(f)]. However, if a provider is
uncomfortable treating a minor without his or her consent,
the provider need not do so.
This law does not authorize a minor to receive replacement
narcotic abuse treatment (such as methadone,
levo-alpha-acetylmethadol (LAAM) or buprenorphine
products) without the consent of his or her parent(s) or
guardian [Family Code Section 6929(e)].

Chapter 2 — Principles of Consent for Mental Health Patients CHA
2.41
©CALIFORNIA HOSPITAL ASSOCIATION
The law explicitly states that where the parent or guardian
has sought medical care and counseling for a drug- or
alcohol-related problem, and the minor receives the care
sought, the physician must disclose medical information
regarding such care to the minor’s parents or guardian
upon their request, even where the minor objects [Family
Code Section 6929(g)]. (However, where the care is
provided in a federally-assisted substance use disorder
program, federal law requires the minor’s consent prior
to release of any patient information.) There is no liability
for such disclosure. This law does not explicitly permit a
hospital or practitioner other than a physician to disclose
information in such circumstances; therefore, it is
recommended that requests for information from a minor’s
parents or guardian be directed to the minor’s physician.
Health and Safety Code Section 1607.5 permits a minor 17
years of age or older to consent to blood donation. A minor
between the ages of 15 and 17 may consent to blood
donation, but the blood bank may accept such donation
only with the written consent of the minor’s parent(s) or
guardian and the written authorization of a physician.
A minor who is at least 15 years of age may make an
anatomical gift with the written consent of a parent or
guardian [Health and Safety Code Section 7150.15].
I. Minors Consenting to Other Procedures
MINORS RECEIVING PREGNANCY OR CONTRACEPTIVE
CARE
A minor, regardless of age or marital status, may consent
to hospital, medical, or surgical care related to treatment
or prevention of pregnancy [Family Code Section 6925].
While the law does not specify the medical treatments that
come within this authorization, it is generally assumed that
contraceptive care (including emergency contraceptive
drugs), abortion, pelvic exams, pregnancy testing, and
prenatal care are medical procedures related to treatment
or prevention of pregnancy. However, this law does not
apply to sterilization procedures.
COMMUNICABLE REPORTABLE DISEASES
When a minor 12 years of age or older may have come into
contact with an infectious, contagious, or communicable
disease that must be reported to the local health officer, or
a related sexually transmitted disease, the minor is able
to consent to medical care related to the diagnosis or
treatment of the disease [Family Code Section 6926]. (See
Title 17, California Code of Regulations, Section 2500(j),
for a list of reportable diseases.) This provision of law
authorizes minors to consent to HIV tests (see “Minors 12
and Older,” page2.56).
In addition, a minor who is 12 years of age or older may
consent to medical care related to the prevention of a
sexually transmitted disease. This provision authorizes
minors to consent to, or refuse to consent to, the
HPV vaccine.
MINOR RAPE VICTIMS
A minor 12 years of age or older who has allegedly been
raped may consent to the furnishing of hospital, medical,
and surgical care related to the diagnosis or treatment of
such condition. This includes access to the “morning after”
pill [Brownfield v. Daniel Freeman Marina Hospital, 208
Cal.App.3d 405(1989)]. The minor may also consent to
the collection of evidence with regard to the alleged rape.
The consent of the minor’s parent(s) or guardian is not
necessary. [Family Code Section 6927; Title 11, California
Code of Regulations, Section 925]
A minor who has been raped has also been sexually
assaulted, according to the legal definitions. It is unclear
why California law contains two different laws pertaining
to these victims (Family Code Sections 6927 and 6928,
which is discussed below). The only difference in the two
laws is that Family Code Section 6928 (regarding sexual
assault) requires the professional person providing medical
treatment to a minor victim of sexual assault to try to
contact the minor’s parent/guardian (unless the treating
professional person reasonably believes the parent/
guardian was the perpetrator). CHA recommends that the
treating professional talk to the minor sexual assault victim
about contacting the parent, and then contact the parent
unless the minor voices significant concern. This discussion
and the outcome should be documented.
NOTE: Providers are required to report cases of alleged
or suspected rape or sexual assault of a minor to local law
enforcement (see chapter 7).
MINOR VICTIMS OF SEXUAL ASSAULT
A minor who has allegedly been sexually assaulted
may consent to the furnishing of hospital, medical, and
surgical care related to the diagnosis and treatment of
such condition. Sexual assault includes, but is not limited
to, rape, sodomy, or oral copulation. The minor may also
consent to collection of medical evidence with regard to the
alleged sexual assault. The consent of the minor’s parent(s)
or guardian is not necessary. [Family Code Section 6928;
Title 11, California Code of Regulations, Section 925]

CHA Mental Health Law Manual 2019
2.42
©CALIFORNIA HOSPITAL ASSOCIATION
The professional person providing the medical treatment
must attempt to contact the minor’s parent(s) or guardian
and note the date and time of such contact or, if
unsuccessful, when contact was attempted. However,
the professional person need not make this contact if he
or she reasonably believes that the parent(s) or guardian
committed the sexual assault on the minor. [Family Code
Section 6928; Title 11, California Code of Regulations,
Section 925]
NOTE: Providers are required to report cases of alleged
or suspected rape or sexual assault of a minor to local law
enforcement (see chapter 7).
MINOR VICTIMS OF INTIMATE PARTNER VIOLENCE
A minor 12 years of age or older and who states he or
she was injured as a result of intimate partner violence
may consent to medical care related to the diagnosis or
treatment of the injury as well as the collection of evidence.
“Intimate partner violence” means an intentional or
reckless infliction of bodily harm perpetrated by a person
with whom the minor has or has had a sexual, dating, or
spousal relationship.
The law states that if a report is made under Penal Code
Section 11160 (see III.“Reporting Injuries by Firearm or
Assaultive or Abusive Conduct (“Suspicious Injuries”),”
page7.3), the provider must:
1. Inform the minor that the report will be made, and
2. Attempt to contact the minor’s parent or guardian and
inform them of the report. The provider must document
in the minor’s medical record the date and time of the
attempt to contact the parent or guardian, and whether
the attempt was successful or unsuccessful. However,
this paragraph does not apply if the provider believes
the minor’s parent or guardian committed the intimate
partner violence.
The law does not say whether the above steps must be
taken if a child abuse report is made. (See chapter 7 for
detailed information about suspicious injury and child
abuse reports.)
[Family Code Section 6930]
NOTE: If the minor is allegedly a victim of rape or sexual
assault, the provider should follow the laws described
under “Minor Rape Victims,” page2.41 or “Minor Victims
of Sexual Assault,” page2.41, instead of this law. This
law likely applies to physical violence that is not sexual
in nature.
J. Summary of Consent Requirements Regarding
Minors
CHA has included a table at the end of this manual
titled “Consent Requirements for Medical Treatment of
Minors” (CHA Table 2-B) summarizing consent issues
regarding minors.
X. TREATMENTS THAT REQUIRE SPECIAL
CONSENT
A. Background
As discussed in II.“Why Consent is Necessary,” page2.1,
California law imposes a duty on physicians to obtain
the patient’s informed consent for a complex procedure.
[Cobbs v. Grant, 8 Cal.3d 229 (1972)] To enable a patient
to make an informed decision about whether to consent to
a procedure, the law requires the physician to explain to the
patient the nature of the proposed treatment; its expected
benefits and effects; its possible risks and complications;
any alternative forms of treatment; their benefits, risks and
complications; and any potentially conflicting interests
(such as research or financial interests) the physician
may have.
The physician generally has discretion to determine the
types of information to provide a patient. However, the
California Legislature, regulatory agencies, and the
courts have imposed special requirements with respect
to the information to be given to a patient in several
circumstances. This chapter details those requirements that
may affect mental health facilities. A complete list of these
circumstances (for example, hysterectomy, sterilization,
reuse of hemodialysis filters, etc.) may be found in chapter
4 of CHA’s Consent Manual.
B. Antipsychotic Medications
This section of the manual describes the laws related to
consent for antipsychotic medications given to mental
health patients, both voluntary and involuntary, in acute
psychiatric hospitals and in psychiatric units of general
acute care hospitals. Skilled nursing facility residents and
inmates in county jails and state prisons are protected by
different laws (see Health and Safety Code Section 1418.9;
Penal Code Sections 2602 and 2603; Title 22, California
Code of Regulations, Sections 72082, 72092 and 72828).
Specific procedures must be followed with respect to
the administration of antipsychotic medications to both
voluntary and involuntary patients. This section describes

Chapter 2 — Principles of Consent for Mental Health Patients CHA
2.43
©CALIFORNIA HOSPITAL ASSOCIATION
these requirements. If a use of an antipsychotic medication
falls within the definition of a drug used as a restraint, the
requirements that apply to the use of restraints should also
be followed (see chapter 5).
“Antipsychotic medication” is defined as any drug
customarily used for the treatment of symptoms of
psychoses and other severe mental and emotional
disorders [Welfare and Institutions Code Section 5008(l);
Title 9, California Code of Regulations, Section 856].
VOLUNTARY PATIENTS
Who May Refuse Antipsychotic Medications
Every person admitted as a voluntary patient to a facility
for psychiatric evaluation or treatment has the right to
refuse the administration of antipsychotic medications.
This includes state and county hospitals, private acute
psychiatric hospitals, skilled nursing facilities, and general
acute care hospitals that provide psychiatric services.
However, for this purpose, a voluntary patient does
not include:
1. Voluntary minor patients, unless the minor is otherwise
authorized by law to seek and consent to treatment for
mental illness; or
2. Conservatees (defined in Welfare and Institutions
Code Section 5350 et seq.) whose conservators have
been given the right to require their conservatees to
receive treatment related specifically to remedying or
preventing the recurrence of the conservatees’ being
gravely disabled.
[Title 9, California Code of Regulations, Section 850]
The right to consent to, or to refuse, antipsychotic
medications on behalf of a voluntary minor patient who is
not authorized by law to consent to his or her own mental
health treatment devolves to the parent, guardian, or other
legal representative.
Although not specifically required by law, it is recommended
that the procedures described below for obtaining and
documenting informed consent for the administration of
antipsychotic medications to voluntary patients be followed
to obtain such consent from a parent or guardian of a
voluntary minor patient who is not authorized by law to
consent to the treatment, and from a conservator who has
the right to require the conservatee to receive the treatment.
Informed Consent of Voluntary Patient Generally
Required
A voluntary patient may be treated with antipsychotic
medications only after being informed of the right to
accept or refuse the medications and consenting to the
administration of the medications [Title 9, California Code
of Regulations, Section 851].
Although not specifically required by law, it is recommended
that the procedures described below for obtaining and
documenting informed consent for the administration of
antipsychotic medications to voluntary patients be followed
to obtain such consent from a parent or guardian of a
voluntary minor patient who is not authorized by law to
consent to the treatment, and from a conservator who has
the right to require the conservatee to receive the treatment.
To make an informed decision, the patient must be
provided sufficient information by the physician who
prescribes the medications. The information must include
the following and should be presented in the patient’s
native language, if possible:
1. The nature of the patient’s mental condition.
2. The reason for taking the medication, including the
likelihood of the patient’s improving or not improving
without the medication.
3. A statement that the patient may withdraw his or her
consent at any time. The patient should be advised
that he or she may withdraw the consent by stating
such intention to any member of the treating staff.
4. The reasonable alternative treatments available, if any.
5. The name and type of medication, range of frequency
of administration, range of dosage amount (including
the use of PRN orders), method of administration (oral
or injection) and duration of taking the medications.
6. The probable side effects of the medication that are
known to commonly occur and any particular side
effects likely to occur to the particular patient.
7. The possible additional side effects that may occur
in patients taking the medication longer than three
months. If applicable, the patient must be advised
that side effects may include persistent involuntary
movement of the face or mouth and might also include
similar movement of the hands and feet, and that
these symptoms of tardive dyskinesia are potentially
irreversible and may appear after the medication has
been discontinued.
8. The right to refuse the medication.

CHA Mental Health Law Manual 2019
2.44
©CALIFORNIA HOSPITAL ASSOCIATION
CHA has developed a form, “Consent to Receive
Antipsychotic Medications” (CHA Form 4-7), that may be
used to provide this information to the patient.
Documentation Requirements
The facility must maintain a written record of each voluntary
patient’s decision to consent to receive antipsychotic
medications. The written record must be a written consent
form signed by the patient indicating that each item
listed above has been discussed with the patient by the
prescribing physician. “Consent to Receive Antipsychotic
Medications” (CHA Form 4-7) complies with the applicable
regulations.
If a voluntary patient has been shown but does not wish
to sign the written consent form, it is sufficient for the
physician to place the unsigned form in the patient’s
medical record that is maintained by the facility, together
with a note indicating that while the patient understands
the nature and effect of antipsychotic medications and
consents to these, the patient does not wish to sign a
written consent form. Space has been provided on the
“Consent to Receive Antipsychotic Medications” form
for such a note. [Title 9, California Code of Regulations,
Section 852]
Exception for Emergency Situations
A physician may administer antipsychotic medications
without consent, if it is impracticable to obtain patient
consent, in emergency situations where:
1. There is a sudden marked change in the patient’s
condition which necessitates immediate action in order
to preserve the life of the patient or others, or
2. To prevent serious bodily harm to the patient or others.
If antipsychotic medication is administered during an
emergency, the medication should be only that which is
required to treat the emergency condition and must be
provided in ways that are least restrictive of the personal
liberty of the patient. [Title 9, California Code of Regulations,
Section 853]
Withdrawal of Consent
A voluntary patient may withdraw consent to the
administration of antipsychotic medications at any time by
stating such intention to any member of the treatment staff
[Title 9, California Code of Regulations, Section 854].
Consequence of Refusal to Consent
The refusal of the patient to consent to the administration
of antipsychotic medications does not, in itself, constitute
sufficient grounds for initiating an involuntary commitment
[Title 9, California Code of Regulations, Section 855].
Guidelines developed by the former California Department
of Mental Health indicate that physicians must exercise
professional judgment to determine which methods of
treatment are available and best suited for individual
patients. If a voluntary patient refuses to consent to
antipsychotic medications, the prescribing physician
might consider:
1. Negotiating with the patient regarding the use of
antipsychotic medications; or
2. Using an alternative method of treatment; or
3. Discharging the person if no other form of treatment is
suitable or available.
If none of the above is a viable alternative, and if (and
only if) the patient meets the requirements for involuntary
detention, then the patient may be involuntarily detained in
an appropriate facility. (See chapter 3 regarding involuntary
detention.)
Violation Reports and Available Remedies
All alleged or suspected violations of the rights of patients
as listed in the law must be reported to the county patients’
rights advocate or, for state hospital patients, to the state
hospital patients’ rights advocate, who must report all
complaints to the director of the California Department
of State Hospitals. The director must take appropriate
action which, depending on the nature of the complaint,
could include:
1. Referral for disciplinary action to the facility governing
body for review and monitoring.
2. Referral to the Medical Board of California regarding a
review of the individual practitioner’s license.
3. Referral for review of the facility license.
4. Compelling negotiations to ensure compliance with
these regulations, withholding part or all of state
mental health funds or taking appropriate court action.
The individual patient may also seek any other remedies
that are available under the law. [Title 9, California Code of
Regulations, Section 857]
INVOLUNTARY PATIENTS
In a 1988 lawsuit, Riese v. St. Mary’s Hospital and Medical
Center, 209 Cal.App.3d 1303 (1987, modified 1988), the
California Supreme Court held that involuntary patients
must not be given antipsychotic medications without their

Chapter 2 — Principles of Consent for Mental Health Patients CHA
2.45
©CALIFORNIA HOSPITAL ASSOCIATION
informed consent unless there is an emergency or a court
has determined that the patient is incompetent to make
an informed decision concerning medication. In 1991 the
California Legislature enacted a law which slightly modified
the Riese holding, allowing involuntary patients to be given
antipsychotic medications without their informed consent in
certain situations:
1. If they do not refuse the medication following
disclosure of the pertinent information
discussed below;
2. In an emergency; or
3. If a court has determined that the patient
lacks capacity to make an informed decision
concerning medication.
[Welfare and Institutions Code Section 5332]
This statutory scheme applies to patients detained under
Welfare and Institutions Code Sections 5150 (72-hour
hold), 5250 (14-day hold), 5260 (additional 14-day hold for
persons imminently suicidal), or 5270.15 (additional 30-day
hold for persons gravely disabled) [Welfare and Institutions
Code Section 5325.2]. When a patient is detained under
one of these laws, the agency or facility providing the
treatment must obtain the patient’s medication history if
possible [Welfare and Institutions Code Section 5332(d)].
Requirements for Administering Antipsychotic
Medication
Antipsychotic medications may be given to involuntary
psychiatric patients only if one of the following conditions is
met:
1. The patient has given informed consent;
2. The patient has been given the information discussed
below and he or she has not refused the medication;
3. An emergency condition exists; or
4. A court order of incapacity has been issued.
(See below for further explanation of each condition.)
Patient Gives Informed Consent
Informed consent requires that a full explanation of the
proposed course of treatment be given to the patient. This
includes discussing the elements described in “Informed
Consent Forms That Contain Medical Information,”
page2.7.
If the patient agrees with the administration of the
medication, he or she should sign a form indicating that
the patient has received the information desired from
a physician and has consented to the medication. The
“Consent to Receive Antipsychotic Medications” form (CHA
Form 4-7) has been developed for this purpose. The signed
form should be placed in the medical record and a copy
given to the patient.
As with any consent to medical treatment, the patient is
free to withdraw consent at any time during the course
of treatment.
The Patient is Given the Necessary Information and
Does Not Refuse the Medication
Antipsychotic medication may be administered to an
involuntary patient if the patient is given the information
discussed in “Informed Consent of Voluntary Patient
Generally Required,” page2.43, and does not refuse
the medication, even if the patient does not expressly
agree to the administration of the medication [Welfare and
Institutions Code Section 5332(a)]. The patient should sign
a form indicating that he or she has received the necessary
information. The “Consent to Receive Antipsychotic
Medications” form (CHA Form 4-7) may be used for this
purpose.
If the patient does not refuse the medication, but does not
wish to sign the form, a note to this effect should be written
on the form or in the medical record and signed by the
person who gives the patient the necessary information. If
the form is used, it should be placed in the medical record
and a copy given to the patient.
The patient may later refuse the administration of
antipsychotic medication, in which case no medication may
be administered unless an emergency exists or an order of
incapacity is issued by a judge.
Exception for Emergency Situations
Antipsychotic medication may be administered to an
involuntary patient despite the patient’s objection if an
emergency exists. An emergency is defined for this
purpose as a situation in which action to impose treatment
over the person’s objection is immediately necessary for
the preservation of life or the prevention of serious bodily
harm to the patient or others, and it is impracticable to first
obtain consent. It is not necessary for harm to take place
or become unavoidable prior to treatment. [Welfare and
Institutions Code Section 5008(m)]
The emergency exception justifies administration of
antipsychotic medications over the patient’s objection
only so long as the emergency condition exists. Once the
condition is stabilized, the patient’s informed consent (or
lack of refusal after the necessary information is given) is
again required. In addition, the medication administered

CHA Mental Health Law Manual 2019
2.46
©CALIFORNIA HOSPITAL ASSOCIATION
in emergencies must be only that required to treat the
emergency condition and must be provided in the manner
least restrictive to the personal liberty of the patient
[Welfare and Institutions Code Section 5332(e)].
Judicial Determination of Incapacity
Antipsychotic medication may be administered over the
patient’s objection in nonemergency situations only if:
1. The treatment staff has determined that treatment
alternatives to involuntary medication are unlikely to
meet the needs of the patient, and
2. A judicial determination of incapacity to refuse the
treatment has been made after a hearing.
[Welfare and Institutions Code Section 5332(b)]
Scope of Hearing. The purpose of the hearing is for the
judge or hearing officer to determine whether the patient
has the capacity to make an informed decision regarding
the proposed treatment. The purpose of the hearing is
not for the judge or hearing officer to decide medical
questions such as whether the patient needs antipsychotic
medication. This issue, if discussed in the hearing, is
pertinent only to help the judge or hearing officer decide if
the patient’s thought processes related to making decisions
regarding treatment are rational or not.
Procedure for Initiating Hearing. If a hospital wishes
to administer antipsychotic medication to an involuntary
patient over the patient’s objection in nonemergency
situations, the hospital must file a petition for a capacity
hearing with the superior court [Welfare and Institutions
Code Section 5333(b)]. The director of the treatment facility
or a designee must:
1. Deliver a copy of the notice of the filing of the petition
along with a copy of the petition to the patient and the
patient’s advocate or counsel;
2. Inform the patient of his or her legal right to a capacity
hearing; and
3. Inform the patient of his or her right to the assistance
of the patients’ rights advocate or an attorney to
prepare for the hearing and to answer any questions
or concerns [Welfare and Institutions Code Sections
5333(c) and 5334(a)].
Treatment facilities, in conjunction with their medical staffs,
must develop internal procedures for facilitating the filing
of petitions for capacity hearings [Welfare and Institutions
Code Section 5332(c)].
The Hearing. A patients’ rights advocate or attorney will
meet with the patient to discuss the capacity hearing
process as soon after the filing of the petition as is
practicable. The patients’ rights advocate or attorney will
assist the patient in preparing for the capacity hearing and
will answer questions or otherwise assist the patient as
appropriate [Welfare and Institutions Code Section 5333(d)].
Capacity hearings must be held within 24 hours of the
filing of the petition whenever possible. If any party needs
additional time to prepare for the hearing, the hearing will
be postponed for 24 hours. In case of hardship, hearings
may also be postponed for an additional 24 hours,
pursuant to local policy developed by the county mental
health director and the presiding judge of the superior court.
In no event may hearings be delayed beyond 72 hours
of the filing of the petition. [Welfare and Institutions Code
Section 5334(a)]
Capacity hearings must be held in an appropriate location
in the facility where the patient is receiving treatment,
and must be held in a manner compatible with, and the
least disruptive of, the treatment [Welfare and Institutions
Code Section 5334(b)]. Hearings will be conducted by a
superior court judge, a court-appointed commissioner or
referee, or a court-appointed hearing officer [Welfare and
Institutions Code Section 5334(c)]. The patient will be
given oral notification of the determination of the judge or
hearing officer at the conclusion of the hearing. As soon
thereafter as is practicable, the patient, his or her advocate
or attorney, and the director of the facility will be given
written notification of the determination, which will include
a statement of the evidence relied upon and the reasons
for the determination [Welfare and Institutions Code Section
5334(d)]. A copy of the determination will be submitted to
the superior court.
Appeal of the Determination. The patient may appeal the
determination to the superior court or the court of appeal.
However, antipsychotic medication may be administered to
the patient pending appeal. [Welfare and Institutions Code
Section 5334(e)(1) and (3)]
The hospital may request the district attorney or county
counsel in the county in which the person is receiving
treatment to appeal the determination to the superior court
or the court of appeal, on behalf of the state [Welfare and
Institutions Code Section 5334(e)(2)].
Duration of Judicial Determination of Incapacity. A
judicial determination of a patient’s incapacity to refuse
treatment with antipsychotic medication remains in effect
only for the duration of the detention period described in
Welfare and Institutions Code 5150 or 5250, or both, or
until capacity has been restored according to standards
developed by the treatment facility in conjunction with
its medical staff, or by court determination, whichever is
sooner [Welfare and Institutions Code Section 5336].

Chapter 2 — Principles of Consent for Mental Health Patients CHA
2.47
©CALIFORNIA HOSPITAL ASSOCIATION
(See “Notice of Effects of Medication,” page3.11, if
medications will be given to a person detained under
Welfare and Institutions Code Section 5150.)
MINORS IN CUSTODY OF THE JUVENILE COURT/
FOSTER CHILDREN
If a child is in the custody of the juvenile court and the
child has been removed from the physical custody of the
parent, only a juvenile court judicial officer has the authority
to order the administration of psychotropic medications for
the child. The juvenile court may issue an order delegating
this authority to a parent upon finding that the parent
poses no danger to the child and has the capacity to
authorize the administration of psychotropic medications.
(See “Psychotropic Medications,” page2.33, for more
information about the administration of psychotropic
medications to a child in the custody of the juvenile court.)
C. Psychosurgery
“Psychosurgery” is defined as any of those operations
referred to as lobotomy, psychiatric surgery, behavioral
surgery and all other forms of brain surgery if the surgery is
performed for the purpose of any of the following:
1. Modification, alteration, or control of thoughts, feelings,
actions or behavior rather than the treatment of a
known and diagnosed physical disease of the brain;
2. Modification or alteration of normal brain function,
brain tissue or brain cells in order to modify, alter or
control thoughts, feelings, actions or behavior; or
3. Treatment of abnormal brain function, brain tissue or
brain cells in order to modify, alter or control thoughts,
feelings, actions or behavior when the abnormality is
not an established cause for those thoughts, feelings,
actions or behavior.
Psychosurgery does not include surgery for relief of pain
caused by physical disease elsewhere in the body.
Psychosurgery also does not include prefrontal sonic
treatment where there is no destruction of brain tissue.
However, all requirements pertaining to psychosurgery
must be followed when prefrontal sonic treatment is
administered and there exists any possibility there will
be destruction of brain cells or brain tissue. [Welfare and
Institutions Code Section 5325(g); Title 9, California Code
of Regulations, Sections 836 and 837] (See D.“Convulsive
Therapy and Insulin Coma Treatment,” page2.49, for
definitions as well as other requirements regarding
prefrontal sonic treatment.)
CONDITIONS UNDER WHICH PSYCHOSURGERY MAY
BE PERFORMED
Welfare and Institutions Code Section 5326.6 governs
the performance of psychosurgery. In order to perform
psychosurgery on a patient, whether admitted to a facility
as a voluntary or involuntary patient, wherever administered,
the following conditions must be met.
Age of Patient
The patient must be over 18 years of age. Under no
circumstances may psychosurgery be performed on a
person under 18 years of age [Title 9, California Code of
Regulations, Section 845].
Informed Consent
The patient must give a valid, written informed consent
[Welfare and Institutions Code Section 5326.6(a)]. For
these purposes, “written informed consent” means
that a person knowingly and intelligently, without duress
or coercion, clearly and explicitly gives written consent to
the treating physician for the proposed therapy. Welfare
and Institutions Code Sections 5326.2, 5326.3, 5326.4
and 5326.5, discussed below, state the requirements for
obtaining and documenting a valid informed consent.
Required Information. To create the basis for a voluntary
informed consent, the following information must be given
to the patient in a clear and explicit manner:
1. The reason for the treatment; that is, the nature and
seriousness of the patient’s illness, disorder or defect.
2. The nature of the procedures to be used in the
proposed treatment, including its probable frequency
and duration.
3. The probable degree and duration (temporary or
permanent) of improvement or remission expected with
and without the treatment.
4. The nature, degree, duration and probability of the
side effects and significant risks, commonly known by
the medical profession, of the treatment, including its
associated therapeutic modalities, especially noting
the degree and duration of memory loss (including its
irreversibility) and how and to what extent side effects
may be controlled, if at all.
5. That there exists a division of opinion as to the efficacy
of the proposed treatment, why and how it works, and
its commonly known risks and side effects.
6. The reasonable alternative treatments.
7. Why the physician recommends this
particular treatment.

CHA Mental Health Law Manual 2019
2.48
©CALIFORNIA HOSPITAL ASSOCIATION
8. That the patient has the right to accept or refuse the
proposed treatment, and that, if consent is given, the
patient has the right to revoke the consent for any
reason, and at any time prior to or between treatments.
Waiting Period Required. The patient may be asked to
give his or her written informed consent only after 24 hours
have elapsed from the time the required information above
has been given to the patient [Welfare and Institutions
Code Section 5326.5(e)].
Consent Form. The law states that the California
Departments of Health Care Services and State Hospitals
must promulgate a standard written consent form setting
forth clearly and in detail the matters listed in Welfare
and Institutions Code Section 5326.2 (see “Required
Information,” page 2.55) and any further information with
respect to each item as deemed generally appropriate
to all patients [Welfare and Institutions Code Section
5326.3]. However, the forms presently available from the
departments are for use by state hospitals only. Until a
form is promulgated by the department for use by other
hospitals, each hospital should prepare a written consent
form in accordance with the requirements in Welfare and
Institutions Code Sections 5326.2, 5326.3, 5326.4 and
5326.5. It is also advisable for each hospital to contact its
local mental health agency to determine whether a form
has been developed for use by local facilities.
The treating physician must use the standard written
consent form, and must also supplement it in writing
with those details that pertain to the particular patient
being treated.
Presentation of “Supplemented” Consent Form and
Oral Explanation to Patient. The treating physician must
present to the patient the supplemented consent form and
orally give a clear and detailed explanation to the patient of
all of the above required information.
Signature of Patient and Witness. After the required
waiting period, the treating physician must obtain the dated
signature of the patient and a witness on the supplemented
consent form.
Documentation Requirements. The fact of the execution
of the written consent form and of the oral explanation
must be entered into the patient’s medical record along
with a copy of the consent form itself. The consent form
must be made available to the patient and to his or her
attorney, guardian, conservator and, if the patient consents,
to a responsible relative of the patient’s choosing.
Consent Process Devoid of Duress or Coercion. The
physician may urge the proposed treatment as the best
one, but may not use, in an effort to gain consent, any
reward or threat, express or implied, nor any other form
of inducement or coercion, including, but not limited to,
placing the patient in a more restricted setting, transfer
of the patient to another facility or loss of the patient’s
privileges. A patient may not be denied any benefits for
refusing treatment.
Patient Capacity to Consent. A person is deemed to
have the capacity to consent or to refuse consent if it
is determined that the person has actually understood
and can knowingly and intelligently act upon the
information specified in “Required Information,” page
2.55. Understanding of the potential benefits and risks
of the proposed treatment or surgery is the primary factor
in determining the capacity to consent or to refuse. A
person must not be deemed to lack capacity to consent
or refuse consent solely by virtue of a psychiatric or
medical diagnosis [Title 9, California Code of Regulations,
Section 840].
Discretionary Involvement of Responsible Relative
A responsible relative of the patient’s choosing (with the
patient’s consent) and the guardian or conservator, if there
is one, must read the consent form and must be given
the information discussed in “Required Information,” page
2.55 by the treating physician. If the patient does not wish
to inform a relative, or if the chosen relative is unavailable
(and the patient either does not wish to designate another
relative or that relative is also unavailable), this requirement
may be dispensed with.
A “responsible relative” for these purposes includes the
spouse, parent, adult child, or adult brother or sister of
the patient.
Documentation by Physician of Reasons for Procedure
The attending physician must enter adequate
documentation in the patient’s medical record of the
reasons for the procedure, that all other appropriate
treatment modalities have been exhausted, and that
this mode of treatment is definitely indicated and is the
least drastic alternative available for the treatment of the
patient at this time. This statement must be signed by the
attending and treating physician(s).
Consultation
Three physicians, one appointed by the facility and two
appointed by the local mental health director, two of whom
must be board certified or board-eligible psychiatrists
or neurosurgeons, must personally examine the patient
and unanimously agree with the attending physician’s
determinations and agree that the patient has the capacity

Chapter 2 — Principles of Consent for Mental Health Patients CHA
2.49
©CALIFORNIA HOSPITAL ASSOCIATION
to give informed consent. This agreement must be
documented in the patient’s medical record and signed
by each physician. [Welfare and Institutions Code Section
5326.6]
Time Delay Between Written Informed Consent and
Surgery
In no case may psychosurgery be performed less than
72 hours following the time the patient gave written consent
[Welfare and Institutions Code Section 5326.6(d)].
Effect of Consent on Right to Refuse Treatment
The giving of consent may not be construed as a waiver of
the right to refuse treatment at a future time. Consent may
be withdrawn at any time, orally or in writing, and must be
given immediate effect.
DOCUMENTATION OF REFUSAL OF PSYCHOSURGERY
If a patient is deemed by the physician to have the
capacity to give informed consent, but refuses to do so,
the physician must indicate in the medical record that
the treatment was refused despite the physician’s advice,
and that he or she explained to the patient the patient’s
responsibility for any untoward consequence of the
refusal. However, this explanation must not be made in a
manner that constitutes duress or coercion. The patient
must not be subject to any loss of privileges due to a
refusal to consent. [Title 9, California Code of Regulations,
Section 841]
REPORTS OF PSYCHOSURGERY
A doctor or facility that administers psychosurgery must
report quarterly to the local behavioral health director,
who is required to transmit a copy of the report to the
director of mental health. The report must include the
number of persons who received psychosurgery, wherever
administered, in the following categories:
1. Involuntary patients who gave informed consent.
2. Voluntary patients who gave informed consent.
(Patients incapable of giving consent must not undergo
psychosurgery.)
The report must also include psychiatric diagnosis, type of
psychosurgery performed, date surgery performed, and
complications that arose during or after the psychosurgery.
A facility that considers psychosurgery a part of its
treatment program must file a quarterly report, regardless
of whether any of these treatment methods were used
during the quarter. [Welfare and Institutions Code Section
5326.15; Title 9, California Code of Regulations, Section
838.1]
D. Convulsive Therapy and Insulin Coma
Treatment
State law sets forth various requirements, discussed below,
to be met prior to initiation of convulsive therapy or insulin
coma treatment on a patient.
All requirements pertaining to the administration of
convulsive treatment must be followed when insulin
coma treatment is administered, or when prefrontal
sonic treatment is administered that involves only direct
stimulation of brain cells or brain tissue. All requirements
pertaining to psychosurgery must be followed when
prefrontal sonic treatment is administered and there exists
any possibility there will be destruction of brain cells or
brain tissue (see C.“Psychosurgery,” page2.47).
DEFINITIONS
“Convulsive treatment” is the planned induction of a
seizure through electrical or chemical means for therapeutic
purposes. When more than one seizure is induced in a
single treatment session, each seizure shall be considered
a separate treatment for record keeping and reporting
purposes.
“Insulin coma treatment” consists of producing a coma for
therapeutic purposes, with or without convulsions, through
the intramuscular administration of insulin.
“Prefrontal sonic treatment” is the direct stimulation
and/or destruction of brain cells or brain tissue by
ultrasound for therapeutic purposes.
[Title 9, California Code of Regulations, Sections 836
and 837]
INVOLUNTARY ADULT PATIENTS
Before convulsive treatment or insulin coma treatment is
administered to an involuntary adult patient, the conditions
described in this section of the manual must be met.
Involuntary patients include the following:
1. Persons involuntarily detained for 72-hour evaluation
and treatment under Welfare and Institutions Code
Section 5150;
2. Persons certified for intensive treatment under Welfare
and Institutions Code Section 5250;
3. Persons certified for additional intensive treatment
as suicidal under Welfare and Institutions Code
Section 5260;
4. Persons post-certified as a demonstrated danger of
substantial physical harm to others under Welfare and
Institutions Code Section 5300;

CHA Mental Health Law Manual 2019
2.50
©CALIFORNIA HOSPITAL ASSOCIATION
5. Persons under temporary or permanent
conservatorship or guardianship;
6. Persons who have been judicially committed, as
defined under Welfare and Institutions Code
Section 5008.1 (mentally disordered sex offenders;
developmentally disabled persons admitted to a state
hospital due to dangerousness; or other persons
committed to the State Department of State Hospitals).
If these provisions conflict with regulations dealing
with the developmentally disabled promulgated under
Chapter 1 (commencing with Section 4500) of the
Welfare and Institutions Code, the latter statute and
regulations shall control.
[Title 9, California Code of Regulations, Section 836.1]
Documentation of Reasons for Treatment
The attending or treating physician must enter adequate
documentation in the patient’s medical record of the
reasons for the procedure, that all reasonable treatment
modalities have been carefully considered, and that the
treatment is definitely indicated and is the least drastic
alternative available for this patient at this time. This
statement in the medical record must be signed by the
attending and treating physician(s).
Committee Review of Treatment
A review of the patient’s medical record must be conducted
by a committee of two physicians, at least one of whom
must have personally examined the patient.
One physician must be appointed by the facility and one
must be appointed by the local mental health director. Both
must be board-certified or board-eligible psychiatrists or
neurologists. This review committee must unanimously
agree with the treating physician’s determinations
entered in the medical record. This agreement must be
documented in the patient’s medical record and signed by
both physicians. [Welfare and Institutions Code Section
5326.7]
The physicians who serve on review committees must not
be personally involved in the treatment of the patient whose
case they are reviewing [Welfare and Institutions Code
Section 5326.55].
Discretionary Involvement of Responsible Relative
A responsible relative of the patient’s choosing and the
patient’s guardian or conservator, if there is one, must
be given the oral explanation by the attending physician
of the information required by Welfare and Institutions
Code Section 5326.2, which is discussed in “Required
Information,” page 2.55. If the patient does not wish to
inform a relative, or if the chosen relative is unavailable
and the patient either does not wish to designate another
relative or that relative is also unavailable, this requirement
may be dispensed with.
A “responsible relative” for these purposes, includes the
spouse, parent, adult child, or adult brother or sister of the
patient [Welfare and Institutions Code Section 5326.6(d)].
Basic Requirements of Informed Consent
The patient must give a valid written informed consent
[Welfare and Institutions Code Section 5326.7(d)]. For
these purposes, a “written informed consent” means
that a person knowingly and intelligently, without duress or
coercion, clearly and explicitly gives written consent to the
treating physician for the proposed therapy. Welfare and
Institutions Code Sections 5326.2, 5326.3, 5326.4 and
5326.5, discussed in “Informed Consent,” page2.47, state
the requirements for obtaining and documenting a valid
informed consent.
Consent Form
For purposes of obtaining written informed consent to
electroconvulsive treatment, the law requires the treating
physician to use the consent form developed by the state
[Title 9, California Code of Regulations, Section 839]. The
form, DHCS 1800/MH 300, may be found at www.dhcs.
ca.gov/formsandpubs/forms/pages/mental_health-forms.
aspx. The treating physician must use the standard written
consent form, and must also supplement it in writing
with those details that pertain to the particular patient
being treated.
Patient Capacity to Consent. A patient has the capacity
to consent or to refuse to consent if he or she has actually
understood and can knowingly and intelligently act upon
the information required to be given to the patient by
the physician. Understanding of the potential benefits
and risks of the proposed treatment is the primary factor
in determining capacity to consent or refuse consent.
A person does not lack capacity solely by virtue of a
psychiatric or medical diagnosis. [Title 9, California Code of
Regulations, Section 840]
Waiting Period Required
The patient may be asked to give his or her written
informed consent only after 24 hours have elapsed from
the time the required information above has been given
to the patient. [Welfare and Institutions Code Section
5326.5(e)]

Chapter 2 — Principles of Consent for Mental Health Patients CHA
2.51
©CALIFORNIA HOSPITAL ASSOCIATION
Presentation of “Supplemented” Consent Form and
Oral Explanation to Patient
The treating physician must present to the patient the
supplemented consent form and orally give a clear and
detailed explanation to the patient of all of the above
required information.
Additional Informed Consent Requirements
Duration of Written Informed Consent. The written
informed consent must be given for a specified maximum
number of treatments over a specified maximum period of
time that may not exceed 30 days. It is revocable at any
time before or between treatments and any withdrawal
of consent, which may be given orally or in writing, must
be given immediate effect. If the patient subsequently
changes his or her mind, a new consent must be obtained.
A renewed written informed consent must be given for any
additional treatments in number or in time, not to exceed
30 days.
Agreement on Capacity to Consent
Review by Patient’s Attorney or Public Defender. The
patient’s attorney, or if none, a public defender appointed
by the court, must agree with the attending physician
that the patient has the capacity to give written informed
consent and actually gave such consent. The attorney must
make an independent judgment of capacity [Welfare and
Institutions Code Section 5326.7(e); Title 9, California Code
of Regulations, Section 840(c)].
Court Review if Capacity Disputed. If either the attending
physician or the attorney believes that the patient does
not have the capacity to give written informed consent,
then a petition must be filed in superior court to determine
the patient’s capacity to give written informed consent.
The court will hold an evidentiary hearing after giving
appropriate notice to the patient, and within three days
after the petition is filed. At the hearing the patient must
be present and represented by legal counsel. If the court
deems the attorney to have a conflict of interest, the
attorney may not represent the patient in this proceeding.
Consent by Other than Patient. If the court determines
that the patient does not have the capacity to give written
informed consent, then treatment may be performed
if written informed consent (as defined in Welfare and
Institutions Code Sections 5326.2 and 5326.5) is given by
the responsible relative chosen by the patient, if any, or the
patient’s conservator or guardian.
Claim of Regained Competency
At any time during the course of treatment of a person who
has been deemed incompetent, that person has the right
to claim regained competency. Should he or she do so, the
person’s competency must be reevaluated according to
“Agreement on Capacity to Consent,” page2.51.
Documentation of Refusal of Convulsive Treatment
No convulsive treatment or insulin coma treatment may be
performed if the patient, whether admitted to the facility
as a voluntary or involuntary patient, is deemed to be
able to give informed consent and refuses to do so. The
physician must indicate in the medical record that the
treatment was refused despite the physician’s advice and
that the physician has explained to the patient the patient’s
responsibility for any untoward consequences of his or her
refusal. However, this explanation must not be made in a
manner that constitutes duress or coercion. The patient
must not be subject to any loss of privileges due to a
refusal to consent [Welfare and Institutions Code Section
5326.85; Title 9, California Code of Regulations, Section
841].
VOLUNTARY ADULT PATIENTS
Before convulsive treatment or insulin coma treatment
may be performed on voluntary patients, including but not
limited to those voluntarily admitted to a facility or receiving
the treatment in a physician’s office, a clinic, or a private
home, the following conditions must be met.
Patient Has Capacity to Consent
If the patient has the capacity to consent to the treatment,
the following steps must be taken.
Documentation of Treatment Reasons, Oral Explanation,
Written Informed Consent. As discussed in “Involuntary
Adult Patients,” page2.49, there must be documentation
of reasons for treatment, the discretionary oral explanation
to a responsible relative chosen by the patient, if any, and
written informed consent.
Verification of Capacity to Consent. A board-certified
or board-eligible psychiatrist or neurologist other than
the patient’s attending or treating physician must have
examined the patient and verified that the patient has the
capacity to give and has given written informed consent.
This verification must be documented in the patient’s
medical record and signed by the treating physician.
[Welfare and Institutions Code Section 5326.75]
Patient Lacks Capacity to Consent
If the required verification of capacity to consent is not
obtained, then all of the requirements for treatment for
involuntary adult patients must be met, as discussed in
“Involuntary Adult Patients,” page2.49.

CHA Mental Health Law Manual 2019
2.52
©CALIFORNIA HOSPITAL ASSOCIATION
MINORS UNDER THE AGE OF 12
Under no circumstances may convulsive treatment or
insulin coma treatment be performed on a minor under
the age of 12 years [Welfare and Institutions Code Section
5326.8]. Under no circumstances may prefrontal sonic
treatment be performed on a person under 18 years of age
[Title 9, California Code of Regulations, Section 845(a)].
MINORS BETWEEN 12 AND 16 YEARS OF AGE
Before convulsive treatment or insulin coma treatment may
be administered to a minor who is 12 years of age to under
16 years of age, the following conditions must be met
[Welfare and Institutions Code Section 5326.8]. However,
under no circumstances may prefrontal sonic treatment
be performed on a person under 18 years of age [Title 9,
California Code of Regulations, Section 845(a)].
Emergency Situation
It is an emergency situation and the treatment is deemed a
lifesaving treatment.
Emergency Certified by Review Committee
The fact of the emergency and the need for and
appropriateness of the treatment are certified unanimously
by a review board of three board-eligible or board-certified
child psychiatrists appointed by the local mental
health director.
Physicians who serve on a review committee must not be
personally involved in the treatment of the patient whose
case they are reviewing [Welfare and Institutions Code
Section 5326.55].
Compliance with Other Laws
The requirements set forth under “Involuntary Adult
Patients,” page2.49, must be followed. Unless the minor
is emancipated, the custodial parents or the person/agency
with legal custody is considered the guardian for purposes
of granting or withholding consent for convulsive therapy.
[Title 9, California Code of Regulations, Section 845]
Documentation
The treatment must be thoroughly documented and
reported immediately to the director of the Department of
Health Care Services.
MINORS 16 AND 17 YEARS OF AGE
A minor aged 16 or 17 years of age must be treated as
an adult for purposes of consent to convulsive therapy or
insulin coma treatment. (See “Involuntary Adult Patients,”
page2.49, for the requirements that apply to minors 16
and 17 years of age who are involuntary patients or who
lack verification of capacity to provide informed consent.
See “Voluntary Adult Patients,” page2.51, for the
requirements that apply to voluntarily admitted minors 16
and 17 years of age.)
An unemancipated minor’s parent(s) or the person/agency
with legal custody is considered the guardian for purposes
of granting or withholding consent. [Welfare and Institutions
Code Sections 5326.7 and 5326.8; Title 9, California Code
of Regulations, Section 845]
However, under no circumstances may prefrontal sonic
treatment be performed on a person under 18 years of age
[Title 9, California Code of Regulations, Section 845(a)].
COMMITTEE REVIEW OF TREATMENT
Facilities in which convulsive treatment or insulin coma
treatment is performed on voluntary or involuntary persons
must designate a qualified committee to review all of
these treatments and to verify their appropriateness and
need. (See Title 9, California Code of Regulations, Section
847 regarding posttreatment review committees.) The
local mental health director is required to establish a
review committee for convulsive treatments administered
anywhere other than in a facility (as defined in Health and
Safety Code Section 1250) in which psychiatric evaluation
or treatment is offered. Records of these committees will
be available in the same manner as are the records of
other hospital utilization and audit committees, and may
be subject to other regulations. Persons serving on these
review committees will enjoy the same immunities as
other persons serving on utilization, peer review, and audit
committees of health care facilities. [Welfare and Institutions
Code Section 5326.91]
REPORTS TO LOCAL BEHAVIORAL HEALTH DIRECTOR
A physician or facility that administers convulsive
treatments must report quarterly to the local behavioral
health director, who is required to transmit a copy of
the report to the director of mental health. The report
must include the number of persons who received
such treatments, wherever administered, in each of the
following categories:
1. Involuntary patients who gave informed consent.
2. Involuntary patients who were deemed incapable
of giving informed consent and received convulsive
treatment against their will.
3. Voluntary patients who gave informed consent.

Chapter 2 — Principles of Consent for Mental Health Patients CHA
2.53
©CALIFORNIA HOSPITAL ASSOCIATION
4. Voluntary patients deemed incapable of giving consent.
A facility that considers convulsive treatment a part of its
treatment program must file a quarterly report, regardless of
whether any of these treatment methods were used during
the quarter [Welfare and Institutions Code Section 5326.15;
Title 9, California Code of Regulations, Section 838]
The reports must be made on a form (MH 309) issued by
the state, available at www.dhcs.ca.gov/formsandpubs/
forms/pages/mental_health-forms.aspx.
EXCESSIVE USE OF CONVULSIVE TREATMENT
The director of the Department of State Hospitals defines
the excessive use of convulsive treatment as more than 15
treatments given to a patient within a 30-day period or a
total of more than 30 treatments given within a one-year
period [Welfare and Institutions Code Section 5326.95;
Title 9, California Code of Regulations, Section 849].
If additional convulsive treatments are indicated in the
judgment of the attending physician, prior approval must
be obtained from the review committee of the facility or
county (see “Involuntary Adult Patients,” page2.49).
LOCAL REGULATION OF CONVULSIVE TREATMENT
VOID
Administration of convulsive treatment is regulated by
numerous state statutes. As such, attempts by local
ordinances to prohibit convulsive treatment have been
found to be preempted by state law and thus are void
[Northern California Psychiatric Society v. City of Berkeley,
178 Cal.App.3d 90 (1986)]. (See also Business and
Professions Code Section 460, which limits the authority of
local governments to regulate health professionals.)
E. Mandatory Consultation — Outpatient and
Discharge Medications
DISCHARGE MEDICATIONS
California law requires that hospitals establish and
implement a written policy to ensure that each patient
receiving discharge medications receives information
regarding each medication. The written policy must be
developed in collaboration with a physician, a pharmacist
and a registered nurse, and approved by the medical staff.
The information given must include directions regarding the
use and storage of each medication, the precautions and
relevant warnings (including any potential impairment of the
ability to operate a vehicle or vessel), and the importance of
compliance with directions. The information must be given
by a pharmacist or registered nurse, unless it has already
been provided by a patient’s prescriber [Business and
Professions Code Section 4074, Health and Safety Code
Section 1262.5(e)].
(See IV.“Aftercare Plan,” page4.6 regarding the required
provision of a written aftercare plan to mental health
patients upon discharge.)
OUTPATIENT MEDICATIONS
Pharmacists must provide oral consultation to
outpatients (or their legal representatives) under the
following conditions:
1. Whenever a prescription drug has not previously been
dispensed to a patient;
2. Whenever a prescription drug not previously dispensed
to a patient in the same dosage form, strength or
with the same written directions is dispensed by
the pharmacy;
3. Upon request of the patient; and
4. Whenever the pharmacist deems it warranted in the
exercise of his or her professional judgment.
The oral consultation must include, at least:
1. Directions for use and storage and the importance of
compliance with directions; and
2. Precautions and relevant warnings, including common
severe side or adverse effects or interactions that may
be encountered.
[Title 16, California Code of Regulations, Section 1707.2]
In addition, whenever a pharmacist deems it warranted
in the exercise of his or her professional judgment, oral
consultation must also include:
1. The name and description of the medication;
2. The route of administration, dosage form, dosage and
duration of drug therapy;
3. Any special directions for use and storage;
4. Precautions for preparation and administration by
the patient, including techniques for self-monitoring
drug therapy;
5. Prescription refill information;
6. Therapeutic contra-indications, avoidance of common
severe side or adverse effects or known interactions,
including serious potential interactions with known
nonprescription medications and therapeutic
contra-indications and the action required if such

CHA Mental Health Law Manual 2019
2.54
©CALIFORNIA HOSPITAL ASSOCIATION
side or adverse effects or interactions or therapeutic
contra-indications are present or occur; and
7. Action to be taken in the event of a missed dose.
In addition, Business and Professions Code Section 4074
requires a pharmacist to inform a patient orally or in writing
of the harmful effects of a prescription drug if:
1. It poses substantial risk to the patient when taken in
combination with alcohol or the drug may impair the
patient’s ability to drive a motor vehicle; and
2. The Board of Pharmacy has determined that the
prescribed drug requires this warning.
If the pharmacist determines that a drug may impair a
patient’s ability to operate a vehicle or vessel, a written
warning label must be affixed to the drug container.
PATIENT DECLINES OR IS UNAVAILABLE
A pharmacist is not required to provide oral consultation
when a patient or the patient’s agent refuses
such consultation.
When the patient or agent is not present (i.e., the
medication is shipped or delivered to the patient), the
pharmacy must ensure that the patient receives written
notice of his or her right to request consultation and a
phone number from which the patient may obtain oral
consultation from a pharmacist who has ready access to
the patient’s record.
Documentation
It is recommended that the pharmacist document
any consultation provided to the patient (or agent)
or, if applicable, a refusal by the patient (or agent) of
offered consultation.
DRUG SUBSTITUTIONS
A pharmacist may make certain drug substitutions such
as dispensing a generic drug in place of a brand-name
drug. In such cases, the patient must be informed of the
substitution [Business and Professions Code Sections
4052.5(e) and 4073(e)].
F. Telemedicine/Telehealth
CONSENT REQUIRED
California law requires that, prior to delivery of health care
via telehealth, the health care provider initiating the use of
telehealth must:
1. Inform the patient about the use of telehealth;
2. Obtain verbal or written consent from the patient for
this use; and
3. Document the consent.
This law does not apply to a patient under the jurisdiction
of the Department of Corrections and Rehabilitation or any
other correctional facility.
CHA Form 8-1, “Conditions of Admission,” includes a
statement that the patient consents to telehealth services.
(See CHA Form 8-1, “Conditions of Admission.”)
ADDITIONAL REQUIREMENTS FOR MEDI-CAL
PATIENTS
A Medi-Cal patient receiving teleophthalmology,
teledermatology or teledentistry by store and forward must
be notified of the right to receive interactive communication
with the distant specialist physician, optometrist or dentist.
If requested, communication with the distant specialist
physician, optometrist or dentist must occur either at
the time of the consultation, or within 30 days of the
patient’s notification of the results of the consultation. If
the reviewing optometrist identifies a disease or condition
requiring consultation or referral pursuant to Business
and Professions Code Section 3041, that consultation
or referral must be with an ophthalmologist or other
appropriate physician and surgeon.
DEFINITIONS
“Asynchronous store and forward” means the
transmission of a patient’s medical information from an
originating site to the health care provider at a distant site
without the presence of the patient.
“Distant site” means a site where a health care provider
who provides health care services is located while providing
these services via a telecommunications system.
“Health care provider” means a person who is licensed
under Division 2 of the Business and Professions Code.
This includes almost every type of licensed health care
provider that exists in California, such as physicians, nurses,
psychologists, marriage and family therapists, physician
assistants, dentists, chiropractors, massage therapists, and
veterinarians.
“Originating site” means a site where a patient is located
at the time health care services are provided via a
telecommunications system or where the asynchronous
store and forward service originates.

Chapter 2 — Principles of Consent for Mental Health Patients CHA
2.55
©CALIFORNIA HOSPITAL ASSOCIATION
“Synchronous interaction” means a real-time interaction
between a patient and a health care provider located at a
distant site.
“Telehealth” means the mode of delivering health
care services and public health via information and
communication technologies to facilitate the diagnosis,
consultation, treatment, education, care management, and
self-management of a patient’s health care while the patient
is at the originating site and the health care provider is at a
distant site. Telehealth includes synchronous interactions
and asynchronous store and forward transfers.
“Teleophthalmology,” “teledermatology and teledentistry
by store and forward” means an asynchronous
transmission of medical or dental information for review
at a later time by an ophthalmologist, dermatologist,
optometrist, or a dentist, where the professional at the
distant site reviews the information without the patient
being present in real time.
[Business and Professions Code Section 2290.5; Welfare
and Institutions Code Section 14132.725]
G. Consent for HIV Testing
California law establishes special requirements for
consent to HIV tests and the disclosure of HIV test results.
“HIV test” is defined as any clinical test, laboratory or
otherwise, used to identify HIV, a component of HIV, or
antibodies or antigens to HIV [Health and Safety Code
Section 120775(c)]. California law also has very strict laws
governing the confidentiality of HIV test results.
Providers should remember that a positive result to an
HIV test must be reported to the local health officer (see
chapter 18).
REQUIRED INFORMATION
Prior to ordering an HIV test, a “medical care
provider” must:
1. Inform the patient that the test is planned,
2. Provide information about the test to the patient,
3. Inform the patient that there are numerous treatment
options available for a person who tests positive for
HIV and that a person who tests negative for HIV
should continue to be routinely tested, and
4. Advise the patient that he or she has the right to
decline the test.
[Health and Safety Code Section 120990(a)]
There are additional disclosure requirements if the patient
is pregnant (see CHA’s Consent Manual, chapter 13). The
disclosure requirements do not apply to a clinical laboratory
[Health and Safety Code Section 120990(i)].
NOTE: The term “medical care provider” is not defined
in this law but is defined elsewhere to mean a health care
professional licensed under Division 2 of the Business and
Professions Code (e.g., physicians, dentists, nurses and
other individual professionals) [Health and Safety Code
Section 109278(b)].
Exception
The disclosure requirement above does not apply when a
patient independently requests an HIV test from a medical
care provider [Health and Safety Code Section 120990(b)].
If the patient independently requests the test, the provider
should document that fact in the medical record. It is not
clear what “independently requesting” an HIV test means.
The sponsors of this language in the law meant it to mean
patients who proactively request an HIV test from their
physician, rather than the physician recommending to the
patient that the test be run.
Alternatively, a provider may wish to give the disclosures to
all patients, whether the provider suggested the test or the
patient requested it. CHA has developed the form “Consent
for the HIV Test” (CHA Form 23-1) that includes the
information that must be disclosed to patients. The provider
may give this form to all patients who undergo HIV testing
(regardless of who initially suggested the test), and put a
copy of the signed form in the patient’s medical record to
fulfill the documentation requirements.
INFORMED CONSENT
The law states that, except for tests ordered in connection
with the required disclosures described above, no person
shall “administer” an HIV test unless the patient or his
or her parent, guardian, conservator, or other person
authorized to make health care decisions for the patient
has provided informed consent to the test. It is not clear
what this provision means. The sponsors of this language
in the law said that they meant it to apply in cases where
a person who was not a health care provider was taking
the sample from the patient to test using a home test kit or
to send to a mail-order lab for HIV testing. They intended
the law to prohibit this without the test subject’s informed
consent. However, it may also apply to instances where the
patient lacks capacity to make his or her own health care
decisions, and consent is provided by a legal representative.
In these cases, The patient or the patient’s legal
representative may provide consent orally or in writing.

CHA Mental Health Law Manual 2019
2.56
©CALIFORNIA HOSPITAL ASSOCIATION
The person “administering” the HIV test must maintain
documentation of consent in the patient’s medical
record. This may be accomplished by having the patient
or legal representative sign a consent form or by having
the ordering practitioner make a note in the medical
record. (See below for information on who may be a legal
representative of a patient for purposes of consenting to an
HIV test.) [Health and Safety Code Section 120990(c)]
CHA has developed the form “Consent for the HIV Test”
(CHA Form 23-1) to include the information that must
be disclosed to patients. (This form should be used only
when the test is performed for purposes other than testing
donated blood since a different form is required to be used
by blood banks and plasma centers.)
Since this consent form contains medical information,
it should be reviewed by an appropriate medical staff
committee or designated physician prior to use in
the hospital.
DOCUMENTING REFUSALS
If a patient declines an HIV test, the medical care provider
must note that fact in the patient’s medical record [Health
and Safety Code Section 120990(a)].
MINORS 12 AND OLDER
A minor 12 years of age or older who may have come
into contact with a communicable disease may consent
to medical care related to the diagnosis or treatment of
the disease, if it is a disease that is required by law to be
reported to the local health officer, or for a related sexually
transmitted disease as determined by CDPH. Both AIDS
and HIV infection are required by law to be reported
[Family Code Section 6926; Health and Safety Code
Sections 120250 and 121022; Title 17, California Code of
Regulations, Sections 2500 and 2641.30-2643.20].
The California Office of AIDS has taken the position, in
connection with its operation of alternative testing sites,
that Family Code Section 6926 gives a minor 12 years
of age or older the legal capacity to consent to the HIV
test. Taken together, these authorities suggest that minors
age 12 or older have the legal authority to consent to the
HIV test.
Care must be taken when applying this principle in
particular situations. It is important to determine that a
minor consenting to the HIV test is competent to give
his or her consent — i.e., that the minor is sufficiently
knowledgeable and mature to appreciate the nature and
consequences of his or her decision (see B.“Capacity
to Consent,” page2.37). Given these concerns, except
in those instances in which the minor has indicated that
privacy is a primary concern and it is clear that the minor
has an appreciation of AIDS and of the HIV test, the health
care provider may wish to recommend that a parent or
guardian be involved in the decision whether to consent
to the HIV test. At the same time, when a minor 12 years
or older initiates the test request, indicates his or her
preference not to involve a parent or guardian, and shows
appreciation of the issues involved, the minor is entitled to
consent to the test. Conversely, if a minor age 12 or older
refuses the HIV test, that refusal should be respected even
if the parent or guardian wants the minor to be tested, if the
minor appreciates the issues and consequences.
The minor’s parents or guardian are not liable for payment
for the HIV testing or treatment [Family Code Section
6926(c)]. Providers should establish procedures to ensure
that parents do not receive a bill for this service, unless
authorized by the minor in writing. The law does not
specify who is responsible for payment. (See C.“Financial
Responsibility for Treatment of Minors,” page2.25.)
ADULTS LACKING CAPACITY AND MINORS UNDER 12
The law is clear that a minor is not authorized to consent to
an HIV test if he or she is under 12 years of age [Health and
Safety Code Section 121020(a)].
When an individual is under 12 years of age or, as a result
of his or her mental or physical condition, or lack of maturity,
lacks the capacity to consent to the HIV test and the test
is necessary to render appropriate care or to practice
preventative measures, written consent may be obtained
from persons lawfully authorized to make health care
decisions for the individual [Health and Safety Code Section
121020(a)(1)]. This includes agents appointed in a power
of attorney for health care (unless the power of attorney
for health care expressly denies the agent the right to
consent to an HIV test), parents of minors (see “Minors 12
and Older,” page2.56), and conservators and guardians
who have been authorized by the court to make health
care decisions for the patient. Where appropriate, this may
also include an adult patient’s closest available relative
(see “Family Members,” page2.22, for a discussion of
the basis for relying upon consent from a patient’s closest
available relative)
. CHA Form 23-1, “Consent for the HIV
Test” may be used to document consent. The patient’s lack
of capacity and the necessity for the test result should be
documented in the medical record.

Chapter 2 — Principles of Consent for Mental Health Patients CHA
2.57
©CALIFORNIA HOSPITAL ASSOCIATION
FOSTER CHILD/DEPENDENT CHILD OF THE COURT/
INFANT IN TEMPORARY CUSTODY
A parent of a child who is a dependent of the juvenile
court (foster child) continues to have the legal authority to
consent to HIV testing, if the child is under 12 years of age.
In addition, a court or social worker may be able to consent,
as described below.
If the subject of the HIV test is a minor adjudged to be a
dependent child of the court (foster child) under Welfare
and Institutions Code Section 360, written consent for
the test may be obtained from the court pursuant to its
authority under Welfare and Institutions Code Sections 362
or 369. The hospital should obtain a copy of the court’s
order in these cases.
If the subject of an HIV test is an infant who is less than 12
months of age who has been taken into temporary custody
under Welfare and Institutions Code Section 305 et seq.
or who has been, or has a petition filed with the court to
be, adjudged a dependent child of the court under Welfare
and Institutions Code Section 360, the social worker may
provide written consent for an HIV test to be performed
when the infant is receiving medical care pursuant to
Welfare and Institutions Code Section 369, if all of the
following have occurred:
1. The attending physician determines that HIV testing is
necessary to render appropriate care to the infant and
documents that determination. When deciding whether
HIV testing is necessary, the physician must consider
appropriate factors, either known to the attending
physician or provided to the attending physician by
the social worker, including, but not limited to, whether
the infant has a parent with a history of behavior that
places the parent at an increased risk of exposure to
HIV, or whether the infant is a victim of sexual abuse,
which has placed the child at risk of exposure to HIV.
2. The social worker provides known information
concerning the infant’s possible risk factors regarding
exposure to HIV to the attending physician.
3. The social worker has made reasonable efforts to
contact the parent or guardian but was unable to do
so, and the social worker has documented his or her
efforts to contact that person.
The attending physician and the social worker must
comply with all state and federal confidentiality laws to
protect the privacy interests of both the infant and the
biological mother.
If an infant tests positive for HIV in a test performed under
this law, the social worker must provide the physician any
available contact information for the biological mother
for purposes of reporting the HIV infection to the local
health officer.
If an infant tests positive for HIV in a test performed under
this law, and the physician determines that immediate HIV
medical care is necessary to render appropriate care to
that infant, the provision of HIV medical care is considered
emergency medical care under Welfare and Institutions
Code Section 369(d). In such cases, care may be provided
without a court order and upon the authorization of the
social worker.
DECEASED PATIENT
The law does not directly authorize anyone to consent to
the testing of a cadaver except in the context of an autopsy,
organ donation, scientific investigation or in case of an
occupational exposure. If the need for an HIV test outside
of these circumstances arises, the hospital should consult
its legal counsel. [Health and Safety Code Sections 120990
and 121020(b)]
OCCUPATIONAL EXPOSURES
Testing may in some instances be performed even without
the patient’s consent where there has been a significant
exposure of health care personnel to potentially infectious
materials. (See CHA’s Consent Manual, chapter 5, for the
procedure for testing under these circumstances.)
CRIMINAL DEFENDANTS AND INMATES OF
CORRECTIONAL INSTITUTIONS
The law allows involuntary testing of criminal defendants
and inmates of correctional institutions in the
following instances:
1. Every person, including a juvenile, who is convicted
of certain sexual offenses shall be ordered by the
court to submit to a blood or oral mucosal transudate
saliva test for evidence of antibodies to the probable
causative agent of AIDS within 180 days of the date of
conviction [Penal Code Section 1202.1]. A hospital that
performs an HIV test pursuant to a court order under
Penal Code Section 1202.1 must disclose the results
of the test to the clerk of the court ordering the test.
The court will then disclose the results to the California
Department of Justice and the local health officer. The
local health officer will then disclose the results to
the test subject and, where requested, to the victim,
but only after professional counseling is provided,
as appropriate.
2. Defendants (including minors) charged with certain
crimes involving sexual offenses and certain other

CHA Mental Health Law Manual 2019
2.58
©CALIFORNIA HOSPITAL ASSOCIATION
arrestees are subject to testing for HIV, AIDS-related
conditions and other communicable diseases
pursuant to court order if a peace officer, custodial
officer, firefighter, emergency medical personnel or
specified nonsworn employees of law enforcement
agencies have been exposed to a defendant’s or
arrestee’s blood or bodily fluids [Health and Safety
Code Sections 121050-121065]. A forensic scientist
or employee who is exposed may also petition a court
for an order for testing. Prior to the filing of a petition
for court-ordered testing, a health care provider must
attempt to obtain the voluntary informed consent of
the arrestee (or the authorized legal representative) to
perform a test for HIV, hepatitis B, and hepatitis C. The
voluntary informed consent must be in writing. CHA
Form 23-1, “Consent for the HIV Test,” may be used to
comply with this requirement. If the arrestee declines to
consent, the peace officer, custodial officer, firefighter,
emergency medical personnel or nonsworn employee
of a law enforcement agency petitioning the court
must obtain a written certification by a health care
professional that an exposure, including the nature and
extent of the exposure, has occurred.
Testing must be performed on specimens of blood
withdrawn from the defendant in a medically approved
manner. Only a physician, registered nurse, licensed
vocational nurse, licensed medical technician or
licensed phlebotomist may withdraw blood for these
purposes. The court’s order should specify the tests
to be performed and designate the persons to whom
disclosure of the results may be made. The test results
must be sent to the designated recipients with the
following disclaimer:
The tests were conducted in a medically approved
manner. Persons receiving this test result should
continue to monitor their own health and should consult
a physician as appropriate. Recipients of these test
results are subject to existing confidentiality protections
for any identifying information about HIV, hepatitis B, or
hepatitis C test results. Medical information regarding
the HIV, hepatitis B, or hepatitis C status of the source
patient shall be kept confidential and may not be further
disclosed, except as otherwise authorized by law.
The peace officer, custodial officer, firefighter,
emergency medical personnel or nonsworn employee
of a law enforcement agency who was exposed
must also be informed of the penalties for unlawful
disclosure of medical information about the defendant/
arrestee pursuant to Health and Safety Code Section
120980. In some cases, the subject of the HIV test
must be asked if he or she wishes to know the results,
and must sign a form if he or she does not wish to be
informed [Health and Safety Code Section 121056(c)
(2) and 121060(c)(2)]. An arrestee’s refusal to sign the
form is deemed to be a refusal to be informed of the
test results.
3. Adults or minors charged with any crime are subject
to testing when, at the request of a victim of the crime,
a court finds that there is probable cause to believe
that the accused committed the crime and that blood,
semen or other bodily fluid capable of transmitting HIV
has been transferred from the accused to the victim.
Testing in such cases may be performed only by the
local health officer as specified in a search warrant
issued by the court. [Penal Code Section 1524.1]
4. Inmates of correctional institutions and other persons
in custody or on probation or parole are subject
to testing for hepatitis B and C and HIV under
circumstances where there is a significant risk that HIV
was transmitted. The test may be ordered by the chief
medical officer of a correctional institution (subject to
review by the superior court). [Penal Code Sections
7500-7554]
EXCEPTIONS: WHEN INFORMED CONSENT IS NOT
REQUIRED
The law clearly allows testing without the patient’s informed
consent in the following cases:
1. A test performed at an alternative testing site. (The
individual’s consent is still required, but to preserve that
person’s anonymity, no consent form need be signed.)
2. Testing performed to determine the suitability of organs
or tissue donated pursuant to the Uniform Anatomical
Gift Act (see Health and Safety Code Section 7150.65).
3. A test ordered by a medical examiner or other
physician on a cadaver when an autopsy is performed.
4. Testing performed as part of a scientific investigation
conducted either by medical researchers operating
under institutional review board approval or by CDPH
under a protocol for unlinked testing. The testing must
be anonymous with the individual’s name and other
identifying information removed so the test results will
not be linked to a particular individual in the study.
5. Where a health care worker has been exposed to the
potentially infectious materials of a patient, provided
that strict procedures for attempting to obtain consent
and testing are followed. These procedures are
described in CHA’s Consent Manual, chapter 5.
[Health and Safety Code Section 120990]

Chapter 2 — Principles of Consent for Mental Health Patients CHA
2.59
©CALIFORNIA HOSPITAL ASSOCIATION
INFORMING THE PATIENT OF TEST RESULTS
The provider who administers or orders the test must
ensure that the patient receives timely information and
counseling, as appropriate, to explain the test results and
the implications for the patient’s health.
If the patient tests positive for HIV infection, the provider
must inform the patient that there are numerous treatment
options available and identify follow-up testing and care
that may be recommended, including contact information
for medical and psychological services. In addition, the
provider must warn the patient about the dangers of
contagion and counsel the patient about precautionary
measures to prevent the spread of the disease to others
[Reisner v. Regents of the University of California, 31 Cal.
App.4th 1195 (1995)].
If the patient tests negative for HIV infection and is known
to be at high risk for HIV infection, the provider must:
1. Advise the patient of the need for periodic retesting,
2. Explain the limitations of current testing technology
and the current window period for verification of
results, and
3. Provide information about methods that prevent or
reduce the risk of contracting HIV, including, but not
limited to, preexposure prophylaxis and postexposure
prophylaxis, consistent with guidance of the Centers
for Disease Control and Prevention.
The provider may offer prevention counseling or a referral to
prevention counseling.

Chapter 3 — Contents
3 Voluntary Admission and Involuntary
Detainment for Mental Health
Treatment
©CALIFORNIA HOSPITAL ASSOCIATION
I. INTRODUCTION ....................................... 3.1
A. Background ....................................................3.1
B. Patient Privacy Considerations ....................3.1
II. ADMISSION AND TREATMENT OF
VOLUNTARY PATIENTS
............................. 3.2
A. Voluntary Admission of Adult Patients ........3.2
Authority to Request Voluntary Admission .........3.2
Caution: Type of Conservatorship
......................3.3
Written Application for Voluntary Admission
....... 3.3
Search of the Patient, Possessions and Room
..3.3
Other Admission Forms
....................................3.4
Right to Leave the Hospital
...............................3.4
B. Voluntary Admission of Minors to
Private Facilities
............................................3.4
Minors Affected ................................................3.4
Required Procedures at Admission
...................3.5
Independent Clinical Review
..............................3.5
C. Voluntary Admission of Minors to
State and County Facilities
...........................3.7
III. ADMISSION AND TREATMENT OF
INVOLUNTARY PATIENTS.......................... 3.7
A. Definitions ......................................................3.7
B. Facility Designation .......................................3.9
C. Interactions With Peace Officers .................3.9
IV. INVOLUNTARY DETENTION OF THE
PATIENT ON A 72-HOUR HOLD
................. 3.9
A. Patients With a Mental Health Disorder ......3.9
Conditions for Detention ...................................3.9
Written Application Required
............................. 3.9
Notice by Person Taking Patient Into
Custody
..........................................................3.10
Notice by Facility Admission Staff
....................3.10
Assessment
...................................................3.11
Notice of Effects of Medication
........................3.11
Services Provided
........................................... 3.11
Period of Detention
......................................... 3.11
Termination of Detention
.................................3.12
Notification of Release to County Behavioral
Health Director and Peace Officer
...................3.12
Immunity From Liability
....................................3.13
Responsibility for Property of Person Taken
Into Custody
................................................... 3.13
B. Patient Impaired by Inebriation ..................3.13
Conditions for Detention .................................3.13
Written Application Required
........................... 3.13
Recommended Form for Written Application
...3.14
Right to Make Two Telephone Calls
................. 3.14
Release Upon Request
...................................3.14
Services Provided
........................................... 3.14
Period of Detention
......................................... 3.14
Termination of Detention
.................................3.14
Immunity From Liability
....................................3.15
C. Patient Impaired by Use of Controlled
Substances ..................................................3.15
D. Other Admission Forms ..............................3.15
E. Special Requirements for a Minor .............3.16
Gravely Disabled Minor ...................................3.16
Requirements for Commitment
.......................3.16
V. CONTINUED TREATMENT OF AN
INVOLUNTARY PATIENT
......................... 3.17
A. Detention for 14-Day Intensive
Treatment
.....................................................3.17
Conditions for Certification ............................. 3.17
Signatures on Certification Notice
...................3.17
Required Form of Certification Notice
.............. 3.17
Delivery of Copies of the Certification Notice
...3.17
Advisement of Rights to Patient
......................3.18
Maximum Period of Detention
.........................3.18
Termination of Certification
............................. 3.18
Damages for Excessive Detention
...................3.19
Facility Preference
...........................................3.19
Temporary Release
.........................................3.19
Immunity From Liability
....................................3.19
Notification of Release to County Behavioral
Health Director and Peace Officer
...................3.19

Chapter 3 — Contents
©CALIFORNIA HOSPITAL ASSOCIATION
CHA Mental Health Law Manual 2019
B. Review of Commitment for 14 Additional
Days of Intensive Treatment ......................3.20
Certification Review Hearings ..........................3.20
Judicial Review Pursuant to a Writ of
Habeas Corpus
..............................................3.22
Patient’s Right to Deny Release of
Information
.....................................................3.23
C. Additional Intensive Treatment for
Suicidal Patient
............................................3.23
Conditions for Confinement ............................3.23
Completion of a Second Notice of
Certification
....................................................3.23
Required Form of Second Notice of
Certification
....................................................3.23
Delivery of Copies of Second Notice of
Certification
...................................................3.24
Advisement of Rights to Patient
......................3.24
Review of Intensive Treatment
......................... 3.24
Termination of Certification for Additional
Intensive Treatment for Suicidal Patient
...........3.24
Damages for Excessive Detention
...................3.24
Facility Preference
...........................................3.25
Temporary Release
.........................................3.25
Immunity From Liability
....................................3.25
D. Additional Intensive Treatment for
Gravely Disabled Person
.............................3.25
Optional Additional 30-Day Period of
Intensive Treatment
.........................................3.25
Conditions for Confinement
.............................3.25
Notice Required
..............................................3.26
Required Form of Second Notice of
Certification
....................................................3.26
Delivery of Copies of Second Notice of
Certification
...................................................3.26
Judicial Review of Intensive Treatment
.............3.26
Damages for Excessive Detention
...................3.27
Facility Preference
...........................................3.27
Immunity From Liability
....................................3.27
Temporary Release
.........................................3.27
Evaluation of Need for Temporary
Conservatorship
.............................................3.28
E. Additional Confinement for a
Person Dangerous to Others
(Post-Certification Procedures)
.................3.28
Grounds for Additional Confinement ................3.28
Petition by Professional Person
.......................3.28
Court Proceedings
..........................................3.29
Termination of Additional Intensive Treatment
and Placement on Outpatient Status
............... 3.29
Immunity From Liability
....................................3.30
F. Additional Treatment for Gravely
Disabled Person (LPS Conservatorship)
...3.31
Conservatorship Recommendation .................3.31
Investigator Action
..........................................3.31
Court Hearing
................................................. 3.31
Conservatorship Established
........................... 3.31
Expiration of Conservatorship
.........................3.32
VI. DETENTION OF PATIENT IN A
NONDESIGNATED FACILITY
.................... 3.32
A. Immunity for Detaining Patient ..................3.32
B. Immunity for Actions of Patient After
Release
.........................................................3.32
C. Hospitals Covered by This Law .................. 3.33
D. Relationship to Other Laws ........................3.33
E. Credit for Time Detained ............................3.33
VII. COURT-ORDERED EVALUATION OF
PERSONS WHO MAY HAVE A MENTAL
HEALTH DISORDER
................................ 3.33
VIII. REPORTING PATIENT ESCAPE,
DISAPPEARANCE, RELEASE OR
TRANSFER ........................................... 3.33
IX. INVOLUNTARY OUTPATIENT
TREATMENT
.......................................... 3.33
A. Contents of Petition ....................................3.33
B. Who May Initiate a Petition ......................... 3.34
C. Procedure .....................................................3.34
FORMS & APPENDICES
12-1
S
Request for Voluntary Admission and Authorization
for Treatment
12-2 Statement of Professional Person Responsible for
Minor’s Admission
12-3
S
Notice to Minors
12-4 Certification of Admitting Physician
12-5 Application for Involuntary Admission — Inebriates
12-6
S
Notice of Certification for Intensive Treatment
12-7
S
Advisement of Rights — Involuntary Patient
12-8
S
Leave of Absence from Psychiatric Service
12-9
S
Request for Release From Involuntary Treatment
12-10
S
Notice of Certification for Second Involuntary
14-Day Period for Intensive Treatment —
Suicidal Patient
12-11 Petition for Postcertification Treatment of Imminently
Dangerous Person
12-12 Detention of Patient With Psychiatric Emergency in
a Nondesignated Health Facility (Health and Safety
Code Section 1799.111)
12-A Summary of Lanterman-Petris-Short Act’s Provision
for Involuntary Evaluation and Treatment and Right
of Review

3 Voluntary Admission and Involuntary
Detainment for Mental Health
Treatment
3.1
©CALIFORNIA HOSPITAL ASSOCIATION
I. INTRODUCTION
A. Background
This chapter discusses the rights and procedural
protections that California law gives to persons who
are voluntarily or involuntarily detained for mental
health services, including evaluation and treatment of a
mental health disorder, inebriation or drug use. These
rights and protections are set forth primarily in the
Lanterman-Petris-Short (LPS) Act [Welfare and Institutions
Code Section 5000 et seq.].
Patients who are a danger to self or others or gravely
disabled may be evaluated and treated on an involuntary
basis under two different sets of laws:
1. Welfare and Institutions Code Section 5150 et seq.,
which allows a patient to be held in a facility that is
designated for these purposes by the county and
approved by the California Department of Health
Care Services. Patients may be detained for up to 72
hours (longer if specified criteria are met). Designated
facilities may be general acute care hospitals or acute
psychiatric hospitals. Patients treated under this set of
laws are given the special rights described in chapter
16, and are protected by strict confidentiality laws in
the Welfare and Institutions Code, described in CHA’s
California Health Information Privacy Manual. (For
more information about detaining these patients, see
III.“Admission and Treatment of Involuntary Patients,”
page3.7.)
2. Health and Safety Code Section 1799.111, which
allows a patient to be held in a non-designated facility
for up to 24 hours while the facility tries to find an
appropriate placement for the patient in a facility that
provides mental health services. Non-designated
facilities are general acute care hospitals, and usually
do not have a psychiatric unit. Patients treated under
this law are not given the special rights described in
chapter 16, and are protected by the confidentiality
laws in the Confidentiality of Medical Information Act.
(For more information about detaining these patients,
see VI.“Detention of Patient in a Nondesignated
Facility,” page3.32.)
B. Patient Privacy Considerations
This chapter describes several instances in which California
law requires the disclosure of protected health information
(PHI) to patients’ rights advocates, independent clinical
reviewers, certification review hearing officers, county
behavioral health directors and others.
The federal privacy regulations issued under the Health
Insurance Portability and Accountability Act (HIPAA) of
1996 permit health care providers to disclose PHI to the
persons or entities listed above under several provisions:
1. For purposes of health care oversight [45 C.F.R.
Section 164.512(d)(1)(iv)]. The California Department of
Public Health (CDPH) is one example of a health care
oversight agency. A health care oversight agency also
includes a person or entity acting under a contract
(or other grant of authority) from a government entity
(including a county) to enforce civil rights laws [45
C.F.R. Section 164.501]. Although the HIPAA rules
are not completely clear on this point, if a particular
disclosure of information is required to be made by
California law (or a federal law) to a county patient’s
rights advocate, an independent clinical reviewer
approved by a county, or a certification review hearing
officer approved by the county for the purpose of
determining whether a patient’s civil rights are being
properly protected (rather than the patient being
hospitalized illegally), the disclosure is likely permissible
under the HIPAA provisions for health care oversight.
Alternatively, the disclosure may be permissible under
the HIPAA provision for disclosures “required by law”
[45 C.F.R. Section 164.512(a)].
2. For law enforcement purposes. These uses/
disclosures have certain requirements that must be
met prior to disclosure, as described in this chapter
and chapters 6 and 7.

CHA Mental Health Law Manual 2019
3.2
©CALIFORNIA HOSPITAL ASSOCIATION
3. For judicial and administrative proceedings. These
uses/disclosures have certain requirements that must
be met prior to disclosure. When disclosure of PHI
is made for purposes of judicial or administrative
proceedings (such as a writ of habeas corpus), a
hospital should consult legal counsel regarding the
advisability of filing documents with the court under
seal and/or obtaining a protective order.
4. To prevent or lessen a serious and imminent threat
to the health or safety of the patient or the public
[45 C.F.R. Section 164.512(j)]. (See IX.“Potentially
Dangerous Patients: Duty to Warn Potential Victims
and Notify Law Enforcement,” page7.33.)
Given the high sensitivity of mental health information,
a hospital should consult legal counsel if a question
arises as to whether it is permissible to disclose PHI in a
particular instance.
II. ADMISSION AND TREATMENT OF
VOLUNTARY PATIENTS
A. Voluntary Admission of Adult Patients
Adults, including persons under conservatorship, may
be voluntarily admitted for treatment of mental disorders,
alcoholism or drug abuse.
AUTHORITY TO REQUEST VOLUNTARY ADMISSION
The patient or, if applicable, the patient’s conservator, may
request admission. Welfare and Institutions Code Section
5350 provides for the appointment of a conservator of the
estate, or of the person and the estate, for a person who
is gravely disabled as a result of a mental health disorder
or impairment by chronic alcoholism. Conservatorship
proceedings are discussed under F.“Additional Treatment
for Gravely Disabled Person (LPS Conservatorship),”
page3.31.
The conservator has the right, if specified in the court order,
to place his or her conservatee in a medical, psychiatric,
nursing, or other state-licensed facility, or a state hospital,
county hospital, hospital operated by the Regents of the
University of California, a U.S. government hospital, or other
nonmedical facility approved by the California Department
of Social Services (DSS) or an agency accredited by the
California Department of Health Care Services (DHCS), or,
in the case of chronic alcoholism, in a county alcoholic
treatment center [Welfare and Institutions Code Section
5358].
An agent designated in an advance health care directive
may not authorize voluntary or involuntary admission of a
patient to a mental health facility [Probate Code Section
4652]. (See chapter 2 for information about advance
directives.)
The law recognizes two types of “gravely disabled”
conservatees. Each type is subject to different placement
parameters, as described below.
Unable to Provide for Basic Needs
Welfare and Institutions Code Section 5008(h)(1)(A) defines
“grave disability” as a condition in which a person, as a
result of a mental health disorder, is unable to provide for
his or her basic personal needs for food, clothing, or shelter.
For a conservatee who is gravely disabled under this
definition, the conservator must place the patient in the
least restrictive alternative placement as designated by
the court. The conservator may transfer the patient to a
less restrictive placement without a further court hearing or
court order.
Mentally Incompetent to Stand Trial
Welfare and Institutions Code Section 5008(h)(1)(B) defines
“grave disability” as a condition in which a person has
been found mentally incompetent under Penal Code
Section 1370 (mentally incompetent to stand trial) and all of
the following facts exist:
1. The complaint, indictment or information pending
against the person at the time of commitment charges
a felony involving death, great bodily harm, or a serious
threat to the physical well-being of another person, and
the indictment or information has not been dismissed.
2. There has been a finding of probable cause on a
complaint pursuant to Penal Code Section 1368.1(a)(2)
(which relates to a felony involving death, great bodily
harm, or a serious threat to the physical well-being of
another person), a preliminary examination pursuant to
Penal Code Section 859b (this is a particular type of
hearing), or a grand jury indictment, and the complaint,
indictment, or information has not been dismissed.
3. As a result of a mental health disorder, the person is
unable to understand the nature and purpose of the
proceedings against him or her and to assist counsel in
the conduct of his or her defense in a rational manner.
4. The person represents a substantial danger of physical
harm to others by reason of a mental disease, defect,
or disorder.

Chapter 3 — Voluntary Admission and Involuntary Detainment for Mental Health Treatment CHA
3.3
©CALIFORNIA HOSPITAL ASSOCIATION
For a conservatee who is gravely disabled under this
definition, the conservator must place the patient in a
placement that achieves the purposes of treatment of the
conservatee and protection of the public. The conservator
may not transfer the patient without written notice to
the court.
CAUTION: TYPE OF CONSERVATORSHIP
A conservatorship under LPS (which is found in the
Welfare and Institutions Code) is different from a
conservatorship under the Probate Code. If a patient is
under a conservatorship, hospitals should obtain and
carefully review the conservatorship documents issued by
the court to determine the type of conservatorship and the
conservator’s scope of authority. A patient may be subject
to both an LPS conservatorship and a Probate Code
conservatorship; however, this is not common.
LPS Conservatorship
An LPS conservatorship is meant for psychiatric patients.
The purpose of an LPS conservatorship is the provision
of individualized psychiatric treatment, supervision, and
placement for a patient who is gravely disabled as a result
of a mental health disorder or impairment by chronic
alcoholism. An LPS conservator may authorize the
admission of the conservatee to a mental health facility.
An LPS conservator may consent to, or refuse, routine
medical treatment (other than psychiatric treatment) only if
the court order establishing the conservatorship specifically
provides this authority. An LPS conservator usually
may not consent for surgery or other complex medical
procedures without an additional, specific court order.
(See F.“Additional Treatment for Gravely Disabled Person
(LPS Conservatorship),” page3.31, for more information
about LPS conservatorships. See C.“Adults Under
Conservatorship,” page2.15, for more information about
an LPS conservator’s authority to consent to, or refuse,
nonpsychiatric medical treatment.)
Probate Code Conservatorship
A conservatorship under the Probate Code is meant
to ensure that the conservatee’s basic needs for food,
clothing, shelter, money management, and health care are
met. Conservatees may be comatose, developmentally
disabled, or have dementia or other medical problems.
Some patients under a Probate Code conservatorship may
have the ability to make their own health care decisions,
while others may not — the letters of conservatorship will
state the authority of the conservator. A Probate Code
conservator may not authorize admission to a mental
health facility. (See C.“Adults Under Conservatorship,”
page2.15, for more information about Probate Code
conservatorships.)
WRITTEN APPLICATION FOR VOLUNTARY ADMISSION
A patient should be voluntarily admitted only if the “Request
for Voluntary Admission and Authorization for Treatment”
form (CHA Form 12-1) or a similar form is completed.
Completion by Physician
The attending physician should certify that the voluntary
patient is mentally competent to understand the nature
of his or her admission and the treatment to be rendered.
The certification should be executed upon admission or
as soon as possible thereafter [Welfare and Institutions
Code Section 6002]. A certification form is included in
the “Request for Voluntary Admission and Authorization for
Treatment” form (CHA Form 12-1).
Copies
One copy of the written application should be made. The
original should be placed in the patient’s medical record;
the copy should be given to the patient or the person
who made the written request for admission on behalf of
the patient.
SEARCH OF THE PATIENT, POSSESSIONS AND ROOM
The “Request for Voluntary Admission and Authorization for
Treatment” form (CHA Form 12-1) notifies the patient that
hospital employees will inventory the patient’s possessions
and remove items that may create a danger to the patient,
other patients, visitors or hospital staff.
As a reminder, mental health patients have the right
to keep and use personal possessions and to have
access to individual storage space for private use. Of
course, this does not mean that patients have the right
to keep potentially dangerous items. However, under
some circumstances a search and/or removal of patient
possessions may constitute a denial of rights, which is
permissible but must be documented. (See II.“Patient
Rights Under State Law,” page4.1, for detailed
information about patient rights and the requirements to be
followed when denying a right.) The hospital should consult
its legal counsel regarding the development of policies and
procedures regarding searches. (See also V.“Searching
Patients and Their Belongings,” page6.13.)

CHA Mental Health Law Manual 2019
3.4
©CALIFORNIA HOSPITAL ASSOCIATION
OTHER ADMISSION FORMS
At the time of admission, the signature of the patient
or the patient’s legal representative on the “Conditions
of Admission” (CHA Form 8-1) and other admission
documents should also be obtained. If the patient lacks
capacity to agree or refuses to agree to admission
documents, the facility should attempt to obtain the
patient’s signature once he or she has regained capacity or
is willing to sign.
RIGHT TO LEAVE THE HOSPITAL
A voluntary adult patient may leave the hospital, clinic, or
institution at any time by giving notice to any member of
the hospital staff of the patient’s desire to leave and by
completing usual discharge procedures. A conservatee
may leave in a like manner if notice is given by the
patient’s conservator.
B. Voluntary Admission of Minors to Private
Facilities
As a general rule, a parent may consent to a minor’s
admission for inpatient mental health treatment, subject
to the limitations described below. There are special
requirements that apply to certain treatments a minor might
receive (e.g., antipsychotic medications and convulsive
therapy), which are discussed in X.“Treatments That
Require Special Consent,” page2.42.
California law specifies procedures and requirements for
the voluntary admission to private acute psychiatric facilities
of minors age 14 and older. State and county hospitals are
not required to follow these procedures and requirements
[Welfare and Institutions Code Sections 6002.10-6002.40].
“Voluntary admission” means, for a minor patient, that
the parent, guardian or other legal representative wants
the minor to be admitted to the hospital. It does not
necessarily mean that the minor agrees or acquiesces
to the hospitalization. (See VII.“Who May Give Consent:
Minors,” page2.24, regarding who may be considered a
legal representative of a minor.)
MINORS AFFECTED
The admission procedures apply to a minor between 14
and 18 years of age admitted to a private mental health
facility and whose admitting diagnosis or condition is
either a mental health disorder only or a mental health
disorder and a substance use disorder. Admission based
on substance use disorder alone is not covered by these
procedures. Additionally, the law applies only when the
costs of treatment are paid or reimbursed by a private
insurer or private health plan or Medi-Cal, not when the
parent personally pays for the service.
Mental Health Disorder
Although resistance to treatment may be a product of a
mental health disorder, the resistance does not, in itself,
imply the presence of a mental health disorder or constitute
evidence that the minor meets admission criteria. A minor
must not be considered to have a mental health disorder
solely for exhibiting behaviors specified under Welfare and
Institutions Code Section 601 (refusal to obey parents,
violation of curfew, or truancy) or 602 (commission of a
crime).
Exclusions
The admission procedures do not apply to the
following minors:
1. Minors under 14 years of age.
2. Minors who are legally emancipated. Minors who are
legally emancipated cannot be voluntarily admitted
by a parent or guardian. They should be treated as
voluntary or involuntary adults.
3. Minors who are detained involuntarily on a 72-hour
hold as gravely disabled or as a danger to self or
others under the Lanterman-Petris-Short Act, Welfare
and Institutions Code Sections 5585.50 and 5585.53.
(These procedures would apply, however, at the time
of a change to voluntary status of a minor who was
initially admitted on a 72-hour hold if the other criteria
are met.)
4. Minors who are voluntarily committed as wards of the
juvenile court under Welfare and Institutions Code
Section 6552 (see below).
5. Minors who have been declared dependents of the
juvenile court under Welfare and Institutions Code
Section 300 (abuse, neglect or abandonment) or
wards of the court under Welfare and Institutions Code
Section 602 (commission of a crime).
Wards and dependents of the juvenile court may, with
the advice of counsel, voluntarily request inpatient mental
health services [Welfare and Institutions Code Section
6552]. The juvenile court must authorize the minor to
request these services first. The juvenile court may
authorize the minor to request mental health services if the
court is satisfied from the evidence that:
1. The minor suffers from a mental health disorder
which may reasonably be expected to be cured or

Chapter 3 — Voluntary Admission and Involuntary Detainment for Mental Health Treatment CHA
3.5
©CALIFORNIA HOSPITAL ASSOCIATION
ameliorated by a course of treatment offered by the
hospital, facility or program in which the minor wishes
to be placed; and
2. There is no other available hospital, facility or program
that might better serve the minor’s medical needs and
best interest.
The juvenile court may issue an order to the minor and to
the person in charge of the hospital, facility or program
ordering that the minor be returned to the juvenile court if
the minor tries to leave before being discharged.
REQUIRED PROCEDURES AT ADMISSION
The facility must see that the following requirements
are met:
1. Prior to accepting the written authorization for
treatment, a facility representative must give a full
explanation of the facility’s treatment philosophy to
the parent, guardian or other person entitled to the
minor’s custody. This explanation must be given orally
and in writing, and must include, where applicable,
the use of seclusion, restraints, medication, and the
degree of involvement of family members in the minor’s
treatment. This must be documented in the minor’s
medical record. The “Statement of Professional Person
Responsible for Minor’s Admission” form (CHA Form
12-2) may be used to document the oral discussion.
Each facility should prepare a written document to
be given to the minor or the minor’s representative.
The admitting parent’s or guardian’s signature on the
“Conditions of Admission” (CHA Form 8-1) and other
admission documents should also be obtained.
2. As part of the admission process, the professional
responsible for the minor’s admission must affirm in
writing that the minor meets the following required
admission criteria:
a. That the minor has a mental health disorder,
or a mental health disorder and a substance
use disorder.
b. That inpatient treatment in the facility is reasonably
likely to be beneficial to the minor’s mental
health disorder.
c. That inpatient treatment in the facility is the least
restrictive, most appropriate available setting in
which to treat the minor, within the constraints of
reasonably available services, facilities, resources,
and financial support.
The “Statement of Professional Person Responsible
for Minor’s Admission” form (CHA Form 12-2) may be
used for this purpose.
3. Upon admission, the facility is required to do
the following:
a. Notify the minor in writing of the availability of an
independent clinical review of further inpatient
treatment. This notice must be witnessed and
signed by a facility representative.
b. Within one working day, notify the county patients’
rights advocate of the minor’s admission.
c. Provide each minor with a booklet prepared by
DHCS outlining the rights of minors in mental
health facilities. The booklet must include the
telephone number of the local advocate and the
hours that the advocate may be reached.
The “Notice to Minors” (CHA Form 12-3) may be used to
provide the written notice to the minor of the availability
of the independent clinical review and to document the
minor’s receipt of the minor’s rights booklet.
INDEPENDENT CLINICAL REVIEW
The following guidelines apply to the independent
clinical review.
Timing
The minor may request an independent clinical review up to
10 days after admission. The review must take place within
five days of the request. The minor may rescind the request
at any time.
Notification and Participation of Patients’ Rights
Advocate
If the minor requests a review, the facility must notify the
patients’ rights advocate of this within one working day of
the request. The advocate must provide information and
assistance to the minor in a manner least disruptive to
patient care in the facility.
Selection of the Person Who Conducts the Hearing
The independent clinical review must be conducted by a
licensed psychiatrist with training and experience in treating
adolescent psychiatric patients. This reviewer must be
a neutral party to the review, having no direct financial
relationship with the treating clinician nor a personal or
financial relationship with the minor’s parents or guardian.
The reviewer must be assigned, on a rotating basis, from
a list prepared by the facility and approved by the county
behavioral health director (see Welfare and Institutions
Code Section 6002.25 about the annual submission and
approval process). The reviewer may be an active member
of the medical staff of the facility so long as he or she has

CHA Mental Health Law Manual 2019
3.6
©CALIFORNIA HOSPITAL ASSOCIATION
no direct financial relationship with the facility (including,
but not limited to, an employment or other contractual
arrangement with the facility) except for compensation
received for the service of providing clinical reviews.
Setting
The review must take place at the facility in a location that
assures privacy and is compatible with, and least disruptive
to, the treatment being provided to the minor. The review
must be held in an informal setting to minimize the anxiety
of the minor and his or her parents and to promote
communication and cooperation among those involved.
Closed Review
The review must be closed to all but the minor, the parents
or legal guardian, a facility representative, the minor’s
advocate, the reviewer, and the person who presents
information in favor of, or in opposition to, the inpatient
treatment. The reviewer has discretion to limit the number
of participants.
Legal Representation
No party may have legal representation in the
review process.
Interpreters
If a party to the review does not comprehend the language
used at the review, the reviewer is responsible for retaining
an interpreter.
Record of the Review
The reviewer must keep a record of the proceeding.
Participation by Minor
The minor has the right to be present, to be assisted by
the patients’ rights advocate, and to question persons
recommending inpatient treatment. The reviewer must be
informed if the minor has received medication while an
inpatient and of the probable effects of the medication. If
the minor is unwilling to attend, the review must be held
without the minor, with the advocate representing the minor.
Information Considered
All reasonably available clinical data relevant to establishing
whether the minor meets the admission criteria must be
considered by the reviewer. The reviewer must privately
interview the minor and must consult the treating clinician
to review alternative treatment options. The person who
presents the clinical information in favor of inpatient
treatment must inform the person who conducts the
interview of the proposed treatment plan for the minor
and, if known, whether the minor has had any previous
independent clinical reviews at any facility, and the
results thereof.
Standard of Review
The standard of review must be:
1. Whether the minor continues to have a mental
disorder;
2. Whether further inpatient treatment is reasonably
likely to be beneficial to the minor’s mental health
disorder; and
3. Whether placement in the facility represents the
least restrictive, most appropriate available setting
in which to treat the minor, within the constraints of
reasonably available services, facilities, resources, and
financial support.
Decision
The reviewer must render a binding decision after
considering all of the clinical information.
If the reviewer determines that further inpatient treatment
is reasonably likely to be beneficial to the minor’s mental
health disorder and that placement in the facility is the least
restrictive, most appropriate available setting in which to
treat the minor, the minor’s inpatient treatment must be
authorized. This determination terminates upon the minor’s
discharge from the facility.
If the reviewer determines that further inpatient treatment
is not reasonably likely to be beneficial to the minor’s
mental health disorder or is not the least restrictive, most
appropriate available setting, the minor must be released
from the facility to a custodial parent or guardian on the
same day the determination is made.
Immunity From Liability
If the minor is released pursuant to the reviewer’s
determination, neither the attending psychiatrist, any
licensed health professional providing treatment to the
minor in the facility, the psychiatrist who releases the
minor, nor the facility in which the minor was admitted or
treated shall be civilly or criminally liable for any conduct
of the released minor (or the conduct of a parent, legal
guardian, or other persons entitled to custody of the
minor). There is an exception to this immunity only to the
extent that a person defined as a psychotherapist under
Evidence Code Section 1010 has a duty to warn if the
patient communicated to the psychotherapist a serious
threat of physical violence against a reasonably identifiable

Chapter 3 — Voluntary Admission and Involuntary Detainment for Mental Health Treatment CHA
3.7
©CALIFORNIA HOSPITAL ASSOCIATION
victim or victims. (See A.“Duty to Warn Potential Victims,”
page7.33, and B.“Duty to Notify Law Enforcement
Agency,” page7.33, for information about these duties.)
Costs
If a private insurer, certified medical plan or private health
care service plan is financially responsible for the costs of
medically necessary mental health services provided to a
minor, then the costs of the clinical review (including the
costs of the patients’ rights advocate and the interpreter, if
any) must be borne by the insurer, certified medical plan or
health plan. For Medi-Cal patients, the costs of the review
must be borne by the county.
Annual Reports
Mental health facilities must prepare and submit annually to
DHCS information including, but not limited to:
1. The number of minors admitted by diagnosis, length of
stay, and source of payment; and
2. The number of requests for an independent clinical
review by diagnosis, source of payment, and outcome
of the independent clinical review.
The California Department of Public Health is required to
monitor compliance with this reporting requirement during
surveys. [Welfare and Institutions Code Section 6002.40(c)]
C. Voluntary Admission of Minors to State and
County Facilities
State and county facilities are excluded from the notice
and review requirements described above. However, in the
case In re Roger S., 19 Cal.3d 921 (1977), the California
Supreme Court held that a parent or guardian may not
admit a minor 14 years of age or older to a state hospital
without a pre-admission hearing to determine whether
the minor is mentally ill. In addition, the U.S. Supreme
Court ruled that postadmission independent review is also
required [Parham v. J.R., 442 U.S. 584 (1979)]. These
rulings do not apply to minors under 14 years of age or to
private facilities (see B.“Voluntary Admission of Minors to
Private Facilities,” page3.4).
“Voluntary admission” means, for a minor patient, that
the parent, guardian or other legal representative wants
the minor to be admitted to the hospital. It does not
necessarily mean that the minor agrees or acquiesces to
the hospitalization.
III. ADMISSION AND TREATMENT OF
INVOLUNTARY PATIENTS
The Lanterman-Petris-Short (LPS) Act establishes
procedural requirements under which persons dangerous
to themselves or others or gravely disabled as a result of a
mental health disorder, inebriation, or the use of narcotics
or restricted dangerous drugs may be involuntarily
detained for specified periods for evaluation and treatment,
which include:
1. An initial 72-hour hold for evaluation and treatment;
2. An additional 14-day intensive treatment period
(see A.“Detention for 14-Day Intensive Treatment,”
page3.17); and
3. An additional 30-day period of intensive treatment
after the 14-day period of treatment (where the county
board of supervisors authorizes such a procedure) (see
D.“Additional Intensive Treatment for Gravely Disabled
Person,” page3.25); and
4. Further confinement depending on the
person’s condition:
a. A second 14-day intensive treatment period
for persons who are imminently suicidal (see
C.“Additional Intensive Treatment for Suicidal
Patient,” page3.23);
b. An additional 180-day confinement for persons
who present a demonstrated danger of substantial
physical harm to others (see E.“Additional
Confinement for a Person Dangerous to Others
(Post-Certification Procedures),” page3.28); or
c. Confinement pursuant to a conservatorship
for persons who are gravely disabled (see
D.“Additional Intensive Treatment for Gravely
Disabled Person,” page3.25).
A chart that may be useful in understanding LPS, entitled
“Summary of the Lanterman-Petris-Short Act’s Provision for
Involuntary Evaluation and Treatment and Right of Review”
(CHA Table 12-A), is included in the back of this manual.
A. Definitions
“Assessment” means the determination of whether
a person shall be evaluated and treated pursuant to
Welfare and Institutions Code Section 5150 [Welfare and
Institutions Code Section 5150.4].
“Attending staff” is defined as a person who has
responsibility for the care and treatment of the patient, as
designated by the local mental health director, and who

CHA Mental Health Law Manual 2019
3.8
©CALIFORNIA HOSPITAL ASSOCIATION
is on the staff of a designated facility [Title 9, California
Code of Regulations, Section 823]. “A member of the
attending staff who is authorized to admit a person to
a designated facility” is defined as a physician who is on
the psychiatric attending staff of either a public or private
designated facility to which the patient will be admitted.
“Crisis intervention” consists of an interview or series
of interviews within a brief period of time, conducted by
qualified professionals, and designed to alleviate personal
or family situations that present a serious and imminent
threat to the health or stability of the person or the family.
The interview or interviews may be conducted in the home
of the person or family, or on an inpatient or outpatient
basis with therapy or other services, as appropriate. The
interview or interviews may include family members,
significant support persons, providers, or other entities or
individuals, as appropriate and as authorized by law. Crisis
intervention may, as appropriate, include suicide prevention,
psychiatric, welfare, psychological, legal, or other social
services. [Welfare and Institutions Code Section 5008(e)]
“Evaluation” consists of multidisciplinary professional
analyses of a person’s medical, psychological, educational,
social, financial, and legal conditions as may appear to
constitute a problem. Persons providing evaluation services
must be properly qualified professionals and may be
full-time, part-time, or contract employees of an agency
providing face-to-face evaluation services, including
telehealth. [Welfare and Institutions Code Section 5008(a)]
“Gravely disabled” means either of the following:
1. A condition in which a person, as a result of a mental
health disorder or, in some cases, chronic alcoholism,
is unable to provide for his or her basic personal needs
for food, clothing or shelter [Welfare and Institutions
Code Section 5008(h)(1)(A)]; or
2. A condition in which a person has been found mentally
incompetent under Penal Code Section 1370 (mentally
incompetent to stand trial) and all of the following
facts exist:
a. The complaint, indictment or information pending
against the person at the time of commitment
charges a felony involving death, great bodily harm,
or a serious threat to the physical well-being of
another person, and the indictment or information
has not been dismissed.
b. There has been a finding of probable cause on
a complaint pursuant to Penal Code Section
1368.1(a)(2) (which relates to a felony involving
death, great bodily harm, or a serious threat to
the physical well-being of another person), a
preliminary examination pursuant to Penal Code
Section 859b (this is a particular type of hearing),
or a grand jury indictment, and the complaint,
indictment, or information has not been dismissed.
c. As a result of a mental health disorder, the person
is unable to understand the nature and purpose of
the proceedings taken against him or her and to
assist counsel in the conduct of his or her defense
in a rational manner.
d. The person represents a substantial danger of
physical harm to others by reason of a mental
disease, defect, or disorder.
[Welfare and Institutions Code Section 5008 (h)(1)(B)]
The term “gravely disabled” does not include persons with
intellectual disabilities by reason of that disability alone.
[Welfare and Institutions Code Section 5008(h)].
Notwithstanding Welfare and Institutions Code Section
5008(h), a person is not gravely disabled if that person
can survive safely without involuntary detention with the
help of responsible family, friends, or others who are willing
and able to help provide for the person’s basic personal
needs for food, clothing, or shelter. However, unless
family, friends, or others specifically indicate in writing their
willingness and ability to help, they must not be considered
willing or able to provide this help [Welfare and Institutions
Code Sections 5250(d) and 5350(e)]. This exception
does not apply to patients who are considered gravely
disabled under Welfare and Institutions Code Section
5008(h)(1)(B) (mentally incompetent to stand trial).
“Gravely disabled minor” is a minor who, as a result of
a mental health disorder, is unable to use the elements of
life that are essential to health, safety, and development,
including food, clothing, and shelter, even though provided
to the minor by others. Intellectual disability or other
developmental disabilities, epilepsy, alcoholism, other
drug abuse, or repeated antisocial behavior do not, by
themselves, constitute a mental health disorder. [Welfare
and Institutions Code Section 5585.25]
”Professional person in charge of a facility” means a
psychiatrist, psychologist, social worker, marriage and
family therapist, or registered nurse with a master’s degree
in psychiatric or public health nursing who is designated by
the governing board of the facility or person having control
of the facility as the professional person clinically in charge
of the facility for purposes of LPS. The designation must be
in writing. [Title 9, California Code of Regulations, Sections
623-627 and 822]
“Mental health disorder” is a term that is not defined in
the law. According to the California Attorney General, the

Chapter 3 — Voluntary Admission and Involuntary Detainment for Mental Health Treatment CHA
3.9
©CALIFORNIA HOSPITAL ASSOCIATION
reference to “mental disorder” (or “mental health disorder,”
the term used as of Jan. 2014) in Welfare and Institutions
Code Section 5150 draws no distinction between disorders
of inorganic or organic origin and therefore includes,
together with inorganic mental disorders, Alzheimer’s
disease, brain injuries and other organic brain disorders [72
Ops.Cal.Atty.Gen. 41 (1989)].
B. Facility Designation
Involuntary treatment and evaluation must take place only
in a facility that is designated for such purposes by the
county and approved by DHCS. These facilities are called
“designated facilities.”
C. Interactions With Peace Officers
Mental health professionals may not interfere with peace
officers who are transporting a person to a designated
facility for assessment under Welfare and Institutions Code
Section 5150. These laws were passed to prevent mental
health personnel from refusing to take a patient and telling
law enforcement officers to take the patient to jail instead,
and to prevent mental health personnel from unreasonably
detaining law enforcement officers. [Welfare and Institutions
Code Sections 5150.1 and 5150.2]
Welfare and Institutions Code Section 5150.1 provides:
No peace officer seeking to transport, or having
transported, a person to a designated facility for
assessment under Welfare and Institutions Code Section
5150, may be instructed by mental health personnel to
take the person to, or keep the person at, a jail solely
because of the unavailability of an acute bed, nor may
the peace officer be forbidden to transport the person
directly to the designated facility. No mental health
employee from any county, state, city, or any private
agency providing Short-Doyle psychiatric emergency
services may interfere with a peace officer performing
duties under Welfare and Institutions Code Section
5150 by preventing the peace officer from entering a
designated facility with the person to be assessed, nor
may any employee of such an agency require the peace
officer to remove the person without assessment as a
condition of allowing the peace officer to depart.
Welfare and Institutions Code Section 5150.2 provides:
In each county whenever a peace officer has transported
a person to a designated facility for assessment under
Welfare and Institutions Code Section 5150, that officer
shall be detained no longer than the time necessary
to complete documentation of the factual basis of the
detention under Welfare and Institutions Code Section
5150 and a safe and orderly transfer of physical custody
of the person. The documentation must include detailed
information regarding the factual circumstances and
observations constituting probable cause for the peace
officer to believe that the individual required psychiatric
evaluation under the standards of Welfare and
Institutions Code Section 5150.
Each county must establish disposition procedures
and guidelines with local law enforcement agencies
as necessary to relate to persons not admitted for
evaluation and treatment and who decline alternative
mental health services and to relate to the safe and
orderly transfer of physical custody of persons under
Welfare and Institutions Code Section 5150, including
those who have a criminal detention pending.
IV. INVOLUNTARY DETENTION OF THE PATIENT
ON A 72-HOUR HOLD
A. Patients With a Mental Health Disorder
CONDITIONS FOR DETENTION
Welfare and Institutions Code Section 5150 states that
when a person, as a result of a mental health disorder,
is a danger to self or others or is gravely disabled, any
of the following persons may, upon probable cause,
take the person into custody and place the person in a
designated facility:
1. A peace officer (including park peace officers and
regional park peace officers);
2. A professional person in charge of a designated
facility; or
3. A member of the attending staff of a designated facility
who is authorized to admit a patient involuntarily; or
4. Any other professional person designated by
the county.
The person may be taken into custody for up to 72 hours
for assessment, evaluation, and crisis intervention, or
placement for evaluation and treatment in a designated
facility. (If the patient is a minor, see E.“Special
Requirements for a Minor,” page3.16.) At a minimum,
assessment and evaluation must be conducted and
provided on an ongoing basis. Crisis intervention may be
provided concurrently with assessment, evaluation, or
other services.
WRITTEN APPLICATION REQUIRED
The receiving/admitting facility must receive a written
application stating:

CHA Mental Health Law Manual 2019
3.10
©CALIFORNIA HOSPITAL ASSOCIATION
1. The circumstances under which the person’s condition
was called to the attention of the peace officer,
professional person in charge of the facility, member of
the attending staff, or professional person designated
by the county.
2. That the officer, member of the attending staff, or
professional person has probable cause to believe that
the person is, as a result of a mental health disorder, a
danger to self or others or gravely disabled.
3. Whether the historical course of the person’s mental
disorder was considered in this determination (see
below).
A state law has been enacted, effective Jan. 1, 2019, to
clarify that a copy of the application must be treated as the
original. Formerly, some ambulance companies and other
entities were declining to provide services to involuntary
patients without having the original document.
When determining if probable cause exists to detain a
person under Welfare and Institutions Section 5150, all
available relevant information about the historical course of
the person’s mental disorder must be considered if it has a
reasonable bearing on the determination as to whether the
person is a danger to self or others or is gravely disabled.
This includes evidence presented by a person who has
provided or is providing mental health or related support
services and evidence presented by family members.
[Welfare and Institutions Code Section 5150.05]
If the probable cause is based on the statement of
someone else, that person may be held liable in a civil
action for intentionally giving a statement which he or she
knows is false.
Recommended Form
In order to comply with the requirements of Welfare and
Institutions Code Section 5150 for a written application,
it is recommended that the DHCS 1801/DMH MH
302, “Application for Assessment, Evaluation, and Crisis
Intervention or Placement for Evaluation and Treatment,”
be used. This form may be found at www.dhcs.ca.gov/
formsandpubs/forms/pages/mental_health-forms.aspx.
CHA recommends supplementing the state form with the
“Certificate of Admitting Physician” (CHA Form 12-4).
NOTICE BY PERSON TAKING PATIENT INTO CUSTODY
When a person is taken into custody under Welfare and
Institutions Code Section 5150, the person who makes
the detention must provide the following information orally
in a language or modality accessible to the person. If
the person cannot understand an oral advisement, the
information must be provided in writing. This information
is included in the DHCS 1801/DMH MH 302 form. The
information should be substantially in the following form:
My name is
.
I am a
(peace officer, mental health professional, etc.)
with
(name of agency). You are not under criminal arrest,
but I am taking you for an examination by mental
health professionals at
(name of facility). You will be told your rights by the
mental health staff.
If the person is taken into custody at his or her residence,
the person must also be told the following information in
substantially the following form:
You may bring a few personal items with you, which
I will have to approve. Please inform me if you need
assistance turning off any appliances or water. You
may make a phone call and leave a note to tell your
friends or family where you have been taken.
The designated facility must keep a record of this
advisement in the patient’s medical record that includes:
1. The name of the person detained for evaluation.
2. The name and position of the peace officer or mental
health professional taking the person into custody.
3. The date the advisement was completed.
4. Whether the advisement was completed.
5. The language or modality used to give the advisement.
6. If the advisement was not completed, a statement of
good cause for not completing the advisement. (See
F.“Denial of Patient Rights,” page4.4, regarding the
requirements for denial of a mental health patient’s
rights.)
NOTICE BY FACILITY ADMISSION STAFF
The admission staff of the designated facility is required to
give each person admitted under Welfare and Institutions
Code Section 5150 specified information about the
involuntary detention, both orally and in writing, in a
language or modality accessible to the person. The
written information must be in English and the language

Chapter 3 — Voluntary Admission and Involuntary Detainment for Mental Health Treatment CHA
3.11
©CALIFORNIA HOSPITAL ASSOCIATION
that is the person’s primary means of communication.
Accommodations for other disabilities that may affect
communications must also be provided. [Welfare and
Institutions Code Section 5150(i)] DHCS has developed a
form, DHCS 1802, “Involuntary Patient Advisement,” that
hospitals may use. The form is found at www.dhcs.ca.gov/
formsandpubs/forms/pages/mental_health-forms.aspx.
A record of this advisement must be kept in the patient’s
medical record and must include the following:
1. The name of the person performing the advisement.
2. The date of the advisement.
3. Whether the advisement was completed.
4. The language or modality used to communicate
the advisement.
5. If the advisement was not completed, a statement
of good cause (see F.“Denial of Patient Rights,”
page4.4, regarding the requirements for denial of a
mental health patient’s rights).
ASSESSMENT
The professional person in charge of a designated facility,
member of the attending staff, or professional person
designated by the county must assess the patient to
determine whether he or she can be properly served
without being detained [Welfare and Institutions Code
Section 5150(c)]. Prior to admitting a patient to a facility for
a treatment and evaluation under Welfare and Institutions
Code Section 5150, the professional person in charge
of the facility, or a designee, must assess the patient in
person to determine the appropriateness of the involuntary
detention [Welfare and Institutions Code Section 5151].
If the patient cannot be properly served without being
detained, the admitting facility must require an application
in writing (see “Written Application Required,” page3.9).
When a patient is evaluated by a professional person in
charge of a designated facility, member of the attending
staff, or professional person designated by the county and
is found to need mental health services, but is not admitted
to the facility, all available alternative services provided
under Welfare and Institutions Code Section 5150(c)
must be offered as determined by the county behavioral
health director. These services include evaluation, crisis
intervention, or other inpatient or outpatient services
provided on a voluntary basis.
When a patient is subject to detention under Welfare and
Institutions Code Section 5150, the treating facility must
obtain the patient’s medication history, if possible [Welfare
and Institutions Code Section 5332].
NOTICE OF EFFECTS OF MEDICATION
A patient detained for evaluation and treatment who
receives medications as a result of mental illness must be
given, as soon as possible after detention, written and oral
information about the probable effects and possible side
effects of the medication [Welfare and Institutions Code
Section 5152(c)].
The following information must be given orally to
the patient:
1. The nature of the mental illness or behavior that is the
reason the medication is being given or recommended.
2. The likelihood of improving or not improving without
the medication.
3. Reasonable alternative treatments available.
4. The name, type, frequency, amount, and method of
dispensing the medication, and the probable length of
time the medication will be taken.
The fact that the information has or has not been given
must be indicated in the patient’s medical record. If the
information has not been given, the facility must document
in the patient’s medical record the justification for not
providing the information.
(See also B.“Antipsychotic Medications,” page2.42, for
additional legal requirements if antipsychotic medications
will be administered.)
SERVICES PROVIDED
Each patient admitted to a facility for a 72-hour treatment
and evaluation period must receive an evaluation as soon
as possible after admission, and must receive the treatment
and care the condition requires for the full period that he or
she is held [Welfare and Institutions Code Section 5152].
PERIOD OF DETENTION
If a designated facility admits a patient, it may detain him or
her for evaluation and treatment for a period not to exceed
72 hours, including Saturdays, Sundays and holidays. If
evaluation and treatment services are not available on
Saturdays, Sundays and holidays, and if DHCS certifies
that evaluation and treatment services cannot reasonably
be made available on those days, they are not counted
in the 72 hours. The certification by DHCS is subject to
renewal every two years. [Welfare and Institutions Code
Section 5151]
The 72 hours is counted from the time the person is
admitted to the facility responsible for the evaluation and
treatment. The time of admission runs from the time the

CHA Mental Health Law Manual 2019
3.12
©CALIFORNIA HOSPITAL ASSOCIATION
person is first detained in the facility and is not dependent
upon completion of admissions procedures or paperwork.
The time is not extended by a preadmission evaluation
period at the facility.
The 72 hours does not include time spent transporting the
patient to the treatment and evaluation facility by peace
officers or other persons designated to take a person into
custody under Welfare and Institutions Code Section 5150.
TERMINATION OF DETENTION
If the professional person in charge of the designated
facility, member of the attending staff, or professional
person designated by the county, determines that
an individual may be properly served without being
involuntarily detained, then evaluation, crisis intervention,
or other inpatient or outpatient services must be provided
on a voluntary basis. This authority shall not be interpreted
to prevent a peace officer from delivering individuals to a
designated facility for assessment. [Welfare and Institutions
Code Section 5150(c)]
If detained, the patient may be released before 72 hours
have elapsed only if the psychiatrist directly responsible
for the person’s treatment believes, as a result of his or her
personal observations, that the person no longer requires
evaluation or treatment. However, in those situations in
which both a psychiatrist and psychologist have personally
evaluated or examined a person on a 72-hour hold and
there is a collaborative treatment relationship between
the psychiatrist and psychologist, either the psychiatrist
or psychologist may authorize the release of the person,
but only after they have consulted with one another. In the
event of a clinical or professional disagreement regarding
the early release, the hold must be maintained unless the
facility’s medical director overrules the decision of the
psychiatrist or psychologist opposing the release. Both
the psychiatrist and psychologist must enter their findings,
concerns, or objections in the patient’s medical record.
If any other professional who is authorized to release the
person believes the person should be released before
72 hours have elapsed, and the psychiatrist directly
responsible for the person’s treatment objects, the matter
must be referred to the medical director of the facility for
the final decision. However, if the medical director is not
a psychiatrist, he or she must appoint a designee who
is a psychiatrist to make these decisions. If the matter is
referred, the person must be released before 72 hours
have elapsed only if the psychiatrist who makes the
final decision believes, as a result of his or her personal
observations, that the person no longer requires evaluation
or treatment. [Welfare and Institutions Code Section 5152]
A psychologist may not order an early release without
potential liability [Ford v. Norton, 89 Cal. App. 4th 974
(2001)], except in the narrow instance outlined in the
previous paragraph.
A patient who has been detained for evaluation and
treatment must be released at the end of the 72-hour
period unless any of the following applies:
1. The patient is referred for further care and treatment on
a voluntary basis;
2. The patient has been certified for intensive treatment
(see A.“Detention for 14-Day Intensive Treatment,”
page3.17); or
3. A conservator or temporary conservator has been
appointed for the patient under Welfare and Institutions
Code Section 5350 et seq. (see F.“Additional
Treatment for Gravely Disabled Person (LPS
Conservatorship),” page3.31).
[Welfare and Institutions Code Section 5152(b)]
NOTIFICATION OF RELEASE TO COUNTY BEHAVIORAL
HEALTH DIRECTOR AND PEACE OFFICER
The professional person in charge of a designated facility
(or designee) must notify the county behavioral health
director (or designee) and the peace officer who placed the
5150 hold (or a person designated by the law enforcement
agency that employs the peace officer) of the patient’s
release if both of the following conditions apply:
1. The peace officer requested notification at the time of
application, and
2. The peace officer certified in writing that the person
was referred to the facility under circumstances that
support the filing of criminal charges.
The only information that may be released is the person’s
name, address, date of admission for the 72-hour
evaluation period, and the date of release [Welfare and
Institutions Code Section 5152.1; 45 C.F.R. Section
164.512(a) and (f)].
The hospital should examine the paperwork completed by
the law enforcement officer to determine if notification upon
release is required.

Chapter 3 — Voluntary Admission and Involuntary Detainment for Mental Health Treatment CHA
3.13
©CALIFORNIA HOSPITAL ASSOCIATION
IMMUNITY FROM LIABILITY
Provided they have complied with the provisions of
applicable law discussed above, the following persons
are not civilly or criminally liable for any action by a patient
released at or before the end of the 72 hours:
1. The professional in charge of the designated facility, or
a designee;
2. The medical director of the facility, or a designee,
described in Welfare and Institutions Code Section
5152;
3. The psychiatrist directly responsible for the person’s
treatment;
4. The psychologist; and
5. The peace officer responsible for the detention of the
person.
[Welfare and Institutions Code Section 5154]
RESPONSIBILITY FOR PROPERTY OF PERSON TAKEN
INTO CUSTODY
Responsibility Defined
When a patient is taken into custody for evaluation, or
within a reasonable time thereafter, the person who takes
the patient into custody must take reasonable precautions
to preserve and safeguard the personal property in the
possession of, or on the premises occupied by, the patient.
The person taking the patient into custody must give
the court a report that generally describes the patient’s
property and its disposition (unless a responsible relative,
guardian or conservator is in possession of the patient’s
personal property). The language outlined below may be
used for this report. If a responsible relative, guardian, or
conservator of the patient has possession of the property,
the report must include only the name of the relative,
guardian, or conservator and the location of the property. In
such a case, the person who took the patient into custody
is no longer responsible for the property once the report
is completed.
For these purposes, “responsible relative” includes the
spouse, parent, adult child, domestic partner, grandparent,
grandchild, or adult brother or sister of the person.
[Welfare and Institutions Code Section 5150(f)]
Reporting Requirement
The required report of a patient’s property made by
the person taking the patient into custody should be
substantially in the following form:
I hereby report to the Superior Court for the County
of
that the
personal property of the person apprehended,
described generally as
was preserved and safeguarded by
(insert name of person taking the patient into custody,
responsible relative, guardian or conservator)
. The property is
now located at
.
Date:
, 20
Signature:
Title:
[Welfare and Institutions Code Section 5211]
B. Patient Impaired by Inebriation
CONDITIONS FOR DETENTION
When a person is a danger to self or others or gravely
disabled as a result of inebriation, a peace officer, member
of the attending staff of a designated facility who is
authorized to place a hold, or a person designated by the
county may, upon reasonable cause, place the person in
a facility designated by the county and approved by the
California Department of Alcohol and Drug Programs as a
facility for 72-hour treatment and evaluation of inebriates
[Welfare and Institutions Code Section 5170]. A list of
these facilities may be found at https://data.chhs.ca.gov/
dataset/dhcs-licensed-residential-facilities-and-or-certifie
d-alcohol-and-drug-programs/resource/1cbf39c4-0674-
4dce-8f6f-4ff24eb8074e. (As of July 1, 2013, the California
Department of Alcohol and Drug Programs became part of
the California Department of Health Care Services.)
If, in the judgment of the admitting staff, the inebriate can
be properly served without being detained, he or she must
be treated on a voluntary basis [Title 9, California Code of
Regulations, Section 9448]. Welfare and Institutions Code
Section 5172.1 permits a person who is a danger to self
or others or gravely disabled as a result of inebriation, to
voluntarily apply for admission to a 72-hour evaluation and
detoxification treatment facility.
WRITTEN APPLICATION REQUIRED
The designated facility must obtain an application in writing
that states the circumstances under which the person’s
condition was called to the attention of the officer, member
of the attending staff, or a designee. It must state that

CHA Mental Health Law Manual 2019
3.14
©CALIFORNIA HOSPITAL ASSOCIATION
the officer, member of the attending staff, or designee
believes as a result of his or her personal observations
that the person is, as a result of inebriation, a danger to
self or others or gravely disabled, or has violated Penal
Code Section 647(f), which makes it a misdemeanor to be
in public under the influence of alcohol or other specified
substances and thus unable to exercise care for one’s
own safety or the safety of others. [Welfare and Institutions
Code Section 5170.3]
RECOMMENDED FORM FOR WRITTEN APPLICATION
It is recommended that in meeting the requirement for a
written application that the “Application for Involuntary
Admission — Inebriates” form (CHA Form 12-5) be used.
RIGHT TO MAKE TWO TELEPHONE CALLS
Immediately after being taken to a designated facility, a
person has the right to make, at his or her own expense,
at least two completed telephone calls (except where
physically impossible). The person must be allowed to
make these calls within three hours of detention. If the
person placed in the evaluation facility does not have
money to make these calls, he or she must be allowed
to make at least two completed local toll-free or collect
telephone calls at no charge. [Welfare and Institutions Code
Section 5170.5]
RELEASE UPON REQUEST
A person who requests to be released from the facility
before 72 hours have elapsed may be released only if the
psychiatrist directly responsible for the person’s treatment
believes, as a result of his or her personal observations,
that the person is not a danger to self or others. If any
other professional who is authorized to release the person
believes the person should be released before 72 hours
have elapsed, and the psychiatrist directly responsible
for the person’s treatment objects, the matter should
be referred to the medical director of the facility for the
final decision. However, if the medical director is not a
psychiatrist, he or she must appoint a designee who is
a psychiatrist to make these decisions. If the matter is
referred, the person may be released before 72 hours have
elapsed only if the psychiatrist who makes the final decision
believes, as a result of his or her personal observations,
that the person is not a danger to self or others. A
psychologist may not order an early release without
potential liability [Ford v. Norton, 89 Cal. App. 4th 974
(2001)]. (If the person is determined to be gravely disabled
as a result of a mental disorder, it may be appropriate to
detain him or her under the provisions for treatment of
mental health disorders.) [Welfare and Institutions Code
Section 5170.7]
NOTE: The law that permits a psychologist, under certain
circumstances, to release a patient before the end of his
or her hold does not apply to patients who are detained
because they are a danger to self or others or gravely
disabled as a result of inebriation.
SERVICES PROVIDED
Each person admitted to a facility for 72-hour treatment
and evaluation must receive an evaluation as soon after
admission as possible and must receive the treatment and
care his or her condition requires for the full period that he
or she is held [Welfare and Institutions Code Section 5172].
PERIOD OF DETENTION
If the facility for 72-hour treatment and evaluation of
inebriates admits the person, it may detain him or her
for evaluation and detoxification treatment, and such
other treatment as may be indicated, for a period not to
exceed 72 hours. Saturdays, Sundays, and holidays must
be included for the purpose of calculating the 72-hour
period. However, a person may voluntarily remain in the
facility for more than 72 hours if the professional in charge
of the facility determines that the person needs and may
benefit from further treatment. However, a person who is
involuntarily detained in the facility has priority for available
treatment and care over a person who has voluntarily
remained in a facility for more than 72 hours. [Welfare and
Institutions Code Section 5171]
TERMINATION OF DETENTION
If, in the judgment of the professional in charge of the
facility that provides the evaluation and treatment, the
person may be properly served without being detained,
then evaluation, detoxification or other treatment, crisis
intervention, or other inpatient or outpatient services must
be provided on a voluntary basis [Welfare and Institutions
Code Section 5171].
If detained, the person may be released before 72 hours
have elapsed only if the psychiatrist directly responsible
for the person’s treatment believes, as a result of his must
her personal observations, that the person no longer
requires evaluation or treatment. If any other professional
who is authorized to release the person believes the
person should be released before 72 hours have elapsed,
and the psychiatrist directly responsible for the person’s
treatment objects, the matter should be referred to
the medical director of the facility for the final decision.
However, if the medical director is not a psychiatrist, he
or she must appoint a designee who is a psychiatrist to
make these decisions. If the matter is referred, the person

Chapter 3 — Voluntary Admission and Involuntary Detainment for Mental Health Treatment CHA
3.15
©CALIFORNIA HOSPITAL ASSOCIATION
may be released before 72 hours have elapsed only if the
psychiatrist who makes the final decision believes, as a
result of his or her personal observations, that the person
no longer requires evaluation or treatment. A psychologist
may not order an early release without potential liability
[Ford v. Norton, 89 Cal. App. 4th 974 (2001)].
NOTE: The law that permits a psychologist, under certain
circumstances, to release a patient before the end of his
or her hold does not apply to patients who are detained
because they are a danger to self or others or gravely
disabled as a result of inebriation.
The patient who has been detained for evaluation and
treatment must be released at the end of the 72-hour
detention period unless any of the following applies:
1. The patient is referred for further treatment on a
voluntary basis.
2. The patient is certified for intensive treatment on
the basis that, as a result of impairment by chronic
alcoholism, he or she is a danger to self or others
or gravely disabled (see A.“Detention for 14-Day
Intensive Treatment,” page3.17).
3. A conservator or temporary conservator has been
appointed for the patient under Welfare and Institutions
Code Section 5350 et seq. (see F.“Additional
Treatment for Gravely Disabled Person (LPS
Conservatorship),” page3.31).
[Welfare and Institutions Code Section 5172]
IMMUNITY FROM LIABILITY
Provided they have complied with the provisions of Welfare
and Institutions Code Sections 5170-5176, which are
discussed above, the following persons are not civilly or
criminally liable for any action by a patient released at or
before the end of the 72 hours:
1. The professional in charge of the designated facility, or
a designee;
2. The medical director of the facility, or a designee,
described in Welfare and Institutions Code Sections
5170.7 and 5172;
3. The psychiatrist directly responsible for the person’s
treatment; and
4. The peace officer responsible for the detention of the
person.
[Welfare and Institutions Code Section 5173]
NOTE: The law that permits a psychologist, under certain
circumstances, to release a patient before the end of his
or her hold does not apply to patients who are detained
because they are a danger to self or others or gravely
disabled as a result of inebriation. Thus, there is no
immunity for a psychologist who releases such a patient.
C. Patient Impaired by Use of Controlled
Substances
If a person is a danger to self or others or gravely disabled
as a result of the use of controlled substances (the
narcotics or restricted dangerous drugs referred to in
Health and Safety Code Section 11000 et seq.), he or
she is subject to the following provisions that apply to the
involuntary detention of a person who is a danger to self or
others or gravely disabled as a result of other causes:
1. An initial 72-hour hold for evaluation and treatment
under Welfare and Institutions Code Section 5150 et
seq. (see A.“Patients With a Mental Health Disorder,”
page3.9).
2. An additional 14-day intensive treatment period under
Welfare and Institutions Code Section 5250 et seq.
(see A.“Detention for 14-Day Intensive Treatment,”
page3.17).
3. Procedures for review of continued confinement, as
provided in Welfare and Institutions Code Section
5275 et seq. (see B.“Review of Commitment for 14
Additional Days of Intensive Treatment,” page3.20).
4. Provisions for court-ordered evaluation of persons with
mental health disorders under Welfare and Institutions
Code Section 5200 et seq. (see VII.“Court-Ordered
Evaluation of Persons Who May Have a Mental Health
Disorder,” page3.33).
5. Protections of legal and civil rights of persons who
are involuntarily detained, as described in Welfare and
Institutions Code Section 5325 et seq. (see II.“Patient
Rights Under State Law,” page4.1).
Any custody, evaluation, treatment, or any other procedure
initiated under these provisions must be related to the
person’s use of controlled substances.
[Welfare and Institutions Code Section 5343]
D. Other Admission Forms
At the time of admission, the signature of the patient
or the patient’s legal representative on the “Conditions
of Admission” (CHA Form 8-1) and other admission
documents should also be obtained. If the patient lacks
capacity to agree or refuses to agree to admission

CHA Mental Health Law Manual 2019
3.16
©CALIFORNIA HOSPITAL ASSOCIATION
documents, the facility should attempt to obtain the
patient’s signature once he or she has regained capacity or
is willing to sign.
E. Special Requirements for a Minor
As with adults, the state has the power to detain a minor
involuntarily if it appears that the minor, as a result of a
mental health disorder, is a danger to self or others or
gravely disabled.
The Children’s Civil Commitment and Mental Health
Treatment Act of 1988 (CCCMHTA), Welfare and Institutions
Code Sections 5585-5585.9, applies to the initial 72 hours
of mental health treatment and evaluation provided to a
minor who, as a result of a mental disorder, is a danger to
self or others or gravely disabled. To the extent that the
CCCMHTA conflicts with any other provisions of law that
relate to 72-hour holds, the CCCMHTA prevails. Evaluation
and treatment of a minor beyond the initial 72-hour period
must comply with the provisions of LPS.
The CCCMHTA applies to minors under 18 years of
age [Family Code Section 6500]. It does not apply to
emancipated minors who are regarded as adults for the
purpose of consenting to medical, dental or psychiatric
care without parental consent, knowledge or liability [Family
Code Section 7050(c)(1); Welfare and Institutions Code
Section 5585.59].
While minors 12 years of age or older are authorized to
consent to outpatient mental health care under Family
Code Section 6924 and Health and Safety Code Section
124260, they are not authorized to consent to inpatient
mental health treatment. (See G.“Minors in Need of
Outpatient Mental Health Treatment or Residential Shelter
Services,” page2.39, for further information about minor
consent to outpatient mental health treatment.)
GRAVELY DISABLED MINOR
“Gravely disabled minor” means a minor who, as a result
of a mental disorder, is unable to use the elements of
life that are essential to health, safety, and development,
including food, clothing, or shelter, even though provided
to the minor by others. Intellectual disability or other
developmental disabilities, epilepsy, alcoholism, other
drug abuse, or repeated antisocial behavior do not, by
themselves, constitute a mental disorder. [Welfare and
Institutions Code Section 5585.25]
REQUIREMENTS FOR COMMITMENT
A minor may be committed involuntarily for 72 hours where:
1. There is probable cause to believe that the minor, as a
result of a mental health disorder, is a danger to self or
others or gravely disabled.
2. Authorization for voluntary treatment by a parent,
guardian or other legal representative is not available.
3. The minor is taken into custody, upon probable cause,
by a peace officer, member of the attending staff
of a designated facility or other professional person
designated by the county. This person must make a
written application to the facility for detention of the
minor stating the circumstances under which the
minor’s condition was called to the attention of the
peace officer or other person, and stating that the
requirements in paragraphs 1 and 2, above, are met.
[Welfare and Institutions Code Section 5585.50]
4. The facility must make every effort to notify the minor’s
parent or legal guardian as soon as possible.
5. Placement is at a facility designated by the county and
approved by DHCS as a facility for 72-hour evaluation
and treatment.
Each county is required to assure that minors under
the age of 16 years are not held with adults receiving
psychiatric treatment under the provisions of LPS,
unless the health facility has specific separate housing
arrangements, treatment staff, and treatment programs
designed to serve children or adolescents. The
director of DSS may provide waivers to counties if this
policy creates undue hardship due to inadequate or
unavailable alternative resources.
However, no minor may be admitted for psychiatric
treatment into the same treatment ward as an adult
who is in the custody of a jailor for a violent crime, is a
known registered sex offender, or has a known history
of, or exhibits inappropriate, sexual, or other violent
behavior which would present a threat to the physical
safety of minors.
6. A detained minor must receive a clinical evaluation
conducted by professionals qualified in the diagnosis
and treatment of minors. The evaluation must consist
of multidisciplinary professional analyses of the minor’s
medical, psychological, developmental, educational,
social, financial, and legal conditions as may appear
to constitute a problem. This evaluation must include
a psychosocial evaluation of the family or living
environment, or both. Every effort must be made to
involve the minor’s parent or legal guardian in the
clinical evaluation.

Chapter 3 — Voluntary Admission and Involuntary Detainment for Mental Health Treatment CHA
3.17
©CALIFORNIA HOSPITAL ASSOCIATION
7. If, in the opinion of the professional who conducts the
evaluation, the minor will require additional treatment,
a treatment plan must be prepared that identifies the
least restrictive placement alternative in which the
minor can receive the necessary treatment. The family,
guardian or caretaker and the minor must be consulted
and informed of the basic recommendation for further
treatment and placement. Every effort must be made
to obtain the consent of the minor’s parent or guardian
prior to treatment and placement, but inability to obtain
this consent does not preclude involuntary treatment,
provided this treatment complies with the provisions
of LPS.
8. The minor must be given an aftercare plan upon
discharge. (See IV.“Aftercare Plan,” page4.6.)
V. CONTINUED TREATMENT OF AN
INVOLUNTARY PATIENT
A. Detention for 14-Day Intensive Treatment
CONDITIONS FOR CERTIFICATION
If a person is detained as mentally disordered or as
impaired by inebriation or use of narcotics or restricted
dangerous drugs for 72 hours under the conditions
discussed under IV.“Involuntary Detention of the Patient
on a 72-Hour Hold,” page3.9, or by reason of a
court-ordered evaluation [Welfare and Institutions Code
Section 5200 et seq. and Section 5225 et seq.], the person
may be certified for not more than 14 days of involuntary
intensive treatment under the following conditions:
1. The professional staff of the agency or facility that
provides evaluation services has analyzed the
person’s condition and found the person is, as a
result of a mental health disorder or impairment by
chronic alcoholism, a danger to self or others or
gravely disabled.
2. The person has been advised of, but has not accepted,
voluntary treatment.
3. The facility is equipped and staffed to provide intensive
treatment, is designated by the county to provide
intensive treatment, and agrees to admit the person.
[Welfare and Institutions Code Section 5250]
The facility must obtain the patient’s medication history, if
possible [Welfare and Institutions Code Section 5332].
SIGNATURES ON CERTIFICATION NOTICE
For a person to be certified as described above, the
certification notice must be signed by two people.
The first person must be the professional, or a designee,
in charge of the agency or facility that provides
evaluation services. A designee of the professional must
be a physician or a licensed psychologist who has a
doctoral degree in psychology and at least five years of
postgraduate experience in the diagnosis and treatment of
emotional and mental disorders.
The second person must be a physician or psychologist
who participated in the evaluation. If possible, the
physician should be a board-certified psychiatrist. The
psychologist must be licensed and have at least five years
of postgraduate experience in the diagnosis and treatment
of emotional and mental disorders.
If the professional in charge, or the designee, is the
physician who performed the medical evaluation or a
psychologist, the second person to sign may be another
physician or psychologist unless one is not available, in
which case a social worker, marriage and family therapist,
professional clinical counselor, or registered nurse who
participated in the evaluation must sign the notice. [Welfare
and Institutions Code Section 5251]
REQUIRED FORM OF CERTIFICATION NOTICE
The “Notice of Certification for Intensive Treatment”
(CHA Form 12-6) complies with the requirements of Welfare
and Institutions Code Section 5252. It is recommended
that this form be used for these notification purposes.
DELIVERY OF COPIES OF THE CERTIFICATION NOTICE
A copy of the certification notice must be personally
delivered to the patient. A copy must also be sent to the
patient’s attorney or the attorney or advocate designated to
represent the patient in the certification review hearing.
The patient must be asked to designate another person
to receive a copy of the certification notice. If the patient
is incapable of making such a designation at the time
of certification, he or she must be asked to designate a
person as soon as he or she is capable.
A copy of the certification notice must be submitted to the
superior court with a copy of the decision that results from
the certification review hearing. [Welfare and Institutions
Code Section 5253]
A hospital that certifies patients should consult legal
counsel regarding the advisability of filing documents with
the court under seal and/or obtaining a protective order
(see HIPAA provision at 45 C.F.R. Section 164.512(e)).

CHA Mental Health Law Manual 2019
3.18
©CALIFORNIA HOSPITAL ASSOCIATION
ADVISEMENT OF RIGHTS TO PATIENT
The person who delivers the copy of the certification notice
to the patient must, at the time of delivery, inform him or
her of the right to have either a certification review hearing
within four days or review by a court pursuant to a writ
of habeas corpus to determine whether probable cause
exists to detain him or her for intensive treatment related to
the mental disorder or impairment by chronic alcoholism.
The patient must be informed of his or her rights with
respect to the certification review hearing, including the
right to the assistance of another person to prepare for the
hearing and/or to answer other questions and concerns
about the involuntary commitment. Also, the patient must
receive an explanation about what judicial review by
habeas corpus entails and be informed of his or her right
to counsel at these hearings, including counsel appointed
by the court under Welfare and Institutions Code Section
5276. [Welfare and Institutions Code Sections 5254 and
5254.1] The processes for certification review hearings and
judicial review by writ of habeas corpus are described in
“Certification Review Hearings,” page3.20, and “Judicial
Review Pursuant to a Writ of Habeas Corpus,” page3.22.
Documentation of Notice to Patient
It is recommended that the person who delivers a copy of
the certification notice and advises the patient of his or her
rights complete the “Advisement of Rights — Involuntary
Patient” form (CHA Form 12-7). This form provides
documentation that the requirements of delivery of copies
of the certification notice as specified in Welfare and
Institutions Code Section 5253 (see “Delivery of Copies of
the Certification Notice,” page3.17), and advisement of
the right to review as specified in Welfare and Institutions
Code Sections 5254 and 5254.1 (see “Advisement of
Rights to Patient,” page3.18) have been met. The form
should be placed in the patient’s medical record.
MAXIMUM PERIOD OF DETENTION
After an involuntary commitment is initiated, the total period
of detention, including intervening periods of voluntary
treatment, must not exceed the total maximum period
during which the person could have been detained if the
person had been detained continuously on an involuntary
basis from the time of the initial involuntary commitment.
Thus, if a patient is admitted as a voluntary patient and
subsequently detained on an involuntary basis, the
maximum period of time is counted from the first date
of involuntary commitment rather than from the date
the patient was admitted to the hospital. [Welfare and
Institutions Code Section 5258]
After the maximum period of involuntary treatment has
passed, the patient may receive further treatment if he
or she:
1. Agrees to remain voluntarily after the time limit has
passed;
2. Is suicidal or is certified for additional intensive
treatment (see “Conditions for Confinement,”
page3.23);
3. Is a danger to others or is certified for 180 days
post-certification treatment (see E.“Additional
Confinement for a Person Dangerous to Others
(Post-Certification Procedures),” page3.28); or
4. Is gravely disabled and a conservatorship is initiated
(see F.“Additional Treatment for Gravely Disabled
Person (LPS Conservatorship),” page3.31).
After consulting with legal counsel, the facility should adopt
a policy regarding procedures to be followed when the total
period of detention exceeds the maximum time periods
allowed for treatment of a patient who is a danger to self or
others or is gravely disabled.
TERMINATION OF CERTIFICATION
Certification may last for no more than 14 days, and may
terminate earlier only if the psychiatrist directly responsible
for the patient’s treatment believes, as a result of his or
her personal observations, that the patient no longer is,
as a result of a mental disorder or impairment by chronic
alcoholism, a danger to self or others or gravely disabled
[Welfare and Institutions Code Section 5257].
However, in those situations in which both a psychiatrist
and psychologist have personally evaluated or examined
a person who is undergoing intensive treatment and there
is a collaborative treatment relationship between the
psychiatrist and psychologist, either the psychiatrist or
psychologist may authorize the release of the person, but
only after they have consulted with one another. In the
event of a clinical or professional disagreement regarding
the early release, the person may not be released unless
the facility’s medical director overrules the decision of the
psychiatrist or psychologist opposing the release. Both
the psychiatrist and psychologist must enter their findings,
concerns or objections into the patient’s medical record.
If any other professional who is authorized to release the
person believes the person should be released during the
14-day additional treatment period, and the psychiatrist
directly responsible for the person’s treatment objects,
the matter is to be referred to the medical director of the
facility for the final decision. If the medical director is not

Chapter 3 — Voluntary Admission and Involuntary Detainment for Mental Health Treatment CHA
3.19
©CALIFORNIA HOSPITAL ASSOCIATION
a psychiatrist, he or she must appoint a designee who
is a psychiatrist to make these decisions. If the matter is
referred, the person must be released during the 14-day
additional treatment period only if the psychiatrist who
makes the final decision believes, as a result of his or
her personal observations, that the person certified no
longer is, as a result of mental disorder or impairment by
chronic alcoholism, a danger to self or others or gravely
disabled. A psychologist may not order an early release
without potential liability [Ford v. Norton, 89 Cal. App. 4th
974 (2001)] except in the narrow instance outlined in the
previous paragraph. The person may remain at the facility
on a voluntary basis, and the facility may provide the
person with appropriate referral information concerning
mental health services.
A person who has been certified for 14 days of intensive
treatment and to whom Welfare and Institutions Code
Section 5226.1 (which involves court-ordered evaluation
for persons impaired by chronic alcoholism or drug abuse)
does not apply, or with respect to whom the criminal
charge has been dismissed under Welfare and Institutions
Code Section 5226.1, must be released at the end of the
14 days unless any of the following applies:
1. The patient agrees to receive further treatment on a
voluntary basis.
2. A temporary conservator has been appointed for the
patient [Welfare and Institutions Code Section 5350 et
seq.].
3. The patient is suicidal and is certified for additional
intensive treatment [Welfare and Institutions Code
Section 5260 et seq.]. (See C.“Additional Intensive
Treatment for Suicidal Patient,” page3.23.)
4. The patient is dangerous to others and
post-certification procedures are initiated [Welfare and
Institutions Code Section 5300 et seq.].
5. The patient is certified for an additional 30 days of
intensive treatment for grave disability [Welfare and
Institutions Code Section 5270.10 et seq.].
DAMAGES FOR EXCESSIVE DETENTION
An individual who is knowingly and willfully responsible for
detaining a person for more than 14 days in violation of the
law is liable to that person in civil damages. [Welfare and
Institutions Code Section 5259.1]
FACILITY PREFERENCE
Whenever a county designates two or more facilities to
provide intensive treatment and the patient or patient’s
family, conservator, or guardian expresses a preference for
one of the facilities, the professional person who certifies
the patient must attempt, if administratively possible, to
comply with the preference [Welfare and Institutions Code
Section 5259.2].
TEMPORARY RELEASE
The professional in charge of an intensive treatment facility,
or a designee, may permit a person certified for intensive
treatment to leave the facility for short periods during the
person’s involuntary intensive treatment. The permission
should be in writing and documented in the patient’s record
[Welfare and Institutions Code Section 5259]. The “Leave of
Absence from Psychiatric Service” form (CHA Form 12-8) is
suggested for use by the hospital.
IMMUNITY FROM LIABILITY
Provided they have complied with the provisions of Welfare
and Institutions Code Sections 5250-5259.3, which are
discussed above, the following persons are not civilly or
criminally liable for any action by a person released at or
before the end of the 14 days:
1. The professional in charge of the facility that provides
intensive treatment, or a designee;
2. The professional person designated by the county;
3. The medical director of the facility, or a designee
described in Welfare and Institutions Code
Section 5257;
4. The psychiatrist directly responsible for the person’s
treatment; and
5. The psychologist.
[Welfare and Institutions Code Section 5259.3]
NOTIFICATION OF RELEASE TO COUNTY BEHAVIORAL
HEALTH DIRECTOR AND PEACE OFFICER
The professional person in charge of a facility that provides
14-day intensive treatment pursuant to Welfare and
Institutions Code Section 5250 or 5270.15, or a designee,
must notify the county behavioral health director, or a
designee, and the peace officer who made the original
application for a 72-hour hold, or a person designated by
the law enforcement agency that employs the peace officer,
when a patient admitted for involuntary treatment has been
released unconditionally if:
1. The peace officer requested notification at the time the
application for the 72-hour evaluation was made; and

CHA Mental Health Law Manual 2019
3.20
©CALIFORNIA HOSPITAL ASSOCIATION
2. The peace officer certified in writing that the person
was referred to the facility under circumstances that
would support the filing of criminal charges.
The only information that may be released is the person’s
name, address, date of admission for the 72-hour
evaluation period, date of certification for intensive
treatment, and the date of release. [Welfare and Institutions
Code Section 5250.1; 45 C.F.R. Section 164.512(a) and (f)].
The hospital should examine the paperwork completed by
the law enforcement officer to determine if notification upon
release is required.
B. Review of Commitment for 14 Additional Days
of Intensive Treatment
Each patient who is certified for 14 days of involuntary
treatment because he or she is a danger to self or others
or gravely disabled has the right to a “certification review
hearing,” unless he or she has requested judicial review
by a writ of habeas corpus. A patient who requests a
writ of habeas corpus review does not have the right to a
certification review hearing unless he or she withdraws the
request for judicial review before it occurs. In such cases,
the patient is entitled to a certification review hearing within
four days of the withdrawal of the request for writ of habeas
corpus review.
The certification review hearing and writ of habeas corpus
review procedures are designed to assure that the
commitment of all patients beyond 72 hours is reviewed
to determine whether probable cause exists to continue
the involuntary confinement. These procedures provide the
mandatory hearings which the federal Ninth Circuit Court of
Appeals, in Doe v. Gallinot, 657 F.2d 1017 (9th Cir. 1981),
held were necessary to meet constitutional requirements.
A patient should not be certified for involuntary treatment
and subsequently released before a writ of habeas corpus
hearing or certification review hearing has been held
except in those rare situations when the patient’s condition
changes before the hearing is held.
As described in “Advisement of Rights to Patient,”
page3.18, at the time a patient is certified for 14 days of
intensive treatment, the patient must be informed that he or
she is entitled to:
1. A certification review hearing to determine whether
or not probable cause exists to detain him or her for
intensive treatment related to a mental disorder or
chronic alcoholism; or
2. Judicial review of the involuntary commitment pursuant
to a writ of habeas corpus.
The procedures for these reviews are discussed below.
CERTIFICATION REVIEW HEARINGS
County Plans
Although the law outlines the general procedures that must
be used for certification review hearings, each county
is required to describe, in its Short-Doyle county plan,
the specific procedures it will use for certification review
hearings. Each county’s plan must address the issues of
how the patient’s representatives and hearing officers will
be selected and trained, how these persons will be notified,
and who will be responsible for the costs associated with
the hearings. The plan also must identify the individuals
who will represent treatment facilities at certification
review hearings, and the schedule for these hearings at
each facility (see Welfare and Institutions Code Sections
5255-5256.8).
If the county has not adopted procedures for certification
review hearings, treatment facilities will not be able to fully
comply with the law. However, interim procedures should
be instituted to assure that patients who are involuntarily
detained for 14 days of intensive treatment are given their
right of review. In this regard, the best interim procedure
is to request judicial review by a writ of habeas corpus.
However, if the patient refuses to request this review and
the courts in the county in which the facility is located
will not conduct such review in the absence of a patient
request, the facility may be required either to release
the patient after the 72-hour intensive evaluation and
treatment period or to continue the involuntary detention
without complying with the review procedures. In such
cases, the facility should consult its legal counsel regarding
appropriate procedures.
Certification Review Hearing Procedures
The procedure for the certification review hearings is
as follows.
Meeting Between the Patient and His or Her
Representative. As soon after the certification as
practicable, an attorney or patient advocate who will
advise and represent the patient is required to meet with
the certified patient and discuss the commitment process,
assist the patient in preparing for the certification review
hearing, answer the patient’s questions, and otherwise
assist the patient as appropriate. Each county must
designate persons who will act as patient representatives
and adopt procedures for informing these persons when

Chapter 3 — Voluntary Admission and Involuntary Detainment for Mental Health Treatment CHA
3.21
©CALIFORNIA HOSPITAL ASSOCIATION
a certification is initiated. In this regard, although the law
does not explicitly designate responsibility for paying for the
services of such a representative, it is the opinion of CHA’s
legal counsel (pending judicial or other clarification of this
ambiguity) that the county, rather than the patient or the
facility, is responsible for these costs.
Timing. The certification review hearing must be held within
four days of the date on which the person is certified for
a period of intensive treatment unless the patient, or his
or her attorney or advocate, requests postponement of
the hearing. Hearings may be postponed for 48 hours. A
hearing in a county with a population of 100,000 or less
may be postponed by the facility or the patient until the
next regularly scheduled hearing date.
If a patient is involuntarily detained for 72 hours but not
placed on a 14-day hold until some later date, the facility
may not be able to comply with the time limit. In these
cases the hearing should be held as soon as possible
and, to the extent feasible, on or before the eighth day of
involuntary treatment.
Location. The certification review hearing must be held in
a location that is compatible with and the least disruptive
of the treatment program. If the hearing is conducted
by a “certification review hearing officer” rather than a
court-appointed commissioner or referee (see below), the
hearing should be held at an appropriate place at the
facility where the certified patient is receiving treatment.
Certification Review Hearing Officer. The certification
review hearing must be conducted by a court-appointed
commissioner or referee or a “certification review hearing
officer.” Each county is responsible for determining who
will conduct the hearings and, if certification review
hearing officers will be used, the county’s board of
supervisors must appoint a panel (composed of the local
behavioral health director, the county public defender,
and the county counsel or district attorney) which will
approve (by unanimous vote) a list of persons who may
act as certification review hearing officers. Persons
eligible to serve as certification review hearing officers
include state-qualified administrative law hearing officers,
physicians, lawyers, and certified law students. In addition,
licensed psychologists, registered nurses, licensed
marriage and family therapists or licensed clinical social
workers who have had a minimum of five years’ experience
in mental health may act as certification review hearing
officers. However, no employee of the county mental health
program or of a facility designated to provide involuntary
treatment may serve as a certification review hearing officer.
Although the law does not specify the party responsible for
paying for the services of the certification review hearing
officer, it is the opinion of CHA’s legal counsel (pending
judicial or other clarification of this ambiguity) that the
county, rather than the patient or the facility, is responsible
for these costs.
Presentation of Evidence. At the hearing, a person who is
designated by the director of the facility in which the patient
is being treated must present evidence in support of the
certification decision. The hearing is informal in nature and
the judicial rules of procedure and evidence do not apply. It
is, however, important for the person presenting evidence
in support of the certification (who should be the patient’s
physician or a mental health professional who is familiar
with the patient’s condition) to be prepared to present facts
and information in support of the determination that the
patient is a danger to self or others or gravely disabled.
The district attorney or county counsel also may present
evidence at the certification review hearing.
Patient’s Rights at the Certification Review Hearing.
The certified patient has the following rights at the
certification review hearing:
1. To be present unless the patient, with his or her
representative’s assistance, has specifically waived
this right;
2. To be assisted by an attorney or advocate;
3. To present evidence on his or her behalf;
4. To question persons presenting evidence in support of
the certification decision;
5. To make reasonable requests for the attendance
of facility employees who have knowledge of, or
participated in, the certification decision; and
6. To have the persons conducting the hearing informed
whether the patient received medication within the
past 24 hours (or a longer period as the hearing officer
may determine), and, if so, the probable effects of
the medication.
Decision. The hearing officer is required to decide whether
a patient should be involuntarily detained. At the conclusion
of the hearing, the patient must be orally notified of the
decision. In addition, the hearing officer must provide a
written decision that identifies the evidence relied upon
and the reasons for the decision, to the patient’s attorney
or advocate and to the facility director. The patient’s
representative is responsible for notifying the patient of the
decision and of his or her right to a judicial review of the
commitment by a writ of habeas corpus proceeding.
A copy of the decision and of the 14-day certification form
must also be submitted to the superior court for the county

CHA Mental Health Law Manual 2019
3.22
©CALIFORNIA HOSPITAL ASSOCIATION
in which the facility is located. The hospital should assure
that the hearing officer does so.
Post-Decision Options. If the hearing officer decides that
there is not probable cause to believe that the patient is
a danger to self or others or gravely disabled, the patient
may not be detained for involuntary treatment and the
facility must release him or her. However, in such cases,
the patient may choose to remain for treatment on a
voluntary basis. Also, the facility is allowed to give the
patient appropriate referral information concerning mental
health services.
If the hearing officer concludes that as a result of a mental
disorder or impairment by chronic alcoholism the patient is
a danger to self or others or gravely disabled, the patient
may be held for the 14-day certification period subject
to his or her right to judicial review by writ of habeas
corpus. If, however, during the 14-day period, the person
who certified the patient determines that the patient is no
longer a danger to self or others or gravely disabled, the
involuntary commitment must end and the person must be
released (unless the patient accepts continuing treatment
on a voluntary basis).
At the end of the 14-day involuntary treatment period,
a patient who remains dangerous to self or others or
gravely disabled may be detained for additional involuntary
treatment in accordance with the procedures applicable to
the certification for:
1. 14 additional days of involuntary treatment for suicidal
patients (see C.“Additional Intensive Treatment for
Suicidal Patient,” page3.23);
2. 30 days for gravely disabled patients (see
D.“Additional Intensive Treatment for Gravely Disabled
Person,” page3.25);
3. 180 days for patients who are dangerous to others (see
E.“Additional Confinement for a Person Dangerous to
Others (Post-Certification Procedures),” page3.28); or
4. A temporary or permanent conservatorship for gravely
disabled patients (see F.“Additional Treatment for
Gravely Disabled Person (LPS Conservatorship),”
page3.31).
JUDICIAL REVIEW PURSUANT TO A WRIT OF HABEAS
CORPUS
Patient Request for Court Hearing or Release Triggers
Judicial Review Process
Every person detained by certification for intensive
treatment has the right to a hearing pursuant to a writ of
habeas corpus for his or her release after he or she, or any
person acting on his or her behalf, has made a request for
release to:
1. The person who delivers the copy of the certification
notice at the time of delivery;
2. A member of the treatment staff of the facility that
provides intensive treatment, at any time during the
14 days of intensive treatment; or
3. The attorney or advocate who represented him or
her at a certification review hearing at which it was
concluded that probable cause existed to detain the
patient for 14 days of involuntary treatment.
A person who delivers a copy of the certification notice
or a member of the treatment staff to whom a request for
release is made must promptly provide the patient or other
person making the request with a copy of a form described
in Welfare and Institutions Code Section 5275 for his or
her signature or mark. The “Request for Release from
Involuntary Treatment” form (CHA Form 12-9) has been
developed to comply with this requirement.
The person who delivers the copy of the certification notice
or the member of the treatment staff, as the case may be,
must:
1. Fill in his or her own name and the date,
2. If the patient signs by mark, fill in the patient’s
name and
3. Deliver the completed copy to the professional in
charge of the intensive treatment facility, or a designee.
As soon as possible, the professional in charge of the
facility or designee must inform the superior court for
the county in which the facility is located of the request
for release.
A person who intentionally violates this requirement is guilty
of a misdemeanor.
Effect of Judicial Review
Judicial review is provided by the superior court for the
county in which the facility that provides the intensive
treatment is located or in the county in which the 72-hour
evaluation was conducted if the patient, or a person acting
on the patient’s behalf, informs the professional staff of
the evaluation facility in writing that judicial review will
be sought.
No patient may be transferred from the county that
provides evaluation services to a different county for
intensive treatment if the staff of the evaluation facility has
been informed in writing that a judicial review will be sought,
until the completion of the judicial review.

Chapter 3 — Voluntary Admission and Involuntary Detainment for Mental Health Treatment CHA
3.23
©CALIFORNIA HOSPITAL ASSOCIATION
The patient must be informed of the right to counsel by
the member of the treatment staff and by the court. If the
patient so elects, the court must immediately appoint the
public defender or another attorney to assist the patient to
prepare a petition for a writ of habeas corpus and, if he or
she so elects, to represent the patient in the proceedings.
The patient is required to pay the costs of legal advice
if able.
The court must either release the patient or order an
evidentiary hearing to be held within two judicial days
after the petition is filed. The patient must be released
immediately if the court finds that:
1. The patient is not, as a result of a mental disorder or
impairment by chronic alcoholism, a danger to self or
others or gravely disabled;
2. The patient had not been advised of, or had accepted,
voluntary treatment; or
3. The facility that provides intensive treatment is
not designated by the county to provide intensive
treatment.
[Welfare and Institutions Code Section 5276]
PATIENT’S RIGHT TO DENY RELEASE OF
INFORMATION
The patient must be advised by the treating facility that
he or she has the right to request that no person be told
the time and place of the certification hearing or of the
subsequent judicial review. [Welfare and Institutions Code
Sections 5256.4(c) and 5276]
C. Additional Intensive Treatment for Suicidal
Patient
CONDITIONS FOR CONFINEMENT
At the expiration of the initial 14-day period of intensive
treatment a person who, as a result of a mental disorder or
impairment by chronic alcoholism, threatened or attempted
to take his or her life during the 14-day period or the
72-hour evaluation period, or was detained for evaluation
and treatment because he or she threatened or attempted
to take his or her life and who continues to present an
imminent threat of taking his or her life, may be confined
for further intensive treatment for an additional period
not to exceed 14 days. [Welfare and Institutions Code
Section 5260]
The additional period of intensive treatment may occur only
if the following conditions have been met:
1. The professional staff of the agency or the facility that
provides intensive treatment services has analyzed the
person’s condition and found that the person presents
an imminent threat of taking his or her life.
2. The person has been advised of, but has not accepted,
voluntary treatment.
3. The facility is equipped and staffed to provide intensive
treatment, is designated by the county to provide
intensive treatment, and agrees to admit the person.
4. The person has, as a result of a mental disorder or
impairment by chronic alcoholism, threatened or
attempted to take his or her life during the 14-day
period of intensive treatment or the 72-hour evaluation
period, or was detained for evaluation and treatment
because of threats or attempts to take his or her life.
The facility must obtain the patient’s medication history, if
possible [Welfare and Institutions Code Section 5332].
COMPLETION OF A SECOND NOTICE OF
CERTIFICATION
For a person to be certified for an additional period of
intensive treatment, a second notice of certification must
be completed and signed by:
1. The professional in charge of the facility providing the
first 14 days of intensive treatment to the person; and
2. By a physician who is, whenever possible, a
board-qualified psychiatrist, or a licensed psychologist
who has a doctoral degree in psychology and at least
five years of postgraduate experience in the diagnosis
and treatment of emotional and mental disorders.
The physician or psychologist who signs must have
participated in the analysis of the patient’s condition
and determined that the conditions referred above
were met. [Welfare and Institutions Code Section 5261]
If the professional in charge is the physician who performed
the medical evaluation, or a psychologist, the second
person to sign may be another physician or psychologist
unless one is not available, in which case a social worker,
marriage and family therapist, professional clinical
counselor, or registered nurse who participated in the
evaluation may sign the notice of certification.
REQUIRED FORM OF SECOND NOTICE OF
CERTIFICATION
The “Notice of Certification to Second Involuntary
14-Day Period for Intensive Treatment — Suicidal
Patient” form (CHA Form 12-10) complies with the

CHA Mental Health Law Manual 2019
3.24
©CALIFORNIA HOSPITAL ASSOCIATION
requirements of Welfare and Institutions Code Section
5262. It is recommended that this form be used for these
notification purposes.
DELIVERY OF COPIES OF SECOND NOTICE OF
CERTIFICATION
Copies of the second notice of certification of imminently
suicidal patients must be filed with the court, and must
be given to the patient, the patient’s attorney, the district
attorney, the public defender, if any, and the facility that
provides intensive treatment. Also, the patient must be
asked to designate a person to receive a copy of the
certification notice. If the patient is unable to make such
a designation at the time he or she is certified, the patient
must be asked to do so as soon as he or she becomes
capable. [Welfare and Institutions Code Section 5263]
A hospital that certifies patients should consult legal
counsel regarding the advisability of filing documents with
the court under seal and/or obtaining a protective order
(see HIPAA provision at 45 C.F.R. Section 164.512(e)).
ADVISEMENT OF RIGHTS TO PATIENT
Upon delivery of the second notice of certification to the
patient, the patient should be informed of his or her right
to a certification review or to judicial review pursuant to a
writ of habeas corpus and be given other information as
discussed under “Advisement of Rights to Patient,” page.
[Welfare and Institutions Code Sections 5254 and 5254.1]
REVIEW OF INTENSIVE TREATMENT
The procedures for review pursuant to a request for
release made by a patient detained by certification for a
second 14-day intensive treatment period are the same
as the review procedures of an initial 14-day commitment,
discussed under B.“Review of Commitment for 14
Additional Days of Intensive Treatment,” page3.20.
TERMINATION OF CERTIFICATION FOR ADDITIONAL
INTENSIVE TREATMENT FOR SUICIDAL PATIENT
A certification for additional treatment for an imminently
suicidal person must be for no more than 14 days of
intensive treatment, and must terminate only when the
psychiatrist directly responsible for the person’s treatment
believes, as a result of his or her personal observations,
that the individual has improved sufficiently to leave, or is
prepared to accept voluntary treatment in the facility that
provides intensive treatment or in another facility.
However, in those situations in which both a psychiatrist
and psychologist have personally evaluated or examined
a person who is undergoing intensive treatment and there
is a collaborative treatment relationship between the
psychiatrist and psychologist, either the psychiatrist or
psychologist may authorize the release of the person, but
only after they have consulted with one another. In the
event of a clinical or professional disagreement regarding
the early release, the person may not be released unless
the facility’s medical director overrules the decision of the
psychiatrist or psychologist opposing the release. Both
the psychiatrist and psychologist must enter their findings,
concerns or objections in to the patient’s medical record.
If any other professional who is authorized to release the
person believes the person should be released before
14 days have elapsed, and the psychiatrist directly
responsible for the person’s treatment objects, the matter
must be referred to the medical director of the facility for
the final decision. However, if the medical director is not
a psychiatrist, he or she must appoint a designee who
is a psychiatrist to make these decisions. If the matter is
referred, the person may be released before 14 days have
elapsed only if the psychiatrist believes, as a result of his or
her personal observations, that the individual has improved
sufficiently to leave, or is prepared to accept voluntary
treatment in the facility that provides intensive treatment or
in another facility. [Welfare and Institutions Code Section
5264] A psychologist may not order an early release
without potential liability [Ford v. Norton, 89 Cal. App. 4th
974 (2001)] except in the narrow instance outlined in the
previous paragraph.
A person who has been certified for 14 days of intensive
treatment and to whom Welfare and Institutions Code
Section 5226.1 (which involves court-ordered evaluation
for persons impaired by chronic alcoholism or drug abuse)
does not apply, or with respect to whom the criminal
charge has been dismissed under Welfare and Institutions
Code Section 5226.1, must be released at the end of the
14 days unless any of the following applies:
1. The patient agrees to receive further treatment on a
voluntary basis.
2. The patient is recommended for conservatorship under
Welfare and Institutions Code Section 5350 et seq.
3. The patient is dangerous to others [Welfare and
Institutions Code Section 5300 et seq.].
DAMAGES FOR EXCESSIVE DETENTION
An individual who is knowingly and willfully responsible for
detaining a person for more than 14 days in violation of the
law is liable to that person in civil damages [Welfare and
Institutions Code Section 5265].

Chapter 3 — Voluntary Admission and Involuntary Detainment for Mental Health Treatment CHA
3.25
©CALIFORNIA HOSPITAL ASSOCIATION
FACILITY PREFERENCE
Whenever a county designates two or more facilities to
provide intensive treatment and the patient or patient’s
family, conservator, or guardian expresses a preference for
one of the facilities, the professional person who certifies
the patient must attempt, if administratively possible, to
comply with the preference [Welfare and Institutions Code
Section 5266].
TEMPORARY RELEASE
The professional in charge of an intensive treatment facility,
or a designee, may permit a person certified for intensive
treatment to leave the facility for short periods during the
person’s involuntary intensive treatment. The permission
should be in writing and documented in the patient’s record.
The “Leave of Absence from Psychiatric Service” form (CHA
Form 12-8) is suggested for use by the hospital [Welfare
and Institutions Code Section 5268].
IMMUNITY FROM LIABILITY
Provided they have complied with Welfare and Institutions
Code Sections 5260-5268, which are discussed above,
the following persons are not civilly or criminally liable for
any action by a person released at or before the end of the
14 days:
1. The professional person in charge of the facility that
provides intensive treatment, or a designee;
2. The medical director of the facility, or a designee
described in Welfare and Institutions Code Section
5264;
3. The psychiatrist directly responsible for the person’s
treatment; and
4. The psychologist.
[Welfare and Institutions Code Section 5267]
D. Additional Intensive Treatment for Gravely
Disabled Person
OPTIONAL ADDITIONAL 30-DAY PERIOD OF INTENSIVE
TREATMENT
Counties have the option to adopt procedures that allow
an additional 30 days of intensive treatment upon the
completion of the 14-day period of intensive treatment
under Welfare and Institutions Code Section 5250. These
provisions [Welfare and Institutions Code Section 5270.10
et seq.] are effective only in the counties in which the
county board of supervisors, by resolution, authorizes the
procedures after assuring that implementation of these
procedures will not result in reduction of current mental
health services. At least 17 counties have adopted 30-day
extensions, including Los Angeles, Orange, Sacramento,
and San Diego. DHCS is charged with ensuring the
maintenance of current service levels through its review and
approval of county Short-Doyle plans.
The provision of an additional intensive treatment period for
gravely disabled persons is intended to reduce the number
of petitions for temporary conservatorship that are filed
on behalf of gravely disabled persons simply to obtain an
additional period of treatment and without the belief that a
conservator is actually needed and without the intention to
go to trial on the petition.
CONDITIONS FOR CONFINEMENT
At the expiration of the initial 14-day period of intensive
treatment under Welfare and Institutions Code Section
5250, a person may be certified for an additional period
of no more than 30 days of intensive treatment only if the
following conditions are met:
1. The professional staff of the agency or facility that
treats the person has found that the person remains
gravely disabled as a result of a mental health disorder
or impairment by chronic alcoholism; and
2. The person remains unwilling or unable to accept
treatment voluntarily.
The facility must make reasonable attempts to notify
family members or others designated by the patient at
least 36 hours prior to the certification review hearing.
The notification must include the time and place of the
certification hearing. However, the facility must first advise
the patient that he or she has the right to request that
this information not be provided. If the patient prohibits
the facility from notifying family or others, this should
be documented.
[Welfare and Institutions Code Section 5270.15]
As mentioned above, a precondition for the additional
30-day period of intensive treatment is the adoption of
Welfare and Institutions Code Section 5270.10 et seq. by
the county board of supervisors.
A person certified for an additional 30 days must be
provided with notice as discussed below and with a
certification review hearing (see “Certification Review
Hearings,” page3.20) unless a judicial review is requested
(see “Judicial Review Pursuant to a Writ of Habeas Corpus,”
page3.22).

CHA Mental Health Law Manual 2019
3.26
©CALIFORNIA HOSPITAL ASSOCIATION
The facility must obtain the patient’s medication history, if
possible [Welfare and Institutions Code Section 5332].
The professional staff that provides intensive treatment
must analyze and evaluate the patient’s condition at
intervals not to exceed 10 days to determine whether
the patient continues to meet the certification criteria.
Termination of the certification period prior to the 30th
day must be made only when the psychiatrist directly
responsible for the person’s treatment believes, as a result
of his or her personal observations, that the individual has
improved sufficiently to leave, or is prepared to accept
voluntary treatment in the facility that provides intensive
treatment or in another facility.
However, in those situations in which both a psychiatrist
and psychologist have personally evaluated or examined
a person who is undergoing intensive treatment and there
is a collaborative treatment relationship between the
psychiatrist and psychologist, either the psychiatrist or
psychologist may authorize the release of the person, but
only after they have consulted with one another. In the
event of a clinical or professional disagreement regarding
the early release, the person may not be released unless
the facility’s medical director overrules the decision of the
psychiatrist or psychologist opposing the release. Both
the psychiatrist and psychologist must enter their findings,
concerns or objections into the patient’s medical record.
If any other professional who is authorized to release the
person believes the person should be released before
30 days have elapsed, and the psychiatrist directly
responsible for the person’s treatment objects, the matter
must be referred to the medical director of the facility for
the final decision. However, if the medical director is not
a psychiatrist, he or she must appoint a designee who
is a psychiatrist to make these decisions. If the matter is
referred, the person may be released before 30 days have
elapsed only if the psychiatrist believes, as a result of his or
her personal observations, that the individual has improved
sufficiently to leave, or is prepared to accept voluntary
treatment in the facility that provides intensive treatment or
in another facility. [Welfare and Institutions Code Section
5270.35] A psychologist may not order an early release
without potential liability [Ford v. Norton, 89 Cal. App. 4th
974 (2001)] except in the narrow instance outlined in the
previous paragraph.
NOTICE REQUIRED
For a person to be certified for an additional period of
intensive treatment, a second notice of certification must
be completed and signed by:
1. The professional in charge of the facility providing
intensive treatment to the person; and
2. A physician who is, whenever possible, a
board-qualified psychiatrist, or a licensed psychologist
who has a doctoral degree in psychology and at least
five years of postgraduate experience in the diagnosis
and treatment of emotional and mental disorders.
The physician or psychologist who signs must have
participated in the evaluation of the patient’s condition
and determined that the conditions referred to above
were met. [Welfare and Institutions Code Section
5270.20]
If the professional in charge of the facility is the physician
who performed the medical evaluation, or a psychologist,
the second person to sign may be another physician or
psychologist unless one is not available, in which case a
social worker, marriage and family therapist, professional
clinical counselor, or registered nurse who participated in
the evaluation must sign the notice of certification.
REQUIRED FORM OF SECOND NOTICE OF
CERTIFICATION
The “Notice of Certification for Intensive Treatment” form
(CHA Form 12-6) is required for all involuntary intensive
treatment under this law. The form is the same as that
for Welfare and Institutions Code Section 5252. It is
recommended that this form be used for these notification
purposes [Welfare and Institutions Code Section 5250.25].
DELIVERY OF COPIES OF SECOND NOTICE OF
CERTIFICATION
Copies of the second notice of certification of a gravely
disabled person for an additional 30-day period of intensive
treatment must be filed with the court and personally
delivered to the patient. In addition, a copy must be sent
to the patient’s attorney, the district attorney, the public
defender, if any, and the facility that provides the intensive
treatment. Also, the patient must be asked to designate a
person to receive a copy of the certification notice. If the
patient is unable to make such a designation at the time
he or she is certified, the patient must be given another
opportunity to do so as soon as he or she is able. [Welfare
and Institutions Code Section 5270.30]
A hospital that certifies patients should consult legal
counsel regarding the advisability of filing documents with
the court under seal and/or obtaining a protective order
(see HIPAA provision at 45 C.F.R. Section 164.512(e)).
JUDICIAL REVIEW OF INTENSIVE TREATMENT
The procedures for judicial review pursuant to a request
for release made by a patient detained for certification
for a 30-day intensive treatment period are the same as

Chapter 3 — Voluntary Admission and Involuntary Detainment for Mental Health Treatment CHA
3.27
©CALIFORNIA HOSPITAL ASSOCIATION
the procedures for judicial review for an initial 14-day
commitment, discussed under “Judicial Review Pursuant to
a Writ of Habeas Corpus,” page.
A certification for additional treatment for a gravely disabled
person must be for no more than 30 days of intensive
treatment, or until the psychiatrist directly responsible for
the patient’s treatment believes, as a result of his or her
personal observations, that the individual has improved
sufficiently to leave, or is prepared to accept voluntary
treatment in the facility that provides the intensive treatment
or in another facility.
However, in those situations in which both a psychiatrist
and psychologist have personally evaluated or examined
a person who is undergoing intensive treatment and there
is a collaborative treatment relationship between the
psychiatrist and psychologist, either the psychiatrist or
psychologist may authorize the release of the person, but
only after they have consulted with one another. In the
event of a clinical or professional disagreement regarding
the early release, the person may not be released unless
the facility’s medical director overrules the decision of the
psychiatrist or psychologist opposing the release. Both
the psychiatrist and psychologist must enter their findings,
concerns or objections into the patient’s medical record.
If any other professional who is authorized to release the
person believes the person should be released before
30 days have elapsed, and the psychiatrist directly
responsible for the person’s treatment objects, the matter
must be referred to the medical director of the facility for
the final decision. However, if the medical director is not
a psychiatrist, he or she must appoint a psychiatrist to
make the final decision. If the matter is referred, the person
must be released before 30 days have elapsed only if the
psychiatrist believes, as a result of his or her personal
observations, that the individual has improved sufficiently
to leave, or is prepared to accept voluntary treatment
in the facility that provides the intensive treatment or in
another facility. [Welfare and Institutions Code Section
5270.35] A psychologist may not order an early release
without potential liability [Ford v. Norton, 89 Cal. App. 4th
974 (2001)] except in the narrow instance outlined in the
previous paragraph.
A person who has been certified for 30 days of intensive
treatment must be released at the end of 30 days unless
any of the following applies:
1. The patient agrees to receive further treatment on a
voluntary basis.
2. The patient is recommended for conservatorship
pursuant to Welfare and Institutions Code Section
5350 et seq.
3. The patient is dangerous to others (see Welfare and
Institutions Code Section 5300 et seq.).
DAMAGES FOR EXCESSIVE DETENTION
An individual who is knowingly and willfully responsible
for detaining a person for more than 30 days in violation
of the provisions described under D.“Additional Intensive
Treatment for Gravely Disabled Person,” page, is liable to
that person in civil damages [Welfare and Institutions Code
Section 5270.40].
FACILITY PREFERENCE
Whenever a county designates two or more facilities to
provide intensive treatment and the patient or patient’s
family, conservator, or guardian expresses a preference for
one of the facilities, the professional person who certifies
the patient must attempt, if administratively possible, to
comply with the preference. [Welfare and Institutions Code
Section 5270.43]
IMMUNITY FROM LIABILITY
Provided they have complied with the provisions of
Welfare and Institutions Code Section 5270.35, which are
discussed above, the professional in charge of the facility
that provides intensive treatment, a designee, and the
professional directly responsible for the person’s treatment
are not civilly or criminally liable for any action by a person
released before or at the end of the 30-day intensive
treatment period [Welfare and Institutions Code Section
5270.50].
NOTE: The law permits a psychologist, under certain
circumstances, to release a patient who is undergoing
intensive treatment before the end of his or her hold.
However, the immunity statute was not amended in a
corresponding manner to provide immunity for these
psychologists. This may have been a drafting error.
TEMPORARY RELEASE
The professional in charge of an intensive treatment facility,
or a designee, may permit a person certified for 30 days
of intensive treatment to leave the facility for short periods
during the person’s intensive treatment [Welfare and
Institutions Code Section 5270.65]. The permission should
be in writing and documented in the patient’s record. The
“Leave of Absence from Psychiatric Service” form (CHA
Form 12-8) is suggested for use by the hospital.

CHA Mental Health Law Manual 2019
3.28
©CALIFORNIA HOSPITAL ASSOCIATION
EVALUATION OF NEED FOR TEMPORARY
CONSERVATORSHIP
Whenever it appears that a gravely disabled person may
need to be detained beyond the initial 14-day period of
intensive treatment, the professional in charge of the facility
must have the person’s condition evaluated to determine
whether it is likely that the person will need an appointment
of a conservator. This evaluation process should be
initiated before the end of the 14-day period of intensive
treatment and prior to proceeding with an additional
30-day certification. If it appears that, with up to 30 days
of additional treatment, the person is likely to improve so
that a conservator will not be needed, the person may
be certified for the additional 30-day period of treatment.
[Welfare and Institutions Code Section 5270.55]
If no conservatorship referral is made during the 14-day
period and during the 30-day certification it appears
that the person is likely to require the appointment of a
conservator, the conservatorship referral procedure should
be made to allow sufficient time for conservatorship
investigation and other related procedures. The
conservatorship hearing must be held by the 30th day of
the certification. In addition, if a temporary conservatorship
is obtained, it is deemed to run concurrently and not
consecutively with the 30-day certification period.
The maximum involuntary detention period for a gravely
disabled person under Welfare and Institutions Code
Sections 5150, 5250 and 5270.15 is 47 days.
E. Additional Confinement for a Person
Dangerous to Others (Post-Certification
Procedures)
GROUNDS FOR ADDITIONAL CONFINEMENT
At the expiration of the 14-day period of intensive treatment
or an additional 14-day period of intensive treatment for an
imminently suicidal patient, a person may be confined for
further treatment for an additional period, not to exceed
180 days, if the patient is dangerous to others. A person is
dangerous to others only if he or she has:
1. Attempted, inflicted or made a serious threat of
substantial physical harm upon another person after
having been taken into custody, and while in custody,
for evaluation and treatment and, as a result of a
mental disorder, the patient presents a demonstrated
danger of inflicting substantial physical harm upon
others; or
2. Attempted or inflicted physical harm upon another
person, which resulted in the patient’s being taken
into custody and, as a result of a mental disorder, the
patient presents a demonstrated danger of inflicting
substantial physical harm upon others; or
3. Made a serious threat of substantial physical harm
upon another person within seven days before the
patient was taken into custody, which at least in part
resulted in the patient’s being taken into custody,
and presents, as a result of a mental disorder, a
demonstrated danger of inflicting substantial physical
harm upon others.
[Welfare and Institutions Code Section 5300]
The determination that a patient presents a “demonstrated
danger” of substantial physical harm to another may be
based on an assessment of the patient’s present mental
condition, including consideration of past behavior of
the patient within six years prior to the time the patient
attempted, inflicted, or threatened physical harm to another,
and other relevant evidence.
Facilities that commit patients under these provisions
have affirmative obligations to provide treatment for the
underlying causes of the patient’s mental disorders. It is not
necessary, however, to find that the patient is amenable
to treatment, that the treatment will be successful or
potentially successful, or that the patient recognizes
his or her problem and will willingly participate in the
treatment program. Instead, it is only necessary to reach
the determinations described above and make a treatment
program available.
For purposes of this law, the term “custody” means
involuntary detention under LPS uninterrupted by a period
of unconditional release (i.e., a release in which the patient
was not required to return) from a facility that provides
involuntary care and treatment.
PETITION BY PROFESSIONAL PERSON
Responsibility
At any time during the initial 14-day intensive treatment
period, the professional in charge of the facility, or a
designee, may ask the public officer required by Welfare
and Institutions Code Section 5114 (i.e., the county’s
district attorney or county counsel) to petition the superior
court in the county in which the facility providing the
treatment is located to present evidence in support of an
order requiring the patient to undergo an additional period
of treatment on the grounds described in paragraphs 1-3
above. The petition must summarize the facts that support

Chapter 3 — Voluntary Admission and Involuntary Detainment for Mental Health Treatment CHA
3.29
©CALIFORNIA HOSPITAL ASSOCIATION
the contention that the patient is dangerous and be
supported by affidavits that describe the behavior in detail.
Copies of the petition for post-certification treatment and
the supporting affidavits must be served on the patient
on the same day they are filed with the clerk of the
superior court.
A hospital that files a petition with the court should consult
legal counsel regarding the advisability of filing documents
with the court under seal and/or obtaining a protective
order (see HIPAA provision at 45 C.F.R. Section 164.512(e)).
Recommended Form of Petition
Welfare and Institutions Code Section 5301 establishes
the form of the petition. The “Petition for Post-certification
Treatment of Imminently Dangerous Person” form (CHA
Form 12-11) complies with this law and it is recommended
that it be used for these purposes. The petition should be
properly captioned for filing with the superior court.
COURT PROCEEDINGS
A court-conducted hearing or a jury trial, if the patient so
requests, must be held to determine whether one or more
of the grounds for additional confinement is present.
Patient’s Right to Counsel and to a Jury Trial
At the time a petition for post-certification treatment is filed,
the court is required to advise the patient of his or her right
to be represented by an attorney and of his or her right to
a jury trial. The court must assist in finding an attorney, or,
if need be, appoint an attorney if the patient is unable to
obtain counsel. If the patient is financially unable to provide
his or her own attorney, the court must appoint the public
defender or another attorney to represent the patient. The
attorney must advise the patient of his or her rights in
relation to the proceeding and represent him or her before
the court. (See Welfare and Institutions Code Sections
5302 and 5303.)
Time Requirements for Proceedings
The hearing on the petition for post-certification treatment
must be held within four judicial days of the filing of
the petition.
At the time of the hearing, if the patient requests a jury
trial, the trial must commence within 10 judicial days of the
filing of the petition unless the patient’s attorney requests
a delay (continuance), which may be for a maximum of 10
additional judicial days.
The patient must be released if no decision has been made
within 30 days after the petition is filed. Otherwise, until
a final decision on the merits is made by the trial court,
the patient must continue to be treated in the intensive
treatment facility until released by order of the superior
court that has jurisdiction over the action, or unless the
petition for post-certification treatment is withdrawn
[Welfare and Institutions Code Section 5303].
Required Presence of Professional at the Hearing or
Jury Trial
The judge may appoint a psychiatrist or psychologist with
forensic skills to examine the patient and testify at the
hearing or jury trial about the patient’s mental condition
and the threat of substantial physical harm that the patient
presents. Neither the professional, nor designee, who
petitioned for the additional period of treatment, nor the
physicians who provide intensive treatment are required
to be present at the hearing or jury trial unless the patient
subpoenas them.
If a psychiatrist or psychologist with forensic skills is not
appointed, the patient, upon advice of counsel, may
waive the presence at the hearing or at the jury trial of
the professional, or designee, who petitioned for the
additional period of treatment and the physician who
provides intensive treatment. In the event of a waiver,
the professional, designee, or other physicians are not
required to be present at the hearing if it is stipulated that
the certification, supporting affidavit(s), and records of the
physicians concerning the mental condition of the person
named in the petition will be received in evidence. [Welfare
and Institutions Code Section 5303.1]
Findings Required for 180-Day Additional Confinement
If the court or the jury finds that a patient is dangerous
to others pursuant to one of the three criteria listed in
“Grounds for Additional Confinement,” page3.28, the
court will remand the patient to the custody of DSH or to a
facility designated by the county of residence for a further
period of intensive treatment not to exceed 180 days from
the date of judgment. The county from which the patient is
remanded must bear any transportation costs incurred in
placing the patient in the appropriate facility. [Welfare and
Institutions Code Section 5304]
TERMINATION OF ADDITIONAL INTENSIVE TREATMENT
AND PLACEMENT ON OUTPATIENT STATUS
The patient must be released from involuntary treatment
at the expiration of 180 days unless the district attorney
or county counsel files a new petition for post-certification
treatment, and the patient has attempted, inflicted or made
a serious threat of substantial physical harm upon another
during the post-certification treatment, and he or she, by

CHA Mental Health Law Manual 2019
3.30
©CALIFORNIA HOSPITAL ASSOCIATION
reason of mental health disorder, presents a demonstrated
danger of inflicting substantial physical harm on others.
The new petition for post-certification treatment must
be filed in the superior court where the original petition
for post-certification treatment was filed. [Welfare and
Institutions Code Section 5304]
A patient may be placed on outpatient status prior to the
expiration of the 180-day period if:
1. The superintendent or professional in charge of the
licensed facility determines that the patient will no
longer be a danger to the health and safety of others
while on outpatient status and will benefit from
outpatient status;
2. The county behavioral health director agrees with
this determination, identifies an appropriate program,
assumes responsibility for supervising the patient on
outpatient status, and submits reports periodically to
the court; and
3. The district attorney or county counsel, the patient’s
attorney, the court, and the county behavioral health
director are given notice of the proposed transfer of
the patient to outpatient status and do not request a
hearing within five days or, if a hearing was requested,
the court approves the transfer after the hearing.
[Welfare and Institutions Code Section 5305]
A patient whose transfer to outpatient status is approved
may remain on outpatient status for the remaining portion
of the 180-day period unless the county behavioral health
director believes the patient again requires inpatient
treatment. A court hearing is required to determine whether
the patient’s outpatient status should be revoked, but the
county behavioral health director may immediately confine
the patient in a hospital pending the court’s decision if the
director believes that delay in hospitalization would pose a
demonstrated danger of harm to the person or to another
(see Welfare and Institutions Code Sections 5306.5, 5307
and 5308 regarding requirements relating to patients on
outpatient status).
Alternatively, the patient may be released from all
treatment prior to the expiration of the 180-day period
if the psychiatrist directly responsible for the person’s
treatment believes, as a result of his or her personal
observations, that the person being involuntary treated no
longer constitutes a demonstrated danger of substantial
physical harm to others. If any other professional who is
authorized to release the person believes the person should
be released prior to the expiration of the commitment
period, and the psychiatrist directly responsible for the
person’s treatment objects, the matter must be referred
to the medical director of the facility for the final decision.
However, if the medical director is not a psychiatrist, he
or she must appoint a designee who is a psychiatrist
to make the final decision. If the matter is referred, the
person must be released prior to the expiration of the
commitment period only if the psychiatrist believes, as
a result of his or her personal observations, that the
individual being involuntarily treated no longer constitutes
a demonstrated danger of substantial physical harm to
others. A psychologist may not order an early release
without potential liability [Ford v. Norton, 89 Cal. App. 4th
974 (2001)].
NOTE: The law that permits a psychologist, under certain
circumstances, to release a patient before the end of
the hold does not apply to patients who are detained for
additional intensive treatment.
The patient may be released five days after notice is given
to the district attorney or county counsel, the patient’s
attorney, the court and the county behavioral health director,
unless one of these parties requests a hearing. If a hearing
is requested, the patient may not be released unless the
court approves the release after the hearing. [Welfare and
Institutions Code Section 5309]
IMMUNITY FROM LIABILITY
Provided they have complied with the provisions of Welfare
and Institutions Code Sections 5300-5309, which are
discussed above, the following persons are not civilly or
criminally liable for any action by a person released at or
before the end of a 90-day period:
1. The superintendent;
2. The professional in charge of the hospital that provides
the involuntary treatment, or a designee;
3. The medical director of the facility, or a designee,
described in Welfare and Institutions Code Section
5309(a); and
4. The psychiatrist directly responsible for the person’s
treatment.
[Welfare and Institutions Code Section 5306]
NOTE: The law that permits a psychologist, under certain
circumstances, to release a patient before the end of his
or her hold does not apply to patients who are detained for
additional intensive treatment. Thus, there is no immunity
for a psychologist who releases such a patient.

Chapter 3 — Voluntary Admission and Involuntary Detainment for Mental Health Treatment CHA
3.31
©CALIFORNIA HOSPITAL ASSOCIATION
F. Additional Treatment for Gravely Disabled
Person (LPS Conservatorship)
This portion of the manual is designed to present only
a basic overview of the process for establishing a
conservatorship under LPS. The facility should consult with
the officials responsible for conservatorship investigations
and with legal counsel before adopting policies for or
initiating conservatorship. [Welfare and Institutions Code
Section 5350 et seq.]
A discussion of the differences between an LPS
conservatorship and a Probate Code conservatorship
is found under “Caution: Type of Conservatorship,”
page3.3.
CONSERVATORSHIP RECOMMENDATION
When the professional in charge of an agency that
provides comprehensive evaluation or a facility that
provides intensive treatment determines that a patient is
gravely disabled as a result of a mental health disorder
or impairment by chronic alcoholism and the person is
unwilling to accept or incapable of accepting treatment
voluntarily, the professional may recommend that a
conservatorship be established. This recommendation
must be made to the officer that provides conservatorship
investigation for the county the person resided in prior to
admission to the facility. The responsible officer may have
developed an application form which should be completed
by the facility. The facility should request these forms from
the patient’s county of residence.
Inpatient
If the professional in charge of a facility that provides
intensive treatment recommends a conservatorship
under Welfare and Institutions Code Section 5352 as
discussed above, the proposed conservatee may be held
in that facility for a period not to exceed three days after
the expiration of the initial 14-day certification period if
this additional time period is necessary to allow for the
filing of the petition for temporary conservatorship and
the establishment of the temporary conservatorship by
the court.
Other Person
The professional in charge of an agency that provides
comprehensive evaluation or a facility that provides
intensive treatment may recommend conservatorship for a
person without the patient being an inpatient in the facility if
the professional, or a designee, has:
1. Examined and evaluated the person and determined
that he or she is gravely disabled, and
2. Determined that future examination on an inpatient
basis is not necessary to make the determination that
the person is gravely disabled.
[Welfare and Institutions Code Section 5352]
INVESTIGATOR ACTION
If the officer who provides the conservatorship investigation
concurs with the recommendation, he or she will file a
conservatorship petition with the superior court in the
patient’s county of residence. A temporary conservatorship
may be requested by the officer and, if granted, the
investigating officer or another person designated by
the county will be appointed to serve as the temporary
conservator. A temporary conservatorship automatically
expires after 30 days unless the court extends the time.
A temporary conservator may require the patient to be
detained in a facility that provides intensive treatment
pending the determination of whether or not a year-long
conservatorship will be established. The patient has the
right to judicial review during this period, as described
in “Judicial Review Pursuant to a Writ of Habeas Corpus,”
page3.22.
COURT HEARING
A court hearing will be held and county counsel
may be appointed to represent the patient if the
county has authorized such appointments. At the
conclusion of the hearing, the judge may rule that no
conservatorship is appropriate, or the judge may order a
year-long conservatorship.
CONSERVATORSHIP ESTABLISHED
If a year-long conservatorship is established, the court
will specify the conservator’s rights and may authorize
the conservator to require the conservatee to receive
treatment related specifically to remedying or preventing
the recurrence of the conservatee’s grave disability, or
to require the conservatee to receive routine medical
treatment unrelated to the conservatee’s grave disability.
[Welfare and Institutions Code Section 5357] (See
C.“Adults Under Conservatorship,” page2.15, for more
information about an LPS conservator’s authority to
consent to, or refuse, nonpsychiatric medical treatment.)
The facility should obtain a copy of the certified
conservatorship papers to determine whether the
conservator has the right to hospitalize the conservatee.
The copy should be placed in the patient’s medical record.

CHA Mental Health Law Manual 2019
3.32
©CALIFORNIA HOSPITAL ASSOCIATION
EXPIRATION OF CONSERVATORSHIP
A conservatorship will automatically expire at the end of
one year unless it is renewed [Welfare and Institutions Code
Section 5361]. The period of service of the termporary
conservator is not included in the one-year period. The
court clerk is required to give the conservator, conservatee,
conservatee’s attorney and the facility where a conservatee
is detained 60 days notice that the year term is about to
expire. An application may be submitted to renew the
conservatorship at any time during this 60-day period.
[Welfare and Institutions Code Section 5362]
VI. DETENTION OF PATIENT IN A
NONDESIGNATED FACILITY
A. Immunity for Detaining Patient
Health and Safety Code Section 1799.111 provides that
specified general acute care hospitals, acute psychiatric
hospitals, licensed professional staff of these hospitals, and
any physician providing emergency medical services in
any department of these hospitals is not civilly or criminally
liable for detaining a patient, if all of the following conditions
exist during the detention:
1. The patient cannot be safely released from the hospital
because, in the opinion of the treating physician (or a
clinical psychologist with the medical staff privileges,
clinical privileges, or professional responsibilities
provided in Health and Safety Code Section 1316.5,
described below), the patient, as a result of a mental
health disorder, presents a danger to himself or herself,
or others, or is gravely disabled. “Gravely disabled”
is defined, for the purpose of this law, as the inability
to provide for basic personal needs for food, clothing,
or shelter.
NOTE: Health and Safety Code Section 1316.5
states that state owned and operated health
facilities that offer services within the scope of
practice of a psychologist must establish rules and
procedures for consideration of an application for
medical staff membership and clinical privileges
submitted by a clinical psychologist. Private health
facilities may appoint clinical psychologists on any
terms and conditions as the facility may establish.
However, if a particular service is offered by a
health facility that permits clinical psychologists
on its medical staff, which service both physicians
and clinical psychologists are authorized by law to
perform, such service may be performed by either,
without discrimination.
2. The hospital staff, treating physician, or appropriate
mental health professional has made, and documented,
repeated unsuccessful efforts to find appropriate
mental health treatment for the patient. Telephone
calls or other contacts required by this paragraph
must commence as soon as the treating physician has
determined when the patient will be medically stable for
transfer. In no case may the contacts required by this
paragraph begin after the patient becomes medically
stable for transfer. If the hospital starts making the
contacts after the patient is medically stable for
transfer, the hospital may lose the legal immunity
conferred by this law.
3. The patient is not detained beyond 24 hours.
4. There is probable cause for the detention.
5. If the patient is detained beyond eight hours, but
less than 24 hours, both of the following additional
conditions must be met:
a. A discharge or transfer for appropriate evaluation
or treatment has been delayed because of
the need for continuous and ongoing care,
observation, or treatment that the hospital
is providing.
b. In the opinion of the treating physician, or a clinical
psychologist with the medical staff privileges or
professional responsibilities provided for in Section
1316.5, the patient, as a result of a mental health
disorder, is still a danger to himself or herself or
others, or is gravely disabled (as defined above).
It appears that minors may be detained under this law,
although the law does not expressly mention minor patients.
CHA has developed a form, “Detention of Patient with
Psychiatric Emergency in a Nondesignated Health Facility
(Health and Safety Code Section 1799.111)” (CHA Form
12-12), that hospitals may use to document compliance
with this law.
B. Immunity for Actions of Patient After Release
The facilities and professionals listed above are not civilly
or criminally liable for the actions of a patient detained up
to 24 hours after release if the following conditions exist
during the detention:
1. The patient has not been admitted to a hospital for
evaluation and treatment under Welfare and Institutions
Code Section 5150.
2. The release from the hospital is authorized by a
physician or a clinical psychologist with the medical

Chapter 3 — Voluntary Admission and Involuntary Detainment for Mental Health Treatment CHA
3.33
©CALIFORNIA HOSPITAL ASSOCIATION
staff privileges or professional responsibilities provided
for in Health and Safety Code Section 1316.5, who
determines, based on a face-to-face examination
of the patient, that the patient does not present a
danger to self or others and is not gravely disabled.
The clinical psychologist may authorize the release
only after consulting with the physician. If there is a
disagreement, the patient must be detained unless the
hospital’s medical director overrules the decision of
the physician opposing the release. The physician and
psychologist must both enter their findings, concerns
or objections in the patient’s medical record.
C. Hospitals Covered by This Law
The hospital does not need to be designated by the county
to hold patients pursuant to this law. In fact, hospitals
that are designated by the county under LPS do not enjoy
these immunities.
D. Relationship to Other Laws
This law does not affect the responsibility of a hospital to
comply with all state laws and regulations pertaining to the
use of seclusion and restraint and psychiatric medications
for psychiatric patients. In addition, patients detained
under this law retain their legal rights regarding consent
for medical treatment (i.e., the hospital cannot treat the
patient without his or her consent, or the consent of the
legal representative if the patient has been determined by a
physician to lack capacity to consent to treatment).
E. Credit for Time Detained
A patient detained under Health and Safety Code
Section 1799.111 must be credited for the time detained
if he or she subsequently is placed on a 72-hour hold
under Welfare and Institutions Code Section 5150. A
transferring hospital should provide to the receiving hospital
documentation regarding the length of time the person was
detained, so that the receiving hospital can comply with
this requirement.
VII. COURT-ORDERED EVALUATION OF PERSONS
WHO MAY HAVE A MENTAL HEALTH
DISORDER
LPS specifies the procedures by which an individual may
apply to the appropriate county agency for a petition for a
court-ordered evaluation of a person alleged to be a danger
to self or others or gravely disabled as a result of mental
health disorder [Welfare and Institutions Code Section
5200].
This procedure is available when involuntary detention is
not or will not be authorized by persons permitted to initiate
involuntary detention under Welfare and Institutions Code
Section 5150 (see “Conditions for Detention,” page3.9).
VIII. REPORTING PATIENT ESCAPE,
DISAPPEARANCE, RELEASE OR TRANSFER
The law requires that hospitals notify law enforcement
officers and/or other persons of specified patient escapes,
disappearances, releases, or transfers. The relevant laws
and their requirements are described in X.“Notifying Law
Enforcement Officers of Patient Presence, Release or
Disappearance,” page7.36.
IX. INVOLUNTARY OUTPATIENT TREATMENT
California law permits courts to order patients to
participate in outpatient mental health treatment [Welfare
and Institutions Code Sections 5345-5349.5]. This law is
operative only in those counties in which the county board
of supervisors, by resolution or through the county budget
process, authorizes its application and makes a finding that
no voluntary mental health program serving adults, and
no children’s mental health program, will be reduced as a
result of the implementation of this law. A county choosing
to implement this law is required to provide a wide range
of outpatient services to both voluntary and involuntary
patients of every cultural and linguistic background, age,
gender, physical disability, etc. A county implementing this
law is also required to undertake detailed data collection,
evaluation and reporting.
A petition must be filed with the court to initiate the process
of involuntary outpatient treatment for a particular patient.
A. Contents of Petition
A court must find by clear and convincing evidence that the
following facts stated in a verified petition are true:
1. The patient is 18 years of age or older.
2. The patient is suffering from a mental illness as defined
in Welfare and Institutions Code Section 5600.3(b)(2)
and (3). This law defines a mental disorder as one that
is severe in degree and persistent in duration, which
may cause behavioral functioning which interferes
substantially with the primary activities of daily living,
and which may result in an inability to maintain stable
adjustment and independent functioning without
treatment for a long or indefinite period of time. These
disorders include, but are not limited to, schizophrenia,

CHA Mental Health Law Manual 2019
3.34
©CALIFORNIA HOSPITAL ASSOCIATION
bipolar disorder, post-traumatic stress disorder, as well
as major affective disorders or other severely disabling
mental disorders. Patients must meet additional criteria
related to functional impairments.
3. There has been a clinical determination that the
patient is unlikely to survive safely in the community
without supervision.
4. The patient has a history of lack of compliance with
mental health treatment, in that at least one of the
following is true:
a. The patient’s mental illness has, at least twice
within the last 36 months, been a substantial
factor in necessitating hospitalization, or receipt of
services in a forensic or other mental health unit
of a state correctional facility or local correctional
facility, not including any period during which
the patient was hospitalized or incarcerated
immediately preceding the filing of the petition.
b. The patient’s mental illness has resulted in one
or more acts of serious and violent behavior
toward himself or herself or another, or threats, or
attempts to cause serious physical harm to himself
or herself or another within the last 48 months,
not including any period in which the patient was
hospitalized or incarcerated immediately preceding
the filing of the petition.
5. The patient has been offered an opportunity to
participate in a treatment plan provided by the local
mental health department and the patient continues to
fail to engage in treatment.
6. The patient’s condition is substantially deteriorating.
7. Participation in the assisted outpatient treatment
program would be the least restrictive placement
necessary to ensure the patient’s recovery and stability.
8. In view of the patient’s treatment history and current
behavior, the patient needs assisted outpatient
treatment to prevent a relapse or deterioration that
would likely result in grave disability or serious harm to
himself or herself, or to others.
B. Who May Initiate a Petition
A petition may be filed by the county behavioral health
director or designee in the superior court in the county in
which the patient is present.
Any of the following persons may request the county
behavioral health director to file a petition:
1. Any adult cohabitant of the patient;
2. Any adult parent, spouse, sibling or child of the patient;
3. The director of any public or private agency, treatment
facility, charitable organization, or licensed residential
care facility providing mental health services to the
patient in whose institution the patient resides;
4. The director of a hospital in which the patient is
hospitalized;
5. A licensed mental health treatment provider who is
either supervising the treatment of, or treating the
mental illness of, the patient; or
6. A peace officer, parole officer, probation officer
assigned to supervise the patient.
Upon request of one of these persons, the county
behavioral health director must conduct an investigation
into the appropriateness of filing a petition. A hospital or
other health care provider should consult its legal counsel
about a patient’s confidentiality rights prior to disclosing
medical information to the county behavioral health
director for purposes of petitioning a court for involuntary
outpatient treatment.
C. Procedure
The petition must contain specified information (see
A.“Contents of Petition,” page3.33), and must be
accompanied by an affidavit of a licensed mental health
treatment provider designated by the local mental health
director. The court will hold a hearing. The patient has
the right to be represented by counsel, to be present at
the hearing, to present evidence, to call witness, and to
cross-examine witness. The patient has the right to judicial
review by habeas corpus and to appeal decisions. If the
court determines that the patient meets the criteria for
assisted outpatient treatment, it may be ordered for an
initial period not to exceed six months. (Procedures exist for
lengthening this time period.) The court order will state the
categories of assisted outpatient treatment that the patient
is to receive. Involuntary medication is not allowed without
a separate order by the court pursuant to Welfare and
Institutions Code Sections 5332-5336, inclusive.
Every 60 days, the director of the outpatient treatment
program must file an affidavit with the court that the patient
continues to meet the criteria for assisted outpatient
treatment. The patient has the right to a hearing if he or
she disagrees.
Failure to comply with an order of assisted outpatient
treatment alone may not be grounds for involuntary civil
commitment or a finding that the patient is in contempt
of court.

Chapter 4 — Contents
4 Rights of Mental Health Patients
©CALIFORNIA HOSPITAL ASSOCIATION
I. INTRODUCTION ....................................... 4.1
II. PATIENT RIGHTS UNDER STATE LAW ........ 4.1
A. Notifying Patients of Their Rights ................4.1
Posters and Booklets ........................................4.1
Documentation
.................................................4.2
B. Patient Rights Under Welfare and
Institutions Code Section 5325
....................4.2
Patients Covered by the Law ............................4.2
List of Rights
....................................................4.2
Waiver of Rights
................................................4.3
C. Patient Rights Under Welfare and
Institutions Code Section 5325.1
.................4.3
D. Rights Noted in Other Laws .........................4.3
Right to Discharge ............................................4.3
Required Statement of California Law
................4.3
E. Complaint Procedures ..................................4.3
Complaint to Advocates ....................................4.3
Complaint to CDPH
..........................................4.4
Complaint to Hospital
.......................................4.4
F. Denial of Patient Rights ................................4.4
Denial for Good Cause ......................................4.4
Exceptions
........................................................4.4
Documentation of Denial of Rights
....................4.5
Disclosure of Denial of Rights
............................4.5
Restoration of Rights
........................................4.6
III. SEXUAL ORIENTATION CHANGE
THERAPY FOR MINORS
............................ 4.6
IV. AFTERCARE PLAN ................................... 4.6
A. Facilities Subject to This Law .......................4.6
B. Contents of the Aftercare Plan ..................... 4.7
C. Persons Who Must Be Given an
Aftercare Plan
................................................4.7
V. MENTAL HEALTH ADVOCACY
PROGRAMS
............................................. 4.7
A. Statewide Protection and Advocacy
Organization ...................................................4.7
Investigations ....................................................4.8
Noninvestigative Purposes
................................4.8
Delay or Denial of Access
..................................4.8
Copying Costs
..................................................4.8
Access to Records of Specified Persons
........... 4.9
Types of Records Available to DRC
...................4.9
Limitations on DRC Access
.............................4.10
Timelines for Compliance
................................ 4.10
Prohibitions on Redisclosure of Information
by DRC
..........................................................4.11
B. County Patients’ Rights Advocates ...........4.11
Duties of County Patients’ Rights Advocates ...4.11
Authority of County Patients’ Rights
Advocate
........................................................ 4.11
Agreement for Advocacy Services for Client
....4.11
Investigation Based Upon Probable Cause
...... 4.12
Access to Persons and Facilities
.....................4.12
Limitations on Access to Patients
....................4.12
Access to Records and Information
.................4.13
C. Retaliation and Discrimination
Prohibited
.....................................................4.15
D. Penalties .......................................................4.15
E. Immunity From Liability ..............................4.15
VI. PSYCHIATRIC ADVANCE DIRECTIVES ..... 4.15
VII. SEXUAL ACTIVITY BETWEEN PATIENT
AND PROVIDER
..................................... 4.16
A. Sexual Activity Between Involuntarily
Confined Patient and Hospital
Employee is a Crime
...................................4.16
B. Unprofessional Conduct .............................4.16
C. Patient Alleges Prior Psychotherapist
Sexual Activity
.............................................4.16
FORMS & APPENDICES
13-3
S
Aftercare Plan
Forms and Appendices can be found at the back of the manual and
online for CHA members at www.calhospital.org/free-resources.
“S” denotes that the form is provided in English and Spanish.

4 Rights of Mental Health Patients
4.1
©CALIFORNIA HOSPITAL ASSOCIATION
I. INTRODUCTION
Both state and federal law contain multiple provisions
regarding patients’ rights. Requirements regarding patient
rights in general — that is, rights that apply to all patients,
not just mental health patients — are described in chapter 1
of CHA’s Consent Manual. Patients’ rights that are specific
to restraint and seclusion are described in chapter 5 of
this manual.
This chapter discusses the rights afforded under state and
federal law to persons who are involuntarily or voluntarily
admitted to a facility for mental health services, including
evaluation and treatment of a mental disorder, inebriation,
or drug use. These rights are codified primarily in the
Lanterman-Petris-Short (LPS) Act [Welfare and Institutions
Code Section 5000 et seq.]. Other relevant principles that
apply to these patients are found in Welfare and Institutions
Code Section 6000 et seq. and in state and federal judicial
decisions interpreting these statutes.
II. PATIENT RIGHTS UNDER STATE LAW
The Lanterman-Petris-Short Act contains two provisions
that discuss the rights of mental health patients:
1. Welfare and Institutions Code Section 5325. A list of
these rights must be prominently posted in the facility
in English, Spanish, and the predominant language of
the community, and explained to patients in a language
or modality accesible to the patient. These rights may
be denied for good cause (with some exceptions).
Details about these rights and denial of rights are
described in this chapter.
2. Welfare and Institutions Code Section 5325.1. This
statute states that persons with mental illness have
the same legal rights and responsibilities guaranteed
to all other persons by the constitutions and laws
of the United States and California. The statute also
states that persons who have been treated for mental
illness may not be subject to discrimination under any
program or activity that receives public funds. Finally,
this statute states the “intent of the legislature” that
persons with mental illness have certain rights. This list
of patient rights differs from the list found in Welfare
and Institutions Code Section 5325. These rights are
not subject to denial. It is not clear why the legislature
enacted a second list of patient rights. Details about
these rights are described in this chapter.
NOTE: As a legal matter, the “intent of the legislature”
is sometimes considered by a judge who is trying to
interpret an ambiguous provision of law. If a law is clear
and unambiguous, the judge will not consider legislative
intent. It is only when a statute can be interpreted in more
than one way that the judge will consider legislative intent
to resolve the ambiguity. It is not clear why the legislature
enacted a list of patient rights as “legislative intent.”
A. Notifying Patients of Their Rights
POSTERS AND BOOKLETS
A facility that treats patients listed in “Patients Covered by
the Law,”page4.2, must post a list of patient rights in
English, Spanish, and the predominant languages of the
community, in all wards and common living areas.
In addition, the facility must notify each patient personally
of his or her rights, both orally and in writing, in a
language the patient can understand. The patient’s
rights must be brought to the patient’s attention by other
means if he or she is unable to read or understand the
information provided.
The California Department of Health Care Services (DHCS)
has developed posters and booklets that facilities may
use to notify patients of their rights. The booklet, “Rights
for Individuals in Mental Health Facilities,” and posters are
available in many languages at www.dhcs.ca.gov/services/
pages/office-of-patients-rights.aspx.
These posters and booklets do not fulfill the
following requirements:
1. Notifying voluntary patients that they can discharge
themselves (see “Right to Discharge,”page4.3).
2. Notifying patients that nobody may be presumed
incompetent due to evaluation or treatment for a
mental disorder or chronic alcoholism (see “Required
Statement of California Law,”page4.3).

CHA Mental Health Law Manual 2019
4.2
©CALIFORNIA HOSPITAL ASSOCIATION
3. Notifying patients about how to file a complaint with
the hospital (see “Complaint to Hospital,”page4.4).
Hospitals should adopt a procedure to ensure that these
requirements are met.
[Welfare and Institutions Code Section 5325; Title 9,
California Code of Regulation, Sections 862; Title 22,
California Code of Regulations, Section 71507]
DOCUMENTATION
A note that the hospital notified, or attempted to notify, the
patient of his or her rights must be entered in the patient’s
medical record within 24 hours of admission. This may
be accomplished by having the patient sign a form that
lists the patients’ rights, or another form acknowledging
receipt of the DHCS booklet. One copy of the signed form
should be given to the patient and the original placed in the
medical record.
If the patient cannot be notified of patients’ rights within
24 hours of admission, a note about the reason should be
entered in the patient’s medical record and the advisement
of rights should occur as soon as the patient is capable
of understanding [Title 9, California Code of Regulations,
Section 862].
B. Patient Rights Under Welfare and Institutions
Code Section 5325
PATIENTS COVERED BY THE LAW
Welfare and Institutions Code Section 5325 lists certain
rights enjoyed by all mental health patients, including:
1. Each person involuntarily detained for evaluation or
treatment under the LPS Act;
2. Each person admitted as a voluntary patient for
psychiatric evaluation or treatment to any facility
(as defined in Health and Safety Code Section
1250), including a general acute care hospital,
acute psychiatric hospital, skilled nursing facility, or
intermediate care facility in which psychiatric evaluation
or treatment is offered; and
3. Each person committed to a state hospital.
LIST OF RIGHTS
The patients’ rights are:
1. To wear one’s own clothes, to keep and use personal
possessions including toilet articles, and to keep and
spend a reasonable sum of one’s own money for
canteen expenses and small purchases.
2. To have access to individual storage space for
private use.
3. To see visitors each day.
4. To have reasonable access to telephones, both to
make and to receive confidential calls, or to have calls
made for them.
5. To have ready access to letter writing materials,
including stamps, and to mail and receive
unopened correspondence.
6. To refuse convulsive treatment including, but not
limited to, electroconvulsive treatment, any treatment
for a mental condition that depends on the induction
of a convulsion by any means, and insulin coma
treatment. NOTE: This right may be denied only under
the conditions specified in Welfare and Institutions
Code Section 5326.7 (see D.“Convulsive Therapy and
Insulin Coma Treatment,”page2.49).
7. To refuse psychosurgery. (NOTE: This right may not
be denied.) “Psychosurgery” is defined as those
operations referred to as lobotomy, psychiatric surgery,
behavioral surgery, and all other forms of brain surgery
if the surgery is performed for the purpose of any of
the following:
a. Modification or control of thoughts, feelings,
actions, or behavior rather than the treatment
of a known and diagnosed physical disease of
the brain.
b. Modification of normal brain function or normal
brain tissue in order to control thoughts, feelings,
actions, or behavior.
c. Treatment of abnormal brain function or abnormal
brain tissue in order to modify thoughts, feelings,
actions, or behavior when the abnormality is not
an established cause for those thoughts, feelings,
actions, or behavior.
Psychosurgery includes prefrontal sonic treatment if
there is any possibility of destruction of brain tissue
or brain cells. [Title 9, California Code of Regulations,
Section 857]
8. To see and receive the services of a patient advocate
who has no direct or indirect clinical or administrative
responsibility for the patient. (NOTE: This right may not
be denied.)
9. Other rights as specified by regulation. (There are no
additional rights specified by regulation at this time.)

Chapter 4 — Rights of Mental Health Patients CHA
4.3
©CALIFORNIA HOSPITAL ASSOCIATION
WAIVER OF RIGHTS
The rights listed above may not be waived by the patient’s
parent, guardian, or conservator. However, these rights
may be denied when “good cause” exists (except as noted
in the list above). The procedure for denying these rights
when good cause exists is discussed in F.“Denial of Patient
Rights,”page4.4.
C. Patient Rights Under Welfare and Institutions
Code Section 5325.1
Welfare and Institutions Code Section 5325.1 expressly
states that persons with mental illness have the same
legal rights and responsibilities guaranteed to all other
persons by the U.S. Constitution and the laws of the state
of California, unless specifically limited by federal or state
law. If an otherwise qualified person is involuntarily detained
for evaluation or treatment, or is admitted as a voluntary
patient to a health facility in which psychiatric evaluation or
treatment is offered, he or she may not be excluded from
participation in, denied the benefits of, or subjected to
discrimination under, any program or activity that receives
public funds.
In addition, Welfare and Institutions Code Section 5325.1
declares the legislative intent that persons with mental
illness shall have rights including, but not limited to,
the following:
1. A right to treatment services which promote the
potential of the person to function independently.
Treatment should be provided in ways that are least
restrictive of the personal liberty of the individual.
2. A right to dignity, privacy, and humane care.
3. A right to be free from harm, including unnecessary
or excessive physical restraint, isolation, medication,
abuse, or neglect. Medication may not be used
as punishment, for the convenience of staff, as a
substitute for a program, or in quantities that interfere
with the treatment program.
4. A right to prompt medical care and treatment.
5. A right to religious freedom and practice.
6. A right to participate in appropriate programs of
publicly supported education.
7. A right to social interaction and participation in
community activities.
8. A right to physical exercise and
recreational opportunities.
9. A right to be free from hazardous procedures.
D. Rights Noted in Other Laws
RIGHT TO DISCHARGE
A person who has the lawful right to discharge himself
or herself from a facility must be informed of that right at
the time of admission to the facility. This information is
not expressly included in the DHCS posters and booklets.
Hospitals should adopt a procedure to ensure that
patients are given this information. If the person decides
to discharge himself or herself from the facility rather
than voluntarily accepting a denial of patients’ rights, that
decision must be documented in the medical record and
the person must be permitted to leave the facility.
REQUIRED STATEMENT OF CALIFORNIA LAW
Welfare and Institutions Code Section 5331 states that a
person who leaves a mental health facility after evaluation
or treatment for a mental disorder or chronic alcoholism,
regardless of whether that evaluation or treatment was
voluntarily or involuntarily received, must be given the
following statement of California law:
No person may be presumed to be incompetent
because he or she has been evaluated or treated for
mental disorder or chronic alcoholism, regardless of
whether such evaluation or treatment was voluntarily
or involuntarily received.
This information is not expressly included in the DHCS
posters and booklets. Hospitals should adopt a procedure
to ensure that patients are given this statement. The law
does not specify when this information must be given to
the patient.
E. Complaint Procedures
A patient may complain to a patients’ rights advocate,
CDPH, or to the hospital. Patients must be given
information about these procedures, as described below.
This information is not expressly included in the DHCS
posters and booklets. Hospitals should adopt a procedure
to ensure that patients are given this information.
COMPLAINT TO ADVOCATES
A patient who believes a right has been abused, punitively
withheld, or unreasonably denied may file a complaint
with a patients’ rights advocate. The patients’ rights
advocates are assigned by each county behavioral health

CHA Mental Health Law Manual 2019
4.4
©CALIFORNIA HOSPITAL ASSOCIATION
director to handle complaints of mental health patients
(see B.“County Patients’ Rights Advocates,”page4.11).
Residents’ rights advocates are assigned to handle
complaints from patients with developmental disabilities.
The posted complaint procedure must contain
the following:
1. Notification that a patient who believes a right of
his/hers has been abused, punitively withheld, or
unreasonably denied may file a complaint with the
patients’ rights advocate.
2. The name of the patients’ rights advocates assigned
to handle complaints, their telephone number(s), and
times they may be contacted.
[Title 9, California Code of Regulations, Section 864]
The patients’ rights advocate must take action to
investigate and resolve a complaint within two working
days of receipt. A complainant who is dissatisfied with
the patients’ rights advocate’s resolution of the complaint
may appeal. The appeals procedure is described in Title 9,
California Code of Regulations, Section 864.
The DHCS poster and booklet have a space on them for
the name and contact information of the local patients’
rights advocate. The booklet also gives the names and
contact information of two statewide organizations.
However, the statement included in paragraph 1. above is
not expressly included. Hospitals should adopt a procedure
to ensure that patients are given this information.
COMPLAINT TO CDPH
Information about how to submit complaints to CDPH must
be posted [Title 22, California Code of Regulations, Section
71507]. The DHCS posters do not contain language that
fulfills this requirement. Therefore, the hospital must post an
additional poster informing patients how to file a complaint
as well as the address and phone number of the CDPH
local district office.
COMPLAINT TO HOSPITAL
Information about how a patient may file a complaint with
the hospital must be provided to the patient [Title 22,
California Code of Regulations, Section 71507(d)]. The
DHCS posters and booklets do not contain language
that fulfills this requirement. Therefore, the hospital must
post another poster or handout informing patients of the
hospital’s complaint procedure must be used. Hospitals
that participate in the Medicare program are required
to have a specified grievance policy (see “Complaint to
Hospital,”page4.4, for details).
F. Denial of Patient Rights
DENIAL FOR GOOD CAUSE
The professional person in charge of the facility or a
designee may, for good cause, deny a person a right
specified under Welfare and Institutions Code Section 5325
(see B.“Patient Rights Under Welfare and Institutions Code
Section 5325,”page4.2).
EXCEPTIONS
The rights to refuse psychosurgery or to see and receive
the services of a patient advocate may not be denied, and
the right to refuse convulsive treatment may be denied only
under the conditions specified in Welfare and Institutions
Code Section 5326.7 (see D.“Convulsive Therapy and
Insulin Coma Treatment,”page2.49).
Definition
The term “professional person in charge of a facility”
means a person as defined in Title 9, California Code of
Regulations, Section 623 (psychiatrist), 624 (psychologist),
625 (social worker), 626 (marriage and family therapist),
or 627 (registered nurse with a master’s degree in
psychiatric or public health nursing) who is designated
by the governing board of the facility or person having
control of the facility as the professional person clinically in
charge of the facility for purposes of LPS. The designation
must be in writing. [Title 9, California Code of Regulations,
Section 822]
Good Cause
Good cause must be established to justify a denial of
rights [Title 9, California Code of Regulations, Section
862 et seq.].
Good cause for denying a patient the exercise of a right
exists when the professional person in charge of a facility or
a designee has good reason to believe:
1. That the exercise of the specific right would be injurious
to the patient; or
2. That there is evidence that the specific right, if
exercised, would seriously infringe upon the rights of
others; or
3. That the institution or facility would suffer serious
damage if the specific right is not denied; and
4. That there is no less restrictive way of protecting the
interests specified above.
[Title 9, California Code of Regulations, Section 865.2]

Chapter 4 — Rights of Mental Health Patients CHA
4.5
©CALIFORNIA HOSPITAL ASSOCIATION
The reason used to justify the denial of a patient right must
be related to the specific right denied. A right must not be
withheld or denied as a punitive measure. A right may not
be considered a privilege to be earned.
Treatment modalities must not include the denial of any
right specified in Welfare and Institutions Code Section
5325. Waivers signed by the patient or by the responsible
relative, guardian, or conservator must not be used as a
basis for denying these rights.
When a right has been denied, staff must use the least
restrictive means of managing the problem that led to
the denial.
Restraint and Seclusion
When a patient is restrained or secluded, a denial of rights
is deemed to have occurred, even though “restraint” and
“seclusion” are not mentioned in the list of patients’ rights
under Welfare and Institutions Code Section 5325. This
is because when a patient is restrained or secluded, the
situation implies the denial of other patients’ rights that are
listed, such as the right of reasonable access to telephones
and the right to have ready access to letter writing
materials.
If a patient is restrained or secluded and does not
specifically request to exercise any listed right, then only
the restraint or seclusion must be documented. If the
patient is restrained or secluded and requests to exercise a
listed right (for example, the patient asks to make a phone
call), then both the restraint (or seclusion) and the other
specifically denied right (in the example, the right to make a
phone call) must be documented. (See chapter 5 for more
information about restraint and seclusion.)
DOCUMENTATION OF DENIAL OF RIGHTS
Each denial of a patient’s rights must be noted in the
medical record [Welfare and Institutions Code Section
5326; Title 9, California Code of Regulations, Sections
865.3 and 865.4]. Documentation must take place
immediately whenever a right is denied, and each denial of
a right must be documented regardless of the gravity of the
reason for the denial or the frequency with which a specific
right is denied in a particular facility or to a particular
individual. As mentioned above, if a patient in seclusion
or restraints is denied any right, the denial must also be
documented. The documentation must include:
1. The specific right denied.
2. The date and time the right was denied.
3. The reason (good cause) for denial of the right.
4. The date of review if the denial of the right extended
beyond 30 days.
5. The signature of the professional person in charge of
the facility or a designee.
The patient must be told the contents of the documentation.
Forms
The former DMH has developed two forms for providers to
use, “Patients’ Rights Denial — Monthly Tally” and “Denial
of Rights/Seclusion and Restraint Monthly Report.”
Both forms may be found at www.dhcs.ca.gov/
formsandpubs/forms/pages/mental_health-Forms.aspx.
The “Patients’ Rights Denial — Monthly Tally” form should
be completed for each patient each month. The form has a
chart showing each day of the month. A number has been
assigned to each right (for example, “5” represents the right
to see visitors each day). If a denial of rights occurs, the
number assigned to the right that was denied is entered
into the box underneath the day of the month the denial
occurred. This form must be filed in the patient’s medical
record.
The “Denial of Rights/Seclusion and Restraint Monthly
Report” form must be completed monthly. This form
captures all patients and all denials of rights in a facility
in a particular month. The form must be submitted to
the local behavioral health director or the county or state
hospital executive director by the 10th day of the following
month. The Monthly Tally must be attached to the Denial of
Rights form.
Quarterly reports of the number of persons, by facility,
whose rights were denied and the specific right or
rights denied must be submitted to the local mental
health director, who must report to DHCS [Welfare and
Institutions Code Section 5326.1, Title 9, California Code of
Regulations, Section 866].
DISCLOSURE OF DENIAL OF RIGHTS
Information in a patient’s medical record about denial of
rights must be available, upon request, to the patient,
patient’s attorney, conservator and/or guardian, the local
mental health director or a designee, or the patients’ rights
program (see chapter 9 regarding HIPAA and the disclosure
of mental health information). The information that must
be made available includes consent forms, the required
documentation for convulsive treatment, documentation
regarding the use of restraints and seclusion, physicians’
orders, nursing notes, and involuntary detention and
conservatorship papers.

CHA Mental Health Law Manual 2019
4.6
©CALIFORNIA HOSPITAL ASSOCIATION
State law calls for this information, except for the identity
of the patient whose rights are denied, to also be made
available upon request to a member of the California State
Legislature or a member of a county board of supervisors
[Welfare and Institutions Code Section 5326.1; Title 9,
California Code of Regulations, Section 867]. However,
legal counsel should be consulted prior to any release to
legislators or supervisors to be sure the facility complies
with HIPAA.
RESTORATION OF RIGHTS
A right may not be denied to a patient when good cause
for its denial no longer exists. Also, as noted above,
when a right has been denied, staff must employ the
least restrictive means of managing the problem that led
to the denial. The date a specific right is restored must
be documented in the patient’s medical record. [Title 9,
California Code of Regulations, Section 865.5]
III. SEXUAL ORIENTATION CHANGE THERAPY
FOR MINORS
California law states that “under no circumstances shall a
mental health provider engage in sexual orientation change
efforts with a patient under 18 years of age.”
“Sexual orientation change efforts,” also known as
reparative therapy or conversion therapy, means any
practices by mental health providers that seek to change
an individual’s sexual orientation. This includes efforts to
change behaviors or gender expressions, or to eliminate
or reduce sexual or romantic attractions or feelings toward
individuals of the same sex.
However, sexual orientation change efforts does not include
psychotherapies that:
1. Provide acceptance, support, and understanding
of clients or the facilitation of clients’ coping, social
support, and identity exploration and development,
including sexual orientation-neutral interventions to
prevent or address unlawful conduct or unsafe sexual
practices; and
2. Do not seek to change sexual orientation.
“Mental health provider” means:
1. A physician and surgeon specializing in the practice of
psychiatry;
2. A psychologist;
3. A psychological assistant, intern, or trainee;
4. A licensed marriage and family therapist, a registered
associate marriage and family therapist, or marriage
and family therapist trainee;
5. A licensed educational psychologist;
6. A credentialed school psychologist;
7. A licensed clinical social worker;
8. An associate clinical social worker;
9. A licensed professional clinical counselor, a registered
associate clinical counselor, or professional clinical
counselor trainee; or
10. Any other person designated as a mental health
professional under California law or regulation.
Any sexual orientation change efforts attempted on a
patient under 18 years of age by a mental health provider
are considered unprofessional conduct and subject the
provider to discipline by the licensing board.
[Business and Professions Code Sections 865-865.2]
IV. AFTERCARE PLAN
All psychiatric inpatient care providers must furnish each
mental health patient and specified other persons a
written aftercare plan upon the patient’s discharge from
the facility [Health and Safety Code Section 1262; Welfare
and Institutions Code Sections 5622 and 5768.5]. CHA
has developed the “Aftercare Plan” form (CHA Form 13-3)
which facilities may use to document compliance with
this law. Facilities are not required to use this particular
form; any form meeting the requirements described in this
section of the manual will work.
“Mental health patient,” for the purposes of this law,
means a person who is admitted to a facility primarily for
the diagnosis or treatment of a mental disorder.
A. Facilities Subject to This Law
The following facilities, both public and private, are subject
to this law:
1. State mental hospitals.
2. General acute care hospitals as defined in Health and
Safety Code Section 1250(a).
3. Acute psychiatric hospitals as defined in Health and
Safety Code Section 1250(b).
4. Psychiatric health facilities as defined in Health and
Safety Code Section 1250.2.

Chapter 4 — Rights of Mental Health Patients CHA
4.7
©CALIFORNIA HOSPITAL ASSOCIATION
5. Mental health rehabilitation centers as defined in
Welfare and Institutions Code Section 5675.
6. Skilled nursing facilities with a special treatment
program service unit for patients with chronic
psychiatric impairments (see Title 22, California Code
of Regulations, Sections 51335 and 72443-72475
about special treatment programs).
7. Facilities authorized under Welfare and Institutions
Code Section 5675 or 5768 (mental health
rehabilitation center pilot projects and other new
programs approved by the California Department of
Social Services (DSS)).
B. Contents of the Aftercare Plan
The aftercare plan must be written and must, to the extent
known, include the following components:
1. The nature of the illness and follow-up required.
2. Medications prescribed and their side effects and
dosage schedules. A signed informed consent form for
medications, when attached to the aftercare plan, may
satisfy this requirement if the consent form includes the
specified information.
3. The patient’s expected course of recovery.
4. Recommendations regarding treatment that are
relevant to the patient’s care.
5. Referral to providers of medical and mental
health services.
6. Other relevant information.
If any item above is not known at the time of discharge, this
should be noted on the aftercare plan.
The aftercare plan for a minor being released from
involuntary treatment must also include “education or
training needs, provided these are necessary for the minor’s
well-being” [Welfare and Institutions Code Section 5585.57].
CHA Form 13-3, “Aftercare Plan,” has space to document
compliance with this requirement.
C. Persons Who Must Be Given an Aftercare Plan
The law states that when a mental health patient is being
discharged from one of the facilities subject to the law, the
patient and the patient’s conservator, guardian, or other
legally authorized representative must be given a written
aftercare plan. As mentioned above, for purposes of this
law, a “mental health patient” is defined as a person
who is admitted to a facility primarily for the diagnosis or
treatment of a mental disorder. This law does not appear to
require that a mental health patient seen in the emergency
room, but never admitted, be given a written aftercare plan;
however, a hospital may wish to provide one.
The law is unclear about when a legally authorized
representative must be given an aftercare plan. In general,
a “legally authorized representative” exists only if the
patient lacks the capacity to make medical decisions for
himself or herself, in the opinion of the attending physician
or psychologist. In such a situation, the legally authorized
representative might be a guardian, conservator, or parent.
(See chapter 2 for a detailed discussion of capacity and
legally authorized representatives.)
In addition, facility personnel must advise the patient that
he or she may designate another person to receive a
copy of the aftercare plan. If the patient designates such
a person, the facility must give that person a copy of the
aftercare plan also.
V. MENTAL HEALTH ADVOCACY PROGRAMS
Advocacy programs, including the county patients’ rights
advocate program and the California Department of State
Hospitals (DSH), DHCS, and the California Department of
Social Services (DSS) advocacy program (contracted to
the statewide protection and advocacy agency), and the
Patients’ Rights Committee of the California Mental Health
Planning Council, are described in Welfare and Institutions
Code Sections 4900-4906 and 5500 et seq. (see also
42 U.S.C. Sections 10805 and 10806).
The county program pertains mainly to mental health
patients. The statewide program’s reach is much broader,
as described below.
State law specifies various circumstances under which a
health care facility must provide individually-identifiable
health information to patient advocates. This portion of the
manual describes the different types of patient advocacy
programs and when information must be disclosed to them.
A. Statewide Protection and Advocacy
Organization
The advocacy responsibilities of DHCS and DSH have been
transferred to a nongovernmental, nonprofit corporation
that acts as a statewide protection and advocacy agency.
The corporation that currently has the contract to act as
the statewide protection and advocacy agency is Disability
Rights California (DRC). [Welfare and Institutions Code
Section 5510]

CHA Mental Health Law Manual 2019
4.8
©CALIFORNIA HOSPITAL ASSOCIATION
This organization is responsible for ensuring that mental
health laws, regulations, and policies regarding the rights
of recipients of mental health services are observed in
state hospitals as well as health and community care
facilities [Welfare and Institutions Code Section 5510]. In
addition, this organization is responsible for ensuring that
laws related to abuse and neglect of disabled persons are
observed in state hospitals and health and community care
facilities.
DRC may also investigate any incident of abuse or neglect
of a disabled person if the incident is reported to DRC or if
DRC, determines there is probable cause to believe abuse
or neglect occurred. The definition of a “person with a
disability” is extremely broad and encompasses persons
with physical disabilities as well as persons with mental
illness and developmentally disabled persons. [Welfare and
Institutions Code Section 4902]
DRC’s authority includes reasonable access to a facility
or program, and authority to examine relevant records.
What is considered “reasonable” differs depending upon
the purpose of DRC’s visit. [Welfare and Institutions Code
Section 4902(b)] DRC may also interview any facility or
program service recipient, employee, or other person who
might have knowledge of the alleged abuse or neglect.
INVESTIGATIONS
DRC must be given reasonable unaccompanied access
to public or private facilities, programs, and services, and
to recipients of services therein, at all times necessary to
investigate incidents of abuse and neglect. Access must
be given to DRC, upon request, when any of the following
has occurred:
1. An incident is reported or a complaint is made to DRC.
2. DRC determines there is probable cause to believe that
an incident has or may have occurred.
3. DRC determines that there is or may be imminent
danger of serious abuse or neglect of an individual with
a disability.
“Reasonable unaccompanied access” means access that
permits DRC, without undue interference, to:
1. Monitor, inspect, and observe conditions in facilities
and programs, and
2. Meet and communicate with residents and service
recipients privately and confidentially on a regular basis,
formally or informally, by telephone, mail, email, and in
person.
Reasonable unaccompanied access also includes the
review of records privately and confidentially, in a manner
that minimizes interference with the activities of the
program or service; that respects patients’ privacy interests
and honors a patient’s request to terminate an interview;
and that does not jeopardize the physical health or safety
of facility or program staff, patients, service recipients, or
DRC staff.
NONINVESTIGATIVE PURPOSES
DRC must be given reasonable unaccompanied access
to public or private facilities, programs and services, and
to recipients of services therein, during normal working
hours and visiting hours for other advocacy services (that is,
noninvestigative purposes).
Access must be provided at times mutually agreeable to
DRC and facility management for the following:
1. Providing information and training on (and referral to
programs addressing the needs of) individuals with
disabilities, and information and training on individual
rights and the protection and advocacy services
available from DRC, including, but not limited to, the
name, address, and telephone number of DRC.
2. Monitoring compliance with respect to the rights and
safety of patients or service recipients.
3. Inspecting, viewing, and photographing all areas of the
facility or program that are used by patients or service
recipients, or that are accessible to them.
DELAY OR DENIAL OF ACCESS
If DRC’s access to facilities, programs, service recipients,
patients, or records is wrongfully delayed or denied, the
facility must promptly provide DRC with a written statement
of reasons. If denial of access results from an alleged lack
of patient authorization, the facility must promptly provide
DRC with the name, address, and telephone number of
the patient’s legal guardian, conservator, or other legal
representative. Access to a facility, program, service
recipient, patient, or records may not be delayed or denied
without the prompt provision of a written statement of
the reasons for the denial. [Welfare and Institutions Code
Section 4902(c)]
COPYING COSTS
A health care provider may charge a reasonable fee to
cover the cost of copying records. This fee may take into
account the costs incurred in locating, identifying, and
making the records available. Charges for copying records

Chapter 4 — Rights of Mental Health Patients CHA
4.9
©CALIFORNIA HOSPITAL ASSOCIATION
that would be available to DRC or the patient under other
laws may not exceed any rates for obtaining copies of the
records specified in the other laws. [Welfare and Institutions
Code Section 4902(e)] (See CHA’s California Health
Information Privacy Manual regarding records that must be
made available to the patient and the photocopying rates
that may be charged.)
ACCESS TO RECORDS OF SPECIFIED PERSONS
DRC must be given access to the records of the following
people with disabilities:
1. A person with a disability alleged to be a victim of
abuse or neglect if the incident is reported to DRC or
DRC determines there is probable cause to believe the
incident occurred.
2. A person who is a client of DRC or who has requested
assistance from DRC, if that person, his or her
agent, legal guardian, conservator, or other legal
representative, has authorized DRC to have access to
the records. If a person with a disability who is able to
authorize DRC to access his or her records expressly
denies this access after being informed by DRC of his
or her right to authorize or deny access, DRC may not
have access to the records [Welfare and Institutions
Code Section 4903(a)(1)].
3. A person, including an individual who cannot be
located, to whom all of the following conditions apply:
a. The individual, due to his or her mental or physical
condition, is unable to authorize DRC to have
access to his or her records.
b. The individual does not have a legal guardian,
conservator, or other legal representative,
or the individual’s representative is a
public entity, including the state or one of
its political subdivisions.
c. DRC has received a complaint that the individual
has been subject to abuse or neglect, or has
determined that probable cause exists to believe
that the individual has been subject to abuse
or neglect.
[Welfare and Institutions Code Section 4903(a)(2)]
4. A person who is deceased, and for whom DRC has
received a complaint that the individual had been
subjected to abuse or neglect, or for whom DRC has
determined that probable cause exists to believe that
the individual had been subjected to abuse or neglect
[Welfare and Institutions Code Section 4903(a)(3)].
5. A person who has a legal guardian, conservator, or
other legal representative with respect to whom a
complaint has been received by DRC, or with respect
to whom DRC has determined that probable cause
exists to believe that the person has been subjected
to abuse or neglect, whenever all of the following
conditions exist:
a. The representative has been contacted by
DRC upon receipt of the representative’s name
and address.
b. DRC has offered assistance to the representative
to resolve the situation.
c. The representative has failed or refused to act on
behalf of the person.
[Welfare and Institutions Code Section 4903(a)(4)]
(See also Welfare and Institutions Code Section 5328.06.)
TYPES OF RECORDS AVAILABLE TO DRC
All of the following individual records must be made
available to DRC.
1. Information and records prepared or received in the
course of providing intake, assessment, evaluation,
education, training, or other supportive services,
including, but not limited to, medical records, financial
records, monitoring reports, or other reports, prepared
or received by a member of the staff of a facility,
program, or service that is providing care, treatment,
or services.
2. Reports prepared by an agency charged with
investigating reports of incidents of abuse, neglect,
injury, or death occurring at the program, facility, or
service while the individual with a disability is under the
care of a member of the staff of a program, facility, or
service, or by or for a program, facility, or service, that
describe any or all of the following:
a. Abuse, neglect, injury, or death.
b. The steps taken to investigate the incidents.
c. Reports and records, including, but not limited
to, personnel records prepared or maintained by
the facility in connection with reports of incidents,
subject to the following:
▪ If a state statute specifies procedures with
respect to personnel records, DRC must follow
those procedures.

CHA Mental Health Law Manual 2019
4.10
©CALIFORNIA HOSPITAL ASSOCIATION
▪ Personnel records are protected from disclosure
in compliance with the state constitutional right
of privacy. The custodian of personnel records
has a right and a duty to resist attempts to
allow the unauthorized disclosure of personnel
records, and may not waive the privacy rights
that are guaranteed pursuant to the state
constitutional right to privacy.
▪ Supporting information that was relied upon
in creating a report including, but not limited
to, all information and records that document
interviews with persons who were interviewed,
physical and documentary evidence that was
reviewed, or related investigative findings.
d. Discharge planning records.
[Welfare and Institutions Code Section 4903(b) and (c)]
This information must be provided, whether written
or in another medium, and whether draft or final. This
information may include, but is not limited to, handwritten
notes, electronic files, photographs, videotapes, audiotapes
or records.
Information About Abuse or Neglect Investigations
A facility must make the following available to DRC when
investigating instances of abuse or neglect:
1. Information in reports prepared by individuals and
entities performing certification or licensure reviews,
or by professional accreditation organizations, as
well as related assessments prepared for a program,
facility, or service by its staff, contractors, or related
entities. However, information subject to any other
provision of state law protecting records produced by
medical care evaluation or peer review committees
need not be disclosed. (See “Limitations on DRC
Access,”page4.10.)
2. Information in professional, performance, building, or
other safety standards, or demographic and statistical
information, relating to the facility.
[Welfare and Institutions Code Section 4903(c)]
This information must be provided, whether written
or in another medium, and whether draft or final. This
information may include, but is not limited to, handwritten
notes, electronic files, photographs, videotapes, audiotapes
or records.
Documents Prepared by State Agencies
DRC must be given access to the following documents:
1. Unredacted facility evaluation or complaint
investigation report forms of the California Department
of Social Services.
2. Unredacted citation, licensing or survey reports,
plans of correction, or statements of deficiency of
the California Department of Public Health, prepared
by authorized licensing personnel or authorized
representatives of those departments who are licensed
or registered health personnel.
[Welfare and Institutions Code Sections 4903(h) and
5328.15(a)]
It should be noted that plans of correction are not
prepared by authorized licensing personnel or authorized
representatives of the state (see also Welfare and
Institutions Code Section 5328.15(c)).
Psychotherapy Notes
Psychotherapy notes may be disclosed to DRC
without a patient authorization to the extent required
by law. If information is disclosed to DRC pursuant to
an authorization from the patient or the patient’s legal
representative, a separate authorization form is required for
the disclosure of the psychotherapy notes.
LIMITATIONS ON DRC ACCESS
Under state law, DRC has no right to access records
protected from discovery as specified in Evidence Code
Sections 1157 and 1157.6, or records protected from
disclosure by the physician-patient privilege or the
psychotherapist-patient privilege [Welfare and Institutions
Code Section 4903(d)]. However, federal judicial decisions
have created some doubt about this legal issue. Legal
counsel should be consulted if such records are requested.
DRC has no right to access records that qualify as “patient
safety work product” as defined in the Patient Safety and
Quality Improvement Act of 2005.
TIMELINES FOR COMPLIANCE
DRC must be given access to medical records and other
records that are relevant to conducting an investigation
not later than three business days after DRC makes a
written request.
However, if DRC determines there is probable cause
to believe that the health or safety of the individual is in
serious and immediate jeopardy, or in a case of death of an
individual with a disability, DRC must be given immediate

Chapter 4 — Rights of Mental Health Patients CHA
4.11
©CALIFORNIA HOSPITAL ASSOCIATION
access to the records, not later than 24 hours after DRC
makes a request. No consent from another party is
required. [Welfare and Institutions Code Section 4903(e)]
PROHIBITIONS ON REDISCLOSURE OF INFORMATION
BY DRC
Confidential information kept or obtained by DRC remains
confidential and may not be subject to disclosure by DRC.
However, DRC may do the following:
1. Share the information with the individual client who is
the subject of the record, report or other document, or
with his or her legally authorized representative, subject
to any limitation on disclosure to recipients of mental
health services under federal law [42 U.S.C. Section
10806]. Federal law contains a provision authorizing
the mental health professional responsible for the
patient to provide to the advocacy agency a written
determination that disclosure of the information to the
patient would be detrimental to the patient’s health.
The advocacy agency may obtain a second opinion
and rely on it instead. [42 U.S.C. Section 10806]
2. Issue a public report of the results of an investigation
that maintains the confidentiality of individual
service recipients.
3. Report the results of an investigation to responsible
investigative or enforcement agencies if an
investigation reveals information about the facility, its
staff, or employees warranting possible sanctions or
corrective action. This information may be reported
to agencies that are responsible for facility licensing
or accreditation, employee discipline, employee
licensing or certification suspension or revocation, or
criminal prosecution.
4. Pursue alternative remedies, including the initiation of
legal action.
5. Report suspected elder or dependent adult abuse.
[Welfare and Institutions Code Section 4903(f)]
B. County Patients’ Rights Advocates
In general, the law states that each county behavioral
health director must appoint, or contract for the services of,
a county patients’ rights advocate to undertake the duties
described below.
For the purposes of the following discussion, the term
“advocate” refers to a “county patients’ rights advocate.”
The provisions regarding the county patients’ rights
advocate program apply to licensed health and community
care facilities and may apply to state hospitals.
DUTIES OF COUNTY PATIENTS’ RIGHTS ADVOCATES
The advocates’ duties include, but are not limited to,
the following:
1. To receive and investigate complaints from or about
recipients of mental health services who reside in
licensed health or community care facilities involving
abuse, unreasonable denial or punitive withholding of
the rights guaranteed by Welfare and Institutions Code
Section 5000 et seq. (including the Lanterman-Petris-
Short Act and the Short-Doyle Act).
2. To monitor mental health facilities, services, and
programs for compliance with patients’ rights laws.
3. To train and educate mental health providers about
mental health law and patients’ rights.
4. To assure that recipients of mental health services
in licensed health and community care facilities are
notified of their rights.
5. To exchange information and cooperate with the
patients’ rights program.
[Welfare and Institutions Code Section 5520]
AUTHORITY OF COUNTY PATIENTS’ RIGHTS
ADVOCATE
An advocate’s rights of access to a patient or records differ
depending upon whether the advocate is acting on behalf
of a client or pursuant to the advocate’s duties to monitor
patients’ rights compliance or to conduct an investigation
(see “Access to Persons and Facilities,”page4.12,
and “Access to Records and Information,”page4.13).
This portion of the manual describes the advocate’s
access rights.
AGREEMENT FOR ADVOCACY SERVICES FOR CLIENT
An advocate may enter into an agreement with a client
to provide advocacy services, which include “activities
undertaken on behalf of persons who are receiving or have
received mental health services to protect their rights or
to secure or upgrade treatment or other services to which
they are entitled” [Welfare and Institutions Code Section
5500(a)].
“Mental health client” or “client” is defined as:
a person who is receiving or has received services from
a mental health facility, service, or program and who has

CHA Mental Health Law Manual 2019
4.12
©CALIFORNIA HOSPITAL ASSOCIATION
personally or through a guardian ad litem, entered into
an agreement with a county patients’ rights advocate for
the provision of advocacy services.
[Welfare and Institutions Code Section 5500(b)]
Agreement Requirements
Generally, the client must be competent to enter into a
binding agreement. The law states that a recipient of
mental health services is presumed competent for the
purpose of entering into an agreement with an advocate
for advocacy services unless the recipient is found by
a superior court to be incompetent to enter into an
agreement with an advocate and a guardian ad litem is
appointed for this purpose [Welfare and Institutions Code
Section 5523(a)]. This is true even if the patient has had a
guardian or conservator appointed.
The mental health client or guardian ad litem must
knowingly and voluntarily enter into the agreement with the
advocate [Welfare and Institutions Code Section 5523(c)].
The agreement must be in a language and modality that the
client understands [Welfare and Institutions Code Section
5523(c)].
The agreement may be revoked at any time by the person
who entered into the agreement (i.e., the client or the
guardian ad litem), either in writing or by an oral declaration
to the advocate [Welfare and Institutions Code Section
5523(c)].
The law does not expressly require the advocate to
inform the mental health facility or professional when an
agreement for advocacy services is either reached or
revoked. However, it is important for health providers to
know whether such an agreement has been entered into
or revoked, as it affects the advocate’s rights of access
to the patient and the patient’s records, and in effect
authorizes the advocate to interview all persons who care
for the patient.
INVESTIGATION BASED UPON PROBABLE CAUSE
An advocate may conduct an investigation if there is
probable cause to believe that the rights of a past or
present recipient of mental health services have been or
may be violated [Welfare and Institutions Code Section
5522].
Investigations that concern violations of a past recipient’s
rights are limited to cases that involve discrimination,
indicate the need for education or training, or have a direct
bearing on violations of the rights of a current recipient
[Welfare and Institutions Code Section 5523(f)]. Any such
investigation of a past patient’s rights are in addition to
routine monitoring functions of the advocate.
Welfare and Institutions Code Section 5326.1 requires that
a county-designated facility file quarterly reports with the
director of DHCS showing the number of patients whose
rights were denied and the right(s) which were denied. An
advocate may access, without patient authorization, the
treatment records of patients reported under Section
5326.1 if those records are pertinent to the investigation
concerning the denial of rights [Welfare and Institutions
Code Section 5328(a)(13)]. This provision does not permit
the advocate to see records of other patients. The records
may be inspected by the advocate even after the patient’s
discharge from the facility. [62 Ops.Cal.Atty.Gen.57, 59
(1979)]
ACCESS TO PERSONS AND FACILITIES
An advocate may distribute educational materials and hold
discussions in groups and with individual patients in order
to notify patients and others of the availability of advocacy
services and to give information about patient rights.
When the advocate seeks access in order to investigate
or resolve a specific complaint or to monitor compliance
with patients’ rights laws, the advocate must be permitted
access to all recipients of mental health services in any
mental health facility, program, or service at all times as
necessary.
For other advocacy purposes, the advocate must be
permitted access to mental health facilities, programs,
services, and recipients of services, but only during usual
working hours and visiting hours [Welfare and Institutions
Code Section 5530(a)].
Upon request, the mental health facility must provide, when
available, reasonable space for the county advocate to
interview clients in privacy [Welfare and Institutions Code
Section 5530(c)]. It is generally advisable to provide space
when an advocate requests privacy to interview patients
who are not clients, as well.
LIMITATIONS ON ACCESS TO PATIENTS
Patients Who Have Not Requested Advocacy Services
The law imposes certain requirements on an advocate
investigating a case involving a recipient of mental
health services who is not a client. In such a case, the
advocate must:
1. Notify the treating professional who is responsible for
the care of a recipient of services whom the advocate
wishes to interview;
2. Notify the facility, service, or program administrator of
the intention to conduct the interview; and

Chapter 4 — Rights of Mental Health Patients CHA
4.13
©CALIFORNIA HOSPITAL ASSOCIATION
3. Consult the treating professional whenever he or she is
reasonably available for consultation to determine the
appropriate time to conduct the interview.
[Welfare and Institutions Code Section 5523(b)]
Patient’s Right to Refuse Access
Each patient has a right to privacy which includes the right
to terminate a visit by an advocate, and the right to refuse
to see a patient advocate [Welfare and Institutions Code
Section 5530(d)].
Persons Rendering Services to the Advocate’s Client
An advocate has the right to interview all persons who
provide diagnostic or treatment services to the advocate’s
client [Welfare and Institutions Code Section 5530(b)].
ACCESS TO RECORDS AND INFORMATION
Under LPS, information must be disclosed to county
patients’ rights advocates when the patient or guardian
ad litem has knowingly and voluntarily authorized the
disclosure [Welfare and Institutions Code Section
5328(a)(13); 45 C.F.R. Section 164.512(a)(1)]. In addition,
the records must be disclosed when an advocate is
investigating the denial of a patient’s right(s). The details of
these LPS provisions are described below.
HIPAA also allows these disclosures. Under HIPAA, a
covered entity may use or disclose PHI with a valid
authorization, or to the extent that the use or disclosure
is required by law [45 C.F.R. Section 164.502(g)(2)]. A
separate authorization is required for psychotherapy notes
if access is pursuant to an authorization; psychotherapy
notes may be disclosed to the extent required by law if
access is pursuant to a valid investigation of a denial of a
patient’s right(s).
Confidential Client Information and Records
The advocate must obtain authorization from the client
to have access to, copy, or use confidential records
and information about the client. The law imposes the
following requirements:
1. The client or guardian ad litem must specifically
authorize the advocate to have access to, copy, or
otherwise use confidential records or information about
the client.
2. The authorization must be given knowingly and
voluntarily and must be in writing.
3. The client or guardian ad litem who has entered
into the advocate client agreement may revoke the
authorization at any time, either in writing or by oral
declaration to the advocate [Welfare and Institutions
Code Section 5541(a)].
4. Before confidential patient information is released to
an advocate, the mental health facility should obtain
a copy of the written authorization and place it in the
patient’s medical record.
If the client provides authorization, an advocate may
discuss information contained in the client’s records with
the client to the extent necessary for effective advocacy.
However, information provided in confidence by members
of a client’s family may be removed from the record before
it is given to the advocate. It is recommended that the
patient’s physician determine whether such information
should be removed. [Welfare and Institutions Code Section
5543(a)]
Any written client information obtained by a county patients’
rights advocate may be used and disseminated in court or
administrative proceedings, and to public agencies or their
authorized officials. However, the information may be used
or disseminated only to the extent required in the provision
of advocacy services and to the extent authorized by the
client [Welfare and Institutions Code Section 5544].
Patient Records in Investigation
An advocate may access, without patient authorization,
the treatment records of patients reported under Section
5326.1 (a patient whose rights have been denied) if those
records are pertinent to the investigation about the denial of
rights. This provision does not permit the advocate to see
records of other patients. The records may be inspected
by the advocate even after the patient’s discharge from
the facility. [Welfare and Institutions Code Section 5326.1;
62 Ops.Cal.Atty.Gen.57, 59 (1979)]
Records of Mental Health Facilities and Programs
An advocate has the right to inspect and/or copy records or
other materials not subject to confidentiality under Welfare
and Institutions Code Section 5328, HIPAA, or other
provisions of law. This right applies to records possessed
by a mental health program, service, or facility; or city,
county, or state agency that relate to an investigation on
behalf of a client or that indicate compliance or lack of
compliance with laws governing patients’ rights. These
records include, but are not limited to, reports on the use
of restraints or seclusion, and autopsy reports [Welfare and
Institutions Code Section 5542]. However, these reports
must not be patient-identifiable or they are subject to
confidentiality laws.

CHA Mental Health Law Manual 2019
4.14
©CALIFORNIA HOSPITAL ASSOCIATION
2003 Memo from Protection & Advocacy, Inc.
In August, 2003, a lawyer working for Protection &
Advocacy, Inc. distributed a memo to county patients’
rights advocates about the advocates’ authority to access
patient health information. The overall point of the memo
was to reassure interested parties in 2003 that the (then)
brand-new HIPAA law did not change advocates’ authority
under state law to access patient records. This conclusion
is correct.
However, the memo did not correctly interpret the
advocates’ authority under state law to access patient
records.
The gist of the memo is on the bottom of page 6 of the
memo. It correctly states that:
1. County patients’ rights advocates may have access to
the facility at all times necessary to investigate specific
complaints.
2. County patients’ rights advocates may interview staff.
3. County patients’ rights advocates may access
records if:
a. They have client authorization;
b. The records aren’t confidential (which would not
include patient medical records) and they relate
to an investigation on behalf of a client, or they
indicate compliance/noncompliance with patients’
rights laws; or
c. The record relates to a denial of patients’ rights
that the facility reported to the local behavioral
health director.
County patients’ rights advocates are not entitled to
review any medical records they want. The California
Legislature has evidenced its intent to protect the privacy
of patient records — it has shown this by its wording of
various statutes:
Welfare and Institutions Code Section 5328(a)(13)) states
that, “[Disclosure may be made] To county patients’
rights advocates who have been given knowing voluntary
authorization by a client or a guardian ad litem. The client
or guardian ad litem, whoever entered into the agreement,
may revoke the authorization at any time, either in writing
or by oral declaration to an approved advocate.” If the
California Legislature wanted county patients’ rights
advocates to have access to all patients’ records, it could
easily have said so. It did not.
Welfare and Institutions Code Section states that,
“Individual patients shall have a right to privacy which shall
include the right to terminate any visit by [patients’ rights
advocates] and the right to refuse to see any patient
advocate.”
Welfare and Institutions Code Section 5540 states
that, “Except as otherwise provided in this chapter or in
other provisions of law, information about and records of
recipients of mental health services shall be confidential in
accordance with the provisions of Section 5328.”
Welfare and Institutions Code Section 5541 states that a
specific client authorization is required for a county patients’
rights advocate to have access to confidential records of
the client.
Welfare and Institutions Code Section 5542 states that
county patients’ rights advocates have the right to inspect
any nonconfidential information.
Welfare and Institutions Code Section 5545 states that,
“Nothing in this chapter [Chapter 6.2] shall be construed to
limit access to recipients of mental health services in any
mental health facility, program, or service or to information
or records of recipients of mental health services for the
purposes of subdivision (b) of Section 5520 or when
otherwise authorized by law to county patients’ rights
advocates or other individuals who are not county patients’
rights advocates.” This law does not expand any entities’
authority to access patient records. It merely states that it
does not limit other authority. Note that the main patient
privacy protection statute, Welfare and Institutions Code
Section 5328, is in chapter 2. That is the primary statute
limiting patients’ rights advocates’ authority to access
records of mental health patients who are not their clients
and who have not been the subject of a rights denied by
the facility.
The portion of the memo that relates to the facility
directory is a correct statement of the Confidentiality of
Medical Information Act, but that Act does not apply to
patients in an acute psychiatric hospital or the psychiatric
unit of a general acute care hospital. Instead, the
Lanterman-Petris-Short Act applies. No information may be
disclosed about these patients.
Costs Charged to the Advocate
Costs of copying or making records available must
be borne by the advocate [Welfare and Institutions
Code Section 5546]. Charges may include:
1. Actual costs of copying the records or other
material; and
2. Additional reasonable clerical costs incurred in locating
and making the records and materials available. These
costs must be based on a computation of the time

Chapter 4 — Rights of Mental Health Patients CHA
4.15
©CALIFORNIA HOSPITAL ASSOCIATION
spent locating and making the records available
multiplied by the employee’s hourly wage.
The law does not address when payment must be made. It
is recommended that payment be received before copies
are released.
C. Retaliation and Discrimination Prohibited
It is illegal to discriminate or retaliate in any manner against
a patient or employee for initiating or participating in an
advocacy proceeding. If a facility attempts to expel a
patient or engages in any discriminatory treatment of a
patient who submits a complaint to a county patients’
rights advocate (or upon whose behalf a complaint is
submitted) within 120 days of the filing of the complaint,
then a rebuttable presumption is raised that the facility
took the action in retaliation for the filing of the complaint.
[Welfare and Institutions Code Section 5550(c)]
D. Penalties
A person or facility is subject to a civil fine of between
$100 and $1,000, as determined by a court for knowingly
obstructing an advocate in the performance of his or her
duties as authorized by law including, but not limited to,
interference with access to:
1. Clients or potential clients;
2. Records of clients or potential clients, whether financial,
medical, or otherwise;
3. Other information, materials, or records; or
4. Anything which otherwise violates the statutory
provisions regarding the county patients’
rights advocates.
[Welfare and Institutions Code Section 5550(b) and (e)]
In addition, a person aggrieved by a violation of the statute
may pursue any other available legal remedies [Welfare and
Institutions Code Section 5523(e)].
E. Immunity From Liability
A person who files a complaint, provides information to an
advocate pursuant to the law or participates in a judicial
proceeding resulting therefrom is presumed to be acting
in good faith and, unless the presumption is rebutted,
is immune from civil, criminal or administrative penalty
[Welfare and Institutions Code Section 5550(a)].
VI. PSYCHIATRIC ADVANCE DIRECTIVES
A psychiatric advance directive is an instrument that mental
health patients may use to document their preferences
regarding future mental health treatment, in preparation for
the possibility of losing capacity to give or withhold consent
to treatment in the future. The mental health advocacy
community advocates the use of such documents,
particularly with respect to involuntary treatment,
psychiatric medications, restraint and seclusion.
Neither California nor federal law recognizes a special
document called a “psychiatric advance directive.” The
California advance health care directive laws and statutory
form were created with end-of-life issues in mind, not
mental health matters. However, the law does not prohibit a
person who executes an advance health care directive from
including instructions regarding mental health treatment.
Whether such wishes are required to be followed by a
health care provider if the patient loses capacity depends
upon several factors, including:
1. Whether the patient would have the legal ability to
consent or withhold consent to the recommended
treatment if he or she were competent. For example,
a patient who is detained pursuant to Welfare
and Institutions Code Section 5150 et seq. is, by
law, unable to withhold consent to be evaluated
for a mental disorder and may not leave the facility.
Therefore, if such a patient has executed an advance
directive denying consent to such care, a hospital need
not comply with this instruction.
2. Whether the wishes stated in the advance directive are
medically ineffective or contrary to generally accepted
health standards. In such a case, the facility need
not comply with the patient’s instructions. However, a
provider that declines to comply must follow certain
procedures (see Probate Code Sections 4735 and
4736).
There are no statutes, regulations, or judicial decisions
regarding “psychiatric” advance directives in California.
However, California law does contain one reference to
advance directives in the context of mental health care.
Health and Safety Code Section 1180.4(a) requires
psychiatric units of general acute care hospitals, acute
psychiatric hospitals, skilled nursing facilities, and other
specified facilities to conduct an assessment of each
patient prior to a placement decision or upon admission,
or as soon thereafter as possible. This assessment must
include, based on the information available at the time,
the patient’s advance directive regarding de-escalation or
the use of seclusion or behavioral restraints. This statute
does not authorize “psychiatric advance directives,” nor

CHA Mental Health Law Manual 2019
4.16
©CALIFORNIA HOSPITAL ASSOCIATION
does it require a provider to comply with a patient’s stated
preferences. It merely requires the specified providers to
assess a patient’s advance directive, if any. (See chapter 5
regarding restraint and seclusion.)
A hospital should consult legal counsel if a situation arises
regarding a psychiatric advance directive. (See chapter 3
of CHA’s Consent Manual for a complete discussion of the
law regarding advance directives.)
VII. SEXUAL ACTIVITY BETWEEN PATIENT AND
PROVIDER
A. Sexual Activity Between Involuntarily Confined
Patient and Hospital Employee is a Crime
Penal Code Section 289.6 prohibits an employee, officer or
agent of a health facility that contracts with a public entity
(including the state or federal government) from engaging
in sexual activity with an adult who has been involuntarily
confined, even if that adult purportedly “consents” to the
sexual activity. Health facilities included in this law are:
1. An acute psychiatric hospital as defined in Health and
Safety Code Section 1250(b).
2. An intermediate care facility/developmentally disabled
habilitative as defined in Health and Safety Code
Section 1250(e).
3. An intermediate care facility/developmentally disabled
as defined in Health and Safety Code Section 1250(g).
4. An intermediate care facility/developmentally disabled
— nursing as defined in Health and Safety Code
Section 1250(h).
5. A congregate living health facility — persons who are
catastrophically and severely disabled –– as defined in
Health and Safety Code Section 1250(i)(2)(C).
6. A correctional treatment center as defined in Health
and Safety Code Section 1250(j).
“Sexual activity” means sexual intercourse, sodomy, oral
copulation, or penetration, however slight, of the genital
or anal openings of another person by a foreign object,
substance, instrument, or device, for the purpose of sexual
arousal, gratification, or abuse.
The first violation of this law constitutes a misdemeanor. A
subsequent violation constitutes a felony.
B. Unprofessional Conduct
The commission of any act of sexual relations, abuse,
or misconduct with a patient or client constitutes
unprofessional conduct and grounds for disciplinary
action for any person licensed under the healing arts
licensure provisions of the Business and Professions
Code. This includes doctors, nurses, pharmacists, dentists,
psychologists, physical therapists, dietitians, clinical
laboratory technologists, speech-language pathologists,
etc. This activity may also be a crime, punishable by a fine
or imprisonment or both.
This law does not apply to consensual sexual contact
between a licensee and his or her spouse (or other person
in an equivalent domestic relationship) when the licensee
provides medical treatment other than psychotherapeutic
treatment to the spouse or other person. [Business and
Professions Code Sections 726 and 729]
C. Patient Alleges Prior Psychotherapist Sexual
Activity
If a psychotherapist or employer of a psychotherapist
becomes aware through a client that the client has alleged
sexual intercourse, sexual behavior or sexual contact
with a previous psychotherapist during the course of a
prior treatment, the psychotherapist or employer must
give the client a brochure about the patient’s rights
and remedies [Business and Professions Code Section
728]. The California Department of Consumer Affairs has
published a booklet, “Professional Therapy Never Includes
Sex,” for psychotherapists to use to fulfill this requirement.
The booklet is available in English and Spanish at www.
mbc.ca.gov/publications. To purchase copies in quantity,
contact the Office of State Printing at (916) 445-5357.
In addition, the psychotherapist or employer must discuss
the brochure with the client.
For purposes of this law, the following definitions apply.
“Psychotherapist” means:
1. A physician specializing in the practice of psychiatry or
practicing psychotherapy,
2. A psychologist, psychological assistant, or trainee
under the supervision of a psychologist,
3. A marriage and family therapist, associate marriage
and family therapist, or marriage and family
therapist trainee,
4. A clinical social worker or associate clinical
social worker,

Chapter 4 — Rights of Mental Health Patients CHA
4.17
©CALIFORNIA HOSPITAL ASSOCIATION
5. A licensed professional clinical counselor, associate
professional clinical counselor, or clinical counselor
trainee (as specified in Business and Professions Code
Section 4999.10 et seq.).
“Sexual behavior” means inappropriate contact or
communication of a sexual nature, but does not include
providing appropriate therapeutic interventions relating to
sexual issues.
“Sexual contact” means the touching of an intimate part of
another person.
Section 728 states that “intimate part” and “touching”
have the same meanings as those terms are defined in
subdivisions (g) and (e), respectively, of Section 243.4 of
the Penal Code:
1. “Intimate part” means the sexual organ, anus, groin,
or buttocks of any person, and the breast of a female
[Penal Code Section 243.4(g)(1)].
2. Despite what Section 728 says, “touching” is not
defined in Penal Code Section 243.4. However,
“touches” is defined to mean physical contact with
another person, whether accomplished directly,
through the clothing of the person committing the
offense, or through the clothing of the victim [Penal
Code Section 243.4(e)(2)].
“The course of a prior treatment” means the period of
time during which a client first commences treatment
for services that a psychotherapist is authorized to
provide under his or her scope of practice, or that the
psychotherapist represents to the client as being within his
or her scope of practice, until the psychotherapist-client
relationship is terminated.

Chapter 5 — Contents
©CALIFORNIA HOSPITAL ASSOCIATION
5 Restraints and Seclusion
I. INTRODUCTION ....................................... 5.1
A. Scope of Chapter...........................................5.1
B. Restraint and Seclusion Laws ......................5.1
Federal Law ......................................................5.1
California Law
................................................... 5.2
Must Comply With All Laws
...............................5.2
C. Accreditation Organization Standards ........5.2
II. PATIENTS’ RIGHTS REGARDING
RESTRAINT AND SECLUSION
................... 5.2
A. Federal Law: CMS Conditions of
Participation and Interpretive Guidelines
....5.2
Survey Procedures ...........................................5.3
B. California Law ................................................5.3
III. GENERAL INFORMATION REGARDING
RESTRAINT AND SECLUSION ................... 5.4
A. Quick Summary of Restraint and
Seclusion Laws
..............................................5.4
B. Techniques .....................................................5.4
Survey Procedures ...........................................5.4
C. Restraints are Medical Devices
Regulated by the FDA
...................................5.4
IV. DEFINITIONS ........................................... 5.4
A. Federal Law: CMS Conditions of
Participation and Interpretive Guidelines
....5.5
Restraint ........................................................... 5.5
Seclusion
..........................................................5.7
Survey Procedures
...........................................5.8
B. California Law ................................................5.8
V. INTAKE ASSESSMENT/CARE PLAN ........... 5.8
A. Federal Law: CMS Conditions of
Participation and Interpretive Guidelines
....5.9
Survey Procedures ...........................................5.9
B. California Law ................................................5.9
Psychiatric Advance Directives ........................ 5.10
VI. LEAST RESTRICTIVE ALTERNATIVE ........ 5.10
A. Federal Law: CMS Conditions of
Participation and Interpretive Guidelines
..5.10
Survey Procedures .........................................5.11
B. California Law ..............................................5.11
VII. ORDER FOR RESTRAINT OR
SECLUSION
........................................... 5.12
A. Federal Law: CMS Conditions of
Participation and Interpretive Guidelines
..5.12
PRN Orders .................................................... 5.12
Who May Order Restraint or Seclusion
............ 5.12
When Order Must Be Obtained
.......................5.12
Protocol, Standing Orders, and PRN Orders
...5.13
Survey Procedures
.........................................5.13
B. California Law ..............................................5.14
VIII. FACE-TO-FACE EVALUATION ................ 5.14
A. Federal Law: CMS Conditions of
Participation and Interpretive Guidelines
..5.14
Exception .......................................................5.15
Content of the Evaluation
................................ 5.15
Consultation With Attending Physician or
Other LIP
........................................................ 5.15
Survey Procedures
.........................................5.16
B. California Law ..............................................5.16
IX. NOTIFICATION OF ATTENDING
PHYSICIAN
............................................ 5.16
A. Federal Law: CMS Conditions of
Participation and Interpretive Guidelines
..5.16
Survey Procedures .........................................5.16
B. California Law ..............................................5.17
X. LIMITS ON LENGTH OF TIME THAT
ORDERS FOR RESTRAINT/SECLUSION
ARE VALID
............................................ 5.17
A. Federal Law: CMS Conditions of
Participation and Interpretive Guidelines
..5.17
Original Order .................................................5.17
Renewal of Order
............................................5.17

Chapter 5 — Contents
©CALIFORNIA HOSPITAL ASSOCIATION
CHA Mental Health Law Manual 2019
Renewal of Order 24 Hours After Original
Order
..............................................................5.17
Exceptions
......................................................5.17
Survey Procedures
.........................................5.18
B. California Law ..............................................5.18
XI. DISCONTINUATION OF RESTRAINT OR
SECLUSION ........................................... 5.18
A. Federal Law: CMS Conditions of
Participation and Interpretive Guidelines
..5.18
Survey Procedures .........................................5.18
B. California Law ..............................................5.19
XII. PATIENT MONITORING ........................... 5.19
A. Federal Law: CMS Conditions of
Participation and Interpretive Guidelines
..5.19
Survey Procedures ..........................................5.19
B. California Law ..............................................5.20
XIII. EMERGENCY SITUATIONS .................... 5.20
A. Federal Law: CMS Conditions of
Participation and Interpretive Guidelines
..5.20
B. California Law ..............................................5.20
XIV. SIMULTANEOUS RESTRAINT AND
SECLUSION
.......................................... 5.20
A. Federal Law: CMS Conditions of
Participation and Interpretive Guidelines
..5.20
Documentation ...............................................5.21
Patient Monitoring and Assessment
................5.21
Survey Procedures
.........................................5.21
B. California Law ..............................................5.21
Face-to-Face Observation...............................5.21
XV. PROHIBITED TECHNIQUES ..................... 5.21
A. Federal Law: CMS Conditions of
Participation and Interpretive Guidelines
..5.21
B. California Law ..............................................5.21
Techniques That are Prohibited for All
Patients
.........................................................5.22
Techniques That are Prohibited for Specified
Patients
.........................................................5.22
Prone Containment Techniques
.......................5.22
Applicability
....................................................5.22
XVI. POST-RESTRAINT OR SECLUSION
REVIEW (CLINICAL/QUALITY REVIEW
AND DEBRIEFING)
............................... 5.22
A. Federal Law: CMS Conditions of
Participation and Interpretive Guidelines
..5.22
B. California Law ..............................................5.23
Clinical and Quality Review..............................5.23
Debriefing
....................................................... 5.23
XVII. REPORTING REQUIREMENTS
RELATED TO RESTRAINT OR
SECLUSION
......................................... 5.24
A. CMS Death Reporting and
Documentation Requirements
...................5.24
Reporting Requirement ...................................5.24
Regional Office Phone Number/Worksheet
......5.24
Documentation Requirement
...........................5.24
CMS Response
..............................................5.25
Survey Procedures
.........................................5.25
B. FDA: Safe Medical Devices Act
Reporting Requirement
...............................5.25
C. Reporting Restraint and Seclusion to
Local Behavioral Health Director
...............5.25
D. California Adverse Event Reporting
Requirement ................................................5.25
E. Regional Centers for Persons with
Developmental Disabilities .........................5.26
Monthly Reporting ..........................................5.26
Incident Reporting
..........................................5.26
Definitions
.......................................................5.27
F. Medication Error .......................................... 5.27
G. California Unusual Occurrence
Reporting Requirement
...............................5.27
H. Staff Injury ....................................................5.27
I. TJC Sentinel Event Requirement ...............5.27
XVIII. STAFF TRAINING REQUIREMENTS ...... 5.27
A. Federal Law: CMS Conditions of
Participation and Interpretive Guidelines
..5.27
Training Intervals ............................................. 5.27
Training Content
.............................................5.27
Who Must Be Trained
......................................5.29
Trainer Requirements
......................................5.29
Training Documentation
..................................5.29
Survey Procedures
.........................................5.29
B. California Law ..............................................5.30

©CALIFORNIA HOSPITAL ASSOCIATION
Chapter 5 — Contents
Chapter 5 — Restraints and Seclusion CHA
FORMS & APPENDICES
25-A Report of a Hospital Death Associated With
Restraint or Seclusion
Forms and Appendices can be found at the back of the manual and
online for CHA members at www.calhospital.org/free-resources.
XIX. LAW ENFORCEMENT RESTRAINT
OR SECLUSION
................................... 5.30
A. Federal Law: CMS Conditions of
Participation and Interpretive Guidelines
..5.30
B. California Law ..............................................5.31
XX. DOCUMENTATION REQUIREMENTS ........ 5.31
A. Federal Law: CMS Conditions of
Participation and Interpretive Guidelines
..5.31
Survey Procedures .........................................5.31
B. California Law ..............................................5.32

5 Restraints and Seclusion
5.1
©CALIFORNIA HOSPITAL ASSOCIATION
I. INTRODUCTION
The use of restraint and seclusion in health care facilities is
highly regulated by both the state and federal governments.
In the year prior to the publication of the Centers for
Medicare & Medicaid Services (CMS) interim final rule
regarding patient rights in 1999, the public, patient
advocacy groups, the media and Congress became
increasingly concerned about the need to ensure basic
protections for patient health and safety in hospitals with
regard to the use of restraint and seclusion. The Hartford
Courant, a Connecticut newspaper, heightened public
awareness of this issue with a series of articles in October
1998 citing the results of a study that identified 142 deaths
from seclusion or restraint use in mental health treatment
facilities in the previous 10 years. The majority of the deaths
were adolescent patients. The Hartford Courant articles
were reprinted around the country, receiving widespread
attention and leading to broad criticism of both private
hospital accreditation organizations and government
agencies charged with oversight of patient protection and
safety.
The goal of the laws regarding restraint and seclusion is to
protect patients’ rights to be free from the inappropriate
use of restraint and seclusion; to protect the patient,
hospital staff, and others from violent or self-destructive
behavior; and to promote patient safety when the use of
either intervention is necessary.
A. Scope of Chapter
This chapter addresses all state and federal laws regarding
restraint and seclusion applicable to general acute care
hospitals (GACHs) and acute psychiatric hospitals (APHs)
with respect to mental health patients.
This chapter does not discuss all laws regarding restraint
and seclusion applicable to skilled nursing facilities,
intermediate care facilities, psychiatric health facilities
or psychiatric residential treatment facilities. In addition,
hospitals operated by the state of California or the
United States government may be subject to additional
requirements not described in this chapter.
B. Restraint and Seclusion Laws
FEDERAL LAW
CMS Conditions of Participation and Interpretive
Guidelines
The primary federal law regarding restraint and seclusion
is found in the regulation published by CMS as part of the
Patients’ Rights Condition of Participation (CoP) [42 C.F.R.
Section 482.13]. All hospitals (acute care, long-term care,
psychiatric, children’s, and cancer) must comply with the
regulation to participate in the Medicare and Medicaid
programs. The requirements of the regulation apply to
all patients in a Medicare- or Medicaid-participating
hospital, not just Medicare or Medicaid beneficiaries.
The requirements apply to inpatients and outpatients
in all locations within the hospital (including medical/
surgical units, critical care units, emergency department,
psychiatric units, etc.). However, critical access hospitals
must comply only if they have a distinct-part psychiatric or
rehabilitative unit.
CMS contracts with “State Survey Agencies” (SAs) to
survey hospitals to assess their compliance with the
CoPs. In California, the SA is the California Department
of Public Health (CDPH). The SAs conduct these
surveys using the State Operations Manual published
by CMS. The State Operations Manual may be found
at www.cms.gov/Regulations-and-Guidance/Guidance/
Manuals/Internet-Only-Manuals-IOMs.html (click on
Publication 100-07). The State Operations Manual has
several appendices that apply to hospitals, for example,
A (hospitals), AA (psychiatric hospitals), V (EMTALA), and
W (critical access hospitals). Each appendix contains
the actual language of a CoP (the regulation) as well as
Interpretive Guidelines and survey probes that elaborate
on regulatory intent and give in-depth detail to surveyors
and hospitals about how to determine compliance with
the CoPs. The SAs recommend to CMS whether hospitals
meet the CoPs. The appendix that contains the Interpretive
Guidelines for restraint and seclusion, referred to
throughout this chapter, is Appendix A (hospitals). Restraint
and seclusion guidelines are found in Tags A-0154 through
A-0214.

CHA Mental Health Law Manual 2019
5.2
©CALIFORNIA HOSPITAL ASSOCIATION
This chapter discusses the requirements of the CMS
CoP regulation related to restraint and seclusion, and
describes the Interpretive Guidelines, including survey
probes to describe what surveyors will look for during
surveys. The Interpretive Guidelines sometimes
distinguish between restraints used to manage nonviolent,
non-self-destructive behavior and restraints used to
manage violent or self-destructive behavior. The reason
for this distinction is that the Interpretive Guidelines apply
to the use of restraints in the medical/surgical and skilled
nursing settings — for example, positioning devices, side
rails, Geri-chairs, etc. This chapter focuses on restraints
used in the mental health setting, which are primarily used
to manage violent or self-destructive behavior. However,
requirements related to both types of restraint use are
described at times when useful to facilitate understanding
of the requirements.
Children’s Health Act of 2000
A federal statute, the Children’s Health Act of 2000
(Pub.L. 106-310), was enacted on Oct. 17, 2000 — after
the publication by CMS of its interim final rule regarding
restraint and seclusion, but before publication of the final
rule.
The Children’s Health Act contained several provisions
not specific to children’s health, including some related to
restraint and seclusion [42 U.S.C. Sections 290ii to 290ii-2].
CMS incorporated these statutory requirements into its final
rule, which amended the hospital CoPs, regarding restraint
and seclusion. Therefore, hospitals in compliance with the
CoPs are also in compliance with the Children’s Health Act
requirements related to restraint and seclusion.
CALIFORNIA LAW
The primary law in California regarding restraint and
seclusion is found in Health and Safety Code Sections
1180.1 to 1180.5. This statute applies to patients admitted
to acute psychiatric hospitals and to psychiatric units of
general acute care hospitals (and other facilities as well). It
does not apply to patients in a medical/surgical unit, an
ICU, or the emergency department of a general acute
care hospital.
Hospital licensing regulations (Title 22) also contain several
requirements regarding the use of restraint and seclusion.
They are discussed in this chapter.
MUST COMPLY WITH ALL LAWS
California hospitals that participate in Medicare or Medicaid
programs must comply with all of the federal requirements
and all of the state requirements described in this chapter.
There is no federal preemption of state law.
C. Accreditation Organization Standards
California hospitals that are accredited by The Joint
Commission (TJC) or other accreditation organizations
must comply with the standards established by those
organizations. TJC standards regarding restraint and
seclusion are substantially similar to the federal law
requirements described in this chapter. (The relevant TJC
standards are PC.03.05.01 through PC.03.05.19.)
Other accrediting organizations may have adopted different
requirements regarding the use of seclusion or restraint.
Hospitals accredited by organizations other than TJC
should carefully check those requirements in addition to
complying with the requirements described in this chapter.
II. PATIENTS’ RIGHTS REGARDING RESTRAINT
AND SECLUSION
Both state and federal law contain multiple provisions
regarding patients’ rights. Requirements regarding patient
rights in general — that is, rights that apply to all patients,
not just mental health patients — are described in chapter 1
of CHA’s Consent Manual. Requirements regarding the
general rights of mental health patients are described in
chapter 4 of this manual. This chapter describes only those
patients’ rights that are specific to restraint and seclusion.
A. Federal Law: CMS Conditions of Participation
and Interpretive Guidelines
Federal law states that all patients have the right to be free
from physical or mental abuse, and corporal punishment.
All patients have the right to be free from restraint or
seclusion, of any form, imposed as a means of coercion,
discipline, convenience, or retaliation by staff. Restraint or
seclusion may be imposed only to ensure the immediate
physical safety of the patient, a staff member, or others
and must be discontinued at the earliest possible time. The
patient also has the right to safe implementation of restraint
or seclusion by trained staff. [42 C.F.R. Section 482.13(e)
and (f)]
The Interpretive Guidelines state that hospital leadership is
responsible for creating a culture that supports a patient’s
right to be free from restraint or seclusion. Leadership
must ensure that systems and processes are developed,
implemented, and evaluated that support patients’ rights
and that eliminate the inappropriate use of restraint or
seclusion. Through its Quality Assurance/Performance
Improvement (QAPI) program, hospital leadership should:
1. Assess and monitor the use of restraint or seclusion in
the facility;

Chapter 5 — Restraints and Seclusion CHA
5.3
©CALIFORNIA HOSPITAL ASSOCIATION
2. Implement actions to ensure that restraint or seclusion
is used only to ensure the physical safety of the patient,
staff and others; and
3. Ensure that the hospital complies with the
requirements set forth in the federal regulation as well
as those set forth by state law and hospital policy
when the use of restraint or seclusion is necessary.
SURVEY PROCEDURES
The Interpretive Guidelines direct surveyors to consider
the following:
1. Review a sample of medical records of patients for
whom restraints were used to manage nonviolent,
non-self-destructive behavior, as well as a sample
of medical records of patients for whom restraint
or seclusion was used to manage violent or
self-destructive behavior.
2. Include in the review patients who are currently in
restraint or seclusion, as well as those who have
been in restraint or seclusion during their hospital stay
(include both violent or self-destructive patients, as well
as nonviolent, non-self-destructive patients).
3. What evidence is there that hospital staff identified the
reason for the restraint or seclusion, and determined
that other less restrictive measures would not be
effective before applying the restraint?
4. Interview staff who work directly with patients to
determine their understanding of the restraint and
seclusion policies. If any patients are currently in
restraint or seclusion, ascertain the rationale for
use and when the patient was last monitored and
assessed.
5. Is the actual use of restraints or seclusion consistent
with hospital restraint and seclusion policies and
procedures, as well as CMS requirements?
6. Review incident and accident reports to determine
whether patient injuries occurred proximal to or during
a restraint or seclusion intervention. Are incidents and
accidents occurring more frequently with restrained or
secluded patients?
7. If record review indicates that restrained or secluded
patients sustained injuries, determine what the hospital
did to prevent additional injury. Determine if the
hospital investigated possible changes to its restraint
or seclusion policies.
8. Obtain data on the use of restraint and seclusion for a
specified time period (e.g., three months) to determine
any patterns in their use for specific units, shifts, days
of the week, etc.
9. Does the number of patients who are restrained or
secluded increase on weekends, on holidays, at night,
on certain shifts; where contract nurses are used;
in one unit more than other units? Such patterns
of restraint or seclusion use may suggest that the
intervention is not based on the patient’s need, but on
issues such as convenience, inadequate staffing or
lack of staff training. Obtain nursing staffing schedules
during time periods in question to determine if staffing
levels impact the use of restraint or seclusion.
10. Interview a random sample of patients who were
restrained to manage nonviolent, non-self-destructive
behavior. Were the reasons for the use of a restraint
to manage nonviolent, non-self-destructive behavior
explained to the patient in understandable terms?
Could the patient articulate his/her understanding?
NOTE: The instructions to surveyors regarding restraints
to manage nonviolent, non-self-destructive behavior may
be more applicable in a medical/surgical or skilled nursing
setting than a mental health setting.
B. California Law
California law is virtually identical to federal law with respect
to the rights of patients who are restrained or secluded.
California law states that:
A patient has the right to be free from the use of
seclusion and behavioral restraints of any form imposed
as a means of coercion, discipline, convenience, or
retaliation by staff. This right includes, but is not
limited to, the right to be free from the use of a drug
used in order to control behavior or to restrict the
person’s freedom of movement, if that drug is not
a standard treatment for the person’s medical or
psychiatric condition.
[Health and Safety Code Section 1180.4(k); Title 9,
California Code of Regulations, Section 865.4] (Although
the last sentence in the state law is not included in the
patients’ rights portion of the federal law, it is included
elsewhere in the federal law.) (See “Drug Used as a
Restraint,”page5.6.)

CHA Mental Health Law Manual 2019
5.4
©CALIFORNIA HOSPITAL ASSOCIATION
III. GENERAL INFORMATION REGARDING
RESTRAINT AND SECLUSION
A. Quick Summary of Restraint and Seclusion
Laws
If a hospital uses restraint or seclusion, the use must be:
1. In accordance with the order of a licensed health
care practitioner acting within the scope of his or her
professional licensure;
2. In accordance with a written modification to the
patient’s plan of care;
3. Used in the least restrictive manner possible;
4. Used in accordance with safe and appropriate
restraining techniques;
5. Selected only when other less restrictive measures
have been found ineffective to protect the patient or
others from harm; and
6. Ended at the earliest possible time.
The patient’s attending physician must be consulted
as soon as possible, if the attending physician did not
order the restraint (see IX.“Notification of Attending
Physician,”page5.16). In addition, the condition of
the restrained or secluded patient must be continually
assessed, monitored, and reevaluated. All staff involved
in the care of restrained or secluded patients must have
ongoing education and training in the proper and safe use
of restraint and seclusion. A debriefing must follow each
episode of restraint or seclusion.
Details of these requirements are discussed in this chapter.
B. Techniques
The use of restraint or seclusion must be implemented
in accordance with safe and appropriate restraint and
seclusion techniques as determined by hospital policy in
accordance with state law [42 C.F.R. Section 482.13(e)
(4)(ii)]. State law does not contain specific requirements
regarding restraint technique, except to describe
certain prohibited techniques (see XV.“Prohibited
Techniques,”page5.21).
Title 22 regulations applicable to acute psychiatric hospitals
require that restraints be easily removable in the event
of fire or other emergency [Title 22, California Code of
Regulations, Section 71545(d)]. In addition, if seclusion
rooms are provided, they must be designed and equipped
to ensure the safety of the patient [Title 22, California Code
of Regulations, Section 71625].
The Interpretive Guidelines state that the use of restraint
or seclusion must never act as a barrier to the provision of
other interventions to meet the patients’ needs.
SURVEY PROCEDURES
The Interpretive Guidelines direct surveyors to consider
the following:
1. Review the hospital’s policies and procedures to
determine if they reflect current standards of practice
regarding safe and appropriate restraint and seclusion
techniques. Are there any references to state law
statutes or any indication that state laws were reviewed
and incorporated?
2. Review a sample of patient medical records
that include patients who required the use of
restraint or seclusion for the management of both
violent, self-destructive behaviors, and nonviolent,
non-self-destructive behaviors.
3. After restraints were applied, was an assessment
immediately made to ensure that restraints were
properly and safely applied?
4. Were the hospital policies and procedures followed?
5. Was the use of restraint or seclusion effective in
achieving the purpose for which it was ordered? If not,
were timely changes made?
6. Was there any evidence of injury to the patient?
C. Restraints are Medical Devices Regulated by
the FDA
The Food and Drug Administration (FDA) regulates restraint
devices as it regulates other medical devices. Any restraint
used by a hospital should be FDA-approved, and used
according to the manufacturer’s instructions.
Under the Safe Medical Devices Act of 1990, hospitals and
other device user facilities must report incidents involving
medical devices (including restraints) that have or may
have caused or contributed to the serious injury or death
of a patient. Details of this reporting requirement are found
in XVII.“Reporting Requirements Related to Restraint or
Seclusion,”page5.24.
IV. DEFINITIONS
Both federal and state law contain definitions of various
terms related to restraint and seclusion. The definition of
“seclusion” is identical under both; however, other terms are
defined differently. As a practical matter, the difference in
definitions is not significant in the mental health setting.

Chapter 5 — Restraints and Seclusion CHA
5.5
©CALIFORNIA HOSPITAL ASSOCIATION
The definitions and requirements in federal law apply to
medical/surgical patients as well as mental health patients.
Although this manual focuses on mental health law, some
discussion of the definitions as applied to medical/surgical
patients is included as helpful to understanding their
meaning as applied to mental health patients.
A. Federal Law: CMS Conditions of Participation
and Interpretive Guidelines
RESTRAINT
Federal law defines a “restraint” as:
1. Any manual method, physical or mechanical device,
material, or equipment that immobilizes or reduces the
ability of a patient to move his or her arms, legs, body
or head freely; or
2. A drug or medication when it is used as a restriction to
manage the patient’s behavior or restrict the patient’s
freedom of movement and is not a standard treatment
or dosage for the patient’s condition.
[42 C.F.R. Section 482.13(e)(1)]
General Rule
The CMS definition is a functional definition. That is, if a
patient is functionally restrained, regardless of the method
used, then the restraint requirements apply. Similarly, if a
patient can easily remove a device, the device would not
be considered a restraint. “Easily remove” means that
the manual method, device, material, or equipment can be
removed intentionally by the patient in the same manner
as it was applied by the staff, considering the patient’s
physical condition and ability to accomplish the objective,
such as transfer to a chair, get to the bathroom in time,
etc. (e.g., side rails can be put down, not climbed over;
buckles can be intentionally unbuckled; ties or knots can
be intentionally untied; etc.). It is important to document
that the patient can unsnap the belt in the wheelchair,
or that the patient can lower the side rails when she
wants to, etc. so that it is clear that such devices do not
constitute restraints.
Examples
The use of an FDA-approved protective restraint would
constitute the restraint of a patient as defined in the federal
regulation. Other devices and practices that could meet the
CMS definition of a restraint include:
1. Tucking a patient’s sheets in so tightly that the patient
cannot move.
2. Use of a “net bed” or an “enclosed bed” that prevents
the patient from freely exiting the bed. However,
placement of a toddler in an “enclosed” or “domed”
crib is not a restraint.
3. Use of “Freedom” splints that immobilize a
patient’s limb.
4. Using side rails that prevent a patient from voluntarily
getting out of bed.
5. Geri-chairs or recliners, but only if the patient cannot
easily remove the restraint appliance and get out of the
chair on his or her own.
These types of “restraints” are more commonly used in
medical/surgical and skilled nursing settings rather than
mental health settings; they are included in this manual
as illustrative.
Positioning Devices
A medically-necessary positioning or securing device
used to maintain the position, limit mobility, or temporarily
immobilize the patient during medical, dental, diagnostic,
or surgical procedures is not considered a restraint. Thus,
an IV arm board or a hand mitt would generally not be
considered a restraint. However, if the board or mitt is
attached to the bed, this would meet the definition of a
restraint. In addition, if the mitts are applied so tightly that
the hand or fingers are immobilized — or if the mitts are
so bulky that the patient’s ability to use his or her hands
is significantly reduced — this would be considered
a restraint.
Physical Escort
A physical escort may include a light grasp to escort the
patient to a desired location. If the patient can easily
remove or escape the grasp, this is not a restraint.
However, if the patient cannot easily remove or escape the
grasp, this is a restraint.
Physical Holding
The Interpretive Guidelines permit the physical holding
of a patient to conduct routine physical exams or tests.
However, patients have the right to refuse physical exams
or tests. Holding a patient in a manner that restricts the
patient’s movement against the patient’s will is considered
a restraint. This includes “therapeutic holds.” CMS states
that physically holding a patient can be just as restrictive,
and just as dangerous, as restraining methods that involve
devices.
The application of force to physically hold a patient, in order
to administer a medication against the patient’s wishes,

CHA Mental Health Law Manual 2019
5.6
©CALIFORNIA HOSPITAL ASSOCIATION
is considered restraint. The patient has a right to be free
of restraint and, in accordance with the patients’ rights
CoP (42 C.F.R. Section 482.13(b)(2)), also has a right to
refuse medications, unless a court has ordered medication
treatment. Additionally, some patients may be medicated
against their will in certain emergency circumstances.
However, in both of these circumstances, health care
staff is expected to use the least restrictive method of
administering the medication to avoid or reduce the use of
force, when possible. The use of force in order to medicate
a patient, as with other restraint, must have a physician’s
order prior to the application of the restraint (use of force).
If physical holding for forced medication is necessary with
a violent patient, the one-hour face-to-face evaluation
requirement would also apply.
In certain circumstances, a patient may consent to an
injection or procedure, but may not be able to hold still
for an injection, or cooperate with a procedure. In such
circumstances, and at the patient’s request, staff may
“hold” the patient in order to safely administer an injection
(or obtain a blood sample, or insert an intravenous line,
if applicable) or to conduct a procedure. This is not
considered restraint.
A staff member picking up, redirecting, or holding an infant,
toddler, or preschool-aged child to comfort the patient is
not considered restraint.
Side Rails
A restraint does not include methods that protect the
patient from falling out of bed. However, side rails are
sometimes used instead to restrict the patient’s freedom
to exit the bed (this is usually not an issue in the mental
health setting). Such use of side rails would be considered
a restraint.
Disoriented patients may view a raised side rail as a barrier
to climb over, may slide between raised, segmented side
rails, or may scoot to the end of the bed to get around
a raised side rail and exit the bed. When attempting to
leave the bed by any of these routes, the patient is at risk
for entrapment, entanglement, or falling from a greater
height posed by the raised side rail, with a possibility for
sustaining greater injury or death than if the patient had
fallen from the height of a lowered bed without raised side
rails. In short, the patient may have an increased risk for
a fall or other injury by attempting to exit the bed with the
side rails raised. The risk presented by side rail use should
be weighed against the risk presented by the patient’s
behavior as ascertained through individualized assessment.
When the clinician raises all four side rails in order to
restrain a patient (that is, to immobilize or reduce the
ability of a patient to move his or her arms, legs, body, or
head freely) to ensure the immediate physical safety of the
patient, then the requirements of the restraint regulation
apply. Raising fewer than four side rails when the bed has
segmented side rails would not necessarily immobilize or
reduce the ability of a patient to move freely as defined in
the regulation. For example, if the side rails are segmented
and all but one segment are raised to allow the patient to
freely exit the bed, the side rail is not acting as a restraint.
Conversely, if a patient is not physically able to get out
of bed regardless of whether the side rails are raised or
not, raising all four side rails for this patient would not be
considered restraint because the side rails have no impact
on the patient’s freedom of movement. In this example, the
use of all four side rails would not be considered restraint.
The use of side rails on stretchers is not considered a
restraint. Neither is the use of a seat belt when transporting
a patient in a wheelchair.
Drug Used as a Restraint
Drugs or medications that are used as part of a patient’s
standard medical or psychiatric treatment, and are
administered within the standard dosage for the patient’s
condition, are not considered restraints [42 C.F.R. Section
482.13(e)(1)(i)(B)].
The Interpretive Guidelines state that the restraint and
seclusion regulations are not intended to interfere with
the clinical treatment of patients who are suffering from
serious mental illness and who need therapeutic doses
of medication to improve their level of functioning so
that they can more actively participate in their treatment.
Similarly, the regulations are not intended to interfere with
appropriate doses of sleeping medication prescribed for
patients with insomnia, anti-anxiety medication prescribed
to calm a patient who is anxious, or analgesics prescribed
for pain management. The regulatory language is intended
to provide flexibility and recognize the variations in patient
conditions.
Whether or not an order for a medication is PRN or a
standing order does not determine whether or not the
use of that drug is considered a restraint. The use of PRN
or standing order medications is prohibited only if the
medication is a drug used as a restraint. Similarly, whether
or not the use of a medication is voluntary, or even whether
the drug is administered as a one-time dose or PRN are not
factors in determining if a drug is being used as a standard
treatment. [71 Fed. Reg. 71378, 71391 (Dec. 8, 2006)]
If a drug is used as a restraint, all restraint requirements
must be followed, including the time-limited orders and the
assessment, documentation, and monitoring requirements.

Chapter 5 — Restraints and Seclusion CHA
5.7
©CALIFORNIA HOSPITAL ASSOCIATION
Criteria used to determine whether the use of a drug or
combination of drugs is a standard treatment or dosage for
the patient’s condition includes all of the following:
1. The drug is used within the pharmaceutical parameters
approved by the FDA and the manufacturer for the
indications that it is manufactured and labeled to
address, including listed dosage parameters;
2. The use of the drug follows national practice
standards established or recognized by the medical
community, or professional medical associations or
organizations; and
3. The use of the drug to treat a specific patient’s clinical
condition is based on that patient’s symptoms, overall
clinical situation, and on the physician’s knowledge
of that patient’s expected and actual response to the
medication.
Another component of “standard treatment or dosage”
for a drug is the expectation that the standard use of a
drug to treat the patient’s condition enables the patient
to more effectively or appropriately function in the world
around them than would be possible without the use of the
medication. If the overall effect of a drug or combination
of drugs is to reduce the patient’s ability to effectively or
appropriately interact with the world around the patient,
then the drug is not being used as a standard treatment or
dosage for the patient’s condition.
As with any use of restraint or seclusion, staff must conduct
a comprehensive patient assessment to determine the
need for other types of interventions before using a drug as
a restraint. For example, a patient may be agitated due to
pain, an adverse reaction to an existing drug or medication,
or other unmet care need or concern.
There are situations where the use of a drug is clearly
outside the standard for a patient or a situation, or a
medication is not medically necessary but is used for
patient discipline or staff convenience (neither of which is
allowed by law).
CMS has provided the following two examples.
Example 1. A patient has Sundowner’s Syndrome, a
syndrome in which a patient’s dementia becomes more
apparent at the end of the day rather than at the beginning
of the day. The patient may become agitated, angry, or
anxious at sundown. This may lead to wandering, pacing
the floors, or other nervous behaviors. The staff finds the
patient’s behavior bothersome, and asks the physician
to order a high dose of a sedative to “knock out” the
patient and keep him in bed. The patient has no medical
symptoms or condition that indicates the need for a
sedative. In this case, for this patient, the sedative is being
used inappropriately as a restraint for staff convenience.
Such use is not permitted.
Example 2. A patient is in a detoxification program. The
patient becomes violent and aggressive. Staff administers
a PRN medication ordered by the patient’s physician
to address these types of outbursts. The use of the
medication enables the patient to better interact with others
or function more effectively. In this case, the medication
used for this patient is not considered a “drug used as a
restraint.” The availability of a PRN medication to manage
outbursts of specific behaviors, such as aggressive, violent
behavior is standard for this patient’s medical condition
(i.e., drug or alcohol withdrawal). Therefore, this patient’s
medication does not meet the definition of “drug used as a
restraint” since it is a standard treatment or dosage for the
patient’s medical or psychiatric condition.
If a drug or medication is used as a standard treatment (as
previously defined) to address the assessed symptoms and
needs of a patient with a particular medical or psychiatric
condition, its use is not subject to the requirements of the
federal regulation. However, the patient would still need to
receive any assessments, monitoring, interventions, and
care that are appropriate for that patient’s needs.
SECLUSION
“Seclusion” is the involuntary confinement of a patient
alone in a room or area from which the patient is physically
prevented from leaving. Seclusion may be used only for
the management of violent or self-destructive behavior that
jeopardizes the immediate physical safety of the patient, a
staff member, or others.
Seclusion is not just confining a patient to an area, but
involuntarily confining the patient alone in a room or area
where the patient is physically prevented from leaving. If a
patient is restricted to a room alone and staff are physically
intervening to prevent the patient from leaving the room
or giving the perception that threatens the patient with
physical intervention if the patient attempts to leave the
room, the room is considered locked, whether the door is
actually locked or not. In this situation, the patient is being
secluded.
A patient physically restrained alone in an unlocked room
does not constitute seclusion. Confinement on a locked
unit or ward where the patient is with others does not
constitute seclusion.
Timeout is not considered seclusion. The Interpretive
Guidelines state that a “timeout” is an intervention in which
the patient consents to being alone in a designated area

CHA Mental Health Law Manual 2019
5.8
©CALIFORNIA HOSPITAL ASSOCIATION
for an agreed upon time frame from which the patient is not
physically prevented from leaving. Therefore, the patient
can leave the designated area when the patient chooses.
The Children’s Health Act defines “time out” to mean
a “behavior management technique that is part of an
approved treatment program and may involve the
separation of the resident from the group, in a nonlocked
setting, for the purpose of calming” [42 U.S.C. Section
290ii].
Quarantining a patient for public health reasons, as
governed by state law, is not considered “seclusion” under
federal law [71 Fed. Reg. 71378, 71404 (Dec. 8, 2006)].
SURVEY PROCEDURES
The Interpretive Guidelines direct surveyors to consider
the following:
1. Determine whether the hospital’s policies and
procedures employ a definition or description of what
constitutes “restraint” and “seclusion” that is consistent
with the federal regulation.
2. Determine whether the hospital’s policies and
procedures employ a definition or description of what
constitutes the use of a drug as a restraint that is
consistent with the federal regulation.
3. While touring hospital units look for restraints in use.
Where a restraint is in use, check the medical record
for appropriate documentation.
4. While touring hospital units look for bed side rail use
to determine whether it is consistent with the definition
of a restraint. Where bed side rails are being used as
a restraint, check the medical record for appropriate
documentation. (This direction to surveyors is more
applicable to the medical/surgical or skilled nursing
setting rather than the mental health setting.)
5. Interview hospital staff to determine whether they know
the definition of a “restraint” (particularly with respect to
use of bed side rails) and “seclusion.”
6. Interview hospital staff to determine whether they
can identify when the use of a drug or medication is
considered a chemical restraint.
B. California Law
For purposes of this chapter, the following definitions apply.
“Behavioral restraint” means “mechanical restraint” or
“physical restraint” used as an intervention when a patient
presents an immediate danger to self or others. It does
not include restraints used for medical purposes, including,
but not limited to, securing an intravenous needle or
immobilizing a person for a surgical procedure, or postural
restraints, or devices used to prevent injury or to improve a
patient’s mobility and independent functioning rather than
to restrict movement.
“Containment” means a brief physical restraint of a patient
for the purpose of effectively gaining quick control of a
patient who is aggressive or agitated or who is a danger to
self or others.
“Mechanical restraint” means the use of a mechanical
device, material, or equipment attached or adjacent to the
patient’s body that he or she cannot easily remove and
that restricts the freedom of movement of all or part of a
person’s body or restricts normal access to the person’s
body, and that is used as a behavioral restraint.
“Physical restraint” means the use of a manual hold to
restrict freedom of movement of all or part of a patient’s
body, or to restrict normal access to the patient’s body, and
that is used as a behavioral restraint. “Physical restraint”
is staff-to-patient physical contact in which the patient
unwillingly participates. “Physical restraint” does not include
briefly holding a patient without undue force in order to
calm or comfort, or physical contact intended to gently
assist a patient in performing tasks or to guide or assist a
patient from one area to another.
“Seclusion” means the involuntary confinement of
a patient alone in a room or an area from which the
patient is physically prevented from leaving. “Seclusion”
does not include a “timeout,” as defined in regulations
relating to facilities operated by the State Department of
Developmental Services.
“Time out” is defined as the “removal of a client from
specified activities for a specific period of time.”
[Health and Safety Code Section 1180.1; Title 9, California
Code of Regulations, Section 865.4; Title 22, California
Code of Regulations, Section 76331]
V. INTAKE ASSESSMENT/CARE PLAN
State and federal laws require that a patient receive an
overall physical and psychiatric exam around the time of
admission and that a plan of care be developed [42 C.F.R.
Sections 482.24(c)(2) and 482.61; Title 22, California Code
of Regulations, Sections 70717(d), 71517(c) and 71549].
This portion of the manual describes only the requirements
related to restraint and seclusion — it is not intended
to describe everything a hospital must consider and
document in its evaluation, assessment, and overall care
planning for a mental health patient.

Chapter 5 — Restraints and Seclusion CHA
5.9
©CALIFORNIA HOSPITAL ASSOCIATION
A. Federal Law: CMS Conditions of Participation
and Interpretive Guidelines
CMS requires that the use of restraint or seclusion be in
accordance with a written modification to the patient’s plan
of care [42 C.F.R. Section 482.13(e)(4)(i)].
CMS notes that it refers to the “modified” plan of care to
reinforce its expectation that restraint or seclusion should
not be a standard response to a particular behavior or
situation [64 Fed. Reg. 36070, 36083 (July 2, 1999)]. CMS
also states that the regulation does not require that a
modification to the patient’s plan of care be made before
initiating or obtaining an order for the use of restraint
or seclusion. The plan of care should be reviewed and
updated in writing to reflect the use of restraint or seclusion
within a time frame specified by hospital policy. The use of
restraint or seclusion should be reflected in the patient’s
plan of care based on an assessment and evaluation of
the patient.
The Patients’ Rights CoP promotes the patient’s right to be
involved in and make decisions about his or her health care.
This includes being informed of his or her health status,
being involved in care planning and treatment, and being
able to request or refuse treatment. This standard applies
to all health care, and is not specific to mental health care
or to the use of restraint or seclusion. The patient should
be informed of changes to the plan of care, including the
use of restraint or seclusion.
Although in general a competent patient may refuse
recommended treatment, in the preamble to the final
Patients’ Rights rule, CMS stated that:
If the patient’s violent or self-destructive behavior
jeopardizes the immediate physical safety of the patient,
a staff member, or others, the patient does not have
the right to refuse the use of restraint or seclusion. In
this situation, the use of restraint or seclusion is an
emergency measure to protect the safety of the patient,
staff, or others. [71 Fed. Reg. 71378, 71392 (Dec. 8,
2006)]
SURVEY PROCEDURES
CMS emphasizes the individualized assessment and
evaluation of the patient in its survey probes. The
Interpretive Guidelines direct surveyors to consider
the following:
1. Determine whether the hospital’s procedures are
consistent with the requirements of the regulation.
Does the plan of care reflect a process of assessment,
intervention, and evaluation when restraint or seclusion
is used?
2. Is there evidence of assessment of the identified
problem or of an individual patient assessment? Does
the patient’s plan of care reflect that assessment?
3. What was the goal of the intervention?
4. What was the described intervention?
5. Who is responsible for implementation?
6. Was the patient informed of the changes in his or her
plan of care?
7. Did the physician or other licensed independent
practitioner (LIP) write orders that included a
time limit? Were these orders incorporated into
the plan of care? (See VII.“Order for Restraint or
Seclusion,”page5.12.)
8. After the discontinuation of the restraint or seclusion,
was this information documented in an update of the
plan of care?
B. California Law
California law requires that each facility conduct an initial
assessment of each patient prior to a placement decision
or upon admission, or as soon thereafter as possible.
The assessment must include input from the patient and
someone the patient desires to be present, such as a family
member or other person designated by the patient, if the
desired family member or other person can be present at
the time of admission.
The initial assessment must include all of the following, to
the extent the information is available at the time of the
initial assessment:
1. Identification of early warning signs, triggers, and
precipitants that cause the patient to escalate.
2. Identification of the earliest precipitant of
aggression for patients with a known or suspected
history of aggressiveness, or patients who are
currently aggressive.
3. Techniques, methods, or tools that would help the
patient control his or her behavior.
4. Preexisting medical conditions or any physical
disabilities or limitations that would place the patient at
greater risk during restraint or seclusion.
5. Any trauma history, including any history of sexual or
physical abuse that the patient feels is relevant.

CHA Mental Health Law Manual 2019
5.10
©CALIFORNIA HOSPITAL ASSOCIATION
6. The patient’s advance directive regarding de-escalation
or the use of seclusion or behavioral restraints. (See
discussion below regarding psychiatric advance
directives.)
For general acute care hospitals, this California requirement
applies only to patients admitted to the psychiatric unit, if
the hospital has one. It does not apply to mental health
patients in the emergency department, an intensive care
unit, or other locations within the hospital [Health and
Safety Code Sections 1180.3 and 1180.4].
PSYCHIATRIC ADVANCE DIRECTIVES
A psychiatric advance directive is an instrument that mental
health patients may use to document their preferences
regarding future mental health treatment, in preparation for
the possibility of losing capacity to give or withhold consent
to treatment in the future. The mental health advocacy
community advocates the use of such documents,
particularly with respect to involuntary treatment,
psychiatric medications, restraint and seclusion.
Neither California nor federal law recognizes a special
document called a “psychiatric advance directive.” The
California advance health care directive laws and statutory
form were created with end-of-life issues in mind, not
mental health matters. However, the law does not prohibit a
person who executes an advance health care directive from
including instructions regarding mental health treatment.
Whether such wishes are required to be followed by a
health care provider if the patient loses capacity depends
upon several factors, including:
1. Whether the patient would have the legal ability to
consent or withhold consent to the recommended
treatment if he or she were competent. For example,
a patient who is detained pursuant to Welfare
and Institutions Code Section 5150 et seq. is, by
law, unable to withhold consent to be evaluated
for a mental disorder and may not leave the facility.
Therefore, if such a patient has executed an advance
directive denying consent to such care, a hospital need
not comply with this instruction.
2. Whether the wishes stated in the advance directive are
medically ineffective or contrary to generally accepted
health standards. In such a case, the facility need not
comply with the patient’s instructions.
There are no statutes, regulations, or judicial decisions
regarding “psychiatric” advance directives in California,
except for the reference in the intake assessment
requirement. It should be noted that this statute does
not authorize “psychiatric advance directives,” nor does
it require a provider to comply with a patient’s stated
preferences. It merely requires the provider to assess a
patient’s advance directive, if any.
A hospital should consult legal counsel if a situation arises
regarding a psychiatric advance directive. (See chapter 3
of CHA’s Consent Manual for a complete discussion of the
law regarding advance directives.)
VI. LEAST RESTRICTIVE ALTERNATIVE
Both state and federal law require that the restraint or
seclusion be used only when less restrictive interventions
are ineffective to protect the patient, staff or others from
harm.
A. Federal Law: CMS Conditions of Participation
and Interpretive Guidelines
Restraint or seclusion may be used only when less
restrictive interventions have been determined to be
ineffective to protect the patient, a staff member, or others
from harm [42 C.F.R. Section 482.13(e)(3)]. In addition,
the type or technique of restraint or seclusion used must
be the least restrictive intervention that will be effective to
protect the patient, a staff member, or others from harm.
This determination may be made by nursing staff or other
trained clinical staff [71 Fed. Reg. 71378, 71393 (Dec. 8,
2006)].
CMS states that less restrictive interventions do not always
need to be attempted, but less restrictive interventions
must be considered and determined by staff to be
ineffective to protect the patient or others from harm
prior to the introduction of more restrictive measures.
Alternatives attempted, or the rationale for not using
alternatives, must be documented.
CMS states that the underpinning of this regulation is
the concept that safe patient care hinges on looking
at the patient as an individual and assessing his or her
condition, needs, strengths, weaknesses, and preferences.
Such an approach relies on caregivers who are skilled in
individualized assessment and in tailoring interventions
to the patient’s needs after weighing factors such as the
patient’s condition, behaviors, history, and environmental
factors.
Prior to the use of restraint or seclusion, a comprehensive
assessment of the patient must determine that the
risks associated with the use of restraint or seclusion
are outweighed by the risk of not using the restraint
or seclusion. CMS recommends a document entitled,

Chapter 5 — Restraints and Seclusion CHA
5.11
©CALIFORNIA HOSPITAL ASSOCIATION
“Learning from Each Other – Success Stories and Ideas
for Reducing Restraint/Seclusion in Behavioral Health,”
sponsored by the American Psychiatric Association,
American Psychiatric Nurses Association, the National
Association of Psychiatric Health Systems, and the
American Hospital Association. This document may be
found at www.nabh.org/nabh-resources. This website also
includes useful forms, assessment tools, and checklists.
SURVEY PROCEDURES
The Interpretive Guidelines direct surveyors to consider
the following:
1. Do the physician’s or other LIP’s orders specify the
reason for restraint or seclusion, the type of restraint,
and the duration of restraint or seclusion? (See
VII.“Order for Restraint or Seclusion,”page5.12.)
2. Does the severity of the behavior justify seclusion or
restraint usage by identifying an immediate and serious
danger to the physical safety of the patient or others?
3. Is there evidence that the hospital considers factors
other than the individual patient in determining
causes for the need for restraints or seclusion (i.e.,
environmental factors)?
4. Does the medical record include documentation of an
individual patient assessment and a revision of the plan
of care?
5. Does the medical record reflect changes in behavior
and staff concerns regarding safety risks to the
patient, staff, or others prompting use of seclusion or
restraints?
6. Did the patient’s behavior place the patient or others
at risk for harm? Was the patient’s behavior violent or
self-destructive?
7. Were other, less restrictive interventions tried and
documented, or is there evidence that alternatives
were considered and determined to be insufficient?
8. Is there clear documentation in the patient’s medical
record describing the steps or interventions used prior
to the use of the needed restraint or seclusion? That is,
what documentation is in the medical record to explain
the rationale for the use of restraint or seclusion?
9. Is the restraint or seclusion intervention the least
restrictive intervention that meets the patient’s clinical
needs and protects the safety of the patient, staff, or
others?
10. Did the staff determine that less restrictive alternatives
would not meet the patient’s clinical needs, or protect
the patient’s safety or the safety of others?
11. Do ongoing documented assessments demonstrate
that the restraint or seclusion intervention is needed at
this time (or at a time in the past) and that the restraint
or seclusion intervention remains the least restrictive
way to protect the patient’s safety?
12. If the time of restraint or seclusion use is lengthy, look
for evidence that the symptoms necessitating the
use of restraint or seclusion have persisted. Is there
evidence to indicate that the staff have evaluated
whether or not the restraint or seclusion can be safely
discontinued?
B. California Law
California law contains several provisions regarding
seclusion and restraint that require the least restrictive
alternative form of treatment be provided to mental health
patients.
Title 9, California Code of Regulations, Section 865.4
states that “seclusion and/or restraints shall never be
used as punishment or as a substitute for a less restrictive
alternative form of treatment.”
Similarly, the Health and Safety Code states that a health
facility must afford patients who are restrained the least
restrictive alternative and the maximum freedom of
movement, while ensuring the physical safety of the patient
and others. The facility must use the least number of
restraint points. [Health and Safety Code Section 1180.4(j)]
This requirement applies to all facilities. However, for
general acute care hospitals, this requirement applies only
to patients admitted to the psychiatric unit, if the hospital
has one. It does not apply to mental health patients in the
emergency department, an intensive care unit, or other
locations within the hospital [Health and Safety Code
Sections 1180.3 and 1180.4].
Title 22 regulations applicable to the psychiatric unit of
general acute care hospitals and to acute psychiatric
hospitals state that “restraint shall be used only when
alternative methods are not sufficient to protect the
patient or others from injury” [Title 22, California Code of
Regulations, Sections 70577(j)(1) and 71545(a)].

CHA Mental Health Law Manual 2019
5.12
©CALIFORNIA HOSPITAL ASSOCIATION
VII. ORDER FOR RESTRAINT OR SECLUSION
A. Federal Law: CMS Conditions of Participation
and Interpretive Guidelines
Federal law states that the use of restraint or seclusion
must be in accordance with the order of a physician
or other licensed independent practitioner (LIP) who is
responsible for the care of the patient as specified under
42 C.F.R. Section 482.12(c) and authorized to order
restraint or seclusion by hospital policy in accordance with
state law.
Section 482.12(c) states:
(c) Standard: Care of patients. In accordance with
hospital policy, the governing body must ensure that the
following requirements are met:
(1) Every Medicare patient is under the care of:
(a) A doctor of medicine or osteopathy (This
provision is not to be construed to limit the
authority of a doctor of medicine or osteopathy
to delegate tasks to other qualified health care
personnel to the extent recognized under state
law or a state’s regulatory mechanism.);
(b) A doctor of dental surgery or dental medicine
who is legally authorized to practice dentistry by
the state and who is acting within the scope of
his or her license;
(c) A doctor of podiatric medicine, but only with
respect to functions which he or she is legally
authorized by the state to perform;
(d) A doctor of optometry who is legally
authorized to practice optometry by the state in
which he or she practices;
(e) A chiropractor who is licensed by the state
or legally authorized to perform the services of a
chiropractor, but only with respect to treatment
by means of manual manipulation of the spine
to correct a subluxation demonstrated by x-ray
to exist; and
(f) A clinical psychologist as defined in 42 C.F.R.
Section 410.71, but only with respect to clinical
psychologist services as defined in 42 C.F.R.
Section 410.71 and only to the extent permitted
by state law.
(2) Patients are admitted to the hospital only on
the recommendation of a licensed practitioner
permitted by the state to admit patients to a
hospital. If a Medicare patient is admitted by
a practitioner not specified in paragraph (c)(1)
above, that patient is under the care of a doctor of
medicine or osteopathy.
(3) A doctor of medicine or osteopathy is on duty or
on call at all times.
(4) A doctor of medicine or osteopathy is
responsible for the care of each Medicare patient
with respect to any medical or psychiatric problem
that —
(a) is present on admission or develops during
hospitalization; and
(b) Is not specifically within the scope of practice
of a doctor of dental surgery, dental medicine,
podiatric medicine, or optometry; a chiropractor;
or clinical psychologist, as that scope is —
(i) Defined by the medical staff;
(ii) Permitted by state law; and
(iii) Limited, under paragraph (c)(1)(e) above,
with respect to chiropractors.
PRN ORDERS
Orders for the use of restraint or seclusion must never
be written as a standing order or on an as-needed
“PRN” basis.
WHO MAY ORDER RESTRAINT OR SECLUSION
Hospitals must have policies and procedures for the
initiation of restraint or seclusion that identify the categories
of LIPs that are permitted to order restraint or seclusion in
that hospital, consistent with state law. (California law is
described in B.“California Law,”page5.3.)
CMS states that, for the purposes of the use of restraint
or seclusion, the attending practitioner must be able to
conduct both a physical and psychological assessment
of the patient in accordance with state law, their scope of
practice, and hospital policy [71 Fed. Reg. 71378, 71398
(Dec. 8, 2006)].
A resident physician who is authorized by state law and the
hospital’s residency program to practice as a physician can
carry out functions reserved for a physician or LIP by the
CMS regulation. A medical student is not an LIP.
Patient or Family Request
A request from a patient or family member for the
application of a restraint is not a sufficient basis for the
use of a restraint intervention. A patient or family member
request for a restraint intervention should prompt an
assessment to determine whether such a restraint
intervention is needed.
WHEN ORDER MUST BE OBTAINED
If possible, the physician or other LIP responsible for the
care of the patient should order the restraint or seclusion
prior to its application. In some situations, however, the

Chapter 5 — Restraints and Seclusion CHA
5.13
©CALIFORNIA HOSPITAL ASSOCIATION
need for restraint or seclusion may occur so quickly that
an order cannot be obtained prior to the application of
restraint or seclusion. In these emergency situations,
the Interpretive Guidelines state that the order must be
obtained either during the emergency application of the
restraint or seclusion, or immediately (within a few minutes)
after the restraint or seclusion has been applied. The
failure to immediately obtain an order is viewed by CMS as
the application of restraint or seclusion without an order.
The hospital should address this process in its restraint
and seclusion policies and procedures. The policies and
procedures should specify who can initiate the emergency
application of restraint or seclusion prior to obtaining an
order from a physician or other LIP.
PROTOCOL, STANDING ORDERS, AND PRN ORDERS
Protocol
A protocol cannot serve as a substitute for obtaining
a physician’s or other LIP’s order prior to restraint or
seclusion. If a hospital uses protocols that include the
use of restraint or seclusion, a specific physician or LIP
order is still required for each episode of restraint or
seclusion. CMS states that the philosophy that serves as
a foundation for its regulation is that restraint or seclusion
use is an exceptional event, not a routine response to a
certain patient condition or behavior. Each patient must be
assessed, and interventions should be tailored to meet the
individual patient’s needs. The creation of a protocol can
run counter to this philosophy if it sets up the expectation
that restraint or seclusion will be used as a routine part of
care. The use of restraint or seclusion is a last resort when
less restrictive measures have been determined ineffective
to ensure the safety of the patient, staff or others; it should
not be a standard response to a behavior or patient need.
However, protocols are not banned by the regulation. A
protocol may contain information that is helpful for staff,
such as how a restraint is to be applied and monitored.
Typically, a hospital will develop an emergency protocol
approved by the medical staff to be used in emergency
situations in a manner consistent with the regulations. As
mentioned above, however, a protocol cannot serve as
a substitute for obtaining a physician or LIP order before
initiating each episode of restraint or seclusion. [64 Fed.
Reg. 36070, 36083 (July 2, 1999); 71 Fed. Reg. 71378,
71395 (Dec. 8, 2006)]
When implementing a protocol that includes restraint
or seclusion, the patient’s medical record must include
documentation of an individualized patient assessment
indicating that the patient’s symptoms and diagnosis meet
the use-triggering criteria listed in the protocol. Hospitals
that utilize protocols involving restraint or seclusion are
expected to provide evidence that the medical staff has
been involved in the development, review, and quality
monitoring of their use. [71 Fed. Reg. 71378, 71396 (Dec.
8, 2006)]
Standing or PRN Orders
Standing orders or PRN orders are not permitted. Each
episode of restraint or seclusion must be initiated in
accordance with the order of a physician or other LIP. If a
patient was recently released from restraint or seclusion,
and exhibits behavior that can be handled only through
the reapplication of restraint or seclusion, a new order is
required. Staff cannot discontinue a restraint or seclusion,
and then re-start it under the same order. This would
constitute a PRN order. A “trial release” constitutes a PRN
use, and therefore is not permitted.
A temporary, directly-supervised release that occurs for the
purpose of caring for a patient’s needs (such as toileting,
feeding, or range-of-motion exercises) is not considered a
discontinuation of the restraint or seclusion. As long as the
patient remains under direct staff supervision, the restraint
is not considered to be discontinued because the staff
member is present and serving the same purpose as the
restraint or seclusion.
The use of PRN orders for drugs is prohibited only when a
drug is being used as a restraint.
Exceptions
1. Geri-chair. If a patient requires a Geri-chair with the
tray locked to be safely out of bed, a standing or PRN
order is permitted.
2. Raised side rails. If a patient requires that all bedrails
be raised (restraint) while in bed, a standing or PRN
order is permitted.
3. Repetitive self-mutilating behavior. If a patient
is diagnosed with a chronic medical or psychiatric
condition, such as Lesch-Nyham Syndrome, and the
patient engages in repetitive self-mutilating behavior,
a standing or PRN order for restraint to be applied in
accordance with specific parameters established in the
treatment plan is permitted.
SURVEY PROCEDURES
The Interpretive Guidelines direct surveyors to consider
the following:
1. Review hospital policies and medical staff bylaws to
ascertain clinical practice guidelines that describe the
responsibilities of medical staff and clinicians who are
privileged to order restraint and seclusion.

CHA Mental Health Law Manual 2019
5.14
©CALIFORNIA HOSPITAL ASSOCIATION
2. Do the hospital’s written policies identify what
categories of practitioners the state recognizes as an
LIP or as having the authority to order restraint and
seclusion?
3. Does the hospital have written policies indicating
which practitioners are permitted to order restraint or
seclusion in the facility?
4. Do the hospital’s written policies conform to state law?
5. Does the hospital have established policies for who
can initiate restraint or seclusion?
6. Does the hospital utilize protocols for the use of
restraint or seclusion? If so, is the use of protocols
consistent with the requirements of the regulation?
7. Do the medical records reviewed identify the physician
or LIP who ordered each use of restraint or seclusion?
8. During the medical record review, verify that a
physician or LIP order was obtained prior to the
initiation of restraint or seclusion. When emergency
application of restraint or seclusion was necessary,
verify that a physician or LIP order was obtained
immediately (within a few minutes) after application of
the restraint or seclusion.
9. Review a random sample of medical records for
patients that have been restrained or secluded. Review
orders, progress notes, flow sheets, and nursing notes
to:
a. Verify that there is a physician or other LIP order
for each episode of restraint or seclusion;
b. Evaluate patterns of use and verify that orders
were obtained when necessary;
c. Verify that the documentation specifically
addresses the patients’ behaviors or
symptoms; and
d. Determine if restraint or seclusion is being
improperly implemented on a PRN basis.
10. Interview staff to determine if actual practice
is consistent with written hospital policies and
procedures.
B. California Law
Title 22 regulations applicable to psychiatric units of general
acute care hospitals and to acute psychiatric hospitals
state that patients may be placed in restraint “only on the
written order of a licensed health care practitioner acting
within the scope of his or her professional licensure.” This
order must include the reason for the restraint and the type
of restraint to be used. Because the Title 22 definitions of
a restraint include seclusion, an order from the LIP is also
required for seclusion.
However, “in a clear case of emergency,” a patient may be
placed in restraint at the discretion of a registered nurse
and a verbal or written order obtained thereafter. A verbal
order must be recorded in the patient’s medical record and
signed by the LIP on his or her next visit.
[Title 22, California Code of Regulations, Sections 70059,
70577(j)(2), 71055 and 71545(b)]
A drug used as a restraint requires a physician order.
Whereas California law clearly permits physicians to order
restraint and seclusion, the law regarding the ability of
licensed psychologists to order restraint and seclusion
in general acute care hospitals and in acute psychiatric
hospitals was less clear until recently. Prior to April 2, 2010,
Title 22 regulations applicable to psychiatric units of general
acute care hospitals and to acute psychiatric hospitals
required that patients be placed in restraint only on the
written order of a physician [Title 22, California Code of
Regulations, Sections 70577(j)(2) and 71545]. However,
effective April 2, 2010, the California Department of Public
Health (CDPH) replaced the word “physician” with “licensed
health care practitioner acting within the scope of his or
her professional licensure” in approximately 99 places
throughout the Title 22 health facility licensing regulations.
CDPH made these changes as an acknowledgment that it
is not CDPH’s role to determine scope of practice — this is
the role of professional licensing boards.
In an issue paper adopted on Jan. 6, 1994, the California
Board of Psychology stated:
The ordering of restraints and seclusion is within the
authorized scope of practice of a licensed psychologist,
provided such order is performed within the field of
competence of the psychologist as established by his or
her education, training and experience.
Hospitals with questions or concerns about the scope
of practice of psychologists should consider the
nondiscrimination requirements of Health and Safety Code
Section 1316.5(b)(2), and consult their legal counsel.
VIII. FACE-TO-FACE EVALUATION
A. Federal Law: CMS Conditions of Participation
and Interpretive Guidelines
When restraint or seclusion is used for the management
of violent or self-destructive behavior that jeopardizes the

Chapter 5 — Restraints and Seclusion CHA
5.15
©CALIFORNIA HOSPITAL ASSOCIATION
immediate physical safety of the patient, a staff member, or
others, the patient must be seen face-to-face within one
hour after the initiation of the intervention:
1. By a physician or other LIP; or
2. By a registered nurse or physician assistant
who has been trained in accordance with the
requirements described in XVIII.“Staff Training
Requirements,”page5.27.
[42 C.F.R. Section 482.13(e)(12)]
This requirement also applies when a drug is used as a
restraint to manage violent or self-destructive behavior.
The one-hour face-to-face evaluation must be conducted
by a physician, other LIP, registered nurse or physician
assistant. CMS states that the practitioner who conducts
this evaluation must be able to complete both a physical
and behavioral assessment of the patient in accordance
with state law, his or her scope of practice, and hospital
policy. Generally, practitioners such as social workers,
psychologists and other mental health workers are not
qualified to conduct a physical assessment, nor is it in
their scope of practice. [71 Fed. Reg. 71378, 71411
(Dec. 8, 2006)]
The evaluation must be conducted in person. A telephone
call or telemedicine methodology is not permitted.
If a patient’s violent or self-destructive behavior resolves
and the restraint or seclusion intervention is discontinued
before the practitioner arrives to perform the one-hour
face-to-face evaluation, the practitioner is still required to
see the patient face-to-face and conduct the evaluation
within one hour after the initiation of this intervention.
The fact that the patient’s behavior warranted the use
of a restraint or seclusion indicates a serious medical or
psychological need for prompt evaluation of the patient
behavior that led to the intervention. The evaluation
would also determine whether there is a continued need
for the intervention, factors that may have contributed to
the violent or self-destructive behavior, and whether the
intervention was appropriate to address the violent or
self-destructive behavior.
EXCEPTION
If a patient is diagnosed with a chronic medical or
psychiatric condition, such as Lesch-Nyham Syndrome,
and the patient engages in repetitive self-mutilating
behavior, a one-hour face-to-face evaluation is not required.
CONTENT OF THE EVALUATION
The physician, LIP, registered nurse, or physician assistant
must evaluate:
1. The patient’s immediate situation;
2. The patient’s reaction to the intervention;
3. The patient’s medical and behavioral condition; and
4. The need to continue or terminate the restraint
or seclusion.
The one-hour face-to-face evaluation includes both a
physical and behavioral assessment of the patient that
must be conducted by a qualified practitioner within the
scope of their practice. An evaluation of the patient’s
medical condition would include a complete review of
systems assessment, behavioral assessment, as well as
review and assessment of the patient’s history, drugs and
medications, most recent lab results, etc. The purpose is to
complete a comprehensive review of the patient’s condition
to determine if other factors, such as drug or medication
interactions, electrolyte imbalances, hypoxia, sepsis, etc.,
are contributing to the patient’s violent or self-destructive
behavior.
Training for a registered nurse (RN) or physician assistant
(PA) to conduct the one-hour face-to-face evaluation
would include all of the training requirements described in
XVIII.“Staff Training Requirements,”page5.27, including
content to evaluate the patient’s immediate situation,
the patient’s reaction to the intervention, the patient’s
medical and behavioral condition (documented training in
conducting physical and behavioral assessment); and the
need to continue or terminate the restraint or seclusion.
CONSULTATION WITH ATTENDING PHYSICIAN OR
OTHER LIP
If the face-to-face evaluation is conducted by a registered
nurse or physician assistant, the registered nurse or
physician assistant must consult the attending physician
or other LIP who is responsible for the care of the patient
under 42 C.F.R. Section 482.12 as soon as possible after
completing the evaluation. Hospital policy should address
the expected time frame for, and the components of, the
consultation.
This consultation should include, at a minimum,
the following:
1. A discussion of the findings of the one-hour
face-to-face evaluation.
2. The need for other interventions or treatments.

CHA Mental Health Law Manual 2019
5.16
©CALIFORNIA HOSPITAL ASSOCIATION
3. The need to continue or discontinue the use of restraint
or seclusion.
The consultation must be conducted prior to a renewal
of the order. Otherwise, CMS considers that the timing
of the consultation is not consistent with the “as soon as
possible” requirements.
SURVEY PROCEDURES
The Interpretive Guidelines direct surveyors to consider
the following:
1. Review the hospital policy regarding the one-hour
face-to-face evaluation.
2. What categories of practitioners does the hospital
policy authorize to conduct the one-hour face-to-face
evaluation?
3. Interview staff to determine if practice is consistent
with hospital policy.
4. Was the one-hour face-to-face evaluation conducted
by a practitioner authorized by hospital policy in
accordance with state law to conduct this evaluation?
5. If the one-hour face-to-face evaluations are conducted
by RNs who are not advanced practice nurses (APN),
verify that those RNs have documented training
that demonstrates they are qualified to conduct a
physical and behavioral assessment of the patient
that addresses: the patient’s immediate situation, the
patient’s reaction to the intervention, the patient’s
medical and behavioral condition, and the need to
continue or terminate the restraint or seclusion.
6. Does documentation of the one-hour face-to-face
evaluation in the patient’s medical record include all the
listed elements of this requirement?
7. Did the evaluation indicate whether changes in the
patient’s care were required, and, if so, were the
changes made?
8. Review the hospital restraint and seclusion policy
regarding consultation with the physician or other
LIP after a face-to-face evaluation conducted by a
registered nurse or physician assistant.
9. Does the hospital policy clarify expectations regarding
the requirement, “as soon as possible?”
10. Does documentation in the patient’s medical record
indicate consultation with the attending physician or
other LIP when the one-hour face-to-face evaluation
was conducted by a trained RN or PA?
11. Is practice consistent with hospital policy and
state law?
B. California Law
California law contains no specific requirements regarding a
face-to-face evaluation. Hospitals should follow federal law.
IX. NOTIFICATION OF ATTENDING PHYSICIAN
A. Federal Law: CMS Conditions of Participation
and Interpretive Guidelines
The attending physician must be consulted as soon
as possible if the attending physician did not order the
restraint or seclusion. This consultation may occur
via telephone.
Hospital medical staff policies determine who is considered
the attending physician. Medicare permits the attending
“physician” to be an LIP (physician, dentist, podiatrist,
chiropractor, or clinical psychologist), if permitted by state
law and hospital policy. The intent of this requirement is to
ensure that the practitioner who has overall responsibility
and authority for the management and care of the patient is
aware of the patient’s condition and is aware of the restraint
or seclusion intervention. When the attending physician is
unavailable, responsibility for the patient must be delegated
to another practitioner, who would then be considered the
attending physician. [Interpretive Guidelines, Tag A-0170]
Hospital policies should address the definition of “as
soon as possible” based on the needs of their particular
patient population.
SURVEY PROCEDURES
The Interpretive Guidelines direct surveyors to consider
the following:
1. Review the patient’s medical record for documentation
that the attending physician was notified immediately
if the attending physician did not order the restraint
or seclusion. Was the attending physician notified “as
soon as possible?”
2. Review the hospital’s policies and procedures
regarding consultation with the attending physician if
the attending physician did not order the restraint or
seclusion.

Chapter 5 — Restraints and Seclusion CHA
5.17
©CALIFORNIA HOSPITAL ASSOCIATION
B. California Law
California law contains no specific requirements regarding
notification of the attending physician. Hospitals should
follow federal law.
X. LIMITS ON LENGTH OF TIME THAT ORDERS
FOR RESTRAINT/SECLUSION ARE VALID
A. Federal Law: CMS Conditions of Participation
and Interpretive Guidelines
ORIGINAL ORDER
Restraint or seclusion used for the management of violent
or self-destructive behavior that jeopardizes the immediate
physical safety of the patient, a staff member, or others
may be ordered only in accordance with the following limits,
for up to a total of 24 hours:
1. Adults 18 years of age or older: 4 hours
2. Children and adolescents 9 to 17 years of age: 2 hours
3. Children under 9 years of age: 1 hour
[42 C.F.R. Section 482.13(e)(8)]
The physician or other LIP may write the order for a
shorter length of time. The requirement that restraint
use be ended at the earliest possible time applies to all
uses of restraint (see XI.“Discontinuation of Restraint or
Seclusion,”page5.18).
These limited time frames apply regardless of whether
each order is considered a separate, distinct, original
order, or whether an order is considered a continuation or
renewal of the original order. [71 Fed. Reg. 71378, 71413
(Dec. 8, 2006)]
RENEWAL OF ORDER
At the end of the time frame, if the continued use of
restraint or seclusion to manage violent or self-destructive
behavior is necessary based on an individualized patient
assessment, another order is required. When the original
order is about to expire, the RN must contact the physician
or other LIP, report the results of the most recent patient
assessment and request that the original order be renewed
(not to exceed the time limits described above). Whether
or not an onsite assessment is necessary prior to renewing
the order is left to the discretion of the physician or other
LIP in conjunction with a discussion with the RN who
is overseeing the care of the patient. Another one-hour
face-to-face patient evaluation is not required when the
original order is renewed.
When the physician or other LIP renews an order or
writes a new order authorizing the continued use of
restraint or seclusion, there must be documentation in
the patient’s medical record that describes the findings of
the physician’s or other LIP’s re-evaluation supporting the
continued use of restraint or seclusion.
RENEWAL OF ORDER 24 HOURS AFTER ORIGINAL
ORDER
If a patient remains in restraint or seclusion for the
management of violent or self-destructive behavior 24
hours after the original order, the physician or other LIP
who is responsible for the care of the patient must see
and assess the patient before writing a new order for the
continued use of restraint or seclusion [42 C.F.R. Section
482.13(e)(8)]. This assessment must be done in person.
CMS views 24 hours of restraint or seclusion for the
management of violent or self-destructive behavior to be
an extreme measure with potential for serious harm to the
patient, and so requires the patient to be seen in person at
least every 24 hours.
EXCEPTIONS
Repetitive Self-Mutilating Behavior
If a patient is diagnosed with a chronic medical or
psychiatric condition, such as Lesch-Nyham Syndrome,
and the patient engages in repetitive self-mutilating
behavior, a standing or PRN order for restraint to be
applied in accordance with specific parameters established
in the treatment plan is permitted. Since the use of
restraints to prevent self-injury is needed for these types
of rare, severe, medical and psychiatric conditions, the
requirements regarding time-limited orders and evaluation
every 24 hours before renewal of the order for the
management of violent or self-destructive behavior do not
apply.
Nonviolent or Non-Self-Destructive Patient
Renewal of an order for restraint used to ensure the
physical safety of a nonviolent or non-self-destructive
patient does not need to meet the above requirements.
(This use of restraints is more typically found in medical/
surgical and skilled nursing settings than in the mental
health setting.) These orders may be renewed as
authorized by hospital policy. Hospitals have the flexibility
to determine time frames for the renewal of orders for
restraint of nonviolent, non-self-destructive patients. These
time frames should be addressed in hospital policies and
procedures. (However, the requirement that restraint use
be ended at the earliest possible time applies to all uses of
restraint.)

CHA Mental Health Law Manual 2019
5.18
©CALIFORNIA HOSPITAL ASSOCIATION
SURVEY PROCEDURES
The Interpretive Guidelines direct surveyors to consider
the following:
1. When restraint or seclusion is used to manage violent
or self-destructive behavior, do orders contain the
appropriate time frames based on the patient’s age?
Does the total number of hours covered by an order or
its renewal exceed 24 hours?
2. If more restrictive state laws apply, are they being
followed? (NOTE: California does not have more
restrictive laws.)
3. Is the renewal order for restraint or seclusion based on
a comprehensive individual patient assessment?
4. Is there evidence in the patient’s medical record that
the symptoms necessitating the continued use of
restraint or seclusion have persisted?
5. If restraint or seclusion is used to manage violent or
self-destructive behavior for longer than 24 hours, is
there documentation of a new written order, patient
assessments, and a re-evaluation by a physician
or other LIP in the medical record? Does the
documentation provide sufficient evidence to support
the need to continue the use of restraint or seclusion?
Is there evidence in the medical record that the
symptoms necessitating the continued use of restraint
or seclusion have persisted?
6. Does the patient’s plan of care address the use of
restraint or seclusion?
7. What is the patient’s documented clinical response to
the continued need for restraint or seclusion?
8. Review the hospital policy on renewal of restraint
orders for the management of nonviolent,
non-self-destructive patient behavior.
9. Interview staff and review the medical record
documentation to ensure that practice is consistent
with the hospital policy.
B. California Law
California law contains no specific requirements regarding
time limitations of orders for restraint and seclusion.
Hospitals should follow federal law.
XI. DISCONTINUATION OF RESTRAINT OR
SECLUSION
A. Federal Law: CMS Conditions of Participation
and Interpretive Guidelines
Restraint or seclusion must be discontinued at the earliest
possible time, regardless of the length of time identified in
the order [42 C.F.R. Section 482.13(e)(9)].
Restraint or seclusion may be employed only while the
unsafe situation continues. Once it ends, the restraint
or seclusion must be discontinued. Staff members are
expected to assess and monitor the patient’s condition
on an ongoing basis to determine whether restraint or
seclusion can safely be discontinued to ensure that the
patient is released from restraint or seclusion at the earliest
possible time. The decision to discontinue the intervention
should be based on the determination that the need for
restraint or seclusion is no longer present, or that the
patient’s needs may be addressed using less restrictive
methods.
A hospital’s policies and procedures should address, at
a minimum:
1. Categories of staff that the hospital authorizes to
discontinue restraint or seclusion in accordance with
state law (described below); and
2. The circumstances under which restraint or seclusion is
to be discontinued.
SURVEY PROCEDURES
The Interpretive Guidelines direct surveyors to consider
the following:
1. Does the hospital have policies and procedures for
ending restraint or seclusion? Do they address, at a
minimum:
a. Who has the authority to discontinue the use of
restraint or seclusion (based on state law and
hospital policies); and
b. Circumstances under which restraint or seclusion
should be discontinued?
2. Do the policies include a requirement to end the
restraint or seclusion as soon as is safely possible?
3. Does the medical record contain evidence that the
decision to continue or discontinue the use of restraint
or seclusion was based on an assessment and
re-evaluation of the patient’s condition?

Chapter 5 — Restraints and Seclusion CHA
5.19
©CALIFORNIA HOSPITAL ASSOCIATION
4. Interview staff to determine whether they are
aware that use of a restraint or seclusion must be
discontinued as soon as is safely possible.
B. California Law
California law does not contain an explicit statement that
restraint or seclusion must be discontinued at the earliest
possible time. However, the California requirement that the
least restrictive alternative be employed, and the totality
of California requirements in general, capture the same
sentiment.
Registered nurses are permitted by California law to
discontinue restraint or seclusion.
XII. PATIENT MONITORING
Both state and federal law require that a patient in restraint
or seclusion be carefully monitored. Whereas the CoPs
permit the hospital some flexibility in determining the time
intervals between assessments, California law is much
stricter — patients must be observed every 15 minutes.
The federal law is described below, but California hospitals
are cautioned to follow the stricter state time frames
(described in B.“California Law,”page5.20).
A. Federal Law: CMS Conditions of Participation
and Interpretive Guidelines
The condition of the patient who is restrained or secluded
must be monitored by a physician, other LIP, or trained staff
at an interval determined by hospital policy in accordance
with state law.
CMS states that ongoing assessment and monitoring of
the patient’s condition by a physician, other LIP or trained
staff is crucial for prevention of patient injury or death, as
well as ensuring that the use of restraint or seclusion is
discontinued at the earliest possible time. Hospital policies
are expected to guide staff in determining appropriate
intervals for assessment and monitoring based on the
individual needs of the patient, the patient’s condition, and
the type of restraint or seclusion used. The selection of an
intervention and determination of the necessary frequency
of assessment and monitoring should be individualized,
taking into consideration variables such as the patient’s
condition, cognitive status, risks associated with the use
of the chosen intervention, and other relevant factors.
In some cases, checks every 15 minutes or vital signs
taken every 2 hours may not be sufficient to ensure the
patient’s safety. In others, it may be excessive or disruptive
to patient care (e.g., it may be unnecessary to mandate
that a patient with wrist restraints, and who is asleep, be
checked every 15 minutes and awakened every 2 hours
to take the patient’s vital signs). Similarly, depending on
the patient’s needs and situational factors, the use of
restraint or seclusion may require either periodic (e.g.,
every 15 minutes, every 30 minutes, etc.) or continual (i.e.,
moment-to-moment) monitoring and assessment.
Hospital policies should address:
1. Frequencies of monitoring and assessment;
2. Assessment content (e.g., vital signs, circulation
checks, hydration needs, elimination needs, level
of distress and agitation, mental status, cognitive
functioning, skin integrity, etc.);
3. Providing for nutritional needs, range of motion
exercises, and elimination needs; and
4. Mental status and neurological evaluations.
With the exception of the simultaneous use of restraint and
seclusion, one-to-one observation with a staff member
in constant attendance is not required unless deemed
necessary based on a practitioner’s clinical judgment. (See
XIV.“Simultaneous Restraint and Seclusion,”page5.20.)
For example, placing staff at the bedside of a patient with
wrist restraints may be unnecessary. However, for a more
restrictive or risky intervention and/or a patient who is
suicidal, self injurious, or combative, staff may determine
that continual face-to-face monitoring is needed. The
hospital is responsible for providing the level of monitoring
and frequency of reassessment that will protect the
patient’s safety.
Hospitals have flexibility in determining which staff performs
the patient assessment and monitoring. This determination
must be in accordance with the practitioner’s scope of
clinical practice and state law. For example, assessment
and monitoring are activities within a registered nurse’s
scope of practice. However, some trained, unlicensed staff
with demonstrated competency may perform components
of monitoring (e.g., checking the patient’s vital signs,
hydration and circulation; the patient’s level of distress and
agitation; or skin integrity), and may also provide for general
care needs (e.g., eating, hydration, toileting, and range of
motion exercises).
SURVEY PROCEDURES
The Interpretive Guidelines direct surveyors to consider
the following:
1. Review hospital policies regarding assessment and
monitoring of a patient in restraint or seclusion.

CHA Mental Health Law Manual 2019
5.20
©CALIFORNIA HOSPITAL ASSOCIATION
a. What evidence do you find that the hospital’s
monitoring policies are put into practice for all
restrained or secluded patients?
b. Do hospital policies identify which categories of
staff are responsible for assessing and monitoring
the patient?
c. Do hospital policies include time frames for
offering fluids and nourishment, toileting/
elimination, range of motion, exercise of limbs
and systematic release of restrained limbs? Is this
documented in the patient’s medical record?
2. Review patient medical records.
a. Was there a valid rationale for the decision
regarding the frequency of patient assessment and
monitoring documented in the medical record?
b. Was documentation consistent, relevant, and
reflective of the patient’s condition?
c. Are time frames described for how often a patient
is monitored for vital signs, respiratory and cardiac
status, and skin integrity checks?
d. Is there documentation of ongoing patient
monitoring and assessment (e.g., skin integrity,
circulation, respiration, intake and output, hygiene,
injury, etc.)?
e. Is the patient’s mental status assessed? Is this
documented in the medical record?
f. Is the patient assessed regarding continued need
for the use of seclusion or restraint?
g. Is there adequate justification for continued use
and is this documented?
h. Is the level of supervision appropriate to meet the
safety needs of the patient who is at a higher risk
for injury (e.g., self-injurious, suicidal)?
B. California Law
Title 22 regulations applicable to psychiatric units of general
acute care hospitals and to acute psychiatric hospitals
require that “patients in restraint by seclusion or mechanical
means shall be observed at intervals not greater than
15 minutes” [Title 22, California Code of Regulations,
Sections 70577(j)(3) and 71545(c)]. State law does not
specify any particular actions a hospital must take when
making the required observations.
XIII. EMERGENCY SITUATIONS
A. Federal Law: CMS Conditions of Participation
and Interpretive Guidelines
Federal law does not contain any special language
regarding emergency situations. All of the federal
requirements should be complied with regardless of
whether the situation is considered an “emergency” or not.
B. California Law
A health facility may use seclusion or behavioral restraints
for behavioral emergencies only when a patient’s behavior
presents an imminent danger of serious harm to self or
others [Health and Safety Code Section 1180.4(b)].
There is no definition in this law for “behavioral
emergencies,” “imminent danger,” or “serious harm.”
This requirement applies to all facilities. For general acute
care hospitals, this requirement applies only to patients
admitted to the psychiatric unit, if the hospital has one. It
does not apply to mental health patients in the emergency
department, an intensive care unit, or other locations within
the hospital [Health and Safety Code Sections 1180.3
and 1180.4]. However, the federal regulation requires that
restraint or seclusion be used only when less restrictive
interventions have been determined to be ineffective
to protect the patient, a staff member, or others from
harm. Therefore, as a matter of practicality, hospitals in
compliance with the federal regulation will be in compliance
with this state requirement throughout the facility.
XIV. SIMULTANEOUS RESTRAINT AND
SECLUSION
At times a patient may be in restraint and in seclusion
at the same time. If so, all requirements applicable to
restraints and all requirements applicable to seclusion must
be followed. In addition, the requirements described below
must be met.
A. Federal Law: CMS Conditions of Participation
and Interpretive Guidelines
Simultaneous restraint and seclusion is permitted only if the
patient is continually monitored:
1. Face-to-face by an assigned, trained staff member; or

Chapter 5 — Restraints and Seclusion CHA
5.21
©CALIFORNIA HOSPITAL ASSOCIATION
2. By trained staff using both video and audio equipment.
This monitoring must be in close proximity to the
patient.
[42 C.F.R. Section 482.13(e)(15)]
For the purposes of this requirement, “continually” means
ongoing without interruption.
A patient who is physically restrained alone in his or her
room is not necessarily being simultaneously secluded.
The question to ask is whether the patient would be able
to leave the room if he or she were not being physically
restrained. If so, then the patient is not also being secluded.
However, if the physical restraint was removed and the
patient was still unable to leave the room because the door
was locked or staff otherwise physically preventing the
patient from leaving, then the patient is also being secluded.
DOCUMENTATION
When the simultaneous use of restraint and seclusion is
employed, there must be adequate documentation that
justifies the decision for simultaneous use.
PATIENT MONITORING AND ASSESSMENT
The use of video and audio equipment does not eliminate
the need for frequent monitoring and assessment of the
patient.
SURVEY PROCEDURES
The Interpretive Guidelines direct surveyors to consider
the following:
1. Review the hospital’s policy regarding simultaneous
use of restraint and seclusion to determine whether it
provides for continual monitoring and complies with all
other requirements regarding restraint and seclusion.
2. Conduct document review and staff interviews to
determine if practice is consistent with the hospital
policy and required uninterrupted audio and visual
monitoring is provided as required.
3. Is the staff member monitoring the patient with video
and audio equipment trained and in close proximity
to ensure prompt emergency intervention if a problem
arises?
4. Does the video equipment cover all areas of the room
or location where the patient is restrained or secluded?
5. Is the audio and video equipment located in an area
that assures patient privacy?
6. Is the equipment appropriately maintained and in
working condition?
B. California Law
California law is somewhat stricter than federal law with
respect to patient observation requirements when a patient
is simultaneously restrained and secluded.
FACE-TO-FACE OBSERVATION
California law requires that a patient who is in seclusion and
in any type of behavioral restraint at the same time must be
kept under constant, face-to-face human observation.
Observation by means of video camera may be used only
in facilities that were permitted to use video monitoring
under federal regulations specific to that facility when
this law became effective (Jan. 1, 2004). Facilities should
consult their legal counsel if in doubt as to whether this
provision applies to them.
[Health and Safety Code Section 1180.4(i)]
This California requirement applies to all health facilities.
However, for general acute care hospitals, this requirement
applies only to patients admitted to the psychiatric unit, if
the hospital has one. It does not apply to mental health
patients in the emergency department, an intensive care
unit, or other locations within the hospital [Health and
Safety Code Sections 1180.3 and 1180.4]. However, a
hospital may wish to consider following this requirement
with respect to all patients who are in simultaneous restraint
and seclusion.
XV. PROHIBITED TECHNIQUES
A. Federal Law: CMS Conditions of Participation
and Interpretive Guidelines
The CMS CoP and Interpretive Guidelines do not specify
any prohibited techniques. However, CMS requires
that the use of restraint or seclusion be implemented
in accordance with safe and appropriate restraint and
seclusion techniques as determined by hospital policy in
accordance with state law. California law does prohibit
some techniques.
B. California Law
California law prohibits specific restraint techniques.
Some of these techniques are prohibited for all patients.
Other techniques are prohibited only for specified types
of patients. These prohibitions are described in the
following sections.

CHA Mental Health Law Manual 2019
5.22
©CALIFORNIA HOSPITAL ASSOCIATION
TECHNIQUES THAT ARE PROHIBITED FOR ALL
PATIENTS
A health facility may not do any of the following:
1. Use a physical restraint or containment technique that
obstructs a patient’s respiratory airway or impairs the
patient’s breathing or respiratory capacity, including
a technique in which a staff member places pressure
on a patient’s back or places his or her body weight
against the patient’s torso or back [Health and Safety
Code Section 1180.4(c)(1)].
2. Use a pillow, blanket, or other item to cover a patient’s
face as part of a physical or mechanical restraint or
containment process [Health and Safety Code Section
1180.4(c)(2)].
3. Place a patient in a facedown “prone” position with the
patient’s hands held or restrained behind the patient’s
back [Health and Safety Code Section 1180.4(g)].
4. Use physical or mechanical restraint or containment
on a patient who has a known medical or physical
condition and there is reason to believe that the
use would endanger the patient’s life or seriously
exacerbate the patient’s medical condition [Health and
Safety Code Section 1180.4(d)].
5. Use physical restraint or containment as an extended
procedure [Health and Safety Code Section 1180.4(h)].
TECHNIQUES THAT ARE PROHIBITED FOR SPECIFIED
PATIENTS
A health facility may not use prone (facedown) mechanical
restraint on a person at risk for positional asphyxiation as a
result of one of the following risk factors, if the risk factor(s)
is known to the health care provider:
1. Obesity
2. Pregnancy
3. Agitated delirium or excited delirium syndromes
4. Cocaine, methamphetamine, or alcohol intoxication
5. Exposure to pepper spray
6. Preexisting heart disease, including, but not limited to,
an enlarged heart or other cardiovascular disorders
7. Respiratory conditions, including emphysema,
bronchitis, or asthma
[Health and Safety Code Section 1180.4(e)(1)]
However, this prohibition regarding prone mechanical
restraint does not apply in the following situations:
1. When the patient has stated a preference for the prone
position. The patient might have stated this preference
during the initial intake assessment (in which case it
should be carefully documented) or later when the use
of restraint is taking place.
2. When the physician judges other clinical risks to take
precedence.
In both of the above situations, a physician must provide
“written authorization.” This written authorization —
presumably a physician order — may not be a standing
order, and must be evaluated on a case-by-case basis by
the physician. [Health and Safety Code Section 1180.4(e)
(2)]
PRONE CONTAINMENT TECHNIQUES
A health facility must avoid the deliberate use of prone
containment techniques whenever possible, using the
best practices in early intervention techniques, such as
de-escalation. If prone containment techniques are used
in an emergency situation, a staff member must observe
the patient for any signs of physical duress throughout the
use of prone containment. Whenever possible, the staff
member observing the patient should not be involved in
restraining the patient. [Health and Safety Code Section
1180.4(f)]
APPLICABILITY
The prohibitions described above apply to all facilities.
However, for general acute care hospitals, the prohibitions
apply only to patients admitted to the psychiatric unit, if
the hospital has one. They do not apply to mental health
patients in the emergency department, an intensive care
unit, or other locations within the hospital [Health and
Safety Code Sections 1180.3 and 1180.4]. However, a
hospital may wish to adopt these prohibitions throughout
its facility.
XVI. POST-RESTRAINT OR SECLUSION
REVIEW (CLINICAL/QUALITY REVIEW AND
DEBRIEFING)
A. Federal Law: CMS Conditions of Participation
and Interpretive Guidelines
The CMS CoP and Interpretive Guidelines do not specify
any required clinical/quality reviews or debriefings after the
use of restraint or seclusion. However, California law does
contain such requirements.

Chapter 5 — Restraints and Seclusion CHA
5.23
©CALIFORNIA HOSPITAL ASSOCIATION
B. California Law
A health facility must conduct two reviews for each episode
of the use of seclusion or behavioral restraint: a clinical/
quality review and a debriefing. The requirements for each
type of review are discussed below.
The review requirements apply to all facilities. However, for
general acute care hospitals, they apply only to patients
admitted to the psychiatric unit, if the hospital has
one. They do not apply to mental health patients in the
emergency department, an intensive care unit, or other
locations within the hospital [Health and Safety Code
Sections 1180.3 and 1180.5]. However, a facility may wish
to conduct these reviews on all mental health patients
who experience an episode of the use of seclusion or
behavioral restraint.
If an adverse event or adverse outcome occurs while a
patient is in seclusion or restraint, the hospital should
follow its adverse event/sentinel event/root cause analysis
policy in addition to conducting the two types of reviews
described in this section.
CLINICAL AND QUALITY REVIEW
A health facility must conduct a clinical and quality review
for each episode of the use of seclusion or behavioral
restraints [Health and Safety Code Section 1180.5(a)]. The
law does not specify which types of professionals in the
facility must conduct this review nor what information
must be considered. A health facility may choose to have
a special committee to review restraint and seclusion use,
or may assign this function to a more general medical
staff quality assurance committee. In order to protect
the documents and deliberations of the committee from
discovery (including subpoena) under the “peer review”
confidentiality provision of Evidence Code Section 1157,
the committee should be formed under the auspices of the
medical staff quality assurance program. (See chapter 8 for
more information about protecting peer review and quality
assurance information from discovery.)
DEBRIEFING
In addition, a health facility must conduct a debriefing
regarding each episode of the use of seclusion or
behavioral restraints. This debriefing must take place as
quickly as possible, but no later than 24 hours after the use
of seclusion or behavioral restraints.
Who Must be Included in the Debriefing
1. The patient’s participation is voluntary. The facility
should encourage the patient to participate in the
debriefing, but may not require the patient to do so.
If the patient chooses not to participate, the hospital
should document both its encouragement and the
refusal.
2. The staff members involved in the incident, if
reasonably available.
3. A supervisor.
4. If the patient requests it, someone the patient desires
to be present, such as a family member or other
person designated by the patient, should be included
(if the desired family member or other person can be
present at the time of the debriefing at no cost to the
facility).
The Purpose and Elements of the Debriefing
The purpose of the debriefing is to do all of the following:
1. Assist the patient to identify the precipitant of the
incident, and suggest methods of more safely and
constructively responding to the incident.
2. Assist the staff to understand the precipitants to the
incident, and to develop alternative methods of helping
the patient avoid or cope with those incidents.
3. Help treatment team staff devise treatment
interventions to address the root cause of the
incident and its consequences, and to modify the
treatment plan.
4. Help assess whether the intervention was necessary
and whether it was implemented in a manner
consistent with staff training and facility policies.
In the debriefing, the health facility must provide the patient
and the staff the opportunity to discuss the following:
1. The circumstances resulting in the use of seclusion or
behavioral restraints; and
2. Strategies to be used by the staff, the patient, or
others that could prevent the future use of seclusion or
behavioral restraints.
[Health and Safety Code Section 1180.5(b) and (c)]
Documentation Requirements Regarding the Debriefing
The law explicitly requires that the health facility document
in the patient’s medical records that the debriefing session
took place and any changes to the patient’s treatment
plan that resulted from the debriefing [Health and Safety

CHA Mental Health Law Manual 2019
5.24
©CALIFORNIA HOSPITAL ASSOCIATION
Code Section 1180.5(d)]. In addition, health facilities
should consider documenting the date and time of the
debriefing, the participants in the debriefing, whether the
patient wanted to participate, whether the patient wanted
a third party to participate, and the fact that each element
described under “The Purpose and Elements of the
Debriefing,”page5.23, was addressed.
XVII. REPORTING REQUIREMENTS RELATED TO
RESTRAINT OR SECLUSION
There are several state and federal reporting requirements
potentially implicated when a patient is restrained or
secluded. These reporting requirements are described
below. One incident can easily lead to multiple reports
being required. The reporting requirements related to the
Safe Medical Devices Act, adverse event reporting, and
unusual occurrences should be reviewed and all necessary
reports should be made in the event of an adverse
event involving restraints or seclusion. In addition, the
requirements regarding sentinel events should be reviewed.
All of these requirements are described in chapter 8.
A. CMS Death Reporting and Documentation
Requirements
REPORTING REQUIREMENT
Hospitals must report the following deaths associated with
the use of seclusion or restraint to CMS by fax no later than
the close of business on the next business day following
knowledge of the patient’s death. (The CMS Regional
Office in California does not accept reports by email.) The
following events must be reported:
1. Each death that occurs while a patient is in restraint
or seclusion, except for deaths subject to the
“Documentation Requirement,”page5.24.
2. Each death that occurs within 24 hours after the
patient was removed from restraint or seclusion
(whether or not the hospital believes that the
use of restraint or seclusion contributed to the
patient’s death), except for deaths subject to the
“Documentation Requirement,”page5.24.
3. Each death known to the hospital that occurs
within one week after restraint or seclusion where
it is reasonable to assume that use of restraint or
seclusion contributed directly or indirectly to a patient’s
death, regardless of the type(s) of restraint used.
“Reasonable to assume” in this context includes,
but is not limited to, deaths related to restrictions of
movement for prolonged periods of time, or death
related to chest compression, restriction of breathing
or asphyxiation.
This requirement applies to deaths that occur in any unit of
the hospital, including an ICU or critical care unit. However,
critical access hospitals are required to report to CMS
only if they have a psychiatric or rehabilitative distinct part
unit. (Critical access hospitals may be required to report
an adverse event related to restraints or seclusion under
another reporting requirement described in this chapter.)
The date and time of the report to CMS must be
documented in the patient’s medical record.
[42 C.F.R. Section 482.13(g)]
REGIONAL OFFICE PHONE NUMBER/WORKSHEET
Hospitals must fax a report to CMS at the Regional
Office for Region IX at (443) 380-8909 to report deaths
associated with the use of seclusion or restraint. The
hospital must use Form CMS-10455, which is included
at the end of this manual as CHA Appendix MH 5-A.
Reporting by email is not acceptable to CMS.
Hospitals with questions about the reporting requirement
may contact Alex Garza or Rosanna Dominguez at:
Division of Survey and Certification
Centers for Medicare & Medicaid Services
90 7th Street, Suite 5-300 (5W)
San Francisco, CA 94103
(415) 744-3735
DOCUMENTATION REQUIREMENT
When no seclusion has been used and when the only
restraints used on the patient are those applied exclusively
to the patient’s wrist(s), and which are composed solely
of soft, non-rigid, cloth-like materials, the hospital staff
does not need to notify CMS of a patient death by the
next business day. Instead, hospital staff must record the
following information in an internal log or other system:
1. The patient’s name,
2. The patient’s date of birth,
3. The patient’s date of death,
4. The name of attending physician or other LIP who is
responsible for the care of the patient,
5. The patient’s medical records number, and
6. The patient’s primary diagnosis(es).
Each entry must be made not later than seven days after
the date of death. An entry must be made for:

Chapter 5 — Restraints and Seclusion CHA
5.25
©CALIFORNIA HOSPITAL ASSOCIATION
1. Any death that occurs while a patient is in restraints as
described above.
2. Any death that occurs within 24 hours after a patient
has been removed from restraints as described above.
The log or other system must be made available in either
written or electronic form to CMS immediately upon
request.
The date and time of the log entry must be documented in
the patient’s medical record.
CMS RESPONSE
CMS will use the information reported by the hospital to:
1. Authorize an onsite investigation (complaint survey)
of the hospital by CDPH, which is the state survey
agency for CMS, and
2. Inform the federally-mandated protection and
advocacy entity, which in California is Disability Rights
California (DRC). DRC’s role and responsibilities
are described in V.“Mental Health Advocacy
Programs,”page4.7.
SURVEY PROCEDURES
The Interpretive Guidelines direct surveyors to consider
the following:
1. Does the hospital have a death reporting policy that
addresses the requirements of the regulation?
2. Review data related to patient deaths while the
patients were in restraint or seclusion to determine if
the hospital followed the requirements related to death
reporting for:
a. Each death that occurred while the patient was
in restraints (whether physical or drugs used as a
restraint) or seclusion;
b. Each death that occurred within 24 hours after
the patient had been removed from restraint or
seclusion; and
c. Each death that occurred within one week after
restraint or seclusion where it is reasonable to
assume that the use of restraint or seclusion
contributed directly or indirectly to a patient’s
death.
3. Interview staff to determine their knowledge of the
hospital’s death reporting policy.
4. Is there evidence that deaths associated with the use
of restraints or seclusion are reported to CMS? Review
medical records of patients who died associated with
the use of restraint or seclusion to determine if the
documentation included the date and time the death
was reported to CMS.
B. FDA: Safe Medical Devices Act Reporting
Requirement
The Food and Drug Administration (FDA) regulates restraint
devices as it regulates other medical devices. Under the
Safe Medical Devices Act of 1990, hospitals and other
device user facilities must report incidents involving medical
devices (including restraints) that may have caused or
contributed to the serious injury or death of a patient.
For purposes of this reporting law, it should be noted that
the FDA uses a different definition of restraint than does the
CMS CoP or California law. The FDA defines a protective
restraint as:
a device, including but not limited to a wristlet, anklet,
vest, mitt, straight jacket, body/limb holder, or other type
of strap, that is intended for medical purposes and that
limits the patient’s movements to the extent necessary
for treatment, examination, or protection of the patient or
others. [21 C.F.R. Section 880.6760]
Whereas the CMS definition of restraint could include a
Geri-chair, a tray table, a side rail, a sheet, or even a staff
member holding a patient, the FDA definition does not.
Therefore, this reporting requirement is somewhat more
narrow than the other reporting requirements discussed
throughout XVII.“Reporting Requirements Related to
Restraint or Seclusion,”page5.24.
Detailed information regarding the Safe Medical Devices
Act of 1990 is found in IX.“Reports Under the Safe Medical
Devices Act of 1990,”page8.11.
C. Reporting Restraint and Seclusion to Local
Behavioral Health Director
When a patient is restrained or secluded, a denial of
rights is deemed to have occurred. (See F.“Denial of
Patient Rights,”page4.4, regarding required monthly
and quarterly reporting to the Department of Health Care
Services.)
D. California Adverse Event Reporting
Requirement
California law requires that 27 specified adverse events be
reported to CDPH within five days of detection. Most of
these events are unlikely to occur in the context of restraint

CHA Mental Health Law Manual 2019
5.26
©CALIFORNIA HOSPITAL ASSOCIATION
or seclusion. However, one of the specified adverse
events that must be reported is “a patient death or serious
disability associated with the use of restraints or bedrails
while being cared for in a health facility.”
In addition, the following adverse events could happen
while a patient is being restrained or secluded and would
be reportable:
1. A patient death or serious disability associated with a
medication error, including, but not limited to, an error
involving the wrong drug, the wrong dose, the wrong
patient, the wrong time, the wrong rate, the wrong
preparation, or the wrong route of administration,
excluding reasonable differences in clinical judgment
on drug selection and dose. This adverse event could
take place in the context of a drug used as a restraint.
2. A patient death associated with a fall while the
patient is being cared for in a health facility. If a
patient were to die as the result of a fall while in
seclusion or while being restrained, this adverse
event would be reportable under the adverse event
reporting requirement.
The details of the adverse event reporting requirement
are described in VII.“CDPH Adverse Events
Reporting,”page8.7.
E. Regional Centers for Persons with
Developmental Disabilities
State law requires specified facilities to report the
use of restraint and seclusion for clients of California
regional centers. Regional centers serve individuals
with developmental disabilities. The facilities that must
report are:
1. Acute psychiatric hospitals that are regional center
vendors (that is, the hospital contracts with one or
more California regional centers for persons with
developmental disabilities). Acute psychiatric hospitals
may wish to check with their contracts department
to determine whether the hospital is a regional
center vendor.
2. Long-term health care facilities that are required to
report to a regional center under Title 17, California
Code of Regulations, Section 54327. “Long-term
health care facilities include:
a. Skilled nursing facility.
b. Intermediate care facility.
c. Intermediate care facility/developmentally disabled.
d. Intermediate care facility/developmentally
disabled habilitative.
e. Intermediate care facility/developmentally
disabled-nursing.
f. Congregate living health facility.
g. Nursing facility.
h. Intermediate care facility/developmentally
disabled-continuous nursing.
i. Pediatric day health and respite care facility.
j. “Long-term health care facility” does not include
a general acute care hospital or an acute
psychiatric hospital, except for that distinct part
of the hospital that provides skilled nursing facility,
intermediate care facility, intermediate care facility/
developmentally disabled, or pediatric day health
and respite care facility services.
3. Regional center vendors that provide crisis or
residential services or supported living services.
General acute care hospitals may wish to check with
their contracts department to determine whether the
hospital is a regional center vendor of crisis services.
MONTHLY REPORTING
Each month, the facilities listed above must report to
the state-contracted protection and advocacy agency,
Disability Rights California, the following:
1. The number of incidents of seclusion and the duration
of time spent per incident in seclusion;
2. The number of incidents of the use of behavioral
restraints and the duration of time spent per incident of
restraint; and
3. The number of times an involuntary emergency
medication is used to control behavior.
These reports must include the name, street address, and
telephone number of the facility.
INCIDENT REPORTING
If a client of a California regional center dies or suffers a
serious injury during, or related to, the use of seclusion,
physical restraint, or chemical restraint, or any combination
thereof, a report must be made to the state-contracted
protection and advocacy agency, Disability Rights California.
The report must be made no later than the close of the
business day following the death or serious injury. The
report must include the encrypted identifier of the person
involved, and the name, street address, and telephone
number of the facility.

Chapter 5 — Restraints and Seclusion CHA
5.27
©CALIFORNIA HOSPITAL ASSOCIATION
DEFINITIONS
For purposes of this law, the following definitions apply.
“Physical restraint” means any behavioral or mechanical
restraint, as defined in B.“California Law,”page5.3.
“Chemical restraint” means a drug that is used to control
behavior and that is used in a manner not required to treat
the patient’s medical conditions.
“Seclusion” means involuntary confinement of a person
alone in a room or an area as defined in B.“California
Law,”page5.3.
F. Medication Error
The Board of Pharmacy has adopted regulations requiring
specified reports to be made if a medication error occurs
(including errors involving a drug used as a restraint). The
details of these reporting requirements are described in
VIII.“Medication Errors,”page8.11.
G. California Unusual Occurrence Reporting
Requirement
Title 22 requires general acute care hospitals and acute
psychiatric hospitals to report an unusual occurrence
which threatens the welfare, safety, or health of patients,
personnel, or visitors. In a letter to general acute care
hospitals and acute psychiatric hospitals (and others)
dated May 29, 2002, the California Department of Health
Services (DHS; now called the California Department of
Public Health (CDPH)) stated that a patient death that
occurs while a patient is restrained or in seclusion for
behavior management is a reportable unusual occurrence.
DHS stated that it is also a reportable unusual occurrence
when the use of restraint or seclusion for either behavior
management or for medical and surgical care may be a
cause or a contributing factor to a patient death or injury.
This report must be made to CDPH and to the local
health officer as soon as reasonably practicable by
telephone. The details of the unusual occurrence reporting
requirement are described in XI.“Reportable “Unusual
Occurrences”,”page8.14.
H. Staff Injury
If an employee is injured during the application of restraint
or seclusion, one or more reports may be required. CHA
has published a guidebook that details all reporting
requirements — to local law enforcement, to CDPH, and
to Cal/OSHA — that may be triggered when an employee
is injured by a patient. For more information about the
Healthcare Workplace Violence Prevention guidebook, or to
order, visit www.calhospital.org/wvp-guidebook.
I. TJC Sentinel Event Requirement
Under its policy on “sentinel events,” The Joint Commission
(TJC) asks hospitals to review all incidents that constitute
a sentinel event and, with some exceptions, to share
with TJC the results of this review (called a “root cause
analysis”). Hospitals are also expected to prepare action
plans to address any issues identified in the root cause
analysis. Information about TJC’s sentinel even requirement
is found under A.“Sentinel Events,”page8.5.
XVIII. STAFF TRAINING REQUIREMENTS
A. Federal Law: CMS Conditions of Participation
and Interpretive Guidelines
Federal law requires that staff be trained and able to
demonstrate competency in the application of restraints,
implementation of seclusion, monitoring, assessment, and
providing care for a patient in restraint or seclusion.
TRAINING INTERVALS
All staff, including contract or agency personnel, must
be trained and must demonstrate competency before
applying restraints; implementing seclusion; or monitoring,
assessing, or providing care for a patient in restraint or
seclusion.
Training must be included as part of orientation. The
required competencies must be demonstrated initially as
part of orientation and subsequently on a periodic basis
consistent with hospital policy. Hospitals have the flexibility
to identify a time frame for ongoing training based on the
level of staff competency, and the needs of the patient
population served. The results of skills and knowledge
assessments, new equipment or policies, or QAPI data
may indicate a need for targeted training or more frequent
or revised training.
Hospitals may develop and implement their own training
programs or use an outside training program.
TRAINING CONTENT
Appropriate staff must have education, training, and
demonstrated knowledge based on the specific needs of
the patient population in the following:

CHA Mental Health Law Manual 2019
5.28
©CALIFORNIA HOSPITAL ASSOCIATION
1. Techniques to identify staff and patient behaviors,
events, and environmental factors that may trigger
circumstances that require the use of a restraint
or seclusion.
2. The use of nonphysical intervention skills.
CMS states that staff may prevent a patient situation
from escalating to the point of needing restraint or
seclusion by using alternative techniques to redirect a
patient, engage the patient in constructive discussion
or activity, or otherwise help the patient maintain
self-control and avert escalation. CMS states that
the use of nonphysical intervention skills does not
mean attempting a complex series of interventions
or a lengthy checklist of steps before restraining
or secluding a patient. “Rather, a whole toolbox of
possible interventions can be implemented during
the course of a patient’s treatment based upon the
assessment of an individual patient’s responses” (see
Interpretive Guidelines, Tag A-0200). CMS does not
provide any information about this “toolbox.”
3. Choosing the least restrictive intervention based on an
individualized assessment of the patient’s medical, or
behavioral status or condition.
CMS states that the underpinning of this regulation is
the concept that safe patient care hinges on looking
at the patient as an individual and assessing his or
her condition, needs, strengths, weaknesses, and
preferences. Such an approach relies on caregivers
who are skilled in individualized assessment and in
tailoring interventions to the patient’s needs after
weighing factors such as the patient’s condition,
behaviors, history, and environmental factors. CMS
recommends a document entitled, “Learning from
Each Other — Success Stories and Ideas for
Reducing Restraint/Seclusion in Behavioral Health,”
sponsored by the American Psychiatric Association,
American Psychiatric Nurses Association, the National
Association of Psychiatric Health Systems, and the
American Hospital Association. This document may be
found at www.nabh.org/nabh-resources. This website
also includes useful forms, assessment tools, and
checklists.
4. CMS requires that appropriate staff be trained, and
demonstrate competency, in the safe application and
use of all types of restraint or seclusion used in the
hospital, including training in how to recognize and
respond to signs of physical and psychological distress
(for example, positional asphyxia) in a timely manner.
5. Clinical identification of specific behavioral changes
that indicate that restraint or seclusion is no
longer necessary.
CMS states that the use of restraint or seclusion must
end at the earliest possible time regardless of the
length of time identified in the order. Staff must be
trained and demonstrate competency in their ability
to identify specific patient behavioral changes that
may indicate that restraint or seclusion is no longer
necessary and can be safely discontinued.
6. Monitoring the physical and psychological well-being
of the patient who is restrained or secluded, including
but not limited to, respiratory and circulatory status,
skin integrity, vital signs, and any special requirements
specified by hospital policy associated with the
one-hour face-to-face evaluation.
7. The use of first aid techniques and certification in
the use of cardiopulmonary resuscitation, including
required periodic recertification.
CMS notes that typical “first aid” courses may not
adequately address the immediate interventions that need
to be rendered to a restrained or secluded patient who is
in distress or injured. Training should include information
that pertains to restrained or secluded patients in distress
or injured — for example, a patient found hanging in a vest
restraint, a restrained patient choking on food, a secluded
suicidal patient found hanging, a secluded suicidal patient
who has cut himself, etc. Staff need to assess their
patient population and identify likely scenarios, develop
a first aid training that addresses those scenarios, and
provide that training to all staff who care for restrained or
secluded patients.
In addition, appropriate staff should be certified in
cardiopulmonary resuscitation.
Special Training for RN or PA to Conduct One-Hour
Face-to-Face Evaluation
Training for an RN or PA to conduct the one-hour
face-to-face evaluation would also include content to
evaluate the patient’s immediate situation, the patient’s
reaction to the intervention, the patient’s medical and
behavioral condition, and the need to continue or terminate
the restraint or seclusion. An evaluation of the patient’s
medical condition would include a complete review of
systems assessment, behavioral assessment, as well as
review and assessment of the patient’s history, medications,
most recent lab results, etc. The purpose of the one-hour
face-to-face evaluation is to complete a comprehensive
review of the patient’s condition and determine if other

Chapter 5 — Restraints and Seclusion CHA
5.29
©CALIFORNIA HOSPITAL ASSOCIATION
factors, such as drug or medication interactions, electrolyte
imbalances, hypoxia, sepsis, etc., are contributing to
the patient’s violent or self-destructive behavior. (See
VIII.“Face-to-Face Evaluation,”page5.14.)
WHO MUST BE TRAINED
The regulation states that “appropriate staff” must be
trained. “Appropriate staff” includes all staff, including
contract or agency personnel, that apply restraint or
seclusion, monitor, assess, or otherwise provide care for
patients in restraint or seclusion. If hospital security guards
or other nonclinical staff, as part of hospital policy, may
assist clinical staff when requested, they are also expected
to be trained and able to demonstrate competency in the
safe application of restraint and seclusion.
Physician and other LIP training requirements must also be
specified in hospital policy. At a minimum, physicians and
other LIPs who may order restraint or seclusion must have
a working knowledge of hospital policy regarding the use of
restraint and seclusion.
Hospitals have the flexibility to identify training requirements
above this minimum requirement based on the competency
level of their physicians and other LIPs and the needs of
the patient population(s) that they serve. Physicians receive
training in the assessment, monitoring, and evaluation
of a patient’s condition as part of their medical school
education. However, physicians generally do not receive
training regarding application of restraint or implementation
of seclusion as part of their basic education. Depending on
the level and frequency of involvement that a physician has
in the performance of these activities, additional training
may or may not be necessary to ensure the competency of
these individuals in this area.
TRAINER REQUIREMENTS
CMS states that individuals providing staff training “must
be qualified as evidenced by education, training, and
experience in techniques used to address patients’
behaviors for the patient populations being served.”
Trainers should demonstrate a high level of knowledge
regarding all of the requirements of the CMS regulations as
well as the hospital’s policies and procedures.
TRAINING DOCUMENTATION
Hospitals must document in staff personnel records that
both training and demonstration of competency were
successfully completed initially during orientation and on a
periodic basis consistent with hospital policy.
SURVEY PROCEDURES
The Interpretive Guidelines direct surveyors to consider
the following:
1. Does the hospital have a documented training program
for the use of restraint and seclusion interventions
employed by the hospital?
2. Does the hospital have documented evidence that all
levels of staff, including agency or contract staff, that
have direct patient care responsibilities and any other
individuals who may be involved in the application of
restraints (e.g., security guards) have been trained
and are able to demonstrate competency in the safe
use of seclusion and the safe application and use of
restraints?
3. Review and verify restraint and seclusion education
staff training documentation for all new employees and
contract staff.
4. Does the training include demonstration of required
competencies?
5. Does the hospital educational program include
techniques related to the specific patient populations
being served?
6. Does the hospital educational program address each
topic discussed in “Training Content,”page5.27?
7. Does the hospital educational program provide more
in-depth training in the areas included in the regulation
for staff members who routinely provide care to
patients who exhibit violent or self-destructive behavior
(e.g., staff who work in the emergency department or
psychiatric unit)?
8. Does the hospital educational program address the
specific requirements for the training of RNs and PAs
that the hospital authorizes to conduct the one-hour
face-to-face evaluation?
9. Observe patients in restraint or seclusion to verify safe
application of the restraint or seclusion.
10. Interview staff to assess their knowledge and
skills in each of the topics discussed in “Training
Content,”page5.27.
11. Review hospital data (i.e., incident reports, patient
injury or death reports, etc.) to identify any patterns of
patient injuries or death that may indicate that staff are
not adequately trained to recognize and respond to
patient signs of physical and psychological distress.
12. Review personnel files of individuals responsible
for providing staff education and training. Do these

CHA Mental Health Law Manual 2019
5.30
©CALIFORNIA HOSPITAL ASSOCIATION
individuals possess education, training, and experience
to qualify them to teach the staff? Are they qualified to
identify and meet the needs of the patient population(s)
being served?
13. Does the hospital have a system for documenting and
ensuring that the individuals providing education and
training have the appropriate qualifications required by
this regulation?
14. Review a sample of staff personnel records, including
contract or agency staff, to determine if the training
and demonstration of competency have been
completed during orientation and on a periodic basis
consistent with hospital policy.
15. Review the hospital policy regarding restraint and
seclusion training requirements for physicians and
other LIPs. Are the minimum training requirements
addressed?
16. Review medical staff credentialing and privileging files
to determine if physicians or other LIPs involved in
restraint and seclusion activities have completed the
required training.
B. California Law
California law contains no requirements regarding staff
training. However, the law does mention some desirable
(not mandatory) topics for training programs. These include:
1. Conducting the intake assessment.
2. Utilizing strategies to engage patients collaboratively
in avoidance and management of crisis situations to
minimize the use of seclusion and restraint.
3. Using conflict resolution, effective communication,
de-escalation, and patient-centered problem solving
strategies to diffuse and safely resolve emerging
crisis situations.
4. Using individual treatment planning that identifies
risk factors, positive early intervention strategies, and
strategies to minimize time spent in seclusion and
restraint. Include patient input.
5. Using strategies to mitigate the emotional and physical
discomfort of patients in seclusion and restraint and
ensure the safety of the patient in seclusion and
restraint. Get patient input regarding what would
alleviate his or her distress.
6. Conducting an effective debriefing. Include strategies
that result in maximum participation and comfort for all
participants to identify factors that lead to the use of
seclusion and restraint and factors that would reduce
the likelihood of future incidents.
(See Health and Safety Code Section 1180.2.)
XIX. LAW ENFORCEMENT RESTRAINT OR
SECLUSION
A. Federal Law: CMS Conditions of Participation
and Interpretive Guidelines
The use of handcuffs, manacles, shackles, other chain-type
restraint devices, or other restrictive devices applied by
nonhospital employed or contracted law enforcement
officials for custody, detention, and public safety reasons
is not governed by the federal regulation regarding
restraint and seclusion. Such devices are considered law
enforcement restraint devices and are not considered safe,
appropriate health care restraint interventions for use by
hospital staff to restrain patients. The law enforcement
officers who maintain custody and direct supervision of
their prisoner (the hospital’s patient) are responsible for
the use, application, and monitoring of these restrictive
devices in accordance with state and federal law. However,
the hospital is still responsible for an appropriate patient
assessment and the provision of safe, appropriate care to
its patient (the law enforcement officer’s prisoner).
CMS does not consider the use of weapons in the
application of restraint or seclusion as a safe, appropriate
health care intervention. For the purposes of the federal
regulation, the term “weapon” includes, but is not limited
to, pepper spray, mace, nightsticks, tazers, cattle prods,
stun guns, and pistols. Security staff may carry weapons
as allowed by hospital policy, and state and federal
law. However, the use of weapons by security staff is
considered a law enforcement action, not a health care
intervention. CMS does not support the use of weapons by
any hospital staff as a means of subduing a patient in order
to place that patient in restraint or seclusion. If a weapon is
used by security or law enforcement personnel on a person
in a hospital (patient, staff, or visitor) to protect people or
hospital property from harm, CMS expects the situation
to be handled as a criminal activity and the perpetrator be
placed in the custody of local law enforcement.
CMS states that it is not appropriate for a hospital to
routinely call upon a law enforcement agency as a means
of applying restraint or seclusion. Hospitals must have
appropriately trained clinical staff. If hospital security guards
or other nonclinical staff, as part of hospital policy, may
assist clinical staff when requested, they are also expected
to be trained and able to demonstrate competency in the
safe application of restraint and seclusion.

Chapter 5 — Restraints and Seclusion CHA
5.31
©CALIFORNIA HOSPITAL ASSOCIATION
B. California Law
California law is silent regarding the use of restraint or
seclusion by law enforcement officers with respect to
hospitalized patients (with the exception of inmates in labor,
who may not be shackled; see Penal Code Sections 3407,
3423 and 6030; Welfare and Institutions Code Sections
222 and 1774).
In early 2009, the news media reported that the U.S.
Immigration and Customs Enforcement Agency (ICE)
contracted with a private California hospital to care for
mentally ill detainees. It was reported that the detainees
were kept shackled pursuant to ICE requirements, and
were denied many of their rights, such as sending and
receiving mail or having access to a phone. It was
suggested that the hospital was violating state law
regarding seclusion and restraint and denial of rights. The
argument was made that although patient’s rights can be
denied for good cause (and must be properly documented
and reported), good cause for denial of rights must be
based on an individual patient assessment, not on a
blanket policy regarding a group of patients, such as
ICE detainees.
Most of the California laws regarding restraint and seclusion
apply only to patients in acute psychiatric hospitals or in
psychiatric units of general acute care hospitals. As a
general rule, inmates and detainees who are restrained
or secluded by law enforcement officials are not admitted
to these settings. If, however, this situation arises, legal
counsel should be consulted.
XX. DOCUMENTATION REQUIREMENTS
Hospitals should document compliance with every state
and federal requirement regarding restraint and seclusion
discussed in this chapter. This portion of the chapter
describes the documentation requirements that CMS and
CDPH have listed in the “documentation” or “medical
records” portions of their regulations. However, it cannot
be emphasized enough that compliance with all of the
requirements discussed throughout this chapter should
be documented — not just compliance with the “medical
records” or “documentation” portions of the regulations.
A. Federal Law: CMS Conditions of Participation
and Interpretive Guidelines
The CMS CoP states that when restraint or seclusion is
used, there must be documentation in the patient’s medical
records of the following:
1. The one-hour face-to-face medical and behavioral
evaluation if restraint or seclusion is used to manage
violent or self-destructive behavior;
2. A description of the patient’s behavior and the
intervention used;
3. Alternatives or other less restrictive interventions
attempted (as applicable);
4. The patient’s condition or symptom(s) that warranted
the use of the restraint or seclusion; and
5. The patient’s response to the intervention(s)
used, including the rationale for continued use of
the intervention.
[42 C.F.R. Section 482.13(e)(16)]
The Interpretive Guidelines state that the patient’s behavior
should be documented in descriptive terms to evaluate
the appropriateness of the interventions used. The
documentation should include a detailed description of the
patient’s physical and mental status assessments and of
any environmental factors (e.g., physical, milieu, activities,
etc.) that may have contributed to the situation at the time
of the intervention. The patient’s condition or symptom(s)
must be identified and documented in the patient’s
medical record.
SURVEY PROCEDURES
The Interpretive Guidelines direct surveyors to consider
the following:
1. Does the patient’s medical record include
documentation of the one-hour face-to-face medical
and behavioral evaluation when restraint or seclusion is
used to manage violent or self-destructive behavior?
2. Does the patient’s medical record include a clear
description of the patient’s behavior that warranted the
use of restraint or seclusion?
3. Was the intervention employed appropriate for the
identified behavior?
4. What was the patient’s clinical response to the
intervention(s)?
5. Does the patient’s medical record document any
alternatives or less restrictive interventions attempted
by staff, if appropriate?
6. What was the effect of less restrictive interventions, if
attempted by staff?
7. Were the interventions selected appropriate to the
targeted patient behaviors?

CHA Mental Health Law Manual 2019
5.32
©CALIFORNIA HOSPITAL ASSOCIATION
8. When an immediate and serious danger to the
patient or others occurred, was the more restrictive
intervention(s) effective? Could a less restrictive
intervention have been used to ensure the safety of the
patient, staff or others?
9. Does the patient’s medical record include descriptions
of the patient’s condition or symptom(s) that warranted
the use of restraint or seclusion?
10. Does the patient’s medical record include descriptions
of the impact of the intervention on the patient behavior
that resulted in the use of restraint or seclusion?
11. Does the patient’s medical record include a detailed
assessment of the patient’s response to the
intervention and a well-reasoned plan for the continued
use of restraint or seclusion?
B. California Law
Each instance of seclusion or restraint must be noted
in the patient’s medical record in accordance with the
documentation requirements regarding denials of rights
(see F.“Denial of Patient Rights,”page4.4, for more
information about documentation of denial of rights)
[Title 9, California Code of Regulations, Section 865.4].
Psychiatric units of general acute care hospitals must
record the type of restraint and the time of application and
removal [Title 22, California Code of Regulations, Section
70577(j)(5)].
General acute care hospitals must record the type of
restraint and the time of application and removal [Title 22,
California Code of Regulations, Section 70749(a)(6)]. This
regulation specifies that this information does not need to
be recorded for soft-tie restraints used for the support and
protection of the patient. The exception likely applies to
medical/surgical uses of restraints, not restraints for mental
health patients.
In addition, state licensing regulations applicable to general
acute care hospitals state that “policies and procedures
which contain competency standards for staff performance
in the delivery of patient care shall be established,
implemented, and updated as needed for each nursing
unit, including standards for the application of restraints.”
The employees’ annual evaluation must include measuring
individual performance against established competency
standards. [Title 22, California Code of Regulations,
Section 70213]

Chapter 6 — Contents
©CALIFORNIA HOSPITAL ASSOCIATION
6 Health Information Privacy Basics
I. INTRODUCTION ....................................... 6.1
A. Important Laws to Know ..............................6.1
B. Enforcement and Penalties ..........................6.3
Federal .............................................................6.3
State
................................................................6.3
II. PATIENT PRIVACY RIGHTS ....................... 6.4
III. HEALTH CARE PROVIDER OBLIGATIONS ... 6.4
IV. USE AND DISCLOSURE OF PATIENT
INFORMATION ......................................... 6.4
A. What Information is Protected? ...................6.4
B. General Rule ..................................................6.5
The Concept of Minimum Necessary .................6.5
Incidental Uses and Disclosures
........................ 6.6
Verification of Identity/Authority
.........................6.6
C. Treatment, Payment and Health Care
Operations......................................................6.6
D. Hospital Directory..........................................6.6
E. Family and Friends: Patients Covered
by CMIA
..........................................................6.7
Patient is Present and Has Decision-Making
Capacity
........................................................... 6.7
Patient is Unavailable or Incapacitated
..............6.7
F. Family and Friends: Patients Covered
by LPS
.............................................................6.7
Which Patients are Covered by These
Notification Requirements?
...............................6.8
Definitions
.........................................................6.8
Notification Obligations
.....................................6.8
Immunity from Liability
......................................6.9
G. Mental Health Advocates ..............................6.9
H. Notifying Law Enforcement Officers
of Patient Presence, Release or
Disappearance
.............................................6.10
“Holdable” Voluntary Patient ............................ 6.10
Involuntary Patient
..........................................6.10
Involuntary Patient Under Criminal
Investigation
...................................................6.10
Dangerous Felon
.............................................6.11
Criminal Defendant Determined to Be
Mentally Incompetent to Stand Trial
.................6.11
Law Enforcement Officer With A Warrant
.........6.11
Patient Had Weapon Confiscated
...................6.12
I. Minor’s Medical Records ............................6.12
General Rule: Access to Records
Corresponds to Consent for Treatment
............6.12
V. SEARCHING PATIENTS AND THEIR
BELONGINGS ........................................ 6.13
A. Culture of Safety and Right to Privacy ......6.13
B. When to Search ...........................................6.13
C. Process of Search .......................................6.14
D. Potentially Dangerous Items ......................6.14
E. Related Laws ...............................................6.14
FORMS & APPENDICES
16-1
S
Authorization for Use or Disclosure of Health
Information
16-2
S
Request to Withhold Public Release of Information
Forms and Appendices can be found at the back of the manual and
online for CHA members at www.calhospital.org/free-resources.
“S” denotes that the form is provided in English and Spanish.

6 Health Information Privacy Basics
6.1
©CALIFORNIA HOSPITAL ASSOCIATION
I. INTRODUCTION
Health information privacy law is complicated. California
health care providers must comply with many state and
federal statutes and regulations governing patient privacy.
Understanding all of them, and how they interact with
each other, is challenging and the answers aren’t always
clear, even to experienced privacy lawyers. This chapter
provides an overview of the most important laws, as well
as guidance on everyday uses and disclosures of health
information in the hospital and clinic setting. This chapter
also addresses searching patients and their belongings.
This chapter is intended to address common situations
encountered by clinical staff and management, rather
than unusual circumstances or technical areas within the
privacy officer’s purview. The hospital’s privacy officer or
legal counsel should be consulted whenever questions
arise. For privacy officers, legal counsel, and others
tasked with health information privacy compliance, the
California Hospital Association publishes the California
Health Information Privacy Manual, which describes in
detail all of the relevant laws about health information
privacy, including permissible and impermissible uses and
disclosures; technical, administrative and physical security
safeguards; risk assessment; breaches; patient access to
their information and other patient privacy rights; employee
health; administrative processes; government and private
enforcement; and penalties. For more information about
this more than 450-page manual, visit www.calhospital.org/
privacy.
A. Important Laws to Know
The important privacy laws that California health care
providers must follow are briefly described below.
1. The Health Insurance Portability and Accountability Act
(HIPAA) regulations published by the U.S. Department
of Health and Human Services (DHHS) form the
overarching federal law about medical privacy. The
regulations give patients certain rights (see II.“Patient
Privacy Rights,” page6.4) and restrict how health
care providers and payers can use and disclose patient
information. Health care providers must comply with
HIPAA and applicable state law. [45 C.F.R. parts 160
and 164]
2. The Confidentiality of Medical Information Act (CMIA) is
California’s general health information privacy law. This
law applies to all general acute care hospital patients
except for some (but not all) mental health patients.
[Civil Code Section 56 et seq.]
3. The Lanterman-Petris-Short Act (LPS) includes several
confidentiality provisions that apply to records of some
(but not all) mental health patients. The confidentiality
provisions of LPS apply to all information and records
obtained in the course of providing services to:
a. Patients who are treated or evaluated under
Welfare and Institutions Code Sections 5150-
5344. These code sections include involuntary
evaluation and treatment in a designated facility
for patients who are a danger to self or others or
gravely disabled. These patients do not include
patients who may be detained involuntarily for up
to 24 hours in a non-designated hospital on an
emergency basis (usually, but not always, in the
emergency department) under Health and Safety
Code Section 1799.111 (chapter 12 of CHA’s
Consent Manual contains a thorough description
of all of these patients); and
b. Patients who are receiving voluntary or involuntary
mental health treatment in a:
• State mental hospital;
• County psychiatric ward, facility or hospital;
• University of California psychiatric facility:
Langley Porter Psychiatric Institute and the
Neuropsychiatric Institute at UCLA. Other
University of California mental health services
providers should consult University of California
counsel regarding their status under LPS;
• Federal hospital, psychiatric hospital or unit;
• Private institution, hospital, clinic or sanitarium
which is conducted for, or that includes a
department or ward conducted for, the care
and treatment of persons who are mentally
disordered;

CHA Mental Health Law Manual 2019
6.2
©CALIFORNIA HOSPITAL ASSOCIATION
• Psychiatric health facility as described in Health
and Safety Code Section 1250.2;
• Mental health rehabilitation center as defined in
Welfare and Institutions Code Section 5675;
• Skilled nursing facility with a special treatment
program service unit for patients with chronic
psychiatric impairments (see Title 22, California
Code of Regulations, Sections 51335 and
72443-72475 about such special treatment
programs);
• Community program funded by the Bronzan-
McCorquodale Act. Because it is often difficult
to determine which patients received services
funded under the Bronzan-McCorquodale
Act, each program and its legal counsel
should review any funds received under the
Bronzan-McCorquodale Act to determine the
applicability, if any, of those confidentiality
provisions as a result of such funding [Welfare
and Institutions Code Sections 5600-5778];
and
• Community program specified in the Welfare
and Institutions Code Sections 4000-4390 and
Welfare and Institutions Code Sections 6000-
6008.
Absent some tie-in to one of the above described
programs, LPS does not apply to other mental health
patients or their records, even though those records
may describe mental health treatment similar to what
is protected under LPS. These records are instead
subject to the Confidentiality of Medical Information Act
(CMIA)
4. California’s Health and Safety Code gives special
confidentiality protection to HIV test results. This law
does not apply to a diagnosis of AIDS; it applies only to
the HIV test results, whether the results are positive or
negative. [Health and Safety Code Section 120980 et
seq.] HIV test results may be disclosed to the patient
and to other health care providers with a need to know
to diagnose or treat the patient. Hospital employees
should check with their privacy officers or legal counsel
before disclosing HIV test results to others.
5. Federal law gives special confidentiality protection to
records of substance use disorder programs. These
rules do not apply to all substance use disorder
patients; they apply only to patients served by
“federally-assisted substance use disorder programs.”
If a not-for-profit hospital has a service line identified
to the public as a substance use disorder program
or unit, or has personnel whose primary function is
the provision of substance use disorder treatment
and who are identified as such providers, the hospital
must follow these strict confidentiality rules. These
rules are described in detail in CHA’s California
Health Information Privacy Manual, available at www.
calhospital.org/privacy.
6. Federal law gives special confidentiality protection
to “psychotherapy notes,” a concept introduced by
HIPAA. “Psychotherapy notes” means:
[N]otes recorded (in any medium) by a health
care provider who is a mental health professional
documenting or analyzing the contents of conversations
during a private counseling session or a group, joint,
or family counseling session and that are separated
from the rest of the individual’s medical record.
[emphasis added]
Psychotherapy notes exclude medication prescription
and monitoring; counseling session start and stop
times; the modalities and frequencies of treatment
furnished; results of clinical tests; and any summary
of diagnosis, functional status, the treatment plan,
symptoms, prognosis, and progress to date.
A psychotherapist is not required to maintain
psychotherapy notes. Most hospitals, skilled nursing
facilities, and other institutional providers do not have
psychotherapy notes, as defined in HIPAA, because
the definition requires the notes to be separate from
the rest of the medical record. If the notes are included
with the rest of the medical record, then they are not
psychotherapy notes and are not subject to the special
restrictions. A separate authorization for the disclosure
of psychotherapy notes, even for treatment purposes
(except by the provider who created the notes), is
almost always required. [42 C.F.R. Sections 164.501,
164.508(a)(2)]
7. The Patient Access to Health Records Act gives
patients the right to review, and obtain copies of, their
medical information [Health and Safety Code Section
123000 et seq.]. HIPAA has a similar provision [45
C.F.R. Section 164.524].
8. Both state and federal law require health care providers
to notify patients and government agencies if a privacy
breach occurs. Clinical staff should immediately notify
the hospital’s privacy officer if they believe a breach
has occurred or if a patient complains about an alleged
breach. The laws are complicated, and what may seem
like a breach may not, in fact, constitute a reportable
incident. On the other hand, if a breach has occurred,

Chapter 6 — Health Information Privacy Basics CHA
6.3
©CALIFORNIA HOSPITAL ASSOCIATION
the timeline for making the required notifications is
short, and the privacy officer will want as much time
as possible to investigate, document, and report. [45
C.F.R. Section 164.402; Civil Code Section 1798.82;
Health and Safety Code Section 1280.15]
9. The law permits hospitals and other businesses to
examine a driver’s license or DMV identification card,
photocopy it, and retain the photocopy. However, a
license or ID card may be scanned or swiped only:
a. To verify the age or authenticity of the card.
b. To comply with a legal requirement.
c. To transmit to a check service company.
d. To collect or disclose information required for
reporting, investigating, or preventing fraud, abuse,
or material misrepresentation.
A hospital or other business may not retain or
use any of the information obtained by electronic
scanning or swiping for any purpose not listed
above. [Civil Code Section 1798.90.1]
10. California law contains limitations on requiring patients
or consumers to submit their Social Security number
(SSN) over the internet, as well as printing SSNs on
identification cards or on materials mailed to the holder
of the number. The law does not prevent the collection,
use or release of an SSN as required by law, or the
use of an SSN for internal verification or administrative
purposes. [Civil Code Section 1798.85]
11. California law limits the information that a business can
require a customer to provide when accepting a check
or a credit card as payment for goods and services
[Civil Code Sections 1725 and 1747.08].
California hospitals (and most other health care providers)
must comply with either the CMIA or LPS, and with all the
other laws listed above. If there is a state law and a federal
law on the same topic, under federal preemption rules,
health care providers must comply with whichever law is
more stringent — that is, the law that is more protective of
the patient’s privacy or that gives the patient greater access
to their information. Complicating matters further, providers
must comply with whichever provision of the laws is stricter.
This means if the state law is more stringent than the
federal law, with the exception of one provision, providers
must comply with the state law and the one provision in
federal law that gives patients greater privacy protection or
greater access to their own information.
B. Enforcement and Penalties
FEDERAL
The DHHS Office for Civil Rights (OCR) is responsible for
enforcing HIPAA. Any person, organization, or group that
believes a hospital or other health care provider has violated
HIPAA may file a complaint with OCR; the complainant
does not need to be the patient. Therefore, complainants
may include a provider’s employees, unions, medical staff
members, business associates, or patients, as well as
accrediting, health oversight or advocacy agencies. OCR
is also required by law to conduct random audits and
compliance reviews.
Noncompliance with the HIPAA rules has serious potential
implications. HIPAA provides for fines of up to $55,010
per violation and criminal penalties of up to 10 years in
prison. A California hospital is subject to both state and
federal penalties.
A state attorney general may also enforce HIPAA.
STATE
The California Department of Public Health (CDPH) is
responsible for investigating violations of California law in
hospitals and other health care facilities, and may assess
fines of up to $25,000 per patient, per privacy breach (with
some limits).
In addition, the CMIA authorizes several levels of
administrative fines or civil penalties, depending upon
whether a violation was negligent, knowing or willful,
or done for financial gain. The upper levels of fines are
$250,000 per violation. These penalties may be sought
by the California Attorney General, any district attorney or
county counsel, or others. A violation of CMIA may also be
punished as a misdemeanor.
There are also financial penalties available under the law for
violations of LPS and the special laws for confidentiality of
HIV test results.
Finally, a patient may recover monetary damages from
a health care provider for a violation of state health
information privacy laws. Many class action lawsuits
have been brought against providers asking for statutory
damages of $1,000 per patient whose information was
hacked or was contained in stolen computer equipment.
Although many of these lawsuits have been successfully
defended, it is clear that privacy breaches are an area of
high-dollar risk.

CHA Mental Health Law Manual 2019
6.4
©CALIFORNIA HOSPITAL ASSOCIATION
II. PATIENT PRIVACY RIGHTS
State and federal laws give patients certain rights regarding
their privacy and their medical information. Patients have a
right to:
1. Obtain a written notice from their health care provider
explaining how it will use and disclose their information.
This is called the Notice of Privacy Practices.
2. Access their medical records. This means patients
can see their records, request copies, and request
a correction/amendment to their record. Limited
exceptions to this right exist; if a health care provider
believes that a patient seeing his or her own medical
record might be detrimental to the patient or another
person, the provider should consult legal counsel or
the privacy officer. Patients are not entitled to take the
original medical record, and may be monitored while
they review the record to ensure no changes are made.
3. Request that a provider not use or disclose certain
information for purposes of treatment, payment,
and health care operations. It is important to know
that although patients have the right to make these
requests, providers are generally not required to
comply. Hospital personnel should be trained that
whenever a patient makes a special request about the
privacy of their information, the hospital’s privacy officer
should be contacted. The bedside nurse or emergency
department physician should not, for example, assure
the patient that their information will not be disclosed
to a certain physician or insurance company. Only
the privacy officer should make such commitments
to patients.
4. Request that information be communicated to them in
particular ways to ensure confidentiality. For example,
the patient may request to have information sent to
work rather than their home. These requests must be
accommodated, if reasonable. Hospitals and other
health care providers should have a process in place
to document these requests, respond to them, and
implement them if reasonable.
5. Obtain an accounting of how their information has
been disclosed for purposes not related to treatment,
payment or health care operations. (See C.“Treatment,
Payment and Health Care Operations,” page6.6.)
6. Refuse to authorize the release of their information
for most purposes that are not related to treatment,
payment or health care operations. (See C.“Treatment,
Payment and Health Care Operations,” page6.6.)
7. Be notified of breaches to the extent required by law.
For more information about these patient rights, consult
your hospital’s privacy officer or legal counsel, or refer to
CHA’s California Health Information Privacy Manual.
III. HEALTH CARE PROVIDER OBLIGATIONS
Hospitals and other health care providers must:
1. Give each patient a Notice of Privacy Practices.
2. Limit the circumstances under which patient
information is used or disclosed.
3. Develop policies, procedures and systems to protect
patient privacy and allow patients to access and
correct their records.
4. Train staff on privacy policies and procedures.
5. Appoint a privacy officer to make sure privacy
procedures are developed, adopted and followed.
6. Appoint a security officer to make sure security
procedures are developed, adopted and followed.
7. Implement appropriate administrative, technical and
physical safeguards to protect patient records from
individuals who shouldn’t see them.
8. Account for specified disclosures of patient information.
9. Establish a complaint mechanism for privacy concerns.
10. Establish and enforce a system of sanctions
for employees who violate privacy policies
and procedures.
11. Establish written agreements with business associates.
12. Notify patients and government agencies of a breach
to the extent required by law.
For more information about these requirements, consult
your hospital’s privacy officer or legal counsel, or refer to
CHA’s California Health Information Privacy Manual.
IV. USE AND DISCLOSURE OF PATIENT
INFORMATION
A. What Information is Protected?
State and federal laws protect individually-identifiable health
information in every form — electronic, on paper or oral.
“Individually-identifiable health information” is health
information that identifies, or there is a reasonable basis
to believe it can be used to identify, a patient. Federal
law in particular has very detailed requirements about

Chapter 6 — Health Information Privacy Basics CHA
6.5
©CALIFORNIA HOSPITAL ASSOCIATION
de-identified information, because computer-savvy people
can take a little bit of health information, combine it with
other publicly available data such as voter registration or
social media information, and determine to which patient
the health information pertains. Hospital staff should
consult the hospital’s privacy officer or legal counsel to
learn if a particular set of data elements is considered
individually-identifiable.
“Health information” is broadly defined to include any
information relating to the physical or mental health or
condition of a patient, the health care provided to a patient,
or payment for health care provided to a patient. This
includes medical records, billing records, and other types
of records.
It is important to understand that the restrictions on the use
and disclosure of individually-identifiable health information
apply to the hospital’s use of patient information internally,
among staff and throughout departments — not just to
disclosures of information outside the facility.
B. General Rule
In general, providers cannot use or disclose
individually-identifiable health information unless:
1. The patient completes an authorization form. An
authorization for a disclosure of medical information
must be in writing and contain several specified
elements. CHA has developed the “Authorization for
Use or Disclosure of Health Information” (CHA Form
16-1) to comply with all state and federal requirements.
If the patient is a minor, deceased, or lacks the
capacity to make health care decisions, the patient’s
legal representative may sign the authorization form.
Hospital staff should consult the privacy officer or legal
counsel about who is considered a legal representative.
2. The use or disclosure is made directly to another
health care provider for the purposes of treatment
or payment.
3. The information is used within the facility for its own
health care operations (see C.“Treatment, Payment
and Health Care Operations,” page6.6).
4. The requirements for communicating with patients’
family or friends are followed (see E.“Family and
Friends: Patients Covered by CMIA,” page6.7 and
F.“Family and Friends: Patients Covered by LPS,”
page6.7).
5. The disclosure is required by law. A health care
provider is permitted to disclose patient-identifiable
information to the extent necessary to make a
legally-mandated report, such as a report of child
abuse, communicable disease, gunshot wound or
other suspicious injury, etc. The information disclosed
must be limited to the minimum information necessary
to comply with the reporting requirement.
It is important to note that this “required by law”
permission does not mean that a health care provider
can disclose information to law enforcement officers.
In fact, there are very strict rules about giving
information to law enforcement officers. The hospital’s
privacy officer or legal counsel should be consulted
before giving a law enforcement officer any patient
information.
6. A specific provision of law permits the use or
disclosure.
There are many complicated exceptions to the general rule.
Front line clinical staff should consult the hospital’s privacy
officer or legal counsel in situations that are not listed
above.
If a question arises about whether a particular use or
disclosure is permissible, providers should remember that
obtaining a written authorization from the patient or the
patient’s legal representative is almost always a safe course
of action.
THE CONCEPT OF MINIMUM NECESSARY
HIPAA introduced the concept of “minimum necessary.”
Providers must limit their use and disclosure of
individually-Identifiable health information to the minimum
amount of information necessary to accomplish the
intended purpose of the use or disclosure. For example,
if the hospital’s auditor needs patient medical record
information to determine if a bill is accurate, the auditor
should be allowed access to only that portion of the
medical record that the bill covers. The auditor should not
be able to see the rest of the medical record.
The minimum necessary standard does not apply to:
1. Disclosures to, or requests by, a health care provider
for treatment purposes. Physicians, nurses and other
providers may need the complete medical record to
provide the best care possible.
2. Uses or disclosures made to the patient. A patient has
the right to access his or her information.
3. Uses or disclosures made according to a patient’s
written authorization. A patient is allowed to authorize
the disclosure of the entire medical record.

CHA Mental Health Law Manual 2019
6.6
©CALIFORNIA HOSPITAL ASSOCIATION
Implementation of Minimum Necessary
A health care provider must identify the employees
or classes of employees who need access to health
information to carry out their duties. For each employee
or class of employees, the provider must identify the
categories of information to which access is needed and
any conditions appropriate to such access. The provider
must make reasonable efforts to limit access to the
minimum information needed.
For routine and recurring disclosures (or requests), a
provider must implement policies and procedures (which
may be standard protocols) that limit the information
disclosed (or requested from another covered entity) to the
amount reasonably necessary to achieve the purpose of the
disclosure (or request).
For all other disclosures (or requests) — that is, nonroutine
and nonrecurring — a provider must develop criteria
designed to limit the information disclosed to what is
reasonably necessary to accomplish the purpose for
which disclosure is sought, and must review each request
for disclosure on an individual basis in accordance with
those criteria.
When the minimum necessary standard applies, a provider
may not use, disclose or request an entire medical record,
except when the entire medical record is specifically
justified as the amount that is reasonably necessary to
accomplish the purpose of the use, disclosure or request.
[45 C.F.R. Section 164.514(d)]
INCIDENTAL USES AND DISCLOSURES
HIPAA recognizes that “incidental” uses and disclosures
will occur. For example, if two hospitalized patients share a
room, it is inevitable that one patient will overhear medical
information about the other. HIPAA explicitly permits
covered entities to use or disclose health information
“incident to a use or disclosure otherwise permitted or
required by” HIPAA, if the hospital has complied with the
minimum necessary standard; implemented appropriate
administrative, technical, and physical safeguards; and
made reasonable attempts to limit incidental uses and
disclosures. For example, if a nurse needs to talk to a
patient about his or her medical condition, it would be
reasonable to ask the roommate’s visitors to step outside
the room temporarily. However, it would not be necessary
to transfer the roommate to another room temporarily.
[45 C.F.R. Section 164.502(a)(1)(iii)]
VERIFICATION OF IDENTITY/AUTHORITY
Health care providers must verify the identity of any person
requesting individually-identifiable information, and their
authority to have it, if the identity or authority is not already
known to the provider. Providers must also obtain any
documentation, statements or representations (whether
oral or written) that are a condition of disclosure. In the
case of parents, guardians, or other legal representatives,
this includes verifying that the person requesting
health information is indeed the parent, guardian, or a
legal representative.
Providers should have policies and procedures to verify the
identity and authority of requestors, and to document this
was done.
C. Treatment, Payment and Health Care
Operations
A health care provider may use or disclose patient
information, without a written authorization from the patient,
for what HIPAA calls “treatment, payment, and health care
operations” (TPO).
“Treatment” means providing, coordinating or managing
a patient’s care, including consultations between providers
and referrals.
“Payment” is defined as activities related to paying or
being paid for services rendered. These include eligibility
and coverage determinations, billing, claims management,
utilization review and the like.
“Health care operations” covers a broad range of
activities such as quality assessment and improvement,
patient education and training, health practitioner training,
contracting for health care services, medical review, legal
services, auditing functions, compliance, business planning
and development, business management and general
administrative activities.
Clinical staff should consult the hospital’s privacy officer or
legal counsel if questions arise about which activities are
considered TPO.
D. Hospital Directory
State and federal health information privacy laws
significantly restrict the information that may be disclosed
without patient authorization to the public, including visitors,
florists, clergy, media and others. A patient has the right
to prevent even this restricted information from being
released. Patients should be advised of this right in the
Notice of Privacy Practices they receive upon admission to

Chapter 6 — Health Information Privacy Basics CHA
6.7
©CALIFORNIA HOSPITAL ASSOCIATION
the hospital. If a patient objects to the release of information
to the public, the patient should be asked to complete the
“Request to Withhold Public Release of Information” (CHA
Form 16-2) or a similar form.
If the patient has not requested that information be withheld
and the request for information contains the patient’s name,
HIPAA and the CMIA allow hospitals to release:
1. The patient’s condition, described in general terms
that do not communicate specific medical information
about the individual (for example, “undetermined,”
“good,” “fair,” “critical,” etc.).
2. The patient’s location within the hospital. Release of
location is intended to facilitate visits by family and
friends, as well as delivery of gifts or flowers. Caution
should be exercised in disclosing this information over
the telephone. Precise directions (e.g., floor or room
number) are best disclosed only on a face-to-face
basis so that there is an opportunity to verify the
individual’s purpose or intended use of the information.
As a reminder, patients in psychiatric units are covered by
the Lanterman-Petris-Short Act, not the CMIA (see 3. on
page 6.1). A hospital should neither confirm nor deny that
a patient is in an acute psychiatric hospital or a psychiatric
unit of a general acute care hospital without the patient’s
authorization.
[45 C.F.R. Section 164.510(a)(1)(i)(C)]; Civil Code Section
56.16]
(See E.“Family and Friends: Patients Covered by CMIA,”
page6.7 below, about disclosures that may be made to
family and friends involved in the care of the patient.)
E. Family and Friends: Patients Covered by CMIA
Both the CMIA and HIPAA (but not LPS) permit disclosure
of limited information to a family member, other relative,
domestic partner, close personal friend, or other person
identified by the patient. Information is limited to the
information directly relevant to that person’s involvement
with the patient’s health care or payment for the care.
This rule applies to minors as well as adults. This rule
does not apply to HIV test results or information held by
federally-assisted substance use disorder programs.
Disclosure or use of health information is also permitted to
notify, or assist in the notification of (including identifying
or locating), a family member, personal representative of
the patient, domestic partner, or other person responsible
for the care of the patient, of the patient’s location, general
condition, or death.
Disclosure to family and friends is subject to the conditions
described below. [Civil Code Section 56.1007; 45 C.F.R.
Section 164.510(b)]
CAUTION: LPS information may not be disclosed under
this provision of law. If a patient is an involuntarily detained
mental health patient, or a patient in an acute psychiatric
hospital, psychiatric unit in a general acute care hospital, or
a mental health patient in a government-operated hospital
or clinic, the patient’s authorization must be obtained prior
to disclosing information to family or friends (see 3. on page
6.1).
PATIENT IS PRESENT AND HAS DECISION-MAKING
CAPACITY
Where the patient is available and has decision-making
capacity, disclosure may be made to family/friends if
the provider:
1. Obtains the patient’s verbal agreement;
2. Provides the patient with the opportunity to object to
the disclosure, and the patient does not do so; or
3. Reasonably infers from the circumstances, based upon
their professional judgment that the patient does not
object to the disclosure. However, this provision does
not apply if the provider is a psychotherapist [Civil
Code Section 56.1007(c)(2))].
PATIENT IS UNAVAILABLE OR INCAPACITATED
If the patient is not present, or the opportunity to agree
or object to the use or disclosure to family/friends cannot
practicably be provided because of the patient’s incapacity
or an emergency circumstance, disclosure may be made
if the provider, in the exercise of professional judgment,
determines the disclosure is in the best interests of the
patient. As a reminder, the provider may disclose only the
information directly relevant to the person’s involvement
with the patient’s health care, payment for the care, or
needed for notification purposes.
F. Family and Friends: Patients Covered by LPS
As a general rule, a hospital may not disclose
patient-identifiable information to family or friends without
the patient’s authorization, unless a special exception to
the law applies. The law is especially strict with respect to
mental health patients whose records are subject to the
LPS confidentiality provisions (see below for information
about which patients are covered). For these patients,
a hospital usually should not disclose even whether the
person is or has been a patient (“we can neither confirm

CHA Mental Health Law Manual 2019
6.8
©CALIFORNIA HOSPITAL ASSOCIATION
nor deny that this person is or has been a patient here”)
without patient permission. However, LPS requires that
limited information be disclosed to family and others in
the situations described below. In each case, the hospital
should disclose only the minimum information necessary to
comply with the law.
WHICH PATIENTS ARE COVERED BY THESE
NOTIFICATION REQUIREMENTS?
The LPS notification requirements apply to patients who are
receiving voluntary or involuntary treatment in a:
1. Hospital designated by the county for patients who are
a danger to self or others or gravely disabled;
2. State mental hospital;
3. County psychiatric ward, facility or hospital;
4. University of California psychiatric facility: Langley
Porter Psychiatric Institute and the Neuropsychiatric
Institute at UCLA. Other University of California mental
health services providers should consult University of
California counsel regarding their status under LPS;
5. Federal hospital, psychiatric hospital or unit;
6. Private institution, hospital, clinic or sanitarium which is
conducted for, or that includes a department or ward
conducted for, the care and treatment of persons who
are mentally disordered;
7. Psychiatric health facility as described in Health and
Safety Code Section 1250.2;
8. Mental health rehabilitation center as defined in Welfare
and Institutions Code Section 5675;
9. Skilled nursing facility with a special treatment
program service unit for patients with chronic
psychiatric impairments (see Title 22, California Code
of Regulations, Sections 51335 and 72443-72475
regarding such special treatment programs);
10. Community program funded by the
Bronzan-McCorquodale Act. Because it is often difficult
to determine which patients received services funded
under the Bronzan-McCorquodale Act, each program
and its legal counsel should review any funds received
under the Bronzan-McCorquodale Act to determine the
applicability, if any, of those confidentiality provisions as
a result of such funding [Welfare and Institutions Code
Sections 5600-5778]; and
11. Community program specified in the Welfare and
Institutions Code Sections 4000-4390 and Welfare and
Institutions Code Sections 6000-6008.
Absent some tie-in to one of the above-described
programs, LPS does not apply to other mental health
patients, even though they may receive mental health
treatment similar to what is covered by LPS. These patients
and their records are instead subject to the Confidentiality
of Medical Information Act (CMIA). For example, mental
health services provided to an involuntary patient in a
private, non-designated hospital emergency department
under Health and Safety Code Section 1799.111 are
subject to the CMIA rather than LPS.
DEFINITIONS
The reporting requirements described below use the terms
“next of kin” and “reasonable attempt,” but do not define
these terms. The facility should specify by policy the order
in which relatives will be notified, and may, for example,
use the priority in which people inherit as a starting point.
Therefore, when an adult patient is admitted, the facility
could decide that it should attempt to contact one of the
following persons, in the priority stated:
1. Spouse or domestic partner
2. Adult son or daughter
3. Either parent
4. Adult brother or sister
5. Grandparents
6. Adult aunt or uncle
If the patient is a minor, the parent(s) or legal guardian
should be contacted.
The hospital should also establish in its policy what actions
constitute a “reasonable attempt” to notify the family.
NOTIFICATION OBLIGATIONS
Notifying Family and Others of Admission
A hospital must make reasonable attempts to notify an
LPS patient’s next of kin or other person designated by the
patient when he or she is admitted for inpatient services
to a 24-hour public or private health facility licensed
under Health and Safety Code Section 1250 (for example,
a general acute care hospital or an acute psychiatric
hospital), unless the patient asks that this information not
be provided. The patient must be advised by the facility that
he or she has the right to request that this information not
be provided.
The following information must be documented in the
patient’s medical record:

Chapter 6 — Health Information Privacy Basics CHA
6.9
©CALIFORNIA HOSPITAL ASSOCIATION
1. That the patient was advised that next of kin would be
notified unless the patient asks that this notification not
be made;
2. The patient’s response to the advisement;
3. The date and circumstances under which the
notification (if any) was made or attempted;
4. The names and relationships to the patient, if any, of
persons or agencies to whom the notification was
made; and
5. The specific information disclosed.
[Welfare and Institutions Code Section 5328.1(b); see also
45 C.F.R. Section 164.512(a)]
Different notification requirements apply to patients who
arrive in the emergency department of a general acute
care hospital who are unconscious or otherwise unable to
communicate. (See CHA’s Consent Manual, chapter 1, for
further information.)
Notifying Family and Others of Inpatient’s Release,
Transfer, Illness or Death
A hospital must make reasonable attempts to notify an
LPS inpatient’s next of kin or other person designated by
the patient of the patient’s release, transfer, serious illness,
injury or death, upon the request of the family member,
unless the patient asks that this information not be provided
[Welfare and Institutions Code Section 5328.1(b); see also
45 C.F.R. Section 164.512(a)].
The hospital must advise the patient that it is required to
and will attempt to contact his or her next of kin or other
person the patient designates, to provide this information.
The hospital also must inform the patient of the right to
request that this information not be disclosed.
The following information must be documented in the
patient’s medical record:
1. That the patient was advised that next of kin would be
notified unless the patient asks that this notification not
be made;
2. The patient’s response to the advisement;
3. The date and circumstances under which the
notification (if any) was made or attempted;
4. The names and relationships to the patient, if any, of
persons or agencies to whom the notification was
made; and
5. The specific information disclosed.
Notifying Family and Others of the Patient’s Condition
Upon request of a family member of a patient (or other
person designated by the patient), a facility must tell
the family member (or the designee) of an LPS patient’s
diagnosis, the prognosis, the medications prescribed,
the side effects of medications prescribed, if any, and
the progress of the patient, if, after notifying the patient
that this information is requested, the patient authorizes
its disclosure [Welfare and Institutions Code Section
5328.1(a)].
The patient’s written authorization should be obtained. The
“Authorization for Use or Disclosure of Health Information”
form (CHA Form 16-1) or a similar form, should be
completed and placed in the patient’s medical record.
If the patient is unable to authorize the release of this
information, the hospital must document the attempt to
obtain the patient’s authorization in the medical record.
Daily efforts must be made to secure the patient’s
authorization or refusal.
However, if a request for information is made by the
spouse, parent, child or sibling of the patient and
the patient is unable to authorize the release of such
information, the requestor must be told of the patient’s
presence in the facility, except to the extent prohibited
by federal law (this last qualification was likely inserted
originally to accommodate the federal substance use
disorder confidentiality regulations, which limit disclosure
of a patient’s presence in a facility) [Welfare and Institutions
Code Section 5328.1(a); see also 45 C.F.R. Section
164.512(a)].
The following information must be documented in the
patient’s medical record:
1. The date and circumstances under which the
notification was made or attempted;
2. The names and relationships to the patient, if any, of
persons or agencies to whom the notification was
made; and
3. The specific information disclosed.
IMMUNITY FROM LIABILITY
Facilities and their employees are not liable for damages
caused, or allegedly caused, by the release of information,
or failure to release information, under this law.
G. Mental Health Advocates
Mental health advocates may have the legal authority to
access patient information and records. This authority
is described in V.“Mental Health Advocacy Programs,”
page4.7.

CHA Mental Health Law Manual 2019
6.10
©CALIFORNIA HOSPITAL ASSOCIATION
H. Notifying Law Enforcement Officers of Patient
Presence, Release or Disappearance
As a general rule, a hospital may not disclose
patient-identifiable information to law enforcement officers
without the written authorization of the patient, unless a
special exception to the law applies (see chapter 6). The
law is especially strict when an officer requests information
about a mental health patient whose records are subject
to the LPS confidentiality provisions (see chapter 6
for information about which patients are covered). For
these patients, a hospital usually should not disclose
even whether the person is or has been a patient (“we
can neither confirm nor deny that this person is or has
been a patient here”). However, LPS requires that limited
information be disclosed to law enforcement officers in
the situations described below. In each case, the hospital
should disclose only the minimum information necessary to
comply with the law.
“HOLDABLE” VOLUNTARY PATIENT
If a voluntary patient who is a danger to self/others or
gravely disabled (that is, the patient meets the criteria
for involuntary commitment for 72-hour treatment and
evaluation) disappears from the hospital, the physician in
charge of the patient or the professional person in charge
of the facility or his or her designee may designate a
governmental law enforcement agency or agencies to be
notified. The whereabouts of the patient must be unknown,
and the disclosure must be necessary for the protection
of the patient or others. The hospital may also notify the
patient’s relatives. The information disclosed should be the
minimum necessary to assist in finding the patient. [Welfare
and Institutions Code Section 5328.3(a); see also 45 C.F.R.
Sections 164.508(a)(2)(ii) and 164.512(j)]
The following information must be documented in the
patient’s medical record:
1. The date and circumstances under which the
notification was made;
2. The names and relationships to the patient, if any, of
persons or agencies to whom the notification was
made; and
3. The specific information disclosed.
The law does not define the term “relatives” or specify
which relatives may be notified. It would make sense to
notify the relative(s) in the best position to find the patient
and take steps to keep the patient and others safe.
[Welfare and Institutions Code Section 5328.6]
INVOLUNTARY PATIENT
LPS-designated hospitals, state hospitals, and Veterans’
Administration facilities must notify the law enforcement
agency of the county or city in which the hospital is
located when a patient listed in one of the following
categories escapes:
1. A patient judicially committed.
2. A patient involuntarily detained under Welfare and
Institutions Code Sections 5000 to 5550. (See chapter
3 regarding involuntary detainment for mental health
evaluation and treatment.)
3. A patient who has been placed in a facility by his or her
conservator pursuant to Welfare and Institutions Code
Section 5350.
The notification must be in writing and include:
1. The name and physical description of the patient;
2. The patient’s home address;
3. The degree of dangerousness of the patient, including
specific information about the patient if he or she is
deemed likely to cause harm to himself or herself or
others; and
4. Any additional information that is necessary to
apprehend and return the patient.
The person in charge of the hospital or facility (or a
designee) may notify the law enforcement agency by
phone and follow up with written notification. The written
notification must include the time and date of the telephonic
notification, the person notified, and the person who made
the notification. [Welfare and Institutions Code Section
7325; see also 45 C.F.R. Section 164.512(a) and (f)]
INVOLUNTARY PATIENT UNDER CRIMINAL
INVESTIGATION
A hospital must notify the county behavioral health
director (or designee) and law enforcement agency upon
the discharge of a patient after a peace officer initiated a
72-hour hold and requested to be notified when the patient
was released. The peace officer must have certified in
writing at the time of detention that the facts would support
the filing of a criminal complaint against the patient. The
information disclosed must be limited to:
1. The patient’s name and address;
2. The date of admission for 72-hour evaluation and
treatment;
3. The date of certification for intensive treatment (if
applicable); and

Chapter 6 — Health Information Privacy Basics CHA
6.11
©CALIFORNIA HOSPITAL ASSOCIATION
4. The date of release.
Notification is required whether the hospital decides not to
detain the patient at all, detains him or her for the full 72
hours, or detains him or her for less than 72 hours.
(See “Notification of Release to County Behavioral Health
Director and Peace Officer,” page 3.12, regarding patients
brought to the facility for a 72-hour evaluation period.
See “Notification of Release to County Behavioral Health
Director and Peace Officer,” page 3.19, regarding patients
receiving 14-day intensive treatment.)
[Welfare and Institutions Code Sections 5152.1, 5250.1 and
5328(a)(16); see also 45 C.F.R. Section 164.512(a) and (f)]
DANGEROUS FELON
A hospital must report to the California Department of
Justice movement and identification information about a
patient committed to the California Department of State
Hospitals, a state hospital, or any other public or private
mental health facility approved by the county behavioral
health director for observation or for an indeterminate
period as a mentally disordered sex offender, a sexually
violent predator, a person committed pursuant to Penal
Code Sections 1026 (not guilty by reason of insanity) or
1370 (mentally incompetent to stand trial), or Welfare and
Institutions Code Section 5300 (imminently dangerous). The
information that may be disclosed is limited to:
1. Patient’s name and address;
2. Fingerprints;
3. Dates of admission and discharge;
4. Date of escape or return from escape;
5. Date of any home leave, parole, or leave of
absence; and
6. The county in which the person will reside upon
release, if known.
[Welfare and Institutions Code Section 5328.2; see also
45 C.F.R. Section 164.512(a) and (f)(1)(i)]
CRIMINAL DEFENDANT DETERMINED TO BE
MENTALLY INCOMPETENT TO STAND TRIAL
A hospital must report the disappearance or transfer
between state hospitals of a patient who is a criminal
defendant who was committed following a determination of
incompetency to stand trial with respect to a pending felony
charge involving death, great bodily harm, or a serious
threat to the physical well-being of another person [Welfare
and Institutions Code Section 5008(h)(1)(B); Penal Code
Section 1370].
Notice of the disappearance or transfer must be made to:
1. The court initially ordering the patient’s commitment;
2. The district attorney for the county that ordered the
commitment; and
3. Governmental law enforcement agencies designated
by the physician in charge of the patient or the person
in charge of the facility.
This notice must be made within 24 hours of the patient’s
disappearance or transfer.
[Welfare and Institutions Code Section 5328.3(b)(1); see
also 45 C.F.R. Section 164.512(a) and (f)]
The following information must be documented in the
patient’s medical record:
1. The date and circumstances under which the report
was made;
2. The names and relationships to the patient, if any,
of persons or agencies to whom the report was
made; and
3. The specific information disclosed.
[Welfare and Institutions Code Section 5328.6]
LAW ENFORCEMENT OFFICER WITH A WARRANT
A facility must advise a law enforcement officer who
personally lodges a warrant of arrest or an abstract of such
a warrant showing that the person sought is wanted for a
serious felony (as defined in Penal Code Section 1192.7) or
a violent felony (as defined in Penal Code Section 667.5),
whether the person named in the arrest warrant is currently
in the facility. The information to be disclosed is limited to
whether or not the person named in the warrant is in the
facility.
An officer may not enter the facility to arrest the person
without obtaining a valid search warrant or the permission
of the facility.
For purposes of this law, “facility” means:
1. A state hospital as defined in Welfare and Institutions
Code Section 4001;
2. A general acute care hospital as defined in Health and
Safety Code Section 1250(a), solely with regard to
information pertaining to a person with mental illness
subject to LPS;
3. An acute psychiatric hospital as defined in Health and
Safety Code Section 1250(b);

CHA Mental Health Law Manual 2019
6.12
©CALIFORNIA HOSPITAL ASSOCIATION
4. A psychiatric health facility as defined in Health and
Safety Code Section 1250.2;
5. A mental health rehabilitation center as defined in
Welfare and Institutions Code Section 5675; and
6. A skilled nursing facility with a special treatment
program for individuals with mental illness, as
described in Title 22, California Code of Regulations,
Sections 51335 and 72445-72475.
[Welfare and Institutions Code Section 5328(a)(20); see also
45 C.F.R. Section 164.512(a) and (f)]
PATIENT HAD WEAPON CONFISCATED
A hospital must report the release of a patient who had a
weapon confiscated to the confiscating law enforcement
agency. (See “Reporting to Confiscating Law Enforcement
Agency,” page 7.37.)
I. Minor’s Medical Records
In general, state and federal health information privacy
laws apply equally to the records of adults and the records
of minors. Minors’ health information enjoys the same
legal privacy protections as that of adults, and the health
information of minors may generally be used and disclosed
in the same ways as that of adults. However, the law
often gives parents or guardians the ability to exercise the
privacy rights of minors on their behalf. This is not always
the case, though, as described more fully below. [45 C.F.R.
Section 164.502(g); Civil Code Section 56.11(c); Health and
Safety Code Sections 123110 and 123115; Welfare and
Institutions Code Section 5328(a)(4)]
Note that disclosures may be made to family and close
personal friends of minors as described In E.“Family and
Friends: Patients Covered by CMIA,” page6.7.
GENERAL RULE: ACCESS TO RECORDS
CORRESPONDS TO CONSENT FOR TREATMENT
The laws governing who may access a minor’s medical
information and disclose a minor’s medical information
to third parties correspond with the laws governing who
may consent to the treatment that the information covers.
Chapter 2 describes the laws about minors’ consent
to treatment.
Access to a minor’s medical and dental records may not
be denied to a parent solely because that parent is not
the minor’s custodial parent [Family Code Section 3025].
However, this law does not give noncustodial parents the
right to access medical records where the minor has the
legal authority to consent to the treatment.
Special laws apply to records of dependent children of the
juvenile court and foster children. The hospital’s privacy
officer or legal counsel should be consulted.
Minor Has Legal Authority to Consent to the Treatment
If the minor has the authority to consent to medical
treatment under state law, then the minor is generally the
person authorized to have access to the records regarding
the treatment, and to decide whether the records may
be released to others (including the parent or other legal
representative). This is true even where the parent or other
legal representative, as a practical matter, solicits and
consents to the treatment. However, the minor may request
that the parent or other legal representative be treated
as the minor’s personal representative under HIPAA. This
means that the minor can request that the parent be told
about the minor’s health conditions and have access to the
minor’s record.
Exceptions. There are several situations in which the minor
has the legal authority to consent to medical treatment, but
the provider is authorized, or required, to provide specified
information to the parents. These situations involve self-
sufficient minors, minor victims of sexual assault, minors
receiving outpatient mental health treatment or residential
shelter services, and minors receiving substance use
disorder treatment. Chapter 2 contains more information
about these situations.
Minor Does Not Have Legal Authority to Consent to the
Treatment
If the parent (or other legal representative) has the authority
to consent to medical treatment for a minor, then the parent
is generally the person authorized to have access to the
minor’s records about the treatment, and to decide whether
the records may be released to others. Three exceptions
are described below.
Exception: Parent Assents to Confidentiality. A parent
(or other legal representative) may assent to an agreement
of confidentiality between a health care provider and the
minor with respect to a health care service for which the
minor does not have the legal authority to consent. In this
case, the provider may not disclose information to the
parent without the minor’s authorization.
Exception: Access by Parent Would Be Detrimental
to Minor. A health care provider may deny a parent (or
other legal representative) access to the minor’s records,
even though the parent had the authority to consent to
the treatment, if the provider determines that access to

Chapter 6 — Health Information Privacy Basics CHA
6.13
©CALIFORNIA HOSPITAL ASSOCIATION
the records by the parent would have a detrimental effect
on the provider’s professional relationship with the minor
patient, or the minor’s physical safety or psychological
well-being. The decision of the health care provider about
whether or not to make the minor’s records available will
not result in any liability to the provider, unless the decision
is found to be in bad faith.
Exception: Dependent Child of the Juvenile Court/
Foster Child. A minor may be removed from the physical
custody of his or her parent or guardian by the juvenile
court because the minor has suffered, or there is a
substantial risk that the minor will suffer, abuse or harm.
Such a minor is called a “dependent child of the court” for
a foster child. A psychotherapist may not disclose mental
health information about the minor to the parent, or to
third parties based on the parent’s authorization. For a
detailed discussion of this law, see CHA’s California Health
Information Privacy Manual or Minors and Health Care Law
Manual.
Cautions
“Mixed” Medical Record. A minor’s medical record may
contain information about treatment that the minor may
consent to, and information about treatment that the parent
or other legal representative must consent to. In such
cases, the health care provider should take extra care to
ensure that records are released appropriately. Records
released to the wrong person, or at the wrong person’s
request, may constitute a privacy breach.
Billing for Services. If a minor has the legal authority to
consent to medical treatment, then the minor is responsible
for payment. Health care providers should establish a
system to ensure that they do not bill parents for services
for which the minor may lawfully consent, as this may be
considered a breach of the minor’s privacy rights (unless
the minor’s consent to bill is obtained). The provider may bill
insurance companies — it is the insurer’s responsibility to
insure that Explanation of Benefits (EOB) forms are not sent
to parents for services the minor can consent to.
Medi-Cal has a special program to pay for some services
for which minors may consent regardless of parental
income or assets, and without contacting the parents.
(See C.“Financial Responsibility for Treatment of Minors,”
page2.25.)
V. SEARCHING PATIENTS AND THEIR
BELONGINGS
A. Culture of Safety and Right to Privacy
Hospitals are responsible for keeping their patients and
employees safe. (See, for example, 42 C.F.R Section
482.13(c)(2) and Title 8, California Code of Regulations,
Section 3342.) At times, this may require searching a
patient and his or her belongings.
Hospitals should have a form and a process to document
the belongings patients bring to the hospital — mundane
items as well as valuables — and where they will be
kept (such as at the patient’s bedside or in the hospital’s
safe). Chapter 20 of CHA’s Consent Manual describes
the legal limitations on a hospital’s liability for patients’
personal belongings and includes a suggested process
for inventorying and documenting belongings. Chapter 11
of CHA’s Consent Manual contains sample language for
the hospital’s “Conditions of Admissions” form informing
the patient that the hospital is not liable for the patient’s
personal articles that are not deposited with the hospital
for safekeeping (such as eyeglasses, dentures, hearing
aids, cell phones, laptops, etc.). This portion of this manual
addresses the purposeful search of patients and their
belongings for potentially dangerous items rather than the
routine cataloguing of patients’ belongings.
There is no state or federal law specifically addressing
patient searches. However, state and federal laws
acknowledge that patients have a general right to privacy.
This right at times must give way to the hospital’s obligation
to keep its patients and employees safe. Hospitals may
wish to develop and implement a patient search policy
to guide clinicians in the hospital’s requirements for, and
process of, searching patients and their belongings. The
policy should address situations where a patient does not
cooperate with a search.
B. When to Search
Health care facilities or units that care for patients who
have been detained as a danger to self or others or
gravely disabled will generally search all patients and their
belongings. Even if a particular patient is not considered to
be potentially dangerous, the hospital cannot take the risk
that another patient in the same room or common area will
obtain a potentially harmful item.
Health care facilities or units that do not care for patients
who may be a danger to self or others or gravely
disabled will usually conduct searches only upon specific

CHA Mental Health Law Manual 2019
6.14
©CALIFORNIA HOSPITAL ASSOCIATION
justification. These facilities may wish to document the
justification in the patient’s medical record or include a
space to document the justification on a search/inventory
form they develop.
If the patient has (or if there is a suspicion that a patient
has) firearms or other dangerous weapons, hospital
policy may require that staff contact security and/or law
enforcement immediately. Clinical staff should not be put
in the position of attempting to remove weapons from a
patient.
C. Process of Search
The patient should be informed that the hospital is required
to keep the patient, other patients, staff and visitors safe,
and that any belongings not sent home with family or
friends may be searched to remove any objects that may
be used in an unsafe or disruptive manner. In addition,
hospitals are required to protect the privacy of other
patients, so the use of cell phones and cameras may be
restricted. Efforts should be made to accomplish the search
in a consensual, non-forcible manner.
Hospital policy should describe when a full search is
required (as opposed to having the patient empty his
or her pockets and submit to a “patdown”). If a full
search is necessary, hospitals typically have the patient
remove all street clothing and change into a paper or
cloth gown, putting their clothing and other belongings
into a bag provided by the hospital. The patient should
be given as much privacy to undress as is safe. An
employee who observes the patient should be of the
same gender as the patient. A hospital employee will then
inventory the possessions (including the contents of any
suitcases, purses and bags). If the patient is able and
willing to cooperate, this should be done in the presence
of the patient. Hospitals often require that two staff
members participate in the search; both should sign the
inventory form.
If a patient wishes to wear his or her own clothes while
hospitalized, the searched clothing may be returned to the
patient if it is safe (no drawstrings, belts, neckties, etc.). If
the patient wishes a friend or family member to take home
any items, this should be documented. The hospital may
wish to have the patient or family member sign for the
item(s) taken home. The patient should be told where the
belongings will be kept and how and when he or she may
access them.
A body cavity search is generally performed only when
the attending physician believes that this level of search is
warranted. This type of search should only be conducted
by a physician, usually in the presence of a second
clinician. At least one of the clinicians should be the same
gender as the patient.
If a patient refuses to cooperate with a needed search, and
holding or restraint is necessary to accomplish it, staff must
follow the hospital restraint policy. Chapter 5 describes
all state and federal laws governing the use of seclusion
and restraint.
The search should be documented so that it is not
unnecessarily repeated.
D. Potentially Dangerous Items
Hospitals should develop a policy about storage,
disposition or destruction of weapons, legal or
illegal drugs, or other potentially harmful objects or
substances encountered.
E. Related Laws
Mental health patients covered by the
Lanterman-Petris-Short Act have certain rights, including
the right to wear their own clothing; the right to have
access to storage space for personal belongings; and the
right to keep and use their own personal possessions,
including toilet articles. These rights may be denied for
good cause. There are documentation and reporting
requirements when rights are denied. A complete
description of mental health patient rights is found in
chapter 4.
In addition, certain mental health patients are prohibited by
law from possessing firearms and other deadly weapons
for a specified period of time after their treatment. The law
requires hospitals to report these patients to the California
Department of Justice. Chapter 7 contains complete
information about weapons prohibitions laws.

Chapter 7 — Contents
©CALIFORNIA HOSPITAL ASSOCIATION
7 Reporting Assaults, Potentially
Dangerous Patients and Firearms
Prohibitions
I. REPORTS REQUIRED BY LAW .................. 7.1
A. Scope of Chapter...........................................7.1
B. Confidentiality Considerations .....................7.1
Child Abuse ...................................................... 7.1
Other Abuse
.....................................................7.1
C. Informing the Patient of Reporting ..............7.1
D. Summary of Assault and Abuse
Reporting Requirements
...............................7.2
II. STATUTORY DUTY TO REPORT CERTAIN
INJURIES AND CONDITIONS..................... 7.2
A. Nature of the Duty to Report ........................7.2
B. Failure to Report ............................................ 7.2
Criminal Liability ................................................ 7.2
Civil Liability
......................................................7.2
III. REPORTING INJURIES BY FIREARM OR
ASSAULTIVE OR ABUSIVE CONDUCT
(“SUSPICIOUS INJURIES”)
........................ 7.3
A. Who Must Report...........................................7.3
B. Reports Required to be Made ......................7.3
Related Reporting Requirements .......................7.3
C. Definitions ......................................................7.4
D. Timing and Form of Report ..........................7.4
E. Notification of Patient/Victim That
Report Will be Made
......................................7.5
F. Medical Record Documentation ..................7.5
G. Immunity From Liability ................................7.5
H. Confidentiality ................................................7.5
IV. SEXUAL ASSAULT AND RAPE ................... 7.5
A. Reporting Requirements ...............................7.5
B. Examination or Referral of Victims ..............7.5
C. Required Examination Report Forms ..........7.6
Forms ...............................................................7.6
D. Consent to the Forensic Examination .........7.6
E. Protocol for Examination and
Treatment of Victim
.......................................7.6
Informational Card ............................................7.6
Postcoital Contraception
...................................7.6
Sexual Assault Counselor
..................................7.6
Notify Rape Victim Counseling Center
...............7.7
Opportunity to Shower/Bathe
............................7.7
Notify Law Enforcement Agency
........................7.7
F. Confidentiality ................................................7.7
G. Forensic Exam of Suspect ............................7.7
V. CHILD ABUSE AND NEGLECT ................... 7.8
A. Basic Reporting Requirement ......................7.8
Unsuitable Home ..............................................7.8
Emotional Damage
...........................................7.8
B. Definitions ......................................................7.8
C. Persons Required or Permitted to
Report
..........................................................7.10
Mandated Reporters ....................................... 7.10
Voluntary Reporters
........................................7.11
Selection of a Person to Report
......................7.11
D. Reporting to Law Enforcement ..................7.11
Content of Report ........................................... 7.11
How Reports are Made
................................... 7.12
Forensic Medical Reports
...............................7.12
Consent for Abuse-Related Exams
..................7.12
E. Special Situations Regarding Reporting ...7.13
When a Child Seeks Treatment for a
Sexually Transmitted Disease, Pregnancy
or Abortion
.....................................................7.13
When Treating Substance Use Disorder
Patients
..........................................................7.14
Maternal Substance Abuse
.............................7.14
Safe Surrender of a Newborn
..........................7.15
Homeless Children
..........................................7.15
F. Privileges Inapplicable ................................7.15
G. Disclosure and Follow-Up Procedures ......7.16
Disclosure to Investigator ...............................7.16
Disclosure to Licensing Agency
.......................7.17

Chapter 7 — Contents
©CALIFORNIA HOSPITAL ASSOCIATION
CHA Mental Health Law Manual 2019
H. Immunity From Liability ..............................7.17
Mandated Reporters ....................................... 7.17
Voluntary Reporters
........................................7.18
Immunity for Providing Access to the Victim
....7.18
Immunity for Photographing of Suspected
Abuse
.............................................................7.18
I. Confidentiality of Reports ...........................7.18
J. Sanctions for a Failure to Report ...............7.18
K. Employer Obligations ..................................7.19
Obtain Employees’ Acknowledgment of
Reporting Obligations
.....................................7.19
Train Employees
.............................................7.19
VI. ABUSE OF ELDERS AND DEPENDENT
ADULTS
................................................ 7.19
A. Introduction..................................................7.19
Who is an Elder or Dependent Adult? ..............7.20
B. Definitions ....................................................7.20
C. Mandatory Reporting of Abuse ..................7.23
Mandated Reporters ....................................... 7.23
What Triggers Reporting Obligation
................. 7.24
D. Nonmandated Reporting ............................7.24
By Mandated Reporters .................................. 7.25
By Other Persons
...........................................7.25
E. Making Reports ...........................................7.25
To Whom Reports are Made; Time Frames ...... 7.25
Telephone or Internet Report
...........................7.26
Written Report
................................................7.26
Selection of a Person to Report
......................7.27
F. Notification of Patient/Victim That
Report Will be Made
....................................7.27
G. Forensic Medical Reports ...........................7.27
Documentation in the Medical Record ............. 7.27
H. Sanctions for a Failure to Report ...............7.27
I. Immunity From Liability ..............................7.28
Providing Access to the Victim ........................ 7.28
Photographing of Suspected Abuse
................7.28
Attorneys’ Fees
...............................................7.28
Employers
......................................................7.28
J. Confidentiality of Reports; Disclosures .....7.28
Disclosure of Information Regarding Abuse .....7.29
Disclosure of Reporter’s Identity
...................... 7.29
K. Employees’ Acknowledgment of
Reporting Obligations
.................................7.29
L. Employer Obligation to Train
Employees
....................................................7.29
M. Federal Requirements ................................. 7.30
Reporting .......................................................7.30
Notifying Employees and Others of
Reporting Obligations
.....................................7.30
Nonretaliation and Signage
.............................7.30
N. Detention of Endangered Adults ................7.30
VII. INJURY OR CONDITION IN A PATIENT
RECEIVED FROM A LICENSED HEALTH
FACILITY RESULTING FROM NEGLECT
OR ABUSE
............................................. 7.31
A. Statutory Duty of Hospital and
Physician to Report
.....................................7.31
Contents of Report .........................................7.31
Notification of Patient/Victim That Report
Will Be Made
..................................................7.31
B. Optional Reporting by Nurses and
Social Workers
.............................................7.31
C. Immunity From Liability ..............................7.31
VIII. SCREENING FOR DOMESTIC
VIOLENCE ........................................... 7.32
A. Screening Policies .......................................7.32
B. Domestic Violence Indicators ....................7.32
C. Reporting Requirements ............................. 7.32
D. Forms ............................................................7.33
IX. POTENTIALLY DANGEROUS PATIENTS:
DUTY TO WARN POTENTIAL VICTIMS
AND NOTIFY LAW ENFORCEMENT
.......... 7.33
A. Duty to Warn Potential Victims ..................7.33
B. Duty to Notify Law Enforcement
Agency
..........................................................7.33
C. Immunity From Liability ..............................7.34
Immunity for Psychotherapists .......................7.34
Immunity for Psychotherapists and Others
......7.35
D. Documenting Decisions ............................. 7.35
X. NOTIFYING LAW ENFORCEMENT
OFFICERS OF PATIENT PRESENCE,
RELEASE OR DISAPPEARANCE
.............. 7.36

©CALIFORNIA HOSPITAL ASSOCIATION
Chapter 7 — Contents
Chapter 7 — Reporting Assaults, Potentially Dangerous Patients and Firearms Prohibitions CHA
FORMS & APPENDICES
13-4 Notice to Law Enforcement Agency: Release of
Person From Hospital From Whom a Firearm or
Other Deadly Weapon Was Confiscated
13-5
S
Notice to Patient: Procedure for Return of
Confiscated Weapon(s)
19-2 Employee Acknowledgment of Child Abuse and
Neglect Reporting Obligations
19-4 Employee Acknowledgment of Elder and
Dependent Adult Abuse Reporting Obligations
19-A Assault and Abuse Reporting Requirements
Forms and Appendices can be found at the back of the manual and
online for CHA members at www.calhospital.org/free-resources.
“S” denotes that the form is provided in English and Spanish.
XI. PATIENTS PROHIBITED FROM
POSSESSING FIREARMS OR OTHER
DEADLY WEAPONS
................................ 7.36
A. Prohibition Against Possessing or
Purchasing a Firearm or Other Deadly
Weapon
........................................................7.36
B. Persons Subject to the Prohibition ...........7.36
C. Reporting Requirements ............................. 7.37
Reporting to California Department of
Justice
............................................................7.37
Reporting to Confiscating Law Enforcement
Agency
........................................................... 7.37
D. Patient Notification Obligations .................7.37
Notice to Patient ............................................. 7.37
Procedure for Return of Weapon
.....................7.38
E. Confidentiality Considerations ...................7.38
F. Immunity From Liability ..............................7.38

7.1
©CALIFORNIA HOSPITAL ASSOCIATION
7 Reporting Assaults, Potentially
Dangerous Patients and Firearms
Prohibitions
I. REPORTS REQUIRED BY LAW
A. Scope of Chapter
Hospitals and other health care providers are required by
law to make certain reports, many of which arise in the
context of mental health services. This chapter addresses
the laws that require reporting of assault and abuse,
including injuries by deadly weapon, rape, child abuse,
elder abuse, dependent adult abuse and injuries/conditions
resulting from abuse or neglect found in a patient received
from a health facility, such as a skilled nursing or community
care facility. These reports must be made whether the
patient is assaulted inside or outside the hospital, if the
triggers for the reporting requirement are met.
NOTE: This manual does not address required reporting of
injured employees to Cal/OSHA, law enforcement agencies,
or CDPH. CHA publishes other guidebooks and manuals
that address employer obligations, including Healthcare
Workplace Violence Prevention and The Cal/OSHA
Safe Patient Handling Regulation guidebook. Visit www.
calhospital.org/publications for information about other
CHA publications.
B. Confidentiality Considerations
State and federal health information privacy laws permit
the disclosure of patient-identifiable information to report
suspicious injuries and suspected abuse as described in
this chapter [45 C.F.R. Section 164.512(a) and (c); Civil
Code Section 56.10(c)(14) and (22)]. The special restrictions
that apply to certain mental health patient information and
records, federally-assisted substance use disorder program
records, and HIV test results must be followed, if applicable
(see chapter 6). In all cases, disclosure should be limited
to the minimum amount of information necessary to fulfill
the reporting requirement. Specifics about the patient’s
diagnosis, medications, and other details are ordinarily not
required to be disclosed to fulfill reporting obligations.
CHILD ABUSE
HIPAA contains a specific provision allowing disclosure
of protected health information (PHI) to appropriate
government authorities authorized by law to receive
reports of child abuse or neglect [45 C.F.R. Section
164.512(b)(1)(ii)].
OTHER ABUSE
HIPAA authorizes disclosure of information about
individuals reasonably believed to be victims of abuse,
neglect or domestic violence to government authorities
legally authorized to receive such reports as follows:
1. To the extent required by law; or
2. If the individual agrees to the disclosure; or
3. To the extent disclosure is expressly authorized by law
and either:
a. Disclosure is necessary to prevent serious harm to
the individual or other potential victims; or
b. The individual is unable to agree to due to
incapacity, the government authority represents
that the PHI is not intended to be used against the
individual, and an immediate enforcement activity
depends upon the disclosure and would be
materially and adversely affected by waiting until
the individual is able to agree to the disclosure.
[45 C.F.R. Section 164.512(c)(1)]
Therefore, if state law requires a report, it may be made. If
state law merely authorizes (but does not require) a report,
it may be made only if the criteria in paragraph 3.a. or 3.b.
are satisfied.
C. Informing the Patient of Reporting
If the patient was a victim of abuse, neglect or domestic
violence (except child abuse or neglect), the health care
provider must promptly inform the patient that a report has
been or will be made, unless:

CHA Mental Health Law Manual 2019
7.2
©CALIFORNIA HOSPITAL ASSOCIATION
1. The provider believes, in the exercise of professional
judgment, that informing the patient would place him
or her at risk of serious harm; or
2. The provider would be informing a personal
representative, and the provider reasonably believes
the personal representative is responsible for the
abuse, neglect or other injury, and that informing the
personal representative would not be in the patient’s
best interest as determined by the provider in the
exercise of professional judgment. [45 C.F.R. Section
164.512(c)(2)]
Verbal notification to the patient is sufficient. A report
must be made even if the patient objects. The health
care provider may wish to suggest that the victim go to
a protected environment due to the risk of the abuser’s
retaliation after the report is made.
If the patient was not a victim of abuse, neglect or
domestic violence (for example, the patient was shot by
accident or attempted suicide), the patient need not be
notified that a report has been or will be made.
D. Summary of Assault and Abuse Reporting
Requirements
CHA has included a table at the end of this manual
titled “Assault and Abuse Reporting Requirements”
(CHA Table 19-A) summarizing assault and abuse
reporting requirements.
II. STATUTORY DUTY TO REPORT CERTAIN
INJURIES AND CONDITIONS
A. Nature of the Duty to Report
California law imposes a duty on hospitals and physicians
to make oral and written reports to local authorities when
a person comes, or is brought to, a hospital, or is under
the professional care of a physician, and the person is
suffering from:
1. An injury caused by a firearm or assaultive or abusive
conduct (see III.“Reporting Injuries by Firearm or
Assaultive or Abusive Conduct (“Suspicious Injuries”),”
page7.3);
2. Sexual assault/rape (see IV.“Sexual Assault and Rape,”
page7.5);
3. Child abuse (see V.“Child Abuse and Neglect,”
page7.8);
4. Abuse of elders and dependent adults (see VI.“Abuse
of Elders and Dependent Adults,” page7.19);
5. An injury or condition resulting from neglect or abuse
in a patient transferred from another health facility (see
VII.“Injury or Condition in a Patient Received From
a Licensed Health Facility Resulting From Neglect or
Abuse,” page7.31).
In addition, hospitals must report violence against hospital
personnel in specified circumstances. These reporting
requirements are described in CHA’s Healthcare Workplace
Violence Prevention guidebook. Go to www.calhospital.org/
wvp-guidebook for more information or to order.
B. Failure to Report
CRIMINAL LIABILITY
A person required to report injuries by firearms or by
assaultive or abusive conduct (see III.“Reporting Injuries
by Firearm or Assaultive or Abusive Conduct (“Suspicious
Injuries”)” below) but who fails to do so is guilty of a
misdemeanor, punishable by imprisonment in the county
jail not exceeding six months or by a fine not exceeding
$1,000, or both.
A mandated reporter who fails to report an incident of
known or reasonably suspected child abuse or neglect
(see V.“Child Abuse and Neglect,” page7.8) is also
guilty of a misdemeanor (same punishment as above). The
law contains similar penalties for failure to report elder
or dependent adult abuse (see VI.“Abuse of Elders and
Dependent Adults,” page7.19).
[Penal Code Sections 11162 and 11166; Welfare and
Institutions Code Section 15630(h)]
CIVIL LIABILITY
In Landeros v. Flood, 17 Cal.3d 399 (1976), the California
Supreme Court ruled that an abused child may recover
damages for subsequent injuries suffered at the hands of
his or her parents, from a hospital or physician if it can be
proven that the hospital or physician knew, or should have
known, that the child was a victim of child abuse or neglect,
but failed to report the abuse in accordance with the law.
This ruling may be extended to other situations, such as
imposition of civil liability for failure to report elder abuse or
an injury or condition resulting from neglect or abuse in a
patient transferred from another health facility.

Chapter 7 — Reporting Assaults, Potentially Dangerous Patients and Firearms Prohibitions CHA
7.3
©CALIFORNIA HOSPITAL ASSOCIATION
III. REPORTING INJURIES BY FIREARM OR
ASSAULTIVE OR ABUSIVE CONDUCT
(“SUSPICIOUS INJURIES”)
Health practitioners employed by specified entities are
required to make reports to a local law enforcement agency
when they treat persons with specified injuries (sometimes
called “suspicious injury reports”). Additionally, every
physician treating such persons also has a duty to make
a report, even if the physician is not an employee. [Penal
Code Sections 11160 and 11161]
A. Who Must Report
Reports must be made by:
1. A health practitioner employed in a health facility,
clinic, physician’s office, local or state public health
department, local government agency, or a clinic or
other type of facility operated by a local or state public
health department; and
2. A physician who has an injured patient under his or her
charge or care.
For purposes of this law, “employed by a local government
agency” includes an employee of an entity under contract
with a local government agency to provide medical services.
This would include paramedics and emergency medical
technicians working for ambulance companies or hospitals
that have a contract with a local government agency. [Penal
Code Section 11160(i)]
The reporting duties under this law apply to each individual.
However, when two or more persons who are required
to report are present and jointly have knowledge of a
reportable event, they may agree among themselves to
report as a team and make a single report. The team may
mutually select a member of the team to make a report by
telephone and a single written report. The written report
must be signed by the selected member of the reporting
team. A member who has knowledge that the member
designated to report has failed to do so must thereafter
make the report.
California’s legislative counsel has opined that licensed
clinical social workers are not required to report suspicious
injuries because they do not provide medical services for a
physical condition [Opinion dated 4-1-98].
No supervisor or administrator may impede or inhibit the
reporting duties required under the law, and no person
making a report may be subject to any penalties for making
the report. However, internal procedures to facilitate
reporting and apprise supervisors and administrators of
reports may be established. The internal procedures must
not require any employee required to make a report to
disclose his or her identity to the employer.
B. Reports Required to be Made
A report must be made when a health practitioner, in his
or her professional capacity or within the scope of his or
her employment, provides medical services for a physical
condition to a patient whom he or she knows or reasonably
suspects is a person:
1. Suffering from any wound or other physical
injury where the injury is by means of a firearm,
whether inflicted by the patient him/herself or by
another person.
2. Suffering from any wound or other physical injury
inflicted upon the person where the injury is the result
of assaultive or abusive conduct.
[Penal Code Section 11160]
The duty to report arises where the health practitioner
provides medical services to a patient for any physical
condition, not just the condition or injury arising from the
assault, battery or firearm incident. A report must be made
even if the injury is not serious. So, for example, if a patient
in a mental health facility is assaulted by another patient
and requires any type of treatment for a physical injury –
even if relatively minor — a report must be made.
A report must also be made by every physician who has
such a person under his or her charge or care [Penal Code
Section 11161(a)].
RELATED REPORTING REQUIREMENTS
If a patient or staff member is assaulted or abused in
a health facility and medical services are provided to
treat the injury, a report must be made under the law
discussed above as well as the laws that are specific to
violence against hospital personnel (see CHA’s Healthcare
Workplace Violence Prevention guidebook for more
information). If death or significant injury occurs to a patient
or staff member resulting from a physical assault on the
grounds of a facility, an adverse event must be reported
to the California Department of Public Health (CDPH) (see
VII.“CDPH Adverse Events Reporting,” page8.7), as well
as reporting under the law described above.

CHA Mental Health Law Manual 2019
7.4
©CALIFORNIA HOSPITAL ASSOCIATION
C. Definitions
“Assaultive or abusive conduct” includes any of the
following offenses, as they are defined in the Penal Code:
1. Murder
2. Manslaughter
3. Mayhem
4. Aggravated mayhem
5. Torture
6. Assault with intent to commit mayhem, rape, sodomy
or oral copulation
7. Administering controlled substances or anesthetic to
aid in commission of a felony
8. Battery
9. Sexual battery
10. Incest
11. Throwing any vitriol, corrosive acid or caustic chemical
with intent to injure or disfigure
12. Assault with a stun gun or taser
13. Assault with a deadly weapon, firearm, assault weapon
or machine gun, or by means likely to produce great
bodily injury
14. Rape
15. Spousal rape
16. Procuring any female to have sex with another man
17. Child abuse or endangerment
18. Abuse of spouse or cohabitant
19. Sodomy
20. Lewd and lascivious acts with a child
21. Oral copulation
22. Sexual penetration by a foreign object
23. Elder abuse
24. An attempt to commit any crime specified in the
offenses listed above.
[Penal Code Section 11160(d)]
“Health practitioner” is defined in the law to include:
1. A physician, surgeon, psychiatrist, psychologist,
dentist, resident, intern, podiatrist, chiropractor,
licensed nurse, dental hygienist, optometrist, marriage
and family therapist, clinical social worker or any other
person who is currently licensed under Business and
Professions Code Section 500 et seq.;
2. An emergency medical technician I or II, paramedic or
other person certified pursuant to Health and Safety
Code Section 1797 et seq.;
3. A psychological assistant registered pursuant to
Business and Professions Code Section 2913;
4. A marriage and family therapist trainee, as defined in
Business and Professions Code Section 4980.03(c);
5. An unlicensed associate marriage and family therapist
registered under Business and Professions Code
Section 4980.44;
6. A state or county public health employee who treats a
minor for venereal disease or any other condition;
7. A coroner; or
8. A medical examiner or any person who performs
autopsies.
[Penal Code Sections 11162.5(a) and 11165.7]
“Injury” does not include any psychological or physical
condition brought about solely through the voluntary
administration of a narcotic or restrictive dangerous drug
[Penal Code Section 11160(c)].
“Reasonably suspects” means that it is objectively
reasonable for a person to entertain such a suspicion,
based upon facts that could cause a reasonable person in
a like position, drawing when appropriate from his or her
training and experience, to suspect [Penal Code Section
11162.5(d)].
D. Timing and Form of Report
A report by telephone must be made immediately
or as soon as practically possible to a local law
enforcement agency.
A written report must be prepared and sent to a local
law enforcement agency within two working days. The
California Office of Emergency Services (Cal OES)
has developed a standard form to be used by health
practitioners. The “Suspicious Injury Report” (Cal OES
2-920) may be found at www.ccfmtc.org.
A report must be made even if the person who suffered the
injury has died, regardless of whether or not the injury or
assaultive or abusive conduct was a factor contributing to
the death, and even if the evidence of the conduct of the
perpetrator of the injury or assaultive or abusive conduct
was discovered during an autopsy.

Chapter 7 — Reporting Assaults, Potentially Dangerous Patients and Firearms Prohibitions CHA
7.5
©CALIFORNIA HOSPITAL ASSOCIATION
E. Notification of Patient/Victim That Report Will
be Made
The patient usually must be notified that a report has
been or will be made. (See C.“Informing the Patient
of Reporting,” page7.1, for information about this
requirement.)
F. Medical Record Documentation
Penal Code Section 11161 recommends (but does not
require) that the medical record of a person who is the
subject of a report include the following:
1. Any comments by the injured person about past
domestic violence or the name of any persons
suspected of inflicting the wound, other physical injury,
or assaultive or abusive conduct upon the person.
2. A map of the injured person’s body showing and
identifying injuries and bruises.
3. A copy of the law enforcement reporting form.
Hospitals may wish to consider putting the forensic medical
reports in a separate section of the medical record to
prevent routine copying and disclosure of these reports for
purposes not related to the criminal justice system, and to
prevent improper release to unauthorized persons.
G. Immunity From Liability
A health practitioner who makes a report of injury or abuse
as required or authorized by law shall not incur civil or
criminal liability as a result. Furthermore, the practitioner
shall not incur civil or criminal liability as a result of providing
access to the victim at the request of an adult protective
services agency or a law enforcement agency.
Health practitioners who have made reports and who incur
attorneys’ fees as a result of legal action taken against
them on the basis of making the report may present a
claim to the California Board of Control for their reasonable
attorney’s fees if the health practitioner prevails in the
legal action.
Immunity is also provided in connection with the taking of
photographs of a person about whom a report is made or
for disseminating the photographs to local law enforcement
with the reports. However, no immunity is provided for any
other use of the photographs.
No employee may be discharged, suspended, disciplined
or harassed for making a report pursuant to this law.
[Penal Code Sections 11161.9 and 11163]
H. Confidentiality
The reports required by this law must be kept confidential
by the health facility, clinic or physician’s office that
submitted the report, and by local law enforcement
agencies [Penal Code Section 11163.2(b)].
However, counties may establish domestic violence death
or elder death review teams, which may include medical
personnel with expertise in domestic violence. Each
organization represented on the team may share otherwise
confidential information, upon written request, with other
team members if pertinent to the review. This includes
medical information covered by the Confidentiality of
Medical Information Act or the Lanterman-Petris-Short Act.
[Penal Code Sections 11163.3 and 11174.8]
In no case shall the person suspected of the assaultive or
abusive conduct or his or her attorney be allowed access
to the injured person’s whereabouts.
In a court proceeding or administrative hearing, neither the
physician-patient privilege nor the psychotherapist-patient
privilege applies to the information required to be reported
under this law [Penal Code Section 11163.2(a)].
IV. SEXUAL ASSAULT AND RAPE
A. Reporting Requirements
Cases of sexual assault and rape must be reported under
Penal Code Section 11160 (described in III.“Reporting
Injuries by Firearm or Assaultive or Abusive Conduct
(“Suspicious Injuries”),” page7.3).
B. Examination or Referral of Victims
Penal Code Section 13823.9(c) requires each county
to designate at least one general acute care hospital to
perform forensic examinations on victims of sexual assault,
including child molestation. All other public and private
general acute care hospitals must either comply with the
legal standards, protocols and guidelines in examining or
treating victims of sexual assault and attempted sexual
assault (including child molestation) or “adopt a protocol
for immediate referral of these victims to a local hospital
that so complies and shall notify local law enforcement
agencies, the district attorney and local victim assistance
agencies of the adoption of the referral protocol.” [Health
and Safety Code Section 1281].

CHA Mental Health Law Manual 2019
7.6
©CALIFORNIA HOSPITAL ASSOCIATION
C. Required Examination Report Forms
Each physician or nurse who conducts an examination for
evidence of a sexual assault or attempted sexual assault
(including child molestation) must use the standard form(s)
adopted by the California Office of Emergency Services
(Cal OES). The health care professional must make the
observations and perform the tests required to complete
the form if the patient consents. Reports must be made on
the forms listed below. [Penal Code Section 13823.5]
FORMS
The forms are:
1. Cal OES 2-923: “Forensic Medical Report: Acute
(less than 72 hours) Adult/Adolescent Sexual Assault
Examination”
2. Cal OES 2-924: “Forensic Medical Report: Abbreviated
Adult/Adolescent Sexual Assault Examination”
3. Cal OES 2-925: “Forensic Medical Report: Nonacute
(greater than 72 hours) Child/Adolescent Sexual
Abuse Examination”
4. Cal OES 2-930: “Forensic Medical Report: Acute
(less than 72 hours) Child/Adolescent Sexual Abuse
Examination”
Copies of these forms and instructions are available
at www.ccfmtc.org. The website also has instructions,
protocols for examination of victims, and other information.
For information about the forms or assistance in completing
them, contact the California Clinical Forensic Medical
Training Center at (916) 930-3080 or see their website at
www.ccfmtc.org.
D. Consent to the Forensic Examination
Forms Cal OES 2-923, OES 2-924, 2-925 and 2-930
contain distinct consent requirements in addition to those
generally included in consent forms used by emergency
departments, including:
1. An acknowledgment of the provider’s duty to
report to law enforcement authorities the name and
whereabouts of any persons who are victims of sexual
assault (see A.“Reporting Requirements,” page7.5).
2. A consent to a separate medical examination for
evidence of sexual assault at public (county) expense
to discover and preserve evidence of the assault.
Consent for a physical examination, treatment and
collection of evidence is required [Penal Code Section
13823.11]. Consent to an examination for evidence
of sexual assault must be obtained prior to the exam
and must include written documentation of each of
the following:
1. Examination for the presence of injuries sustained as a
result of the assault.
2. Examination for evidence of sexual assault and
collection of physical evidence.
3. Photographs of injuries.
The victim (or parent or guardian) must be informed that he
or she may refuse to consent to an evidentiary exam, and
that such a refusal will not result in a denial of treatment
of injuries, possible pregnancy and sexually transmitted
diseases if the victim wishes to obtain treatment. (See
“Consent for Abuse-Related Exams,” page7.12, for
information about minors ability to consent to sexual
assault examination and treatment.)
E. Protocol for Examination and Treatment of
Victim
Cal OES has prepared protocols for examination of victims,
available at www.ccfmtc.org. This portion of the manual
identifies several preliminary legal requirements.
INFORMATIONAL CARD
Before starting an evidentiary or other physical exam for a
sexual assault, the physician or nurse must give the victim
an informational card designed by law enforcement for
sexual assault victims [Penal Code Section 680.2(a)]. This
requirement applies only if the law enforcement agency
has given cards to the medical provider in a language
understood by the victim. Hospitals should check with their
local law enforcement agency to obtain a supply of these
cards. [Penal Code Section 264.2(b)(2)]
POSTCOITAL CONTRACEPTION
If the sexual assault could result in pregnancy, the
victim must be provided with the option of postcoital
contraception. If the victim requests it, postcoital
contraception must be dispensed at no cost to the victim.
[Penal Code Section 13823.11]
SEXUAL ASSAULT COUNSELOR
The victim has the right to have a sexual assault counselor
and at least one other support person of the victim’s
choosing present at any medical evidentiary or physical
examination. The victim must be informed by the medical
provider of this right, either orally or in writing, prior to the

Chapter 7 — Reporting Assaults, Potentially Dangerous Patients and Firearms Prohibitions CHA
7.7
©CALIFORNIA HOSPITAL ASSOCIATION
examination. A support person may be excluded from the
exam if the law enforcement officer or medical provider
determines that the presence of that individual would
be detrimental to the purpose of the exam. [Penal Code
Section 264.2]
NOTIFY RAPE VICTIM COUNSELING CENTER
The law enforcement officer or agency is supposed to
notify the local rape victim counseling center whenever a
victim is transported to a hospital for a medical evidentiary
or physical exam. The hospital may verify with the
law enforcement officer or agency that the rape victim
counseling center has been notified, if the victim approves.
In addition, the hospital may notify the rape victim
counseling center, if the victim approves. [Penal Code
Section 264.2(b)(1)]
OPPORTUNITY TO SHOWER/BATHE
After conducting a medical evidentiary or physical
examination, the medical provider is required to give the
victim the opportunity to shower or bathe at no cost, unless
a showering or bathing facility is not available. [Penal Code
Section 264.2(b)(5)]
NOTIFY LAW ENFORCEMENT AGENCY
A medical provider must, within 24 hours of obtaining
sexual assault forensic evidence from the victim, notify the
law enforcement agency having jurisdiction over the alleged
violation if the medical provider knows the appropriate
jurisdiction. If the medical provider does not know the
appropriate jurisdiction, the medical provider must notify
the local law enforcement agency. [Penal Code Section
264.2(b)(6)]
F. Confidentiality
The suspected sexual assault forms Cal OES 2-923, OES
2-924, 2-925 and 2-930 are subject to the same principles
of confidentiality applicable to any other aspect of the
medical record [Penal Code Section 13823.5(c)]. No
information may be disclosed except that which is required
to complete the form, except as permitted or required by
another law (for example, in response to a court order or
pursuant to child abuse or elder abuse reporting laws). The
special confidentiality rules regarding child/elder/dependent
adult abuse reports are described in the respective portions
of this chapter.
G. Forensic Exam of Suspect
A health practitioner who, in his or her professional capacity
or within the scope of his or her employment, performs a
forensic medical examination on a person in the custody
of law enforcement from whom evidence is sought in
connection with the commission or investigation of sexual
assault, must prepare a written report. The report must
be on the form developed by Cal OES, and must be
immediately provided to the law enforcement agency that
has custody of the person examined. The required form is
Cal OES 2-950, “Forensic Medical Report: Sexual Assault
Suspect Examination” and is available at www.ccfmtc.org.
Instructions and an examination protocol are also available
at this website.
The health practitioners covered by this law are those
who are employed in a health facility, clinic, physician’s
office, local or state public health department, or a clinic
or other type of facility operated by a local or state public
health department.
The examination and report are subject to the
Confidentiality of Medical Information Act, the
physician-patient privilege, and the privilege of official
information pursuant to Evidence Code Section 1040 et
seq. However, the report must be released upon oral or
written request to any person or agency involved in any
related investigation or prosecution of a criminal case.
The persons to whom the report must be released upon
request include, but are not limited to, a law enforcement
officer, district attorney, city attorney, crime laboratory,
county licensing agency, and a coroner. The report may
be released to defense counsel or another third party only
through discovery of documents in the possession of a
prosecuting agency or by court order.
A health practitioner who makes a report in accordance
with this law is immune from civil or criminal liability.
No person, agency, or their designee required or authorized
to report pursuant to this law, who takes photographs
of a suspect is civilly or criminally liable for taking the
photographs, causing the photographs to be taken, or
disseminating the photographs to a law enforcement officer,
district attorney, city attorney, crime laboratory, county
licensing agency, or coroner with the reports required in
accordance with this law. However, the photographs may
not be used in any other way.
No health practitioner may be required to perform a
forensic medical examination as part of his or her duties as
a health practitioner, except for those health practitioners
who have entered into a contract to perform forensic
medical exams.
[Penal Code Section 11160.1]

CHA Mental Health Law Manual 2019
7.8
©CALIFORNIA HOSPITAL ASSOCIATION
V. CHILD ABUSE AND NEGLECT
A. Basic Reporting Requirement
Health practitioners and others who have knowledge of
or observe a child in his or her professional capacity or
within the scope of his or her employment whom he or she
knows or reasonably suspects has been the victim of child
abuse or neglect are required to report to a designated
law enforcement agency. The initial report must be
made immediately, or as soon as practically possible, by
telephone. A follow-up written report must then be made
within 36 hours. These requirements, as well as definitions
of terms used in the law, are explained in this section of
the manual.
California’s child abuse and neglect reporting laws cover
children under the age of 18. [Penal Code Sections
11164-11174.3]
This reporting requirement applies even if the child has
died, regardless of whether or not the possible abuse
was a factor contributing to the child’s death, and even if
suspected child abuse was discovered during an autopsy.
[Penal Code Section 11166(a)]
UNSUITABLE HOME
A mandated reporter who knows or reasonably suspects
that the home or institution in which a child resides is
unsuitable for the child because of abuse or neglect of the
child is required to bring the condition to the attention of
the agency to which he or she makes a report of the abuse
or neglect, and must do so at the same time as the report
is made [Penal Code Section 11166(f)].
EMOTIONAL DAMAGE
A mandated reporter who has knowledge of or who
reasonably suspects that a child is suffering serious
emotional damage or is at substantial risk of suffering
serious emotional damage, evidenced by states of being
or behavior, including, but not limited to, severe anxiety,
depression, withdrawal or untoward aggressive behavior
toward self or others, may (but is not required to) make
a report to the appropriate agency. [Penal Code Section
11166.05]
B. Definitions
“Abuse or neglect in out-of-home care” includes:
1. Physical injury or death inflicted upon a child by
another person (by other than accidental means);
2. Sexual abuse;
3. Neglect;
4. Unlawful corporal punishment or injury; or
5. The willful harming or injuring of a child or the
endangering of the person or health of a child.
This applies where the person responsible for the child’s
welfare is:
1. A licensee, administrator or employee of a licensed
community care or child day care facility or a facility
licensed to care for children; or
2. The administrator or employee of a public or private
residential home, school or other institution.
This term does not include an injury caused by a peace
officer’s reasonable and necessary force while acting within
the course and scope of the officer’s employment as a
peace officer. [Penal Code Section 11165.5]
“Child abuse or neglect” includes the following:
1. A physical injury or death that is inflicted by other than
accidental means on a child by another person;
2. Sexual abuse;
3. Neglect;
4. Unlawful corporal punishment or injury;
5. Willful harming or injuring of a child or endangering of
the person or health of a child; and
6. Abuse or neglect in out-of-home care.
[Penal Code Section 11165.6]
NOTE: Child abuse does not include a mutual affray
between minors or an injury caused by a peace officer’s
reasonable and necessary force used while acting within
the course and scope of the officer’s employment as a
peace officer. “Affray” is not defined in the law, but the
dictionary defines it as a fight, quarrel or brawl.
“Neglect” means the negligent treatment or maltreatment
of a child by a person responsible for the child’s welfare
under circumstances indicating harm or threatened harm
to the child’s health or welfare. The term includes both acts
and omissions on the part of the responsible person. [Penal
Code Section 11165.2]
“Neglect” includes “general neglect” which means:
the negligent failure of a person having the care or
custody of a child to provide adequate food, clothing,
shelter, medical care or supervision where no physical
injury to the child has occurred.

Chapter 7 — Reporting Assaults, Potentially Dangerous Patients and Firearms Prohibitions CHA
7.9
©CALIFORNIA HOSPITAL ASSOCIATION
“Neglect” also includes “severe neglect” which means:
the negligent failure of a person having the care or
custody of a child to protect the child from severe
malnutrition or medically diagnosed nonorganic failure to
thrive. “Severe neglect” also means those situations of
neglect where a person having the care or custody of a
child willfully causes or permits the person or health of
the child to be placed in a situation such that his or her
person or health is endangered, as proscribed by section
11165.3, including the intentional failure to provide
adequate food, clothing, shelter or medical care.
A child receiving treatment by spiritual means as provided
in Welfare and Institutions Code Section 16509.1 or
not receiving specified medical treatment for religious
reasons, shall not be, for that reason alone, considered a
neglected child.
The law also provides that “an informed and appropriate
medical decision made by (the) parent or guardian after
consultation with a physician or physicians who have
examined the child does not constitute neglect” [Penal
Code Section 11165.2]. This provision leaves open
the question as to what constitutes an “informed and
appropriate medical decision,” but it appears to require
reporting in situations in which the physician or another
member of the health care team believes that a decision
made by a child’s parent or guardian after receiving the
relevant information is not appropriate, in the sense that it
is not consistent with the child’s best interests.
“Reasonable suspicion” means that it is objectively
reasonable for a person to entertain a suspicion, based
upon facts that could cause a reasonable person in a
like position, drawing, when appropriate, on his or her
training and experience, to suspect child abuse or neglect.
“Reasonable suspicion” does not require certainty that
child abuse or neglect has occurred nor does it require a
specific medical indication of child abuse or neglect. Any
reasonable suspicion is sufficient. However, the pregnancy
of a minor does not, in and of itself, constitute a basis
for a reasonable suspicion of sexual abuse (see “When a
Child Seeks Treatment for a Sexually Transmitted Disease,
Pregnancy or Abortion,” page7.13). [Penal Code Section
11166(a)] In addition, the laws regarding “safe surrender”
of a newborn and maternal substance abuse contain
provisions stating that these activities in and of themselves
do not trigger child abuse reporting. (See “Maternal
Substance Abuse,” page7.14, and “Safe Surrender of a
Newborn,” page7.15.)
“Sexual abuse” means sexual assault or sexual exploitation
[Penal Code Section 11165.1].
“Sexual assault” means conduct in violation of various
Penal Code sections including rape, rape in concert,
statutory rape, incest, sodomy, lewd or lascivious acts
upon a child, oral copulation, sexual penetration and
child molestation.
Conduct described as “sexual assault” includes, but is not
limited to, all of the following:
1. Penetration, however slight, of the vagina or anal
opening of one person by the penis of another person,
whether or not there is emission of semen.
2. Sexual contact between the genitals or anal
opening of one person and the mouth or tongue of
another person.
3. Intrusion by one person into the genitals or anal
opening of another person, including the use of an
object for this purpose, except that it does not include
acts performed for a valid medical purpose.
4. The intentional touching of the genitals or intimate
parts, including the breasts, genital area, groin, inner
thighs and buttocks, or the clothing covering them, of
a child, or of the perpetrator by a child, for purposes of
sexual arousal or gratification, except that it does not
include acts which may reasonably be construed to
be normal caretaker responsibilities; interactions with,
or demonstrations of affection for, the child; or acts
performed for a valid medical purpose.
5. The intentional masturbation of one’s genitals in the
presence of a child.
“Sexual exploitation” refers to any of the following:
1. Conduct involving matter depicting a minor engaged
in obscene acts, which violates the law prohibiting the
preparation, sale or distribution of obscene matter or
employment of minors to perform obscene acts.
2. A person who knowingly promotes, aids, or assists,
employs, uses, persuades, induces, or coerces a
child, or a person responsible for a child’s welfare who
knowingly permits or encourages a child to engage in,
or assist others to engage in, prostitution or to either
pose or model alone or with others for purposes of
preparing a film, photograph, negative, slide, drawing,
painting or other pictorial depiction involving obscene
sexual conduct. (“Person responsible for a child’s
welfare” means a parent; guardian; foster parent; or
a licensed administrator or employee of a public or
private residential home, residential school or other
residential institution.)
3. A person who depicts a child in, or who knowingly
develops, duplicates, prints, downloads, streams,
accesses through any electronic or digital media, or

CHA Mental Health Law Manual 2019
7.10
©CALIFORNIA HOSPITAL ASSOCIATION
exchanges, a film, photograph, videotape, video
recording, negative or slide in which a child is engaged
in an act of obscene sexual conduct, except for
those activities by law enforcement and prosecution
agencies and other persons described in Penal Code
Section 311.3.
“Commercial sexual exploitation” refers to either of
the following:
1. The sexual trafficking of a child, as described in Penal
Code Section 236.1(c).
2. The provision of food, shelter, or payment to a child
in exchange for the performance of any sexual act
described in this law or Penal Code Section 236.1(c).
“Unlawful corporal punishment or injury” means a
situation where a person willfully inflicts upon a child cruel
or inhuman corporal punishment or injury resulting in a
traumatic condition. It does not include an amount of force
that is reasonable and necessary for a person employed
by or engaged in a public school to quell a disturbance
threatening physical injury to a person or damage to
property, for purposes of self-defense, or to obtain
possession of weapons or other dangerous objects within
the control of the pupil, as authorized by Education Code
Section 49001. It also does not include the exercise of the
degree of physical control authorized by Education Code
Section 44807. In addition, unlawful corporal punishment or
injury does not include an injury caused by a peace officer’s
reasonable and necessary force while acting within the
course and scope of the officer’s employment as a peace
officer. [Penal Code Section 11165.4]
“Willful harming or endangering of a child” means a
situation in which any person willfully causes or permits a
child to suffer, or inflicts upon a child, unjustifiable physical
pain or mental suffering, or having the care and custody of
the child, willfully causes or permits the person or health
of the child to be placed in a situation in which the child’s
person or health is endangered. [Penal Code Section
11165.3]
C. Persons Required or Permitted to Report
MANDATED REPORTERS
Penal Code Section 11165.7 requires specified health care
providers and clergy members (among others) to report
suspected child abuse and neglect. Persons required by
law to report are called “mandated reporters.”
The law describes more than 44 categories of professionals
or individuals who are considered mandatory reporters
under the law [Penal Code Section 11165.7]. These
categories of mandated reporters include social workers;
teachers; teacher’s aides and assistants; certain court
employees; licensed day care workers; employees of child
care institutions; peace officers; firefighters; probation
officers; parole officers; custodial officers; specified
district attorney investigators; local child support agency
caseworkers; persons providing in-home supportive
services to minors; film developers; commercial computer
technicians (who work for a company in the business of
repairing or installing computers for a fee); and various
community professionals and workers in schools, day care
programs, youth centers and camps.
Health care providers that are mandated reporters are
physicians, surgeons, psychiatrists, psychologists, dentists,
residents, interns, podiatrists, chiropractors, licensed
nurses, dental hygienists, optometrists, marriage and family
therapists, clinical social workers, professional clinical
counselors, or any other person who is currently licensed
under Business and Professions Code Section 500 et seq.;
an emergency medical technician I or II, paramedic, or
other person certified pursuant to Health and Safety Code
Section 1797 et seq.; a psychological assistant registered
pursuant to Business and Professions Code Section
2913; a marriage and family therapist trainee, as defined
in Business and Professions Code Section 4980.03(c);
an unlicensed associate marriage and family therapist
registered under Business and Professions Code Section
4980.44; an alcohol and drug counselor; a professional
clinical counselor trainee; an associate professional clinical
counselor; a state or county public health employee who
treats a minor for venereal disease or any other condition;
a coroner; or a medical examiner or any person who
performs autopsies. [Penal Code Sections 11162.5 and
11165.7]
Clergy
“Clergy member” means a priest, minister, rabbi, religious
practitioner, or similar functionary of a church, temple, or
recognized denomination or organization [Penal Code
Section 11165.7(a)(32)]. Any clergy member who has
knowledge of, or observes a child in his or her professional
capacity or within the scope of his or her duties, whom
he or she knows or reasonably suspects has been the
victim of child abuse or neglect, must comply with the
requirements of this law. However, a clergy member who
acquires knowledge or reasonable suspicion of child abuse
or neglect during a “penitential communication” is not
required to report. A “penitential communication” means
a communication, intended to be in confidence, including,
but not limited to, a sacramental confession, made to

Chapter 7 — Reporting Assaults, Potentially Dangerous Patients and Firearms Prohibitions CHA
7.11
©CALIFORNIA HOSPITAL ASSOCIATION
a clergy member, who in the course of the discipline or
practice of his or her church, denomination or organization,
is authorized or accustomed to hear those communications,
and under the discipline, tenets, customs or practices of
his or her church, denomination or organization, has a
duty to keep those communications secret. This exception
must not be construed to modify or limit a clergy member’s
duty to report known or suspected child abuse or neglect
when he or she is acting in some other capacity that would
otherwise make the clergy member a mandated reporter
[Penal Code Section 11166(d)]. A custodian of records of a
clergy member is also a mandated reporter.
Alcohol and Drug Counselor
Alcohol and drug counselors are mandatory reporters.
An “alcohol and drug counselor” is a person providing
counseling, therapy, or other clinical services for a
state-licensed or certified drug, alcohol, or drug and
alcohol treatment program.
VOLUNTARY REPORTERS
Penal Code Section 11166(g) permits, but does not require,
reporting from any other person (who is not a mandated
reporter) who has knowledge of or reasonably suspects
a child has been the victim of child abuse or neglect
[Penal Code 11166(g)]. This includes a mandated reporter
who acts in his or her private capacity and not in his or
her professional capacity or within the scope of his or
her employment.
Volunteers
Although hospital volunteers (and other volunteers, except
volunteers of a Court Appointed Special Advocate Program)
are not mandated reporters, the law encourages volunteers
who have contact with children to obtain training in the
identification and reporting of child abuse and to report
known or suspected instances of child abuse to agencies
specified under the law to receive such reports [Penal Code
Section 11165.7(b)]. Employers are encouraged to provide
training to volunteers [Penal Code Section 11165.7(g)].
SELECTION OF A PERSON TO REPORT
Reporting information about possible child abuse to a
supervisor, employer, coworker or other person is not
a substitute for reporting to a law enforcement agency.
However, in a hospital or clinic, two or more mandated
reporters may become jointly aware of the same instance of
reportable child abuse or neglect. The law allows the team
to select, by mutual agreement, a single member who will
be responsible for making the telephone report and making
and signing the written report. However, if any member of
the team knows the designated member failed to report, he
or she must thereafter make the report.
The law allows the hospital or clinic to create internal
procedures to facilitate reporting and apprise supervisors
and administrators of reports. However, a hospital’s internal
policy may not direct employees to allow their supervisor to
file or process a mandated report under any circumstances.
No supervisor or administrator may impede or inhibit child
abuse reporting, and employees must not be subject to
sanctions for making a report. [Penal Code 11166]
The internal procedures must not require an employee
required to make reports by the statute to disclose his
or her identity to the employer [Penal Code Section
11166(i)(2)].
D. Reporting to Law Enforcement
A telephone report, followed by a written report, must be
made to any police department (not including a school
district police or security department), sheriff’s department,
county probation department (if designated by the county
to receive child abuse reports) or the county welfare
department. Agencies that are required to receive child
abuse reports may not refuse to accept them. They must
maintain a record of all reports received. [Penal Code
Section 11165.9]
CONTENT OF REPORT
Reports of suspected child abuse or neglect must include
the following information [Penal Code Section 11167]:
1. The name, business address and telephone number of
the mandated reporter, and the capacity that makes
the person a mandated reporter.
If the person is not a mandated reporter, he or she is
not required to include his or her name [Penal Code
Section 11167(f)]. If the name is given, the person’s
identity is confidential and may be disclosed only in
limited circumstances.
2. The information that gave rise to the reasonable
suspicion of child abuse or neglect and the source or
sources of that information.
If a report is made, the following information, if known,
must also be included in the report:
1. The child’s name, address and present location, and, if
applicable, the child’s school, grade and class.

CHA Mental Health Law Manual 2019
7.12
©CALIFORNIA HOSPITAL ASSOCIATION
2. The names, addresses and telephone numbers of the
child’s parents or guardians.
3. The name, address, telephone number and other
relevant personal information about the person or
persons who might have abused or neglected the child.
A mandated reporter may include with the report any
nonprivileged documentary evidence related to the
incident [Penal Code Section 11166(a)]. (See F.“Privileges
Inapplicable,” page7.15.)
The mandated reporter shall make a report even if some of
this information is not known or is uncertain to him or her.
HOW REPORTS ARE MADE
An initial telephone report must be made immediately
or as soon as is practically possible after receiving the
information concerning the incident [Penal Code Section
11166(a)].
A written follow-up report must be sent by mail, facsimile,
or email to the law enforcement agency within 36 hours of
receiving the information concerning the incident.
Required Form
The California Department of Justice has adopted
“Suspected Child Abuse Report,” form SS 8572, which
must be used for the written report. The form may be
obtained from the local social services department or child
protective services agency. (The form may be downloaded
at www.ag.ca.gov/childabuse/pdf/ss_8572.pdf or www.
ccfmtc.org.)
Procedure
The person or the team member designated to report
should fill in and sign the written report. The same person
should make both the telephone and the written report.
FORENSIC MEDICAL REPORTS
A medical professional who examines a child for physical
injury or sexual assault that is suspected child abuse must
complete a medical report within 36 hours of receiving the
information concerning the incident. This medical report
should be submitted along with “Suspected Child Abuse
Report,” form SS 8572. This medical report should be
the “Medical Report: Suspected Child Physical Abuse and
Neglect Examination” (Cal OES 2-900) or one of the forms
described in “Forms,” page7.6. The forms, instructions,
and examination protocols may be found at www.ccfmtc.
org.
A medical exam relating to sexual assault must be
documented on standard forms adopted by Cal OES
[Penal Code Section 13823.5]. That office developed the
forms described in “Forms,” page7.6. Therefore, when
there is evidence of child sexual abuse, one of these
forms must be used. When no sexual abuse is indicated,
form Cal OES 2-900 is the more appropriate form since
it is better suited to gathering evidence of physical abuse
or neglect.
For information about the forms or assistance in completing
them, contact the California Clinical Forensic Medical
Training Center at (916) 930-3080.
Documentation in the Medical Record
The forensic medical reports must become part of the
patient’s medical record pursuant to guidelines established
by the advisory committee of Cal OES. Hospitals may
wish to consider putting the forensic medical reports in a
separate section of the medical record to prevent routine
copying and disclosure of these reports for purposes
not related to the criminal justice system, and to prevent
improper release to unauthorized persons. The completed
forms are subject to the special confidentiality laws
pertaining to the release of forensic medical examination
records (see G.“Disclosure and Follow-Up Procedures,”
page7.16, and I.“Confidentiality of Reports,” page7.18).
[Penal Code Section 11171(d)]
The hospital’s initial report to law enforcement is not
required to be placed in the medical record. Hospitals
should develop a policy regarding maintenance of reports
to maintain confidentiality of the reporter’s identity (see
I.“Confidentiality of Reports,” page7.18).
CONSENT FOR ABUSE-RELATED EXAMS
Special Law for X-Rays
A physician or dentist (or their agents at their direction)
may take skeletal X-rays of a child without the consent of
the child’s parent or guardian, but only for the purpose
of diagnosing the case as one of possible child abuse or
neglect and determining the extent of such child abuse or
neglect [Penal Code Section 11171.2].
Additionally, if a peace officer in the course of investigation
of child abuse or neglect has reasonable cause to believe
that the child has been physically abused, the officer may
apply to a magistrate for an order directing that the child
be X-rayed without parental consent [Penal Code Section
11171.5]. X-rays performed pursuant to such an order must
be performed by a physician or dentist or their agents.

Chapter 7 — Reporting Assaults, Potentially Dangerous Patients and Firearms Prohibitions CHA
7.13
©CALIFORNIA HOSPITAL ASSOCIATION
Reimbursement by the county for administrative costs of
such X-rays will not exceed 5 percent of the cost of the
X-rays.
Other Treatment
If further treatment beyond X-rays is necessary and the
parents object, the hospital should consult legal counsel. It
may be appropriate to seek a petition to declare the minor
a dependent child of the juvenile court pursuant to Welfare
and Institutions Code Section 300 for the purposes of
assuring that he or she receives the proper medical care.
If the minor has been raped or sexually assaulted, the minor
may give consent to medical treatment (see below).
Rape
A minor 12 years of age or older who has allegedly been
raped may consent to the furnishing of hospital, medical,
and surgical care related to the diagnosis or treatment of
such condition. This includes information concerning, and
access to, the “morning after” pill [Brownfield v. Daniel
Freeman Marina Hospital, 208 Cal.App.3d 405(1989)]. The
minor may also consent to the collection of evidence with
regard to the alleged rape. The consent of the minor’s
parent(s) or guardian is not necessary. [Family Code
Section 6927; Title 11, California Code of Regulations,
Section 925]
A minor who has been raped has also been sexually
assaulted, according to the legal definitions. It is unclear
why California law contains two different statutes pertaining
to these victims (Family Code Sections 6927 and 6928,
which is discussed below). The only difference in the two
statutes is that Family Code Section 6928 (regarding
sexual assault) requires the professional person providing
medical treatment to a minor victim of sexual assault must
attempt to contact the minor’s parent/guardian unless the
treating professional person reasonably believes the parent/
guardian was the perpetrator. CHA recommends that the
treating professional talk to the minor sexual assault victim
about contacting the parent, and then contact the parent
unless the minor voices significant concern. This discussion
and the outcome should be documented.
Sexual Assault
A minor who is alleged to have been sexually assaulted
may consent to the furnishing of hospital, medical and
surgical care related to the diagnosis and treatment of
such condition. Sexual assault includes, but is not limited
to, rape, sodomy, or oral copulation. The minor may also
consent to collection of medical evidence with regard to the
alleged sexual assault. The consent of the minor’s parent(s)
or guardian is not necessary [Family Code Section 6928;
Title 11, California Code of Regulations, Section 925].
The professional person providing the medical treatment
must attempt to contact the minor’s parent(s) or guardian
and note the date and time of such contact or, if
unsuccessful, when contact was attempted. However,
the professional person need not make this contact if he
or she reasonably believes that the parent(s) or guardian
committed the sexual assault on the minor. [Family Code
Section 6928]
E. Special Situations Regarding Reporting
WHEN A CHILD SEEKS TREATMENT FOR A SEXUALLY
TRANSMITTED DISEASE, PREGNANCY OR ABORTION
The pregnancy of a minor, in and of itself, does not
constitute the basis for reasonable suspicion of child abuse
[Penal Code Section 11166(a)]. Neither does, by itself, a
request for birth control assistance [67 Ops.Cal.Atty.Gen.
235 (1984)], which a minor is legally authorized to obtain
under Family Code Section 6925 (see chapter 2).
Notwithstanding the foregoing, child abuse reporting may
be required when particular types of medical attention are
rendered to a child if there are additional facts indicating
that the child was sexually assaulted [67 Ops. Cal. Atty.
Gen. 235 (1984)]. Thus, reporting may be required when a
minor seeks treatment for a sexually transmitted disease
or pregnancy or requests an abortion or birth control
assistance and there is reasonable suspicion to believe that
there has been a violation of the law amounting to sexual
assault (as defined above). (See “Minors Under 14 Years of
Age: Lewd and Lascivious Conduct Versus Statutory Rape”
below, for discussion of reports concerning children under
age 14.)
Reasonable Suspicion
In People v. Stockton Pregnancy Control Medical Clinic,
203 Cal.App.3d 225, 239-240 (1988), which is discussed
below, the court stated:
The [Child Abuse and Neglect Reporting] Act makes clear
that professionals subject to the Act must evaluate facts
known to them in light of their training and experience to
determine whether they have an objectively reasonable
suspicion of child abuse ... However, nothing in the Act
requires professionals such as health practitioners to
obtain information they would not ordinarily obtain in the
course of providing care or treatment. Thus, the duty to
report must be premised on information obtained by the

CHA Mental Health Law Manual 2019
7.14
©CALIFORNIA HOSPITAL ASSOCIATION
health practitioner in the ordinary course of providing
care and treatment according to standards prevailing in
the medical profession.
According to the California Attorney General [67 Ops.
Cal.Atty.Gen. 235 (1984)], the facts to be used to
evaluate whether there is reasonable suspicion to believe
that a child who seeks care for a sexually transmitted
disease, pregnancy or abortion was the victim of child
abuse include:
1. The child’s medical history;
2. Other information available to the professional through
consultation or examination; and
3. Whether the child is immature or mentally deficient.
Pregnancy in a mentally or physically impaired child
or an intellectually disabled child does, according to
the California Attorney General, raise a reasonable
suspicion of child abuse.
Minors Under 14 Years of Age: Lewd and Lascivious
Conduct Versus Statutory Rape
As noted above, the commission of a lewd or lascivious
act upon a child under 14 years of age, which is a violation
of Penal Code Section 288, constitutes sexual assault. In
Planned Parenthood Affiliates v. Van de Kamp, 181 Cal.
App.3d 245 (1986), the Court of Appeal held that no child
abuse report need be made where the conduct involved
is voluntary sexual activity between minors who are
both under age 14 and are of a similar age. This ruling
was affirmed in People v. Stockton Pregnancy Control
Medical Clinic, supra, 203 Cal.App.3d at 234, where the
court stated:
In practical effect, the [Child Abuse and Neglect
Reporting] Act, as construed in Planned Parenthood,
exempts from reporting as “child abuse” the voluntary
sexual conduct of sexually mature boyfriends and
girlfriends (i.e., minors age 14 and older) and the conduct
of younger children of similar ages who voluntarily play
doctor or otherwise engage in sexual experimentation.
However, the appellate court in the Stockton case also
held that a report of child abuse is still required where the
sexual activity, even though voluntary, is between a minor
under age 14 and a person of disparate age. This includes
instances in which the other person is an adult or a minor
age 14 or older. Penal Code Section 288(c)(1) clarifies
that it is deemed an offense where lewd or lascivious
acts are committed with a minor of 14 or 15 years and
the defendant is at least 10 years older than the victim.
Moreover, Penal Code Section 261.5 sets forth degrees of
liability for sexual intercourse with a minor more than two
years younger than the age of the perpetrator.
WHEN TREATING SUBSTANCE USE DISORDER
PATIENTS
Alcohol and/or drug abuse is not, in and of itself, a sufficient
basis for reporting child abuse or neglect [Penal Code
Section 11165.7(a)(38)].
The federal laws regulating the disclosure of patient
records maintained in connection with the treatment of
substance use disorders by federally assisted programs
expressly permit the reporting under state law of incidents
of suspected child abuse and neglect to appropriate
state or local authorities [42 U.S.C. Section 290dd-2(e)]
(see chapter 6 regarding federal laws governing the
confidentiality of substance use disorder information).
MATERNAL SUBSTANCE ABUSE
When a Report Must Be Made
A positive toxicology screen at the time of an infant’s
delivery is not in and of itself a sufficient basis for reporting
child abuse or neglect. However, any indication of maternal
substance abuse requires an assessment of the needs
of the mother and child under Health and Safety Code
Section 123605. If other factors are present that indicate
risk to a child, then a child abuse report must be made.
However, a report based on risk to a child which relates
solely to the inability of the parent to provide the child with
regular care due to the parent’s substance abuse must be
made only to a county welfare or probation department
and not to a law enforcement agency. [Penal Code Section
11165.13]
Needs Assessment
Each county must establish protocols between county
health departments, county welfare departments, and all
public and private hospitals in the county regarding the
application and use of an assessment of the needs of, and
a referral for, a substance abuse-exposed infant to a county
welfare department.
The needs assessment must be performed by a health
practitioner or a medical social worker before the infant is
released from the hospital.
The purpose of the needs assessment is to:
1. Identify needed services for the mother, child or family,
including, where applicable, services to assist the
mother in caring for her child and services to assist
maintaining children in their homes.
2. Determine the level of risk to the newborn upon release
to the home and the corresponding level of services
and intervention, if any, necessary to protect the

Chapter 7 — Reporting Assaults, Potentially Dangerous Patients and Firearms Prohibitions CHA
7.15
©CALIFORNIA HOSPITAL ASSOCIATION
newborn’s health and safety, including a referral to the
county welfare department for child welfare services.
3. Gather data for information and planning purposes.
[Health and Safety Code Section 123605; Penal Code
Section 11165.13]
Government Facilities
In Ferguson et al. v. City of Charleston et al., 532 U.S. 67
(2001), the U.S. Supreme Court ruled that a state hospital’s
performance of a drug test to obtain evidence of a patient’s
criminal conduct for law enforcement purposes is an
unreasonable search if the patient has not consented to
the procedure. In that case, a state hospital worked with
local law enforcement personnel to develop policies to
identify and report pregnant drug users. Criteria for testing
pregnant women were developed which, according to the
court, were not sufficiently related to illegal drug use to
constitute probable cause or even a basis for a reasonable
suspicion. No search warrants were sought. Chain of
custody procedures and documentation were developed
to make sure test results could be used in subsequent
criminal proceedings. The hospital policy set forth the range
of possible criminal charges and the logistics of police
notification and arrests. The policy did not discuss different
courses of medical treatment for either the mother or infant.
For purposes of this case, it was assumed that the women
did not consent to taking the urine sample (although there
were no allegations that the urine was forcibly removed),
testing the urine for drugs, or reporting the positive result to
law enforcement.
The court found that the focus of the policy was on the
arrest and prosecution of drug-abusing mothers, not
medical care. The court held that because the hospital is
a state hospital, the members of its staff are government
actors and subject to the Fourth Amendment prohibitions
against unreasonable search and seizure. The court stated
that when a hospital undertakes to obtain evidence from
its patients for the specific purpose of incriminating those
patients, the hospital has a special obligation to make sure
that the patients are fully informed about their constitutional
rights. The court sent the case back to a lower court
to determine whether informed consent was given by
the patients.
The court distinguished this case from circumstances
in which physicians, in the course of ordinary medical
procedures aimed at helping the patient, come across
information that under rules of law or ethics is subject to
reporting requirements. However, the court also stated
that the “reasonable expectation of privacy enjoyed by the
typical patient undergoing diagnostic tests in a hospital
is that the results of those tests will not be shared with
nonmedical personnel without her consent.”
Government hospitals should work with their legal counsel
to develop a drug testing policy that satisfies the concerns
outlined by the court in the Ferguson case.
SAFE SURRENDER OF A NEWBORN
The voluntary surrendering of a newborn in accordance
with California’s “safe surrender” law is not, in and of itself,
a sufficient basis for reporting child abuse or neglect.
HOMELESS CHILDREN
The fact that a child is homeless or is classified as an
unaccompanied minor is not, in and of itself, a sufficient
basis for reporting child abuse or neglect. However, this
law is not intended to limit reports when a mandated
reporter has knowledge of or observes an unaccompanied
minor whom the mandated reporter knows or reasonably
suspects to be the victim of abuse or neglect. [Penal Code
Section 11165.15]
For purposes of this law, “homeless children and youths”
means individuals who lack a fixed, regular, and adequate
nighttime residence, and includes:
1. Children and youths who are sharing the housing
of other persons due to loss of housing, economic
hardship, or a similar reason; are living in motels,
hotels, trailer parks, or camping grounds due to the
lack of alternative adequate accommodations; are
living in emergency or transitional shelters; or are
abandoned in hospitals;
2. Children and youths who have a primary nighttime
residence that is a public or private place not
designed for or ordinarily used as a regular sleeping
accommodation for human beings; and
3. Children and youths who are living in cars, parks,
public spaces, abandoned buildings, substandard
housing, bus or train stations, or similar settings.
“Unaccompanied youth” includes a homeless child or
youth not in the physical custody of a parent or guardian.
[42 U.S.C. Section 11301 et seq.; 42 U.S.C.
Section 11434a]
F. Privileges Inapplicable
Neither the physician-patient privilege nor the
psychotherapist-patient privilege applies to information that
must be reported pursuant to child abuse reporting laws in

CHA Mental Health Law Manual 2019
7.16
©CALIFORNIA HOSPITAL ASSOCIATION
a court proceeding or administrative hearing [Penal Code
Section 11171.2].
In People v. Stritzinger, 34 Cal.3d 505 (1983), the
California Supreme Court held that the child abuse
or neglect reporting requirements supersede the
psychotherapist-patient privilege, and that confidential
information must be disclosed by a psychotherapist in
order to fulfill the reporting requirements. However, the
court also held that only the information which must be
reported may be disclosed, and that a psychotherapist
cannot disclose information received after the report
was made if it pertains to the identical situation that was
reported.
The California Attorney General has opined that the child
abuse reporting requirements supersede the confidentiality
provisions of the Lanterman-Petris-Short Act (see chapter
17 regarding the Lanterman-Petris-Short Act requirements)
[65 Ops.Cal.Atty.Gen. 345 (1982)]. Facilities should consult
their legal counsel regarding the scope of disclosure that is
required by the child abuse reporting statute.
G. Disclosure and Follow-Up Procedures
DISCLOSURE TO INVESTIGATOR
Information relevant to the incident of child abuse or
neglect and information relevant to a report made pursuant
to Penal Code Section 11166.05 (see “Emotional Damage,”
page7.8) may be given to an investigator from an agency
that is investigating a known or suspected case of child
abuse or neglect [Penal Code Section 11167(b)]. However,
the only information that may be disclosed is that which
is relevant to the incident of child abuse or neglect. Thus,
medical information regarding the involved persons (e.g., a
suspected victim or perpetrator) should be disclosed only if
it appears to satisfy this relevancy test.
Scope of Information to be Released
In Ferraro v. Chadwick, 221 Cal.App.3d 86 (1990), parents
who were reported for child abuse sued the reporting
hospital and physician alleging that statements made
and information provided after the initial report of child
abuse were outside the immunity provided under Penal
Code Section 11172 (see the discussion of immunity
in G.“Immunity From Liability,” page7.5). In rejecting
this argument, the court made several points relevant
to the scope of permissible disclosure of information
to investigators:
1. The type of report or communication contemplated by
Section 11167(b) most often is going to occur after an
initial report of suspected abuse.
2. Section 11167 anticipates that, in the course of an
investigation into suspected abuse, the reporter
(“particularly if the reporter is a doctor”) is going
to be contacted and interviewed by the agency
conducting the investigation, and the law approves
communications between the reporter and the
investigating agency.
3. The child abuse reporting laws both authorize and
protect these subsequent communications, regardless
of whether they were in response to law enforcement
inquiries or were initiated by the doctor and/or hospital.
These comments show that the court in Ferraro obviously
considered release of information under Penal Code
Section 11167(b) to be authorized reports under the
immunity statute. However, the only information that may
be disclosed is information that is relevant to the incident
of suspected abuse. Thus, medical information regarding
the involved persons, whether a suspected victim or
perpetrator, should be disclosed under this provision only if
it appears to satisfy this relevancy test.
If the information being requested does not appear to meet
this test, then the law enforcement officers should be asked
to obtain a court order or search warrant. As the California
Attorney General points out in its Child Abuse Prevention
Handbook (revised January 2000) (p. 56):
As in all areas of criminal law, all searches, seizures,
and arrests made in the course of child abuse
investigations must comply with the requirements of the
Fourth Amendment.
Mental Health and Substance Abuse Information
There are also some restrictions that have particular
application to mental health information (see chapter 6
regarding laws governing the confidentiality of mental
health information).
While the psychotherapist-patient privilege does not apply
to information required to be reported pursuant to the child
abuse reporting laws, at least one court has ruled that the
privilege continues to apply to information not required to
make the report. In People v. Stritzinger, 34 Cal.3d 505
(1983), the court ruled that while a psychotherapist was
required to disclose privileged information in order to make
a child abuse report, the psychotherapist should not have
disclosed information received after the report was made
that did not disclose new incidents of abuse.

Chapter 7 — Reporting Assaults, Potentially Dangerous Patients and Firearms Prohibitions CHA
7.17
©CALIFORNIA HOSPITAL ASSOCIATION
In addition, the California Attorney General has stated its
view that while the child abuse reporting laws override
the Lanterman-Petris-Short confidentiality law for mental
health information, it does so only to permit persons to
report “what they know or have observed” [65 Ops.Cal.Atty.
Gen 345, 355 (1982)]. According to the Attorney General’s
opinion, the reporting law does not give child protection
agencies direct access to mental health records and
information protected by the Lanterman-Petris-Short Act.
Similarly, the federal law regarding the confidentiality of
substance use disorder program records contains an
exception to confidentiality to report suspected child abuse
[42 U.S.C. Section 290dd-2(e)]. However, this exception
does not permit disclosure of patient records in any legal
proceeding that may later arise from the initial child abuse
report. Records requested for court proceedings may
be released only if the requestor has complied with the
procedures set forth in the federal regulations that apply
to federally-funded substance use disorder programs.
[42 C.F.R. Sections 2.12(c)(12) and 2.61-2.67] (See chapter
6 regarding laws governing the confidentiality of substance
use disorder information.)
DISCLOSURE TO LICENSING AGENCY
Information relevant to an incident of child abuse or
neglect (including the investigation report and other
pertinent materials) as well as information relevant to a
report made pursuant to Penal Code Section 11166.05
(see “Emotional Damage,” page7.8), may be given to
the California Department of Social Services, or the county
licensing agency that has contracted with the state for
the performance of its services, when it is investigating
a known or suspected case of child abuse or neglect
[Penal Code Sections 11167(c), 11167.5(b)(6), 11170(b)
(4)]. However, the only information that may be disclosed
is that which is relevant to the incident of child abuse or
neglect. Thus, medical information regarding the involved
persons (e.g., a suspected victim or perpetrator) should be
disclosed only if it appears to satisfy this relevancy test.
Interestingly, as used in the child abuse law, “licensing
agency” does not appear to include the California
Department of Public Health (CDPH) (see Penal Code
Section 11165.11 for the definition of “licensing agency”).
However, CDPH has other legal authority to review hospital
records; an attorney should be consulted if doubt exists as
to whether particular records should be disclosed to CDPH.
H. Immunity From Liability
MANDATED REPORTERS
No mandated reporter shall incur any civil or criminal liability
as a result of making a report required or authorized by the
child abuse reporting law. This immunity applies even if the
mandated reporter acquired the knowledge or reasonable
suspicion of child abuse or neglect outside of his or her
professional capacity or outside the scope of his or her
employment. [Penal Code Section 11172]
Two court decisions have emphasized that this immunity
for mandated reporters is absolute — that is, the immunity
applies regardless of whether or not the person making
the report knew or should have known that the report
was not true [Krikorian v. Barry, 196 Cal.App.3d 1211
(1987); Storch v. Silverman, 186 Cal.App.3d 671 (1986)].
Additionally, the immunity applies not only to the person
who makes the report (i.e., telephones the agency and
submits the written report) but to any other mandated
reporter involved in the identification of an instance of
child abuse even though they did not personally report
it to the authorities [Storch v. Silverman, supra, 186 Cal.
App.3d at 681]. This recognizes that in many instances,
especially in hospitals, the discovery of child abuse will be a
collaborative event, involving more than one person.
In Krikorian v. Barry, supra, 196 Cal.App.3d at 1223, the
court held that Penal Code Section 11172 immunity
encompasses not only the actual act of reporting but also:
conduct giving rise to the obligation to report, such as
the collection of data, or the observation, examination or
treatment of the suspected victim or perpetrator of child
abuse, performed in a professional capacity or within the
scope of employment.... [Accord, McMartin v. Children’s
Institute International, 212 Cal.App.3d 1393 (1989), cert.
den., 494 U.S. 1057 (1990)]
Mandated reporters are immunized not only for activity
related to the initial mandated report but also with respect
to activity after the initial report that is authorized under
the child abuse reporting law. [Ferraro v. Chadwick, 221
Cal.App.3d 86 (1990) and Thomas v. Chadwick, 224 Cal.
App.3d 813 (1990) modified, 224 Cal.App.3d 1637]
Attorneys’ Fees
In addition, the California Legislature recognized that
while the immunity from liability prevents imposition of
liability, it cannot prevent the filing of a lawsuit against a
person who reports. Thus, to limit the financial hardship
that persons may incur as a result of fulfilling their legal
reporting responsibilities, the law allows a person who is
sued as a result of fulfilling his or her mandatory reporting

CHA Mental Health Law Manual 2019
7.18
©CALIFORNIA HOSPITAL ASSOCIATION
obligation to recover from the state the attorneys’ fees
spent defending the action, if the person prevails. The
state is required to reimburse the person for reasonable
attorneys’ fees at hourly rates based upon the rates
charged by the California Attorney General, up to $50,000
[Penal Code Section 11172(d)]. A claim may be filed with
the Department of General Services.
VOLUNTARY REPORTERS
Penal Code Section 11172 also provides that any other
person reporting a suspected instance of child abuse or
neglect (i.e., those making voluntary reports) shall not incur
civil or criminal liability as a result of making the report
unless it can be proved that the report was false and that
the person knew it was false or that the report was made
with reckless disregard of its truth or falsity. In such a case,
the person making the report is liable for any damages
caused [Penal Code Section 11172(a)].
IMMUNITY FOR PROVIDING ACCESS TO THE VICTIM
Health practitioners and other persons are granted
immunity from civil or criminal liability for providing access
to a suspected or known victim of child abuse or neglect to
a government agency investigating a report of suspected
child abuse or neglect [Penal Code Section 11172(b)].
IMMUNITY FOR PHOTOGRAPHING OF SUSPECTED
ABUSE
Mandated reporters (and others taking photographs at
the mandated reporter’s direction) are not subject to civil
or criminal liability for photographing a suspected victim
of child abuse or neglect, or causing photographs to be
taken, without parental consent, or for disseminating the
photographs or images with the required reports. However,
this law does not give immunity from liability for other uses
of the photographs [Penal Code Section 11172(a)].
The health care provider may wish to obtain photographs
to assist the investigating agency and to provide
documentation should a question arise about the
justification for a report made by the hospital.
I. Confidentiality of Reports
Reports of child abuse and the information contained in
them, as well as certain child abuse or neglect investigative
reports, are confidential and may be disclosed only as
provided by statute [Penal Code Section 11167.5(a)].
Those to whom the statute permits disclosure include
various law enforcement and governmental agencies,
coroners and medical examiners, multidisciplinary teams,
hospital scan teams, agencies responsible for licensing
facilities that care for children, adoption agencies, and
others as specified. (See Penal Code Sections 11167-
11170.5 and G.“Disclosure and Follow-Up Procedures,”
page7.16.) Such disclosures should typically be made by
the agency to which the original report is made, rather than
by initial reporters.
The identity of all persons who make child abuse reports is
confidential and may be disclosed only among the following
agencies receiving or investigating mandated reports:
1. To the prosecutor in a criminal prosecution or in an
action initiated under Welfare and Institutions Code
Section 602 arising from alleged child abuse;
2. To counsel appointed to represent the child pursuant to
Welfare and Institutions Code Section 317(c);
3. To the county counsel or prosecutor in a proceeding
under Family Code Section 7800 et seq. or Welfare
and Institutions Code Section 300 et seq.; or
4. To a licensing agency when abuse or neglect in
out-of-home care is reasonably suspected.
In addition, the identity may be disclosed when the reporter
waives confidentiality or by court order.
No agency or person may disclose the identity of a person
who makes a child abuse report to that person’s employer,
except with the employee’s consent or by court order.
[Penal Code Section 11167(d)]
Notwithstanding these confidentiality requirements, a
representative of a child protective services agency
performing an investigation that results from a report of
suspected child abuse or neglect made pursuant to the
child abuse reporting law, at the time of the initial contact
with the individual who is subject to the investigation,
shall advise the individual of the complaints or allegations
against him or her, in a manner that is consistent with the
requirement to protect the identity of the reporter. [Penal
Code Section 11167(e)]
Violation of this confidentiality requirement is a
misdemeanor punishable by imprisonment in a county jail
not to exceed six months, by a fine of $500, or by both that
imprisonment and fine. [Penal Code Section 11167.5(a)]
J. Sanctions for a Failure to Report
A person who is required to, but fails to, report an instance
of known or reasonably suspected child abuse or neglect
may be found guilty of a misdemeanor. The punishment
may include up to six months imprisonment in the county

Chapter 7 — Reporting Assaults, Potentially Dangerous Patients and Firearms Prohibitions CHA
7.19
©CALIFORNIA HOSPITAL ASSOCIATION
jail, a fine of up to $1,000, or both [Penal Code Section
11166(c)]. A supervisor or administrator who impedes or
inhibits an employee’s reporting of child abuse may be
subject to up to six months imprisonment in the county
jail or a fine not to exceed $1,000, or both. A mandated
reporter who willfully fails to report abuse or neglect, or
a person who impedes or inhibits a report of abuse or
neglect, where that abuse or neglect results in death or
great bodily injury, will be punished by not more than one
year in a county jail, a fine of up to $5,000, or both [Penal
Code Section 11166.01] The statutory provisions do not
affect the principle established in Landeros v. Flood, 17
Cal.3d 399 (1976), which imposes civil liability for a failure
to report child abuse (see “Civil Liability,” page7.2).
If a mandated reporter intentionally conceals his or her
failure to report an incident known by the mandated
reporter to be abuse or severe neglect under this section,
the failure to report is a continuing offense until an agency
specified in Section 11165.9 discovers the offense [Penal
Code Section 11166(c)].
K. Employer Obligations
OBTAIN EMPLOYEES’ ACKNOWLEDGMENT OF
REPORTING OBLIGATIONS
Hospitals and other employers of mandated reporters are
required to provide forms on which the mandated reporters
acknowledge that they are aware of the child abuse and
neglect reporting requirements and will comply with them.
The form must inform the employee that he or she is a
mandated reporter and inform the employee of his or her
reporting obligations under Penal Code Section 11166 and
of his or her confidentiality rights under Penal Code Section
11167(d). The employer must provide a copy of Penal Code
Sections 11165.7, 11166 and 11167 to the employee.
These statements must be retained by the employer. The
employer must bear the costs of printing, distributing and
filing the acknowledgment forms [Penal Code Section
11166.5].
The statements must be signed by any person hired after
Jan. 1, 1985, who is required to report.
Because this requirement applies only to employees hired
by a hospital, it does not apply specifically to medical staff
members who have no employment relationship with the
hospital. However, hospitals may choose to have medical
staff members acknowledge their awareness of their
obligations to report suspected instances of child abuse or
neglect, particularly if the medical staff members may be
treating possible victims of child abuse who present to the
emergency room.
The hospital may supplement its form by discussing any
special policy it has regarding notifying supervisors and
administration about reports that will be or are made, and
how the reporting is coordinated when several employees
become aware of the same instance of suspected child
abuse or neglect. Hospitals may use the “Employee
Acknowledgment of Child Abuse and Neglect Reporting
Obligations” form (CHA Form 19-2) for this purpose.
TRAIN EMPLOYEES
The law also strongly encourages employers to provide
their employees who are mandated reporters with
training in child abuse and neglect identification and
reporting. Whether or not employers provide this training,
the employers must provide their employees who are
mandated reporters with the required notice of their status
as a mandated reporter.
VI. ABUSE OF ELDERS AND DEPENDENT
ADULTS
A. Introduction
The Elder Abuse and Dependent Adult Civil Protection Act
[Welfare and Institutions Code Sections 15600-15659]
imposes mandatory reporting requirements for abuse of
elders and dependent adults. The reporting requirements
for elders and dependent adults are identical. Abuse of
an elder or dependent adult is a criminal act [Penal Code
Section 368].
Under the law, any mandated reporter who, in his or her
professional capacity, or within the scope of his or her
employment, has observed or has knowledge of an incident
that reasonably appears to be abuse, or is told by an
elder or dependent adult that he or she has experienced
behavior, including an act or omission, constituting abuse,
must report the known or suspected instance of abuse
by telephone or through a confidential Internet reporting
tool (when available) immediately or as soon as practicably
possible. If initially reported by telephone, a written report
or an Internet report must be sent within two working days.
Quicker reporting is required if the abuse occurred in a
long-term care facility. (See “To Whom Reports are Made;
Time Frames,” page7.25, for time frames.)
Abuse of an elder or a dependent adult includes physical
abuse, neglect, financial abuse, abandonment, isolation,
abduction or other treatment with resulting physical harm
or pain or mental suffering, or the deprivation by a care
custodian of goods or services that are necessary to avoid

CHA Mental Health Law Manual 2019
7.20
©CALIFORNIA HOSPITAL ASSOCIATION
physical harm or mental suffering [Welfare and Institutions
Code Section 15610.07]. Abuse does not include the use
of reasonable and necessary force by a peace officer acting
within the course of his or her employment [Penal Code
Section 11174.4].
WHO IS AN ELDER OR DEPENDENT ADULT?
Elders are persons 65 years of age or older. Dependent
adults are persons between ages 18 and 64 with physical
or mental limitations that restrict their ability to carry
out normal activities or protect their rights, including
persons with physical or developmental disabilities or
age-diminished physical or mental abilities. A person may
be considered a dependent adult even if he or she lives
independently. The law also expressly states that any
person between the ages of 18 and 64 who is admitted
as an inpatient
in an acute care hospital or other 24-hour
health facility is a dependent adult. (See Welfare and
Institutions Code Sections 15610.23 and 15610.27 for
definitions of relevant facilities.) [Welfare and Institutions
Code Sections 15610.23 and 15610.27]
B. Definitions
“Abandonment” means the desertion or willful forsaking
of an elder or dependent adult by anyone having care or
custody of that person under circumstances in which a
reasonable person would continue to provide care and
custody [Welfare and Institutions Code Section 15610.05].
“Abuse of an elder or a dependent adult” means physical
abuse, neglect, abandonment, isolation, abduction, or other
treatment with resulting physical harm or pain or mental
suffering, or the deprivation by a care custodian of goods
or services that are necessary to avoid physical harm or
mental suffering. Abuse of an elder or a dependent adult
also includes financial abuse as defined below. [Welfare and
Institutions Code Section 15610.07]
“Adult protective services agency” means a county
welfare department, except persons who do not work
directly with elders or dependent adults as part of their
official duties, including members of support staff and
maintenance staff [Welfare and Institutions Code Section
15610.13].
“Care custodian” means an administrator or an employee
of any of specified public or private facilities or agencies, or
persons providing care or services for elders or dependent
adults, including members of the support staff and
maintenance staff [Welfare and Institutions Code Section
15610.17]. These facilities and agencies include the
following: 24-hour health facilities as defined in Health and
Safety Code Sections 1250, 1250.2 and 1250.3; clinics;
home health agencies; agencies providing publicly funded
in-home supportive services, nutrition services, or other
home- and community-based support services; adult day
health care centers and adult day care; Alzheimer’s Disease
day care resource centers; community care facilities as
defined in Health and Safety Code Section 1502; residential
care facilities for the elderly as defined in Health and Safety
Code Section 1569.2; respite care facilities; and other
protective, public, sectarian, mental health, or private
assistance or advocacy agencies and persons providing
health services or social services to elders or dependent
adults. (See Welfare and Institutions Code Section
15610.17 for a complete list of “care custodians.”)
“Clergy member” means a priest, minister, rabbi, religious
practitioner or similar functionary of a church, synagogue,
temple, mosque or recognized religious denomination
or organization. Clergy member does not include unpaid
volunteers whose principal occupation or vocation does not
involve active or ordained ministry in a church, synagogue,
temple, mosque or recognized religious denomination
or organization, and who periodically visit elder or
dependent adults on behalf of that church, synagogue,
temple, mosque or recognized religious denomination
or organization. [Welfare and Institutions Code Section
15610.19]
“Endangered adult” means a dependent or elder adult
who is at immediate risk of serious injury or death, due to
suspected abuse or neglect and who demonstrates the
inability to take action to protect himself or herself from the
consequences of remaining in that situation or condition
[Welfare and Institutions Code Section 15701.25].
“Financial abuse” occurs when a person or entity takes,
secretes, appropriates, obtains, or retains (or assists
another to do so) real or personal property of an elder
or dependent adult for a wrongful use or with intent to
defraud or both, or by undue influence. A person or entity
shall be deemed to have taken, secreted, appropriated,
obtained, or retained for a wrongful use if, among other
things, the person did so knowing (or if the person should
have known) that this would likely be harmful to the elder
or dependent adult. Property includes any property right,
including by means of an agreement, donative transfer, or
testamentary bequest, regardless of whether the property
is held directly or by a representative. A representative is a
conservator, trustee or other representative of the estate of
an elder or dependent adult, or an attorney-in-fact acting
within the authority of the power of attorney. [Welfare and
Institutions Code Section 15610.30]

Chapter 7 — Reporting Assaults, Potentially Dangerous Patients and Firearms Prohibitions CHA
7.21
©CALIFORNIA HOSPITAL ASSOCIATION
“Goods and services necessary to avoid physical harm
or mental suffering” include, but are not limited to, all
of the following [Welfare and Institutions Code Section
15610.35]:
1. The provision of medical care for physical and mental
health needs.
2. Assistance in personal hygiene.
3. Adequate clothing.
4. Adequately heated and ventilated shelter.
5. Protection from health and safety hazards.
6. Protection from malnutrition, under those
circumstances where the results include, but are not
limited to, malnutrition and deprivation of necessities or
physical punishment.
7. Transportation and assistance necessary to secure any
of the needs set forth above.
“Health practitioner” includes a physician; psychiatrist;
psychologist; dentist; resident; intern; podiatrist;
chiropractor; registered nurse; dental hygienist; licensed
clinical social worker or associate clinical social worker;
associate clinical marriage and family therapist; licensed
professional clinical counselor; any other person who is
currently licensed under Business and Professions Code
Section 500 et seq.; emergency medical technician I or
II; paramedic; person certified pursuant to Health and
Safety Code Section 1797 et seq.; psychological assistant
registered pursuant to Business and Professions Code
Section 2913; marriage and family therapist trainee, as
defined in Business and Professions Code Section
4980.03; unlicensed associate marriage and family
therapist registered under Business and Professions Code
Section 4980.44; a professional clinical counselor trainee;
an associate professional clinical counselor; state or county
public health or social service employee who treats an elder
or a dependent adult for any condition; substance use
disorder counselor; or a coroner [Welfare and Institutions
Code Section 15610.37].
“Imminent danger” means a substantial probability that
an elder or dependent adult is in imminent or immediate
risk of death or serious physical harm, through either his
or her own action or inaction, or as a result of the action or
inaction of another person [Welfare and Institutions Code
Section 15610.39].
“Isolation” means any of the following [Welfare and
Institutions Code Section 15610.43]:
1. Acts intentionally committed for the purpose of
preventing, and that do serve to prevent, an elder
or dependent adult from receiving his or her mail or
telephone calls.
2. Telling a caller or prospective visitor that an elder or
dependent adult is not present, does not wish to talk
with the caller, or does not wish to meet with the visitor
where the statement is:
a. False;
b. Contrary to the express wishes of the elder or
dependent adult, whether he or she is competent
or not; and
c. Made for the purpose of preventing the elder or
dependent adult from having contact with family,
friends or concerned persons.
3. False imprisonment, as defined in Penal Code
Section 236.
4. Physical restraint of an elder or dependent adult for
the purpose of preventing him or her from meeting
with visitors.
These acts are subject to a rebuttable presumption that
they do not constitute isolation if they are performed
pursuant to the instructions of a physician licensed to
practice medicine in California, who is caring for the
elder or dependent adult at the time the instructions are
given, and who gives the instructions as part of his or her
medical care.
Also, these acts shall not constitute isolation if they are
performed in response to a reasonably perceived threat of
danger to property or physical safety.
“Local law enforcement agency” means a city police
or county sheriff’s department, or a county probation
department, except persons who do not work directly with
elders or dependent adults as part of their official duties,
including members of support staff and maintenance staff
[Welfare and Institutions Code Section 15610.45].
“Long-term care facility” means any of the following
[Welfare and Institutions Code Section 15610.47]:
1. A long-term health care facility, as defined in Health
and Safety Code Section 1418(a).
2. A community care facility, as defined in Health and
Safety Code Section 1502(a), whether licensed
or unlicensed.
3. A swing bed in an acute care facility, or an extended
care facility.
4. An adult day health care center as defined in Health
and Safety Code Section 1570.7(b).

CHA Mental Health Law Manual 2019
7.22
©CALIFORNIA HOSPITAL ASSOCIATION
5. A residential care facility for the elderly as defined in
Health and Safety Code Section 1569.2.
“Long-term care ombudsman” means the California
Long-Term Care Ombudsman, local ombudsman
coordinators, and other persons currently certified as
ombudsmen by the California Department of Aging as
described in Welfare and Institutions Code Section 9700 et
seq. [Welfare and Institutions Code Section 15610.50].
“Mental suffering” means:
1. Fear, agitation, confusion, severe depression or other
forms of serious emotional distress that is brought
about by forms of intimidating behavior, threats,
harassment or by deceptive acts performed; or
2. False or misleading statements made with malicious
intent to agitate, confuse, frighten or cause severe
depression or serious emotional distress of the elder or
dependent adult.
[Welfare and Institutions Code Section 15610.53]
“Neglect” means:
1. The negligent failure of a person having the care or
custody of an elder or a dependent adult to exercise
that degree of care that a reasonable person in a like
position would exercise; or
2. The negligent failure of an elder or dependent adult
to exercise that degree of self-care that a reasonable
person in a like position would exercise.
Neglect includes, but is not limited to, all of the following:
1. Failure to assist in personal hygiene, or in the provision
of food, clothing or shelter.
2. Failure to provide medical care for physical and mental
health needs. No person shall be deemed neglected
or abused for the sole reason that he or she voluntarily
relies on treatment by spiritual means through prayer
alone in lieu of medical treatment.
3. Failure to protect from health and safety hazards.
4. Failure to prevent malnutrition or dehydration.
If a person cannot provide the above for himself or
herself due to poor cognitive functions, mental limitation,
substance abuse or chronic poor health, this also
constitutes neglect.
[Welfare and Institutions Code Section 15610.57]
“Physical abuse” means all of the following, as these terms
are defined in the Penal Code [Welfare and Institutions
Code Section 15610.63]:
1. Assault
2. Battery
3. Assault with a deadly weapon or force likely to produce
great bodily injury
4. Unreasonable physical constraint, or prolonged or
continual deprivation of food or water
5. Sexual assault, which means any of the following:
a. Sexual battery
b. Rape
c. Rape in concert
d. Spousal rape
e. Incest
f. Sodomy
g. Oral copulation
h. Sexual penetration
i. Lewd or lascivious act
6. Use of a physical or chemical restraint or psychotropic
medication under any of the following conditions:
a. For punishment
b. For a period significantly beyond that for which the
restraint or medication is authorized by a physician
licensed in California who is providing medical
care to the elder or dependent adult at the time
the instructions are given
c. For any purpose not authorized by the physician
“Reasonable suspicion” means an objectively reasonable
suspicion that a person would entertain, based upon facts
that could cause a reasonable person in a like position,
drawing when appropriate upon his or her training and
experience, to suspect abuse [Welfare and Institutions
Code Section 15610.65].
“Serious bodily injury” means an injury involving extreme
physical pain, substantial risk of death, or protracted loss
or impairment of function of a bodily member, organ, or of
mental faculty, or requiring medical intervention, including,
but not limited to, hospitalization, surgery, or physical
rehabilitation [Welfare and Institutions Code Section
15610.67].
“Substance use disorder counselor” is a person providing
counseling services in an alcoholism or drug abuse
recovery and treatment program licensed, certified, or
funded under Part 2 (commencing with Section 11760) of
Division 10.5 of the Health and Safety Code.

Chapter 7 — Reporting Assaults, Potentially Dangerous Patients and Firearms Prohibitions CHA
7.23
©CALIFORNIA HOSPITAL ASSOCIATION
“Undue influence” means excessive persuasion that
causes another person to act or refrain from acting by
overcoming that person’s free will and results in inequity.
In determining whether a result was produced by undue
influence, all of the following must be considered:
1. The vulnerability of the victim. Evidence of vulnerability
may include, but is not limited to, incapacity, illness,
disability, injury, age, education, impaired cognitive
function, emotional distress, isolation, or dependency,
and whether the influencer knew or should have known
of the alleged victim’s vulnerability.
2. The influencer’s apparent authority. Evidence of
apparent authority may include, but is not limited to,
status as a fiduciary, family member, care provider,
health care professional, legal professional, spiritual
adviser, expert, or other qualification.
3. The actions or tactics used by the influencer. Evidence
of actions or tactics used may include, but is not
limited to, all of the following:
a. Controlling necessaries of life, medication, the
victim’s interactions with others, access to
information, or sleep.
b. Use of affection, intimidation, or coercion.
c. Initiation of changes in personal or property
rights, use of haste or secrecy in effecting those
changes, effecting changes at inappropriate
times and places, and claims of expertise in
effecting changes.
4. The equity of the result. Evidence of the equity of the
result may include, but is not limited to, the economic
consequences to the victim, any divergence from the
victim’s prior intent or course of conduct or dealing,
the relationship of the value conveyed to the value
of any services or consideration received, or the
appropriateness of the change in light of the length
and nature of the relationship.
Evidence of an inequitable result, without more, is not
sufficient to prove undue influence.
[Welfare and Institutions Code Section 15610.70]
C. Mandatory Reporting of Abuse
Certain categories of persons, referred to as mandated
reporters, are required to report any suspected abuse, as
defined, of elders or dependent adults.
MANDATED REPORTERS
Persons required to report elder or dependent adult
abuse are:
1. Elder or dependent adult “care custodians” (see
definition on page7.20; every employee of a hospital
is a “care custodian”).
2. Health practitioners (see page7.21.)
3. Clergy members.
4. Employees of a county adult protective services
agency or local law enforcement agency.
5. Any person who has assumed full or intermittent
responsibility for the care or custody of an elder or
dependent adult, whether or not that person receives
compensation, including administrators, supervisors,
and any licensed staff of a public or private facility that
provides care or services for elder or dependent adults
[Welfare and Institutions Code Section 15630(a)].
Exception
A mandated reporter who is a clergy member who acquires
knowledge or reasonable suspicion of elder or dependent
adult abuse during a penitential communication is not
required to report. “Penitential communication” means
a communication that is intended to be in confidence,
including, but not limited to, a sacramental confession
made to a clergy member who, in the course of the
discipline or practice of his or her church, denomination
or organization is authorized or accustomed to hear
those communications and under the discipline,
tenets, customs or practices of his or her church,
denomination or organization, has a duty to keep those
communications secret.
However, this exception does not modify or limit a clergy
member’s duty to report known or suspected elder and
dependent adult abuse if he or she is acting in the capacity
of a care custodian, health practitioner or employee of an
adult protective agency.
A clergy member who is not regularly employed on either
a full-time or part-time basis in a long-term care facility or
does not have care or custody of an elder or dependent
adult is not required to report abuse or neglect that is
not reasonably observable or discernible to a reasonably
prudent person having no specialized training or experience
in elder or dependent care.

CHA Mental Health Law Manual 2019
7.24
©CALIFORNIA HOSPITAL ASSOCIATION
WHAT TRIGGERS REPORTING OBLIGATION
General Rule
A report must be made by a mandated reporter who, in
his or her professional capacity or within the scope of his
or her employment [Welfare and Institutions Code Section
15630(b)]:
1. Has observed or has knowledge of an incident
that reasonably appears to be physical abuse,
abandonment, abduction, isolation, financial abuse or
neglect; or
2. Is told by an elder or dependent adult that he or she
has experienced behavior, including an act or omission,
constituting physical abuse, abandonment, abduction,
isolation, financial abuse or neglect; or
3. Reasonably suspects abuse.
No Duty to Investigate
A mandated reporter does not have a duty to investigate
a known or suspected incident of abuse. In fact, criminal
liability may arise where a mandated reporter undertakes
an investigation and determines that no report is needed
[People v. Davis, 126 Cal. App. 4th 1416 (2005)]. It is up
to the mandated reporter to report the facts giving rise to
the suspicion of abuse, and it is up to law enforcement to
investigate and determine whether abuse occurred.
Incidents That Do Not Need to Be Reported
A physician, registered nurse or psychotherapist as defined
in Evidence Code Section 1010 need not report an incident
if all of the following conditions exist:
1. The mandated reporter has been told by an elder
or dependent adult that he or she has experienced
behavior constituting physical abuse, abandonment,
abduction, isolation, financial abuse or neglect.
2. The mandated reporter is not aware of any
independent evidence that corroborates the statement
that the abuse has occurred.
3. The elder or dependent adult has been diagnosed
with a mental illness or dementia, or is the subject of
a court-ordered conservatorship because of a mental
illness or dementia.
4. The physician, registered nurse or psychotherapist as
defined in Evidence Code Section 1010 reasonably
believes, in the exercise of clinical judgment, that the
abuse did not occur.
(See “Definition of Psychotherapist,” page7.34, for a list
of which professionals are considered “psychotherapists”
pursuant to Evidence Code Section 1010.)
In addition, in a long-term care facility, a mandated reporter
need not report an incident where all of the following
conditions exist:
1. The mandated reporter is aware that there is a proper
plan of care.
2. The mandated reporter is aware that the plan of care
was properly provided or executed.
3. A physical, mental or medical injury occurred as a
result of care provided pursuant to the above.
4. The mandated reporter reasonably believes that the
injury was not the result of abuse.
This exception applies only to those categories of
mandated reporters that the California Department of
Public Health (CDPH) determines have access to plans
of care and have the training and experience necessary
to determine whether the conditions specified have been
met. A mandated reporter in a long-term care facility is not
required to seek, nor is precluded from seeking, information
regarding a known or suspected incident of abuse prior to
reporting.
D. Nonmandated Reporting
In addition to the reports of abuse that must be made
by mandated reporters, reports of other types of elder
or dependent adult abuse may be made by any person,
whether mandated reporters or other persons. Other forms
of elder or dependent adult abuse may include intimidation,
cruel punishment or other treatment that endangers an
elder or dependent adult’s emotional well-being. If a report
is not required to be made under California law, then it may
not be made by the patient’s health care provider unless
it also complies with federal privacy regulations, which
require that:
1. The victim agrees to the disclosure; or
2. The health care provider, in the exercise of professional
judgment, believes the disclosure is necessary to
prevent serious harm to the victim or other potential
victims; or
3. If the victim is unable to agree because of incapacity, a
law enforcement or other public official authorized to
receive the report represents that the protected health
information to be disclosed is not intended to be used
against the victim and that an immediate enforcement
activity that depends upon the disclosure would be
materially and adversely affected by waiting until the
victim is able to agree to the disclosure. [45 C.F.R.
Section 164.512(c); Civil Code Section 56.10(c)(14)]

Chapter 7 — Reporting Assaults, Potentially Dangerous Patients and Firearms Prohibitions CHA
7.25
©CALIFORNIA HOSPITAL ASSOCIATION
BY MANDATED REPORTERS
If making the report satisfies the standards described
above, then a mandated reporter may file a report where
that person knows, or reasonably suspects, that types of
elder or dependent adult abuse for which reports are not
mandated have been inflicted on an elder or dependent
adult or that the emotional well-being of an elder or
dependent adult is endangered in any other way [Welfare
and Institutions Code Section 15630(c)].
If the suspected abuse occurred in a long-term care
facility other than a state mental health hospital or a state
developmental center, the report may be made to the
long-term care ombudsman program.
If the suspected abuse occurred in a state mental health
hospital or a state developmental center, the report may
be made to the designated investigator of the California
Department of State Hospitals or the California Department
of Developmental Services, or to a local law enforcement
agency or to the local ombudsman.
If the suspected abuse occurred in any other place,
the report may be made to the county adult protective
services agency.
If the conduct involves criminal activity not constituting
abuse, it may also be immediately reported to the
appropriate law enforcement agency, if such reporting
complies with federal privacy regulations (see chapter 6).
(See also M.“Federal Requirements,” page7.30.)
BY OTHER PERSONS
A person who is not a mandated reporter who knows or
reasonably suspects that an elder or dependent adult has
been the victim of abuse may report that abuse as follows
[Welfare and Institutions Code Section 15631]:
1. If the abuse is alleged to have occurred in a long-term
care facility, the report may be made to a long-term
care ombudsman program or local law enforcement
agency, or both.
2. If the abuse is alleged to have occurred in any place
other than a long-term care facility, the report may be
made to the county adult protective services agency or
local law enforcement agency.
However, the federal privacy requirements described
in D.“Nonmandated Reporting,” page7.24, must be
met before a report may be made by the victim’s health
care provider.
E. Making Reports
TO WHOM REPORTS ARE MADE; TIME FRAMES
Abuse Occurring in a Long-Term Care Facility
If suspected or alleged abuse occurred in a long-term care
facility (except a state mental health hospital or a state
developmental center), the following reporting requirements
apply.
Physical Abuse. If suspected or alleged physical abuse
occurred in a long-term care facility and results in serious
bodily injury:
1. A telephone report must be made to the local law
enforcement agency immediately, but also no later than
within two hours of the mandated reporter observing,
obtaining knowledge of, or suspecting the physical
abuse; and
2. A written report must be made to the local
ombudsman, the facility’s licensing agency (CDPH
for hospitals and nursing facilities, Department of
Social Services for board and care facilities), and the
local law enforcement agency within two hours of the
mandated reporter observing, obtaining knowledge of,
or suspecting the physical abuse.
If suspected or alleged physical abuse occurred in a
long-term care facility and does not result in serious
bodily injury:
1. A telephone report must be made to the local law
enforcement agency within 24 hours of the mandated
reporter observing, obtaining knowledge of, or
suspecting the physical abuse; and
2. A written report must be made to the local
ombudsman, the facility’s licensing agency (CDPH
for hospitals and nursing facilities), and the local law
enforcement agency within 24 hours of the mandated
reporter observing, obtaining knowledge of, or
suspecting the physical abuse.
However, if the suspected abuse is allegedly caused by a
resident with a physician’s diagnosis of dementia, and there
is no serious bodily injury (as reasonably determined by
the mandated reporter, drawing upon his or her training or
experience), the reporter must:
1. Report to the local ombudsman or law enforcement
agency by telephone, immediately or as soon as
practicably possible; and
2. Make a written report within 24 hours.

CHA Mental Health Law Manual 2019
7.26
©CALIFORNIA HOSPITAL ASSOCIATION
Abuse Other Than Physical Abuse. If suspected or
alleged abuse other than physical abuse occurred in a
long-term care facility (except a state mental health hospital
or a state developmental center), a telephone report and
a written report must be made to the local ombudsman or
the local law enforcement agency within the time frames
noted above for physical abuse that does not result in
serious bodily injury (see above).
A report must also be made to CDPH immediately or within
24 hours [Health and Safety Code Section 1418.91; Title
22, California Code of Regulations, Section 72541].
Abuse Occurring in a State Facility
If the suspected or alleged abuse occurred in a state
mental health hospital or a state developmental center, the
report must be made to designated investigators of the
California Department of State Hospitals or the California
Department of Developmental Services, or to the local
law enforcement agency. The report must be made by
telephone or through a confidential Internet reporting
tool immediately or as soon as practicably possible after
receiving the information concerning the incident. If the
initial report is made by telephone, a written report or an
Internet report must be sent to the appropriate agency
within two working days of receiving the information
concerning the incident.
If the suspected or alleged abuse or neglect resulted in
any of the following incidents, a report must be made
to designated investigators of the State Department of
State Hospitals or the State Department of Developmental
Services, and also to the local law enforcement agency:
1. A death.
2. A sexual assault, as defined in Welfare and Institutions
Code Section 15610.63.
3. An assault with a deadly weapon, as described Penal
Code Section 245, by a nonresident of the state
mental hospital or state developmental center.
4. An assault with force likely to produce great bodily
injury, as described in Penal Code Section 245.
5. An injury to the genitals when the cause of the injury
is undetermined.
6. A broken bone when the cause of the break
is undetermined.
Abuse Occurring Elsewhere
If the suspected or alleged abuse occurred in any other
place, the report must be made to the adult protective
services agency or the local law enforcement agency.
The report must be made by telephone or through a
confidential Internet reporting tool immediately or as soon
as practicably possible after receiving the information
concerning the incident. If the initial report is made by
telephone, a written report or an Internet report must be
sent to the appropriate agency within two working days of
receiving the information concerning the incident.
TELEPHONE OR INTERNET REPORT
A report by telephone or through a confidential Internet
reporting tool must include, if known:
1. The name of the person making the report.
a. If the person is one who is not a mandated
reporter, the person is not required to include
his or her name [Welfare and Institutions Code
Section 15633.5(d)].
b. If the name is given, the person’s identity
is confidential and disclosed only under
limited circumstances.
2. The name and age of the elder or dependent adult.
3. The present location of the elder or dependent adult.
4. The names and addresses of family members or any
other adult responsible for the elder’s or dependent
adult’s care.
5. The nature and extent of the elder’s or dependent
adult’s condition.
6. The date of the incident.
7. Any other information requested by the agency
receiving the report, including information that led the
person to suspect elder or dependent adult abuse.
[Welfare and Institutions Code Section 15630(e)]
WRITTEN REPORT
If the initial report is made by telephone, a written report or
an Internet report must be sent to the appropriate agency
[Welfare and Institutions Code Section 15630(b)]. Reports
should be submitted on forms adopted by the California
Department of Social Services [Welfare and Institutions
Code Section 15658(a)]. The current form is “Report of
Suspected Dependent Adult/Elder Abuse” (SOC 341). This
form can be obtained from county adult protective services
agencies, long-term care ombudsman coordinators or at
www.ccfmtc.org.

Chapter 7 — Reporting Assaults, Potentially Dangerous Patients and Firearms Prohibitions CHA
7.27
©CALIFORNIA HOSPITAL ASSOCIATION
SELECTION OF A PERSON TO REPORT
In the hospital, two or more people may become jointly
aware of the same instance of reportable elder or
dependent adult abuse. The law allows them to select, by
mutual agreement, a single person who will be responsible
for making the report. However, if one of these persons
knows that the designated person failed to report, that
person must thereafter make the report [Welfare and
Institutions Code Section 15630(d)].
The law allows the hospital to create internal procedures
to facilitate reporting, ensure confidentiality and apprise
supervisors and administrators of reports. These
procedures must make clear that reporting duties are
individual, that no supervisor or administrator may impede
or inhibit such reporting, and that a person is not subject
to sanctions for making a report [Welfare and Institutions
Code Section 15630(f)].
F. Notification of Patient/Victim That Report Will
be Made
The victim must be notified that a report has been or will
be made. (See C.“Informing the Patient of Reporting,”
page7.1, for information about this requirement.)
G. Forensic Medical Reports
Cal OES has developed forensic medical report forms,
instructions, and examination protocols, available at www.
ccfmtc.org. The form that providers must use for elder and
dependent adult abuse and neglect is “Forensic Medical
Report: Elder and Dependent Adult Abuse and Neglect
Examination” (Cal OES 2-602).
DOCUMENTATION IN THE MEDICAL RECORD
The forensic medical forms must become part of the
patient’s medical record pursuant to guidelines established
by the agency or agencies designated by the California
Offices of Emergency Services advisory committee.
Hospitals may wish to consider putting the forensic medical
reports in a separate section of the medical record to
prevent routine copying and disclosure of these reports for
purposes not related to the criminal justice system, and
to prevent improper release to unauthorized persons. The
completed forms are subject to the special confidentiality
laws pertaining to release of forensic medical examination
records (see I.“Confidentiality of Reports,” page7.18).
[Penal Code Section 11161.2(b)(3)]
The hospital’s initial report to law enforcement is not
required to be placed in the medical record. Hospitals
should develop a policy regarding maintenance of reports
to maintain confidentiality of the reporter’s identity (see
J.“Confidentiality of Reports; Disclosures,” page7.28).
H. Sanctions for a Failure to Report
A person who is required, but fails, to report an instance
of elder or dependent adult abuse may be found guilty
of a misdemeanor. A person who impedes or inhibits a
report may also be found guilty of a misdemeanor. The
punishment may include up to six months imprisonment
in the county jail, a fine of up to $1,000, or both. Any
mandated reporter who willfully fails to report an instance
of elder or dependent adult abuse, or impedes or inhibits
a report, where that abuse results in death or great bodily
injury, is punishable by not more than one year in a county
jail or by a fine of up to $5,000 or both. If a mandated
reporter intentionally conceals his or her failure to report an
incident known by the mandated reporter to be abuse or
severe neglect, the failure to report is a continuing offense
until the responsible law enforcement agency discovers the
offense. [Welfare and Institutions Code Section 15630(h)]
It is illegal for a person to do any of the following under
circumstances likely to produce great bodily harm or death:
1. Willfully cause or permit any elder or dependent adult
to suffer, or
2. Inflict unjustifiable physical pain or mental suffering
upon any elder or dependent adult, or
3. Having the care or custody of any elder or dependent
adult, willfully cause or permit the person or health of
the elder or dependent adult to be injured, or willfully
cause or permit the elder or dependent adult to be
placed in a situation in which his or her person or
health is endangered.
This illegal behavior is punishable by imprisonment in a
county jail not exceeding one year, by a fine not to exceed
$6,000 upon a first conviction or $10,000 for a subsequent
conviction, by both that fine and imprisonment, or by
imprisonment in the state prison for two, three, or four
years. If in the commission of this offense the victim suffers
great bodily injury, as defined, or death, the defendant shall
receive an additional term in the state prison. [Penal Code
Section 368]

CHA Mental Health Law Manual 2019
7.28
©CALIFORNIA HOSPITAL ASSOCIATION
I. Immunity From Liability
No care custodian, clergy member, health practitioner,
mandated reporter of suspected financial abuse of an elder
or dependent adult, or employee of an adult protective
services agency or local law enforcement agency shall incur
any civil or criminal liability as a result of making a report
required or authorized by the statute. No other person
reporting a suspected instance of dependent adult abuse
shall incur civil or criminal liability as a result of making any
report authorized by the law unless it can be proved that
a false report was made and the person knew it was false
[Welfare and Institutions Code Section 15634(a)].
PROVIDING ACCESS TO THE VICTIM
No care custodian, clergy member, health practitioner,
mandated reporter of suspected financial abuse of
an elder or dependent adult, or employee of an adult
protective services agency or local law enforcement
agency investigating a report of known or suspected elder
or dependent adult abuse shall incur any civil or criminal
liability for providing an adult protective services agency or
local law enforcement agency with access to a victim of
suspected or known dependent adult abuse, when done
at the request of the agency [Welfare and Institutions Code
Section 15634(b)].
PHOTOGRAPHING OF SUSPECTED ABUSE
No person required to make a report, nor any person
taking photographs at his or her direction, shall incur
any civil or criminal liability for taking photographs of a
suspected victim of elder or dependent adult abuse, or
causing photographs to be taken of such a victim, or for
disseminating such photographs with the reports required
by statute. However, the law does not confer immunity from
liability with respect to any other use of such photographs
[Welfare and Institutions Code Section 15634(a)].
If the hospital can do so, it may wish to obtain such
photographs to provide documentation should a question
arise in the future concerning the justification for any report
made by hospital personnel.
ATTORNEYS’ FEES
A care custodian, clergy member, health practitioner or
employee of an adult protective services agency or local
law enforcement agency who is sued as a result of making
a report that is required or authorized under the statute
may recover from the state the attorneys’ fees spent
defending against the action, if the person prevails. The
state is required to reimburse the person for the reasonable
attorneys’ fees at hourly rates based upon the rates
charged by the California Attorney General, up to $50,000.
A claim may be filed with the Department of General
Services. [Welfare and Institutions Code Section 15634(c)]
EMPLOYERS
The failure of any employee or other person associated
with the employer to report physical abuse of elders or
dependent adults or otherwise meet the requirements of
the abuse reporting law is the sole responsibility of such
person. The person’s employer or facility shall incur no civil
or other liability for the failure of these persons to comply
with the abuse reporting law [Welfare and Institutions Code
Section 15659(f)].
J. Confidentiality of Reports; Disclosures
Reports of elder and dependent adult abuse are
confidential and may be disclosed only as provided by
statute [Welfare and Institutions Code Section 15633].
According to the statute, reports (and the information
contained therein) may be disclosed only as follows:
1. To persons or agencies to whom disclosure of
information or the identity of the reporter is permitted
(see below).
2. Persons who are trained and qualified to serve on
multidisciplinary personnel teams may disclose to one
another information and records that are relevant to
the prevention, identification or treatment of abuse of
elderly or dependent adults.
Disclosure is not authorized by this statute if such
disclosure is prohibited by any other applicable provision of
state or federal law. (See chapter 6 for further information
about privacy implications.)
However, these disclosures may be made only:
1. If the victim agrees to the disclosure; or
2. If the health care provider, in the exercise of
professional judgment, believes the disclosure is
necessary to prevent serious harm to the victim or
other potential victims; or
3. If the victim is unable to agree because of incapacity, a
law enforcement or other public official authorized to
receive the report represents that the protected health
information to be disclosed is not intended to be used
against the victim and that an immediate enforcement
activity that depends upon the disclosure would be
materially and adversely affected by waiting until the
victim is able to agree to the disclosure. [45 C.F.R.
Section 164.512(c)]

Chapter 7 — Reporting Assaults, Potentially Dangerous Patients and Firearms Prohibitions CHA
7.29
©CALIFORNIA HOSPITAL ASSOCIATION
DISCLOSURE OF INFORMATION REGARDING ABUSE
Information relevant to the incident of elder or dependent
adult abuse may be given to an investigator from an adult
protective services agency, a local law enforcement agency,
the office of the district attorney, the office of the public
guardian, the probate court, the bureau, or an investigator
of the Department of Consumer Affairs, Division of
Investigation who is investigating a known or suspected
case of elder or dependent adult abuse. [Welfare and
Institutions Code Section 15633]
In addition, a health care provider may, upon written
request, disclose otherwise confidential medical information
to an elder death review team in certain circumstances (see
CHA’s California Health Information Privacy Manual; order
online at www.calhospital.org/privacy).
[Penal Code Section 11174.8]
DISCLOSURE OF REPORTER’S IDENTITY
The identity of persons making reports is confidential and
may be disclosed only among the following agencies or
persons representing an agency:
1. An adult protective services agency.
2. A long-term care ombudsperson program.
3. A licensing agency.
4. A local law enforcement agency.
5. The office of the district attorney.
6. The office of the public guardian.
7. The probate court.
8. The Bureau of Medi-Cal Fraud within the Office of the
California Attorney General.
9. The California Department of Consumer Affairs,
Division of Investigation.
10. Counsel representing an adult protective
services agency.
The identity of a person who reports under this law may
also be disclosed under the following circumstances:
1. To the district attorney in a criminal prosecution.
2. When a person reporting waives confidentiality.
3. By court order.
[Welfare and Institutions Code Section 15633.5]
K. Employees’ Acknowledgment of Reporting
Obligations
Hospitals, and other employers of health practitioners,
clergy members and care custodians, are required to
provide forms on which persons hired for such positions
acknowledge that they are aware of the elder and
dependent adult abuse reporting requirements (specifically,
Welfare and Institutions Code Section 15630) and will
comply with them. A copy of Welfare and Institutions
Code Section 15630 must be provided to each employee.
These statements must be signed by the employee prior
to commencing employment (for employees hired after
Jan. 1, 1995). The signed statements must be retained
by the employer. The law does not specify how long the
statements must be retained; it is recommended that
they be retained at least as long as the employee remains
employed. [Welfare and Institutions Code Section 15659]
A form developed by the California Department of Social
Services may be used (SOC 341A) and can be downloaded
at www.cdss.ca.gov/inforesources/Forms-Brochures/
Forms-Alphabetic-List/Q-T#soc. CHA has also developed a
form, “Employee Acknowledgment of Elder and Dependent
Adult Abuse Reporting Obligations” (CHA Form 19-4), that
hospitals may use.
The hospital may supplement the acknowledgment and
notice by discussing any special policy it has regarding
notifying supervisors and administration about reports that
will be or are made, and how the reporting is coordinated
when several employees become aware of the same
instance of suspected elder or dependent adult abuse.
L. Employer Obligation to Train Employees
Every long-term care facility (as defined in Health and
Safety Code Section 1418), every community care facility
(as defined in Health and Safety Code Section 1502), and
every residential care facility for the elderly (as defined in
Health and Safety Code Section 1569.2) that provides
care to adults, must train its employees in recognizing and
reporting elder and dependent adult abuse, as prescribed
by the California Department of Justice. It is recommended
that general acute care hospitals also provide this training.
These facilities must also provide all staff being trained
a written copy of the reporting requirements and written
notification of the staff’s confidentiality rights under
Welfare and Institutions Code Section 15633.5 (see
I.“Confidentiality of Reports,” page7.18). The “Employee
Acknowledgment of Elder and Dependent Adult Abuse
Reporting Obligations” (CHA Form 19-4) fulfills these
requirements. Facilities may provide employees being

CHA Mental Health Law Manual 2019
7.30
©CALIFORNIA HOSPITAL ASSOCIATION
trained a copy of the portion of CHA’s Consent Manual that
describes the California elder and dependent adult abuse
reporting laws to comply with this requirement.
New employees must be trained within 60 days of the
first day of employment. [Welfare and Institutions Code
Section 15655]
The California Department of Justice, in cooperation
with the California Department of Public Health and the
California Department of Social Services has developed a
minimal core training program that facilities may use.
M. Federal Requirements
REPORTING
The Elder Justice Act requires specified long-term care
facilities to report a reasonable suspicion of a crime
against a resident or other person receiving care from the
facility. The age of the resident and the location where the
crime occurred are irrelevant under this law. If the incident
results in serious bodily injury, it must be reported within
two hours of becoming aware of it. Otherwise, reporting
must take place within 24 hours. (See “Abuse Occurring
in a Long-Term Care Facility,” page7.25, for information
regarding to whom reports must be made.)
Failure to report as required by federal law may result in a
civil money penalty of up to $300,000 and exclusion from
participation in federal health care programs.
NOTIFYING EMPLOYEES AND OTHERS OF REPORTING
OBLIGATIONS
The Elder Justice Act requires the owner or operator of
a long-term care facility to annually notify each covered
individual of his/her obligation to comply with the federal
reporting requirements. A “covered individual” includes
each individual who is an owner, operator, employee,
manager, agent or contractor of the facility.
NONRETALIATION AND SIGNAGE
Facilities must adopt a non-retaliation policy and post signs
that specify the rights of employees under this law and tell
how an employee may file a complaint with the Secretary of
the U.S. Department of Health and Human Services against
a facility that violates this law. The Centers for Medicare &
Medicaid Services (CMS) is required to develop a model
sign. However, at the time of publication of this manual,
CMS had not done so. However, CMS issued a guidance
about the poster, S&C: 11-30-NH (revised 1-20-12)
available at www.cms.gov/Medicare/Provider-Enrollment-
and-Certification/SurveyCertificationGenInfo/downloads/
SCLetter11_30.pdf.
[42 U.S.C. Section 1320b-25]
N. Detention of Endangered Adults
The law allows (but does not require) a physician treating an
adult, if he/she determines that the adult is an endangered
adult (defined in B.“Definitions,” page7.20), to delay the
release of the endangered adult until:
1. A local law enforcement agency takes custody of the
endangered adult;
2. The responding agency determines that the adult is not
endangered; or
3. The responding agency takes other appropriate action
to ensure the safety of the endangered adult.
This law applies whether or not medical treatment is
required by the adult. [Welfare and Institutions Code
Section 15703.05]
Law enforcement officers and other designated persons
may take an endangered adult to temporary emergency
protective custody in certain circumstances for up to 72
hours. In such cases, the endangered adult must be taken
to a hospital if medical evaluation and treatment is required.
[Welfare and Institutions Code Section 15703]
During the 72-hour custody, the endangered adult will be
transferred to an appropriate temporary residence while
an investigation is conducted and a judicial hearing takes
place. The temporary residence may include a hospital
[Welfare and Institutions Code Section 15701.05].
Following the judicial hearing, the court may order the
provision of protective services on an emergency basis
for up to 14 business days. The court must specifically
designate the approved services in the emergency order.
An emergency order for protective services does not
include hospitalization unless the court order specifically
states otherwise. The emergency order will designate an
appropriate temporary conservator of the endangered adult
who is responsible for the care of the endangered adult and
who may consent for the provision of protective services,
including health related services, for the endangered adult.
This law specifically states that it must not be used to
circumvent the involuntary commitment process provided
for in Welfare and Institutions Code Section 5150 et seq.
[Welfare and Institutions Code Sections 15703-15705.40].
(See chapter 3 regarding involuntary commitment laws.)

Chapter 7 — Reporting Assaults, Potentially Dangerous Patients and Firearms Prohibitions CHA
7.31
©CALIFORNIA HOSPITAL ASSOCIATION
VII. INJURY OR CONDITION IN A PATIENT
RECEIVED FROM A LICENSED HEALTH
FACILITY RESULTING FROM NEGLECT OR
ABUSE
A. Statutory Duty of Hospital and Physician to
Report
Hospitals and physicians must report by telephone and in
writing within 36 hours to the local police and the county
health department if a patient is received from a health
facility or community care facility (as defined in Health and
Safety Code Sections 1250 et seq. and 1502 et seq.) who
exhibits a physical injury or condition which, in the opinion
of the examining physician, reasonably appears to be the
result of neglect or abuse. [Penal Code Section 11161.8]
Although the initial justification for and apparent legislative
intent was to require reporting in cases of suspected
neglect or abuse in patients received from nursing homes
only, the present statutory language is much broader and
requires reporting with respect to neglected or abused
patients of any age received from essentially any licensed
health care facility or community care facility.
This law was written long before the law regarding elder
and dependent adult abuse and neglect was amended
to require reporting of abuse that occurs in a long-term
care facility within two or 24 hours. Facilities should follow
the requirements of both laws if the patient is an elder or
dependent adult. (See VI.“Abuse of Elders and Dependent
Adults,” page7.19.)
CONTENTS OF REPORT
Telephone and written reports must state the character and
extent of the physical injury or condition.
Telephone Report
Although both the physician and hospital have an
independent duty to report, a single telephone report
will satisfy the requirement for an oral report. It is
recommended that the examining physician make the
telephone report.
Written Report
The “Report of Injury or Condition Resulting from Neglect
or Abuse (To a Patient Received from a Licensed Health
Facility)” (CHA Form 19-3) has been developed to meet
this reporting requirement. It is recommended that the
form be completed and signed by the examining physician
and then forwarded to the hospital administrator, or his or
her designee, for signature and transmission to both the
local police authority having jurisdiction and the county
health department.
NOTIFICATION OF PATIENT/VICTIM THAT REPORT
WILL BE MADE
The patient must be informed that a report has been or
will be made. (See C.“Informing the Patient of Reporting,”
page7.1.)
B. Optional Reporting by Nurses and Social
Workers
A registered nurse, licensed vocational nurse or licensed
clinical social worker employed at the admitting hospital
may report to the local police authority and the county
health department the fact that a patient received from
a health facility or community care facility, (as defined in
Health and Safety Code Sections 1250 and 1502), exhibits
a physical injury or condition which, in the opinion of the
nurse or social worker, reasonably appears to be the result
of neglect or abuse. [Penal Code Section 11161.8]
Reporting by nurses and social workers is not required by
statute, and hence, penalties for failure to report do not
apply. Except for victims of child abuse, federal privacy
regulations restrict the making of an optional report to
situations in which:
1. The victim agrees to the disclosure; or
2. The health care provider, in the exercise of professional
judgment, believes the disclosure is necessary to
prevent serious harm to the victim or other potential
victims; or
3. If the victim is unable to agree because of incapacity, a
law enforcement or other public official authorized to
receive the report represents that the protected health
information to be disclosed is not intended to be used
against the victim and that an immediate enforcement
activity that depends upon the disclosure would be
materially and adversely affected by waiting until the
victim is able to agree to the disclosure. [45 C.F.R.
Section 164.512(c)]
No employee may be discharged, suspended, disciplined
or harassed for making such a report.
C. Immunity From Liability
Penal Code Section 11161.8 provides that no person shall
incur any civil or criminal liability as a result of making a
report authorized by the law.

CHA Mental Health Law Manual 2019
7.32
©CALIFORNIA HOSPITAL ASSOCIATION
VIII. SCREENING FOR DOMESTIC VIOLENCE
A. Screening Policies
General acute care hospitals, acute psychiatric hospitals,
special hospitals, psychiatric health facilities and chemical
dependency recovery hospitals must establish written
policies and procedures for routine screening of patients for
purposes of detecting spousal or partner abuse [Health and
Safety Code Section 1259.5]. The policies must include
guidelines on all of the following:
1. Identifying, through routine screening, spousal or
partner abuse among patients.
2. Documenting patient injuries or illnesses attributable to
spousal or partner abuse.
3. Educating appropriate hospital staff about the criteria
for identifying, and the procedures for handling,
patients whose injuries or illnesses are attributable to
spousal or partner abuse.
4. Advising patients exhibiting signs of spousal or
partner abuse of crisis intervention services that
are available either through the hospital or through
community-based intervention and counseling services.
5. Providing patients who exhibit signs of spousal or
partner abuse with information on domestic violence
and a referral list, to be updated periodically, of private
and public community agencies that serve persons
experiencing spousal or partner abuse, including
hotlines, shelters, legal services and information about
temporary restraining orders.
This law does not define “spousal abuse” or “partner
abuse.” However, Penal Code Section 273.5 states that
any person who willfully inflicts upon a person who is his or
her current or former spouse, cohabitant, fiancé or fiancée,
or dating partner, or the mother or father of his or her child,
corporal injury resulting in a traumatic condition is guilty of
a felony, and upon conviction thereof shall be punished by
imprisonment or by a fine or by both. As used in this law,
“traumatic condition” means a condition of the body, such
as a wound, or external or internal injury, including, but not
limited to, injury as a result of strangulation or suffocation,
whether of a minor or serious nature, caused by a physical
force. For purposes of this section, “strangulation” and
“suffocation” include impeding the normal breathing or
circulation of the blood of a person by applying pressure on
the throat or neck.
The Penal Code section discussed above does not discuss
abuse of persons who are dating but not cohabiting or
coparenting, or abuse of same-sex partners. However,
such abuse should also be reported as assaultive or
abusive conduct (see III.“Reporting Injuries by Firearm
or Assaultive or Abusive Conduct (“Suspicious Injuries”),”
page7.3).
Emotional or verbal abuse does not appear to be
reportable.
Similar requirements apply to licensed clinics [Health and
Safety Code Section 1233.5; Penal Code Section 13700].
B. Domestic Violence Indicators
Some indicators that may raise a suspicion of domestic
violence include:
1. Patient’s explanation of injury is inconsistent with
appearance of injury
2. Unexplained delay in seeking treatment
3. Patient is under or overly concerned with an injury
4. History of non-specific physical or somatic complaints
5. Overly attentive or aggressive partner
6. Multiple injuries with varying stages of healing
The health care provider may wish to question the patient
when he or she is alone and ask something along the lines
of, “Because violence is so prevalent in our society, I ask
all my patients about abuse. Have you ever been hurt or
threatened by a partner or ex-partner?”
If the patient answers in the affirmative, providers may
take a history, assess patient safety, provide emotional
support, provide medical/legal/social services referral
information, and document. Providers may wish to discuss
with the patient the legal obligation to report (if applicable)
and provide the patient with referrals so they can go to
a protected environment due to the risk of the abuser’s
retaliation after a report is made.
C. Reporting Requirements
Domestic violence must be reported if it meets the
requirements of any of the following reporting laws:
1. Injury by firearm or assaultive or abusive conduct
(also known as “suspicious injury reporting”) (see
III.“Reporting Injuries by Firearm or Assaultive or
Abusive Conduct (“Suspicious Injuries”),” page7.3).
2. Sexual assault or rape (see IV.“Sexual Assault and
Rape,” page7.5).
3. Elder or dependent adult abuse (see VI.“Abuse of
Elders and Dependent Adults,” page7.19).

Chapter 7 — Reporting Assaults, Potentially Dangerous Patients and Firearms Prohibitions CHA
7.33
©CALIFORNIA HOSPITAL ASSOCIATION
D. Forms
Cal OES has developed a form (Cal OES 2-502),
instructions, and examination protocol for use in cases of
domestic abuse. They may be found at www.ccfmtc.org.
IX. POTENTIALLY DANGEROUS PATIENTS: DUTY
TO WARN POTENTIAL VICTIMS AND NOTIFY
LAW ENFORCEMENT
A. Duty to Warn Potential Victims
The California Supreme Court held in Tarasoff v. Regents
of the University of California, 17 Cal.3d 425 (1976), that
a psychotherapist has a duty to warn, or take other
appropriate action to protect, the foreseeable victim or
victims of a patient’s violent tendencies, if:
1. A psychotherapist-patient relationship exists,
2. The psychotherapist knows or should know that the
patient is dangerous, and
3. There is a foreseeable victim or victims of the patient’s
violent tendencies.
According to the court, when a therapist determines
(or pursuant to the standards of the profession should
determine) that a patient presents a serious danger of
violence to another, the therapist has a duty to use
reasonable care to protect the intended victim against the
danger. Depending on the nature of the case, the discharge
of this duty may require the therapist to take one or more
steps, including warning the intended victim or others likely
to apprise the victim of the danger, notifying the police, or
taking other steps that may be reasonably necessary under
the circumstances. After the court’s decision, the California
legislature enacted an immunity statute under which, if a
warning is required, the psychotherapist must at least notify
both the potential victim(s) and law enforcement.
In carrying out this duty, the psychotherapist may need
to release confidential patient information. The court held
that in these situations, the justification for protecting
the patient’s confidentiality (e.g., to encourage patients
to seek treatment and fully disclose information to their
psychotherapist) is outweighed by the need to warn
potential victims so that they can protect themselves. In
addition, the Confidentiality of Medical Information Act and
Welfare and Institutions Code Section 5328(a)(18) allow the
release of confidential information when a psychotherapist
believes that a patient presents a serious danger of
violence to a reasonably foreseeable victim or victims.
Also, the psychotherapist-patient privilege does not apply
if the psychotherapist has reasonable cause to believe
that the patient is in such mental or emotional condition
as to be dangerous to himself or to the person or property
of another, and that disclosure of the communication is
necessary to prevent the threatened danger (see Evidence
Code Section 1024). The HIPAA privacy regulations also
permit these disclosures [45 C.F.R. Section 164.512(j)(l)(i)].
B. Duty to Notify Law Enforcement Agency
A licensed psychotherapist is required to report, within
24 hours, to a local law enforcement agency the identity
of a person who has communicated to the licensed
psychotherapist a serious threat of physical violence
against a reasonably identifiable victim or victims.
A “licensed psychotherapist,” for purposes of this
requirement, is defined in Evidence Code Section 1010,
subdivisions (a) to (e), as a person who is, or is reasonably
believed by the patient to be:
1. A person authorized to practice medicine in any state
or nation who devotes, or is reasonably believed by
the patient to devote, a substantial portion of his or her
time to the practice of psychiatry.
2. A licensed psychologist.
3. A licensed clinical social worker, when he or
she is engaged in applied psychotherapy of a
nonmedical nature.
4. A credentialed school psychologist.
5. A licensed marriage and family therapist.
[Welfare and Institutions Code Sections 8100(b)(1) and
8105(c)]
Note that the definition of “psychotherapist” for the
purposes of this requirement is narrower than the
definition of “psychotherapist” under the immunity statute
discussed below.
The report to law enforcement should be made by
telephone and be followed by a written letter documenting
the telephone report. A copy of the letter should be
retained by the hospital. The psychotherapist may also
need to warn potential victims, as described above. (See
also 45 C.F.R. Section 164.512(j)(l)(i).)

CHA Mental Health Law Manual 2019
7.34
©CALIFORNIA HOSPITAL ASSOCIATION
C. Immunity From Liability
IMMUNITY FOR PSYCHOTHERAPISTS
Civil Code Section 43.92 provides immunity to
psychotherapists for failure to protect from a patient’s
violent behavior except if the patient has communicated to
the psychotherapist a serious threat of physical violence
against persons. That statute describes a duty to warn and
protect as well as how that duty might be met.
NOTE: Effective Jan. 1, 2014, the California legislature
changed the name of the “duty to warn and protect” to
the “duty to protect” in this law. However, the law explicitly
stated that changing the name shall not be “construed to
be a substantive change, and any duty of a psychotherapist
shall not be modified as a result of changing the wording in
this section.” The law also stated that “it is the intent of the
Legislature that a court interpret this section ... in a manner
consistent with the interpretation of this section as it read
prior to Jan. 1, 2013.” [Civil Code Section 43.92(c) and(d)]
Duty to Warn and Protect
Unless the patient has communicated to the
psychotherapist a serious threat of physical violence
against a reasonably identifiable victim or victims, a
psychotherapist (as defined in Evidence Code Section
1010 below) is not liable for:
1. Failing to protect from a patient’s threatened violent
behavior, or
2. Failing to protect from a patient’s violent behavior.
NOTE: A 2004 decision by the California Court of Appeal
expands the duty to warn under the law described in
this part of the manual. In Ewing v. Goldstein, 120 Cal.
App.4th 807 (2d Dist. 2004), the Court of Appeal ruled that
under Civil Code Section 43.92, a psychotherapist has a
duty to warn of a patient’s threat even if the patient never
communicated the threat directly to the psychotherapist,
as long as the patient’s threat was communicated to
the psychotherapist by a member of the patient’s family.
This ruling that a duty to warn may arise based on
communications to the psychotherapist by someone other
than the patient creates a duty to warn that exceeds the
literal language of Section 43.92. Psychotherapists should
consider what action they need to take in light of this
decision and consider whether to consult with their legal
counsel. Providers should review any documents (including
policies or forms) they use to inform patients about the
limits of confidentiality.
Satisfying the Duty
If there is a duty to warn and protect under the limited
circumstances specified above, the law states that the duty
is discharged by the psychotherapist making reasonable
efforts to communicate the threat to both the victim or
victims and a law enforcement agency. A psychotherapist
may also discharge the duty by taking other reasonable
measures, depending on the circumstances of the situation.
Placing the patient on an involuntary hold under Welfare
and Institutions Code Section 5150 might be a reasonable
measure also.
Definition of Psychotherapist
“Psychotherapist” is defined for purposes of this law in
Evidence Code Section 1010, subdivisions (a) to (p), to
mean a person who is, or is reasonably believed by the
patient to be:
1. A person authorized to practice medicine in any state
or nation who devotes, or is reasonably believed by
the patient to devote, a substantial portion of his or her
time to the practice of psychiatry.
2. A licensed psychologist.
3. A licensed clinical social worker, when he or she is
engaged in applied psychotherapy of a nonmedical
nature.
4. A credentialed school psychologist.
5. A licensed marriage and family therapist.
6. A person registered as a psychological assistant who
is under the supervision of a licensed psychologist or
board certified psychiatrist as required by Business
and Professions Code Section 2913, or a person
registered as an associate marriage and family
therapist who is under the supervision of a licensed
marriage and family therapist, licensed clinical social
worker, licensed psychologist, licensed professional
clinical counselor, or licensed physician certified in
psychiatry, as specified in Business and Professions
Code Section 4980.44.
7. A person registered as an associate clinical social
worker who is under supervision as specified in
Business and Professions Code Section 4996.23.
8. A person registered with the Board of Psychology
as a registered psychologist and who is under the
supervision of a licensed psychologist or board
certified psychiatrist.
9. A psychological intern as defined in Business and
Professions Code Section 2911 who is under the

Chapter 7 — Reporting Assaults, Potentially Dangerous Patients and Firearms Prohibitions CHA
7.35
©CALIFORNIA HOSPITAL ASSOCIATION
supervision of a licensed psychologist or board
certified psychiatrist.
10. A trainee, as defined in Business and Professions
Code Section 4980.03(c), who is fulfilling his or her
supervised practicum required by Business and
Professions Code Section 4980.36(d) or 4980.37(c)
and is supervised by a licensed psychologist, a board
certified psychiatrist, licensed clinical social worker, a
licensed marriage and family therapist, or a licensed
professional clinical counselor.
11. A California licensed registered nurse who possesses
a master’s degree in psychiatric-mental health nursing
and is listed as a psychiatric-mental health nurse by
the Board of Registered Nursing.
12. An advanced practice registered nurse who is
certified as a clinical nurse specialist pursuant to
Business and Professions Code Section 2838 et
seq. and who participates in expert clinical practice in
psychiatric-mental health nursing.
13. A person providing outpatient mental health treatment
or counseling services to minors as authorized by
Family Code Section 6924. This includes psychiatrists,
psychologists, social workers, and marriage and
family therapists, as well as services provided by a
governmental agency, an entity having a contract with
a governmental agency to provide the services, a
runaway house, or a crisis resolution center.
14. A person licensed as a professional clinical counselor
under Business and Professions Code Section
4999.10 et seq.
15. A person registered as an associate professional
clinical counselor who is under the supervision of a
licensed professional clinical counselor, a licensed
marriage and family therapist, a licensed clinical social
worker, a licensed psychologist, or a licensed physician
and surgeon certified in psychiatry, as specified in
Business and Professions Code Sections 4999.42 to
4999.48.
16. A clinical counselor trainee, as defined in Business
and Professions Code Section 4999.12(g), who is
fulfilling his or her supervised practicum required by
Business and Professions Code Section 4999.32(c)
(3) or 4999.33(c)(3), and is supervised by a licensed
psychologist, a board certified psychiatrist, a licensed
clinical social worker, a licensed marriage and family
therapist, or a licensed professional clinical counselor.
IMMUNITY FOR PSYCHOTHERAPISTS AND OTHERS
As indicated in chapter 3, Welfare and Institutions Code
Sections 5154, 5173, 5259.3, 5267 and 5270.50 provide
immunity to various persons involved in the treatment,
evaluation and certification of involuntary mental health
patients, including the professional in charge of a
facility, the medical director and the psychiatrist directly
responsible for the patient’s treatment, provided that
certain conditions are met. This immunity may apply even
where a psychiatrist fails to carry out his or her obligation
under Tarasoff to warn or otherwise protect the foreseeable
victim of an involuntary patient’s violent tendencies [Lowe
v. County of San Diego, 183 Cal.App.3d 515 (1986), cert.
den.; Karash v. San Diego, 480 U.S. 946 (1987)].
D. Documenting Decisions
In order to carry out the duty to warn and to notify law
enforcement, the psychotherapist must strike a careful
balance between protecting the patient’s confidentiality and
protecting the potential victim. Initially, the psychotherapist
should gather relevant information about the patient,
including the patient’s past treatment. The therapist’s
decision about whether it is likely that the patient will carry
out his or her threats, or that the patient presents a danger
to another person, should be documented along with
the information that led to the decision. This will provide
important protection against claims that the therapist
should not have released information to law enforcement
and/or the potential victim (if a warning/notification is
given) or that the therapist did not carry out his or her duty
to warn the potential victim or notify law enforcement (if
a warning/notification is not given). If a warning is given,
the therapist should disclose only the information that is
necessary to enable the potential victim to recognize the
seriousness of the threat and take proper precautions to
protect himself or herself. A general indication to a person
that perhaps the person should avoid the patient may not
be a sufficient warning. Also, depending upon the patient’s
therapeutic condition and possible reaction, it may be
advisable to inform the patient that the warning will be
given. However, the law does not require that the patient be
so informed.
Situations in which a psychotherapist may have a duty
to warn a potential victim or notify law enforcement
often involve difficult decisions, and hospitals
and psychotherapists should seek legal advice in
specific situations.

CHA Mental Health Law Manual 2019
7.36
©CALIFORNIA HOSPITAL ASSOCIATION
X. NOTIFYING LAW ENFORCEMENT OFFICERS
OF PATIENT PRESENCE, RELEASE OR
DISAPPEARANCE
As a general rule, a hospital may not disclose
patient-identifiable information to law enforcement officers
without the written authorization of the patient, unless a
special exception to the law applies. These exceptions
and required reporting of patient presence, release
or disappearance are described in H.“Notifying Law
Enforcement Officers of Patient Presence, Release or
Disappearance,” page6.x.
XI. PATIENTS PROHIBITED FROM POSSESSING
FIREARMS OR OTHER DEADLY WEAPONS
State law prohibits certain psychiatric patients and former
psychiatric patients from possessing or purchasing firearms
and other deadly weapons. Allowing these persons to
possess or purchase firearms or other deadly weapons
is also illegal. In order to implement these laws, facilities
that provide psychiatric treatment are required to make
the reports discussed in C.“Reporting Requirements,”
page7.37. [Welfare and Institutions Code Sections
8100-8108]
A. Prohibition Against Possessing or Purchasing
a Firearm or Other Deadly Weapon
The persons described in B.“Persons Subject to the
Prohibition,” page7.36, are not permitted to possess,
control, purchase, receive, or attempt to purchase or
receive, any firearm or other deadly weapon.
Besides firearms, “deadly weapon” includes certain types
of ammunition, knives, explosives, clubs, and martial arts
weapons (see Penal Code Section 16590). Facilities should
consult their legal counsel if in doubt about whether a
particular article comes within the definition of a deadly
weapon. (See also Penal Code Sections 16430 and
16520.)
A person who knowingly supplies, sells, gives or allows
possession of a firearm by a person described below
will be incarcerated in the state prison for two to four
years. A person who knowingly supplies, sells, gives or
allows possession of another deadly weapon by a person
described below is subject to incarceration for one year or
less and/or fine.
If a person described below is found to have in his or
her possession a firearm or other deadly weapon, the
weapon must be confiscated by a law enforcement agency
or peace officer [Welfare and Institutions Code Section
8102(a)].
B. Persons Subject to the Prohibition
The following persons are subject to the prohibition against
possessing or purchasing a firearm or other deadly weapon
for the time period specified:
1. A person taken into custody, assessed and admitted
to a designated facility under Welfare and Institutions
Code Sections 5150-5152 because that person is a
danger to self or others (not gravely disabled). The
prohibition is effective for five years from the date
of discharge [Welfare and Institutions Code Section
8103(f)].
2. A person certified for intensive treatment under Welfare
and Institutions Code Sections 5250, 5260 or 5270.15.
The prohibition is effective for five years from the date
of discharge [Welfare and Institutions Code Section
8103(g)].
3. A person undergoing inpatient treatment, whether on
a voluntary or involuntary basis, who is a danger to
self or others. The prohibition ends once the patient is
discharged from the facility. [Welfare and Institutions
Code Section 8100(a) and (d)] The attending health
professional primarily responsible for the patient’s
treatment should document the determination that
the patient has a mental health disorder and probable
cause exists to believe he or she is a danger to self
or others. With respect to voluntary patients, “danger
to self” means a voluntary patient who has made a
serious threat of, or attempted, suicide with the use
of a firearm or other deadly weapon [Welfare and
Institutions Code Section 8100(f)].
4. A person who communicates to a licensed
psychotherapist a serious threat of physical violence
against a reasonably identifiable victim or victims, and
the psychotherapist reports this threat to the local
law enforcement agency. For purposes of this law,
“psychotherapist” is defined in Evidence Code Section
1010, subdivisions (a) through (e), inclusive, as a
person who is, or is reasonably believed by the patient
to be:
a. A person authorized to practice medicine in any
state or nation who devotes, or is reasonably
believed by the patient to devote, a substantial
portion of his or her time to the practice
of psychiatry.
b. A licensed psychologist.
c. A licensed clinical social worker, when he or
she is engaged in applied psychotherapy of a
nonmedical nature.

Chapter 7 — Reporting Assaults, Potentially Dangerous Patients and Firearms Prohibitions CHA
7.37
©CALIFORNIA HOSPITAL ASSOCIATION
d. A credentialed school psychologist.
e. A licensed marriage and family therapist.
The prohibition ends five years after the date of the
report. [Welfare and Institutions Code Section 8100(b)]
5. A person who has been adjudicated by a court of any
state to be a mentally disordered sex offender or a
danger to others as a result of a mental disorder or
mental illness. The prohibition is of indefinite duration.
[Welfare and Institutions Code Section 8103(a)]
6. A person who has been found not guilty of certain
crimes by reason of insanity, or mentally incompetent
to stand trial. (Facilities should consult their legal
counsel if in doubt about whether a particular crime
falls within this law.) The prohibition is of indefinite
duration. [Welfare and Institutions Code Section
8103(b), (c) and (d)]
7. A person who has been placed under conservatorship
by a court pursuant to Welfare and Institutions Code
Section 5350 or the law of any other state because
the person is gravely disabled as a result of a mental
health disorder or impairment by chronic alcoholism, if
the court determined that possession of a firearm or
other deadly weapon would present a danger to the
patient or to others. The prohibition ends when the
conservatorship ends. [Welfare and Institutions Code
Section 8103(e)]
Some of the persons listed above may gain the right to
possess or purchase a firearm by obtaining a court order
to this effect. Facilities should consult their legal counsel if
in doubt about whether a particular patient has the right to
possess a firearm.
C. Reporting Requirements
Facilities must make reports to the California Department
of Justice (DOJ), as described below. The law does not
require facilities to notify patients that the reports described
below have been made.
REPORTING TO CALIFORNIA DEPARTMENT OF
JUSTICE
Initial Reporting
California law requires hospitals to report electronically to
DOJ information DOJ deems necessary to identify those
persons described in paragraphs 1., 2., 3. above. (Persons
described in paragraphs 4.-7. are reported to DOJ by local
law enforcement or by the courts.) The facility must report
within 24 hours of admission. Information about online
reporting may be obtained by calling the California DOJ at
(916) 227-7550.
A copy of the completed online form should be printed and
retained by the hospital. Facilities will be reimbursed by the
California DOJ for submitting reports at a rate of 50 cents
per report. Facilities must submit a quarterly invoice to DOJ.
Reporting at Time of Discharge
Facilities must report to DOJ the discharge of persons
described in paragraph 1. or 2. of B.“Persons Subject to
the Prohibition,” page7.36. However, discharge reports
are not to be made for persons who are discharged within
31 days after admission [Welfare and Institutions Code
Section 8103(h)].
REPORTING TO CONFISCATING LAW ENFORCEMENT
AGENCY
If a patient was detained or apprehended for examination
of his or her mental condition, or is a person described in
B.“Persons Subject to the Prohibition,” page7.36, and
has had a weapon or weapons confiscated pursuant to
Welfare and Institutions Code Section 8102, health facility
personnel must notify the confiscating law enforcement
agency upon release of the patient. “Notice to Law
Enforcement Agency: Release of Person From Whom A
Firearm or Other Deadly Weapon Was Confiscated” (CHA
Form 13-4) can be used for this purpose. A copy of this
form should be retained by the hospital. [Welfare and
Institutions Code Section 8102(b)]
D. Patient Notification Obligations
NOTICE TO PATIENT
Prior to, or concurrent with, the discharge of a person
described in paragraph 1. or 2. of B.“Persons Subject
to the Prohibition,” page7.36, the facility must inform
that person that he or she is prohibited from owning,
possessing, controlling, receiving, or purchasing any
firearm or other dangerous weapon for five years after
discharge. The facility must also tell the patient that he or
she may request a court hearing for an order permitting
the patient to own, possess, control, receive, or purchase
a firearm. The facility should have each such patient sign a
form stating that he or she received this information. The
California DOJ has developed a form for this purpose,
“Patient Notification of Firearms Prohibition and Right to
Hearing Form” (BOF 4009B). (This form may be ordered
from the California DOJ at the phone number given above.)

CHA Mental Health Law Manual 2019
7.38
©CALIFORNIA HOSPITAL ASSOCIATION
A copy of the signed form should be given to the patient;
the original should be retained by the hospital. If the person
requests a hearing at the time of discharge, the facility must
forward the form to the superior court, unless the person
states that he or she will submit the form. [Welfare and
Institutions Code Section 8103]
PROCEDURE FOR RETURN OF WEAPON
If a patient was detained or apprehended for examination
of his or her mental condition or was a person described
in B.“Persons Subject to the Prohibition,” page7.36, and
had a weapon confiscated by a law enforcement agency,
the hospital must notify the patient of the procedure for the
return of the weapon. When the patient is released, the
facility should have the patient sign a form stating that he
or she received this information. A form for this purpose,
“Notice to Patient: Procedure for Return of Confiscated
Weapon(s)” (CHA Form 13-5), is included at the end of
this manual. A copy of the signed form should be given to
the patient; the original should be retained by the hospital
[Welfare and Institutions Code Section 8102(b)].
E. Confidentiality Considerations
State and federal health information privacy laws permit
health facilities and practitioners to make reports that are
required by law [45 C.F.R. Section 164.512(a); Civil Code
Section 56.10(c)(14); see also 65 Ops. Cal. Atty. Gen. 345
(1982)].
Reports submitted to the DOJ regarding patients described
in paragraphs 1. and 2. under B.“Persons Subject to
the Prohibition,” page7.36, are confidential and may be
used only for court proceedings and by DOJ to determine
a patient’s eligibility to own, possess, control, receive, or
purchase a firearm [Welfare and Institutions Code Section
8103(f)(2)(A) and g(2)(A)]. Hospitals should retain copies of
reports made, but should consider keeping them separate
from the medical record or in a separate portion of the
medical record to prevent routine copying and disclosure
for purposes not related to the criminal justice system, and
to prevent improper release to unauthorized persons.
F. Immunity From Liability
Mental health facilities and treating health professionals are
immune from civil liability for making a report required or
authorized in the law [Welfare and Institutions Code Section
8108].

Chapter 8 — Contents
©CALIFORNIA HOSPITAL ASSOCIATION
8 Adverse Events and Incident Reports
I. INTRODUCTION ....................................... 8.1
II. LEGAL ASPECTS OF INTERNAL INCIDENT
AND QUALITY REPORTING
....................... 8.1
A. Incident Reports ............................................8.1
B. Medical Staff Quality Assurance Reports ...8.1
C. Coordinating Incident and Quality
Assurance Reporting
....................................8.2
D. Patient Safety Organizations ........................8.2
E. Considerations in Developing the
Internal Reporting Process
...........................8.2
III. PREPARING CONFIDENTIAL INCIDENT
REPORTS ................................................ 8.3
A. General Principle ...........................................8.3
B. Maintaining the Privilege ..............................8.3
Disclosure to CDPH ..........................................8.3
C. Documenting Incident in the Medical
Record
...........................................................8.4
IV. REQUIRED PATIENT SAFETY PLAN ........... 8.4
A. Written Plan....................................................8.4
B. Patient Safety Committee ............................. 8.5
C. Patient Safety Event Definition ..................... 8.5
V. THE JOINT COMMISSION
REQUIREMENTS
...................................... 8.5
A. Sentinel Events ..............................................8.5
B. Periodic Performance Review ......................8.6
VI. NOTIFYING THE PATIENT OR FAMILY ........ 8.6
A. Outcomes of Care .........................................8.7
B. Statements of Sympathy/Apologies ............8.7
VII. CDPH ADVERSE EVENTS REPORTING ....... 8.7
A. Types of Events That Must be Reported .....8.7
Surgical Events ................................................. 8.8
Product or Device Events
..................................8.8
Patient Protection Events
.................................. 8.8
Care Management Events
................................. 8.8
Environmental Events
........................................8.9
Criminal Events
................................................. 8.9
Final Item
..........................................................8.9
B. Required Time Frame for Reporting ............8.9
C. How to Report ................................................ 8.9
D. Communication With Affected Patient(s) ....8.9
E. Relationship With Other Reporting
Requirements.................................................8.9
F. CDPH Investigations and Reports .............8.10
Ongoing Threat of Imminent Danger ................8.10
No Threat of Imminent Danger
........................8.10
Definition
........................................................8.10
Follow-Up
.......................................................8.10
CDPH Public Reporting of Adverse Events
...... 8.10
G. Penalties for Failure to Report ...................8.10
VIII. MEDICATION ERRORS .......................... 8.11
IX. REPORTS UNDER THE SAFE MEDICAL
DEVICES ACT OF 1990 .......................... 8.11
A. When and To Whom Reports of
Adverse Events Must be Made
...................8.11
Individual Reports ...........................................8.11
Annual Reports
............................................... 8.11
Where to Submit Reports
................................8.12
Definitions
.......................................................8.12
Forms to be Used
........................................... 8.12
Questions
....................................................... 8.12
Disclaimers
..................................................... 8.13
B. Restraints .....................................................8.13
C. Required Policies and Procedures ............8.13
Required Documentation ................................8.13
D. Request From FDA for Additional
Information
..................................................8.13

Chapter 8 — Contents
©CALIFORNIA HOSPITAL ASSOCIATION
CHA Mental Health Law Manual 2019
FORMS & APPENDICES
20-1 Adverse Event Report Form — Sample
21-1 Incident Report
21-2 Report to Attorney
Forms and Appendices can be found at the back of the manual and
online for CHA members at www.calhospital.org/free-resources.
“S” denotes that the form is provided in English and Spanish.
E. Device Tracking ...........................................8.13
Patient Confidentiality Rights ...........................8.14
Device Tracking Records
.................................8.14
X. REPORTING REQUIREMENTS RELATED
TO RESTRAINT OR SECLUSION
.............. 8.14
XI. REPORTABLE “UNUSUAL
OCCURRENCES”
................................... 8.14

8 Adverse Events and Incident Reports
8.1
©CALIFORNIA HOSPITAL ASSOCIATION
I. INTRODUCTION
This chapter describes the legal issues involved in
establishing incident report and quality improvement
systems that protect the sensitive information generated
from subpoena or other discovery attempts in a lawsuit
against the hospital. This chapter also describes the legal
and accreditation requirements for notifying patients of
adverse events, implementing patient safety plans, and
reporting adverse events to government agencies.
II. LEGAL ASPECTS OF INTERNAL INCIDENT
AND QUALITY REPORTING
Appropriate reporting of incidents within a facility is
important for many reasons. First, the proper personnel
within the hospital must be alerted to the fact that an
incident has occurred so that they may immediately act
to mitigate any potential negative effects of the incident.
In addition, appropriate personnel must investigate the
incident when memories and evidence are fresh, and then
take the necessary steps to revise systems, policies and
procedures as appropriate to improve quality.
The California Legislature has recognized that incident
reporting and related quality improvement activities
require a level of confidence on the part of hospital staff
that the documents and information they create will
not be used against them in litigation. Accordingly, the
California Legislature has adopted two legal protections
from discovery by plaintiffs’ lawyers for certain documents
and other information. These legal protections, the
attorney-client privilege and the peer review protection from
discovery, are discussed below. In addition, the United
States Congress has adopted protections described in
D.“Patient Safety Organizations,”page8.2.
It is always the obligation of the entity claiming the benefit
of a nondisclosure privilege to show that the privileges
and protections apply in that particular instance. The
legal issues governing the confidentiality of the reports
discussed in this chapter are complex, and intended
confidentiality is easily thwarted by inadvertent uses or
disclosures of the reports. Few areas of health care are as
rife with misconceptions as to the circumstances under
which the law provides protection. Because of this, it is
extremely important for providers to seek legal assistance
in the design of their reporting systems and legal review of
any modifications made to them.
A. Incident Reports
Many hospitals have used the traditional incident report
system whereby an “Incident Report” (CHA Form 21-1)
or similar form of report is prepared by nursing staff or
other hospital personnel with the intent that the report will
remain confidential and be transmitted to the hospital’s
attorney (perhaps through its insurance carrier) for use in
litigation that might arise out of an incident. One purpose
of the incident report is to alert the hospital attorney to
potential claims. Another is to document the facts and
circumstances of the incident in a record that is created
at the time the incident occurs. If properly prepared and
maintained, incident reports may be protected from
discovery by the attorney-client privilege. This means that
persons suing the hospital would not be able to obtain the
documents, even by use of a subpoena. The procedure for
preparing the reports and preserving their confidentiality
is discussed in III.“Preparing Confidential Incident
Reports,”page8.3. As noted above, legal counsel should
be consulted regarding the design and implementation of
an incident reporting system.
B. Medical Staff Quality Assurance Reports
An alternative or supplement to the incident report system
is a quality assurance reporting system operated through
the medical staff quality assurance process. Under
this approach, reports describing incidents potentially
affecting the quality of patient care are transmitted to the
medical staff committee that has responsibility for the
hospital’s quality assurance program, usually through
the hospital’s quality assurance coordinator. This report,
unlike the incident report, is not prepared for the hospital’s
attorney for use in litigation, and therefore does not claim
protection under the attorney-client privilege. It is, however,
prepared for the medical staff committee responsible
for quality assurance. As such, the report is intended

CHA Mental Health Law Manual 2019
8.2
©CALIFORNIA HOSPITAL ASSOCIATION
to constitute a medical staff committee document and
to qualify for protection from discovery under the “peer
review” confidentiality of Evidence Code Section 1157 (if
properly prepared and maintained). The goal here is the
same as with the incident report — i.e., to protect the
document from compelled disclosure. Although there are
some exceptions to the confidentiality of Evidence Code
Section 1157, it protects against compelled disclosure
in malpractice and most other private civil actions. (See,
however, Arnett v. Dal Cielo, 14 Cal.4th 4 (1996) regarding
the exception to Evidence Code Section 1157 protection
for administrative investigative subpoenas used in
connection with government investigations.)
As with the incident report, the details of the system
through which the report is completed and distributed are
important. It is particularly important to show an acceptable
connection between the reporting process and the medical
staff committee structure.
C. Coordinating Incident and Quality Assurance
Reporting
It is possible for the quality assurance reporting system
to tie into the incident reporting system. To do this, the
coordinator who is responsible for receiving the quality
assurance report completes, when appropriate, a “Report
to Attorney” form (CHA Form 21-2) or similar report form.
Like the incident report, the “Report to Attorney” form is
transmitted to the hospital’s attorney (perhaps through its
insurance carrier) for use in litigation that might arise out of
an incident. The “Report to Attorney” form is intended to
be protected by the attorney-client privilege in the same
manner as the incident report. It bears repeating that since
the privileges and protections involved are somewhat
technical in nature, hospital legal counsel should be
consulted regarding the structure and implementation of
such a system.
D. Patient Safety Organizations
A hospital may participate in a Patient Safety Organization
(PSO) and develop a Patient Safety Evaluation System
(PSES). Data, reports, records, memoranda, analyses, and
other information developed as part of a PSES may be
considered patient safety work product (PSWP) under the
Patient Safety and Quality Improvement Act of 2005. PSWP
is protected from discovery or access by subpoena, court
order, administrative order, inspection processes and other
demands for access.
A complete discussion of PSOs, including the confidentiality
of PSWP, is included in CHA’s California Hospital
Compliance Manual.
E. Considerations in Developing the Internal
Reporting Process
A medical staff quality assurance reporting system that
is protected by Evidence Code Section 1157 should be
designed to achieve the goals of improving the quality of
care, correcting problems and protecting patients, whereas
the incident reporting process that is protected by the
attorney-client privilege should be designed to gather the
information that will be needed to defend against liability
claims.
The medical staff quality assurance system should be
designed so that the practitioners involved in any incident
that is reported will be given appropriate feedback about
the findings from the review and the aspects of any plan of
correction that is developed that will affect them in future
cases. This feedback should be given routinely when
the concerns are identified rather than accumulated in
a confidential file that is disclosed only in the context of
a hearing on disciplinary action. Care must be taken to
balance the confidentiality of the person submitting the
report with the need to know sufficient details regarding the
report to allow for a meaningful response.
It is also appropriate to plan for feedback to staff who
submit reports, so the health care professionals may
work cooperatively to improve care. Although it would be
inappropriate to disclose information about disciplinary
warnings or actions issued to any individual (medical staff
member, nurse or other member of the health care team), it
is appropriate to convey information about deficiencies that
were identified and the plan of correction to avoid future
deficiencies, and to encourage the staff to work together to
implement the plan of correction.
The peer review protections will allow the disclosure of
information in the course of a quality assurance and peer
review process that requires identification of issues and
development of plans of correction. They also will allow
disclosures of the information for the purpose of improving
care provided by nonmedical staff members. For example,
the information may be used to redesign a pharmacy
medication order protocol for a certain drug or for planning
a nurse education course in a particular subject such
as administration and monitoring of Pitocin during labor.
These alternate uses are fully protected as long as the
system is subject to the medical staff committee oversight.
As is noted above, care must be taken in designing the
programs to take advantage of the protections from
discovery that are available. A hospital-wide quality
assurance plan that has no medical staff committee
oversight or participation will not meet the requirements
for the protection from discovery that is available for the

Chapter 8 — Adverse Events and Incident Reports CHA
8.3
©CALIFORNIA HOSPITAL ASSOCIATION
records and proceedings of medical staff committees
having the responsibility for evaluating and improving the
quality of care. However, a multidisciplinary process that
includes nonphysicians as well as medical staff members
can be fully protected when that process provides for the
proper medical staff committee oversight.
III. PREPARING CONFIDENTIAL INCIDENT
REPORTS
A. General Principle
California courts have held that incident reports may be
regarded as confidential attorney-client communications
if the hospital can show that the purpose and intent of the
reports is to provide a confidential communication between
the hospital and its attorney, even if they are communicated
through the hospital’s insurance carrier [Sierra Vista
Hospital v. Superior Court, 248 Cal.App.2d 359 (1967)]. In
the Sierra Vista case, the hospital was able to show that:
1. The employee who prepared the report knew it was
intended to be made as a confidential communication
to the hospital’s attorney;
2. The report form itself stated that it was confidential
and not to be made part of the patient’s medical
record; and
3. The hospital retained no copies of the form at the
hospital, and did not give a copy to the medical staff or
anyone else.
The holding of the Sierra Vista case was reaffirmed in
the decision in Scripps Health v. Superior Court, 109 Cal.
App.4th 529 (4th Dist. 2003). The Scripps Health case is
notable for hospitals and systems that collect such reports
for use by in-house counsel since the incident reports in
this case were prepared for the health system’s in-house
attorney who used them for the system’s self-insurance,
risk management and quality assurance programs, as
directed by the legal department.
B. Maintaining the Privilege
Privileges may be lost by disclosure of the privileged
material. In order to prevent any inadvertent disclosure of
incident reports, appropriate physical and/or electronic
security measures must be maintained. No copy of the
report should be included in the patient’s medical record
nor should a copy be reviewed or signed by the attending
physician or any other member of the medical staff.
If a report must be made to CDPH or The Joint
Commission, a separate document containing only that
information which must be reported should be submitted.
(See VII.“CDPH Adverse Events Reporting,”page8.7,
for adverse event reports that must be made to CDPH.
See V.“The Joint Commission Requirements,”page8.5
for more information about reporting to The Joint
Commission.)
DISCLOSURE TO CDPH
Peer Review Documents
CDPH and CMS take the position that they are legally
entitled to access peer review information, even if it is
protected from discovery during court proceedings by the
California Evidence Code. There is some legal support for
this position, as CDPH and CMS must assess whether
the hospital is complying with regulations governing the
medical staff, the hospital governing body, and quality
assurance. CMS, in particular, reminds hospitals that as
a federal government agency it need not recognize this
state law. Information that is protected from discovery
under Evidence Code 1157 may remain protected even if
it is disclosed to CDPH in the course of an investigation
by CDPH [Fox v. Kramer, 22 Cal.4th 531 (2000)]. If CMS
or CDPH requests peer review information protected
by Evidence Code Section 1157 during a survey, the
hospital should clearly indicate every report, document
and interview that is entitled to 1157 protection, ask
the surveyors to note this in their records and reports,
and inform them that the hospital intends to assert the
applicability of peer review protection. Generally, the
surveyors will not copy these documents.
Attorney-Client Privileged Documents
CDPH and CMS do not assert that they are entitled
to access documents protected by the attorney-client
privilege. California courts have held that incident
reports may be regarded as confidential attorney-client
communications if the hospital can show that the purpose
and intent of the reports is to provide a confidential
communication between the hospital and its attorney.
Patient Safety Work Product Documents
The Patient Safety and Quality Improvement Act (PSQIA)
of 2005 was enacted to facilitate and accelerate
improvements in health care quality and patient safety. The
law encourages the voluntary and confidential reporting of
events that may adversely affect patients to Patient Safety
Organizations (PSOs). PSOs then aggregate and analyze

CHA Mental Health Law Manual 2019
8.4
©CALIFORNIA HOSPITAL ASSOCIATION
the data to identify and better understand underlying
causes of risks or ham, and share those findings back to
participating providers.
The PSQIA alleviates health care providers’ fears that trial
lawyers, government agencies, or others might obtain
and misuse information about these events by providing
federal legal confidentiality protections to the information
that is assembled and reported by providers to a PSO. The
confidentiality protections preempt any state or local law
that allows or requires disclosure of information defined
as “patient safety work product.” Thus, surveyors should
not ask hospitals for access to patient safety work product
documents, and hospitals should not provide access to
these documents. This applies whether the surveyors are
conducting a state survey or a federal survey.
“Patient safety work product” means any data, reports,
records, memoranda, analyses (such as root cause
analyses), or written or oral statements (or copies of any of
this material):
1. Which could improve patient safety, health care quality,
or health care outcomes; and
a. Which are assembled or developed by a provider
for reporting to a PSO and are reported to a PSO,
which includes information that is documented
as within a patient safety evaluation system for
reporting to a PSO, and such documentation
includes the date the information entered the
patient safety evaluation system; or
b. Are developed by a PSO for the conduct of patient
safety activities; or
2. Which identify or constitute the deliberations or
analysis of, or identify the fact of reporting pursuant to,
a patient safety evaluation system.
However, patient safety work product does not include a
patient’s medical record, billing and discharge information,
or any other original patient or provider information; nor
does it include information that is collected, maintained, or
developed separately, or exists separately, from a patient
safety evaluation system. Such separate information or a
copy thereof reported to a PSO shall not by reason of its
reporting be considered patient safety work product.
A complete discussion of PSOs, including the confidentiality
of PSWP, is included in CHA’s California Hospital
Compliance Manual. Hospitals with questions about which
documents may or may not be released to surveyors
pursuant to the PSQIA should consult legal counsel.
C. Documenting Incident in the Medical Record
While a copy of the incident report or PSWP itself should
not be included in the patient’s medical record or reviewed
by the attending physician, this prohibition should not be
construed as a recommendation that the patient’s medical
record contain no information relating to an incident that
affects the patient or the patient’s care. The occurrence
of any such incident and its effect on the patient can and
must be included in the medical record for the use of the
attending physician in properly treating the patient as a
result of the occurrence. Such information should, however,
be recorded separately in the medical record and not be
recorded simply by inserting a copy of the incident report in
the record.
The incident report and/or PSWP contain additional,
more detailed information which is not necessary to the
continued treatment of the patient and which should
not be included in the patient’s medical record; it is this
more detailed information that is intended to be protected
from discovery.
Likewise, no documentation should be put in the medical
record regarding notification of risk management or
consultation with legal counsel.
IV. REQUIRED PATIENT SAFETY PLAN
California law requires general acute care hospitals, acute
psychiatric hospitals, and special hospitals to develop,
implement, and comply with a patient safety plan for the
purpose of improving the health and safety of patients and
reducing preventable patient safety events [Health and
Safety Code Sections 1279.6 and 1279.7].
A. Written Plan
The patient safety plan must be developed by the
hospital, in consultation with the hospital’s various health
care professionals. The plan must provide for at least
the following:
1. A patient safety committee or equivalent committee in
composition and function. The responsibilities of the
committee are described below.
2. A reporting system for patient safety events that allows
anyone involved, including, but not limited to, health
care practitioners, hospital employees, patients, and
visitors, to make a report of a patient safety event to
the hospital. Hospitals should work with their legal
counsel to integrate this reporting system with the
hospital’s incident reporting system and the medical

Chapter 8 — Adverse Events and Incident Reports CHA
8.5
©CALIFORNIA HOSPITAL ASSOCIATION
staff quality assurance report system, as appropriate.
Reports by non-hospital employees (patients and
visitors) are likely not covered by the attorney-client
privilege or Evidence Code Section 1157, although
discussions and reports generated by the patient
safety committee in response to reports by patients
and visitors may enjoy these protections if the
committee is organized and operated properly. In
addition, hospitals should also work with their legal
counsel to integrate reports by patients and visitors
into their grievance process as appropriate.
3. A process for a team of hospital staff to conduct
analyses, including, but not limited to, root cause
analyses of patient safety events. The team must be
composed of the hospital’s various categories of health
care professionals, with the appropriate competencies
to conduct the required analyses. Again, hospitals
should work with their legal counsel to organize the
team/committee and its operations so that its reports
and deliberations may enjoy the protections of the
attorney-client privilege and Evidence Code Section
1157 as described in this chapter.
4. A reporting process that supports and encourages a
culture of safety and reporting patient safety events.
5. A process for providing ongoing patient safety training
for hospital personnel and health care practitioners.
6. Measures to prevent adverse events associated with
misconnecting enteral feeding and epidural lines. The
requirement to include these measures in the patient
safety plan ended on July 1, 2016 for enteral feeding
connectors, and Jan. 1, 2017 for epidural connectors.
As of those dates, health facilities are prohibited from
using a connection that would fit into a connection
port other than the type it was intended for, unless
an emergency or urgent situation exists and the
prohibition would impair the ability to provide health
care. If a hospital is not able to purchase a sufficient
supply of compliant tubing connectors, the hospital
should address this issue in its patient safety plan
and describe the measures it is taking to manage the
noncompliant tubing connectors, including training.
7. A facility-wide hand hygiene program.
B. Patient Safety Committee
The committee must be composed of the hospital’s various
health care professionals, including, but not limited to,
physicians, nurses, pharmacists, and administrators. The
committee must do all of the following:
1. Review and approve the patient safety plan.
2. Receive and review reports of patient safety events.
3. Monitor implementation of corrective actions for patient
safety events.
4. Make recommendations to eliminate future patient
safety events.
5. Review and revise the patient safety plan at least once
a year, but more often if necessary, to evaluate and
update the plan, and to incorporate advancements in
patient safety practices.
Hospitals should work with their legal counsel to maximize
the likelihood that the reports and deliberations of this
committee qualify for the attorney-client privilege and the
peer review confidentiality protections of Evidence Code
Section 1157 as described in this chapter.
C. Patient Safety Event Definition
Patient safety events must be defined by the patient safety
plan and must include, but not be limited to:
1. All adverse events or potential adverse events,
as described in Health and Safety Code
Section 1279.1 (see VII.“CDPH Adverse Events
Reporting,”page8.7), that are determined to be
preventable; and
2. Health care-associated infections, as defined in the
federal Centers for Disease Control and Prevention’s
National Healthcare Safety Network, or its successor,
that are determined to be preventable. CDPH may
instead accept the recommendation of the Healthcare
Associated Infection Advisory Committee, or its
successor.
Hospitals may wish to include “sentinel events” in the
definition of patient safety events (see A.“Sentinel
Events,”page8.5).
V. THE JOINT COMMISSION REQUIREMENTS
A. Sentinel Events
Under its policy on “sentinel events,” The Joint Commission
(TJC) asks hospitals to review all incidents that constitute
a sentinel event and, with some exceptions, to share with
TJC the results of this review (called a “root cause analysis”).
Hospitals are also expected to prepare action plans to
address any issues identified in the root cause analysis.
A “sentinel event” is defined as “an unexpected
occurrence involving death or serious physical or

CHA Mental Health Law Manual 2019
8.6
©CALIFORNIA HOSPITAL ASSOCIATION
psychological injury or the risk thereof. The phrase ‘or
risk thereof’ includes any process variation for which
a recurrence would carry a significant chance of a
serious adverse outcome.” (See The Joint Commission
Comprehensive Accreditation Manual for Hospitals,
glossary.)
Since a sentinel event, by definition, involves an event
that could lead to litigation, hospitals have reason to be
concerned regarding the confidentiality of the information
generated by the root cause analysis process. Many
hospitals have sought to conduct their root cause analysis
through a medical staff committee process that may be
protected under Evidence Code Section 1157. Others
have used attorney-directed investigations in order to
bring the information under the attorney-client privilege or
attorney-work product privilege. Once such confidentiality
protection is established, the concern becomes whether
disclosing this information to TJC may waive whatever
privilege or legal protection would otherwise apply to the
information.
TJC asks (but does not require) that hospitals report their
sentinel events to TJC and share their root cause analyses
and action plans with them as well. TJC is aware of the
concerns about loss of confidentiality with respect to the
root cause analyses if they are shared with TJC. As a result,
TJC has offered hospitals several alternatives for handling
sentinel events and the root cause analysis process. These
alternatives cover a range of options for sharing information
with TJC, including the option (“alternative 4”) not to share
any information at all. Information on these alternatives
can be found at www.jointcommission.org/se_Alternatives.
Decisions on how best to protect sentinel event reviews
should be made in consultation with legal counsel.
CDPH has stated that sentinel events should be reported
to CDPH as adverse events or unusual occurrences,
whichever is appropriate.
B. Periodic Performance Review
In addition to the sentinel event process, TJC requires
that accredited organizations conduct a self-assessment
through a process called Periodic Performance Review
(PPR). PPR requires accredited organizations to assess
themselves against applicable TJC standards, to develop
plans of action to address areas of noncompliance and
to identify measures of success to demonstrate that the
identified deficiencies have been addressed and resolved.
Under the full PPR process, all information developed
by accredited organizations to comply with PPR is to
be shared with TJC, which will use the information in
connection with the survey and accreditation process.
As with the sentinel event process, hospitals have decisions
to make as to how to conduct these self-assessments
and the extent to which they wish to protect the results of
such assessments from compelled disclosure (such as a
subpoena in a medical malpractice case) and from waiver
of confidentiality protection. To address industry concerns
regarding the possible loss of confidentiality protection for
data shared with it, TJC has followed the approach it has
used with regard to sentinel events and developed several
options for hospital compliance with PPR requirements that
involve disclosure of varying amounts of information. (See
discussion under A.“Sentinel Events,”page8.5.)
NOTE: In order to use any of the alternatives to full
participation in the full PPR, the accredited organization
must affirm that it has made its decision not to do the full
PPR only after careful consideration with legal counsel.
VI. NOTIFYING THE PATIENT OR FAMILY
State law requires that patients be informed of specified
reportable adverse events. In addition, The Joint
Commission requires that patients be informed of the
outcomes of care, including unanticipated outcomes.
In addition to these requirements, there is a growing
consensus that disclosure of medical mistakes is ethically
appropriate. However, these conversations can be
very difficult.
The state law adverse event requirement is discussed
under VII.“CDPH Adverse Events Reporting,”page8.7.
The Joint Commission requirement is described below.
This section of the manual also describes California law
that permits health care providers to express sympathy to
patients, or to apologize, without admitting liability.
Many organizations have done considerable work outlining
how best to approach patients and their families about
negative outcomes, whether they are the result of a medical
error or not. For example, the Agency for Healthcare
Research and Quality has published a toolkit to help
hospital leaders and clinicians communicate accurately and
openly with patients and families when something goes
wrong with their care. The toolkit, called “Communication
and Optimal Resolution (CANDOR),” may be found at
https://www.ahrq.gov/professionals/quality-patient-safety/
patient-safety-resources/resources/candor/introduction.
html.

Chapter 8 — Adverse Events and Incident Reports CHA
8.7
©CALIFORNIA HOSPITAL ASSOCIATION
A. Outcomes of Care
TJC requires that patients be informed of the outcomes
of care, including unanticipated outcomes (see The Joint
Commission Comprehensive Accreditation Manual for
Hospitals, RI.01.02.01, EP 20, 21, 22). According to this
standard, the hospital must provide the patient or surrogate
decision maker with the information about the outcomes
of care that the patient needs to participate in current and
future health care decisions.
The hospital must also inform the patient or surrogate
decision maker about unanticipated outcomes of care that
relate to sentinel events considered reviewable by TJC.
In addition, the licensed independent practitioner (usually
the physician) responsible for managing the patient’s
care, or his or her designee, must inform the patient about
unanticipated outcomes of care related to sentinel events
when the patient is not already aware of the occurrence or
when further discussion is needed.
B. Statements of Sympathy/Apologies
When discussing an unanticipated outcome or adverse
event, it is human nature to want to express sympathy
or sorrow. Sometimes people hesitate to express these
sentiments for fear they will be used against them in a
lawsuit. This fear is unwarranted. California law states that
the following is inadmissible as evidence of an admission
of liability in a civil or administrative action (such as a
malpractice lawsuit):
The portion of statements, writings, or benevolent
gestures expressing sympathy or a general sense of
benevolence relating to the pain, suffering or death of a
person involved in an accident and made to the person
or to the family of that person.
A statement of fault, however, is admissible.
“Accidents” include any occurrence not the result
of willful action. This includes medical errors and
alleged malpractice.
“Benevolent gestures” means actions that convey a
sense of compassion or commiseration emanating from
humane impulses.
“Family” means the spouse, parent, grandparent,
stepparent, child, grandchild, sibling, half-sibling or
spouse’s parent.
[Evidence Code Section 1160, Government Code Section
11440.45]
Hospitals may wish to keep this law in mind when
discussing unanticipated outcomes with patients.
VII. CDPH ADVERSE EVENTS REPORTING
In response to media attention on medical errors, the
California Legislature passed, and the Governor signed,
legislation requiring general acute care hospitals, acute
psychiatric hospitals, and special hospitals to report
specified adverse events to CDPH [Health and Safety Code
Sections 1279.1, 1279.2, 1279.3 and 1280.4]. Outpatient
settings must also report adverse events. “Outpatient
settings” are defined as:
1. Any facility, clinic, unlicensed clinic, center, office, or
other setting that is not part of a general acute care
facility, as defined in Health and Safety Code Section
1250, and where anesthesia, except local anesthesia or
peripheral nerve blocks, or both, is used in compliance
with the community standard of practice, in doses that,
when administered have the probability of placing a
patient at risk for loss of the patient’s life-preserving
protective reflexes. A clinic or ambulatory surgery
center that does not meet this definition — i.e., does
not use general anesthesia — is not subject to this
reporting requirement.
2. Facilities that offer in vitro fertilization, as defined in
Health and Safety Code Section 1374.55(b).
Outpatient settings do not include, among other
settings, any setting where anxiolytics and analgesics
are administered, when done so in compliance with the
community standard of practice, in doses that do not have
the probability of placing the patient at risk for loss of the
patient’s life-preserving protective reflexes.
[Health and Safety Code Sections 1248 and 1248.15]
CDPH has confirmed that distinct-part nursing facilities
(DP-NFs) need not report adverse events under this law.
However, other reporting requirements may apply (for
example, the “unusual occurrences” reporting requirement
may apply; see E.“Relationship With Other Reporting
Requirements,”page8.9).
A. Types of Events That Must be Reported
For purposes of this reporting requirement, “adverse
event” includes the surgical events, product or device
events, patient protection events, care management events,
environmental events, criminal events, and one other item
described below. The term “serious disability,” which is
used in many places in the list of adverse events, means:
a physical or mental impairment that substantially limits
one or more of the major life activities of an individual,
or the loss of bodily function, if the impairment or loss
lasts more than 7 days or is still present at the time of
discharge from an inpatient health facility, or the loss of
a body part.

CHA Mental Health Law Manual 2019
8.8
©CALIFORNIA HOSPITAL ASSOCIATION
The complete list of reportable adverse events is included
below. Many do not apply in the mental health setting, such
as the list of surgical events. However, many of them can
occur in a psychiatric hospital or in the psychiatric unit of
a general acute care hospital, so employees should be
familiar with the list. The list of adverse events includes
the following.
SURGICAL EVENTS
1. Surgery performed on a wrong body part that is
inconsistent with the documented informed consent for
that patient. This does not include a situation requiring
prompt action that occurs in the course of surgery or
a situation that is so urgent as to preclude obtaining
informed consent.
2. Surgery performed on the wrong patient.
3. The wrong surgical procedure performed on a patient,
which is a surgical procedure performed on a patient
that is inconsistent with the documented informed
consent for that patient. This does not include a
situation requiring prompt action that occurs in the
course of surgery, or a situation that is so urgent as to
preclude the obtaining of informed consent.
4. Retention of a foreign object in a patient after surgery
or other procedure, excluding objects intentionally
implanted as part of a planned intervention and objects
present prior to surgery that are intentionally retained.
5. Death during or up to 24 hours after induction of
anesthesia after surgery of a normal, healthy patient
who has no organic, physiologic, biochemical, or
psychiatric disturbance and for whom the pathologic
processes for which the operation is to be performed
are localized and do not entail a systemic disturbance.
PRODUCT OR DEVICE EVENTS
1. Patient death or serious disability associated with
the use of a contaminated drug, device, or biologic
provided by the health facility when the contamination
is the result of generally detectable contaminants in the
drug, device, or biologic, regardless of the source of
the contamination or the product.
2. Patient death or serious disability associated with the
use or function of a device in patient care in which the
device is used or functions other than as intended. For
purposes of this requirement, “device” includes, but
it not limited to, a catheter, drain, or other specialized
tube, infusion pump, or ventilator.
3. Patient death or serious disability associated with
intravascular air embolism that occurs while being
cared for in a facility, excluding deaths associated with
neurosurgical procedures known to present a high risk
of intravascular air embolism.
PATIENT PROTECTION EVENTS
1. An infant discharged to the wrong person.
2. Patient death or serious disability associated
with patient disappearance for more than four
hours, excluding events involving adults who have
competency or decision-making capacity.
3. A patient suicide or attempted suicide resulting in
serious disability while being cared for in a health
facility due to patient actions after admission to
the health facility, excluding deaths resulting from
self-inflicted injuries that were the reason for the
admission to the health facility.
CARE MANAGEMENT EVENTS
1. A patient death or serious disability associated with a
medication error, including, but not limited to, an error
involving the wrong drug, the wrong dose, the wrong
patient, the wrong time, the wrong rate, the wrong
preparation, or the wrong route of administration,
excluding reasonable differences in clinical judgment
on drug selection and dose.
2. A patient death or serious disability associated with
a hemolytic reaction due to the administration of
ABO-incompatible blood or blood products.
3. Maternal death or serious disability associated with
labor or delivery in a low-risk pregnancy while being
cared for in a facility, including events that occur
within 42 days postdelivery and excluding deaths from
pulmonary or amniotic fluid embolism, acute fatty liver
of pregnancy, or cardiomyopathy.
4. Patient death or serious disability directly related to
hypoglycemia, the onset of which occurs while the
patient is being cared for in a health facility.
5. Death or serious disability, including kernicterus,
associated with failure to identify and treat
hyperbilirubinemia in neonates during the first
28 days of life. For purposes of this requirement,
“hyperbilirubinemia” means bilirubin levels greater
than 30 milligrams per deciliter.
6. A Stage 3 or 4 ulcer, acquired after admission to a
health facility, excluding progression from Stage 2 to

Chapter 8 — Adverse Events and Incident Reports CHA
8.9
©CALIFORNIA HOSPITAL ASSOCIATION
Stage 3 if Stage 2 was recognized upon admission.
(See AFL 15-03.1 regarding unstageable pressure
ulcers, which may be found at https://www.cdph.
ca.gov/Programs/CHCQ/LCP/Pages/LNCAFL15.aspx.)
7. A patient death or serious disability due to spinal
manipulative therapy performed at the health facility.
ENVIRONMENTAL EVENTS
1. A patient death or serious disability associated with an
electric shock while being cared for in a health facility,
excluding events involving planned treatments, such as
electric countershock.
2. Any incident in which a line designated for oxygen
or other gas to be delivered to a patient contains the
wrong gas or is contaminated by a toxic substance.
3. A patient death or serious disability associated with
a burn incurred from any source while the patient is
being cared for in a health facility.
4. A patient death associated with a fall while the patient
is being cared for in a health facility.
5. A patient death or serious disability associated with the
use of restraints or bedrails while being cared for in a
health facility.
CRIMINAL EVENTS
1. Any instance of care ordered by or provided
by someone impersonating a physician, nurse,
pharmacist, or other licensed health care provider.
2. The abduction of a patient of any age.
3. The sexual assault of a patient within or on the grounds
of a health facility.
4. The death or significant injury of a patient or staff
member resulting from a physical assault that occurs
within or on the grounds of a facility.
FINAL ITEM
The list of adverse events specified in the law contains
a final item that contains a circular definition. The final
“catchall” category to be reported is “an adverse event or
series of adverse events that cause the death or serious
disability of a patient, personnel, or visitor.” However, an
“adverse event” is defined as those events listed in the
above sections (surgical events, product or device events,
patient protection events, care management events,
environmental events, and criminal events). Therefore,
the final category arguably does not capture any events
that are not already described in the law. Hospitals that
are considering reporting an event under the “catchall”
category should consult legal counsel to determine
whether a report under this law is required. Even if a report
under this law is determined not to be required, however,
hospitals may need to report the incident pursuant to
another reporting requirement. (See E.“Relationship With
Other Reporting Requirements,”page8.9.)
B. Required Time Frame for Reporting
The report must be made no later than five days after the
adverse event has been detected. However, if the adverse
event is an ongoing urgent or emergent threat to the
welfare, health, or safety of patients, personnel, or visitors,
the report must be made not later than 24 hours after the
adverse event has been detected.
C. How to Report
CDPH has developed a web-based reporting tool that
health care facilities may use to report adverse events, as
well as privacy breaches, called the “California Healthcare
Event and Reporting Tool” (CalHEART). Information about
the online reporting tool may be found in CDPH All Facility
Letter 13-12 at https://www.cdph.ca.gov/Programs/CHCQ/
LCP/Pages/LNCAFL2013.aspx. Hospitals are not required
to use this tool; a paper form may be submitted instead.
CHA has developed a form, “Adverse Event Report Form”
(CHA Form 20-1), that hospitals may use to report an
adverse event to CDPH. CDPH has stated it will accept the
CHA form.
D. Communication With Affected Patient(s)
The hospital must inform the patient or the party
responsible for the patient of the adverse event by the
time the report is made. In addition, The Joint Commission
requirement to inform the patient of unanticipated
outcomes of care may apply. (See VI.“Notifying the Patient
or Family,”page8.6.)
E. Relationship With Other Reporting
Requirements
This law does not change or otherwise affect other hospital
reporting requirements regarding reportable diseases or
unusual occurrences. Hospitals may also need to report
adverse events according to the following requirements:

CHA Mental Health Law Manual 2019
8.10
©CALIFORNIA HOSPITAL ASSOCIATION
1. Unusual occurrences — see XI.“Reportable “Unusual
Occurrences”,”page8.14.
2. Safe Medical Devices Act — see IX.“Reports Under
the Safe Medical Devices Act of 1990,”page8.11.
3. Restraint/seclusion death reporting — see
X.“Reporting Requirements Related to Restraint or
Seclusion,”page8.14.
4. Medication errors — see VIII.“Medication
Errors,”page8.11.
5. Injuries by firearm or assaultive or abusive conduct —
see III.“Reporting Injuries by Firearm or Assaultive or
Abusive Conduct (“Suspicious Injuries”),”page7.3.
6. Violence against hospital personnel — see CHA’s
Healthcare Workplace Violence Prevention guidebook,
available to order online at www.calhospital.org/
wvp-guidebook.
7. Radiation overdoses — see CHA’s Consent Manual for
information about reporting radiation overdoses.
In addition, a root cause analysis pursuant to The Joint
Commission’s sentinel event requirements may be required.
(See A.“Sentinel Events,”page8.5)
F. CDPH Investigations and Reports
ONGOING THREAT OF IMMINENT DANGER
CDPH must make an on-site inspection or investigation
whenever it receives an adverse event report or a complaint
indicating an ongoing threat of imminent danger of death or
serious bodily harm. The on-site inspection or investigation
must take place within 48 hours or two business days
(whichever is greater) after receipt of the report or
complaint. The investigation must be completed within
45 days. If CDPH does not meet this time frame, it must
provide written notice to the facility and the complainant
(if any) of the basis for the extenuating circumstances
preventing it from meeting the time frame, and the
anticipated completion date. Until CDPH determines
by on-site inspection that the adverse event has been
resolved, CDPH must conduct an unannounced inspection
at least once per year of any hospital that has reported an
adverse event.
NO THREAT OF IMMINENT DANGER
If CDPH receives a complaint or report, but determines
from the information available to it that there is no threat
of imminent danger of death or serious bodily harm to
that patient or other patients, no on-site inspection is
required, but an investigation must be undertaken and
completed within 45 days. If CDPH does not meet this
time frame, it must provide written notice to the facility and
the complainant (if any) of the basis for the extenuating
circumstances preventing it from meeting the time frame,
and the anticipated completion date.
DEFINITION
For purposes of this law, a “complaint” means any oral or
written notice to CDPH (other than an adverse event report
from the hospital) of an alleged violation of any applicable
state or federal law, or an allegation of facts that might
constitute such a violation.
FOLLOW-UP
CDPH must notify the hospital and the complainant in
writing of its determination as a result of its investigation.
CDPH PUBLIC REPORTING OF ADVERSE EVENTS
CDPH provides information about substantiated adverse
events and the outcomes of inspections and investigations
on its website by posting the hospital’s statement of
Deficiencies (CDPH Form 2567) and the hospital’s plan of
correction.
The information provided by CDPH names individual
hospitals, and may include compliance information history.
The names of patients, health care professionals and health
care workers will not be divulged by CDPH.
G. Penalties for Failure to Report
The adverse event reporting law contains specific penalties
for failure to report. A hospital that fails to report an adverse
event may be assessed a civil penalty in an amount not
to exceed $100 per day for each day that the adverse
event is not reported following the initial five-day period
or 24-hour period, as applicable. If the hospital disputes
a determination by CDPH regarding an alleged failure to
report an adverse event, the hospital may, within 10 days,
request a hearing pursuant to Health and Safety Code
Section 100171. Penalties do not have to be paid until all
appeals have been exhausted.
CDPH has additional authority to fine hospitals for failing
to comply with hospital licensing requirements. It is unclear
whether both fines may apply, or if CDPH is limited to
assessing penalties under this provision.

Chapter 8 — Adverse Events and Incident Reports CHA
8.11
©CALIFORNIA HOSPITAL ASSOCIATION
VIII. MEDICATION ERRORS
Several reporting requirements may be triggered if a
medication error occurs in a hospital.
A pharmacist is required to notify the prescriber and the
patient of a medication error, if the drug was administered
to or by the patient, or if the error resulted in a clinically
significant delay in therapy. The notification must include
the steps required to avoid injury or mitigate the error.
[Title 16, California Code of Regulations, Section 1711] (In
addition, Business and Professions Code Section 4125
requires that medication errors be documented, and
protects such documents from discovery in most cases.)
In addition, a medication error may be reportable under
the Safe Medical Devices Act if a device, such as an
infusion pump, was involved (see IX.“Reports Under the
Safe Medical Devices Act of 1990,”page8.11). Also, a
medication error may constitute an adverse event that
must be reported to CDPH (see VII.“CDPH Adverse
Events Reporting,”page8.7). Finally, a medication
error may constitute an “unusual occurrence” and thus
be reportable to CDPH under that reporting requirement
(see XI.“Reportable “Unusual Occurrences”,”page8.14),
depending on the facts and circumstances of the incident.
Hospitals must comply with all requirements of all
applicable reporting laws.
IX. REPORTS UNDER THE SAFE MEDICAL
DEVICES ACT OF 1990
The Safe Medical Devices Act requires hospitals and other
providers to report incidents involving medical devices
(including restraints) that have or may have caused or
contributed to the serious injury or death of a patient
[21 U.S.C. Section 360i(b)]. In addition to the individual
reports required, hospitals must provide the FDA with
annual summaries of the individual reports made during
the preceding year (see below). Regulations implementing
the reporting requirements are found at 21 C.F.R. part
803. Detailed information about this reporting requirement
may be found at www.fda.gov/MedicalDevices/Safety/
ReportaProblem/default.htm.
It is important to note that the requirement to report
incidents involving medical devices is not limited to
circumstances in which the device malfunctions. When an
incident is, or may be, the result of user error, it should be
reported. In addition, if an infection results, or may have
resulted, from the use of a medical device, that should be
reported also. The FDA monitors these types of events
to determine if different labeling, instructions, design, or
cleaning procedures are needed.
A. When and To Whom Reports of Adverse Events
Must be Made
INDIVIDUAL REPORTS
Hospitals and other health care providers (“device user
facilities”) must make individual (per-incident) reports when
they receive or otherwise become aware of information
reasonably suggesting that a medical device has or
may have caused or contributed to the death or serious
injury of a patient. Reports of individual adverse events
are to be made on FDA Form 3500A, also known as the
“MEDWATCH” form,” or an electronic equivalent approved
by the FDA [21 C.F.R. Section 803.11]. (See “Forms to be
Used,”page8.12.) The information required is specified in
the MEDWATCH form and described in 21 C.F.R. Section
803.32.
Reports of deaths are made to the FDA and to the device
manufacturer if the identity of the manufacturer is known
[21 C.F.R. Section 803.30(a)(1)].
Reports of serious injury are made to the device
manufacturer if the identity of the manufacturer is known;
if the identity of the manufacturer is not known, the report
must be made to the FDA [21 C.F.R. Section 803.30(a)(2)].
Reports must be made as soon as practicable but no later
than 10 work days after becoming aware of the information.
(“Work day” means Monday through Friday, excluding
federal holidays.)
Adverse events need not be reported if there is information
that would cause a person who is qualified to make a
medical judgment (e.g., a physician, nurse, risk manager
or biomedical engineer) to reach a reasonable conclusion
that a device did not cause or contribute to a death or
serious injury, or that a malfunction would not be likely to
cause or contribute to a death or serious injury if it were to
recur. Information which leads the qualified person to this
determination must be contained in the medical device
reporting (MDR) event file [21 C.F.R. Section 803.20(c)(2)].
ANNUAL REPORTS
Annual summaries of individual reports must be made to
the FDA by January 1 of each year using FDA Form 3419,
“Medical Device Reporting Semiannual User Facility Report,”
or an electronic equivalent as approved by the FDA. If no
reports were submitted to the FDA or device manufacturers
during the previous year, the hospital need not submit an
annual report. [21 C.F.R. Section 803.33]

CHA Mental Health Law Manual 2019
8.12
©CALIFORNIA HOSPITAL ASSOCIATION
WHERE TO SUBMIT REPORTS
All reports made to the FDA (individual reports and annual
reports) should be sent to:
Food and Drug Administration
Center for Devices and Radiological Health
Medical Device Reporting
P. O. Box 3002
Rockville, MD 20847-3002
Each report and its envelope must be specifically identified
— e.g., as “User Facility Report” or “Annual Report.”
[21 C.F.R. Section 803.12]
DEFINITIONS
“Become aware” means than an employee of an entity
required to report has acquired information reasonably
suggesting a reportable adverse event has occurred.
Device user facilities are considered to have “become
aware” when medical personnel who are employed by,
or otherwise formally affiliated with (e.g., medical staff),
the facility, obtain information about a reportable event
[21 C.F.R. Section 803.3]. This requirement means that
hospitals and other covered providers must provide
appropriate training and notice to those employees and
other personnel whose knowledge of reportable events will
trigger the facility’s obligation to report, as well as the time
clock (10 work days) for making such reports.
In making reports, facilities must provide all information
specified in the law that is “reasonably known” to them.
This includes information found in documents in the
possession of the device user facility and any information
that becomes available as a result of reasonable follow-up
within the facility. However, a device user facility is not
required to evaluate or investigate the event by obtaining
or evaluating information that is not reasonably known to
it [21 C.F.R. Section 803.30(b)]. (There may, of course, be
other reasons to conduct such investigations, and in such
instances the information discovered would be considered
to be reasonably known to the facility. The medical
device reporting law, however, does not require such
investigations.)
“Caused or contributed” means that a death or serious
injury was or may have been attributed to a medical device,
or that a medical device was or may have been a factor in
a death or serious injury, including events occurring as a
result of failure, malfunction, improper or inadequate design,
manufacture, labeling or user error [21 C.F.R. Section
803.3].
The reporting obligations apply to “device user facilities,”
which includes hospitals, ambulatory surgical facilities,
nursing homes, and outpatient diagnostic and treatment
facilities (but not physicians’ offices) [21 C.F.R. Section
803.3].
“Serious injury” means an illness or injury that:
1. Is life threatening;
2. Results in permanent impairment of a body function or
permanent damage to the body structure; or
3. Necessitates medical or surgical intervention to
preclude impairment of a body function or permanent
damage to a body structure [21 C.F.R. Section 803.3].
FORMS TO BE USED
Forms may be obtained from:
Food and Drug Administration
Division of International and Consumer Education
Center for Devices and Radiological Health
10903 New Hampshire Ave., Bldg. 66, Rm. 4621
Silver Spring, MD 20993-0002
(800) 638-2041
www.fda.gov/medwatch/getforms.htm
email: [email protected]
The MEDWATCH Medical Device Reporting Code
Instruction Manual contains adverse event codes for use
with FDA Form 3500A [21 C.F.R. Section 803.21]. The
manual is available at www.fda.gov/medicaldevices/
deviceregulationandguidance/guidancedocuments/
ucm106737.htm.
QUESTIONS
The FDA asks that questions about reporting be mailed or
faxed to the FDA at the following address:
Food and Drug Administration
Reporting Systems Monitoring Branch (HFZ-533)
Center for Devices and Radiological Health
Medical Devices Reporting Inquiries
1350 Piccard Drive
Rockville, MD 20850
Phone: (240) 276-3464
Fax: (240) 276-3454
The FDA prefers that questions be faxed; however,
questions about medical device reporting may also be
asked by phone, (240) 276-3464. To report a public health
emergency, call the FDA office of Emergency Operations
at (866) 300-4374 and follow with an email to emergency.
[email protected] or a fax to (301) 847-8544.

Chapter 8 — Adverse Events and Incident Reports CHA
8.13
©CALIFORNIA HOSPITAL ASSOCIATION
DISCLAIMERS
A report or other information submitted by a reporting entity
under this law, and any release by the FDA of that report or
information, does not necessarily reflect an admission that
the device, or the reporting entity or its employees, caused
or contributed to the reportable event. The reporting entity
need not admit and may deny that the report or information
submitted under this law constitutes an admission that
the device, the party submitting the report, or employees
thereof, caused or contributed to a reportable event.
[21 C.F.R. Section 803.16]
B. Restraints
FDA regulates restraint devices as it regulates other
medical devices. Thus, hospitals and other device user
facilities must report incidents involving restraints that have
or may have caused or contributed to the serious injury or
death of a patient.
For purposes of this reporting law, it should be noted that
the FDA uses a different definition of restraint than does
the Centers for Medicare & Medicaid Services Conditions
of Participation or California law. The FDA defines a
“protective restraint” as:
a device, including but not limited to a wristlet, anklet,
vest, mitt, straight jacket, body/limb holder, or other type
of strap, that is intended for medical purposes and that
limits the patient’s movements to the extent necessary
for treatment, examination, or protection of the patient or
others [21 C.F.R. Section 880.6760].
Whereas the CMS definition of restraint could include
a geri-chair, a tray table, a side rail, a sheet, or even a
staff member holding a patient, the FDA definition does
not. Therefore, this reporting requirement is somewhat
more narrow than the CMS reporting requirement for
deaths associated with seclusion or restraints discussed
under X.“Reporting Requirements Related to Restraint or
Seclusion,”page8.14.
C. Required Policies and Procedures
Hospitals must develop and implement written policies and
procedures that provide for the following:
1. Timely and effective identification, communication and
evaluation of events that may be subject to medical
device reporting requirements;
2. A standardized review process/procedure for
determining when an event meets the criteria for
reporting to the FDA; and
3. Timely transmission of complete medical device reports
to the FDA and/or the device manufacturer.
The policies and procedures must also include
documentation and record keeping requirements as
described under “Required Documentation” below,
including information that was evaluated to determine if an
event was reportable [21 C.F.R. Section 803.17].
REQUIRED DOCUMENTATION
Facilities must establish and maintain medical device
reporting (MDR) event files. MDR event files must be
prominently identified as such and filed to facilitate timely
access. The files may be written or electronic, and may
incorporate references to other information, such as
medical records or engineering reports, in lieu of copying
and maintaining duplicates in this file. MDR event files must
include the following:
1. Information related to adverse events, including all
documentation of the hospital’s deliberations and
decision-making processes used to determine if a
device-related death, serious injury or malfunction was
or was not reportable under this part; and
2. Copies of all Safe Medical Devices Act forms and other
information related to the event that was submitted to
the FDA or manufacturer.
MDR event files must be retained for two years following
an adverse event. Hospitals must permit FDA employees to
access, copy and verify the records noted above [21 C.F.R.
Sections 803.13, 803.17 and 803.18].
D. Request From FDA for Additional Information
The FDA may determine that protection of the public
health requires additional or clarifying information for the
medical device reports submitted to the FDA under this
law. In these instances, and in cases when the additional
information is beyond the scope of FDA reporting forms or
is not readily accessible, the agency will notify the reporting
entity in writing of the additional information that is required.
Any request from the FDA must state the reason or
purpose for which the information is being requested,
specify the due date for submitting the information and
clearly identify the reported event. All verbal requests will be
confirmed in writing by the FDA. [21 C.F.R. Section 803.15]
E. Device Tracking
Device manufacturers and distributors are required to
develop formal schemes for tracking specified (“tracked”)

CHA Mental Health Law Manual 2019
8.14
©CALIFORNIA HOSPITAL ASSOCIATION
medical devices [21 U.S.C. Section 360i(e)]. Hospitals,
licensed practitioners, retail pharmacists and other types
of device user facilities are considered “final distributors”
[21 C.F.R. Section 821.3].
Under the regulations, a final distributor must provide the
manufacturer with specified information at the time that it
purchases a tracked device [21 C.F.R. Section 821.30(a)]
and at the time that a tracked device is implanted in or
provided to a patient [21 C.F.R. Section 821.30(b)].
At the time that the device is implanted in or provided
to the patient, the hospital must provide to the device
manufacturer the following information:
1. The name and address of the final distributor (i.e., the
hospital itself).
2. The unique device identifier (UDI), lot number, batch
number, model number or serial number of the device,
or other identifier used by the manufacturer to track
the device.
3. The name, address, telephone number and Social
Security number (if available) of the patient receiving
the device unless not released by the patient (see
“Patient Confidentiality Rights,”page8.14).
4. The date the device was provided to the patient or for
use in the patient.
5. The name, mailing address and telephone number of
the prescribing physician.
6. The name, mailing address and telephone number of
the physician regularly following the patient if different
from the prescribing physician.
7. When applicable, the date the device was explanted,
and the name, mailing address and telephone
number of the explanting physician, the date of the
patient’s death, or the date the device was returned
to the manufacturer, permanently retired from use or
otherwise permanently disposed of.
[21 C.F.R. Section 821.30(b)]
PATIENT CONFIDENTIALITY RIGHTS
A patient receiving a device subject to tracking may refuse
to release, or refuse permission to release, his or her name,
address, telephone number and Social Security number,
or other identifying information for the purpose of tracking
[21 CFR Section 821.55]. FDA guidance states that
hospitals must document the refusal and the forwarding of
such documentation back to the device manufacturer.
DEVICE TRACKING RECORDS
Hospitals must permit FDA employees to access, copy and
verify device tracking records, as well as all other records
and information related to the events and persons identified
in such records [21 C.F.R. Section 821.50]. In addition,
hospitals must make any records required to be kept by
the device tracking law available to the manufacturer of
the tracked device for audit upon written request by an
authorized representative of the manufacturer [21 C.F.R.
Section 821.30(d)].
Device tracking records must be maintained for the useful
life of the tracked device. The useful life of a device is
the time a device is in use or in distribution for use. A
record may be retired if the person maintaining the record
becomes aware that the device is no longer in use, has
been explanted, returned to the manufacturer or the patient
has died. [21 C.F.R. Section 821.60]
Records required to be kept by the device tracking law
must be kept in a centralized point [21 C.F.R. Section
821.50].
X. REPORTING REQUIREMENTS RELATED TO
RESTRAINT OR SECLUSION
There are several state and federal reporting requirements
potentially implicated when an adverse event occurs to
a patient who is, or has been, in restraints or seclusion.
These reporting requirements are described in chapter 5.
XI. REPORTABLE “UNUSUAL OCCURRENCES”
Hospitals are required to notify CDPH immediately, via
telephone, of the following:
1. Any discontinuance or disruption of services;
2. Upon the threat of a walkout of a substantial number of
employees; or
3. An earthquake, fire, power outage or other calamity
that causes damage to the facility or threatens the
safety or welfare of patients or clients.
[Title 22, California Code of Regulations, Sections 70746
(general acute care hospitals) and 71544 (acute psychiatric
hospitals)]
Title 22 also requires general acute care hospitals and
acute psychiatric hospitals to report any occurrence such
as an epidemic outbreak, poisoning, fire, major accident,
disaster, other catastrophe or unusual occurrence
which threatens the welfare, safety, or health of patients,
personnel, or visitors, as soon as reasonably practicable,

Chapter 8 — Adverse Events and Incident Reports CHA
8.15
©CALIFORNIA HOSPITAL ASSOCIATION
by telephone or telegraph, to the local health officer
and to CDPH. The hospital must furnish other pertinent
information related to the occurrence as may be requested
by the local health officer or CDPH [Title 22, California
Code of Regulations, Sections 70737 (general acute care
hospital), 71535 (acute psychiatric hospital) and 72541
(skilled nursing facility)].
Exactly which types of incidents constitute an “unusual
occurrence” has not been further clarified by CDPH. CDPH
is aware that its employees as well as hospital employees
have inconsistent interpretations of this requirement. CDPH
has indicated that sentinel events should be considered
unusual occurrences, and reported to CDPH even if the
hospital does not report to The Joint Commission. (See
A.“Sentinel Events,”page8.5, regarding sentinel
events.) CDPH has also indicated that a patient death
that occurs while a patient is restrained or in seclusion for
behavior management is a reportable unusual occurrence.
In addition, CDPH has indicated that incidents that are
covered by the news media constitute unusual occurrences
that should be reported to CDPH. However, CDPH has
not promulgated regulations regarding these informal
interpretations. There are no financial penalties for a late
report or failure to report under this law.

Chapter 9 — Contents
©CALIFORNIA HOSPITAL ASSOCIATION
9 Payment for Medi-Cal Emergency
and Post-Stabilization Mental Health
Services
I. INTRODUCTION ....................................... 9.1
A. Background ....................................................9.1
B. Scope of This Chapter ..................................9.1
II. MEDI-CAL PAYMENT FOR MENTAL
HEALTH SERVICES
.................................. 9.2
A. What Mental Health Services Are
Covered by MHPs?
........................................9.2
B. What Mental Health Services Are
Covered by MCPs?
........................................9.4
C. Must MHPs and MCPs Pay for
Emergency and Post-Stabilization
Services Rendered by Non-Contracted
Providers?
......................................................9.5
Emergency Services .........................................9.5
Post-Stabilization Services
................................ 9.5
D. Important Definitions ....................................9.6
E. How Do MHPs and MCPs Coordinate
Their Payment and Care Management
Obligations?
...................................................9.6
III. HOW HOSPITALS CAN GET REIMBURSED:
A CASE-BY-CASE ANALYSIS
..................... 9.7
FORMS & APPENDICES
MH 9-A Medical Necessity for MHP Coverage
MH 9-B Types of MCPs and MHPs
MH 9-C Pertinent DHCS Plan Letters
MH 9-D DHCS Chart: Medi-Cal Mental Health Services
MH 9-E Pertinent Legal Definitions of Emergency
Psychiatric Conditions
Forms and Appendices can be found at the back of the manual and
online for CHA members at www.calhospital.org/free-resources.

9.1
©CALIFORNIA HOSPITAL ASSOCIATION
9 Payment for Medi-Cal Emergency
and Post-Stabilization Mental Health
Services
I. INTRODUCTION
Consider this scenario: A Medi-Cal patient
presents to a hospital’s emergency department
(ED) complaining of chest pain. The hospital does
not have an inpatient psychiatric unit. The hospital
provides a medical screening exam and further
evaluation and treatment; cardiac conditions are
ruled out. The patient is diagnosed with a severe
anxiety disorder. The patient’s anxiety disorder is
treated and the patient is discharged home.
Question: Who is responsible for paying for the
services rendered to rule out cardiac conditions?
Who is responsible for paying for the services
rendered to diagnose and treat the mental
health conditions?
California hospitals struggle with situations like this every
day, trying to determine who is responsible for paying for
the various services rendered — those related to “physical
health” conditions, and those related to mental health
conditions. Does the hospital bill the Medi-Cal managed
care plan (MCP) only? Or the county mental health plan
(MHP) only? Both the MCP and the MHP for different
services rendered? Or do other factors affect the analysis?
What can the hospital do when both the MCP and MHP
deny financial responsibility?
This chapter analyzes the various and sometimes
conflicting laws governing who is responsible to pay for
services rendered in an ED to Medi-Cal patients with
mental health conditions.
A. Background
The State of California administers the Medi-Cal program
through the Department of Health Care Services (DHCS).
DHCS contracts with both MCPs and MHPs to serve
Medi-Cal patients. MCPs provide care for the patients’
physical conditions, as well as for specified, lower-acuity
mental health conditions.
1
Because counties have
historically played an important role in providing access to
mental health services for Medi-Cal beneficiaries, DHCS
delegates payment for other mental health services
to MHPs.
Due to the various co-morbidities associated with mental
health patients, the line delineating payment responsibility
between MCPs and MHPs is often blurred. For example,
when a patient presents with multiple diagnoses, especially
both mental and physical in nature, both a MCP and MHP
may be responsible for payment.
While reading this chapter, it’s important to keep in mind
that the federal Emergency Medical Treatment and Labor
Act (EMTALA) and state hospital licensing requirements
to provide emergency services to psychiatric patients, are
different from the Medi-Cal requirements to pay for those
services. As a result, hospitals are often not reimbursed for
all the services they’re required to provide.
Hospitals should know that MHPs are not licensed under
the Knox-Keene Health Care Service Plan Act, and are
not regulated by the California Department of Managed
Health Care (DMHC). Most MCPs are licensed under the
Knox-Keene Act and are regulated by DMHC, except
for county operated health systems with respect to their
Medi-Cal lines of service.
B. Scope of This Chapter
This chapter reviews the laws and DHCS interpretations
about payment for ED services, including emergency
medical services, emergency psychiatric services, and
non-emergency services. This chapter also provides
1 This chapter focuses on the typical allocation of payment responsibilities
between MCPs and MHPs in California. Certain counties, such as Solano
County, and plans, such as Kaiser Geographic Managed Care, are different
and not the focus of this chapter. This chapter also does not focus on the
responsibility of other types of managed care, such as PACE programs, SCAN
programs or the San Francisco Family Mosaic Project.

CHA Mental Health Law Manual 2019
9.2
©CALIFORNIA HOSPITAL ASSOCIATION
some arguments that may help hospitals obtain improved
reimbursement for mental health services rendered to
Medi-Cal patients presenting to the ED with a mental
health condition.
Due to the complexities of reimbursement for mental health
conditions, this chapter is not fully comprehensive. For
example, this chapter does not address the memoranda
of understanding (MOU) that DHCS requires between
MCPs and MHPs to coordinate mental health services for
Medi-Cal patients.
2
Also, this chapter does not address
coordination of benefits between Medi-Cal and other
health coverage, e.g., where a Medi-Cal patient has private
insurance, or is enrolled in Medi-Cal managed care and
Medicare fee-for-service or Medicare Advantage, or for a
patient enrolled in a Cal MediConnect plan. Nor does this
chapter address payment responsibility for a patient who
is enrolled in Medi-Cal fee-for-service instead of Medi-Cal
managed care. Hospitals may wish to seek separate
guidance for these fact-specific issues.
This chapter is organized as follows:
• Section II — Medi-Cal Payment for Mental Health
Services. Section II describes the mental health services
covered by MHPs and MCPs; the respective obligations
of MHPs and MCPs to pay for emergency and
post-stabilization services rendered by non-contracted
providers; and coordination of payment and care
management between MHPs and MCPs.
• Section III — How Hospitals Can Get Reimbursed:
A Case-by-Case Analysis. Section III applies the
general payment principles described in Section II to
eight scenarios where a patient presents to an ED with a
complaint that includes a psychiatric condition.
• Appendix MH 9-A, “Medical Necessity for MHP
Coverage.” This appendix contains the state regulations
describing medical necessity for MHP coverage of
psychiatric inpatient, emergency and outpatient specialty
mental health services.
2 Boilerplate MCP Contract, Exh. A, Attachment 11, Provision
6.B, available at www.dhcs.ca.gov/provgovpart/Documents/
ImpRegSB2PlanBp32014.pdf (accessed May 25, 2019). Citations to the
boilerplate contracts are to the two plan model contracts, but parallel
provisions are found in the county operated health system and geographic
managed care model boilerplate contracts.
If an MOU is not posted on the MCP or MHP’s website and is not readily
available upon request from the MCP, MHP or county behavioral health
department, a hospital may make a formal request for it under the California
Public Records Act.
• Appendix MH 9-B, “Types of MCPs and MHPs.” This
appendix briefly describes the types of MCPs and MHPs
throughout the state and their governing authorities.
• Appendix MH 9-C, “Pertinent DHCS Plan Letters.”
This appendix contains excerpts of DHCS plan
letters related to emergency services for mental
health conditions.
• Appendix MH 9-D, “DHCS Chart: Medi-Cal Mental
Health Services.” This appendix contains a DHCS chart
describing MCP and MHP financial responsibilities for
mental health services for Medi-Cal patients.
• Appendix MH 9-E, “Pertinent Legal Definitions of
Emergency Psychiatric Conditions.” This appendix
compares Medicaid, Medi-Cal, licensing and EMTALA
definitions that apply to emergency psychiatric conditions.
II. MEDI-CAL PAYMENT FOR MENTAL HEALTH
SERVICES
A. What Mental Health Services Are Covered by
MHPs?
The state contracts with a MHP in each county to provide
or arrange for, and pay for, all medically necessary,
covered Specialty Mental Health Services (SMHS) for
Medi-Cal patients who reside in that county.
3
“Covered
SMHS” means specified health services, including
psychiatric health facility services, psychiatric inpatient
hospital services, and other mental health services, that
meet the criteria for “medical necessity” set forth in MHP
regulations at Title 9, California Code of Regulations
(CCR) Sections 1820.205, 1830.205 or 1830.210. These
criteria are outlined in Appendix MH 9-A, “Medical
Necessity for MHP Coverage.” Many counties have
informational documents on their website which may be
helpful to hospitals. (See www.file.lacounty.gov/SDSInter/
dmh/159129_MediCalGuide_English_July2013.pdf for an
example.)
Historically, the state contractually required MHPs to
pay for “services for emergency psychiatric conditions
received by a beneficiary from providers, whether or not
3 Boilerplate MHP Contract 2017-22, Exh. A, Attachment 2, available
at https://www.dhcs.ca.gov/services/MH/Documents/PPQA%20Pages/
Boilerplate_2017-2022_MHP_Contract-Exhibits_A_B_and_E.pdf (accessed
May 25, 2019). While this contract is identified on the DHCS website as
effective July 1, 2017, through June 30, 2022, the contract was not made
publicly accessible on the DHCS website until 2018. Thus, it is unclear as to
when this contract actually became effective.

Chapter 9 — Payment for Medi-Cal Emergency and Post-Stabilization Mental Health Services CHA
9.3
©CALIFORNIA HOSPITAL ASSOCIATION
the provider has a subcontract” with the MHP.
4
The prior
contract between the state and the MHP does not define
the term “emergency psychiatric condition,” but required
the MHP to consider certain ICD-9 diagnosis codes as
included. While not defined in the prior contract, the term
“emergency psychiatric condition” is defined in Title 9,
CCR Section 1810.216 as a condition meeting the medical
necessity criteria in Title 9, CCR, Section 1820.205 when
the patient, “due to a mental disorder, is a current danger
to self or others, or immediately unable to provide for or
utilize, food, shelter or clothing, and requires psychiatric
inpatient hospital or psychiatric health facility services.”
5
Unfortunately, there is little explanation in the contract,
the regulations or other guidance that detail the precise
parameters of the MHP’s obligation to cover services for
emergency psychiatric conditions.
As discussed in footnote 4, CHA believes that the State
amended its contract with MHPs in or around 2018. That
version of the contract specifies that the MHP “shall
authorize out of network services when a beneficiary with
an emergency psychiatric condition is admitted on an
emergency basis for psychiatric inpatient hospital services
or psychiatric health facility services.”
6
The more recent
version of the contract is silent as to what Medi-Cal payor
is responsible to pay for emergency services associated
with a severe mental health diagnosis in the absence of an
admission to a psychiatric inpatient hospital or psychiatric
health facility.
7
4 Boilerplate MHP Contract 2013-18, Exh. A, Attachment I, Provision 3,
available at https://www.dhcs.ca.gov/services/MH/Documents/2013-2018_
MHP_Contract.pdf. Even though the DHCS website identifies this contract
as effective July 1, 2013, through June 30, 2017, the title of the document
suggests that it may have been effective through 2018, which would be
consistent with the timing of the more recent contract becoming uploaded to
the DHCS website.
5 As shown in Appendix E, the definition of “emergency psychiatric
condition” in the MHP regulations varies from the definition of “psychiatric
emergency medical condition” in the California emergency services licensing
laws (Health & Safety Code Section 1317.1). The licensing laws, which govern
the emergency care that a hospital must provide, do not require “medical
necessity” or that a hospital maintain a psychiatric service, in order for a
psychiatric condition to be deemed an “emergency condition” that the hospital
must treat or effectuate a transfer.
6 Boilerplate MHP Contract 2017-22, Exh. A, Attachment 6, Provision G.
7 However, as recently as Sept. 26, 2018, DHCS issued All Plan Letter
18-043, which requires MHPs to state in their member handbooks that “prior
authorization is not required for emergency services and the beneficiary has
the right to use the hospital or other setting for emergency care.” Pages 58-59
of the template handbook available at https://www.dhcs.ca.gov/services/
MH/Documents/Information%20Notices/IN_18-043_Beneficiary_Handbook/
MHP_Beneficiary_Handbook.pdf (accessed May 25, 2019) states that the
MHP is required to… [p]rovide timely access to care, including making
services available 24 hours a day, seven days a week, when medically
necessary to treat an emergency psychiatric condition or an urgent or crisis
condition.” This is consistent with the statement on page 16 of the handbook
that “[e]mergency services are covered 24 hours a day, seven days a week for
Medi-Cal beneficiaries.”
California regulations also require a MHP to cover services
rendered when a patient with an emergency psychiatric
condition is admitted for psychiatric inpatient hospital
services to the extent provided in Title 9, CCR Section
1820.225 (an “emergency admission”) or admitted for
psychiatric health facility services under the conditions
described in Title 9, CCR Section 1830.245, whether
in-network or out-of-network. Approval for payment for
such services associated with an emergency psychiatric
condition may be subject to the patient meeting certain
medical necessity and other criteria, as well as timely
notification by the hospital or psychiatric health facility to
the MHP. [Title 9, CCR Sections 1820.225 and 1830.245]
DHCS has issued several plan letters, including Medi-Cal
Managed Care Policy Letter (MMCD) 00-01 and All Plan
Letter (APL) 13-021, excerpts of which are included in
Appendices MH 9-C, “Pertinent DHCS Plan Letters” and
MH 9-D, “DHCS Chart: Medi-Cal Mental Health Services,”
respectively. These DHCS documents attempt to clarify
when the MCP is responsible for payment, and when the
MHP is responsible for payment, but the documents are
not entirely consistent. However, based on these letters, it
is likely DHCS’ position that the MHP is responsible for the
following emergency, inpatient and outpatient services:
1. Emergency/inpatient services if the patient:
a. Has an included diagnosis;
b. Cannot be safely treated at lower level of care; and
c. Requires inpatient hospital services due to
one of the following as a result of an included
mental disorder:
• Symptoms or behaviors that represent a
current danger to self or others, or significant
property destruction;
• Symptoms or behaviors that prevent the
beneficiary from providing for, or utilizing, food,
clothing, or shelter;
• Symptoms or behaviors that present a severe
risk to the beneficiary’s physical health;
• Symptoms or behaviors that represent a recent,
significant deterioration in ability to function;
• Psychiatric evaluation or treatment can only
be performed in an acute psychiatric inpatient
setting or through urgent or emergency
intervention provided in the community or
clinic; and

CHA Mental Health Law Manual 2019
9.4
©CALIFORNIA HOSPITAL ASSOCIATION
• Serious adverse reactions to medications,
procedures or therapies requiring continued
hospitalization.
8
d. Facility charges for emergency services when
the patient meets medical necessity criteria and
is admitted for psychiatric inpatient services at
the same facility that provided the emergency
services.
9
e. Facility charges directly related to the professional
services of a mental health specialist provided
in the ED when the services do not result in
the patient’s admission for psychiatric inpatient
hospital services in the same or another facility.
10
f. Professional services of a mental health specialist
provided in an ED of any hospital to a patient
whose condition meets medical necessity criteria
or when required to assess whether medical
necessity is met.
11
2. Outpatient services if:
a. The patient has an included mental
health diagnosis;
b. The patient has a significant impairment in an
important area of life function, or a reasonable
probability of deterioration in an important area
of life function, or a reasonable probability
of not progressing developmentally as
individually appropriate;
c. The focus of treatment is to address impairment;
d. The expectation that proposed treatment will
significantly diminish impairment, prevent
significant deterioration; and
e. The condition would not be responsive to physical
health care-based treatment.
12
B. What Mental Health Services Are Covered by
MCPs?
The state contracts with MCPs to provide or arrange
for medically necessary covered services for Medi-Cal
patients assigned to them, including outpatient mental
health services. “Outpatient mental health services” are
defined as:
8 APL 13-021.
9 Medi-Cal Managed Care Policy Letter (MMCD) 00-01.
10 Id.
11 Id.
12 Id.
outpatient services that [the MCP] will provide for
Members with mild to moderate mental health conditions
including: individual or group mental health evaluation
and treatment (psychotherapy); psychological testing
when clinically indicated to evaluate a mental health
condition; psychiatric consultation for medication
management; and outpatient laboratory, supplies, and
supplements.
13
SMHS are excluded from the scope of MCP services.
14
MCPs are required to pay for certain medically necessary
mental health services, such as “[e]mergency room
professional services as described in Title 22, CCR
Section 53855, except services provided by psychiatrists,
psychologists, licensed clinical social workers, marriage,
family and child counselors [now called marriage and family
therapists], or other specialty mental health providers” and
“[f]acility charges for emergency room visits which do not
result in a psychiatric admission.”
15
DHCS has stated that the MHP is responsible for the
following emergency and outpatient services:
1. Emergency Services:
a. All professional services except the professional
services of a mental health specialist when
required for the emergency services and care of a
patient, regardless of whether the condition meets
MHP medical necessity criteria
16
; and
b. All facility and professional charges for emergency
services and care of a patient when such services
do not result in admission. This includes patients
with an excluded diagnosis or whose condition
does not meet medical necessity criteria.
17
2. Outpatient Services:
a. When the patient has been diagnosed with
a mental health disorder as defined by the
DSM
18
resulting in mild to moderate distress or
impairment of mental, emotional or behavioral
functioning.
19
13 Boilerplate MCP Contract, Exh. E, Attachment 1.
14 Boilerplate MCP Contract, Exh. A, Attachment 11, Provision 6.
15 Boilerplate MCP Contract, Exh. A, Attachment 10, Provision 8.E.
16 MMCD 00-01.
17 MMCD 00-01; see also Dual Plan Letter 15-006, p. 5.
18 “DSM” refers to the Diagnostic and Statistical Manual of Mental
Disorders, Fourth Edition, DSM-IVE (1994), published by the American
Psychiatric Association.
19
APL 13-021.

Chapter 9 — Payment for Medi-Cal Emergency and Post-Stabilization Mental Health Services CHA
9.5
©CALIFORNIA HOSPITAL ASSOCIATION
C. Must MHPs and MCPs Pay for Emergency and
Post-Stabilization Services Rendered by Non-
Contracted Providers?
EMERGENCY SERVICES
Under federal Medicaid law and the waivers governing the
MCP and MHP programs,
20
MCPs and MHPs are required
to pay for emergency services and post-stabilization
services regardless of whether the provider has a contract
with the plan.
21
The Centers for Medicare & Medicaid
Services (CMS) has stated that this obligation applies only
if the patient has an “emergency medical condition” as
defined below.
If a psychiatric condition does not give rise to an
“emergency medical condition” within the definition below
— that is, there is no risk of serious jeopardy to the health
of the patient — then the patient is not considered to have
an emergency medical condition under federal law and the
MCP or MHP is not required to pay. [67 Fed. Reg. 40989,
41030 (June 14, 2002)] However, DHCS has suggested
that the scope of emergency services required to be
covered under California law may expand to “screening,
examination, and evaluation to determine if a psychiatric
emergency medical condition exists, and the care and
treatment necessary to relieve or eliminate the psychiatric
medical condition, within the capability of the facility.”
22
Federal Medicaid law defines an emergency medical
condition as a medical condition manifesting itself by acute
symptoms of sufficient severity (including severe pain)
such that a prudent layperson, with an average knowledge
of health and medicine, could reasonably expect the
absence of immediate medical attention to result in: serious
jeopardy to the health of the individual or, in the case of a
pregnant woman, the health of the woman or her unborn
child; serious impairment to bodily functions; or serious
dysfunction of any bodily organ or part. [42 C.F.R. Section
422.113(b)(1)(i)] (See D.“Important Definitions,”page9.6
as to variances in the definition of “emergency medical
condition” in the federal Medicaid law and in the federal
EMTALA regulations (42 C.F.R. Section 489.24(b)).)
Emergency services are defined as covered inpatient and
outpatient services that are rendered by a provider qualified
to furnish emergency services; and needed to evaluate
or stabilize an emergency medical condition [42 C.F.R.
Section 422.113(b)(1)(ii)].
20 The MHP program is governed by the 1915(b) waiver while the MCP
program is governed by the 1115 waiver. These citations are to the sections of
the Social Security Act authorizing the waivers.
21
2 U.S.C. Section 1396u-2(b)(2); 42 C.F.R. Section 438.114(c); Title 9,
CCR Section 1810.345(e); Boilerplate MHP Contract, Exh. A, Attachment I,
Provision 3; Boilerplate MCP Contract, Exh. A, Attachment 8, Provision 13.
22
MCD Policy Letter No. 00-01 Rev., excerpted in Appendix C.
The most recent version of the boilerplate MHP contract
appears to exempt MHPs from the requirements of
42 C.F.R. section 422.113.
23
The legal impact of this
exemption for emergency services is unclear as it appears
to be inconsistent with both the 1915(b) waiver and state
law at California Code of Regulations, Title 9, Section
1810.345(e).
POST-STABILIZATION SERVICES
Federal Medicaid law defines “post-stabilization services”
as covered services that are:
1. Related to an emergency medical condition;
2. Provided after an enrollee is stabilized; and
3. Provided either to maintain the stabilized condition, or
under certain circumstances, to improve or resolve the
enrollee’s condition.
[42 C.F.R. Section 422.113(c)(1)]
The physician treating the enrollee must decide when the
enrollee is considered stabilized for transfer or discharge,
and that decision is binding on an MCP or MHP [42 C.F.R.
Section 422.113(b)(3)].
Under the federal Medicaid regulations, a MCP or MHP
is financially responsible for post-stabilization services
obtained within, or outside, the plan network that meet one
of the following:
1. Are pre-approved by a plan provider or other plan
representative; or
2. Are not pre-approved by a plan provider or other
plan representative, but are administered to maintain
the patient’s stabilized condition within one hour
of a request to the plan for pre-approval of further
post-stabilization care; or
3. Are not pre-approved by a plan provider or other plan
representative, but administered to maintain, improve,
or resolve the patient’s stabilized condition if:
a. The plan does not respond to a request for
pre-approval within one hour;
b. The plan cannot be contacted; or
c. The plan representative and the treating physician
cannot reach an agreement concerning the
patient’s care, and a plan physician is not available
for consultation. In this situation, the plan must
give the treating physician the opportunity to
consult with a plan physician. The treating
physician may continue with care of the patient
23 Boilerplate MHP Contract 2017-22, Exh. E, Provision 7.D.

CHA Mental Health Law Manual 2019
9.6
©CALIFORNIA HOSPITAL ASSOCIATION
until a plan physician is reached or one of the
criteria below is met.
[42 C.F.R. Section 422.113(c)(2)]
If no pre-approval has been obtained, the MCP or MHP’s
financial responsibility for post-stabilization services ends
when one of the following has occurred:
1. A plan physician with privileges at the treating hospital
assumes responsibility for the patient’s care; or
2. A plan physician assumes responsibility for the
patient’s care through transfer; or
3. A MCP or MHP plan representative and the treating
physician reach an agreement concerning the patient’s
care; or
4. The patient is discharged.
[42 C.F.R. Section 422.113(c)(3)]
Again, the law is unsettled as to the impact of the 2018
amendment to the state MHP contract on the obligation of
MHPs to cover post-stabilization care.
In summary, psychiatric emergency services are covered
to the extent that a mental health diagnosis is such that a
prudent layperson could reasonably expect the absence of
immediate medical attention to result in serious jeopardy
to the health of the individual; serious impairment to bodily
functions; or serious dysfunction of any bodily organ or part,
inpatient and outpatient services needed to evaluate or
stabilize the condition would constitute covered emergency
services. Post-stabilization psychiatric services are covered
if provided after the patient’s psychiatric condition is
stabilized in order to maintain the stabilized condition or to
improve or resolve the enrollee’s condition.
D. Important Definitions
A question that frequently arises is whether the terms
“emergency medical condition” and “psychiatric emergency
medical condition” for Medi-Cal reimbursement purposes
have the same definition as these terms as applied under
EMTALA or state licensing laws for emergency psychiatric
medical conditions? The answer is “no.”
As shown in Appendix MH 9-E, “Pertinent Legal Definitions
of Emergency Psychiatric Conditions,” the definition of
“emergency medical condition” in the federal Medicaid
law [42 U.S.C. Section 1396u-2(b)(2)(C)] varies from
the definition of “emergency medical condition” in the
federal EMTALA regulations (42 C.F.R. Section 489.24(b)).
The EMTALA regulations explicitly include “psychiatric
disturbances” and “symptoms of substance abuse” in
the definition of “emergency medical condition” —
“a medical condition manifesting itself by acute symptoms
of sufficient severity (including severe pain, psychiatric
disturbances and/or symptoms of substance abuse)
such that the absence of immediate medical attention
could reasonably be expected to” jeopardize the health of
the patient. The federal Medicaid law does not mention
psychiatric disturbances.
The mental health parity law [42 U.S.C. Section 300gg]
requires a Medicaid managed care plan to provide
out-of-network benefits for mental health/substance use
disorders if it provides out-of-network benefits for medical/
surgical conditions. However, this requirement is applied
across a state’s Medicaid program, and does not mean that
the same plan that might be liable for the medical/surgical
benefit is necessarily liable for the mental health/substance
use benefit. [42 C.F.R. Section 438.920(b)]
At the state level, the definition of “psychiatric emergency
medical condition” in the MHP regulations varies from the
definition of “psychiatric emergency medical condition” in
the California emergency services licensing law (Health and
Safety Code Section 1317.1). The MHP regulations require
“medical necessity” and psychiatric hospital services in order
for the psychiatric condition to be deemed an “emergency
condition.” The licensing definition does not impose either
requirement for a psychiatric condition to be deemed an
emergency condition.
It is noted that all of the definitions of “emergency medical
condition” and “psychiatric emergency medical condition”
apply when the patient may be a danger to himself/herself,
which may include grave disability; however, the Medicaid
definition does not include a situation where a patient may
be a danger to others, but not to himself/herself.
E. How Do MHPs and MCPs Coordinate Their
Payment and Care Management Obligations?
MCPs and MHPs are required to execute memoranda of
understanding (MOUs) to coordinate care between them.
24
There have been over 100 MOUs executed in the State of
California.
25
Each MOU should include the following topics:
1. Basic requirements
2. Covered services and populations
3. Oversight responsibilities of the MCP and MHP
4. Screening, assessment and referral
5. Care coordination
24 Title 9, CCR Sections 1810.370, 1810.415, 1850.505, 1850.515,
1850.525; MCP Boilerplate Contracts, Exh. A, Attachment 11 and Attachment
12; All Plan Letter 13-018.
25
Lewis, K. and Coursolle, A., National Health Law Program, Mental Health
Services in Medi-Cal, p. 7 (Jan. 12, 2017).

Chapter 9 — Payment for Medi-Cal Emergency and Post-Stabilization Mental Health Services CHA
9.7
©CALIFORNIA HOSPITAL ASSOCIATION
6. Information exchange
7. Reporting and quality improvement requirements
8. Dispute resolution
9. After-hours policies and procedures, and
10. Member and provider education.
However, the National Health Law Program study cited in
footnote 26 reported that many MOUs fail to include some
of these required topics.
26
Review of a MOU may help a hospital understand how
its local MCP and MHP have agreed to coordinate care,
including screening, assessment and referral of ED patients.
Accordingly, hospitals may wish to review their local MOU(s)
in connection with their review of the analysis in this
chapter, which does not include any analysis of the MOUs
across the state. Hospitals may be able to rely on promises
from MCPs and MHPs to each other in order to effectuate
better care coordination for patients who present at their
ED with mental health conditions.
If a MOU is not available on the Internet, a hospital may
wish to request a copy of the agreement from the MHP
pursuant to the California Public Records Act.
III. HOW HOSPITALS CAN GET REIMBURSED: A
CASE-BY-CASE ANALYSIS
CHA has applied the general principles of the various
laws and DHCS interpretations described above to the
following eight scenarios to help hospitals identify which
type of plan likely is responsible for reimbursing the hospital
for emergency psychiatric services. However, individual
circumstances may affect the outcome of each scenario.
For example, a contract between a hospital and a specific
plan may set forth the payment responsibilities by that plan
to the hospital. If there is no contract between a hospital
and a specific plan, the facts, such as whether notice of
stabilization was given or whether the plan pre-approved
the care, will determine whether there may be an implied
contract between the hospital and the plan.
Each scenario below begins with a patient presenting to a
hospital ED, either voluntarily or involuntarily. However, the
scenarios differ as to whether the hospital has inpatient
psychiatric beds, whether the patient has a psychiatric
emergency condition, whether the patient’s psychiatric
condition is stabilized in the ED, whether the patient
is stabilized when admitted to a psychiatric inpatient
bed, whether the patient is transferred to an inpatient
psychiatric facility, whether the patient is actually admitted
26 Ibid.
to a psychiatric inpatient bed and whether the patient is
discharged to the community.
27
Scenario
#
Hospital
ED
Hospital
w/Psych.
Inpt.
Pt. has
Psych.
Emgcy
28
Stabilized
in ED
Trans-
ferred
to
Psych
Inpt.
Admitted
to Psych
Inpt.
Final
Status
1
Yes Either Yes Yes No
No
Discharged
to
Comm.
2
Yes Either No NA No
No
Discharged
to
Comm.
3.a Yes Yes Yes Possible Yes
No
Transferred
to
Another
Hospital
3.b NA Yes Yes Possible No
Yes
Admitted
4
Yes Yes Yes No No
Yes
Admitted
5.a Yes No Yes
Sufficient
for
Transfer
Yes
See
5.b.1/
5.b.2
Transferred
to
Another
Hospital
5.b.1 NA Yes Yes
Received
Transfer No
Yes
Admitted
5.b.2 NA Yes Yes
Received
Transfer No
No
Discharged
to
Comm.
Each scenario assumes that the patient is given a medical
screening examination to assess the emergent nature
of the patient’s medical or psychiatric condition. In most
instances, the MCP is likely responsible to pay for the
medical screening examination.
Scenario 1: Patient presents at the ED of a hospital
with or without inpatient psychiatric services. The
patient is experiencing depression and suicidal
ideation. The patient is determined by a physician
or other professional to have an emergency
psychiatric condition. The patient’s psychiatric
condition is stabilized in the ED after a licensed
clinical social worker consults with the patient and
obtains information from family members about a
recent break-up with a girlfriend. After several hours,
the patient is discharged home with a referral for
follow-up outpatient care.
This patient required a level of care that did not require
an acute inpatient stay. Accordingly, consistent with the
27 The involvement or intervention in the emergency services process by
county-designated mental health professionals does not affect which plan is
responsible for payment.
28
In other words, the patient is determined by a physician or other
professional to have an emergency psychiatric condition within the meaning
of EMTALA and the California hospital licensing laws [Health & Safety Code
Section 1317.1].

CHA Mental Health Law Manual 2019
9.8
©CALIFORNIA HOSPITAL ASSOCIATION
MCP-State contract, MMCD 00-01 and APL 13-021, it is
likely that the MCP is responsible for paying for the ED visit,
including both the facility and professional charges. The
MCP will not pay for services provided by mental health
specialists, such as the consult with the LCSW.
29
Instead,
it is the MHP’s responsibility to pay for the professional
services of mental health specialists provided in the ED
to patients meeting MHP medical necessity criteria or
required to assess whether MHP criteria are met, and any
facility charges directly related to mental health specialists’
services.
30
It is likely that the MCP is responsible for mental
health specialists’ services required for the emergency
services and care of a patient with an excluded diagnosis.
Hospitals should have a billing policy in place to ensure
that facility fees are not inadvertently collected from
both the MHP and the MCP in those instances where
both may be responsible for facility fees for professional
services provided.
Scenario 2: Patient presents at the ED of a hospital
without inpatient psychiatric services. Although the
patient is experiencing auditory hallucinations, and
it is determined by a physician or other professional
that the patient has a psychiatric condition, the
patient does not have an emergency psychiatric
condition. The patient is provided further evaluation
and treatment and is subsequently discharged
without an inpatient admission.
The analysis for this scenario is likely the same as Scenario
1 because the patient’s condition and level of care did not
require an acute inpatient stay.
Scenarios 3.a and 3.b: Patient presents to the ED
of a hospital with inpatient psychiatric services. The
patient has suicidal ideation with a specific plan.
The patient is determined by a physician or other
professional to have an emergency psychiatric
condition, and is transferred to another facility that
provides acute inpatient psychiatric services due to
its lack of capacity or capability to admit the patient
(e.g., transfer of an adolescent or child from a
psychiatric facility that does not admit minors).
29 Specialty mental health providers include psychiatrists, psychologists,
licensed clinical social workers, and marriage and family therapists (previously
called marriage, family and child counselors).
30
MMCD 00-01. This includes hospitals that provide and do not provide
acute psychiatric services.
3.a. Sending hospital. Both the MCP and the MHP may
be responsible for reimbursement for hospital charges.
More specifically, pursuant to the MMCD 00-01, the MCP
may be responsible for facility charges incurred by the
sending hospital. However, because the patient’s condition
ultimately resulted in a psychiatric admission and because
the service was “for an emergency psychiatric condition,”
the MHP may also be responsible for the facility charges for
services rendered by the sending hospital to the extent that
the patient meets the medical necessity criteria. Hospitals
may wish to review their contracts with the local MHP or
MCP (if applicable) or the MOU between their local MHP
and MCP for further clarification. Some MOUs have a gap
where:
1. Patients that are admitted at the same hospital are the
responsibility of the MHP,
2. Patients that are not admitted for inpatient psychiatric
services are the responsibility of the MCP, and
3. No provision identifies responsibility where the patient
is admitted for inpatient psychiatric services at another
facility.
Our experience has indicated that there is no standard
between counties as to MHP or MCP reimbursement to
sending hospitals as in this scenario for services rendered
in the emergency department.
With respect to professional fees, the MHP likely is
responsible for professional services of mental health
specialists provided in the ED to patients meeting MHP
medical necessity criteria or required to assess whether
MHP criteria are met.
31
The MCP is likely responsible for
other professional charges, including professional services
not provided by mental health specialists and services
provided by mental health specialists to patients who do
not meet the medical necessity criteria.
3.b. Receiving hospital. Pursuant to the MHP-State
contract and MMCD 00-01 and APL 13-021, the MHP
is responsible for the inpatient acute psychiatric care
rendered to this patient if the patient meets medical
necessity criteria. The MCP continues to have responsibility
for professional services necessary to meet the physical
needs of the patient while admitted at the receiving
hospital
32
, although the MHP may be responsible for
routine hospital services and certain ancillary services.
33
To the extent that the patient does not have a diagnosis
listed in Appendix MH 9-A, “Medical Necessity for MHP
Coverage,” but requires inpatient acute psychiatric care,
31 Ibid.
32 Ibid.
33 Welfare and Institutions Code Section 14722; Cal. Code Regs., Title 9,
Section 1810.350; MMCD 00-01.

Chapter 9 — Payment for Medi-Cal Emergency and Post-Stabilization Mental Health Services CHA
9.9
©CALIFORNIA HOSPITAL ASSOCIATION
the hospital should consult its legal counsel to pursue
payment options for the services rendered.
Scenario 4: Patient presents to the ED of a hospital
with inpatient psychiatric services. The patient has
suicidal ideation with a specific plan. The patient
is determined by a physician or other professional
to have an emergency psychiatric condition, and is
admitted to the same hospital.
Pursuant to the MHP-State contract and MMCD 00-01
and APL 13-021, if the patient meets the medical necessity
criteria for MHP coverage, the MHP should be responsible
for the care rendered to this patient as an emergency
admission. The emergency charges are likely to be
incorporated into the reimbursement for the inpatient stay.
However, the MCP may be responsible for professional
services not rendered by a mental health specialist
when required for the emergency services and care of
the member.
MHPs may take the position that specific notice is required
in order for emergency admissions to be reimbursable
[California Code of Regulations, Title 9, Section 1820.225].
Non-contract hospitals with psychiatric lines of service
should familiarize themselves with the expectations of their
counties. Even if the requirements imposed by a county
may not be legally valid (e.g., some of these requirements
may constitute non-quantitative limitations in violation of
the mental health parity law [42 U.S.C. Section 300gg]),
compliance with the MHP expectations will remove a
potential obstacle to claim payment.
If the patient does not have a diagnosis listed in Appendix
MH 9-A, “Medical Necessity for MHP Coverage,” the
hospital should consult its legal counsel to pursue payment
options for the services rendered.
Scenarios 5.a, 5.b.1 and 5.b.2: Patient presents to
the ED of a hospital that does not provide inpatient
psychiatric services. The patient has suicidal ideation
with a specific plan. The patient is determined by
the ED physician or other professional to have an
emergency psychiatric condition and is transferred
to a hospital that provides inpatient psychiatric
services, with the expectation of an admission.
5.a. Sending hospital. Pursuant to the MMCD 00-01, the
MCP may be responsible for facility charges incurred by the
sending hospital. However, because the patient’s condition
may have required a psychiatric admission and because
the service was “for an emergency psychiatric condition,”
the MHP may also be responsible for the facility charges for
services rendered by the sending hospital to the extent that
the patient meets the medical necessity criteria. Hospitals
may wish to consult their contracts with their local MHP or
MCP (if applicable) or the MOU between their local MHP
and MCP for further clarification.
With respect to professional services, the MHP is
responsible for professional services of mental health
specialists provided in the ED to patients meeting MHP
medical necessity criteria or required to assess whether
MHP criteria are met.
34
The MCP is likely responsible for
other professional charges, including professional services
not provided by mental health specialists and services
provided by mental health specialists to patients who do
not meet the medical necessity criteria.
5.b.1. Receiving hospital that admits the patient.
Pursuant to the MHP-State contract and MMCD 00-01
and APL 13-021, the MHP is responsible for the inpatient
psychiatric services rendered if the patient meets medical
necessity criteria. The MCP continues to have responsibility
for professional services necessary to meet the physical
needs of the patient while admitted at the receiving
hospital.
35
To the extent that the patient does not have a
diagnosis listed in Appendix MH 9-A, “Medical Necessity
for MHP Coverage,” but requires inpatient psychiatric care,
the hospital may wish to consult its legal counsel to pursue
payment options for the services rendered.
Receiving hospital that does not admit the patient. In
some instances, the receiving hospital will determine that
the patient does not require inpatient psychiatric care. In
these cases, the payment responsibility for the services
rendered by the receiving hospital should follow the
rationale set forth in Scenarios 1 and 2.
34 MMCD 00-01.
35 Ibid.

1-1
S
Consent to Surgery or Special Procedure*
1-2
S
Informed Consent to Surgery or Special
Procedure*
2-1
S
Self-Sufficient Minor Information
2-2
S
Caregiver’s Authorization Affidavit
2-3
S
Authorization for Third Party to Consent to
Treatment of Minor Lacking Capacity to Consent
2-A Decision Makers for Medical Treatment of Adults
2-B Consent Requirements for Medical Treatment of
Minors*
2-D Health Care Decisions for Unrepresented Patients
2-E Considerations for Revising the Hospital’s Policy
and Procedure Regarding Decision Making for
Unrepresented Patients
4-7
S
Consent to Receive Antipsychotic Medications
8-1
S
Conditions of Admission
MH 9-A Medical Necessity for MHP Coverage
MH 9-B Types of MCPs and MHPs
MH 9-C Pertinent DHCS Plan Letters
MH 9-D DHCS Chart: Medi-Cal Mental Health Services
MH 9-E Pertinent Legal Definitions of Emergency
Psychiatric Conditions
12-1
S
Request for Voluntary Admission and Authorization
for Treatment
12-2 Statement of Professional Person Responsible for
Minor’s Admission
12-3
S
Notice to Minors
12-4 Certification of Admitting Physician
12-5 Application for Involuntary Admission — Inebriates
12-6
S
Notice of Certification for Intensive Treatment
12-7
S
Advisement of Rights — Involuntary Patient
12-8
S
Leave of Absence from Psychiatric Service
12-9
S
Request for Release From Involuntary Treatment
12-10
S
Notice of Certification for Second Involuntary
14-Day Period for Intensive Treatment — Suicidal
Patient
12-11 Petition for Postcertification Treatment of
Imminently Dangerous Person
12-12 Detention of Patient With Psychiatric Emergency in
a Nondesignated Health Facility (Health and Safety
Code Section 1799.111)
12-A Summary of Lanterman-Petris-Short Act’s
Provision for Involuntary Evaluation and Treatment
and Right of Review
13-3
S
Aftercare Plan
13-4 Notice to Law Enforcement Agency: Release of
Person From Hospital From Whom a Firearm or
Other Deadly Weapon Was Confiscated
13-5
S
Notice to Patient: Procedure for Return of
Confiscated Weapon(s)
16-1
S
Authorization for Use or Disclosure of Health
Information*
16-2
S
Request to Withhold Public Release of Information
19-2 Employee Acknowledgment of Child Abuse and
Neglect Reporting Obligations
19-4 Employee Acknowledgment of Elder and
Dependent Adult Abuse Reporting Obligations
19-A Assault and Abuse Reporting Requirements
20-1 Adverse Event Report Form — Sample
21-1 Incident Report
21-2 Report to Attorney
23-1
S
Consent for the HIV Test
25-A Report of a Hospital Death Associated With
Restraint or Seclusion
These documents are provided in English in the back of the manual. All forms, including Spanish versions, when available,
can be found online for CHA members at www.calhospital.org/free-resources. “S” denotes that the form is provided in
English and Spanish.
List of Forms and Appendices
* Indicates forms that are new or revised in this edition.

(03/19)
Page 1 of 4
©CALIFORNIA HOSPITAL ASSOCIATION
FORM 1-1
Consent to Surgery or Special Procedure
1. Your doctors have recommended the following operation or procedure:
and the following type of anesthesia:
Upon your authorization and consent, this operation or procedure, together with any different
or further procedures which, in the opinion of the doctor(s) performing the procedure, may
be indicated due to an emergency or newly-discovered information, will be performed on
you. The operations or procedures will be performed by the doctor named below (or in
the event the doctor is unable to perform or complete the procedure, a qualified substitute
doctor), together with associates and assistants, including anesthesiologists, pathologists,
and radiologists from the medical staff of (name of hospital)
to whom the doctor(s) performing
the procedure may assign designated responsibilities.
2. Name of the practitioner who is performing the procedure or administering the medical
treatment
1
:
The hospital maintains personnel and facilities to assist your doctors in their performance of
various surgical operations and other special diagnostic or therapeutic procedures. However,
your doctors, surgeons, and the persons in attendance for the purpose of performing
specialized medical services such as anesthesia, radiology, or pathology are not employees,
representatives or agents of the hospital or of doctor(s) performing the procedure. They are
independent medical practitioners.
3. All operations and procedures carry the risk of unsuccessful results, complications, injury, or
even death, from both known and unforeseen causes, and no warranty or guarantee is made
as to result or cure. You have the right to be informed of:
• The nature of the operation or procedure, including other care, treatment or medications;
• Potential benefits, risks or side effects of the operation or procedure, including potential
problems that might occur with the anesthesia to be used and during recuperation;
• The likelihood of achieving treatment goals;
• Reasonable alternatives and the relevant risks, benefits and side effects related to such
alternatives, including the possible results of not receiving care or treatment; and
• Any independent medical research or significant economic interests your doctor may
have related to the performance of the proposed operation or procedure.
Except in cases of emergency, operations or procedures are not performed until you have
had the opportunity to receive this information and have given your consent. You have the
right to give or refuse consent to any proposed operation or procedure at any time prior to its
performance.
1 CMS recommends that consent forms state, if applicable, that physicians other than the operating practitioner, including but not limited to
residents, will be performing important tasks related to the surgery, in accordance with the hospital’s policies (and, in the case of residents,
based on their skill set and under the supervision of the responsible practitioner) and that qualified medical practitioners who are not physicians
will perform important parts of the surgery or administration of anesthesia within their scope of practice, as determined under state law, and for
which they have been granted privileges by the hospital.

Form 1-1 Consent to Surgery or Special Procedure
Page 2 of 4
(03/19)
©CALIFORNIA HOSPITAL ASSOCIATION
4. If your doctor determines that there is a reasonable possibility that you may need a blood
transfusion as a result of the surgery or procedure to which you are consenting, your doctor
will inform you of this and will provide you with information concerning the benefits and risks
of the various options for blood transfusion, including predonation by yourself or others. You
also have the right to have adequate time before your procedure to arrange for predonation,
but you can waive this right if you do not wish to wait.
Transfusion of blood or blood products involves certain risks, including the transmission of
disease such as hepatitis or Human Immunodeficiency Virus (HIV), and you have a right to
consent or refuse consent to any transfusion. You should discuss any questions that you may
have about transfusions with your doctor.
5. By your signature below, you authorize the pathologist to use his or her discretion in
disposition or use of any cells, tissue, body part, hardware or foreign object removed from
your person during the operation or procedure set forth above, subject to the following
conditions (if any):
6. Your signature on this form indicates that:
• You have read and understand the information provided in this form;
• Your doctor has adequately explained to you the operation or procedure and the
anesthesia set forth above, along with the risks, benefits, and alternatives, and the other
information described above in this form;
• You have had a chance to ask your doctors questions;
• You have received all of the information you desire concerning the operation or
procedure and the anesthesia; and
• You authorize and consent to the performance of the operation or procedure and the
anesthesia.
Date:
Time: AM / PM
Signature:
(patient/legal representative)
If signed by someone other than patient, indicate relationship:
Print name:
(legal representative)

Form 1-1 Consent to Surgery or Special Procedure
(03/19)
Page 3 of 4
©CALIFORNIA HOSPITAL ASSOCIATION
Physician Certification
2
I, the undersigned physician, hereby certify that I have discussed the procedure described in this
consent form with this patient (or the patient’s legal representative), including:
1. The risks and benefits of the procedure;
2. Any adverse reactions that may reasonably be expected to occur;
3. Reasonable alternatives and the relevant risks, benefits and side effects related to such
alternatives, including the possible results of not receiving care or treatment;
4. The potential problems that may occur during recuperation; and
5. Any research or economic interest I may have regarding this treatment.
I understand that I am responsible for filling in all blanks in paragraphs 1. and 2. above. I further
certify that the patient was encouraged to ask questions and that all questions were answered.
Date: Time: AM / PM
Signature:
(physician)
Print name:
(legal representative)
Consent to Blood Transfusion
Your signature below indicates that:
1. You have received a copy of the brochure, A Patient’s Guide to Blood Transfusion.
2. You have received information from your doctor concerning the risks and benefits of blood
transfusion and of any alternative therapies and their risks and benefits.
3. You have had the opportunity to discuss this matter with your doctor, including predonation.
4. Subject to any special instructions listed below, you consent to such blood transfusion
as your doctor may order in connection with the operation or procedure described in this
consent form.
2 The Physician Certification is not a required element of this form, but is one way of providing for physician documentation of the consent
process. Other options include a progress note in the patient’s medical record, a note in the patient’s history and physical, or documentation
provided from the physician’s office (e.g., an informed consent form signed by both the patient and the physician). NOTE: Even if the physician
provides a copy of a consent form signed in the physician’s office, the patient should still be asked to sign the hospital’s consent form.

Form 1-1 Consent to Surgery or Special Procedure
Page 4 of 4
(03/19)
©CALIFORNIA HOSPITAL ASSOCIATION
Special Instructions:
(Describe here any specific instructions for patient’s blood transfusion, e.g., predonation, direct do-
nation, etc.)
Date: Time: AM / PM
Signature:
(patient/legal representative)
If signed by someone other than patient, indicate relationship:
Print name:
(legal representative)
Interpreter’s Statement
I have accurately and completely read the foregoing document to (patient or patient’s legal
representative) in the
patient’s or legal representative’s primary language (identify language) .
He/she understood all of the terms and conditions and acknowledged his/her agreement by signing
the document in my presence.
Date: Time: AM / PM
Signature:
(interpreter)
Print name:
(interpreter)
NOTE: This form should include taglines as required by the Affordable Care Act.
(See www.calhospital.org/taglines, for detailed information.)
Reference: CoP Interpretive Guidelines, Tags A-0466 and A-0955

(03/19)
Page 1 of 4
©CALIFORNIA HOSPITAL ASSOCIATION
FORM 1-1S
Consentimiento Para Effectuar Cirugía o
Procedimiento Especial
1. Sus doctores han recomendado la siguiente operación o procedimiento:
y el siguiente tipo de anestesia:
Trassu autorización y consentimiento, se le realizará esta operación o procedimiento,
junto con cualquier otroprocedimiento diferente o añadido que, en la opinión del médico
o médicos que realizan el procedimiento pueda estar indicadodebido a una emergencia
o nueva información. Las operaciones o procedimientos serán efectuados por el doctor o
doctores que se nombran más abajo (o en caso de que alguno de estos doctores no pueda
efectuar o completar el procedimiento, por un doctor sustituto calificado), junto a otros
asociados y asistentes, entre ellos, anestesistas, patólogos y radiólogos del cuerpo médico
(nombre del hospital) , a quienes el o los
doctores que realicen el procedimiento podrían asignar responsabilidades designadas.
2. Nombre del médico que realiza la intervención o administra el tratamiento:
El hospital mantiene personal e instalaciones para ayudar a los doctores en el desempeño
de las diferentes operaciones quirúrgicas y otros procedimientos terapéuticos o diagnósticos
especiales. No obstante, sus médicos, cirujanos y las personas que asisten con el fin de
prestar servicios médicos especializados, tales como anestesia, radiología o patología, no
son empleados, representantes ni agentes del hospital ni del doctor o doctores que realizan
el procedimiento, sino que son profesionales médicos independientes.
3. Todas las operaciones y procedimientos conllevan el riesgo de resultados fallidos,
complicaciones, lesiones o incluso la muerte, tanto por causas conocidas como imprevistas,
y no se otorga ninguna garantía respecto al resultado o la curación. Usted tiene derecho a
que se le informe acerca de:
• La naturaleza de la operación o procedimiento, incluidos otros cuidados médicos,
tratamientos o medicamentos;
• Los beneficios, riesgos o efectos secundarios potenciales de la operación o
procedimiento, incluidos los problemas potenciales que podrían presentarse durante la
recuperación por la anestesia utilizada;
• Las alternativas razonables y los riesgos, beneficios y efectos secundarios pertinentes
relacionados con dichas alternativas, incluidos los posibles resultados de no recibir
atención o tratamiento, y
• Cualquier interés en investigaciones médicas independientes u otros intereses
significativos que su doctor pueda tener en relación con la realización de la operación o
procedimiento propuesto.

Page 2 of 4
(03/19)
©CALIFORNIA HOSPITAL ASSOCIATION
Form 1-1S Consent to Surgery or Special Procedure
Excepto en casos de emergencia, las operaciones y los procedimientos no se efectúan
sino hasta que usted haya tenido la oportunidad de recibir esta información y otorgar su
consentimiento. Usted tiene derecho a dar o rehusar su consentimiento para toda operación
o procedimiento que se proponga en cualquier momento, antes de que éstos se efectúen.
4. Si su doctor determina que existe la posibilidad razonable de que usted requerirá una
transfusión de sangre como resultado de la cirugía o procedimiento para el cual está
otorgando su consentimiento, se lo informará y se le proporcionará información sobre los
beneficios y los riesgos de las diversas opciones de transfusión de sangre, incluida la
donación adelantada realizada por usted u otras personas. Usted también tiene derecho
a contar con suficiente tiempo antes de su procedimiento para gestionar la donación
adelantada, pero puede renunciar a este derecho si no desea esperar.
La transfusión de sangre o derivados sanguíneos conlleva ciertos riesgos, incluyendo la
transmisión de enfermedades como la hepatitis o el virus de la inmunodeficiencia humana
(VIH), y usted tiene derecho a dar o rehusar el consentimiento para cualquier transfusión. Si
tiene preguntas sobre las transfusiones, debe consultarlas con su doctor.
5. Al firmar a continuación, usted autoriza al patólogo a hacer uso de su criterio en la
eliminación o uso de células, tejidos, partes del cuerpo, dispositivos o cuerpos extraños
extraídos de su persona durante la operación o procedimiento expuesto anteriormente,
sujeto a las siguientes condiciones (si las hubiere):
.
6. Su firma en este formulario indica que:
• Leyó y entendió la información provista en este formulario;
• Su doctor le explicó adecuadamente la operación o procedimiento y la anestesia que
se utilizará, arriba mencionados, así como los riesgos, beneficios, alternativas y la otra
información descrita en este formulario;
• Tuvo oportunidad de hacerle preguntas a sus doctores;
• Recibió toda la información que desea sobre la operación o procedimiento y la
anestesia, y
• Autoriza y otorga su consentimiento para la realización de la operación o procedimiento
y la anestesia.
Fecha:
Hora: AM / PM
Firma:
(paciente o representante legal)
Si no lo firma el paciente, indique la relación con éste:
Nombre en letra de imprenta:
(representante legal)

(03/19)
Page 3 of 4
©CALIFORNIA HOSPITAL ASSOCIATION
Form 1-1S Consent to Surgery or Special Procedure
Physician Certification
I, the undersigned physician, hereby certify that I have discussed the procedure described in this
consent form with this patient (or the patient’s legal representative), including:
• The risks and benefits of the procedure;
• Any adverse reactions that may reasonably be expected to occur;
• Reasonable alternatives and the relevant risks, benefits and side effects related to such
alternatives, including the possible results of not receiving care or treatment;
• The potential problems that may occur during recuperation;
• The likelihood of achieving treatment goals; and
• Any research or economic interest I may have regarding this treatment.
I understand that I am responsible for filling in all blanks in paragraphs 1. and 2. above. I further
certify that the patient was encouraged to ask questions and that all questions were answered.
Date:
Time: AM / PM
Signature:
(physician)
Print name:
(physician)
Consentimiento para Transfusión de Sangre
Su firma al pie indica que:
1. Recibió una copia del folleto “Guía de Transfusión de Sangre para Pacientes.”
2. Recibió información de su doctor sobre los riesgos y beneficios de las transfusiones de
sangre y de otras terapias alternativas con sus riesgos y beneficios.
3. Tuvo oportunidad de conversar con su doctor sobre este asunto, incluyendo el tema de la
donación adelantada.
4. Sujeto a las instrucciones especiales que se detallan a continuación, otorga su
consentimiento para cualquier transfusión de sangre que su doctor indique en relación con
la operación o procedimiento que se describe en este formulario de consentimiento.
Instrucciones especiales:
(Describa en este espacio cualquier instrucción específica relacionada con la transfusión de sangre
del paciente; por ejemplo, donación adelantada, donación directa, etc.)
Page 4 of 4
(03/19)
©CALIFORNIA HOSPITAL ASSOCIATION
Form 1-1S Consent to Surgery or Special Procedure
Fecha: Hora: AM / PM
Firma:
(paciente o representante legal)
Si no lo firma el paciente, indique la relación con éste:
Nombre en letra de imprenta:
(representante legal)
Interpreter’s Statement
I have accurately and completely read the foregoing document to (patient or patient’s legal
representative) in
the patient’s or legal representative’s primary language (identify language)
. He/she understood all of the terms and conditions
and acknowledged his/her agreement by signing the document in my presence.
Date: Time: AM / PM
Signature:
(interpreter)
Print name:
(interpreter)
NOTE: This form should include taglines as required by the Affordable Care Act.
(See www.calhospital.org/taglines, for detailed information.)
Reference: CoP Interpretive Guidelines, Tags A-0466 and A-0955

(03/19)
Page 1 of 4
©CALIFORNIA HOSPITAL ASSOCIATION
FORM 1-2
Informed Consent to Surgery or Special
Procedure
1. This form is called an “Informed Consent Form.” It is your doctor’s obligation to provide you
with the information you need in order to decide whether to consent to the surgery or special
procedure that your doctors have recommended. The purpose of this form is to verify that
you have received this information and have given your consent to the surgery or special
procedure recommended to you. You should read this form carefully and ask questions of
your doctors so that you understand the operation or procedure before you decide whether
or not to give your consent. If you have questions, you are encouraged and expected to ask
them before you sign this form. Your doctors are not employees or agents of the hospital.
They are independent medical practitioners.
2. Your doctors have recommended the following operation or procedure:
and
the following type of anesthesia:
Upon your authorization and consent, this operation or procedure, together with any different
or further procedures which, in the opinion of the doctor(s) performing the procedure, may
be indicated due to an emergency or newly-discovered information, will be performed on
you. The operations or procedures will be performed by the doctor named below (or, in
the event the doctor is unable to perform or complete the procedure, a qualified substitute
doctor), together with associates and assistants, including anesthesiologists, pathologists,
and radiologists from the medical staff of (name of hospital)
to whom the doctor(s) performing the procedure
may assign designated responsibilities.
3. Name of the practitioner who is performing the procedure or administering the medical
treatment
1
:
The hospital maintains personnel and facilities to assist your doctors in their performance of
various surgical operations and other special diagnostic or therapeutic procedures. However,
your doctors, surgeons and the persons in attendance for the purpose of performing
specialized medical services such as anesthesia, radiology, or pathology are not employees,
representatives or agents of the hospital or of doctor(s) performing the procedure. They are
independent medical practitioners.
4. All operations and procedures carry the risk of unsuccessful results, complications, injury or
even death, from both known and unforeseen causes, and no warranty or guarantee is made
as to result or cure. You have the right to be informed of:
• The nature of the operation or procedure, including other care, treatment or medications;
• Potential benefits, risks or side effects of the operation or procedure, including potential
problems that might occur with the anesthesia to be used and during recuperation;
1 CMS recommends that consent forms state, if applicable, that physicians other than the operating practitioner, including but not limited to
residents, will be performing important tasks related to the surgery, in accordance with the hospital’s policies (and, in the case of residents,
based on their skill set and under the supervision of the responsible practitioner) and that qualified medical practitioners who are not physicians
will perform important parts of the surgery or administration of anesthesia within their scope of practice, as determined under state law, and for
which they have been granted privileges by the hospital.

Form 1-2 — Informed Consent to Surgery or Special Procedure
Page 2 of 4
(03/19)
©CALIFORNIA HOSPITAL ASSOCIATION
• The likelihood of achieving treatment goals;
• Reasonable alternatives and the relevant risks, benefits and side effects related to such
alternatives, including the possible results of not receiving care or treatment; and
• Any independent medical research or significant economic interests your doctor may have
related to the performance of the proposed operation or procedure.
Except in cases of emergency, operations or procedures are not performed until you have
had the opportunity to receive this information and have given your consent. You have the
right to give or refuse consent to any proposed operation or procedure at any time prior to its
performance.
5. By your signature below, you authorize the pathologist to use his or her discretion in
disposition or use of any cells, tissue, body part, hardware or foreign object removed from
your person during the operation or procedure set forth above, subject to the following
conditions (if any):
6. Your doctor will discuss with you the risks and benefits of the recommended operation or
procedure, including the following (the patient’s doctor is responsible for the content of the
information provided below):
a. The nature of the operation or procedure and the anesthesia, including the surgical site
and laterality if applicable:
b. The expected benefits or effects of the operation or procedure and anesthesia:
c. The possible risks and/or complications of the operation or procedure and anesthesia,
including potential problems that might occur during recuperation include, but are not
limited to:
d. Due to the following specific medical condition(s):
, additional risks and/or
complications of the operation or procedure and anesthesia include, but are not limited
to:
e. Alternative methods of treatment, including the nature of such treatments, their expected
benefits or effects, and their possible risks and complications include:
f. Other issues discussed with the patient:
7. If your doctor determines that there is a reasonable possibility that you may need a blood
transfusion as a result of the surgery or procedure to which you are consenting, your doctor
will inform you of this and will provide you with information concerning the benefits and risks
of the various options for blood transfusion, including predonation by yourself or others. You
also have the right to have adequate time before your procedure to arrange for predonation,
but you can waive this right if you do not wish to wait.
Transfusion of blood or blood products involves certain risks, including the transmission of
disease such as hepatitis or Human Immunodeficiency Virus (HIV), and you have a right to
Form 1-2 — Informed Consent to Surgery or Special Procedure
(03/19)
Page 3 of 4
©CALIFORNIA HOSPITAL ASSOCIATION
consent or refuse consent to any transfusion. You should discuss any questions that you may
have about transfusions with your doctor.
8. Your signature on this form indicates that:
a. You have read and understand the information provided in this form;
b. Your doctor has adequately explained to you the operation or procedure and the
anesthesia set forth above, along with the risks, benefits, and the other information
described above in this form;
c. You have had a chance to ask your doctors questions;
d. You have received all of the information you desire concerning the operation or
procedure and the anesthesia; and
e. You authorize and consent to the performance of the operation or procedure and the
anesthesia.
Date:
Time: AM / PM
Signature:
(patient/legal representative)
If signed by someone other than patient, indicate name and relationship:
Print name:
(legal representative)
Physician Certification
2
I, the undersigned physician, hereby certify that I have discussed the procedure described in this
consent form with this patient (or the patient’s legal representative), including:
• The risks and benefits of the procedure;
• Any adverse reactions that may reasonably be expected to occur;
• Reasonable alternatives and the relevant risks, benefits and side effects related to such
alternatives, including the possible results of not receiving care or treatment; and
• The potential problems that may occur during recuperation; and
• Any research or economic interest I may have regarding this treatment.
I understand that I am responsible for filling in all blanks in paragraphs 2, 3 and 6. I further certify
that the patient was encouraged to ask questions and that all questions were answered.
Date:
Time: AM / PM
Signature:
(physician)
Print name:
(physician)
2 While the Physician Certification is optional for the Consent to Surgery or Special Procedure (CHA Form 1-1), CHA recommends that it be
included in this Informed Consent form containing medical information for which the physician is responsible.

Form 1-2 — Informed Consent to Surgery or Special Procedure
Page 4 of 4
(03/19)
©CALIFORNIA HOSPITAL ASSOCIATION
Consent to Blood Transfusion
Your signature below indicates that:
1. You have received a copy of the brochure, A Patient’s Guide to Blood Transfusion.
2. You have received information from your doctor concerning the risks and benefits of blood
transfusion and of any alternative therapies and their risks and benefits.
3. You have had the opportunity to discuss this matter with your doctor, including predonation.
4. Subject to any special instructions listed below, you consent to such blood transfusion
as your doctor may order in connection with the operation or procedure described in this
consent form.
Special Instructions:
(Describe here any specific instructions for patient’s blood transfusion, e.g., predonation, direct
donation, etc.)
Date: Time: AM / PM
Signature:
(patient/legal representative)
If signed by someone other than patient, indicate relationship:
Print name:
(legal representative)
Interpreter’s Statement
I have accurately and completely read the foregoing document to (patient or patient’s legal
representative)
in the patient’s or legal
representative’s primary language (identify language) . He/
she understood all of the terms and conditions and acknowledged his/her agreement by signing the
document in my presence.
Date: Time: AM / PM
Signature:
(interpreter)
Print name:
(interpreter)
NOTE: This form should include taglines as required by the Affordable Care Act.
(See www.calhospital.org/taglines, for detailed information.)
Reference: CoP Interpretive Guidelines, Tags A-0466 and A-0955

(03/19)
Page 1 of 5
©CALIFORNIA HOSPITAL ASSOCIATION
FORM 1-2S
Consentimiento Informado Para Effectuar Cirugía
o Procedimiento Especial
1. Este formulario se llama “Formulario de consentimiento informado”. Su doctor tiene
la obligación de darle toda la información necesaria para que usted pueda decidir si
quiere dar su consentimiento para la cirugía o procedimiento especial que sus doctores
le recomendaron. El propósito de este formulario es verificar que usted recibió esta
información y dio su consentimiento para la cirugía o procedimiento especial que le
recomendaron. Debe leer este formulario detenidamente y hacerle preguntas a sus
doctores para que entienda la operación o procedimiento antes de decidir si dará o no su
consentimiento. Si tiene preguntas, se le anima y se espera que las haga antes de firmar
este formulario. Sus doctores no son empleados ni agentes del hospital. Son profesionales
médicos independientes.
2. Sus doctores han recomendado la siguiente operación o procedimiento:
y el siguiente tipo de anestesia:
Trassu autorización y consentimiento, se le realizará esta operación o procedimiento,
junto con cualquier otroprocedimiento diferente o añadido que, en la opinión del médico
o médicos que realizan el procedimiento pueda estar indicadodebido a una emergencia
o nueva información. Las operaciones o procedimientos serán efectuados por el doctor o
doctores que se nombran más abajo (o en caso de que alguno de estos doctores no pueda
efectuar o completar el procedimiento, por un doctor sustituto calificado), junto a otros
asociados y asistentes, entre ellos, anestesistas, patólogos y radiólogos del cuerpo médico
(nombre del hospital) , a quienes el o los
doctores que realicen el procedimiento podrían asignar responsabilidades designadas.
3. Nombre del médico que realiza la intervención o administra el tratamiento:
El hospital mantiene personal e instalaciones para ayudar a los doctores en el desempeño
de las diferentes operaciones quirúrgicas y otros procedimientos terapéuticos o diagnósticos
especiales. No obstante, sus médicos, cirujanos y las personas que asisten con el fin de
prestar servicios médicos especializados, tales como anestesia, radiología o patología, no
son empleados, representantes ni agentes del hospital ni del doctor o doctores que realizan
el procedimiento, sino que son profesionales médicos independientes.
4. Todas las operaciones y procedimientos conllevan el riesgo de resultados fallidos,
complicaciones, lesiones o incluso la muerte, tanto por causas conocidas como imprevistas,
y no se otorga ninguna garantía respecto al resultado o la curación. Usted tiene derecho a
que se le informe acerca de:
• La naturaleza de la operación o procedimiento, incluidos otros cuidados médicos,
tratamientos o medicamentos;
• Los beneficios, riesgos o efectos secundarios potenciales de la operación o procedimiento,
incluidos los problemas potenciales que podrían presentarse durante la recuperación por
la anestesia utilizada;

Page 2 of 5
(03/19)
©CALIFORNIA HOSPITAL ASSOCIATION
Form 1-2S — Informed Consent to Surgery or Special Procedure
• La probabilidad para lograr las metas del tratamiento;
• Las alternativas razonables y los riesgos, beneficios y efectos secundarios pertinentes
relacionados con dichas alternativas, incluidos los posibles resultados de no recibir
atención o tratamiento, y
• Cualquier interés en investigaciones médicas independientes u otros intereses significativos
que su doctor pueda tener en relación con la realización de la operación o procedimiento
propuesto.
Excepto en casos de emergencia, las operaciones y los procedimientos no se efectúan
sino hasta que usted haya tenido la oportunidad de recibir esta información y otorgar su
consentimiento. Usted tiene derecho a dar o rehusar su consentimiento para toda operación
o procedimiento que se proponga en cualquier momento, antes de que éstos se efectúen.
5. Al firmar a continuación, usted autoriza al patólogo a hacer uso de su criterio en la
eliminación o uso de células, tejidos, partes del cuerpo, dispositivos o cuerpos extraños
extraídos de su persona durante la operación o procedimiento expuesto anteriormente,
sujeto a las siguientes condiciones (si las hubiere):
6. Su doctor conversará con usted sobre los riesgos y beneficios de la operación o
procedimiento recomendando, incluidos los siguientes puntos (El médico del paciente es
responsable del contenido de la información proporcionada abajo):
a. La naturaleza de la operación o procedimiento y la anestesia, incluyendo el lugar y lado
del cuerpo donde se realizará la operación, si corresponde:
b. Los beneficios o efectos esperados de la operación o procedimiento y de la anestesia:
Entre los posibles riesgos y complicaciones de la operación o procedimiento y de la
anestesia, incluyendo los problemas potenciales que podrían presentarse durante la
recuperación, están los siguientes (sin limitarse a ellos):
c. Debido a la o las siguientes afecciones médicas especiales:
otros
riesgos y complicaciones adicionales de la operación o procedimiento y de la anestesia,
incluyen, sin limitarse a ellos:
d. Entre los métodos alternativos de tratamiento, incluyendo la naturaleza de dichos
tratamientos, sus beneficios o efectos esperados y sus posibles riesgos y
complicaciones, están los siguientes:
e. Otros asuntos que se discutieron con el paciente:
7. Si su doctor determina que existe la posibilidad razonable de que usted requerirá una
transfusión de sangre como resultado de la cirugía o procedimiento para el cual está
otorgando su consentimiento, se lo informará y se le proporcionará información sobre los
beneficios y los riesgos de las diversas opciones de transfusión de sangre, incluida la

(03/19)
Page 3 of 5
©CALIFORNIA HOSPITAL ASSOCIATION
Form 1-2S — Informed Consent to Surgery or Special Procedure
donación adelantada realizada por usted u otras personas. Usted también tiene derecho
a contar con suficiente tiempo antes de su procedimiento para gestionar la donación
adelantada, pero puede renunciar a este derecho si no desea esperar.
La transfusión de sangre o derivados sanguíneos conlleva ciertos riesgos, incluyendo la
transmisión de enfermedades como la hepatitis o el virus de la inmunodeficiencia humana
(VIH), y usted tiene derecho a dar o rehusar el consentimiento para cualquier transfusión. Si
tiene preguntas sobre las transfusiones, debe consultarlas con su doctor.
8. Su firma en este formulario indica que:
• Leyó y entendió la información provista en este formulario;
• Su doctor le explicó adecuadamente la operación o procedimiento y la anestesia que
se utilizará, arriba mencionados, así como los riesgos, beneficios, alternativas y la otra
información descrita en este formulario;
• Tuvo oportunidad de hacerle preguntas a sus doctores;
• Recibió toda la información que desea sobre la operación o procedimiento y la anestesia;
y
• Autoriza y otorga su consentimiento para la realización de la operación o procedimiento y
la anestesia.
Fecha: Hora: AM / PM
Firma:
(paciente o representante legal)
Si no lo firma el paciente, indique la relación con éste:
Nombre en letra de imprenta:
(representante legal)

Page 4 of 5
(03/19)
©CALIFORNIA HOSPITAL ASSOCIATION
Form 1-2S — Informed Consent to Surgery or Special Procedure
Physician Certification
I, the undersigned physician, hereby certify that I have discussed the procedure described in this
consent form with this patient (or the patient’s legal representative), including:
• The risks and benefits of the procedure;
• Any adverse reactions that may reasonably be expected to occur;
• Reasonable alternatives and the relevant risks, benefits and side effects related to such
alternatives, including the possible results of not receiving care or treatment; and
• The potential problems that may occur during recuperation;
• The likelihood of achieving treatment goals; and
• Any research or economic interest I may have regarding this treatment.
I understand that I am responsible for filling in all blanks in paragraphs 2, 3 and 6 above. I further
certify that the patient was encouraged to ask questions and that all questions were answered.
Date:
Time: AM / PM
Signature:
(physician)
Print name:
(physician)
Consentimiento para Transfusión de Sangre
Su firma al pie indica que:
• Recibió una copia del folleto Guía de Transfusión de Sangre para Pacientes.
• Recibió información de su doctor sobre los riesgos y beneficios de las transfusiones de
sangre y de otras terapias alternativas con sus riesgos y beneficios.
• Tuvo oportunidad de conversar con su doctor sobre este asunto, incluyendo el tema de la
donación adelantada.
• Sujeto a las instrucciones especiales que se detallan a continuación, otorga su
consentimiento a cualquier transfusión de sangre que su doctor indique en relación con la
operación o procedimiento que se describe en este formulario de consentimiento.
Instrucciones especiales:
(Describa en este espacio cualquier instrucción específica relacionada con la transfusión de sangre
del paciente; por ejemplo, donación adelantada, donación directa, etc.)

(03/19)
Page 5 of 5
©CALIFORNIA HOSPITAL ASSOCIATION
Form 1-2S — Informed Consent to Surgery or Special Procedure
Fecha: Hora: AM / PM
Firma:
(paciente o representante legal)
Si no lo firma el paciente, indique la relación con éste:
Nombre en letra de imprenta:
(representante legal)
Interpreter’s Statement
I have accurately and completely read the foregoing document to (patient or patient’s legal
representative) in the
patient’s or legal representative’s primary language (identify language) . He/
she understood all of the terms and conditions and acknowledged his/her agreement by signing the
document in my presence.
Date: Time: AM / PM
Signature:
(interpreter)
Print name:
(interpreter)
NOTE: This form should include taglines as required by the Affordable Care Act.
(See www.calhospital.org/taglines, for detailed information.)
Reference: CoP Interpretive Guidelines, Tags A-0466 and A-0955
FORM 2-1
Self-Sufficient Minor Information
(03/09)
Page 1 of 1
©CALIFORNIA HOSPITAL ASSOCIATION
For the purposes of obtaining diagnosis or treatment at the (name of hospital)
or by any
physician, surgeon or dentist associated with it, the undersigned certifies the following facts are true:
1. I am 15 years of age or older, having been born on .
(insert date as mm/dd/yy)
2. I am living separate and apart from my parents or legal guardian.
(place of residence of patient) (phone)
(place of residence of parents or guardian) (phone)
3. I am managing my own financial affairs.
(place of employment)
(other source of financial support — explain)
4. I understand that I will be financially responsible for the charges for my medical, dental, or
hospital diagnosis, treatment and care and that I may not disaffirm this contract on the grounds
that I am a minor.
Date:
Time: AM / PM
Signature:
(patient)
Print name:
(patient)
Date: Time: AM / PM
Signature:
(witness)
Print name:
(witness)
NOTE: This form should include taglines as required by the Affordable Care Act.
(See www.calhospital.org/taglines, for detailed information.)
Reference: Family Code Section 6922

©CALIFORNIA HOSPITAL ASSOCIATION
(03/09)
Page 1 of 1
FORM 2-1S
Formulario de Informacion para el Menor de Edad
Autosuficiente
Con el fin de obtener un diagnóstico o tratamiento en el hospital (nombre del hospital)
o por
cualquier médico, cirujano o dentista asociado con dicho hospital, el suscrito da fe que la siguiente
información es verídica:
1. Tengo 15 años de edad o más y nací el
(escriba la fecha de la siguiente forma: mes/día/año)
2. Mi domicilio es distinto y separado del de mis padres o de mi tutor.
(domicilio del paciente) (teléfono)
(domicilio de los padres o del tutor) (teléfono)
3. Manejo mis propios asuntos financieros.
(lugar de empleo)
(otras fuentes de ayuda financeria—explique)
4. Entiendo que tendré la responsabilidad financiera de los gastos que resulten del diagnóstico,
atención y tratamiento médico, dental, o del hospital que se me proporcionen, y que no podré
negar el presente consentimiento por ser menor de edad.
Fecha:
Hora: AM / PM
Firma:
(paciente)
Nombre en letra de imprenta:
(paciente)
Fecha: Hora: AM / PM
Firma:
(testigo)
Nombre en letra de imprenta:
(testigo)
NOTE: This form should include taglines as required by the Affordable Care Act.
(See www.calhospital.org/taglines, for detailed information.)
Reference: Family Code Section 6922

FORM 2-2
Caregiver’s Authorization Affidavit
(03/17)
Page 1 of 2
©CALIFORNIA HOSPITAL ASSOCIATION
Use of this affidavit is authorized by Part 1.5 (commencing with Section 6550) of Division 11 of the
California Family Code.
Instructions:
Completion of items 1-4, inclusive, and the signing of the affidavit is sufficient to authorize
enrollment of a minor in school and authorize school-related medical care. School-related medical
care means medical care that is required by state or local governmental authority as a condition
for school enrollment, including immunizations, physical exams and medical exams conducted in
schools. Completion of items 5-8, inclusive, is additionally required to authorize any other medical
care. Please print clearly.
□ I am requesting enrollment of the minor in school and to authorize school-related medical care.
Completion of items 1-4 only is required.
□ I am requesting to authorize medical care not school-related. Completion of items 1-8 is required.
The minor named below lives in my home, and I am 18 years of age or older.
1. Name of minor:
2. Minor’s birth date:
3. My name (adult giving authorization):
4. My home address:
5. I am a grandparent, aunt, uncle, or other qualified relative of the minor (see back of this form for
a definition of “qualified relative”).
6. Check one or both (for example, if one parent was advised and the other cannot be located):
□ I have advised the parent(s) or other person(s) having legal custody of the minor of my intent
to authorize medical care, and have received no objection.
□ I am unable to contact the parent(s) or other person(s) having legal custody of the minor at
this time, to notify them of my intended authorization.
7. My date of birth:
8. My California driver’s license or ID card number:
WARNING: DO NOT SIGN THIS FORM IF ANY OF THE STATEMENTS ABOVE ARE
INCORRECT, OR YOU WILL BE COMMITTING A CRIME PUNISHABLE BY A FINE,
IMPRISONMENT OR BOTH.
I declare under penalty of perjury under the laws of the State of California that the foregoing is true
and correct.
Date: Time: AM / PM
Signature:
(legal representative)
Print name:
(legal representative)

Form 2-2 Caregiver’s Authorization Affidavit
Page 2 of 2
(03/17)
©CALIFORNIA HOSPITAL ASSOCIATION
Please NOTE:
• This declaration does not affect the rights of the minor’s parents or legal guardian regarding
the care, custody, and control of the minor, and does not mean that the caregiver has legal
custody of the minor.
• A person who relies on this affidavit has no obligation to make any further inquiry or investigation.
IMPORTANT INFORMATION
To Caregivers
“Qualified relative,” for purposes of item 5, means a spouse, parent, stepparent, brother, sister,
stepbrother, stepsister, half-brother, half-sister, uncle, aunt, niece, nephew, first cousin, or any person
denoted by the prefix “grand” or “great,” or the spouse of any of the persons specified in this
definition, even after the marriage has been terminated by death or dissolution.
The law may require you, if you are not a relative or currently licensed, certified, or approved foster
parent, to obtain resource family approval pursuant to Health and Safety Code Section 1517
or Welfare and Institutions Code Section 16519.5 in order to care for a minor. If you have any
questions, please contact your local department of social services.
If the minor stops living with you, you are required to notify any school, health care provider, or
health care service plan to which you have given this affidavit. The affidavit is invalid after the
school, health care provider or health care service plan receives notice that the minor no longer
lives with you.
If you do not have the information requested in item 8 (California driver license or identification
card), provide another form of identification such as your social security number or Medi-Cal
number.
To School Officials
Section 48204(a)(5) of the Education Code provides that this affidavit constitutes a sufficient basis
for determination of residency of the minor, without the requirement of a guardianship or other
custody order, unless the school district determines from actual facts that the minor is not living with
the caregiver.
The school district may require additional reasonable evidence that the caregiver lives at the
address provided in item 4.
To Health Care Providers and Health Care Service Plans
A person who acts in good faith reliance upon a Caregiver’s Authorization Affidavit to provide
medical or dental care, without actual knowledge of facts contrary to those stated on the affidavit,
is not subject to criminal liability or to civil liability to any person, and is not subject to professional
disciplinary action, for that reliance if the applicable portions of the form are completed.
This affidavit does not mean that the minor is automatically a dependent for health care coverage
purposes.
NOTE: This form should include taglines as required by the Affordable Care Act.
(See www.calhospital.org/taglines, for detailed information.)
Reference: Family Code Sections 6550 to 6552

(03/17)
Page 1 of 3
©CALIFORNIA HOSPITAL ASSOCIATION
FORM 2-2S
Declaracion Jurada de Autorizacion de una
Persona Que Cuida a un Menor de Edad
El uso de esta declaración jurada está autorizado por la Parte 1.5 (a partir de la sección 6550) de
la División 11 del Código de Familia de California.
Instrucciones:
Para autorizar la matrícula y la atención médica en la escuela de un menor de edad basta con
completar los puntos del 1 al 4 y firmar la declaración jurada. La atención médica en la escuela
se refiere a los cuidados médicos que las autoridades gubernamentales locales o estatales exigen
como condición de la matrícula escolar, incluyendo inmunizaciones, exámenes físicos y exámenes
médicos realizados en las escuelas. Para autorizar cualquier otro tipo de atención médica se deben
completar además los puntos del 5 al 8. Por favor escriba claramente en letra de molde.
□ Solicito inscripción del menor de edad en la escuela y autorizo la atención médica relacionada
con la escuela. Sólo se requiere llenar los puntos 1 a 4.
□ Solicito autorizar atención médica no relacionada con la escuela. Se requiere llenar los puntos 1
a 8.
El menor de edad nombrado a continuación reside en mi domicilio y tengo 18 años de edad o
más.
1. Nombre del menor de edad:
2. Fecha de nacimiento del menor de edad:
3. Mi nombre:(adulto que presta autorización)
4. Dirección de mi domicilio:
5. Soy abuelo, tía, tío u otro pariente calificado del menor de edad (para una definición de
“pariente calificado” sírvase consultar el dorso de este formulario).
6. Marque un casillero o ambos (por ejemplo, si le avisaron a un padre y el otro no se puede
localizar):
□ He avisado al/los padre(s) u otra(s) persona(s) con custodia legal del menor de edad de mi
intención de autorizar atención médica y no he recibido ninguna objeción.
□ No he podido ponerme en contacto con el/los padre(s) u otra(s) persona(s) con custodia
legal del menor de edad en el presente para notificarles que propongo prestar autorización.
7. Mi fecha de nacimiento:
8. El número de mi licencia de conducir o tarjeta de identificación de California:

Page 2 of 3
(03/17)
©CALIFORNIA HOSPITAL ASSOCIATION
Form 2-2S Caregiver’s Authorization Affidavit
ADVERTENCIA: NO FIRME ESTE FORMULARIO SI ALGUNA DE LAS DECLARACIO-
NES QUE ANTECEDEN SEA INCORRECTA O SI ESTARÁ COMETIENDO UN DELITO
SUJETO A MULTAS, ENCARCELAMIENTO O AMBOS
Declaro bajo pena de perjurio bajo las leyes del Estado de California que lo que antecede es
verdadero y correcto.
Fecha: Hora: AM / PM
Firma:
(representante legal)
Nombre en letra de imprenta:
(representante legal)
Sírvase NOTAR :
• Esta declaración no afecta los derechos de los padres o tutores legales del menor de edad
acerca del cuidado, custodia y control del menor, y no significa que el que cuida a dicho
menor de edad tenga custodia legal del menor de edad.
• Una persona que se base en esta declaración jurada no tiene ninguna obligación de realizar
ninguna otra averiguación o investigación.
INFORMACION IMPORTANTE
A los Que Cuidan a Menores de Edad
Para los objetivos del punto 5, “familiar calificado” significa un cónyuge, padre, padrastro, hermano,
hermana, hermanastro, hermanastra, medio hermano, media hermana, tío, tía, sobrina, sobrino,
primo hermano, abuelo, abuelo, bisabuelo, bisabuela o el cónyuge de las personas especificadas
en esta definición, incluso después de que el matrimonio haya finalizado a causa de fallecimiento o
disolución.
Si usted no es pariente o actualmente padre de crianza con licencia, certificado o aprobado,
la ley puede requerir que obtenga la aprobación de recursos familiar en virtud del Código de
Salud y Seguridad de California, seccion 1517 o el Código de Bienestar e Instituciones, sección
16519.5 para poder cuidar de un menor de edad. Si tiene preguntas, póngase en contacto con su
departamento local de servicios sociales.
Si el menor deja de vivir con usted, usted debe notificar a la escuela, proveedor de atención
médica o plan de servicios médicos a los que les haya entregado esta declaración jurada. La
declaración jurada expirará en cuanto la escuela, proveedor de atención médica o plan de servicios
médicos reciba notificación de que el menor ya no reside con usted.
Si no tiene la información requerida en el punto 8 (licencia de conducir o tarjeta de identificación
de California), provea alguna otra forma de identificación, como su número del Seguro Social o de
Medi-Cal.

(03/17)
Page 3 of 3
©CALIFORNIA HOSPITAL ASSOCIATION
Form 2-2S Caregiver’s Authorization Affidavit
A Los Funcionarios de las Escuelas
La Sección 48204 del Código de Educación estipula que esta declaración jurada constituya un
fundamento suficiente para determinar la residencia del menor de edad, sin el requisito de una
orden de tutela o de algún otro orden de custodia, a menos que el distrito escolar determine
mediante hechos concretos que el menor no está viviendo con la persona que lo cuida.
El distrito escolar podrá requerir pruebas adicionales razonables de que la persona que cuida al
menor de edad vive en la dirección provista en el punto 4.
A los Proveedores de Servicios de Salud y a los Planes de Servicios de Atencion de la
Salud
Una persona que actúe de buena fe con base en una Declaración Jurada de Autorización del
Encargado del Menor y proporcione atención médica o dental sin tener conocimiento real de
hechos contrarios a los que establece la declaración jurada no estará sujeta a cargos penales ni
civiles por ningún tercero, ni tampoco estará sujeta a acciones disciplinarias profesionales por sus
actos si todas las partes aplicables del formulario se completan.
Esta declaración jurada no significa que el menor de edad es automáticamente un dependiente
para fines de la cobertura de la atención de la salud.
NOTE: This form should include taglines as required by the Affordable Care Act.
(See www.calhospital.org/taglines, for detailed information.)
Reference: Family Code Sections 6550 to 6552

(03/09)
Page 1 of 2
©CALIFORNIA HOSPITAL ASSOCIATION
FORM 2-3
Authorization for Third Party to Consent to
Treatment of Minor Lacking Capacity to Consent
I am the □Parent
□ Guardian
□ Other person having legal custody
(describe legal relationship)
of (name of minor) , a minor.
I hereby authorize (name of agent) , to act as
my agent to consent to any X-ray examination, anesthetic, medical, surgical or dental diagnosis
or treatment, and hospital care which is recommended by, and to be rendered under the general
or special supervision of, any licensed doctor or dentist, whether such diagnosis or treatment is
rendered at the doctor’s office or at a hospital.
I understand that this authorization is given in advance of any specific diagnosis, treatment, or
hospital care being required, but is given to provide authority to the above-named agent to give
consent to any and all such diagnosis, treatment, or hospital care which a licensed doctor or dentist
recommends.
This authorization is given pursuant to the provisions of Family Code Section 6910.
I hereby authorize any hospital providing treatment to the above-named minor pursuant to the
provisions of Family Code Section 6910 to surrender physical custody of the minor to the above-
named agent upon the completion of treatment. This authorization is given pursuant to Health and
Safety Code Section 1283.
These authorizations shall remain effective until (month and day) ,
20 , unless sooner revoked in writing delivered to the agent named above.
Date:
Time: AM / PM
Signature:
Print name:
(over)

Form 2-3 Authorization for Third Party to Consent to Treatment of Minor Lacking Capacity to Consent
Page 2 of 2
(03/09)
©CALIFORNIA HOSPITAL ASSOCIATION
Medically Relevant Information
Minor’s Name:
Minor’s date of birth:
Allergies to drugs or food:
Conditions for which minor is currently being treated:
Current medications:
Restrictions on activity:
Primary care physician (name and telephone number):
Insurance Company:
Mother’s name:
Mother’s address:
Mother’s telephone numbers:
(work) (home) (other)
Father’s name:
Father’s address:
Father’s telephone numbers:
(work) (home) (other)
NOTE: This form should include taglines as required by the Affordable Care Act.
(See www.calhospital.org/taglines, for detailed information.)

(03/09)
Page 1 of 2
©CALIFORNIA HOSPITAL ASSOCIATION
FORM 2-3S
Autorización para que un Tercero Pueda dar su
Consentimiento al Tratamiento de un Menor de
Edad
Yo soy □ El padre o la madre
□ El tutor
□ Otra persona que tiene la custodia legal
(describa la relación legal)
de (nombre del menor) , menor de edad.
Por medio del presente autorizo a (nombre del representante) , a
actuar como mi representante y dar consentimiento para todo estudio de radiografías, diagnóstico
o tratamiento anestésico, médico, quirúrgico o dental y atención hospitalaria que sea recomendada
por cualquier médico o dentista con licencia quien prestará supervisión general o especial del
mismo, ya sea que dicho diagnóstico o tratamiento se brinde en el consultorio del médico o en un
hospital.
Entiendo que esta autorización se otorga antes de cualquier diagnóstico, tratamiento o atención
hospitalaria que se requiera, pero se otorga a fin de dar autoridad al representante nombrado
anteriormente a dar consentimiento para todo y cualquiera de dichos diagnósticos, tratamientos u
atención hospitalaria que recomiende un médico o dentista con licencia.
Esta autorización se otorga en conformidad con las disposiciones del Artículo 6910 del Código de
Familia.
Por medio del presente autorizo a todo hospital que brinde tratamiento al menor de edad
nombrado anteriormente en conformidad con las disposiciones del Artículo 6910 del Código de
Familia a entregar la custodia física del menor al representante nombrado anteriormente al finalizar
el tratamiento. Esta autorización se otorga en conformidad con el Artículo 1283 del Código de
Salud y Seguridad.
Estas autorizaciones tendrán vigencia hasta (mes y día) del 20
a menos que sea antes revocada por escrito entregada al representante nombrado anteriormente.
Fecha: Hora: AM / PM
Firma:
Nombre en letra de imprenta:
(sobre)

Page 2 of 2
(03/09)
©CALIFORNIA HOSPITAL ASSOCIATION
Form 2-3S Authorization for Third Party to Consent to Treatment of Minor Lacking Capacity to Consent
Informacíon Médica Pertinente
Nombre del menor:
Fecha de nacimiento del menor:
Alergias a medicamentos o alimentos:
Padecimientos por los cuales el menor está recibiendo tratamiento:
Medicamentos actuales:
Restricciones de las actividades:
Médico de atención primaria (nombre y teléfono):
Compañía de seguros:
Nombre de la madre:
Dirección de la madre:
Teléfonos de la madre:
(trabajo) (casa) (otro)
Nombre del padre:
Dirección del padre:
Teléfonos del padre:
(trabajo) (casa) (otro)
NOTE: This form should include taglines as required by the Affordable Care Act.
(See www.calhospital.org/taglines, for detailed information.)

Appendix 2-A Decision Makers for Medical Treatment of Adults
(03/17)
Page 1 of 1
©CALIFORNIA HOSPITAL ASSOCIATION

Appendix 2-B Consent Requirements for Medical Treatment of Minors
(01/19)
Page 1 of 1
©CALIFORNIA HOSPITAL ASSOCIATION

APPENDIX 2-D
Health Care Decisions for Unrepresented Patients
(03/18)
Page 1 of 8
©CALIFORNIA HOSPITAL ASSOCIATION
Model Policy for General Acute Care Hospitals
The purpose of this policy is to provide a process for making ethically and medically appropriate
treatment decisions on behalf of persons who lack health care decision-making capacity and for
whom there is no surrogate decision maker.
Preamble
This policy guides health care professionals through a process to make medical treatment decisions
on behalf of an incapacitated patient who lacks a surrogate decision maker and when there is no
known family member who is willing and able to make medical treatment decisions on behalf of the
patient. Despite their incapacity, such “unrepresented” patients are entitled to have ethically and
medically appropriate medical decisions made on their behalf and to have these decisions made in
their best interest. The process set forth in this policy is intended to meet these goals. This policy
is considered necessary since no clear- cut legal guidelines exist that cover these circumstances.
This policy is designed to provide uniformity and consistency within the institutional setting of
California’s general acute care hospitals
1
on the process to make medical treatment decisions for
unrepresented patients.
Decisions made without clear knowledge of an unrepresented patient’s specific treatment
preferences must be made in the patient’s best interest, taking into consideration the patient’s
personal history, values and beliefs to the extent that these are known. Decisions about treatment
should be based on sound medical advice and should be made without the influence of material
conflicts of interest. These decisions must be made with a focus on the patient’s interests, and
not the interests of providers, the institutions, or other affected parties. In this regard, appropriate
health care decisions include both the provision of needed medical treatment and the avoidance
of nonbeneficial or excessively burdensome treatment, or treatment that is medically ineffective or
contrary to generally-accepted health care standards.
2
This policy is procedural in nature and applies to most medical decisions for which informed
consent is usually required. This policy is meant to support the institution’s underlying consent
policy.
Adoption of this policy does not preclude any party from seeking judicial intervention. Appropriate
judicial remedies may include a timely court order authorizing the provision, withdrawing, or
withholding of treatment or appointment of a conservator; however, courts are not necessarily the
proper forum in which to make health care decisions.
3
When Use of This Policy is Appropriate
This policy may be used when all of the following conditions are met:
1. The patient has been determined by the primary physician (with assistance from appropriate
consulting physicians if necessary) to lack capacity to make health care decisions. Capacity
means a patient’s ability to understand the nature and consequences of proposed health
care, including its significant benefits, risks, and alternatives, and to make and communicate

Appendix 2-D Health Care Decisions for Unrepresented Patients
Page 2 of 8
(03/18)
©CALIFORNIA HOSPITAL ASSOCIATION
a health care decision. Conditions for which psychiatric or psychological treatment may be
required do not, in and of themselves, constitute a lack of capacity to make health care
decisions.
2. No agent, conservator, or guardian has been designated to act on behalf of the patient.
3. There is no individual health care directive or instruction in the patient’s medical record or
other available sources that would eliminate the need for a surrogate decision maker.
4. No surrogate decision maker or family member can be located who is reasonably available
4
and who is willing and able to serve. Efforts to locate a surrogate should be diligent and
may include contacting the facility from which the patient was referred, and contacting public
health or social service agencies known to have provided treatment for the patient.
This policy does not address the criteria for determining and appointing an appropriate decision
maker when one or more are available and willing to serve. And finally, this policy is not meant to be
applied in emergency medical situations.
Policy
When use of this policy is appropriate (as outlined above), medical decisions will be made by a
multi- disciplinary team whose members shall include, but not be limited to, individuals directly
involved with the care of the patient. It is recommended that the multi-disciplinary team include an
attending physician, nurse familiar with the patient, social worker familiar with the patient, chair or
vice-chair of the ethics committee, non-medical (community) member of the ethics committee or
other appropriate committee and, if available and appropriate, consulting clinicians and pastoral
care staff.
5
It is very important to include on the multi-disciplinary team a person who will represent
the patient’s interests. Some patients may have a family member or friend who is unable or unwilling
to take full responsibility for making health care decisions on behalf of the patient, but who is
willing to serve as part of this team. If no such person exists, the hospital may consider including
an ombudsman, patient advocate, bioethicist, community member, or other person whose role is
to protect the patients’ interests. If it is not practicable to include such a person on the IDT in a
particular case, document the reasons therefore.
In order to determine the appropriate medical treatment for the patient, the multi-disciplinary team
should:
1. Review the diagnosis and prognosis of the patient and assure itself of the accuracy thereof.
2. Determine appropriate goals of care by weighing the following considerations:
a. Patient’s previously-expressed wishes, if any and to the extent known
b. Relief of suffering and pain
c. Preservation or improvement of function
d. Recovery of cognitive functions
e. Quality and extent of life sustained
f. Degree of intrusiveness, risk or discomfort of treatment
g. Cultural or religious beliefs, to the extent known

Appendix 2-D Health Care Decisions for Unrepresented Patients
(03/18)
Page 3 of 8
©CALIFORNIA HOSPITAL ASSOCIATION
3. Establish a care plan based upon the patient’s diagnosis and prognosis and the
determination of appropriate goals of care. The care plan should determine the appropriate
level of care, including categories or types of procedures and treatments.
4. Notify the patient that:
a. He or she has been determined incapacitated;
b. It has been determined that he or she lacks a surrogate decision maker;
c. Medical intervention has been prescribed; and
d. He or she has the opportunity to seek judicial review of the above determinations.
5. A sample notification form is attached. Health care providers should modify it to fit their
circumstances.
6. If the patient will be administered antipsychotic drugs, consider obtaining the review of an
independent physician.
7. Limit end-of-life decisions (such as withholding or withdrawing life-sustaining treatment, or
ordering hospice care) to patients who are terminally ill.
Except to the extent that such a factor is medically relevant, any medical treatment decision made
pursuant to this policy shall not be biased based on the patient’s age, sex, race, color, religion,
ancestry, national origin, disability, marital status, sexual orientation (or any other category prohibited
by law), the ability to pay for health care services, or avoidance of burden to family/others or to
society.
Under the terms of this policy, the multi-disciplinary team may make the same treatment decisions,
and will have the same limitations, as does an agent appointed pursuant to a power of attorney for
health care specified under current law.
6,7
However, this policy shall not apply to decisions pertaining
to disposition of remains, autopsies, or anatomical gifts; specific laws apply to these procedures.
8
The multi-disciplinary team must assure itself that the medical decision is made based on sound
medical advice, is in the patient’s best interest and takes into account the patient’s values, to the
extent known. In determining the best interest of the patient, it is not required that life support be
continued in all circumstances, where treatment is otherwise nonbeneficial or is medically ineffective
or contrary to generally-accepted health care standards, when the patient is terminally ill and
suffering, or where there is no reasonable expectation of the recovery of cognitive functions.
Agreement on Treatment
1. If all members of the multi-disciplinary team agree to the appropriateness of providing
treatment, it shall be provided.
2. If all members of the multi-disciplinary team agree to the appropriateness of withholding or
withdrawing treatment, it shall be withdrawn or withheld. Any implementation of a decision to
withhold or withdraw life-sustaining medical treatment will be the responsibility of the primary
treating physician.
9

Appendix 2-D Health Care Decisions for Unrepresented Patients
Page 4 of 8
(03/18)
©CALIFORNIA HOSPITAL ASSOCIATION
Disagreement on Treatment
If the members of the multi-disciplinary team disagree about the care plan, the ethics committee,
ethics resource expert(s) or other resource experts will meet with the team to explore their
disagreement and facilitate resolution.
1. If agreement is reached either to provide or to forgo treatment, the decision of the multi-
disciplinary team then becomes final.
2. If agreement still is not reached, current treatments will be continued and any other medically
necessary treatments provided, until such time that the issue is resolved through court
intervention or the disagreement is otherwise resolved.
10
Court-imposed legal remedies
should be sought only in extreme circumstances and as a last resort.
3
In all cases, appropriate pain relief and other palliative care shall be continued.
Exceptional Circumstances
Legal counsel should be consulted if a decision to withdraw or withhold treatment is likely to result
in the death of the patient and the situation arises in any of the following circumstances:
1. The patient’s condition is the result of an injury that appears to have been inflicted by a
criminal act.
2. The patient’s condition was created or aggravated by a medical incident.
3. The patient is pregnant.
4. The patient is a parent with sole custody or responsibility for support of a minor child.
Documentation
Signed, dated and timed medical record progress notes will be written for the following:
1. The findings used to conclude that the patient lacks medical decision-making capacity.
2. The finding that there is no advance health care directive, no conservator, guardian or other
available decision maker, and no health care instructions in the patient’s medical record or
other available sources.
3. The attempts made to locate surrogate decision makers and/or family members and the
results of those attempts.
4. Notification to the patient that he or she has been determined to be incapable of making
medical decisions, that there is no substitute decision maker available, the nature of the
prescribed medical intervention, and how to seek review.
5. The bases for the decision to treat the patient and/or the decision to withhold or withdraw
treatment.
6. Any information from the ethics committee or other consult, should it be convened.

Appendix 2-D Health Care Decisions for Unrepresented Patients
(03/18)
Page 5 of 8
©CALIFORNIA HOSPITAL ASSOCIATION
End Notes
1 This policy is intended for use in general acute care hospitals. California Health and Safety Code Section 1418.8 sets
forth a statutory decision-making process for patients in a skilled nursing facility or intermediate care facility.
2 California Probate Code Section 4735 states that: “A health care provider or health care institution may decline to
comply with an individual health care instruction or health care decision that requires medically ineffective health
care or health care contrary to generally accepted health care standards applicable to the health care provider or
institution.”
3 California Probate Code Section 4650(c) states that: “In the absence of controversy, a court is normally not the proper
forum in which to make health care decisions, including decisions regarding life-sustaining treatment.”
4 California Probate Code Section 4717 states that:
(a) Notwithstanding any other provision of law, within 24 hours of the arrival in the emergency department of
a general acute care hospital of a patient who is unconscious or otherwise incapable of communication, the
hospital shall make reasonable efforts to contact the patient’s agent, surrogate, or a family member or other
person the hospital reasonably believes has the authority to make health care decisions on behalf of the
patient. A hospital shall be deemed to have made reasonable efforts, and to have discharged its duty under
this section, if it does all of the following:
(1) Examines the personal effects, if any, accompanying the patient and any medical records regarding the
patient in its possession, and reviews any verbal or written report made by emergency medical technicians
or the police, to identify the name of any agent, surrogate, or a family member or other person the hospital
reasonably believes has the authority to make health care decisions on behalf of the patient.
(2) Contacts or attempts to contact any agent, surrogate, or a family member or other person the hospital
reasonably believes has the authority to make health care decisions on behalf of the patient, as identified in
paragraph (1).
(3) Contacts the Secretary of State directly or indirectly, including by voice mail or facsimile, to inquire
whether the patient has registered an advance health care directive with the Advance Health Care Directive
Registry, if the hospital finds evidence of the patient’s Advance Health Care Directive Registry identification
card either from the patient or from the patient’s family or authorized agent.
(b) The hospital shall document in the patient’s medical record all efforts made to contact any agent, surrogate,
or a family member or other person the hospital reasonably believes has the authority to make health care
decisions on behalf of the patient.
(c) Application of this section shall be suspended during any period in which the hospital implements its
disaster and mass casualty program, or its fire and internal disaster program.
5 California Probate Code Section 4736 states that:
A health care provider or health care institution that declines to comply with an individual health care instruction
or health care decision shall do all of the following: (a) Promptly so inform the patient, if possible, and any
person then authorized to make health care decisions for the patient. (b) Unless the patient or person then
authorized to make health care decisions for the patient refuses assistance, immediately make all reasonable
efforts to assist in the transfer of the patient to another health care provider or institution that is willing to comply
with the instruction or decision. (c) Provide continuing care to the patient until a transfer can be accomplished
or until it appears that a transfer cannot be accomplished. In all cases, appropriate pain relief and other
palliative care shall be continued.
Institutions should designate by policy the particular types and numbers of providers who may constitute the multi-
disciplinary team, and should ensure that non-medical/community representatives are properly prepared to serve on
the multi-disciplinary team.
6 California Probate Code Section 4617 states that:
“Health care decision” means a decision made by a patient or the patient’s agent, conservator, or surrogate,
regarding the patient’s health care, including the following: (a) Selection and discharge of health care providers
and institutions. (b) Approval or disapproval of diagnostic tests, surgical procedures, and programs of

Appendix 2-D Health Care Decisions for Unrepresented Patients
Page 6 of 8
(03/18)
©CALIFORNIA HOSPITAL ASSOCIATION
medication. (c) Directions to provide, withhold, or withdraw artificial nutrition and hydration and all other forms
of health care, including cardiopulmonary resuscitation.
California Probate Code Section 4683 states that: “Subject to any limitations in the power of attorney for health
care: (a) An agent designated in the power of attorney may make health care decisions for the principal to the same
extent the principal could make health care decisions if the principal had the capacity to do so.”
7 California Probate Code Section 4652 states that: “This division does not authorize consent to any of the following on
behalf of a patient: (a) Commitment to or placement in a mental health treatment facility. (b) Convulsive treatment (as
defined in Section 5325 of the Welfare and Institutions Code). (c) Psychosurgery (as defined in Section 5325 of the
Welfare and Institutions Code). (d) Sterilization. (e) Abortion.”
8 Health and Safety Code Sections 7100 (disposition of remains), 7113 (autopsy), and 7150 et seq. (anatomical gift).
9 California Probate Code Section 4734 states that:
(a) A health care provider may decline to comply with an individual health care instruction or health care
decision for reasons of conscience.
(b) A health care institution may decline to comply with an individual health care instruction or health care
decision if the instruction or decision is contrary to a policy of the institution that is expressly based on reasons
of conscience and if the policy was timely communicated to the patient or to a person then authorized to make
health care decisions for the patient.
10 California Probate Code Section 4736 states that:
A health care provider or health care institution that declines to comply with an individual health care instruction
or health care decision shall do all of the following: (a) Promptly so inform the patient, if possible, and any
person then authorized to make health care decisions for the patient. (b) Unless the patient or person then
authorized to make health care decisions for the patient refuses assistance, immediately make all reasonable
efforts to assist in the transfer of the patient to another health care provider or institution that is willing to comply
with the instruction or decision. (c) Provide continuing care to the patient until a transfer can be accomplished
or until it appears that a transfer cannot be accomplished. In all cases, appropriate pain relief and other
palliative care shall be continued.
Sample Notification Form for Unrepresented Patients
Patient Name:
Your doctor, Dr. , has carefully evaluated your
physical, medical and cognitive condition and concluded that you don’t have the ability to make
decisions about your medical treatment.
The hospital has tried to find a family member or friend of yours to make health care decisions for
you. The hospital hasn’t been able to find anyone to do that. If you have a family member or friend
who you want to make health care decisions for you, please tell us.
Your doctor has recommended the following treatment, believing that this is the best treatment for
you under the circumstances:

Appendix 2-D Health Care Decisions for Unrepresented Patients
(03/18)
Page 7 of 8
©CALIFORNIA HOSPITAL ASSOCIATION
A team of health care professionals, including your doctor and nurses and others, agrees that this is
the best treatment for you.
Unless your doctor receives direction otherwise, your doctor intends to proceed with this treatment.
You can ask a judge to stop this treatment. You can also ask a judge to let you make your own
health care decisions. You can contact a judge at:
[Hospital to insert contact information for local Superior Court]
Here are some people who might be able to help you contact a judge:
[Hospital to list any local resources, such as an ombudsman, law school legal assistance clinic,
Adult Protective Services, any assistance the local Superior Court offers, etc.]
Hospital Employee to Complete:
I gave a copy of this form to the above-named patient on [date] at
[time] a.m./p.m.
Signature:
Print name:
ORIGINAL TO PATIENT
COPY IN MEDICAL RECORD
NOTE: This form should include taglines as required by the Affordable Care Act.
(See www.calhospital.org/taglines, for detailed information.)

APPENDIX 2-E
Considerations for Revising the Hospital’s Policy
and Procedure Regarding Decision Making for
Unrepresented Patients
(03/18)
Page 1 of 2
©CALIFORNIA HOSPITAL ASSOCIATION
Hospitals that have adopted the CMA/CHA/Alliance model policy, “Health Care Decisions for
Unrepresented Patients,” may wish to revise their policy & procedure to address the deficiencies
in state law identified in the recent Superior Court case, California Advocates for Nursing Home
Reform v. Chapman. Hospitals may wish to consider the suggestions outlined below.
□ 1. Your policy should require that the hospital or physician notify the patient that:
a. He or she has been determined incapacitated;
b. It has been determined that he or she lacks a surrogate decision maker;
c. Medical intervention has been prescribed; and
d. He or she has the opportunity to seek judicial review of the above determinations.
The hospital may wish to develop a notification form to give to the patient (see the sample
form at the end of the revised CMA/CHA Alliance Model Policy). A copy of the form can
be put in the medical record to document that notice was given. This form should include
the name of the physician who determined that the patient lacks capacity to make health
care decisions, confirmation that the information identified in a. through d. was provided,
and the type of treatment that the physician has recommended. The form may also include
the address of the county Superior Court and contact information for any resources that
might assist the patient if he or she wishes to contest the determinations. Resources might
include a local ombudsman, law school legal assistance clinic, Adult Protective Services, any
assistance the local Superior Court offers, etc.
The notification should be given to the patient sufficiently in advance of treatment to allow
the patient to contest the determinations, to the extent possible. If it is inadvisable to delay
treatment, this fact should be documented. How far in advance of treatment a patient should
be notified will depend upon what is reasonable given all the facts and circumstances. There
is no one-size-fits-all answer to this question. (Remember that the law implies consent in
emergency situations, and this notification process is thus not required in emergencies.)
If the patient does not speak English sufficiently well to understand the form, an interpreter
should be used. If the patient has impaired vision, appropriate auxiliary aids should be used.
If a patient is comatose, in a persistent vegetative state, or otherwise so obviously unable to
comprehend this information, these circumstances should be documented.
(continued on next page)

Appendix 2-E Considerations for Revising the Hospital’s Policy and Procedure Regarding Decision Making for Unrepresented Patients
Page 2 of 2
(03/18)
©CALIFORNIA HOSPITAL ASSOCIATION
□ 2. Include a patient representative on the hospital’s interdisciplinary team (IDT), when
practicable.
Some patients may have a family member or friend who is unable or unwilling to take full
responsibility for making health care decisions on behalf of the patient, but who is willing to
serve as part of the IDT. If no such person exists, the hospital may consider including on the
IDT an ombudsman, patient advocate, bioethicist, community member, or other person whose
role is to protect the patients’ interests.
If it is not practicable to include such a person on the IDT in a particular case, document the
reasons therefore.
□ 3. If the patient will be administered antipsychotic drugs, consider obtaining the review of an
independent physician. There is no legal definition of “independent” — it is unclear whether
the court meant that the second physician should be independent from the hospital, or
from the prescribing physician, or both. Hospitals that choose to adopt a policy for
independent review should make their best efforts to secure a physician that seems
independent to a reasonable judge or jury.
□ 4. Limit end of life decisions (such as withholding or withdrawing life-sustaining treatment, or
ordering hospice care) to patients who are terminally ill.
□ 5. The hospital’s policy should clearly state that the patient’s wishes will be taken into account
when making health care decisions, to the extent those wishes are known.
□ 6. Consider obtaining the review of an independent physician in difficult cases.

FORM 4-7
Consent to Receive Antipsychotic Medications
(03/08)
Page 1 of 2
©CALIFORNIA HOSPITAL ASSOCIATION
To:
(name of patient)
Your attending physician, (physician name) , has
recommended that you be treated with this antipsychotic medication:
The hospital needs to maintain a written record of your decision to consent to the administration
of this medication. You may be treated with antipsychotic medications only after you have been
informed of your right to accept or refuse such medications. In order to allow you to make an
informed decision, you must be provided with sufficient information by the physician prescribing
such medications, which must include the following:
1. The nature of your mental condition;
2. The reasons for your taking the medication, including the likelihood of your improving or not
improving without such medication;
3. The reasonable alternative treatments available, if any;
4. The name and type, range of frequency of administration, range of dosage amount (including
use of PRN or “as needed” order), method of administration (oral or injection), and duration
of taking the medications;
5. The probable side effects of these drugs known to commonly occur, and any particular side
effects likely to occur in your particular case;
6. The possible additional side effects which may occur if you take such medication longer than
three months. You should have been advised that such side effects may include persistent
involuntary movement of the face or mouth or might at times include similar movement of
the hands and feet, and that these symptoms of tardive dyskinesia are potentially irreversible
and may appear after medications have been discontinued (your doctor will tell you if this
possible side effect does not apply to the medication recommended for you).
7. You may refuse the medication. If you consent, you may withdraw it at any time by your
stating such intention to any member of the treating staff.
Your physician is not the employee or agent of the hospital. He or she is an independent medical
practitioner.
Your signature below constitutes your acknowledgment: (1) that you have read and agree to the
foregoing; (2) that the medications listed above have been adequately explained and/or discussed
with you by your supervising physician, and that you have received all of the information you
desire concerning such medication and treatment; and (3) that you authorize and consent to the
administration of such medications and treatment.
(over)

Form 4-7 Consent to Receive Antipsychotic Medications
Page 2 of 2
(03/08)
©CALIFORNIA HOSPITAL ASSOCIATION
Date: Time: AM / PM
Signature:
(patient/legal representative)
If signed by someone other than patient, indicate relationship:
Print name:
(legal representative)
Notations by physicians (if applicable):
NOTE: This form should include taglines as required by the Affordable Care Act.
(See www.calhospital.org/taglines, for detailed information.)
Reference: Title 9, California Code of Regulations, Sections 850-856

(03/08)
Page 1 of 2
©CALIFORNIA HOSPITAL ASSOCIATION
FORM 4-7S
Consentimiento para Recibir Medicamentos
Antipsicóticos
Para:
(nombre del/de la paciente)
El médico que lo/la atiende (nombre del médico) , ha
recomendado que usted reciba tratamiento con esta medicación antipsicótica:
El hospital debe mantener un registro escrito de su decisión de autorizar la administración de
este medicamento. Puede recibir tratamiento con los medicamentos antipsicóticos únicamente
después de que se le haya informado acerca de su derecho de aceptar o rechazar estos
medicamentos. Para permitirle que tome una decisión informada, el médico que le receta estos
medicamentos debe brindarle toda la información necesaria, la cual debe incluir lo siguiente:
1. La naturaleza de su enfermedad mental;
2. Los motivos por los cuales debe tomar los medicamentos, incluso la posibilidad de
presentar una mejora o no sin estos medicamentos;
3. Los tratamientos alternativos razonables disponibles, si los hubiera;
4. El nombre y tipo de medicamento, la frecuencia de la administración, cantidad de dosis
(incluido el uso de un pedido “según sea necesario” o PRN), método de administración (por
vía oral o inyectable) y duración del tratamiento con el medicamento;
5. Los posibles efectos secundarios que habitualmente se presentan con estos medicamentos
y cualquier otro efecto secundario que pueda presentarse en su caso en particular;
6. Los posibles efectos secundarios adicionales que pueden presentarse si toma este
medicamento por más de tres meses. Es importante que le hayan informado que tales
efectos secundarios pueden incluir: movimiento involuntario persistente en el rostro o
en la boca o, en ocasiones, puede incluir movimientos similares en las manos y pies.
También se le debe haber informado que estos síntomas de discinesia tardía posiblemente
sean irreversibles y que pueden aparecer después de haber suspendido el tratamiento
con el medicamento (su médico le dirá si este posible efecto secundario no se aplica al
medicamento que le recomendaron).
7. Puede negarse a recibir el medicamento. Si da su consentimiento, puede retirarlo en
cualquier momento. Para ello, debe avisarle a cualquier miembro del personal que lo
atiende.
Su médico no es empleado o agente del hospital. Es un profesional de la salud independiente
Su firma a continuación confirma lo siguiente: (1) que leyó y está de acuerdo con lo que se
menciona anteriormente; (2) que el médico que lo supervisa le explicó de manera adecuada
todo sobre los medicamentos que se mencionan anteriormente, y que recibió toda la información
relacionada con dicho medicamento y el tratamiento; y (3) que autorizó y dio su consentimiento
para la administración de estos medicamentos y para el tratamiento.
(sobre)

Page 2 of 2
(03/08)
©CALIFORNIA HOSPITAL ASSOCIATION
Form 4-7S Consent to Receive Antipsychotic Medications
Fecha: Hora: AM / PM
Firma:
(paciente/representante legal)
Si no lo firma el paciente, indique la relación con éste:
Nombre en letra de imprenta:
(representante legal)
Anotaciones del médico (si corresponde):
NOTE: This form should include taglines as required by the Affordable Care Act.
(See www.calhospital.org/taglines, for detailed information.)
Reference: Title 9, California Code of Regulations, Sections 850-856

FORM 8-1
Conditions of Admission
(03/13)
Page 1 of 4
©CALIFORNIA HOSPITAL ASSOCIATION
Patient’s Name:
Consent to Medical and Surgical Procedures
I consent to the procedures that may be performed during this hospitalization or while I am an
outpatient. These may include, but are not limited to, emergency treatment or services, laboratory
procedures, X-ray examinations, medical or surgical treatment or procedures, telehealth services,
anesthesia, or hospital services provided to me under the general and special instructions of my
physician or surgeon. I understand that the practice of medicine and surgery is not an exact science
and that diagnosis and treatment may involve risks of injury or even death. I acknowledge that no
guarantees have been made to me regarding the result of examination or treatment in this hospital.
Nursing Care
This hospital provides only general nursing care and care ordered by the physician(s). If I want a
private duty nurse, I agree to make such arrangements. The hospital is not responsible for failure
to provide a private duty nurse and is hereby released from any and all liability arising from the fact
that the hospital does not provide this additional care.
Legal Relationship Between Hospital and Physicians
All physicians and surgeons providing services to me, including the radiologist, pathologist,
emergency physician, anesthesiologist and others, are not employees, representatives or agents of
the hospital. They have been granted the privilege of using the hospital for the care and treatment
of their patients, but they are not employees, representatives or agents of the hospital. They are
independent practitioners.
Patient initials:
I understand that I am under the care and supervision of my attending physician. The hospital
and its nursing staff are responsible for carrying out my physician’s instructions. My physician or
surgeon is responsible for obtaining my informed consent, when required, to medical or surgical
treatment, special diagnostic or therapeutic procedures, or hospital services provided to me under
my physician’s general and special instructions.
Maternity Patients
If I deliver an infant(s) while a patient of this hospital, I agree that these same Conditions of
Admission apply to the infant(s).
Form 8-1 Conditions of Admission
Page 2 of 4
(03/13)
©CALIFORNIA HOSPITAL ASSOCIATION
Personal Belongings
As a patient, I am encouraged to leave personal items at home. The hospital maintains a fireproof
safe for the safekeeping of money and valuables. The hospital is not liable for the loss or damage
to any money, jewelry, documents, eyeglasses, dentures, hearing aids, cell phones, laptops, other
personal electronic devices, or other articles that are not placed in the safe. Hospital liability for loss
of any personal property deposited with the hospital for safekeeping is limited by law to five hundred
dollars ($500) unless I receive a written receipt for a greater amount from the hospital.
Financial Agreement
I agree to promptly pay all hospital bills in accordance with the charges listed in the hospital’s
charge description master and, if applicable, the hospital’s charity care and discount payment
policies and state and federal law. I understand that I may review the hospital’s charge description
master before (or after) I receive services from the hospital. I understand that all physicians and
surgeons, including the radiologist, pathologist, emergency physician, anesthesiologist, and others,
will bill separately for their services. If any account is referred to an attorney or collection agency
for collection, I will pay actual attorneys’ fees and collection expenses. All delinquent accounts shall
bear interest at the legal rate, unless prohibited by law.
Patient initials:
Assignment of All Rights and Benefits
I irrevocably assign and transfer to the hospital all rights, benefits, and any other interests in
connection with any insurance plan, health benefit plan, or other source of payment for my care.
This assignment shall include assigning and authorizing direct payment to the hospital of all
insurance and health plan benefits payable for this hospitalization or for these outpatient services. I
agree that the insurer or plan’s payment to the hospital pursuant to this authorization shall discharge
its obligations to the extent of such payment. I understand that I am financially responsible for
charges not paid according to this assignment, to the extent permitted by state and federal law.
I agree to cooperate with, and take all steps reasonably requested by, this hospital to perfect,
confirm, or validate this assignment.

Form 8-1 Conditions of Admission
(03/13)
Page 3 of 4
©CALIFORNIA HOSPITAL ASSOCIATION
Health Plan Contracts
This hospital maintains a list of health plans with which it contracts. A list of such plans is available
upon request from the financial office. All physicians and surgeons, including the radiologist,
pathologist, emergency physician, anesthesiologist, and others, will bill separately for their services.
It is my responsibility to determine if the hospital or the physicians providing services to me contract
with my health plan.
I certify that I have read the foregoing and received a copy thereof. I am the patient, the patient’s
legal representative, or am otherwise authorized by the patient to sign the above and accept its
terms on his/her behalf.
Date: Time: AM / PM
Signature:
(patient/legal representative)
If signed by someone other than patient, indicate relationship:
Print name:
(legal representative)
Signature:
(witness)
Print name:
(witness)

Form 8-1 Conditions of Admission
Page 4 of 4
(03/13)
©CALIFORNIA HOSPITAL ASSOCIATION
Financial Responsibility Agreement by Person Other Than the Patient or the
Patient’s Legal Representative
I agree to accept financial responsibility for services rendered to the patient and to accept the terms
of the Financial Agreement, Assignment of Insurance Benefits, and Health Plan Contracts provisions
above.
Date:
Time: AM / PM
Signature:
(financially responsible party)
Print name:
(financially responsible party)
Address:
Phone number:
Signature:
(witness)
Print name:
(witness)
A COPY OF THIS DOCUMENT SHOULD BE GIVEN TO THE
PATIENT AND ANY OTHER PERSON WHO SIGNS THIS DOCUMENT.
NOTE: This form should include taglines as required by the Affordable Care Act.
(See www.calhospital.org/taglines, for detailed information.)

(03/13)
Page 1 of 4
©CALIFORNIA HOSPITAL ASSOCIATION
FORM 8-1S
Condiciones para la Admision
Nombre del Paciente:
Consentimiento a Procedimientos Médicos y Quirúrgicos
Doy mi consentimiento a los procedimientos que podrían efectuarse durante esta hospitalización
o mientras sea paciente externo. Estos podrían incluir, entre otros, tratamiento o servicios de
emergencia, procedimientos de laboratorio, rayos X, tratamientos o procedimientos médicos
o quirúrgicos, servicios de salud telefónicos, anestesia, o servicios de hospital que se me
proporcionen, sin limitarse a éstos, bajo las instrucciones generales y especiales de mi médico o
cirujano. Entiendo que la práctica de la medicina y la cirugía no constituyen ciencias exactas y que
el diagnóstico y tratamiento pueden conllevar riesgo de lesión y hasta de muerte. Reconozco que
no se han hecho garantías respecto al resultado del examen o tratamiento en este hospital.
Atención de Enfermería
Este hospital suministra únicamente atención de enfermería general, y atención solicitada por
el(los) médico(s). Si deseo un(a) enfermero(a) privado(a), estoy de acuerdo en hacer los arreglos
necesarios. El hospital no es responsable en caso de que no se proporcionara un(a) enfermero(a)
privado(a) y por medio del presente queda eximido de cualquier y toda responsabilidad que se
origine a partir del hecho de que el hospital no proporciona esta atención adicional.
Los Médicos Son Practioners Medicos Independientes
Todos los médicos y cirujanos que me proporcionen servicios, incluido el radiólogo, patólogo,
médico de emergencias, anestesiólogo y otros, no son empleados, representantes ni agentes del
hospital. Se les ha otorgado el privilegio de utilizar el hospital para la atención y el tratamiento de
sus pacientes, pero no son empleados, representantes o agentes del hospital. Son profesionales
independientes.
Iniciales del paciente:
Entiendo que estoy bajo la atención y supervisión de mi médico. El hospital y su personal
de enfermería son responsables del cumplimiento de las instrucciones de mi médico. Es la
responsabilidad de mi médico o cirujano obtener el consentimiento informado del paciente,
en caso necesario, para el tratamiento médico o quirúrgico, los procedimientos diagnósticos o
terapéuticos especiales, o los servicios de hospital que me proporcionen bajo las instrucciones
generales y especiales de mi médico.
Pacientes de Maternidad
Si diera a luz a mi bebé como paciente de este hospital, estoy de acuerdo en que estas mismas
Condiciones de Admisión se aplicarán al bebé.

Page 2 of 4
(03/13)
©CALIFORNIA HOSPITAL ASSOCIATION
Form 8-1S Conditions of Admission
Objetos Personales
Como paciente, se me aconseja que deje mis artículos personales en casa. El hospital tiene una
caja fuerte a prueba de incendios para el depósito de dinero y objetos de valor. El hospital no se
hace responsable por el daño o por la pérdida de dinero, joyas, documentos, anteojos, dentaduras,
audífonos para la sordera, teléfonos celulares, computadoras portátiles, otros dispositivos
electrónicos personales o artículos no depositados en la caja fuerte. La responsabilidad del
hospital por la pérdida de bienes personales depositados en la caja fuerte del hospital para su
protección se limita a quinientos dólares ($500) a menos que el hospital me entregue un recibo por
una cantidad mayor.
Acuerdo Sobre la Responsabilidad Financiera
Estoy de acuerdo en pagar puntualmente todas las factures del hospital según los cargos que
aparezcan en el detalle de cargos de la factura principal del hospital y, en caso aplicable, las
políticas del programa de atención médica de caridad y pago con descuento, y las leyes estatales
y federales. Entiendo que puedo revisar el archivo maestro de descripción de cargos del hospital
antes (o después) de recibir los servicios de esta institución. Entiendo que todos los médicos y
cirujanos, incluido el radiólogo, patólogo, médico de emergencias, anestesiólogo y otros, facturarán
sus servicios por separado. En caso de que la cuenta se entregue a un abogado o a una agencia
de cobranzas para conseguir la liquidación, pagaré los honorarios del abogado y los costos de la
cobranza. Todas las cuentas vencidas acumularán intereses a la tasa legal a menos de que la ley
lo prohíba.
Asignación de Todos los Derechos y Beneficios
Irrevocablemente asigno y transfiero al hospital todos los derechos, beneficios y demás intereses
en relación con cualquier plan de seguros, plan de beneficios de salud u otra fuente de pago para
mi atención. Esta asignación incluirá la asignación y autorización del pago directo al hospital de
todos los beneficios del seguro y del plan de salud pagaderos por esta hospitalización o por los
servicios de paciente externo. Estoy de acuerdo con que el pago de la compañía de seguros o el
plan de pagos al hospital según lo acordado en esta autorización deberá cubrir las obligaciones
de la compañía de seguros o del plan hasta donde abarque dicho pago. Entiendo que soy
financieramente responsable de cargos que no se paguen de acuerdo con esta asignación, en la
medida que lo permita la ley estatal o federal. Acepto cooperar con el hospital, y realizar todo lo
que este solicite de manera razonable, para perfeccionar, confirmar o validar esta asignación.
(03/13)
Page 3 of 4
©CALIFORNIA HOSPITAL ASSOCIATION
Form 8-1S Conditions of Admission
Contratos del Plan de Atención Médica
Este hospital mantiene una lista de los planes de atención médica con los que tiene contrato. A
petición, se encuentra disponible una lista de estos planes en la oficina de finanzas. Todos los
médicos y cirujanos, incluido el radiólogo, patólogo, médico de emergencias, anestesiólogo y
otros, facturarán sus servicios por separado. Es mi responsabilidad determinar si el hospital o los
médicos que me proporcionan servicios tienen algún contrato con mi plan de salud.
Doy fe de que he leído lo anterior y que he recibido una copia del documento. Soy el paciente, el
representante legal del paciente o estoy autorizado por el paciente para firmar este documento y
aceptar sus términos y condiciones en su nombre.
Fecha: Hora: AM / PM
Firma:
(paciente o representante legal)
Si no lo firma el paciente, indique la relación con éste:
Nombre en letra de imprenta:
(representante legal)
Firma:
(testigo)
Nombre en letra de imprenta:
(testigo)

Page 4 of 4
(03/13)
©CALIFORNIA HOSPITAL ASSOCIATION
Form 8-1S Conditions of Admission
Acuerdo de Responsabilidad Financiera por Parte de una Persona que no Sea el
Paciente ni el Representante Legal del Paciente
Estoy de acuerdo en aceptar la responsabilidad financiera por los servicios prestados al paciente
y en aceptar las condiciones del Acuerdo sobre la Responsabilidad Financiera, de la Asignación
de Beneficios de Seguro, y de las disposiciones de la Obligación de un Plan de Atención Médica
expuestos anteriormente.
Fecha: Hora: AM / PM
Firma:
(persona con responsabilidad financiera)
Nombre en letra de imprenta:
(persona con responsabilidad financiera)
Dirección:
Teléfono:
Firma:
(testigo)
Nombre en letra de imprenta:
(testigo)
A COPY OF THIS DOCUMENT SHOULD BE GIVEN TO THE
PATIENT AND ANY OTHER PERSON WHO SIGNS THIS DOCUMENT.
NOTE: This form should include taglines as required by the Affordable Care Act.
(See www.calhospital.org/taglines, for detailed information.)

MH APPENDIX 9-A
Medical Necessity for MHP Coverage
(05/19)
Page 1 of 4
©CALIFORNIA HOSPITAL ASSOCIATION
For MHP coverage as a psychiatric inpatient service or an emergency psychiatric condition, the patient
must meet the following:
Has one of the following diagnoses in the DSM-IVE:
• Pervasive development disorders;
• Disruptive behavior and attention deficit
disorders;
• Feeding and eating disorders of infancy or early
childhood;
• Tic disorders;
• Elimination disorders;
• Other disorders of infancy, childhood, or
adolescence, cognitive disorders (dementia with
delusions or depressed mood);
• Substance induced disorders (with psychotic,
mood, or anxiety disorder);
• Schizophrenia and other psychotic disorders;
• Mood disorders;
• Anxiety disorders;
• Somatoform disorders;
• Dissociative disorders;
• Eating disorders;
• Intermittent explosive disorder;
• Pyromania;
• Adjustment disorders;
• Personality disorders.
Cannot be safely treated at a lower level of care and
Requires psychiatric inpatient hospital services as the
result of a mental disorder as the result of one of the
following:
• Has symptoms or behaviors due to a mental
disorder that:
— Represent a current danger to self or others, or
significant property destruction;
— Prevent the beneficiary from providing for, or
utilizing, food, clothing or shelter;
— Present a severe risk to the beneficiary’s physical
health; or
— Represent a recent, significant deterioration in
ability to function.
• Requires admission for one of the following:
— Further psychiatric evaluation;
— Medication treatment; or
— Other treatment that can reasonably be provided
only if the patient is hospitalized.
[Title 9, California Code of Regulations, Section 1820.205]

MH Appendix 9-A Medical Necessity for MHP Coverage
Page 2 of 4
(05/19)
©CALIFORNIA HOSPITAL ASSOCIATION
For MHP coverage for outpatient specialty mental health services, the patient and/or service must meet the
following:
Has one of the following diagnoses in the DSM-IVE:
• Pervasive developmental disorders, except autistic
disorders
• Disruptive behavior and attention deficit disorders
• Feeding and eating disorders of infancy and early
childhood
• Elimination disorders
• Other disorders of infancy, childhood, or
adolescence
• Schizophrenia and other psychotic disorders,
except psychotic disorders due to a general
medical condition
• Mood disorders, except mood disorders due to a
general medical condition
• Anxiety disorders, except anxiety disorders due to a
general medical condition
• Somatoform disorders
• Factitious disorders
• Dissociative disorders
• Paraphilias
• Gender identity disorder
• Eating disorders
• Impulse control disorders not elsewhere
classified
• Adjustment disorders
• Personality disorders, excluding antisocial
personality disorder
• Medication-induced movement disorders related to
other included diagnoses
Have one of the following impairments as a result of
the mental disorder(s) on the left:
• A significant impairment in an important area of life
functioning
• A reasonable probability of significant deterioration
in an important area of life functioning
• Except as provided in Section 1830.210, a
reasonable probability a child will not progress
developmentally as individually appropriate. For the
purpose of this Section, a child is a person under
the age of 21 years
and the service meets each of the following criteria:
• The focus of the proposed intervention is to
address the condition identified in Subsection (b)
(2) above.
• The expectation is that the proposed intervention
will:
— Significantly diminish the impairment, or
— Prevent significant deterioration in an important
area of life functioning, or
— Except as provided in Section 1830.210,
allow the child to progress developmentally as
individually appropriate.
— For a child who meets the criteria of Section
1830.210(1), meet the criteria of Section
1830.210(b) and (c).
• The condition would not be responsive to physical
health care-based treatment.
[Title 9, California Code of Regulations, Section 1830.205]
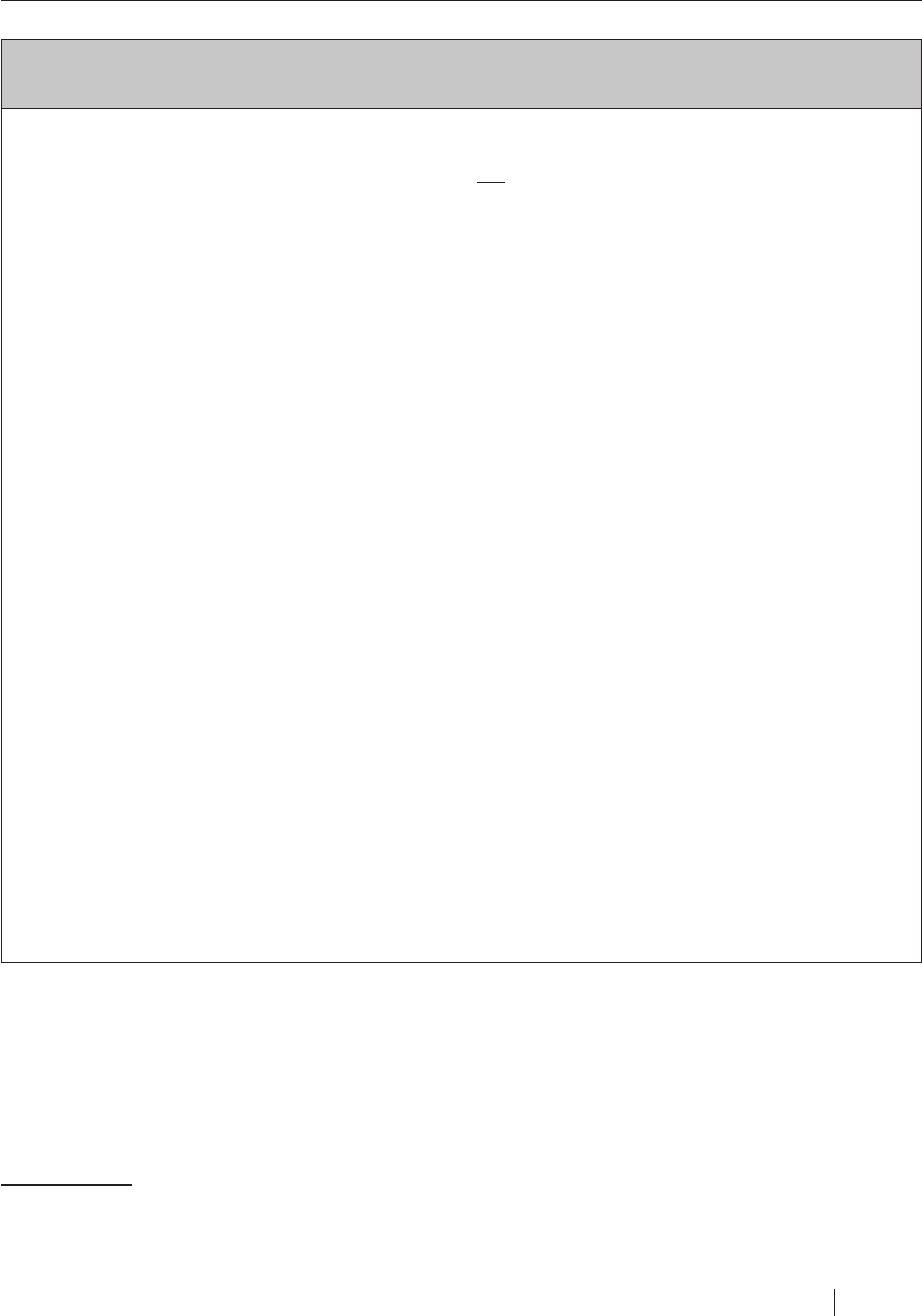
MH Appendix 9-A Medical Necessity for MHP Coverage
(05/19)
Page 3 of 4
©CALIFORNIA HOSPITAL ASSOCIATION
For MHP coverage for outpatient specialty mental health services for eligible beneficiaries under 21 years
of age, the patient and/or service must meet the following:
Has one of the following diagnoses in the DSM-IVE:
• Pervasive developmental disorders, except autistic
disorders
• Disruptive behavior and attention deficit disorders
• Feeding and eating disorders of infancy and early
childhood
• Elimination disorders
• Other disorders of infancy, childhood, or
adolescence
• Schizophrenia and other psychotic disorders,
except psychotic disorders due to a general
medical condition
• Mood disorders, except mood disorders due to a
general medical condition
• Anxiety disorders, except anxiety disorders due to a
general medical condition
• Somatoform disorders
• Factitious disorders
• Dissociative disorders
• Paraphilias
• Gender identity disorder
• Eating disorders
• Impulse control disorders not elsewhere
classified
• Adjustment disorders
• Personality disorders, excluding antisocial
personality disorder
• Medication-induced movement disorders related to
other included diagnoses
The beneficiary has a condition that would not be
responsive to physical health care-based treatment,
and
The services are necessary to correct or ameliorate
defects and physical and mental illnesses and
conditions discovered by the screening services with
respect to the mental disorder.
1
1
1 Other standards apply for eligibility for targeted case management.
[Title 9, California Code of Regulations, Section 1830.210]

APPENDIX MH 9-B
Types of MCPs and MHPs
(05/19)
Page 1 of 1
©CALIFORNIA HOSPITAL ASSOCIATION
Identifying the Players and Governing Authorities
Medi-Cal Managed Care Plans
There are three main models of Medi-Cal managed care plans, including county-operated health
systems (COHS), geographic managed care plans and two-plan model/regional model plans.
The COHS serve beneficiaries in Del Norte, Humboldt, Lake, Lassen, Marin, Mendocino, Merced,
Modoc, Monterey, Napa, Orange, San Luis Obispo, San Mateo, Santa Barbara, Santa Cruz, Shasta,
Siskiyou, Solano, Sonoma, Trinity, Ventura and Yolo Counties. Geographic managed care serves
beneficiaries in Sacramento and San Diego Counties. All other counties, with the exception of San
Benito that has a unique Medi-Cal managed care program, are served through a two-plan, modified
two-plan or regional model.
Non-COHS Medi-Cal managed care plans are subject to a myriad of rules: federal Medicaid laws,
the 1115 waiver, state Medi-Cal laws, the contracts between the non-COHS Medi-Cal plans and the
state and the Knox-Keene Act. The state has adopted laws governing non-COHS Medi-Cal managed
care plans.
Unlike non-COHS Medi-Cal managed care plans, COHS Medi-Cal managed care plans are subject
to few state laws and are exempt from certain federal requirements. They are also exempt from
Knox-Keene licensure with respect to their Medi-Cal lines of business. However, they continue to be
subject to the 1115 waiver and certain legal requirements are made applicable to them pursuant to
their contracts with the state.
Cal MediConnect Plan
Cal MediConnect plans operate in seven counties (Los Angeles, Orange, Riverside, San Bernardino,
San Diego, San Mateo, and Santa Clara) and administer the Medi-Cal and Medicare benefits for
dual-eligible beneficiaries enrolled in the Cal MediConnect program.
Cal MediConnect plans are subject to the plans’ three-way contracts with CMS and DHCS, the
memorandum of understanding between DHCS and CMS and state and federal laws governing dual
demonstration projects. In addition, non-COHS Cal MediConnect plans are subject to the Knox-
Keene Act. In some areas, the Cal MediConnect plans apply Medicare Advantage rules when the
patient is receiving services that would have otherwise been covered by Medicare if the patient was
not enrolled in Cal MediConnect. In these situations, if the patient is receiving care that would have
otherwise been covered by Medi-Cal, then the plans apply Medi-Cal rules.
County Mental Health Plan
County mental health plans operate as prepaid inpatient health plans under federal law. They are
subject to the state’s 1915(b) Medi-Cal Specialty Mental Health Services Waiver, their contracts with
the state, federal laws governing prepaid inpatient health plans and applicable state law. They are
not health care service plans subject to the Knox- Keene Act.

APPENDIX MH 9-C
Pertinent DHCS Plan Letters
(05/19)
Page 1 of 3
©CALIFORNIA HOSPITAL ASSOCIATION
MMCD 00-01 Excerpt (Redlines from Revised Guidance from DHCS)
Emergency Services and Care
The assignment of financial responsibility to the Plan or the MHP for charges resulting from
emergency services to determine whether a psychiatric emergency exists under the conditions
provided in Title 9, CCR, Section 1820.225, and the care and treatment necessary to relieve or
eliminate the emergent condition is generally determined by:
• The diagnosis assigned to the emergent condition;
• The type of professional performing the services; and
• Whether such services result in the admission of the Plan member for psychiatric inpatient
hospital services at the same or a different facility.
It is suggested that the assignment of financial responsibility for emergency room facility charges
and professional services be addressed as a component of the MOU.
Emergency Room Facility Charges and Professional Services
Financial responsibility for charges resulting from the emergency services and care of a Plan
member whose condition meets the medical necessity criteria for coverage by the MHP is
contractually assigned as follows:
• The Plan shall cover and pay for the facility charges resulting from the emergency services
and care of a Plan member whose condition meets MHP medical necessity criteria when
such services and care do not result in the admission of the member for psychiatric inpatient
hospital services or when such services result in an admission of the member for psychiatric
inpatient hospital services at a different facility.
• The MHP shall cover and pay is responsible for the facility charges resulting from the
emergency services and care of a Plan member whose condition meets MHP medical
necessity criteria when such services and care do result in the admission of the member
for psychiatric inpatient hospital services at the same facility. The facility charge is not paid
separately, but is included in the per diem rate for the inpatient stay.
• The Plan shall cover and pay for the facility charges resulting from the emergency services
and care of a Plan member whose condition meets MHP medical necessity criteria at a
hospital that does not provide psychiatric inpatient hospital services, when such services and
care do result in the transfer and admission of the member to a hospital or psychiatric health
facility that does provide psychiatric inpatient hospital services. The Plan is not responsible
for the separately billable facility charges related to the professional services of a mental
health specialist at the hospital of assessment. The MHP may pay this charge, depending on
its arrangement with the hospital.

Appendix MH 9-C Pertinent DHCS Plan Letters
Page 2 of 3
(05/19)
©CALIFORNIA HOSPITAL ASSOCIATION
• The MHP is responsible for facility charges directly related to the professional services of a
mental health specialist provided in the emergency room when these services do not result
in an admission of the member for psychiatric inpatient hospital services at that facility or
any other facility.
• The Plan shall cover and pay for the medical professional services required for the
emergency services and care of a member whose condition meets MHP medical necessity
criteria when such services and care do not result in the admission of the member for
psychiatric inpatient hospital services.
• The MHP shall cover and pay for the professional services of a mental health specialist
required for the emergency services and care of provided in an emergency room to a Plan
member whose condition meets MHP medical necessity criteria or when mental health
specialist services are required to assess whether MHP medical necessity is met when such
services and care do result in the admission of the member for psychiatric inpatient hospital
services.
• The Plan shall cover and pay for all professional services except the professional services of
a mental health specialist, when required for the emergency services and care of a member
whose condition meets MHP medical necessity criteria.
Payment responsibility for charges resulting from the emergency services and care of a Plan
member with an excluded diagnosis or for a plan member whose condition does not meet MHP
medical necessity criteria shall be assigned as follows:
• The plan shall cover and pay for the facility charges and the medical professional services
required for the emergency services and care of a Plan member with an excluded diagnosis
or a Plan member whose condition does not meet MHP medical necessity criteria and such
services and care do not result in the admission of the member for psychiatric inpatient
hospital services.
• Payment for the professional services of a mental health specialist required for the
emergency services and care of a Plan member with an excluded diagnosis is the
responsibility of the Medi-Cal FFS system.
NOTE: Effective Jan. 1, 2000, SB 349 (Chapter 544, Statutes of 1999), redefines the definition
of emergency services and care as it applies only to health care service plans where coverage
for mental health is included as a benefit. SB 349 redefines the Health and Safety Code definition
of emergency services and care to include an additional screening, examination, and evaluation
to determine if a psychiatric emergency medical condition exists, and the care and treatment
necessary to relieve or eliminate the psychiatric medical condition, within the capability of the facility.
The provisions of SB 349 are a clarification of the definition of emergency services and care and a
clarification of an existing responsibility and not the addition of a new responsibility. SB 349 does
not change the assigned responsibilities of the Plan and the MHP to pay for emergency services as
described above.

Appendix MH 9-C Pertinent DHCS Plan Letters
(05/19)
Page 3 of 3
©CALIFORNIA HOSPITAL ASSOCIATION
Matrix of Managed Care Plan, Mental Health Plan Responsibilities — Sample
Responsibility Type of Service
Included Diagnosis and
Meets MHP Impairment
and Intervention
Criteria
Excluded
Diagnosis
Included Diagnosis,
But Does Not Meet
MHP Impairment and
Intervention Criteria
Emergency
Departments
Facility Charges MCP for initial triage and
medical services
MHP for any facility
charges related to a
covered psychiatric
service
NOTE: When a
beneficiary is admitted to
a psychiatric bed at the
same facility, there is no
separate payment for the
ER by the MHP or the
MCP
MCP MCP
Psychiatric
Professional Services
MHP EDS No MHP, MCP, or EDS
payment
Medical Professional
Services
MCP MCP MCP

MH APPENDIX 9-D
DHCS Chart: Medi-Cal Mental Health Services
(05/19)
Page 1 of 2
©CALIFORNIA HOSPITAL ASSOCIATION
DIMENSION MEDI-CAL
1
MHP
2
OUTPATIENT MHP INPATIENT
ELIGIBILITY Mild to Moderate Impairment
in Functioning
A member is covered by the
MCP for services if he or she
is diagnosed with a mental
health disorder as defined by
the current DSM
3
resulting
in mild to moderate distress
or impairment of mental,
emotional, or behavioral
functioning:
• Primary care providers
identify the need for a
mental health screening
and refer to a specialist
within their network. Upon
assessment, the mental
health specialists can
assess the mental health
disorder and the level
of impairment and refer
members that meet medical
necessity criteria to the
MHP for a Specialty Mental
Health Services (SMHS)
assessment.
• When a member’s
condition improves under
SMHS and the mental
health providers in the MCP
and MHP coordinate care,
the member may return to
the MH provider in the MCP
network.
NOTE: Conditions that
the current DSM identifies
as relational problems are
not covered, i.e., couples
counseling or family
counseling.
Significant Impairment in
Functioning
A member is eligible for
services if he or she meets
all of the following medical
necessity criteria:
1. Has an included mental
health diagnosis;
4
2. Has a significant
impairment in an important
area of life function, or a
reasonable probability of
significant deterioration
in an important area
of life function, or a
reasonable probability
of not progressing
developmentally as
individually appropriate;
3. The focus of the proposed
treatment is to address the
impairment(s) described
in #2;
4. The expectation that the
proposed treatment will
significantly diminish
the impairment, prevent
significant deterioration in
an important area of life
function, and
5. The condition would
not be responsive to
physical health care-based
treatment.
NOTE: For members under
age 21 who meet criteria for
EPSTD specialty mental health
services, the criteria allow for
a range of impairment levels⁵
and include treatment that
allows the child to progress
developmentally as individually
appropriate.
Emergency and Inpatient
A member is eligible for
services if he or she meets the
following medical necessity
criteria:
1. An included diagnosis;
2. Cannot be safely treated at
a lower level of care;
3. Requires inpatient hospital
services due to one of
the following which is the
result of an included mental
disorder:
a. Symptoms or behaviors
which represent a
current danger to self
or others, or significant
property destruction;
b. Symptoms or behaviors
which prevent the
beneficiary from
providing for, or utilizing,
food, clothing, or shelter;
c. Symptoms or behaviors
which present a severe
risk to the beneficiary’s
physical health;
d. Symptoms or behaviors
which represent a
recent, significant
deterioration in ability to
function;
e. Psychiatric evaluation
or treatment which can
only be performed in
an acute psychiatric
inpatient setting or
through urgent or
emergency intervention
provided in the
community or clinic; and
f. Serious adverse
reactions to
medications,
procedures or therapies
requiring continued
hospitalization.

MH Appendix 9-D DHCS Chart: Medi-Cal Mental Health Services
Page 2 of 2
(05/19)
©CALIFORNIA HOSPITAL ASSOCIATION
DIMENSION MEDI-CAL
1
MHP
2
OUTPATIENT MHP INPATIENT
SERVICES Mental health services when
provided by licensed mental
health care professionals
(as defined in the Medi-Cal
provider bulletin) acting within
the scope of their license:
• Individual and group mental
health evaluation and
treatment (psychotherapy)
• Psychological testing
when clinically indicated to
evaluate a mental health
condition
• Outpatient services for the
purposes of monitoring
medication therapy
• Outpatient laboratory,
medications, supplies, and
supplements
• Psychiatric consultation
Medi-Cal Specialty Mental
Health Services:
• Mental Health Services
― Assessment
― Plan development
― Therapy
― Rehabilitation
― Collateral
• Medication Support
Services
• Day Treatment Intensive
• Day Rehabilitation
• Crisis Residential
• Adult Crisis Residential
• Crisis Intervention
• Crisis Stabilization
• Targeted Case
Management
• Acute psychiatric
inpatient hospital services
• Psychiatric Health Facility
Services
• Psychiatric Inpatient
Hospital Professional
Services if the beneficiary
is in fee-for-service
hospital
1 Medi-Cal Managed Care Plan.
2 County Mental Health Plan Medi-Cal Specialty Mental Health Services.
3 Current policy is based on DSM IV and will be updated to DSM 5 in the future.
4 As specified in Title 9, CCR, Sections 1820.205 and 1830.205 for adults and 1830.210 for those under age 21.
5 See footnote 4

MH APPENDIX 9-E
Pertinent Legal Definitions of Emergency
Psychiatric Conditions
(05/19)
Page 1 of 1
©CALIFORNIA HOSPITAL ASSOCIATION
FEDERAL DEFINITIONS CALIFORNIA DEFINITIONS
EMTALA Definition Medicaid Definition California Hospital
Licensing Definition
Medi-Cal MHP Definition
“Emergency medical
condition”
“Emergency medical
condition”
“Psychiatric emergency
medical condition”
“Emergency psychiatric
condition”
a medical condition
manifesting itself by acute
symptoms of sufficient
severity (including
severe pain, psychiatric
disturbances and/or
symptoms of substance
abuse) such that the
absence of immediate
medical attention could
reasonably be expected
to result in
a medical condition
manifesting itself by acute
symptoms of sufficient
severity (including
severe pain) such that a
prudent layperson, with
an average knowledge
of health and medicine,
could reasonably
expect the absence
of immediate medical
attention to result in
a mental disorder that
manifests itself by acute
symptoms of sufficient
severity that it renders the
patient as being either of
the following —
a condition that meets
the criteria in Section
1820.205
1
when the
beneficiary with the
condition, due to a mental
disorder —
(i) placing the health of
the individual (or, with
respect to a pregnant
woman, the health of the
woman or her unborn
child) in serious jeopardy;
(i) serious jeopardy to the
health of the individual or,
in the case of a pregnant
woman, the health of the
woman or her unborn
child, or
(i) an immediate danger
to himself or herself or to
others, or
(i) is a current danger to
self or others, or
(ii) serious impairment to
bodily functions; or
(ii) serious impairment to
bodily functions; or
(ii) immediately unable to
provide for, or utilize, food,
shelter, or clothing, due to
the mental disorder.
(ii) immediately unable to
provide for or utilize, food,
shelter or clothing, and
(iii) Serious dysfunction
of any bodily organ or
part; or
with respect to a
pregnant woman who is
having contractions
(i) that there is
inadequate time to
effect a safe transfer to
another hospital before
delivery; or
(ii) that transfer may
pose a threat to the
health or safety of the
woman or the unborn
child.
(iii) serious dysfunction of
any bodily organ or part.
(iii) requires psychiatric
inpatient hospital or
psychiatric health facility
services.
1 Title 9, CCR Section 1820.205 defines the term “medical necessity.” See Appendix A.

FORM 12-1
Request for Voluntary Admission and
Authorization for Treatment
(03/10)
Page 1 of 2
©CALIFORNIA HOSPITAL ASSOCIATION
Psychiatric Unit:
I hereby request admission to the above-named psychiatric unit and consent to the care and
treatment ordered by my attending physician or his or her associates. I understand that these
physicians are independent contractors and are not employees or agents of the hospital.
If my request is granted, I agree to conform to all the rules and regulations of the unit. If I wish
to leave the hospital, I will give notice of my desire to leave to a hospital staff member and will
complete all usual discharge or temporary absence procedures.
I understand that the hospital may inventory my personal belongings and possessions and remove
items it considers potentially dangerous to my safety and welfare, or to the safety and welfare of
other patients, visitors, or hospital staff.
I understand that my attending physician may wish to permit me the maximum amount of freedom
of action commensurate with my condition, as this may be an important factor in my treatment
program. This freedom of action may lead to possible self-injury and I release the hospital, its
employees and agents, as well as my attending physician or his or her associates, from any and all
responsibility in case such freedom leads to injury, except where the injury was the proximate result
of negligence on the part of the hospital, its employees and agents, or my attending physician and
his or her associates.
Date: Time: AM / PM
Signature:
(patient/legal representative)
If signed by someone other than patient, indicate relationship:
Print name:
(legal representative)
(over)

Form 12-1 Request for Voluntary Admission and Authorization for Treatment
Page 2 of 2
(03/10)
©CALIFORNIA HOSPITAL ASSOCIATION
Certificate of Attending Physician
I hereby certify that I am the attending physician of the above-named patient, that I have examined
the patient with reference to mental condition and, based on that examination, it is my opinion that
the patient understands the nature of the admission to the psychiatric unit of this hospital and the
care and treatment to be rendered, and that the patient was mentally competent at the time of the
examination to make this application for admission.
Additional comments:
Date: Time: AM / PM
Signature:
(physician)
Print name:
(physician)
NOTE: This form should include taglines as required by the Affordable Care Act.
(See www.calhospital.org/taglines, for detailed information.)

(03/10)
Page 1 of 2
©CALIFORNIA HOSPITAL ASSOCIATION
FORM 12-1S
Solicitud de Admisión Voluntaria y Autorización
Para el Tratamiento
Unidad psiquiátrica:
Por la presente, solicito la admisión a la unidad psiquiátrica mencionada anteriormente y doy
mi consentimiento para la atención y el tratamiento que ordenó el médico que me atiende o
sus colaboradores. Entiendo que estos médicos son contratistas independientes y que no son
empleados ni agentes del hospital.
Si se concede mi solicitud, me comprometo a cumplir con todas las normas y los reglamentos
de la unidad. En el caso de que desee dejar el hospital, informaré sobre mi deseo de irme a un
miembro del personal del hospital y llevaré a cabo todos los procedimientos normales para que me
den de alta o la ausencia temporal.
Entiendo que el hospital puede hacer un inventario de mis efectos personales y pertenencias, y
quitarme los elementos que considere potencialmente peligrosos para mi seguridad y bienestar, o
para la seguridad y el bienestar de otros pacientes, visitantes o miembros del personal del hospital.
Entiendo que el médico que me atiende puede considerar conveniente permitirme la máxima
cantidad de libertad de acción que sea acorde a mi enfermedad, ya que esto puede ser un factor
importante en mi programa de tratamiento. Esta libertad de acción podría conducirme a posibles
autolesiones, y eximo al hospital, a sus empleados y agentes, y al médico que me atiende o a
sus colaboradores de toda responsabilidad en caso de que tal libertad me conduzca a lesiones,
excepto si la lesión fuera consecuencia inmediata de la negligencia por parte del hospital, sus
empleados y agentes, o del médico que me atiende y sus colaboradores.
Fecha: Hora: AM / PM
Firma:
(paciente/representante legal)
En caso de que lo firmase una persona que no sea el paciente, indique la relación:
Nombre en letra de imprenta:
(representante legal)
(sobre)

Page 2 of 2
(03/10)
©CALIFORNIA HOSPITAL ASSOCIATION
Form 12-1S Request for Voluntary Admission and Authorization for Treatment
Certificate of Attending Physician
I hereby certify that I am the attending physician of the above-named patient, that I have examined
the patient with reference to mental condition and, based on that examination, it is my opinion that
the patient understands the nature of the admission to the psychiatric unit of this hospital and the
care and treatment to be rendered, and that the patient was mentally competent at the time of the
examination to make this application for admission.
Additional comments:
Date: Time: AM / PM
Signature:
(physician)
Print name:
(physician)
NOTE: This form should include taglines as required by the Affordable Care Act.
(See www.calhospital.org/taglines, for detailed information.)

FORM 12-2
Statement of Professional Person Responsible for
Minor’s Admission
(04/15)
Page 1 of 1
©CALIFORNIA HOSPITAL ASSOCIATION
(To be placed in minor’s medical record.)
Minor’s Name:
I affirm that the above-named minor meets the following criteria:
1. The minor has a mental health disorder, or a mental health disorder and a substance abuse
disorder.
2. Inpatient treatment in this facility is reasonably likely to be beneficial to the minor’s mental
health disorder.
3. Inpatient treatment in this facility is the least restrictive, most appropriate available setting
in which to treat the minor, within the constraints of reasonably available services, facilities,
resources, and financial support.
I have provided the minor’s admitting parent or guardian with a full explanation, both orally and
in writing, of the facility’s treatment philosophy, including, where applicable, the use of seclusion,
restraints, medications, and the extent of family involvement.
Date:
Time: AM / PM
Signature:
(hospital representative)
Print name:
(hospital representative)
Title:
Reference: Welfare & Institutions Code Sections 6002.10 and 6002.15(a) and (b)

FORM 12-3
Notice to Minors
(03/13)
Page 1 of 1
©CALIFORNIA HOSPITAL ASSOCIATION
You are entitled to an independent clinical review of your continued inpatient treatment at this facility.
This review must be requested within 10 days of your admission. If you request such a review, the
patients’ rights advocate will provide you with information and assistance related to this review.
You will be provided a booklet published by the California Department of Health Care Services
describing the rights of minors in mental health facilities. The booklet will include the telephone
number of the patients’ rights advocate and the hours that the advocate may be reached.
Please sign below indicating your receipt of this Notice to Minors.
I have received the Notice to Minors.
Date: Time: AM / PM
Signature:
(minor)
Print name:
(minor)
Witness by Facility Representative (required):
Date: Time: AM / PM
Signature:
(facility representative)
Print name:
(facility representative)
Title:
(facility representative)
NOTE: This form should include taglines as required by the Affordable Care Act.
(See www.calhospital.org/taglines, for detailed information.)
Reference: Welfare and Institutions Code Section 6002.15(c)

(03/13)
Page 1 of 1
©CALIFORNIA HOSPITAL ASSOCIATION
FORM 12-3S
Aviso a los Menores de Edad
Usted tiene derecho a una revisión clínica independiente respecto a su tratamiento continuado
como paciente interno de esta institución. Esta revisión deberá ser solicitada dentro de los díez
días siguientes a su admisión. Si usted solicita dicha revisión, el defensor de los derechos de los
pacientes le proporcionará la información y asistencia relativas a esta revisión.
Usted recibirá un folleto publicado por el Departamento de Servicios de Salud del estado,
describiendo los derechos de los menores de edad en las instituciones de salud mental. El folleto
incluirá el teléfono del defensor de los derechos de los pacientes y el horario en que usted puede
comunicarse con dicho defensor.
Por favor firme al calce, indicando que ha recibido este Aviso a los Menores de Edad.
He recibido el Aviso a los Menores de Edad.
Fecha: Hora: AM / PM
Firma:
(menor)
Nombre en letra de imprenta:
(menor)
Witness by Facility Representative (required):
Date: Time: AM / PM
Signature:
(facility representative)
Print name:
(facility representative)
Title:
(facility representative)
NOTE: This form should include taglines as required by the Affordable Care Act.
(See www.calhospital.org/taglines, for detailed information.)
Reference: Welfare and Institutions Code Section 6002.15(c)

FORM 12-4
Certification of Admitting Physician
(03/16)
Page 1 of 1
©CALIFORNIA HOSPITAL ASSOCIATION
The undersigned does hereby certify that he/she:
1. Is a physician and surgeon licensed to practice in the State of California,
2. Is a member of the attending staff or is otherwise authorized by a facility designated by the
county and approved by the California Department of Health Care Services as a facility for
72-hour treatment and evaluation,
3. Has made a physical and mental examination of the patient, considered the historical course
of the patient’s mental disorder, if that information was available, and
4. Believes that there is probable cause to believe that the patient is, as a result of mental
health disorder:
□ A danger to others □ A danger to himself/herself □ Gravely disabled
And for that reason requires hospital admission for evaluation or treatment on other than a voluntary
inpatient or outpatient basis.
Date: Time: AM / PM
Signature:
(physician)
Print name:
(physician)
Reference: Welfare and Institutions Code Section 5150

FORM 12-5
Application for Involuntary Admission —
Inebriates
(03/11)
Page 1 of 1
©CALIFORNIA HOSPITAL ASSOCIATION
Pursuant to Welfare and Institutions Code Section 5170 et seq.
I, the undersigned, being one of the following persons:
□ Staff member of a designated facility □ Other designated professional person
□ A peace officer
State that as a result of my personal observations, there is probable cause to believe that (name of
patient) , as a result of inebriation, is:
□ A danger to others □ A danger to himself/herself □ Gravely disabled
I have advised the patient of his/her rights: □ Yes □ No
The patient’s condition was brought to my attention by the following circumstances:
Date: Time: AM / PM
Signature:
(staff member/peace officer/other)
Print name:
(staff member/peace officer/other)
Certificate of Admitting Physician
The undersigned does hereby certify that he/she: (1) is a physician and surgeon licensed to
practice in the State of California, (2) is a member of the attending staff (or is otherwise authorized
by) a facility designated by the county and approved by the California Department of Alcohol and
Drug Programs as a facility for 72-hour treatment and evaluation of inebriates, (3) has made a
physical and mental examination of the patient, and (4) believes that there is probable cause to
believe that the patient is, as a result of inebriation, is:
□ A danger to others □ A danger to himself/herself □ Gravely disabled
and for that reason requires hospital admission for evaluation or treatment on other than a voluntary
inpatient or outpatient basis.
Date: Time: AM / PM
Signature:
(physician)
Print name:
(physician)

FORM 12-6
Notice of Certification for Intensive Treatment
(04/15)
Page 1 of 2
©CALIFORNIA HOSPITAL ASSOCIATION
Pursuant To: (Check applicable box)
□ Welfare and Institutions Code 5250 (Additional 14 days of intensive treatment)
□ Welfare and Institutions Code 5270.15 (Additional 30 days of intensive treatment)
The authorized agency providing evaluation services in the County of has
evaluated the condition of:
Name: Age: Sex: Marital Status:
Address:
We, the undersigned, allege that the above-named person is, as a result of mental health disorder
or impairment by chronic alcoholism (check all applicable boxes):
□ A danger to others
□ A danger to himself/herself
□ Gravely disabled as defined in Welfare and Institutions Code Section 5008(h)(1)
The specific facts which form the basis for our opinion that the above-named person meets one or
more of the classifications indicated above are as follows (certifying persons to detail facts):
The above-named person has been informed of this evaluation, and has been advised of the need
for, but has not been able or willing to accept treatment on a voluntary basis, or to accept referral to,
the following services:
Therefore we certify the above-named person to receive intensive treatment related to the mental
health disorder or impairment by chronic alcoholism beginning this day of (month) ,
20 , in the intensive treatment facility named: .
We hereby state that we delivered a copy of this notice this day to the above-named person. We
informed him or her that unless judicial review is requested, a certification review hearing will be
held within four days of the date on which the person is certified for a period of intensive treatment
to determine whether or not probable cause exists to detain him or her for intensive treatment
related to the mental health disorder or impairment by chronic alcoholism. We informed the above-
named person that an attorney or advocate will visit him or her to provide assistance in preparing
for the hearing or to answer questions regarding his or her commitment or to provide other
assistance. The court has been notified of this certification on this day.
(over)

Form 12-6 Notice of Certification for Intensive Treatment
Page 2 of 2
(04/15)
©CALIFORNIA HOSPITAL ASSOCIATION
Also, on this day the above-named person has been informed of his/her legal right to a judicial
review by habeas corpus, and the term “habeas corpus” has been explained to him/her, and that
he/she has been informed of his/her right to counsel, including court-appointed counsel pursuant to
Welfare and Institutions Code Section 5276.
Date: Time: AM / PM
Signature:
(physician/staff member of facility)
Print name:
(physician/staff member of facility)
Date: Time: AM / PM
Signature:
(representing intensive treatment facility)
Print name:
(representing intensive treatment facility)
Date: Time: AM / PM
Signature:
(countersignature)
Print name:
(countersignature)
COPIES:
Patient:
Patient’s attorney or representative:
Other person designated by patient:
Superior Court (to be submitted with the psychiatric certification review hearing decision)
Reference: Welfare and Institutions Code Section 5252 to 5254.1

(04/15)
Page 1 of 2
©CALIFORNIA HOSPITAL ASSOCIATION
FORM 12-6S
Aviso de Certificación Para Tratamiento Intensivo
Conforme Al: (Marque la casilla que corresponda)
□ Código de Instituciones y Bienestar 5250 (14 días adicionales de tratamiento intensivo)
□ Código de Instituciones y Bienestar 5270.15 (30 días adicionales de tratamiento intensivo)
El organismo autorizado que brinda los servicios de evaluación en el Condado de
ha evaluado el estado de salud de:
Nombre: Edad: Sexo: Estado civil:
Dirección:
Nosotros, los suscritos, declaramos que la persona antes mencionada es así, como resultado
de un trastorno de salud mental o deterioro por alcoholismo crónico (marque todas las casillas
correspondientes):
□ Representa un peligro para los demás
□ Representa un peligro para sí mismo/misma
□ Presenta una discapacidad grave según lo define la sección 5008(h)(1) del Código de
Instituciones y Bienesta
Los hechos específicos que fundamentan nuestra opinión de que la persona que se menciona
anteriormente cumple con una o más de las clasificaciones antes indicadas son los siguientes
(personas certificadas para detallar los hechos):
La persona mencionada anteriormente fue informada sobre esta evaluación y se le notificó sobre
la necesidad de recibir los siguientes servicios, pero no puede o no está dispuesto a aceptar la
derivación ni el tratamiento de manera voluntaria:
Por lo tanto, certificamos para que la persona antes mencionada reciba un tratamiento intensivo
relacionado con trastorno de salud mental o deterioro por alcoholismo crónico que comenzará el
día de (mes) de 20 , en el centro de tratamiento
intensivo llamado: .
Por la presente declaramos que hemos entregado una copia de este aviso el día de la fecha
indicada a la persona antes mencionada. Le informamos a él o a ella que a menos que se solicite
una revisión judicial, se realizará una audiencia de revisión de la certificación dentro de los cuatro
días a partir de la fecha en la que la persona se certifique para un período de tratamiento intensivo,
para determinar si existe o no una causa probable para detenerlo a él o ella para tratamiento
intensivo relacionado con un trastorno de salud mental o deterioro por alcoholismo crónico.
(sobre)

Page 2 of 2
(04/15)
©CALIFORNIA HOSPITAL ASSOCIATION
Form 12-6S Notice of Certification for Intensive Treatment
Hemos informado a la persona antes mencionada que un abogado o defensor lo visitará a él o
ella para brindar asistencia en la preparación de la audiencia o para responder preguntas sobre su
compromiso o proporcionar otro tipo de asistencia. La corte ha sido notificada de esta certificación
el día de la fecha indicada.
Además, en el día de la fecha, la persona mencionada anteriormente fue notificada sobre su
derecho legal a una revisión judicial mediante el hábeas corpus, se le explicó el significado del
término “hábeas corpus”, y se le informó acerca de su derecho a recibir asesoramiento, lo que
incluye la asignación de un abogado por parte del tribunal según la sección 5276 del Código de
Instituciones y Bienestar.
Fecha: Hora: AM / PM
Firma:
(médico/miembro del personal del establecimiento médico)
Nombre en letra de imprenta:
(médico/miembro del personal del establecimiento médico)
Fecha: Hora: AM / PM
Firma:
(establecimiento de tratamiento intensivo que representa)
Nombre en letra de imprenta:
(establecimiento de tratamiento intensivo que representa)
Fecha: Hora: AM / PM
Signature:
(contrafirma)
Nombre en letra de imprenta:
(contrafirma)
COPIAS:
Paciente:
Abogado o representante del paciente:
Otra persona designada por el paciente:
Tribunal Superior (para presentar con la decisión de la audiencia de revisión de la certificación
psiquiátrica)
Reference: Welfare and Institutions Code Section 5252 to 5254.1

FORM 12-7
Advisement of Rights — Involuntary Patient
(03/18)
Page 1 of 1
©CALIFORNIA HOSPITAL ASSOCIATION
This is to certify that on (date) , the undersigned
advised (name of patient) , a patient at
(name of hospital) , of the
following:
1. That the patient is being certified for not more than 14 days of involuntary intensive treatment
for:
□ Mental health disorder
□ Impairment by chronic alcoholism
□ Use of narcotics or restricted dangerous drugs
And I have personally delivered a copy of the certification notice to him/her.
2. His/her legal rights to designate any person whom he/she wishes informed regarding his/
her certification or judicial review (the patient understands that he/she has the right to
request that this information not be provided), and the patient has designated the following
person(s): (names, relationships and address)
;
3. His/her legal right to a certification review hearing or a habeas corpus hearing by the
superior court to review this certification for involuntary treatment in order to determine
whether he/she is a danger to others or to himself/herself or is gravely disabled; whether he/
she has been advised of, but has not accepted voluntary treatment; and whether the facility
providing intensive treatment is equipped and staffed to provide treatment, is designated by
the county to provide intensive treatment, and has agreed to admit him/her; and
4. His/her legal right to assistance of an advocate at a certification review hearing or to
counsel, including court-appointed counsel at no cost to him/her if he/she is unable to pay
for such legal services, to prepare for and represent him/her at a writ of habeas corpus
hearing.
I believe as a result of my own personal observation that (name of patient)
has the capacity to comprehend the nature of the
notice of certification and of the right to counsel to a certification review hearing and habeas corpus
hearing.
Date: Time: AM / PM
Signature:
(hospital representative)
Print name:
(hospital representative)
NOTE: This form should include taglines as required by the Affordable Care Act.
(See www.calhospital.org/taglines, for detailed information.)
Reference: Welfare and Institutions Code Sections 5253 and 5254.1

(03/18)
Page 1 of 1
©CALIFORNIA HOSPITAL ASSOCIATION
FORM 12-7S
Adviso de Derechos a los Pacientes Involuntarios
El presente es para certificar que el suscrito firmante ha informado en esta fecha a (nombre
del paciente) , un/a
paciente en (nombre del hospital) :
1. Que el/la paciente se certifica por no más de 14 días de tratamiento intensivo involuntario
por:
□ Trastorno de salud mental
□ Incapacidad por alcholismo crónico
□ Uso de estupefacientes o de drogas peligrosas restringidas
Y que ha entregado personalmente una copia de la certificación a dicho/a paciente;
2. Acerca de sus derechos legales para designar a cualquier persona que desee para que se
le informe acerca de su certificación o reconsideración judicial (el/la paciente entiende que
él/ella tiene derecho a solicitar que no se provea esta información), y que él/la paciente ha
designado a la(s) siguiente(s) persona(s): (nombres, relación y direcciones)
;
3. Acerca de su derecho legal a que se celebre una audiencia para la revisión de la
certificación o de hábeas corpus ante el Tribunal Superior para reconsiderar esta
certificación de tratamiento involuntario, a fin de determinar si él/ella representa un peligro
para los demás o para sí mismo/a o si está seriamente incapacitado/a; si se le ha
informado acerca de, pero no ha aceptado tratamiento voluntario; y si la institución que
proveyó el tratamiento intensivo está equipada y cuenta con personal idóneo para proveer
ese tipo de tratamiento, si ha sido designada por el condado para proveer tratamiento
intensivo, y si ha acordado ingresarlo/a; y,
4. Acerca de su derecho legal a que lo/la asista un abogado durante la audiencia para la
reconsideración de la certificación, o para asesorarlo/a, incluyendo abogados nombrados
por el tribunal sin costo alguno para él/ella si no puede pagar dichos servicios, y para
prepararlo/a para que lo/la represente durante una audiencia para el mandamiento de
hábeas corpus.
Creo como resultado de mis observaciones personales que (nombre del paciente)
tiene la capacidad de entender
el contenido del aviso de certificación y el derecho a contar con un abogado durante una audiencia
para la reconsideración de la certificación y para el mandamiento de hábeas corpus.
Fecha: Hora: AM / PM
Firma:
(representante del hospital)
Nombre en letra de imprenta:
(representante del hospital)
NOTE: This form should include taglines as required by the Affordable Care Act.
(See www.calhospital.org/taglines, for detailed information.)
Reference: Welfare and Institutions Code Sections 5253 and 5254.1

FORM 12-8
Leave of Absence from Psychiatric Service
(02/94)
Page 1 of 1
©CALIFORNIA HOSPITAL ASSOCIATION
Patient’s Name:
Date:
The above-named patient may be placed on a temporary leave of absence from the psychiatric
service of (name of hospital)
at (time and date)
to (responsible person) .
Address of responsible person:
Telephone:
To be readmitted at:
(time and date)
Signature:
(attending psychiatrist)
Patient readmitted at:
(time and date)
By:
If, during the patient’s absence, there is any need to contact the hospital, the following number
should be called:
PREPARE IN DUPLICATE
ONE COPY TO PATIENT, ONE COPY TO MEDICAL RECORD

(02/94)
Page 1 of 1
©CALIFORNIA HOSPITAL ASSOCIATION
FORM 12-8S
Permiso Para Ausentarse de Servicios
Psiquiatricos
Nombre del Pacente:
Fecha:
El paciente arriba mencionado podrá ausentarse temporalmente del servicio psiquiátrico de
(nombre del hospital)
a las (hora y fecha) bajo la responsabilidad de
(persona responsible) .
Dirección de la persona:
Teléfono:
El paciente ingresará nuevamente el:
(hora y fecha)
Firma:
(psiquíatra del caso)
El paciente ingresó nuevamente el:
(hora y fecha)
Por:
Si durante la ausencia del paciente fuera necesario ponerse en contacto con el hospital, llamar al
siguiente teléfono:
PREPARE IN DUPLICATE
ONE COPY TO PATIENT, ONE COPY TO MEDICAL RECORD

FORM 12-9
Request for Release From Involuntary Treatment
(03/08)
Page 1 of 1
©CALIFORNIA HOSPITAL ASSOCIATION
Date:
I, (member of treatment staff or person delivering copy of certification notice)
,
have today received a request for the release of (name of patient)
from the undersigned patient on his/her own behalf or from the undersigned person on behalf of the
patient.
Signature (or mark):
(patient making request for release)
Print name:
(patient making request for release)
Signature (or mark):
(patient making request for release)
Print name:
(person making request on behalf of patient)
Signature:
(member of treatment staff or person delivering copy of certification notice)
Print name:
(member of treatment staff or person delivering copy of certification notice)
NOTE: This form should include taglines as required by the Affordable Care Act.
(See www.calhospital.org/taglines, for detailed information.)
Reference: Welfare and Institutions Code Section 5275

(03/08)
Page 1 of 1
©CALIFORNIA HOSPITAL ASSOCIATION
FORM 12-9S
Peticion Para Dar de Alta del Tratamiento
Involuntario
Fecha:
Yo, (miembro del personal de tratamiento o la persona que haya entregado la copia del aviso de
certificación) , he recibido
hoy la petición para dar de alta a (nombre del paciente)
por parte del paciente suscrito a nombre propio o de la persona suscrita a nombre del paciente.
Firma (o marca):
(paciente que hace la petición para de alta)
Nombre en letra de imprenta:
(paciente que hace la petición para de alta)
Firma (o marca):
(persona que hace la petición a nombre del paciente)
Nombre en letra de imprenta:
(persona que hace la petición a nombre del paciente)
Firma:
(miembro del personal de tratamiento o persona que entrega la copia del aviso de
certificación)
Nombre en letra de imprenta:
(miembro del personal de tratamiento o persona que entrega la
copia del aviso de certificación)
NOTE: This form should include taglines as required by the Affordable Care Act.
(See www.calhospital.org/taglines, for detailed information.)
Reference: Welfare and Institutions Code Section 5275

FORM 12-10
Notice of Certification for Second Involuntary
14-Day Period for Intensive Treatment — Suicidal
Patient
(03/11)
Page 1 of 2
©CALIFORNIA HOSPITAL ASSOCIATION
To the Superior Court of the State of California for the County of .
The authorized agency providing 14-day intensive treatment, County of
, has
custody of:
Name:
Address:
Date of birth: Sex: Marital Status:
Religious Affiliation:
The undersigned allege that the above-named person presents an imminent threat of taking his/her
own life. This allegation is based upon the following facts:
This allegation is supported by the accompanying affidavits signed by:
The above-named person has been informed of this allegation and has been advised of, but has not
been able or willing to accept referral to, the following services:
Therefore we certify the above-named person to receive additional intensive treatment for no more
than 14 days beginning this day of (month) , 20 , in the
intensive treatment facility herein named: .
We hereby state that a copy of this notice has been delivered this day to the above-named person
and that he/she has been clearly advised of his/her continuing legal right to a judicial review by
habeas corpus, that the term “habeas corpus” has been explained to him/her, and his/her right to
counsel, including court-appointed counsel pursuant to Welfare and Institutions Code Section 5276.
Date: Time: AM / PM
Signature:
(physician/staff member of facility)
Date: Time: AM / PM
Countersignature:
(representing intensive treatment facility)
(over)

Form 12-10 Notice of Certification for Second Involuntary 14-Day Period for Intensive Treatment — Suicidal Patient
Page 2 of 2
(03/11)
©CALIFORNIA HOSPITAL ASSOCIATION
COPIES:
Patient:
Patient’s attorney or representative:
Other person designated by patient:
Superior Court (to be submitted with the psychiatric certification review hearing decision)
District Attorney
Facility Providing Intensive Treatment
Reference: Welfare and Institutions Code Sections 5262, 5263 and 5276

(03/11)
Page 1 of 2
©CALIFORNIA HOSPITAL ASSOCIATION
FORM 12-10S
Aviso de Remision a un Segundo Periodo
Involuntario de 14-Dias para Tratamiento
Intensivo — Paciente Suicida
Al Tribunal Superior del Estado de California para el Condado de .
La dependencia autorizada que proporciona tratamiento intensivo de 14 días, Condado de
tiene la custodia de:
Nombre:
Dirección:
Fecha del nacimiento: Sexo: Estado Civil:
Afiliación religiosa:
Los suscritos afirman que la persona arriba nombrada presenta la amenaza inminente de
suicidarse. La presente afirmación se basa en los siguientes hechos:
Se apoya a la presente afirmación con las declaraciones juradas firmadas por:
Se le ha notificado a la persona arriba nombrada de dicha afirmación, y se le ha informado de los
siguientes servicios, pero no ha querido o no ha sido capaz de aceptar ser referido a los mismos:
En tal virtud, remitimos a la persona antes mencionada para recibir tratamiento intensivo adicional
por un plazo no mayor de 14 días a partir de este día de (mes)
de 20 , en la institución e tratamiento intensivo
nombrada a continuación: .
We hereby state that a copy of this notice has been delivered this day to the above-named person
and that he/she has been clearly advised of his/her continuing legal right to a judicial review by
habeas corpus, that the term “habeas corpus” has been explained to him/her, and his/her right to
counsel, including court-appointed counsel pursuant to Welfare and Institutions Code Section 5276.
Date: Time: AM / PM
Signature:
(physician/staff member of facility)
Date: Time: AM / PM
Countersignature:
(representing intensive treatment facility)
(sobre)

Page 2 of 2
(03/11)
©CALIFORNIA HOSPITAL ASSOCIATION
Form 12-10S Notice of Certification for Second Involuntary 14-Day Period for Intensive Treatment — Suicidal Patient
COPIES:
Patient:
Patient’s attorney or representative:
Other person designated by patient:
Superior Court (to be submitted with the psychiatric certification review hearing decision)
District Attorney
Facility Providing Intensive Treatment
Reference: Welfare and Institutions Code Sections 5262, 5263 and 5276

FORM 12-11
Petition for Postcertification Treatment of
Imminently Dangerous Person
(04/15)
Page 1 of 2
©CALIFORNIA HOSPITAL ASSOCIATION
Attorney’s Name: Telephone:
Address:
SUPERIOR COURT OF THE STATE OF CALIFORNIA FOR THE COUNTY OF
In the Matter of: Case No:
) PETITION FOR POSTCERTIFICATION TREATMENT
, ) OF A DANGEROUS PERSON
)
) Date:
)
) Time:
)
) Dept:
I, , (the professional person in charge of
the intensive treatment facility) (the
designee of , the professional person in
charge of the treatment facility), in which (hereinafter referred
to as “patient”) has been under treatment pursuant to the certification by
and , hereby petition the court for an
order requiring the patient to undergo an additional period of treatment, not to exceed 180 days,
pursuant to the provisions of Article 6 (commencing with Section 5300) of Chapter 2 of Part 1 of
Division 5 of the Welfare and Institutions Code. This petition is based upon my allegation that:
1. The patient named above has attempted, or inflicted, or made a serious threat of substantial
physical harm upon the person of another after having been taken into custody, and
while in custody, for evaluation, and that, by reason of mental health disorder, presents a
demonstrated danger of inflicting substantial physical harm upon others; or that
2. The patient named above has attempted or inflicted physical harm upon the person
of another, that act having resulted in his/her being taken into custody, and that he/
she presents, as a result of mental health disorder, a demonstrated danger of inflicting
substantial physical harm to others; or that
3. The patient named above had made a serious threat of substantial physical harm upon the
person of another within seven days of being taken into custody, that threat having at least
in part resulted in his/her being taken into custody, and that he/she presents, as a result of
mental health disorder, a demonstrated danger of inflicting substantial physical harm upon
others.
(over)

Form 12-11 Petition for Postcertification Treatment of Imminently Dangerous Person
Page 2 of 2
(04/15)
©CALIFORNIA HOSPITAL ASSOCIATION
My allegation is based upon the following facts:
The allegation is supported by the accompanying affidavits signed by:
Date: Time: AM / PM
Signature:
NOTE: Copies of the petition and supporting affidavits must be served upon the patient named
above the same day as they are filed with the clerk of the superior court.

FORM 12-12
Detention of Patient With Psychiatric Emergency
in a Nondesignated Health Facility
(Health and Safety Code Section 1799.111)
(05/11)
Page 1 of 3
©CALIFORNIA HOSPITAL ASSOCIATION
A licensed general acute care or psychiatric hospital (that is not a county-designated facility
pursuant to Section 5150 of the Welfare and Institutions Code), licensed professional staff of
those hospitals, and physicians, providing emergency medical services in any department of those
hospitals will not be held civilly or criminally liable for detaining a patient if all of the following
conditions exist during the detention.
Name of Patient:
1. The law requires probable cause for detaining the patient/believing the patient is, as a result
of a mental disorder, a danger to self or others or gravely disabled. Describe the patient’s
behavior and/or statements, and circumstances under which the patient was detained (use
direct quotes from the patient, law enforcement officers, and/or others when appropriate).
2. Based upon the above information, I believe that the patient named above cannot be safely
released from the hospital because he or she is, as a result of a mental disorder, one or
more of the following:
□ A danger to self
□ A danger to others
□ Gravely disabled (for purposes of a detention under Health and Safety Code Section
1799.111, “gravely disabled” means an inability of the patient to provide for his or her
basic personal needs for food, clothing, or shelter)
Signature of treating physician and surgeon (or clinical psychologist with the medical staff privileges,
clinical privileges, or professional responsibilities provided in Health and Safety Code Section
1316.5*)
Name:
Signature:
Date: Time: AM / PM
(over)

Form 12-12 — Detention of Patient With Psychiatric Emergency in a Nondesignated Health Facility
Page 2 of 3
(05/11)
©CALIFORNIA HOSPITAL ASSOCIATION
The hospital staff, treating physician and surgeon, or appropriate licensed mental health professional
must make and document repeated unsuccessful efforts to find appropriate mental health treatment
for the detained patient. Required telephone calls or other contacts must commence at the earliest
possible time when the treating physician and surgeon has determined the time at which the patient
will be medically stable for transfer. The hospital may not wait until after the time when the patient
becomes medically stable for transfer to start making these contacts. Document efforts to find
appropriate mental heath treatment for the patient:
Date/Time Person/Facility Contacted Results of Contact:
The patient may not be detained beyond 24 hours. Date and time patient first detained:
If the patient is detained beyond eight hours, but less than 24 hours, both of the following additional
conditions must be met:
1. A discharge or transfer for appropriate evaluation or treatment for the patient has been
delayed because of the need for continuous and ongoing care, observation, or treatment that
the hospital is providing.
Describe the care, observation, or treatment the hospital is providing in the lines below or in
the medical record.
2. The patient named above continues to be, as a result of a mental disorder, one or more of
the following:
□ A danger to self
□ A danger to others
□ Gravely disabled (for purposes of a detention under Health and Safety Code Section
1799.111, “gravely disabled” means an inability of the patient to provide for his or her
basic personal needs for food, clothing, or shelter)
Signature of treating physician and surgeon (or clinical psychologist with the medical staff privileges,
clinical privileges, or professional responsibilities provided in Health and Safety Code Section
1316.5*)
Name:
Signature:
Date: Time: AM / PM

Form 12-12 — Detention of Patient With Psychiatric Emergency in a Nondesignated Health Facility
(05/11)
Page 3 of 3
©CALIFORNIA HOSPITAL ASSOCIATION
To receive immunity from civil or criminal liability for any actions of the patient after release, all of the
following conditions must exist during the detention:
1. The patient was not been admitted to a licensed general acute care hospital or a licensed
acute psychiatric hospital for evaluation and treatment pursuant to Section 5150 of the
Welfare and Institutions Code.
2. The release from the hospital is authorized by a physician and surgeon or a clinical
psychologist with the medical staff privileges or professional responsibilities provided for
in Section 1316.5, who determines, based on a face-to-face examination of the patient
detained, that the patient does not present a danger to himself or herself or others and is not
gravely disabled. In order for this paragraph to apply to a clinical psychologist, the clinical
psychologist must have a collaborative treatment relationship with the physician and surgeon.
The clinical psychologist may authorize the release of the patient from the detention, but
only after he or she has consulted with the physician and surgeon. In the event of a clinical
or professional disagreement regarding the release of a patient subject to the detention, the
detention must be maintained unless the hospital’s medical director overrules the decision
of the physician and surgeon opposing the release. Both the physician and surgeon and
the clinical psychologist must enter their findings, concerns, or objections in the patient’s
medical record.
NOTE: A patient detained under this law must be credited for the time detained, up to 24 hours,
in the event he or she is placed on a subsequent 72-hour hold pursuant to Section 5150 of the
Welfare and Institutions Code in a designated facility.
*Health and Safety Code Section 1316.5 states that state owned and operated health facilities that
offer services within the scope of practice of a psychologist must establish rules and procedures for
consideration of an application for medical staff membership and clinical privileges submitted by a
clinical psychologist. Private health facilities may enable the appointment of clinical psychologists on
such terms and conditions as the facility may establish. If a particular service is offered by a health
facility which permits clinical psychologists on its medical staff which both physicians and clinical
psychologists are authorized by law to perform, such service may be performed by either, without
discrimination.
Reference: Health and Safety Code Sections 1316.5 and 1799.111

Table 12-A Summary of Lanterman-Petris-Short Act’s Provision for Involuntary Evaluation and Treatment and Right of Review
(03/09)
Page 1 of 1
©CALIFORNIA HOSPITAL ASSOCIATION
W&I = Welfare and Institutions Code

FORM 13-3
Aftercare Plan
(04/10)
Page 1 of 3
©CALIFORNIA HOSPITAL ASSOCIATION
Patient’s Name:
Patient Number:
Nature of the illness:
Recommended follow-up:
Medications prescribed and side effects and dosage schedules (a signed informed consent form
for medications, if attached to this form, may satisfy this requirement):
Patient’s expected course of recovery:
Recommendations regarding treatment that are relevant to the patient’s care:
If the patient is a minor being released from involuntary treatment, address education or training
needs, if necessary, for the minor’s well-being:
Other information/instructions:
(over)

Form 13-3 Aftercare Plan
Page 2 of 3
(04/10)
©CALIFORNIA HOSPITAL ASSOCIATION
Referrals
Name/Agency:
Address:
Phone:
Comments:
Name/Agency:
Address:
Phone:
Comments:
Name/Agency:
Address:
Phone:
Comments:
(NOTE: If any item listed above is not completed, it must be explained why.)
Date:
Signature of person preparing this aftercare plan:
I have received a copy of this aftercare plan. I have also been advised that I may designate another
person to receive a copy of this aftercare plan, and I designate the following person:
(If patient declines to designate another person, this should be noted)

Form 13-3 Aftercare Plan
(04/10)
Page 3 of 3
©CALIFORNIA HOSPITAL ASSOCIATION
Date: Time: AM / PM
Signed:
(patient)
Print name:
(patient)
Date: Time: AM / PM
Signed:
(legal representative)
Print name:
(legal representative)
Date: Time: AM / PM
Signed:
(designated recipient of aftercare plan)
Print name:
(designated recipient of aftercare plan)
NOTE: This form should include taglines as required by the Affordable Care Act.
(See www.calhospital.org/taglines, for detailed information.)
Reference: Health and Safety Code Section 1262; Welfare and Institutions Code Sections 5585.57, 5622 and 5768.5

(04/10)
Page 1 of 3
©CALIFORNIA HOSPITAL ASSOCIATION
FORM 13-3S
Plan de Cuidados Posteriores
Nombre del paciente:
Número de paciente:
Naturaleza de la enfermedad:
Seguimiento recomendado:
Medicamentos recetados, efectos secundarios y cronograma de dosis (un formulario de
consentimiento informado firmado para los medicamentos, si se adjunta a este formulario, puede
satisfacer este requisito):
Período de recuperación previsto para el paciente:
Recomendaciones con respecto al tratamiento que sean pertinentes para la atención del paciente:
Si el paciente es un menor al que se da de alta de un tratamiento involuntario, aborde las
necesidades de educación o capacitación, si fuera necesario, para el bienestar del menor:
Otra información/instrucciones:
(sobre)
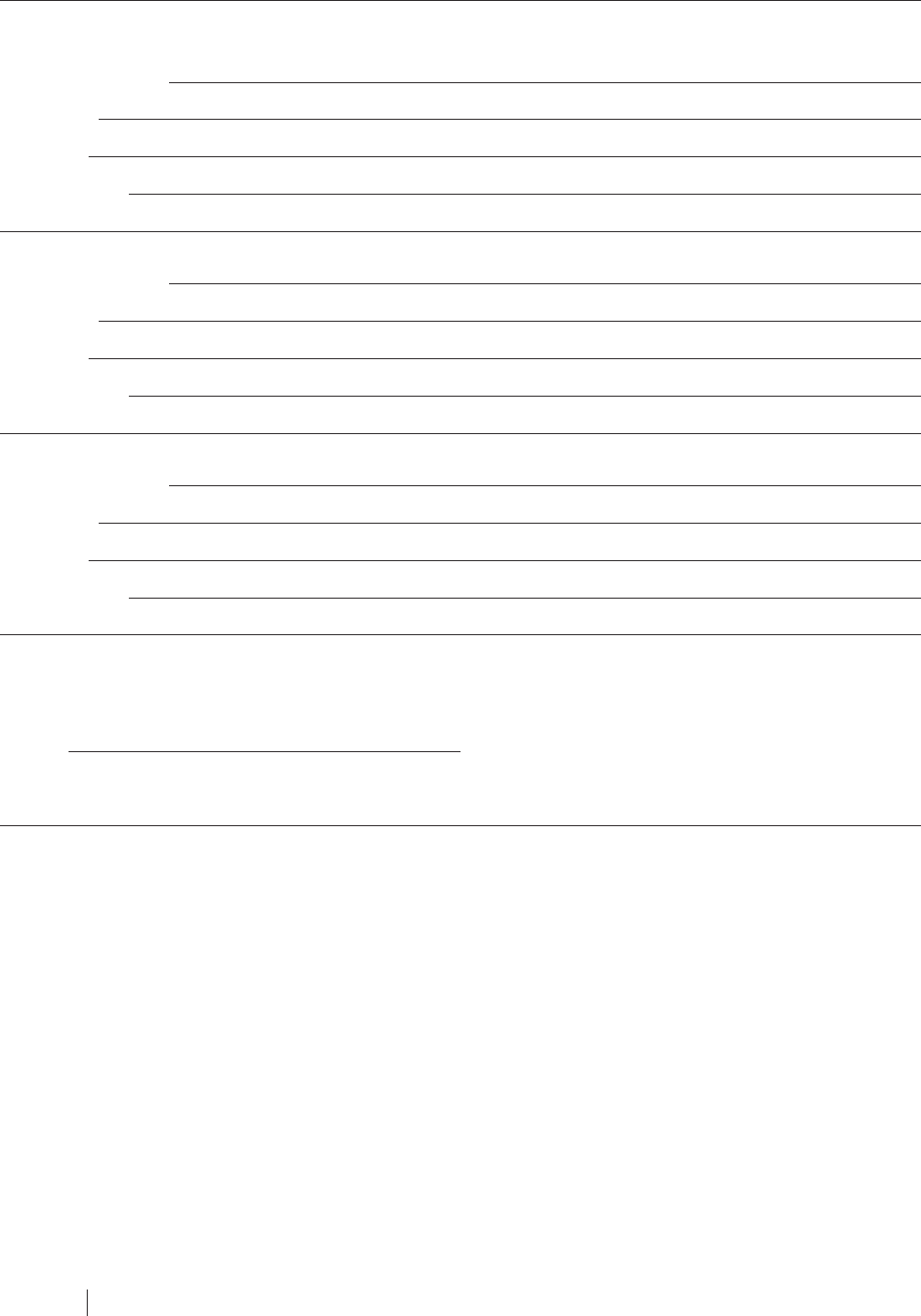
Page 2 of 3
(04/10)
©CALIFORNIA HOSPITAL ASSOCIATION
Form 13-3S Aftercare Plan
Derivaciones
Nombre/Agencia:
Dirección:
Teléfono:
Comentarios:
Nombre/Agencia:
Dirección:
Teléfono:
Comentarios:
Nombre/Agencia:
Dirección:
Teléfono:
Comentarios:
(OBSERVACIÓN: Si no se completa alguno de los puntos indicados anteriormente, se debe
explicar el motivo).
Fecha:
Firma de la persona que prepara este plan de atención posterior a la hospitalización:

(04/10)
Page 3 of 3
©CALIFORNIA HOSPITAL ASSOCIATION
Form 13-3S Aftercare Plan
He recibido una copia de este plan de atención posterior a la hospitalización. También se me ha
advertido que puedo designar a otra persona para que reciba una copia de este plan de atención
posterior a la hospitalización, y designo a la siguiente persona:
(Se debe indicar si el paciente se rehúsa a designar a otra persona)
Fecha: Hora: AM / PM
Firma:
(paciente)
Nombre en letra de imprenta:
(paciente)
Fecha: Hora: AM / PM
Firma:
(representante legal)
Nombre en letra de imprenta:
(representante legal)
Fecha: Hora: AM / PM
Firma:
(destinatario designado del plan de atención posterior a la hospitalización)
Nombre en letra de imprenta:
(destinatario designado del plan de atención posterior a la hospitalización)
NOTE: This form should include taglines as required by the Affordable Care Act.
(See www.calhospital.org/taglines, for detailed information.)
Reference: Health and Safety Code Section 1262; Welfare and Institutions Code Sections 5585.57, 5622 and 5768.5

FORM 13-4
Notice to Law Enforcement Agency: Release of
Person From Hospital From Whom a Firearm or
Other Deadly Weapon Was Confiscated
(04/06)
Page 1 of 1
©CALIFORNIA HOSPITAL ASSOCIATION
Name of Law Enforcement Agency which confiscated the weapon(s):
Address of Law Enforcement Agency which confiscated the weapon(s):
This notice is given to you as required by Welfare and Institutions Code Section 8102(b).
(name of patient) was released on (date) .
This patient was provided the required notice regarding the procedure to obtain return of a
confiscated weapon(s).
Date: Time: AM / PM
Signature:
(patient)
Print name:
(patient)
A COPY OF THIS FORM MUST BE PLACED IN THE MEDICAL RECORD.

FORM 13-5
Notice to Patient: Procedure for Return of
Confiscated Weapon(s)
(04/14)
Page 1 of 1
©CALIFORNIA HOSPITAL ASSOCIATION
Name of Patient:
This notice is given to you as required by Welfare and Institutions Code Section 8102(b).
You had one or more firearms or other deadly weapons confiscated from you by a law enforcement
officer pursuant to Welfare and Institutions Code Section 8102. The procedure for the return of your
weapon is found in Penal Code Section 33850 and Welfare and Institutions Code Section 8102.
The law enforcement agency which confiscated your weapon(s) has 30 days (longer in certain
cases) to initiate a petition in the superior court for a hearing to determine whether the return of the
weapon(s) would be likely to result in endangering you or others. The confiscating law enforcement
agency must also send you a notice of your right to a hearing on this issue. The law enforcement
agency may ask the court to extend the time to file a petition; however, the petition must be filed
within 60 days of your discharge from the facility even if the court grants an extension. You will have
30 days to respond to the court clerk to confirm your desire for a hearing. If you do not respond, a
default order forfeiting your weapon(s) will be issued. If you request a hearing, it must be set within
30 days of your request. The court clerk will notify you and the district attorney of the date, time, and
place of the hearing.
If the law enforcement agency does not file a petition, it must make your weapon(s) available for
return to you. If you fail to respond to a petition, your weapon may be forfeited.
I certify by my signature below that I have been given the information above related to the procedure
for the return of a confiscated weapon(s).
Date: Time: AM / PM
Signature:
(patient/legal representative)
Print name:
(patient/legal representative)
NOTE: This form should include taglines as required by the Affordable Care Act.
(See www.calhospital.org/taglines, for detailed information.)
A COPY OF THIS FORM MUST BE GIVEN TO THE PATIENT.
THE ORIGINAL MUST BE PLACED IN THE MEDICAL RECORD.

(04/14)
Page 1 of 1
©CALIFORNIA HOSPITAL ASSOCIATION
FORM 13-5S
Aviso al Paciente: Procedimiento Para la
Devolucion de Una o Mas Armas Confiscadas
Nombre del Paciente:
Este aviso se le entrega en conformidad con los requisitos del Código de Bienestar Social e
Instituciones, Sección 8102(b).
En conformidad con la Sección 8102 del Código de Bienestar Social e Instituciones, un agente
de la ley le confiscó una o más armas de fuego u otras armas mortíferas. El procedimiento para la
devolución de su arma se encuentra en la sección 33850 del Código Penal y en la sección 8102
del Código de Instituciones y Bienestar.
La agencia de la ley que le confiscó el arma (las armas) tendrá 30 días (en ocasiones más tiempo)
para presentar una petición ante el tribunal superior para que se realice una audiencia con el fin
de determinar si la devolución del arma (de las armas) podría resultar en poner a usted o a otras
personas en peligro. La agencia de la ley que haya confiscado el arma también deberá enviarle un
aviso explicándole su derecho a que se realice una audiencia sobre este asunto. La agencia de
la ley podrá solicitar al tribunal que prologue el plazo para presentar una petición. Sin embargo,
la petición se deberá presentar dentro de los 60 días de la fecha en que sea dado de alta de
la institución, aunque el tribunal otorgue una prórroga. Usted tendrá 30 días para responder al
actuario del tribunal confirmando que desea que se celebre la audiencia. Si no responde, se emitirá
una orden de incumplimiento y de confiscación de su arma (sus armas). Si solicita una audiencia,
la misma deberá fijarse dentro de los 30 días de su solicitud. El actuario del tribunal notificará a
usted y al procurador de distrito la fecha, la hora y el lugar de la audiencia.
Si la agencia de la ley no presenta una petición, deberá poner a su disposición el arma (las armas)
para su devolución. Si no responde a la petición, su arma puede ser confiscada.
Certifico con mi firma a continuación que se me ha proporcionado la información que antecede
relativa al procedimiento para la devolución de arma(s) confiscada(s).
Fecha: Hora: AM / PM
Firma:
(paciente o representante legal)
Nombre en letra de imprenta:
(paciente o representante legal)
NOTE: This form should include taglines as required by the Affordable Care Act.
(See www.calhospital.org/taglines, for detailed information.)
A COPY OF THIS FORM MUST BE GIVEN TO THE PATIENT.
THE ORIGINAL MUST BE PLACED IN THE MEDICAL RECORD.

FORM 16-1
Authorization for Use or Disclosure of Health
Information
(03/18)
Page 1 of 3
©CALIFORNIA HOSPITAL ASSOCIATION
Completion of this document authorizes the disclosure and use of health information
about you. Failure to provide all information requested may invalidate this
authorization.
Name of patient:
Use and Disclosure of Health Information
I hereby authorize
(name of hospital or other provider)
to release to:
(Persons/Organizations authorized to receive the information)
(Address — street, city, state, zip code)
The following information:
a. □All health information pertaining to my medical history, mental or physical
condition and treatment received; OR
□Only the following records or types of health information
(including any dates):
b. I specifically authorize release of the following information
(check as appropriate):
□Mental health treatment information
(initial)
□HIV test results
(initial)
□The following substance use disorder treatment information:
(initial)
(over)

Form 16-1 Authorization for Use or Disclosure of Health Information
Page 2 of 3
(03/18)
©CALIFORNIA HOSPITAL ASSOCIATION
A separate authorization is required to authorize the disclosure or use of
psychotherapy notes, as defined in the federal regulations implementing the Health
Insurance Portability and Accountability Act.
1
Purpose
Purpose of requested use or disclosure: □ Patient request OR □ Other:
Limitations, if any:
Expiration
This authorization expires on (date):
My Rights
• I may refuse to sign this authorization. My refusal will not affect my ability to
obtain treatment or payment or eligibility for benefits.
2
• I may inspect or obtain a copy of the health information that I am being asked to
allow the use or disclosure of.
• I may revoke this authorization at any time, but I must do so in writing
3
and submit
it to the following address:
.
My revocation will take effect upon receipt, except to the extent that others have
acted in reliance upon this authorization.
1 Health care providers that do not maintain psychotherapy notes as defined in HIPAA may wish to delete this sentence.
2 If any of the HIPAA recognized exceptions to this statement applies, then this statement must be changed to describe the consequences to
the individual of a refusal to sign the authorization when that covered entity can condition treatment, health plan enrollment, or benefit eligibility
on the failure to obtain such authorization. A covered entity is permitted to condition treatment, health plan enrollment or benefit eligibility
on the provision of an authorization as follows: (i) to conduct research-related treatment, (ii) to obtain information in connection with a health
plan’s eligibility or enrollment determinations relating to the individual or for its underwriting or risk rating determinations, or (iii) to create health
information to provide to a third party or for disclosure of the health information to such third party. Under no circumstances, however, may an
individual be required to authorize the disclosure of psychotherapy notes.
3 Patients of federally-assisted substance abuse programs and patients whose records are covered by LPS may revoke an authorization verbally.

Form 16-1 Authorization for Use or Disclosure of Health Information
(03/18)
Page 3 of 3
©CALIFORNIA HOSPITAL ASSOCIATION
• I have a right to receive a copy of this authorization.
4
• Information disclosed pursuant to this authorization could be redisclosed by the
recipient. Such redisclosure is in some cases not prohibited by California law
and may no longer be protected by federal confidentiality law (HIPAA). However,
California law prohibits the person receiving my health information from making
further disclosure of it unless another authorization for such disclosure is obtained
from me or unless such disclosure is specifically required or permitted by law.
Signature
Date:
Time: AM / PM
Signature:
(patient/legal representative)
If signed by a person other than the patient, indicate relationship:
Print name:
(legal representative)
Notes for Providers that Use this Form:
• If the purpose of the authorization is to use the information for marketing by
a third party that remunerates the provider, a statement to this effect must be
included in this authorization form.
• If the purpose of the authorization is for the sale of protected health information
(PHI), this form must state whether the PHI can be further exchanged for
remuneration by the initial recipient.
• A provider that discloses health information pursuant to an authorization must
communicate any limitation contained in the authorization to the recipient [Civil
Code Section 56.14]. The required notification may be accomplished by giving
the recipient a copy of the authorization form.
NOTE: This form should include taglines as required by the Affordable Care Act.
(See www.calhospital.org/taglines, for detailed information.)
4 Under HIPAA, the individual must be provided with a copy of the authorization when it has been requested by a covered entity for its own uses
and disclosures (see 45 C.F.R. Section 164.508(c)(4)).
(03/18)
Page 1 of 3
©CALIFORNIA HOSPITAL ASSOCIATION
FORM 16-1S
Autorización Para Utilizar o Divulgar Información
Médica
Al completar este documento autoriza la divulgación y el uso de su información
médica. Esta autorización puede perder su validez si no proporciona toda la
información solicitada.
Nombre del paciente:
Uso y Divulgación de Información Médica
Por medio del presente autorizo a:
(nombre del hospital o del proveedor)
a divulgar a:
(Personas u organizaciones autorizadas a recibir la información)
(Domicilio — calle, ciudad, estado, código postal)
la siguiente información:
a. □Toda la información médica referente a mi historia médica, estado mental o
físico y tratamiento recibido; O
□Sólo los siguientes expedientes o tipo de información (incluso las fechas):
b. Autorizo específicamente la divulgación de la siguiente información (marque
donde corresponde):
□Información sobre tratamiento de salud mental (inicial)
□Resultados de análisis de VIH (inicial)
□La siguiente información sobre uso de la substancia para el tratamiento
del trastorno:
(inicial)
(sobre)

Page 2 of 3
(03/18)
©CALIFORNIA HOSPITAL ASSOCIATION
Form 16-1S Authorization for Use or Disclosure of Health Information
Se requiere una autorización adicional para permitir la divulgación o el uso de
notas de psicoterapia, según se define en las regulaciones federales de la Ley de
Portabilidad y Responsabilidad de Seguros Médicos.
Objetivo
Objetivo del uso o divulgación solicitados: □ Solicitud de paciente O □ Otro:
Limitaciones, si existen:
Vencimiento
Esta autorización vence el (fecha):
Mis Derechos
• Puedo negarme a firmar esta autorización. Mi negativa no afectará mi calificación
para obtener tratamiento o pago ni mi calificación para obtener beneficios.
• Puedo inspeccionar u obtener una copia de la información médica cuyo uso o
divulgación se me solicita que autorice.
• Puedo revocar esta autorización en cualquier momento, pero debo hacerlo por
escrito y presentar mi revocación en este domicilio:
.
Mi revocación tendrá vigencia cuando se reciba, excepto en la medida en que
otras personas hayan actuado basados en esta autorización.
• Tengo el derecho de recibir una copia de esta autorización.
• El destinatario de la información divulgada en virtud de esta autorización puede
volver a divulgarla. Dicha nueva divulgación en algunos casos no es +prohibido
por la ley del Estado de California, y puede no estar protegida por la ley federal
de confidencialidad (HIPAA). Sin embargo, la ley de California prohíbe que la
persona que recibe la información sobre mi salud la revele, a menos que yo
autorice dicha revelación o que ésta sea requerida por la ley o permitida por
ésta.

(03/18)
Page 3 of 3
©CALIFORNIA HOSPITAL ASSOCIATION
Form 16-1S Authorization for Use or Disclosure of Health Information
Firma
Fecha:
Hora: AM / PM
Firma:
(paciente o representante legal)
Si no lo firma el paciente, indique la relación con éste:
Nombre en letra de imprenta:
(representante legal)
Notes for Providers that Use this Form:
• If the purpose of the authorization is to use the information for marketing by
a third party that remunerates the provider, a statement to this effect must be
included in this authorization form.
• If the purpose of the authorization is for the sale of protected health information
(PHI), this form must state whether the PHI can be further exchanged for
remuneration by the initial recipient.
• A provider that discloses health information pursuant to an authorization must
communicate any limitation contained in the authorization to the recipient [Civil
Code Section 56.14]. The required notification may be accomplished by giving
the recipient a copy of the authorization form.
NOTE: This form should include taglines as required by the Affordable Care Act.
(See www.calhospital.org/taglines, for detailed information.)

FORM 16-2
Request to Withhold Public Release of
Information
(03/03)
Page 1 of 1
©CALIFORNIA HOSPITAL ASSOCIATION
Name of Patient:
□ I do not want any information about me, including my general medical condition and my
location within the hospital, to be made available to the public. I understand the hospital
cannot effectively screen the identity of persons making inquiries, so this prohibition extends
to all callers, which may include family, friends and clergy.
□ I do not want my name or religious affiliation given to a member of the clergy, such as a priest
or rabbi, if they do not ask for me by name.
Date: Time: AM / PM
Signature:
(patient/legal representative)
If signed by other than patient, indicate relationship:
Print name:
(legal representative)
NOTE: This form should include taglines as required by the Affordable Care Act.
(See www.calhospital.org/taglines, for detailed information.)

(03/03)
Page 1 of 1
©CALIFORNIA HOSPITAL ASSOCIATION
FORM 16-2S
Solicitud Para Prohibir la Divulgación de
Información al Público
Nombre del Paciente:
□ No deseo que ninguna información acerca de mí, incluso mi condición médica general y
mi ubicación dentro del hospital esté a disposición del público. Entiendo que el hospital no
puede efectuar una identificación sistemática eficaz de las personas que hacen indagaciones,
por lo tanto esta prohibición se extiende a todas las personas que llamen, lo cual puede incluir
a mis familiares, amigos y clero.
□ No deseo mi nombre o afiliación religiosa dada a un miembro del clero, tal como un sacerdote
o un rabbi, si él no pide mí por nombre.
Fecha: Hora: AM / PM
Firma:
(paciente o representante legal)
Si no lo firma el paciente, indique la relación con éste:
Nombre en letra de imprenta:
(representante legal)
NOTE: This form should include taglines as required by the Affordable Care Act.
(See www.calhospital.org/taglines, for detailed information.)

FORM 19-2
Employee Acknowledgment of Child Abuse and
Neglect Reporting Obligations
(04/06)
Page 1 of 2
©CALIFORNIA HOSPITAL ASSOCIATION
Penal Code Sections 11165.7, 11166 and 11167 require specified health care practitioners and
other persons who have knowledge of or observe a child in his or her professional capacity or
within the scope of his or her employment whom he or she knows or reasonably suspects has
been the victim of child abuse or neglect to report the known or suspected instance of child abuse
immediately or as soon as practicably possible by telephone and to prepare and send a written
report thereof within 36 hours of receiving the information concerning the incident.
You are a person who is required to report known or suspected child abuse or neglect. The
reporting obligations that you must fulfill are described in Penal Code Sections 11165.7, 11166 and
11167 attached to this form. You must read this attachment.
The identity of all persons who make child abuse reports is confidential and disclosed only among
agencies receiving or investigating mandated reports, to the prosecutor in a criminal prosecution
or in an action initiated under Welfare and Institutions Code Section 602 arising from alleged child
abuse, or to counsel appointed to represent the child pursuant to Welfare and Institutions Code
Section 317(c), or to the county counsel or prosecutor in a proceeding under Family Code Section
7800 et seq. or Welfare and Institutions Code Section 300 et seq., or to a licensing agency when
abuse or neglect in out-of-home care is reasonably suspected, or when those persons waive
confidentiality, or by court order. No such agency or person may disclose the identity of any person
who makes a child abuse report to that person’s employer, except with the employee’s consent or
by court order. [Penal Code Section 11167(d)]
NOTE: The hospital may wish to supplement this form by providing the new employee a copy of
chapter 17 of CHA’s Consent Manual, which describes the child abuse reporting requirements. If
this approach will be used, this form should indicate:
We have attached a copy of the portion of CHA’s Consent Manual that describes
the California Child Abuse and Neglect Reporting Act. You should read this material
carefully. If you have any questions regarding your reporting obligations, please
discuss your questions with [insert the name and title of the person who should
answer questions].
NOTE: The hospital may supplement this form by discussing any special policy it has regarding
notifying supervisors and administration about reports that will be or are made, and how the
reporting is coordinated when several employees become aware of the same instance of suspected
child abuse or neglect. Such a discussion could, for example, include the following statement:
Your supervisor and administration should be notified whenever you believe that
you may be required to report suspected child abuse or neglect. In addition, usually
several hospital employees and medical staff members will learn about the same
instance of suspected abuse or neglect. The patient’s attending physician (or other
designated person) shall be responsible for making the reports or for identifying the
member of the health care team who shall assume this responsibility.
(over)

Form 19-2 Employee Acknowledgment of Child Abuse and Neglect Reporting Obligations
Page 2 of 2
(04/06)
©CALIFORNIA HOSPITAL ASSOCIATION
I have read the attached information regarding child abuse and neglect reporting obligations under
California law. I understand that I must comply with these legal requirements, and I agree to do so.
Date: Time: AM / PM
Signature:
(employee)
Print name:
(employee)
NOTE: The employer is required by law to attach a copy of Penal Code Sections 11165.7, 11166
and 11167 to this form.
Reference: Penal Code Sections 11165.7, 11166 and 11167

FORM 19-4
Employee Acknowledgment of Elder and
Dependent Adult Abuse Reporting Obligations
(03/13)
Page 1 of 2
©CALIFORNIA HOSPITAL ASSOCIATION
The Elder Abuse and Dependent Adult Civil Protection Act (Welfare and Institutions Code Sections
15600-15659) requires specified health care practitioners, clergy members, care custodians and
other persons who have knowledge of or reasonably suspect abuse or neglect of an elder or
dependent adult to report by telephone or through a confidential Internet reporting tool (if available
and appropriate). If the initial report is made by phone, a follow-up written report or an Internet
report must later be sent. The reporting time frames are described in the attached document.
You are a person who is required to report known or suspected abuse or neglect of an
elder or dependent adult. The reporting obligations you must fulfill are described in Welfare and
Institutions Code Section 15630, attached to this form. You must read this attachment.
NOTE: The hospital may wish to supplement this form by providing the new employees a copy
of chapter 17 of CHA’s Consent Manual, which describes the elder and dependent adult abuse
reporting requirements. If this approach will be used, this form should indicate:
We have attached a copy of the portion of the California Hospital Association’s
Consent Manual that describes the California elder and dependent adult abuse
and neglect reporting law. You should read this material carefully. If you have any
questions regarding your reporting obligations, please discuss your questions with
[insert the name and title of the person who should answer questions].
NOTE: The hospital may supplement this form by discussing any special policy it has regarding
notifying supervisors and administration about reports that will be or are made, and how the
reporting is coordinated when several employees become aware of the same instance of suspected
elder or dependent adult abuse. Such a discussion could, for example, include the following
statement:
Your supervisor and administration should be notified whenever you believe that you
may be required to report suspected elder or dependent adult abuse or neglect. In
addition, usually several hospital employees and medical staff members will learn
about the same instance of suspected abuse or neglect. The patient’s attending
physician (or other designated person) shall be responsible for making the reports
or for identifying the member of the health care team who shall assume this
responsibility.
The identity of persons who report elder or dependent adult abuse or neglect is confidential and
may be disclosed only among the following agencies or persons representing an agency:
1. An adult protective services agency.
2. A long-term care ombudsperson program.
3. A licensing agency.
4. A local law enforcement agency.
5. The office of the district attorney.
(over)

Form 19-4 Employee Acknowledgment of Elder and Dependent Adult Abuse Reporting Obligations
Page 2 of 2
(03/13)
©CALIFORNIA HOSPITAL ASSOCIATION
6. The office of the public guardian.
7. The probate court.
8. The bureau.
9. The Department of Consumer Affairs, Division of Investigation.
10. Counsel representing an adult protective services agency.
In addition, the identity of a person who reports elder or dependent adult abuse or neglect may be
disclosed under the following circumstances:
1. To the district attorney in a criminal prosecution.
2. When the reporter waives his or her confidentiality rights.
3. By court order.
[Welfare and Institutions Code Section 15633.5]
I have read the attached information regarding elder and dependent adult abuse reporting
obligations under California law. I understand that I must comply with these legal requirements, and
I agree to do so.
Date: Time: AM / PM
Signature:
(employee)
Print name:
(employee)
NOTE: The employer is required by law to attach a copy of Welfare and Institutions Code Section
15630 to this form.
Reference: Welfare and Institutions Code Sections 15633.5 and 15659

Table 19-A Assault and Abuse Reporting Requirements
(03/15)
Page 1 of 1
©CALIFORNIA HOSPITAL ASSOCIATION

FORM 20-1
Adverse Event Report Form — Sample
(10/18)
Page 1 of 4
CALIFORNIA HOSPITAL ASSOCIATION
[HOSPITAL LETTERHEAD]
(Must include hospital name and address elsewhere
if this form is not reproduced on hospital letterhead)
[Date of report]
State of California, Department of Public Health
Licensing and Certification District Office
[Street Address]
[City], CA [ZIP]
To Whom It May Concern:
This hospital believes it may have detected the adverse event indicated below as defined in Health
and Safety Code Section 1279.1, and is hereby reporting pursuant to Health and Safety Code
Section 1279.1.
Due to the short time frame required for reporting in the law, the information this hospital has may
be incomplete. If further investigation shows that no adverse event as defined in this law took place,
you will be notified. However, in order to comply with the law’s short time frame, this hospital is
taking a precautionary measure and reporting accordingly.
This hospital may have detected the adverse event checked below:
□ 1. Surgery performed on a wrong body part that is inconsistent with the documented
informed consent for that patient. This does not include a situation requiring prompt
action that occurs in the course of surgery or a situation that is so urgent as to preclude
obtaining informed consent.
□ 2. Surgery performed on the wrong patient.
□ 3. The wrong surgical procedure performed on a patient, which is a surgical procedure
performed on a patient that is inconsistent with the documented informed consent for that
patient. This does not include a situation requiring prompt action that occurs in the course
of surgery or a situation that is so urgent as to preclude obtaining informed consent.
□ 4. Retention of a foreign object in a patient after surgery or other procedure, excluding
objects intentionally implanted as part of a planned intervention and objects present prior
to surgery that are intentionally retained.
□ 5. Death during or up to 24 hours after induction of anesthesia after surgery of a normal,
healthy patient who has no organic, physiologic, biochemical, or psychiatric disturbance
and for whom the pathologic processes for which the operation is to be performed are
localized and do not entail a systemic disturbance.

Form 20-1 Adverse Event Report Form — Sample
Page 2 of 4
(10/18)
CALIFORNIA HOSPITAL ASSOCIATION
□ 6. Patient death or serious disability associated with the use of a contaminated drug,
device, or biologic provided by the health facility when the contamination is the
result of generally detectable contaminants in the drug, device, or biologic,
regardless of the source of the contamination or the product.
□ 7. Patient death or serious disability associated with the use or function of a device in
patient care in which the device is used or functions other than as intended. For
purposes of this subparagraph, “device” includes, but it not limited to, a catheter, drain,
or other specialized tube, infusion pump, or ventilator.
□ 8. Patient death or serious disability associated with intravascular air embolism that occurs
while being cared for in a facility, excluding deaths associated with neurosurgical
procedures known to present a high risk of intravascular air embolism.
□ 9. An infant discharged to the wrong person.
□ 10. Patient death or serious disability associated with patient disappearance for more than
four hours, excluding events involving adults who have competency or decision making
capacity.
□ 11. A patient suicide or attempted suicide resulting in serious disability while being cared
for in a health facility due to patient actions after admission to the health facility,
excluding deaths resulting from self-inflicted injuries that were the reason for
the admission to the health facility.
□ 12. A patient death or serious disability associated with a medication error, including, but not
limited to, an error involving the wrong drug, the wrong dose, the wrong patient, the
wrong time, the wrong rate, the wrong preparation, or the wrong route of administration,
excluding reasonable differences in clinical judgment on drug selection and dose.
□ 13. A patient death or serious disability associated with a hemolytic reaction due to the
administration of ABO-incompatible blood or blood products.
□ 14. A maternal death or serious disability associated with labor or delivery in a low-risk
pregnancy while being cared for in a facility, including events that occur within 42 days
postdelivery and excluding deaths from pulmonary or amniotic fluid embolism, acute fatty
liver of pregnancy, or cardiomyopathy.
□ 15. Patient death or serious disability directly related to hypoglycemia, the onset of which
occurs while the patient is being cared for in a health facility.
□ 16. Death or serious disability, including kernicterus, associated with failure to identify and
treat hyperbilirubinemia in neonates during the first 28 days of life. For purposes of this
subparagraph, “hyperbilirubinemia” means bilirubin levels greater than 30 miligrams per
deciliter.
□ 17. A Stage 3 or 4 ulcer, acquired after admission to a health facility, excluding progression
from Stage 2 to Stage 3 if Stage 2 was recognized upon admission.
□ 18. A patient death or serious disability due to spinal manipulative therapy performed at the
health facility.

Form 20-1 Adverse Event Report Form — Sample
(10/18)
Page 3 of 4
CALIFORNIA HOSPITAL ASSOCIATION
□ 19. A patient death or serious disability associated with an electric shock while being
cared for in a health facility, excluding events involving planned treatments, such as
electric countershock.
□ 20. Any incident in which a line designated for oxygen or other gas to be delivered to a
patient contains the wrong gas or is contaminated by a toxic substance.
□ 21. A patient death or serious disability associated with a burn incurred from any source
while being cared for in a health facility.
□ 22. A patient death associated with a fall while being cared for in a health facility.
□ 23. A patient death or serious disability associated with the use of restraints or bedrails while
being cared for in a health facility.
□ 24. Any instance of care ordered by or provided by someone impersonating a physician,
nurse, pharmacist, or other licensed health care provider.
□ 25. The abduction of a patient of any age.
□ 26. The sexual assault of a patient within or on the grounds of a health facility.
□ 27. The death or significant injury of a patient or staff member resulting from a physical
assault that occurs within or on the grounds of a facility. [Note: if this item is checked
because a staff member suffered death or significant injury due to a physical assault
on the grounds of the facility, please indicate the staff member’s name at the bottom
of the form, rather than a patient’s name.]
□ 28. An adverse event or series of adverse events that cause the death or serious disability
of a patient, personnel, or visitor. [Note: An “adverse event” is defined as the incidents
described in items 1. through 27., above. Thus, this category probably does not capture
any additional adverse events not described in items 1. through 27. above. If for some
reason an adverse event report is made about an event not listed in items 1. through 27.
above, a brief description of the event should be included on this form. If a hospital
has an adverse event that causes the death or serious disability of a patient, personnel,
or visitor but is not listed above in items 1. through 27., legal counsel should be
consulted to determine whether it should be reported. A different reporting
requirement may apply.]
Hospital’s code to link this report to its file regarding this potential adverse event:
Date hospital detected the adverse event:
Please contact me at [insert phone number] or at [insert fax number] if you require further
information.
Sincerely,
[Name]
[Title]
(over)

Form 20-1 Adverse Event Report Form — Sample
Page 4 of 4
(10/18)
CALIFORNIA HOSPITAL ASSOCIATION
NOTE: “Serious disability” means:
a. A physical or mental impairment that substantially limits one or more of the major life
activities of an individual, if the impairment lasts more than seven days or is still present at
the time of discharge from an inpatient health care facility, or
b. The loss of bodily function, if the loss lasts more than seven days or is still present at the
time of discharge from an inpatient health care facility, or
c. The loss of a body part.
*Generally, this report must be made within five days of detection. However, if the adverse event
is an ongoing or urgent threat to the welfare, health, or safety of patients, personnel or visitors, a
report must be made within 24 hours of detection.

FORM 21-1
Incident Report
(Complete Immediately for Every Incident and Send to
Administrator)
(03/13)
Page 1 of 2
©CALIFORNIA HOSPITAL ASSOCIATION
(Hospital Name) (For Addressograph Plate)
(City)
Administrator:
Please forward to Hospital Attorney
Confidential Report of an Incident
(Not a Part of the Medical Record)
Patient: Age: Sex: Room:
(Last Name, First Name) (M / F)
Admitting Diagnosis: Date of Admission:
If Outpatient, Date of Visit: Reason for Visit:
Attending Physician:
Date of Incident: Time: AM / PM
Were Bed Rails Up? Was Safety Belt In Use?
Was Patient Rational? Hi/Lo Bed Position:
Drugs Given Within 12 Hours Prior to Incident:
Sedatives: Dose: Time: AM / PM
Narcotics: Dose: Time: AM / PM
Dr. Notified By:
At Time: AM / PM Time Doctor Responded: AM / PM
Nurse’s Account of the Incident (Include Exact Location):

Form 21-1 Incident Report
Page 2 of 2
(03/13)
©CALIFORNIA HOSPITAL ASSOCIATION
List Witnesses or Persons Familiar With Details of Incident and Other Patients in the Same Room:
Name:
Address:
Phone:
Name:
Address:
Phone:
Name:
Address:
Phone:
History of Incident as Related By the Patient:
Immediate Actions (and their outcomes):
Notifications:
a. Will/was report made under the Safe Medical Devices Act? Yes No (circle one)
b. Will/was report made to the California Department of Public Health as an adverse event or
unusual occurrence? Yes No (circle one)
c. Will/was patient or legal representative notified of any unexpected outcome?
Yes No (circle one)
d. Will/was attending physician notified? Yes No (circle one)
Doctor’s Report of Patient’s Condition (From Progress Notes):
Date of Report: Time: AM / PM
Signature:
(Nurse or Supervisor Reporting)

FORM 21-2
Report to Attorney
(03/10)
Page 1 of 2
©CALIFORNIA HOSPITAL ASSOCIATION
This Report is Confidential—
Not Part of the Medical Record
Date of Report: / / Time: AM / PM
MM DD YY
Name of Patient or Person Involved:
Medical Record Number or Other Identifying Information:
Check One:
□ Inpatient Admitting Diagnosis:
□ Outpatient/ER Reason for Visit:
□ Visitor/Volunteer
Sex: □Male □Female
Age: Yrs.
If under 1 year, circle one: 0-14 days 15-29 days 1-6 months 7-11 months
Newborn Problems:
□ Not Applicable □ Apgar less than 5 at 5 minutes
□ Coma □ Gestation less than 35 weeks
□ Convulsion
Date/time of admission: / / AM / PM (circle one)
MM DD YY
Date/time of event or effect: / / AM / PM (circle one)
MM DD YY
Description of what happened (include exact location):
If drug, IV infusion, treatment or equipment involved, specify name:
Description of immediate actions and outcome:
Lost/damaged property:

Form 21-2 Report to Attorney
Page 2 of 2
(03/10)
©CALIFORNIA HOSPITAL ASSOCIATION
Severity of outcome:
□ Minor outcome: Medical review, extra observations or monitoring
□ Moderate outcome: Minor diagnostic investigations or treatments (e.g. blood test,
urinalysis, first aid treatment)
□ Moderate/Significant outcome: Treatment with another drug, surgical intervention/
cancellation, transfer to another area with no increased length of stay
□ Significant outcome: Hospital admission or increased length of stay/morbidity which
continued at discharge
□ Severe outcome: Permanent disability or contributed to the patient’s death
Notifications:
a. Will/was report made under the Safe Medical Devices Act? Yes No (circle one)
b. Will/was report made to the California Department of Public Health as an adverse event or
unusual occurrence? Yes No (circle one)
c. Will/was patient or legal representative notified of any unexpected outcome?
Yes No (circle one)
d. Will/was attending physician notified? Yes No (circle one)
Witnesses to event or effect:
Name:
Address:
Phone:
Name:
Address:
Phone:
This report completed by:
Name:
Title:
Phone:

FORM 23-1
Consent for the HIV Test
(03/08)
Page 1 of 2
©CALIFORNIA HOSPITAL ASSOCIATION
Patient’s Name:
I am consenting to be tested to see whether I have been infected with the Human Immunodeficiency
Virus (HIV), which is the probable causative agent of Acquired Immune Deficiency Syndrome
(AIDS).
The Meaning of the Test
This test is not a test for AIDS but only for the presence of HIV. Being infected with HIV does not
mean that I have AIDS or that I will have AIDS or other related illnesses in the future. Other factors
must be reviewed to determine whether I have AIDS.
Most test results are accurate, but sometimes results can be wrong or uncertain. Test results could
indicate that I am infected with HIV when I am not (false positive) or they could fail to detect that I
am infected with HIV when I really am (false negative). Sometimes, the test cannot tell whether or
not I am infected at all. If I have been recently infected with HIV, it may take some time before a test
will detect the infection. For these reasons, I may have to repeat the test.
Confidentiality
California law limits the disclosure of my HIV test results. As a general rule, the law states that no
one but my doctor and other caregivers may be told about the test results unless I give specific
written consent to let other people know. However, in some cases, my test results could be
disclosed to my spouse, any sexual partner(s) or needle-sharing partner(s), the county health
officer, to a health care worker who has had a substantial exposure to my blood or other potentially
infectious material or to some other persons as required or authorized by law. Information relating to
my test results is kept in my medical record.
Benefits and Risks of the Test
The test results can help me make better decisions about my health care and my personal life. The
test results can help me and my doctor make decisions concerning medical treatments. There are
numerous treatment options available for persons who test positive for HIV. If the results are positive,
I know that I can infect others and that I can act to prevent this.
Potential risks of the test include psychological stress while awaiting the results and distress if the
results are positive.
Obligations of Ordering Medical Care Providers
A doctor or other medical care provider who orders an HIV test is required to:
• Inform the patient that an HIV test is planned;
• Provide information to the patient about the HIV test;
• Inform the patient that there are numerous treatment options available for a person who tests
positive for HIV and that a person who tests negative for HIV should continue to be routinely
tested; and

Form 23-1 Consent for the HIV Test
Page 2 of 2
(03/08)
©CALIFORNIA HOSPITAL ASSOCIATION
• Advise the patient that he or she has the right to decline the HIV test.
I understand that if I am pregnant, my doctor will give me additional information about HIV and the
HIV test as it applies to my condition.
More Information
I understand that before I decide to take this test I should be sure that I have asked my doctor any
questions I may have about the test, its meaning, its risks and benefits, and any alternatives to the
test.
Consent for HIV Test
By my signature below, I confirm that:
• I have read and understood the information in this form and I understand it;
• I have been given all of the information I desire concerning the HIV test, its meaning, expected
benefits, possible risks, and any alternatives to the tests, and I have had my questions answered;
• I understand that I have the right to decline an HIV test; and
• I give my consent for the performance of a test to detect HIV.
Date:
Time: AM / PM
Signature:
(patient/legal representative)
If signed by someone other than patient, indicate relationship*:
Print name:
(legal representative)
*This consent may be signed by a person other than the patient only under the following circum-
stances:
1. The patient is under twelve (12) years of age or, as a result of his/her physical or mental
condition, is incompetent to consent to the HIV antibody blood test; and
2. The person who consents to the test on the patient’s behalf is lawfully authorized to make
health care decisions for the patient, e.g., an agent appointed by the patient in a power
of attorney for health care; the parent or guardian of a minor; an appropriately authorized
conservator; or, under appropriate circumstances, the patient’s closest available relative (see
chapters 2 and 23 of CHA’s Consent Manual); and
3. It is necessary to obtain the patient’s HIV antibody test results in order to render appropriate
care to the patient or to practice preventative measures.
NOTE: This form should include taglines as required by the Affordable Care Act.
(See www.calhospital.org/taglines, for detailed information.)
Reference: Health and Safety Code Section 121020

(03/08)
Page 1 of 3
©CALIFORNIA HOSPITAL ASSOCIATION
FORM 23-1S
Consentimiento para la Prueba del Anticuerpo
Contra el VIH
Nombre del Paciente:
Por el presente doy mi consentimiento para hacer una prueba que determine si he sido infectado(a)
con el Virus de Inmunodeficiencia Humana (VIH), el cual es probablemente el agente causante del
Síndrome de Inmunodeficiencia Adquirida (SIDA).
Elsignificado de la Prueba
Esta prueba no se usa para detectar el SIDA, sino solamente la presencia del VIH. El estar
infectado(a) con el VIH no significa que tenga SIDA o que voy a tener SIDA, u otras enfermedades
relacionadas en el futuro. Para determinar si tengo SIDA, deberán considerarse otros factores.
La mayoría de los resultados de la prueba son exactos, pero algunas veces los resultados pueden
ser erróneos o inciertos. Los resultados de las pruebas podrían indicar que estoy infectado(a) con
el VIH, cuando en realidad no lo estoy (positivo falso) o podrían no detectar que estoy infectado(a)
con el VIH cuando sí lo estoy (negativo falso). Otras veces el examen no puede determinar si una
persona está infectada o en realidad no lo está. Si he sido infectado(a) recientemente con el VIH,
puede pasar algún tiempo antes de que una prueba detecte la infección. Por estos motivos, es
posible que deba repetir la prueba.
Confidencialidad
La ley de California limita la divulgación de los resultados de mi prueba VIH. Por lo general, la ley
indica que nadie, con la excepción de mi médico y de otros proveedores de servicios de atención
de la salud, puede obtener los resultados de la prueba, a menos que yo consienta específicamente
por escrito que otras personas conozcan dichos resultados. Sin embargo, en algunos casos los
resultados de mi prueba podrían ser divulgados a mi cónyuge, a mi(s) compañero(s) sexual(es) o a
la(s) persona(s) con quien(es) haya compartido agujas, al funcionario de salud del condado o a un
proveedor de servicios de atención de la salud que haya estado expuesto en forma considerable
a mi sangre o a otros materiales potencialmente infecciosos o a otras personas, según lo requiera
o autorice la ley. La información relacionada con los resultados de mi prueba se conserva en mi
expediente médico.
Beneficios y Riesgos de la Prueba
Los resultados de la prueba pueden ayudarme a tomar mejores decisiones en cuanto al cuidado
de mi salud y mi vida personal. Los resultados de la prueba pueden ayudarnos a mí y a mi
médico a tomar decisiones con respecto a mi tratamiento médico. Existen numerosas opciones
de tratamiento disponsibles para las personas que presentan resultados positivos a las pruebas
de detección de VIH. Si los resultados son positivos, sé que puedo infectar a otras personas y que
puedo tomar acción para evitarlo.
Los posibles riesgos de la prueba incluyen tensión sicológica, mientras espero los resultados y
ansiedad, si los resultados son positivos.

Page 2 of 3
(03/08)
©CALIFORNIA HOSPITAL ASSOCIATION
Form 23-1S Consent for the HIV Test
Obligaciones Para los Proveedores de Atención Médica Que Solicitan las Pruebas
Un médico u oto proveedor de atención médica que solicita una prueba de detección de VIH debe:
• Informar al paciente que se planea realizar una prueba de detección de VIH.
• Proporcionar al paciente información sobre la prueba de detección de VIH.
• Informar al paciente que existen numerosas opciones de tratamiento disponible para las
personas que presentan resultados positivos a las pruebas de detección de VIH y que una
persona que presenta resultados negativos en una prueba de detección de VIH debería seguir
sometiéndose a pruebas periódicamente, e
• Informar al paciente que tience el derecho de rechazar la prueba de detección de VIH.
Entiendo que, si estuviera embarazada, mi médico me proporcionará información adicional sobre el
VIH y sobre la prueba de detección de VIH en relación a mi estado.
Más Información
Entiendo que antes de que decida tomar esta prueba, debo asegurarme de que he haber hablado
con mi médico sobre cualquier pregunta que tenga sobre la prueba, su significado, sus riesgos y
beneficios, así como cualesquiera alternativas a dicha prueba.
Consentimiento Para la Prueba de Detección del VIH
Al firmar abajo, confirmo que:
• He leído y comprendido la información en este formulario y la entiendo;
• Se me ha proporcionado toda la información que deseo con respecto a la prueba del VIH,
su significado, los beneficios esperados, los posibles riesgos y cualesquiera alternativas a la
prueba y que se me han contestado mis preguntas;
• Entiendo que tengo el derecho de rechazar una prueba de detección de VIH; y
• Doy mi consentimiento para que se realice el examen para detectar el VIH.
Fecha:
Hora: AM / PM
Firma:
(paciente o representante legal)
Si no lo firma el paciente, indique la relación con éste*:
Nombre en letra de imprenta:
(representante legal)

(03/08)
Page 3 of 3
©CALIFORNIA HOSPITAL ASSOCIATION
Form 23-1S Consent for the HIV Test
*Este formulario de consentimiento solamente podrá ser firmado por otra persona que no sea el
paciente bajo las siguientes circunstancias:
1. El paciente tiene menos de doce (12) años de edad o, como resultado de su condición
física o mental, es incompetente para consentir a la prueba de sangre para detectar el
anticuerpo contra el VIH; y
2. La persona que consiente a esta prueba a favor del paciente está legalmente autorizada
para tomar decisiones relacionadas con la atención médica del paciente; por ej., un
representante nombrado por el paciente en un poder notarial para la atención de la
salud; el padre o tutor de un menor; un conservador debidamente autorizado; o, en
circunstancias adecuadas, el familiar disponible más cercano al paciente (véase el Manual
de Consentimiento de CHA, capítulos 2 y 23); y
3. Es necesario obtener del paciente los resultados de la prueba del anticuerpo contra el VIH a
fin de prestarle la debida atención médica o de tomar medidas preventivas.
*This consent may be signed by a person other than the patient only under the following circum-
stances:
1. The patient is under twelve (12) years of age or, as a result of his/her physical or mental
condition, is incompetent to consent to the HIV antibody blood test; and
2. The person who consents to the test on the patient’s behalf is lawfully authorized to make
health care decisions for the patient, e.g., an agent appointed by the patient in a power
of attorney for health care; the parent or guardian of a minor; an appropriately authorized
conservator; or, under appropriate circumstances, the patient’s closest available relative (see
chapters 2 and 23 of CHA’s Consent Manual); and
3. It is necessary to obtain the patient’s HIV antibody test results in order to render appropriate
care to the patient or to practice preventative measures.
NOTE: This form should include taglines as required by the Affordable Care Act.
(See www.calhospital.org/taglines, for detailed information.)
Reference: Health and Safety Code Section 121020

APPENDIX 25-A
Report of a Hospital Death Associated With
Restraint or Seclusion
(06/14)
Page 1 of 1
©CALIFORNIA HOSPITAL ASSOCIATION
Form CMS-10455 (11/13) 1
REPORT OF A HOSPITAL DEATH ASSOCIATED WITH RESTRAINT OR SECLUSION
A. Hospital Information:
Hospital Name CCN
Address
City State Zip Code
Person Filing the Report Filer’s Phone Number
B. Patient Information:
Name Date of Birth
Primary Diagnosis(es)
Medical Record Number Date of Admission Date of Death
Cause of Death
C. Restraint Information (check only one):
While in Restraint, Seclusion, or Both
Within 24 Hours of Removal of Restraint, Seclusion, or Both
Within 1 Week, Where Restraint, Seclusion or Both Contributed to the Patient’s Death
Type (check all that apply):
Physical Restraint Seclusion Drug Used as a Restraint
If Physical Restraint(s), Type (check all that apply):
01 Side Rails
02 Two Point, Soft Wrist
03 Two Point, Hard Wrist
04 Four Point, Soft Restraints
05 Four Point, Hard Restraints
06 Forced Medication Holds
07 Therapeutic Holds
08 Take-downs
09 Other Physical Holds (specify):
10 Enclosed Beds
11 Vest Restraints
12 Elbow Immobilizers
13 Law Enforcement Restraints
If Drug Used as Restraint:
Drug Name Dosage
DEPARTMENT OF HEALTH AND HUMAN SERVICES
CENTERS FOR MEDICARE & MEDICAID SERVICES
Form Approved
OMB No. 0938-1210
Index
Index
1
©CALIFORNIA HOSPITAL ASSOCIATION
A
Abortion
Child abuse, 7.13
Abuse—SeeChild abuse, SeeElder and dependent adult
abuse
Domestic, 7.32 to 7.33
Forensic medical reports, 7.12, 7.27
Records related to abuse, 7.11 to 7.19
Spousal, 7.32 to 7.33
Accounting of disclosures, 6.4
Advance directives, 2.14, 4.15, 5.10
Adverse event reporting, 5.25, 8.7 to 8.10
Advocacy programs, 4.7 to 4.15
Aftercare plan, 4.6
Alcohol or drug abuse, 2.40 to 2.41, 3.2, 6.2
Antipsychotic medications, 2.42 to 2.47
Apology, 8.7
Attorney
Attorney-client privilege, 8.1
Report of incident to attorney, 8.1
Authorization
For use or disclosure of health information, 6.5
B
Battery, unconsented treatment as, 2.1
Breach of privacy or security, 6.3
C
California Department of Health Care Services (DHCS),
3.2
California Department of Public Health (CDPH), 3.1, 6.3,
8.3
California Department of Social Services (CDSS), 3.2
Capacity
Definition of, 2.12
CDPH—SeeCalifornia Department of Public Health
(CDPH)
CDSS—SeeCalifornia Department of Social Services
(CDSS)
Child abuse, 7.8 to 7.19
Abuse-related exams, 7.12
Reporting of, 6.5, 7.8 to 7.19
Clergy
Reporting child abuse, 7.10
Reporting elder or dependent adult abuse, 7.20
Complaint procedure, 4.3
Conditions of admission
Mental health patients, adults (voluntary), 3.4
Mental health patients, (involuntary), 3.15
Confidentiality of Medical Information Act (CMIA),
1.2 to 1.3, 6.1
Consent
Antipsychotic medication, 2.42
Capacity, 2.13
Conservator, 2.15
Convulsive therapy, 2.49
Duration, 2.9
HIV testing, 2.55 to 2.59
How to obtain, 2.9 to 2.12
Informed, 2.5 to 2.9
Intimate partner violence, 2.42
Mental health treatment, 2.39
Minors, 2.24 to 2.39
Psychosurgery, 2.47
Role of hospital, 2.8
Role of the physician, 2.6
Conservatorship, 2.15
AIDS/HIV testing, 2.56
Consent to experimental treatment, 2.16, 2.21
Consent to sterilization, 2.16, 2.22
Electroconvulsive therapy, 2.16, 2.22
Lanterman-Petris-Short Act, 2.15, 3.28
Mental health patient, 3.2, 3.28, 3.31
Convulsive treatment, 2.16, 2.22
Gravely disabled patient, 3.2, 3.8
Involuntary admission to facility, 2.16, 2.21, 3.7,
3.28, 3.31
Voluntary admission to facility (adult), 2.16, 2.21
Permanent, 3.22
Probate Code, 2.15, 3.31
Temporary, 3.22, 3.31
Contraception
Emergency, 7.6
Minor consent to, 2.41

CHA Mental Health Law Manual 2019
2
Index
©CALIFORNIA HOSPITAL ASSOCIATION
Conversion therapy, 4.6
Convulsive therapy, 2.14, 2.49 to 2.53
Conservator may not consent to, 2.16, 2.22
Court order authorizing medical treatment, 2.20, 2.26
Crimes, reporting, 7.1 to 7.38
D
Deadly weapon
Possessed by psychiatric patient, 7.36 to 7.38
Death
Child abuse, 7.8 to 7.19
Dependent adult abuse, 7.19 to 7.30
Elder abuse, 7.19 to 7.30
In restraints, 8.9
In seclusion, 8.9
Notifying family and others, 6.9
Release of information regarding, 6.7
Restraints, 5.2, 8.9
Seclusion, 5.2, 8.9
Sentinel event, 8.5
Dependent adult abuse, 7.19 to 7.30
Photographs of, 7.28
Dependent child of juvenile court, 2.27, 6.12
Detention of patient
Endangered adult, 7.30
Disability Rights California, 4.7 to 4.15
Disappearance of patient
Notifying law enforcement officers, 6.10
Discharge medications, 2.53
Discharge of patient
Mental health patient, 4.6, 6.10
Temporary release, 3.19, 3.25, 3.27
Documentation—See Authorization
Domestic abuse or violence, 7.32 to 7.33
Driver’s License, 6.3
Drug substitutions, 2.54
Duty to warn of dangerous psychiatric patient,
7.33 to 7.35
E
Elder and dependent adult abuse, 7.19 to 7.30
Photographs of, 7.28
Electroconvulsive therapy
Conservator may not consent to, 2.16, 2.22
Elements of informed consent, 2.5
Emergency treatment, 2.3, 2.44, 2.45, 5.14
Endangered adult, 7.30
Error, 8.6, 8.11
Evidentiary exam, 2.41, 7.7, 7.12
Experimental treatment
Who may consent, 2.16, 2.21
F
Family notification, 3.16, 6.7
FDA—SeeFood and Drug Administration (FDA)
Financial interest of physician, 2.5
Food and Drug Administration (FDA), 5.25
Forensic medical reports, 7.12, 7.27
G
Grievance procedure
Privacy complaint, 6.3
Guardianship, 2.29 to 2.30
HIV testing, 2.56
H
Habeas corpus, 3.18, 3.20, 3.22
Health Insurance Portability and Accountability Act
(HIPAA) of 1996, 1.2, 1.3, 6.1
Homeless children, 7.15
Human Immunodeficiency Virus (HIV)
Confidentiality, 6.2
Consent to HIV test, 2.55 to 2.59
Deceased patients, 2.57
Minors, 2.56
Prisoners, 2.57
Release of test results, 6.2
Testing, 2.55 to 2.59
Without consent of patient, 2.58
Test results, 1.3
I
Immunity
Child abuse reports, 7.17 to 7.18
Dependent adult abuse reports, 7.28
Detention of mental health patient awaiting transfer,
3.32
Elder adult abuse reports, 7.28
Firearms in possession of psychiatric patients, 7.38
Notification of family of mental health patient, 6.9
Photographing child abuse victim, 7.18
Photographing elder or dependent adult abuse
victim, 7.28
Providing access to abuse victim, 7.18, 7.28
Release of involuntary mental health patients, 3.6,
3.13, 3.15, 3.19, 3.25, 3.27, 3.32
Reporting neglected/abused patient transferred from
a health facility, 7.31
Transfer-related actions, 3.32
Incident reports, 8.1
Independent clinical review, 3.5
Informed consent, 2.5 to 2.9
Injury or neglect in transferred patient, 7.31

Index CHA
Index
3
©CALIFORNIA HOSPITAL ASSOCIATION
Insulin coma therapy, 2.49 to 2.53
Interdisciplinary team consent, 2.18 to 2.24
Interpreter
Admission of minor to mental health facility, 3.6
Intimate partner violence, 2.42
J
Joint Commission, The
Outcomes of care, 8.7
Periodic performance review, 8.6
Reporting outcome of care to patient, 8.7
L
Laboratory test results—See alsoHuman
Immunodeficiency Virus (HIV), Tuberculosis screening
Lanterman-Petris-Short Act, 1.1 to 1.2, 3.1, 6.1, 6.7
Law enforcement, 5.30
Release of information to, 2.57
Law enforcement officers
Duty to notify of dangerous patient, 7.33 to 7.35
Release of information to, 3.12, 3.19, 6.10,
7.1 to 7.38
Reporting crimes, 7.1 to 7.38
M
Malpractice, unconsented treatment as, 2.2
Maternity patient
Maternal substance abuse, 7.14 to 7.15
Minor, 7.13
Substance abuse, 7.14
Mature minor doctrine, 2.37
Medical devices
Reporting injuries, 8.11
Safe Medical Devices Act, 8.11 to 8.14
Tracking, 8.13
Medical errors, 8.5
Medical record
Alcohol or drug abuse patient, 6.2
Amendment of, 6.4
Confidentiality of Medical Information Act (CMIA), 6.1
Contents
Abuse forensic medical reports, 7.12, 7.27
Incident report, 8.1
Mental health patient, 6.1
Patient privacy rights, 6.4
Substance abuse patient, 6.2
Medical record, release of information
Deceased patient, 2.57
Medical record, release of information from, 6.1 to 6.14
Accounting for disclosures, 6.4
Alcohol or drug abuse patient, 6.2
Breach, 6.2
HIV test results, 6.2
Law enforcement officers, to, 3.12, 3.19
Mental health patient, 6.7, 6.10
Patient, to the, 6.4
Substance abuse patient, 6.2
Medical staff quality assurance, 8.1
Medication assisted treatment, 2.35
Medication errors, 8.11
Medications
Discharge, 2.53
Drug substitutes, 2.54
Emergency contraception, 7.6
Errors, 5.27
Outpatient, 2.53
Mental health advocate, 4.7 to 4.15
Mental health patient
Adults, voluntary admission, 3.2
Possession of weapon, 7.36 to 7.38
Records, 6.1 to 6.14
Mental health treatment, 2.16, 2.21
Military, 2.38
Minimum necessary, 6.5
Minor patients, 2.24 to 2.39
Abandoned, 2.33
Adopted, 2.28, 2.32
Alcohol or drug abuse, 2.40
Blood donation, 2.42
Born out of wedlock, 2.28
Capacity to consent, 2.37
Caregiver authorization affidavit, 2.30
Contraception, 2.41
Disagreement with parents, 2.25, 2.36
Divorced parents, 2.27
Emancipation, 2.37
Financial responsibility for, 2.25
Foster parents, 2.34
Gravely disabled, 3.16
Guardian consent, 2.29
HIV testing, 2.56
Homeless, 7.15
Intimate partner violence, 2.42
Married or previously married, 2.39
Mental health treatment, 2.39
Minors in custody of juvenile court, 2.27
Minors in custody of probation officer, 2.34
Minors in custody of social worker, 2.34
Minors on active duty with U.S. armed forces, 2.38
Nonabandoned minors
Parents are unavailable, 2.32
Outpatient mental health treatment, 2.39
Parental consent, 2.27
Pregnancy care, 2.41
Privacy rights, 2.25, 6.12 to 6.13

CHA Mental Health Law Manual 2019
4
Index
©CALIFORNIA HOSPITAL ASSOCIATION
Rape victims, 2.41, 7.5 to 7.7
Refusal of treatment, 2.26
Self-sufficient minors, 2.38
Sexual assault victims, 2.41, 7.5 to 7.7
Substance abuse, 2.40
Third party consent, 2.30
Victims of child abuse, 2.35
Where refusal of treatment may cause serious harm,
2.26
Withdrawal or withholding of life-sustaining
treatment, 2.26
N
Noncustodial parent, 2.28
Notice of Privacy Practices, 6.4
Notification of family, 3.16
O
Occupational injuries
Exposure to blood or bodily fluids, 2.57 to 2.58
Office for Civil Rights (OCR), 6.3
Opioids, 2.35
Outcomes, informing patients, 8.7
Outpatient medications, 2.53
P
Partner abuse, 7.19 to 7.30, 7.32 to 7.33
Patient-authorized disclosures, 6.5
Patient death—SeeDeath
Patient rights, 4.1 to 4.6, 5.2 to 5.3
Access to medical records, 6.2
Denial of rights, 4.4
Family notification, 6.7
Privacy, 6.1 to 6.14
Patient Safety Organization (PSO), 8.2
Patient safety plan, 8.4
Patients’ rights advocates—SeeMental health advocate
Periodic performance review, 8.6
Pharmacy, 8.11
Photograph, consent to
Child abuse, 7.18
Dependent or elder abuse, 7.28
Sexual assault suspect, 7.7
Physician
Medical staff quality assurance, 8.1
Physician-patient privilege, 7.15
Psychotherapist-patient privilege, 7.15
Prisoners
Discharge information and movement information to
law enforcement officers, 3.12, 3.19
Release of information, 3.12, 3.19
Reporting crimes, 7.1 to 7.38
Privacy officer, 6.4
Privacy right, 7.1
Privacy rights, 2.40
Privilege
Attorney-client, 8.1 to 8.3
Evidence Code 1157
Medical staff quality assurance, 8.1
Physician-patient, 7.15
Psychotherapist-patient, 7.15
Probation officer, 2.34
Property of patient
Searching, 6.13
Protected health information (PHI)
Use and disclosure
CMIA—SeeConfidentiality of Medical
Information Act (CMIA)
LPS—SeeLanterman-Petris-Short Act
Protection and advocacy, 4.14
Psychiatric advance directives, 2.14 to 2.24,
4.15 to 4.16, 5.10
Psychiatric records, 6.1 to 6.14—See
alsoPsychotherapy notes
Psychosurgery, 2.14, 2.47 to 2.49
Minor may not be subject to, 2.40
Psychotherapist, 2.38
Duty to warn, 7.34 to 7.35
Psychotherapist-patient privilege, 1.3, 7.15
Psychotherapy notes, 6.2
Psychotropic medications, 2.40, 2.42 to 2.47, 3.11
Involuntary patient, 2.44 to 2.47, 3.11
Minor, 2.40, 2.47
Public health officer, 8.15
Q
Quality assurance, 8.1
R
Rape, 2.41
Refusal of treatment, 2.2
Minor, 2.26
Religious beliefs, 2.26
Reparation therapy, 4.6
Reporting
Adverse events, 8.7 to 8.10
Assault and abuse, 7.1 to 7.38
Child abuse, 7.8 to 7.19
Crimes, 7.1 to 7.38
Dependent adult abuse, 7.19 to 7.30
Disclosure of medical information,
6.4
Diseases/conditions, 7.1 to 7.38
Elder abuse, 7.19 to 7.30
Medical errors, 8.4, 8.11

Index CHA
Index
5
©CALIFORNIA HOSPITAL ASSOCIATION
Medication errors, 5.27, 8.11
Minor with sexually-related condition, 7.13
Safe Medical Devices Act, 8.11 to 8.14
Sexual assault/rape, 7.5, 7.9, 7.22
Unusual occurrences, 5.27, 8.14
Report to attorney, 8.1
Residential shelter services, 2.39
Restraint, 4.5, 5.1 to 5.32
S
Safe Medical Devices Act, 5.25, 8.11 to 8.14
Searching patients and belongings, 6.13
Seclusion, 4.5, 5.1 to 5.32
Security officer, 6.4
Self-sufficient minor, 2.38
Sentinel event, 5.27, 8.5
Sexual activity with patient, 4.16
Sexual assault, 7.5 to 7.7, 7.9, 7.13
Adults, 7.6
Minors, 2.41, 7.13
Records, 7.5, 7.6
Sexually transmitted disease, 7.13
Sexual orientation change therapy, 4.6
Social Security numbers, 6.3, 8.14
Social worker, 2.34
Spousal abuse, 7.19 to 7.30, 7.32 to 7.33
Staff injury, 5.27
Sterilization, 2.14
Sterilization, consent to
Conservator consent to, 2.16, 2.22
Strike, 8.14
Substance abuse records—SeeAlcohol or drug abuse
Substance use disorder records—SeeAlcohol or drug
abuse
Support person, 7.6
Surrogate decision maker, 2.14
Sympathy, statements of, 8.7
T
Tarasoff v. Regents of the University of California, 7.33
Telemedicine/telehealth, 2.54
Consent, 2.54
Therapeutic privilege, 2.4
Tissue
Release of medical information regarding, 2.58
Use for research or commercial purposes, 2.2,
2.5
Transfer, patient
Injury in, 7.31
Neglect in, 7.31
U
Unanticipated outcomes, 8.7
Unrepresented patient, 2.19
Unusual occurrences, 8.14
Unusual occurrences reporting, 5.27
V
Verification of identity, 6.6
W
Weapons
Psychiatric patients, prohibition against possession,
7.36 to 7.38
Workplace exposures—SeeOccupational injuries
X
X-rays
Consent to, 7.12
