QUALITY CONTROL MANUAL
Radiologist’s Section
MRI Technologist’s Section
Medical Physicist/MRI Scientist’s Section
American College of Radiology
Committee on Quality Assurance in Magnetic Resonance Imaging
Ron Price, PhD, FACR, chairman
Jerry Allison, PhD, FACR
Georey Clarke, PhD, FACR
Michael Dennis, PhD
R. Edward Hendrick, PhD, FACR
Carl Keener, PhD
Je Masten, MS
Moriel Nessaiver, PhD
Joe Och, MS
Donna Reeve, MS
Priscilla Butler, MS, ACR Sta Member
Dina Hernandez, RT, ACR Sta Member
Leonard Lucey, JD, ACR Sta Member
Pam Wilcox, MBA, ACR Sta Member
2015
Magnetic Resonance Imaging
© Copyright 2015, American College of Radiology. All rights reserved.

Magnetic Resonance Imaging Quality Control Manual iii
Contents
PREFACE . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .vi
REVISIONS . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3
Radiologist’s Section
INTRODUCTION ..............................................4
DEFINITIONS. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 6
A. Quality Assurance . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 6
B. Quality Assurance Committee .........................6
C. Quality Control . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 6
RADIOLOGISTS’ RESPONSIBILITIES ............................8
A. The Supervising Radiologist ...........................8
B. All MRI Radiologists (Interpreting Physicians) . . . . . . . . . . . 8
C. Interpretive Quality Assurance .........................9
D. Radiologist’s Leadership Role in MRI Quality Control . . . . 9
E. MRI Quality Assurance Procedures Manual .............10
OTHER PROFESSIONALS’ RESPONSIBILITIES ..................12
A. The Responsibilities of the Qualied Medical Physicist or
MRI Scientist .........................................12
B. Baseline Measurements and Action Limits .............12
C. Purchase Specications and Acceptance Testing ......12
D. MRI QC Technologist’s Responsibilities . . . . . . . . . . . . . . . . 13
E. Quality Control of Hard-Copy and Soft-Copy Images ...14
CONCLUSION ...............................................15
REFERENCES ...............................................16
A. Downloadable from ACR Website .....................16
B. Other Publications. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 16
MRI Technologist’s Section
REVISIONS. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 19
INTRODUCTION .............................................20
IMPORTANT POINTS .........................................22
A. Quality Control Testing Frequency ....................22

iv Magnetic Resonance Imaging Quality Control Manual
Contents
B. Designated Quality Control Technologist(s) . . . . . . . . . . . . 22
C. Quality Control Log . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 23
D. Quality Control Data Review . . . . . . . . . . . . . . . . . . . . . . . . . . 23
E. Alternative Phantoms ................................23
F. Alternative Procedures ................................24
G. Action Limits .........................................24
TECHNOLOGIST’S WEEKLY MRI QUALITY CONTROL . . . . . . . . . . . 25
A. Setup and Table Position Accuracy ....................26
B. Axial Image Data: Prescan Parameters .................29
C. Image Data Measurements ...........................32
FILM PRINTER QUALITY CONTROL ...........................47
VISUAL CHECKLIST ..........................................51
REFERENCES . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 52
APPENDIX ..................................................53
Medical Physicist/MRI Scientist’s Section
REVISIONS . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 56
ROLE OF THE QUALIFIED MEDICAL PHYSICIST OR MRI SCIENTIST
IN THE IMAGE QC PROGRAM ................................57
A. Changes Since 2004 Version ..........................58
ESTABLISHING THE QUALITY CONTROL PROGRAM ...........60
A. Phantom Section .....................................60
B. Methods and Action Limits for Weekly Quality
Control Tests. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 61
C. Establishing Action Limits for Weekly MR Image Quality
Control Tests .........................................62
ANNUAL MRI SYSTEM PERFORMANCE EVALUATION ..........70
A. Magnetic Field Homogeneity .........................72
1. Spectral Peak Option ...............................74
2. Bandwidth-Dierence Option . . . . . . . . . . . . . . . . . . . . . . . 74
3. Phase Map Option . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 77
4. Phase-Dierence Map Option . . . . . . . . . . . . . . . . . . . . . . . 80

Magnetic Resonance Imaging Quality Control Manual v
Contents
B. Slice-Position Accuracy ...............................87
C. Slice-Thickness Accuracy. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 88
D. Radiofrequency Coil Checks ..........................90
1. Volume Coil Tests . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 96
2. Surface Coil Tests ..................................103
3. RF Array Coils. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .105
E. Soft-Copy (Monitor) Quality Control ..................109
F. MR Safety Program Assessment. . . . . . . . . . . . . . . . . . . . . . .111
REFERENCES . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .113
APPENDIX .................................................116
A. MRI Equipment Evaluation Summary Form ...........116
B. MRI Safety Program Assessment Checklist ............116
C. Hard-Copy (Film) Quality Control Operating Levels ....116

vi Magnetic Resonance Imaging Quality Control Manual
Preface
e Magnetic Resonance Imaging Accreditation Program of the
American College of Radiology was established to attest to the quality
of the performance of magnetic resonance imaging at accredited
facilities. Accreditation received through this program assures patients,
referring physicians and others that magnetic resonance imaging studies
at accredited sites are only performed by well-trained and competent
personnel using properly functioning equipment.
All sites accredited by the American College of Radiology in magnetic
resonance imaging have agreed to carry out a continuous program of
magnetic resonance imaging equipment quality control. e Committee
on MRI Accreditation has received many inquires regarding what would
constitute an adequate magnetic resonance imaging equipment quality
control program and what the appropriate roles of various health care
professionals at these clinics should be.
is manual is designed to assist facilities in testing and maintaining
their magnetic resonance imaging equipment in accordance with the
broad principles delineated in the ACR-AAPM Technical Standard
for Diagnostic Medical Physics Performance Monitoring of Magnetic
Resonance Imaging Equipment [Res. 34–2014]. e committee has
applied these principles to describe which personnel are responsible for
which specic tasks and delineate methods for evaluating equipment
performance with many tests using the American College of Radiology’s
magnetic resonance imaging phantom.
Members of the ACR Subcommittee on MRI Accreditation physics
who generously donated their time and experience to produce the
ACR Magnetic Resonance Imaging Quality Control Manual are listed
on the title page. Special thanks goes to Pamela Wilcox, executive
vice president of Quality & Safety, and Leonard Lucey, senior director
of accreditation, who have kept this project and the other ACR
accreditation programs on track over the years.
Anthony Scuderi, M.D.
Chairman, ACR Committee on MRI Accreditation
PREFACE
Radiologist’s Section
2015
Magnetic Resonance Imaging
QUALITY CONTROL MANUAL

2 Magnetic Resonance Imaging Quality Control Manual
Contents
REVISIONS ...................................................3
INTRODUCTION ..............................................4
DEFINITIONS .................................................6
A. Quality Assurance ...................................6
B. Quality Assurance Committee ........................6
C. Quality Control ......................................6
RADIOLOGISTS’ RESPONSIBILITIES ............................8
A. The Supervising Radiologist ..........................8
B. All MRI Radiologists (Interpreting Physicians) .........8
C. Interpretive Quality Assurance ........................9
D. Radiologist’s Leadership Role in MRI Quality Control ...9
E. MRI Quality Assurance Procedures Manual .......... 10
OTHER PROFESSIONALS’ RESPONSIBILITIES ................. 12
A. The Responsibilities of the Qualied Medical Physicist or
MRI Scientist ....................................... 12
B. Baseline Measurements and Action Limits ........... 12
C. Purchase Specications and Acceptance Testing .... 12
D. MRI QC Technologist’s Responsibilities ............. 13
E. Quality Control of Hard-Copy and Soft-Copy Images . 14
CONCLUSION .............................................. 15
REFERENCES .............................................. 16
A. Downloadable from ACR Website ................... 16
B. Other Publications ................................. 16

4 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
II. Introduction
Magnetic resonance imaging (MRI) is now a mature and widely used
imaging method. ere is signicant variability, however, in the quality
of MRI exams performed at dierent sites. Achieving the full potential of
MRI requires careful attention to quality assurance (QA), both in regard
to equipment performance and to the execution of imaging studies. In
response to the concerns of both referring physicians and those institutions
reimbursing for the costs of performing MRI, the American College of
Radiology (ACR) has initiated a voluntary MRI accreditation program.
is program has followed the approach of the ACR Mammography
Accreditation Program, which has established practices and standards
for QA and quality control (QC) in mammography.
e MRI Accreditation Program looks at the general practice of clinical
MRI. Specic clinical examinations and QC data are required. Sites are
asked to send their best examinations for selected clinical studies for
peer-review. As part of the program, QC data must be collected using a
head phantom test object.
During this time, the ACR has also developed specic standards related
to MRI and appropriateness criteria. With improved standards, widely
accepted acknowledgment of the worth of accreditation, and a growing
body of criteria underpinning MRI practice, the ACR Committee on
Standards and Accreditation (now called the Commission on Quality
and Safety) recognized the need to reassess the mechanisms by which
a radiology department or MRI clinic maintains high quality over time.
Quality radiological care, long envisioned as something that owed
directly from the radiologist, has become the responsibility of the
entire radiology group, including MRI technologists, qualied medical
physicists, qualied MRI scientists, administrators, service engineers,
nurses, and other physicians. All of these individuals play a part in
maintaining quality and guaranteeing benecial outcomes. e process,
rather than the individual, is the focus of continuous QA and analysis.
e key to continuous quality improvement is a vigorous and adaptive QA
program. e Radiologist’s Section details the radiologist’s responsibilities
in an ongoing MRI QC program. e MR supervising radiologist has
the responsibility for ensuring that all QA requirements are met. e
qualied medical physicist/MRI scientist is responsible for overseeing all
equipment-related QA practices. e QC technologist is specially trained
and given responsibility to conduct QA/QC activities not assigned to the
lead MRI radiologist or the medical physicist/MRI scientist, including
weekly QC testing of the MRI system.
Details of the tests to be performed by the technologist and the qualied
medical physicist/MRI scientist are given in two separate sections, the
MRI Technologist’s Section and the Medical Physicist/MRI Scientist’s
Section. e stated frequency for QC tests is a minimum frequency. A
test should be done more frequently when it is being introduced and
whenever inconsistent results are found. In addition, it is important to
adopt the attitude that QA and QC are continuous, not episodic, processes.
INTRODUCTION

Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 5
II. Introduction
RADIOLOGIST’S SECTION RADIOLOGIST’S SECTION
An eective QC program will not eliminate all problems but can allow
for the identication of problems before they seriously aect clinical
results. QC in more recently developed clinical applications such as
magnetic resonance (MR) angiography, cardiac MRI, diusion-weighted
and susceptibility-weighted MRI, MR elastography, MR spectroscopy,
functional MRI, and MR image-guided biopsy and therapy have not been
addressed in this manual.
e radiologist and technologist must look at every study with QA in
mind. Deviations from high-quality performance may occur quickly
or gradually. Abrupt changes in quality may be detected during routine
clinical work. More gradual or subtle changes may require regular
QC testing for detection. e QC program provides a framework
within which even gradual or subtle problems can be identied,
isolated, and resolved.

6 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
III. Denitions
A. Quality Assurance
Quality assurance in MRI is a comprehensive concept that comprises all
of the management practices developed by the MR imaging team led by
the MR supervising radiologist to ensure that:
1. Every imaging procedure is necessary and appropriate to the
clinical problem at hand
2. e images generated contain information critical to the solution
of the problem
3. e recorded information is correctly interpreted and made
available in a timely fashion to the patient’s physician
4. e examination results in the lowest possible risk, cost, and
inconvenience to the patient consistent with objectives above
B. Quality Assurance Committee
e QA program includes many facets, including ecacy studies,
continuing education, QC, preventive maintenance, safety, and calibration
of equipment. An essential part of the QA program is the QA Committee
(QAC). is group has responsibility for oversight of the program,
setting the goals and direction, determining policies, and assessing the
eectiveness of QA activities. e QAC should consist of the following:
• One or more radiologists
• A qualied medical physicist or MRI scientist
• A supervisory MR technologist
• Other radiology department personnel involved in caring
for MRI patients, including a nurse, desk attendant, medical
secretary, or others
• Personnel outside the radiology department, including medical
and paramedical sta such as referring physicians
Anyone who helps provide care to the patient to be studied with MRI
should be considered as a possible member of the QAC because his or her
eorts aect the quality of care and the satisfaction of the patient.
C. Quality Control
Quality control is an integral part of quality assurance.
Quality control is a series of distinct technical procedures that ensure the
production of a satisfactory product, in this case, high-quality diagnostic
images. Four steps are involved:
1. Acceptance testing to detect defects in equipment that is newly
installed or has undergone major repair
DEFINITIONS

Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 7
III. Denitions
RADIOLOGIST’S SECTION RADIOLOGIST’S SECTION
2. Establishment of baseline performance of the equipment
3. Detection and diagnosis of changes in equipment performance
before they become apparent in images
4. Verication that the causes of deterioration in equipment
performance have been corrected
Acceptance testing should take place before the rst patient is scanned
and aer major repairs. Major repairs include replacement or repair of
the following subsystem components:
• Gradient ampliers
• Gradient coils
• Magnet
• Radiofrequency (RF) amplier
• Digitizer boards
• Signal processing boards
A baseline check should be carried out on the MRI system as a whole
and on additional subsystems, such as repaired, replaced, or upgraded
RF coils. All records should be kept at a central location near the
MRI scanner(s).
Specics of the QC program for MRI are provided by the ACR in
this manual.

8 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
IV. Radiologists’ Responsibilities
A. The Supervising Radiologist
e supervising radiologist’s specic responsibilities in MRI QC are to:
1. Ensure that technologists have adequate training and continuing
education in MRI.
2. Provide an orientation program for technologists based on a
carefully established procedures manual (see Section E).
3. Ensure that an eective QC program exists for all MR imaging
performed at the site. e supervising radiologist should
provide motivation, oversight, and direction to all aspects of
the QC program.
4. Select the technologist to be the primary QC technologist,
performing the prescribed QC tests.
5. Ensure that appropriate test equipment and materials are available
to perform the technologist’s QC tests.
6. Arrange stang and scheduling so that adequate time is available
to carry out the QC tests and to record and interpret the results.
7. Provide frequent and consistent positive and negative feedback
to technologists about clinical image quality and QC procedures.
8. Participate in the selection of a qualied medical physicist or
MRI scientist who will administer the QC program and perform
the physicist’s tests.
9. Review the technologist’s test results at least every three months,
or more frequently if consistency has not yet been achieved.
10. Review the results of the qualied medical physicist or MRI
scientist annually, or more frequently when needed.
11. Oversee or designate a qualied individual to oversee the MRI
safety program for employees, patients, and other individuals in
the surrounding area.
12. Ensure that records concerning employee qualications, MRI
protocols, and procedures, QC, safety, and protection are
properly maintained and updated in the MRI QA Procedures
Manual (Section E).
B. All MRI Radiologists (Interpreting Physicians)
Responsibilities of all MRI radiologists (interpreting physicians) in MRI
QC are to:
1. Ensure that established protocols are followed.
2. Follow the facility procedures for corrective action when asked to
interpret images of poor quality.
RADIOLOGISTS’
RESPONSIBILITIES

Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 9
IV. Radiologists’ Responsibilities
RADIOLOGIST’S SECTION RADIOLOGIST’S SECTION
3. Participate in the facility’s practice improvement program.
4. Provide documentation of their current qualications to
each MRI facility where they practice, according to the ACR
Accreditation Program and local rules.
C. Interpretive Quality Assurance
In addition, the radiologist needs to be involved in an ongoing process of
QA to assess the quality of MRI interpretation. Such a program should
include the following:
•
A double reading in which two physicians interpret the same study
• A process that allows a random selection of studies to be reviewed
on a regularly scheduled basis
• Exams and procedures representative of the actual clinical
practice of each physician
• Reviewer assessment of the agreement of the original report with
subsequent review (or with surgical or pathological ndings)
• A classication of peer-reviewed ndings with regard to level of
quality concerns (e.g., a 4-point scoring scale)
• Policies and procedures for action on signicant discrepant
peer-reviewed ndings for the purpose of achieving quality
outcomes improvement
• Summary statistics and comparisons generated for each physician
by modality
• Summary data for each facility/practice by modality
Procedures for interpretive QA are not specically addressed in this
manual.
e QC tests outlined in this ACR Quality Control Manual are divided
into a MRI Technologist’s Section and a Medical Physicist/MRI Scientist’s
Section. Relevant tests are described in detail in a “cookbook” style in
these two accompanying sections. e radiologist should ensure that
these sections are available to the appropriate personnel.
D. Radiologist’s Leadership Role in MRI Quality
Control
1. Radiologists performing MRI must assume the primary
responsibility for the quality of MRI and for the implementation
of an eective QA program at their site. e sta’s commitment
to high quality will oen mirror that of the radiologist in charge.
e individuals performing QC tests need to know that the
radiologist understands the program and is interested in the

10 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
IV. Radiologists’ Responsibilities
results. e radiologist needs to review the test results and trends
periodically and provide direction when problems are detected.
2. e radiologist must make sure that adequate time is available
for the QC program. Most tests take little time (see the MRI
Technologist’s Section, Table 1). However, the necessary time
must be incorporated into the daily schedule.
3. To ensure consistency in QC test performance, a single
technologist should be selected for each MRI system. It is not
desirable, for example, to rotate this assignment among a group
of technologists. Such a practice would introduce into the test
results variability extraneous to the items being tested.
4. A qualied medical physicist or MRI scientist on-site (or one
who is readily available) should administer each facility’s QC
program, perform the tests designated as medical physicist QC
tests and oversee the work of the QC technologist(s). Where
this is not feasible and during the MRI scientist’s or qualied
medical physicist’s absence, the radiologist should oversee the
QC program.
5. e radiologist is ultimately responsible for the quality of
images produced under his or her direction and bears ultimate
responsibility for both proper QC testing and QA procedures
in MRI.
E. MRI Quality Assurance Procedures Manual
Working as a team, the radiologist, QC technologist, and qualied
medical physicist or MRI scientist should develop and follow an MRI QA
procedures manual that is available to all members of the sta. e QC
testing described in this ACR QC Manual should be a central part of the
site’s QA procedures manual.
In addition, the site’s procedures manual should contain:
1. Clearly assigned responsibilities and clearly developed procedures
for QA/QC testing
2. Records of the most recent QC tests performed by the QC
technologist and qualied medical physicist or MRI scientist
3. A description of the orientation program for operators of MRI
equipment, including its duration and content
4. Procedures for proper use and maintenance of equipment
5. MRI techniques to be used, including pertinent information
on positioning, coils, pulse sequences, and contrast agent
administration
6. Precautions to protect the patient and equipment from potential
hazards associated with the strong static magnetic, pulsed
magnetic eld gradients, and RF elds associated with MRI

Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 11
IV. Radiologists’ Responsibilities
RADIOLOGIST’S SECTION RADIOLOGIST’S SECTION
7. Proper maintenance of records, including records of QC and QA
testing, equipment service and maintenance, and QA meetings
8. Procedures for the cleaning and disinfection of MRI systems and
ancillary equipment

12 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
V. Other Professionals’ Responsibilities
A. The Responsibilities of the Qualied Medical
Physicist or MRI Scientist
e responsibilities of the qualied medical physicist or MRI scientist
relate to equipment performance, including image quality and patient
safety. An MRI equipment performance review should take place at the
time the equipment is commissioned and at least annually thereaer. e
qualied medical physicist/MRI scientist shall repeat appropriate tests
aer major repair or upgrade to the MRI system.
Specic tests include the following:
1. Magnetic eld homogeneity evaluation
2. Slice-position accuracy
3. Slice-thickness accuracy
4. RF coil checks, including signal-to-noise ratio and image intensity
uniformity of volume coils
5. So-copy (monitors) QC
6. MR safety program assessment
B. Baseline Measurements and Action Limits
e qualied medical physicist or MRI scientist is responsible for
running baseline QC measurements. e qualied medical physicist
or MRI scientist establishes performance criteria for the technologist’s
QC program. is applies specically to the determination of “action
limits,” which are the values of specic parameters obtained from the
QC tests at which service is requested to address a particular problem in
image quality.
During the annual review, the qualied medical physicist or MRI scientist
also examines the records of the weekly QC tasks performed by the QC
technologist(s). Following this review and the completion of the tests
listed above, recommendations may be made regarding improvements in
equipment performance or improvements in the QC process.
C. Purchase Specications and Acceptance Testing
Many manufacturers sell MRI systems with a large variety of features
and a wide range of prices. e quality of available units varies, but due
to its complexity an MRI system’s quality may be dicult to discern
before the purchase.
e quality of new equipment can be ensured through the use of purchase
specications. Purchase specications also describe to vendors the type
of equipment that is desired by the purchaser. Purchase specications
usually require vendors to provide detailed technical and performance
specications to the purchaser prior to the selection of equipment. ese
OTHER
PROFESSIONALS’
RESPONSIBILITIES

Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 13
V. Other Professionals’ Responsibilities
RADIOLOGIST’S SECTION RADIOLOGIST’S SECTION
vendor-provided specications can then be used to help determine the
equipment to be purchased and provide a set of quantitative performance
specications to be compared with measurements on the MRI equipment
during acceptance testing.
e purchase should be made contingent on satisfactory performance
during acceptance testing. Acceptance testing is more rigorous than the
QC program detailed here and should be conducted by an experienced
medical physicist or MRI scientist. e QC program described in this
manual can provide a minimum set of acceptance tests but is intended
primarily to document consistency of performance aer the unit has
been accepted and put into service.
Once acceptance testing has been completed, there must be adequate
applications training for the entire MR sta.
D. MRI QC Technologist’s Responsibilities
e MRI QC technologist’s responsibilities revolve around image quality.
More specically, the functions performed by the technologist that aect
image quality are patient positioning, image production, image archiving,
and lm processing.
e specic weekly QC procedures to be conducted by the radiological
technologist include the following:
1. Setup and table position accuracy
2. Center frequency
3. Transmitter gain or attenuation
4. Geometric accuracy measurements
5. High-contrast spatial resolution
6. Low-contrast detectability
7. Artifact evaluation
8. Film printer quality control (if applicable)
9. Visual checklist
Although it is written primarily for the QC technologist, the radiologist
should read in detail Section III, Important Points, in the MRI
Technologist’s Section.

14 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
V. Other Professionals’ Responsibilities
E. Quality Control of Hard-Copy and Soft-Copy
Images
Image display QC is essential for accurate interpretation of MR images.
If images are interpreted from lm, the supervising radiologist should
regularly review the MRI QC technologist’s records on hard copy
image QC. e interpreting radiologist should notice and call the MRI
technologist’s attention to image quality problems, including artifacts,
whenever they occur.
If images are interpreted from lm, radiologists should refer to the MRI
Technologist’s Section V, Film Printer Quality Control, and be thoroughly
familiar with these procedures. Sensitometry should be performed and
results plotted before patient images are printed for interpretation. e
radiologist should be comfortable reviewing the results of sensitometric
testing and should ensure that appropriate steps are taken when test
results are outside of control limits.
It is more common for radiology departments and MRI clinics to obtain
diagnoses from images displayed on review workstations with high-
quality monitors. Proper viewing conditions and computer workstation
monitor performance are essential in MRI, as in other areas of radiology.
e radiologist should give particular attention to the information given
in the Medical Physicist/MRI Scientist’s Section IV.E.

Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 15
VI. Conclusion
RADIOLOGIST’S SECTION RADIOLOGIST’S SECTION
In addition to this technical QC program, the MRI radiologist needs
to be involved in an ongoing program to assess the quality of MRI
interpretations. Procedures for interpretive QA are not addressed in this
manual, but have been published in the radiological literature.
e public expects our profession to provide accurately interpreted MR
images of the highest quality. Only a strong, consistent commitment to
QA by all parties involved in performing MRI will validate that trust.
CONCLUSION

16 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
VII. References
A. Downloadable from ACR Website
– Magnetic Resonance Imaging Accreditation Program Requirements
– Breast Magnetic Resonance Imaging Accreditation Program Requirements
– Phantom Test Guidance for the ACR MRI Accreditation Program
– ACR-AAPM Technical Standard for Diagnostic Medical Physics
Performance Monitoring of Magnetic Resonance Imaging (MRI)
Equipment
– ACR Practice Parameter for Performing and Interpreting Magnetic
Resonance Imaging (MRI)
– ACR Manual on Contrast Media, version 9, published 2013
– ACR MRI Terminology Glossary Resource
B. Other Publications
– Kanal E, Barkovich AJ, Bell C, et al. ACR guidance document on MR
safe practices: 2013. Journal of Magnetic Resonance Imaging. 2013;37(3):
501-530.
– Gilk T, Kanal E. Interrelating sentinel event alert #38 with the ACR guidance
document on MR safe practices: 2013. An MRI accreditation safety review
tool. Journal of Magnetic Resonance Imaging. 2013;37(3):531-543.
REFERENCES

MRI Technologist’s Section
2015
Magnetic Resonance Imaging
QUALITY CONTROL MANUAL

18 Magnetic Resonance Imaging Quality Control Manual
Contents
REVISIONS ................................................................................................... 19
INTRODUCTION.......................................................................................... 20
IMPORTANT POINTS ................................................................................. 22
A. Quality Control Testing Frequency ......................................... 22
B. Designated Quality Control Technologist(s) ....................... 22
C. Quality Control Log ...................................................................... 23
D. Quality Control Data Review ................................................... 23
E. Alternative Phantoms ................................................................. 23
F. Alternative Procedures ................................................................ 24
G. Action Limits .................................................................................. 24
TECHNOLOGIST’S WEEKLY MRI QUALITY CONTROL ..................... 25
A. Setup and Table Position Accuracy ........................................ 26
B. Axial Image Data: Prescan Parameters ................................. 29
C. Image Data Measurements ....................................................... 32
FILM PRINTER QUALITY CONTROL ...................................................... 47
VISUAL CHECKLIST .................................................................................... 51
REFERENCES ................................................................................................ 52
APPENDIX ..................................................................................................... 53

20 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
II. Introduction
A well-designed, well-documented, and reliably executed quality control
(QC) program is essential to consistent production of high quality MR
images. e American College of Radiology (ACR) has developed the
material in this manual to assist radiologists, radiological technologists,
and qualied medical physicists or magnetic resonance imaging (MRI)
scientists in establishing and maintaining such QC programs. is is in
accordance with the ACR’s educational and patient service missions and
in response to growing requests from the diagnostic imaging community
for guidance on MRI QC [1,2].
is section of the manual describes the MRI technologist’s duties in
the QC program. At rst glance, the careful and necessarily detailed
descriptions may make it seem as if the technologist’s part is complex
and time-consuming, but that is not the case. It can be carried out with a
minimal investment in time and equipment. In essence, the technologist’s
responsibilities include regularly performing a set of short QC procedures,
recording the procedure results in a QC log, and initiating appropriate
corrective actions as needed.
ere are seven main parts to this section: Part II is this introduction.
Part III discusses important points of general relevance, such as the QC
log. Parts IV, V, and VI describe the individual QC procedures. Part VII
is a list of useful references. Part VIII is an appendix, which contains
examples of useful data forms.
Each procedure description follows the same format:
• Objective
• Frequency
• Required equipment
• Test procedure steps
• Data interpretation and corrective actions
Table 1 provides an overview of the technologist’s QC tests; it lists the
required procedures, the minimum frequency for performing each test,
and approximately how long each task should take.
e MRI technologist, qualied medical physicist or MRI scientist, and
radiologist constitute a QC team. It is important that they work together
as a team. Each should be aware of the others’ responsibilities, especially
as they relate to their own.
With respect to the technologist, the qualied medical physicist or MRI
scientist has two important QC functions:
• e qualied medical physicist or MRI scientist is responsible
for verifying the correct implementation and execution of the
technologist’s QC procedures. Normally this will entail some
supervision and guidance from the qualied medical physicist or
MRI scientist at the initiation of the QC program. e qualied
INTRODUCTION

Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 21
II. Introduction
MRI
TECHNOLOGIST’S SECTION
medical physicist or MRI scientist must conduct a review of
the QC log maintained by the technologist on an annual basis,
although a quarterly review is preferred.
• e qualied medical physicist or MRI scientist is a resource
to answer questions concerning image quality and to provide
assistance in identifying and correcting image quality problems.
Note: If the medical physicist determines that there is a need
for corrective action, the facility should provide a copy
of its medical physicist’s full report to its equipment
service engineer.
With respect to the technologist, the radiologist has three important QC
roles:
• e radiologist informs the technologist about image quality
problems noticed in the course of interpreting clinical images.
is is oen the rst indicator of a QC problem.
• When image quality problems arise, the radiologist decides
whether patient studies can continue or must be postponed
pending corrective action.
• e radiologist participates in the initial assessment of image
quality at establishment of the QC program, and is responsible
for monitoring QC results.

22 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
III. Important Points
A. Quality Control Testing Frequency
e technologist’s QC testing procedure frequencies given in Table 1 and
in the rest of this manual are the minimum recommended frequencies.
However, we strongly recommend that the tests be done on a daily basis.
If problems are detected oen, if the equipment is unstable, or if the
system has just been subject to a signicant repair or upgrade, then it
may be necessary to carry out some of the procedures more frequently.
Table 1. Minimum Frequencies of Performing Technologist’s QC Tests
Procedure
Minimum
Frequency
Approx.
Time (min)
Setup Weekly 7*
Table Position Accuracy Weekly 3
Center Frequency/Transmitter Gain
or Attenuation
Weekly 1
Geometric Accuracy Measurements Weekly 2*
High-Contrast Spatial Resolution Weekly 1
Low-Contrast Detectability Weekly 2
Artifact Evaluation Weekly 1
Film Printer Quality Control
(if applicable)
Weekly 10
Visual Checklist Weekly 5
*Some measurement can be performed simultaneously.
B. Designated Quality Control Technologist(s)
A QC technologist should be charged with the QC procedures for
a particular piece of equipment. Using the same personnel leads to
greater consistency in measurements and greater sensitivity to incipient
problems. is does not mean that a single technologist must perform
the QC on all devices. It is acceptable, and oen convenient, to have
dierent technologists responsible for QC on dierent devices. When
the designated QC technologist for a given piece of equipment is not
available, the QC procedures should still be carried out on schedule by a
backup QC technologist. To ensure that the performance of QC tasks is
not linked to specic personnel’s work schedules, an adequate number of
technologists should be trained in the QC procedures.
IMPORTANT POINTS

Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 23
III. Important Points
MRI
TECHNOLOGIST’S SECTION
C. Quality Control Log
A QC log shall be maintained and the results of QC activities recorded
in the log at the time they are performed. Blank forms for this purpose
are provided in the appendix (Section VIII) for each of the procedures
described in this section. ese forms may be freely copied. Sites may also
choose to develop their own forms.
e content of the QC log will vary between facilities, depending on their
size, administrative organization, and the preferences of the QC team.
Small facilities may have a single log encompassing all of their equipment;
large facilities will oen have separate logs for equipment at separate
locations. In general, the QC log should have the following:
1. A section describing the facility’s QC policies and procedures for
the equipment covered by the log
2. A section of data forms where QC procedure results are recorded
for each piece of equipment covered by the log
3. A section for recording notes on QC problems and corrective
actions
e QC log shall be kept in a location accessible to, and known to, all
members of the QC team and the service engineer, so that they may
refer to it when questions arise. e section of the log for recording QC
problems and corrective actions can facilitate communications between
the service engineer and QC team members who oen have dierent
work schedules.
D. Quality Control Data Review
e QC log data will be reviewed at least annually by the qualied medical
physicist/MRI scientist and/or supervising radiologist. e purpose of the
review is to make sure no image quality problems have been inadvertently
overlooked, and to verify that the QC procedures are being performed
on schedule with at least the minimum recommended frequency. It is
recommended that this review be part of a Quality Assurance Committee
meeting (Radiologist’s Section III.B).
E. Alternative Phantoms
Currently, the ACR MRI Accreditation Program has two phantoms
(large and small). e large phantom is used for whole-body magnets,
and the small phantom is used for extremity magnets. is manual
describes QC using either of the two phantoms. A committee of MRI
physicists and radiologists designed the ACR phantoms with the goals
of producing eective, versatile, and economical MRI system tests. e
ACR phantom is mandatory for application to the accreditation program,
so all accredited sites will already have one. e procedures described
here for weekly QC were written specically for the ACR phantoms. e
decision to use an alternative phantom should be made by the qualied
MRI physicist/scientist.

24 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
III. Important Points
Alternative phantoms should only be used if they are capable of providing
tests substantially equivalent to the ACR phantoms and aer they have
been reviewed and approved by a qualied medical physicist or MRI
scientist. If this decision is made, then the physicist shall document
the necessary procedures, analysis methods, and action criteria for the
tests to be performed with the alternative phantom and provide the QC
technologist training in these methods. e alternate test procedures
should, at a minimum, provide QC parameters substantially equivalent
to the procedures listed in Table 1.
F. Alternative Procedures
Test procedures enumerated in this document should be considered
the minimum set of tests and should be used unless the recommended
procedures are for some reason unavailable or not possible on
a particular scanner. e details of alternative QC tests shall be
described in detail and placed in the site’s MRI QA Procedures Manual
(Radiologist’s Section IV.E).
Additional tests may be required if the system is used routinely for
advanced clinical MRI procedures. Such studies would include, but are
not limited to, imaging to obtain reference data for stereotactic therapeutic
procedures, MR spectroscopy, cardiac MRI, diusion-weighted and
susceptibility-weighted MRI, MR elastography, functional MRI, MR-
guided biopsy, and advanced angiographic and blood perfusion methods
using contrast agents. Enumeration of QC tests for these advanced MRI
applications is beyond the scope of this manual. e qualied medical
physicist or MRI scientist is responsible for determining and setting up
the methods and frequencies for these tests.
G. Action Limits
Performance criteria for the various QC measurements are specied
in terms of action limits (also known as control limits), which dene
the range of acceptable values; outside of which corrective action is
required. Suggested performance criteria are dened for each procedure.
In some cases, the stability of the equipment and the consistency of the
technologist’s measurements may be such that the measured values are
always well within the action limits. In those cases a tightening of the
action limits may be useful for greater sensitivity to developing problems.
It is the responsibility of the qualied medical physicist or MRI scientist
to set the action criteria and verify that they are adequately sensitive to
detect MRI equipment problems.
e qualied medical physicist or MRI scientist should write the action
limits on the top line of the data form for the Weekly MRI Equipment
Quality Control (Section VIII.A).

Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 25
IV. Technologist’s Weekly MRI Quality Control
MRI
TECHNOLOGIST’S SECTION
To ensure that the MR scanner is producing images of quality equal to
that produced when the scanner is known to be functioning correctly,
phantom image acquisition and analysis should be performed at
least weekly. Aer these data are acquired, the technologist performs
simple measurements to verify that system performance is within the
action limits.
e ACR technologist’s tests should be performed in addition to any
testing required by the manufacturer. In contrast to the manufacturer’s
tests, which oen involve automated analysis and storage of the QC
data in directories unavailable to the technologist, the data-collection
methods recommended here require that the technologist acquire and
assess images at least weekly. ese methods permit the QC technologist
to identify and report poor MRI system performance at or near the time
system degradation occurs.
Acceptance testing should take place before the rst patient is scanned
and aer major repairs. Major repairs include replacement of or repair of
the following subsystem components: gradient ampliers, gradient coils,
magnet, RF amplier, digitizer boards, and signal processing boards. A
baseline check should be carried out on the MRI system as a whole and on
additional subsystems, such as repaired, replaced, or upgraded RF coils.
All records should be kept at a central location near the MRI scanner(s).
Action limits are established by the qualied medical physicist/MRI
scientist at the initiation of the weekly QC program in order to establish
scanner-specic baseline values for the low-contrast detectability (LCD)
and center frequency. Action limits should be reevaluated whenever there
are hardware changes or service activities that alter the signal acquisition
and excitation electronics.
e recommended weekly QC scanning series is the same sagittal
localizer and axial T1-weighted sequence as acquired for the ACR MRI
Accreditation Program. e following specic documents are available
from the ACR website (www.acr.org):
• Site Scanning Instructions for Use of the MR Phantom for the
ACR MRI Accreditation Program
• Site Scanning Instructions for the Use of the Small MR Phantom
for the ACR MRI Accreditation Program
• Phantom Test Guidance for the ACR MRI Accreditation Program
• Phantom Test Guidance for Use of the Small MRI Phantom for
the ACR MRI Accreditation Program
e weekly QC procedure is organized into three parts:
1. Position the large phantom in the head coil or, for extremity MRI
systems, position the small phantom in the knee coil. Use the
computer interface to set up scanning and identify the patient as
a phantom.
2. Record center frequency and transmitter attenuation (or
transmitter gain).
TECHNOLOGIST’S
WEEKLY MRI
QUALITY CONTROL

26 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
IV. Technologist’s Weekly MRI Quality Control
3. Analyze the images aer scanning. Measure the phantom
dimensions. Assess high-contrast resolution and LCD. Note
image artifacts.
A. Setup and Table Position Accuracy
To determine that the MRI scanner is performing patient setup, data
entry, and prescan tasks properly.
Weekly
e ACR MRI phantom is used. Data are recorded on the Data Form for
Weekly MRI Equipment Quality Control (Section VIII.A).
1. Place the ACR large phantom in the head coil or, for extremity
MRI units, place the small phantom in the knee coil, in accordance
with the instructions that came with the phantom. To ensure
good reproducibility of the measurements, it is important to place
the phantom in the same position, properly centered and square
within the coil, each time. On the anterior side of the ACR large
phantom (the side labeled “NOSE”), there is a black line running
in the head-to-foot direction to help align the phantom squarely
and a small positioning cross-line used to center the phantom.
Because of its small size it can be dicult to use to ensure that the
phantom is positioned squarely within the magnet. It is generally
easier, and more reproducible, to observe the laser on the top of
the grid structure inside the phantom. Position the phantom so
that the axial alignment light is on the superior (head direction)
edge of the grid structure. By ensuring that the thickness of the
line is uniform along the edge, you will prevent any “yaw” in the
phantom, assuming that the axial light is square. See Figure 1.
e small phantom should be centered and aligned as a knee
would be positioned in the knee coil. Position the laser in a
similar fashion to that described above for the large phantom.
Move the phantom into the magnet to the proper location
for scanning.
OBJECTIVE
FREQUENCY
REQUIRED EQUIPMENT
TEST PROCEDURE

Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 27
IV. Technologist’s Weekly MRI Quality Control
MRI
TECHNOLOGIST’S SECTION
Figure 1. Illustration of the use of the central grid structure for alignment of the large
phantom when the head coil has a central bar that blocks visualization of the small
cross-line positioning marker. The phantom is properly positioned when the laser
light is aligned with the superior (head direction) edge of the grid structure. If the
laser light is accurately aligned, the phantom will be correctly positioned at the
magnet isocenter after moving the phantom to the proper location for scanning.
It is recommended that a three-plane localizer be used initially
to ensure the phantom is properly positioned. In particular,
examine the coronal image to ensure that the phantom is not
rotated about the anterior/posterior axis and the sagittal image
to ensure it is not tipped front-to-back. e localizer images
cannot replace the sagittal sequence listed below because these
fast localizer images do not have adequate spatial resolution
to permit accurate prescription of axial slices, measurement of
phantom length, or evaluation of table position.
2. e ACR sagittal localizer sequence should use the following
parameters:
For the large phantom: 1 slice, sagittal spin-echo, TR=200
ms, TE=20 ms, slice thickness=20 mm, FOV=25 cm,
matrix=256 × 256, NEX=1, scan time: 51-56 seconds (s).
For the small phantom: 1 slice, sagittal spin-echo, TR=200
ms, TE=20 ms, slice thickness=20 mm, FOV=12 cm,
matrix=152 × 192, NEX=1, scan time: 32 s. If the 20-mm thick
slice causes artifacts, a 10-mm slice may be used.

28 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
IV. Technologist’s Weekly MRI Quality Control
If the positioning laser is properly calibrated and the table positioning
system functions properly, the superior edge of the grid structure should
be at magnet isocenter. Every vendor provides a method to determine the
S/I or z-coordinate of a location in the image. It usually entails placing a
cursor or a region of interest (ROI) on the image and then reading the z
coordinate or S/I value (Figure 2). If the location of the superior edge of
the grid structure is within ±5 mm of the magnet isocenter, enter “YES”
in column 2, “Table position accuracy OK?” of the Data Form for Weekly
MRI Equipment Quality Control (Section VIII.A).
Figure 2. a) An example taken from a scanner where a square ROI has been placed
with its center on the anterior/superior edge of the grid, exactly where the laser was
positioned. In this example, the z-coordinate is +1.06 mm (see data inset), which is
acceptable because it is less than ±5 mm. b) An example taken from a scanner and
showing the cursor on the superior edge of the grid is exactly at isocenter, SØ.ØØ
mm; the S indicates distance from isocenter in the superior z-direction.
DATA INTERPRETATION
AND CORRECTIVE ACTION

Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 29
IV. Technologist’s Weekly MRI Quality Control
MRI
TECHNOLOGIST’S SECTION
If the computer booted without a problem and the scanner interface
(including mouse, keyboard and display) works properly, enter “YES” in
column 3, “Console OK?” of the Data Form for Weekly MRI Equipment
Quality Control (Section VIII.A). If there are problems with either the
table or the console, note these problems (right margin of data sheet)
and contact the MRI service organization following the QC procedure.
Proceed with part B.
B. Axial Image Data: Prescan Parameters
1. Center Frequency
Prior to the performance of any imaging protocol, it is essential that the
MRI system is set on resonance. MRI system manufacturers provide
specic user protocols for resonance frequency adjustment, and most
are completely automated. e phantom is positioned in the center of
the magnet (with all gradient elds turned o), and the RF frequency is
adjusted by controlling the RF synthesizer center frequency to achieve
maximum signal. Operating an MRI scanner o-resonance reduces an
image’s signal-to-noise ratio (SNR), adversely aecting LCD.
Resonance frequency checks are especially important for mobile units and
resistive magnet systems that undergo frequent ramping of the magnetic
eld. Changes in the resonance frequency reect changes in the static
magnetic eld (B
0
). Changes in the B
0
eld may be due to superconductor
“run down” (typically less than 1 ppm per day on superconducting
magnets), changes in current density due to thermal or mechanical eects,
shim-coil changes, or eects due to external ferromagnetic materials.
Weekly
e ACR MRI phantom is used to acquire all image data. Data are
recorded on the Data Form for Weekly MRI Equipment Quality Control
(Section VIII.A).
1. Determine where the center frequency and transmitter
attenuation are displayed during the prescan portion of test
phantom series. e scanner, prior to image acquisition, generally
determines the center frequency automatically. is information
is not normally annotated on the images but is oen included on
a page of scan parameters that can be accessed by the user at the
scanner console. Some scanners also display the center frequency
on the console at the conclusion of the automated prescanning
adjustments. Information on how to nd the center frequency for
any particular scanner usually can be obtained from the scanner
user’s manual, the MRI system vendor’s applications specialist or
the service engineer.
2. Display the central, sagittal slice through the ACR phantom
acquired in the previous test to prescribe slice locations of
the axial T1-weighted series. For the large phantom, the
recommended slice prescription is 11 slices, starting at the
vertex of the crossed 45° wedges at the inferior end of the ACR
OBJECTIVE
FREQUENCY
REQUIRED EQUIPMENT
TEST PROCEDURE

30 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
IV. Technologist’s Weekly MRI Quality Control
phantom and ending at the vertex of the crossed 45° wedges
at the superior end of the phantom (Figure 3a). For the small
phantom, the recommended slice prescription is seven slices,
slice 1 is centered on the vertex of the angle formed by the cross
wedges at the indicated end of the phantom. is prescription is
cross-referenced onto the sagittal localizer (Figure 3b).
3. Set up the acquisition of the axial slices through the length of the
phantom, making sure that the slice prescription is referenced to
structures in the phantom in a reproducible way, and at least one
of the slices lies in the uniform region of the phantom.
e recommended sequence for this acquisition for the large
phantom is the ACR T1-weighted axial series: 11 slices, spin-
echo, TR=500 ms, TE=20 ms, FOV=25 cm, slice thickness=5
mm, slice gap=5 mm, matrix=256 × 256, NEX=1.
e recommended sequence for this acquisition for the small
phantom is the ACR T1-weighted axial series: 7 slices, spin-echo,
TR=500 ms, TE=20 ms, FOV=12 cm, slice thickness=5 mm, slice
gap=3 mm, matrix=152 × 192, NEX=1.
4. During the prescan, the system will automatically check the
center frequency and set the transmitter attenuation or gain.
1. Record the center frequency and RF transmitter attenuation or
gain values in the fourth and h columns of the Data Form for
Weekly MRI Equipment Quality Control (Section VIII.A).
2. If the prescribed action limit (entered on the top line of the
data form) is exceeded, repeat the prescan and record the
measurement.
3. If the action limit is still exceeded, consult with the qualied
medical physicist/MRI scientist regarding the excessive change
in the measured frequency of the ACR imaging series. Notify the
service engineer of this result.
DATA INTERPRETATION
AND CORRECTIVE ACTION

Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 31
IV. Technologist’s Weekly MRI Quality Control
MRI
TECHNOLOGIST’S SECTION
Figure 3. a) Sagittal image of ACR large phantom with positions of the 11 axial slices
of the T1-weighted series superimposed. b) Sagittal image of ACR small phantom.
Resonance frequency should be recorded in the Data Form
for Weekly MRI Equipment Quality Control (Section VIII.A)
for trend analysis. e action limits for center frequency are
expressed in terms of the permissible weekly change in hertz
perweek. Typically for superconducting magnets the change
from week to week should be less than few parts per million
(ppm). Parts per million can be converted to hertz by multiplying
by the Larmor frequency (in megahertz). For example, for a 1.5T
scanner, the Larmor frequency is about 64 MHz. erefore, 1
ppm equals about 64 Hz; 2 ppm equals 128 Hz. For a 3T scanner,
the Larmor frequency is about 128 MHz, so 1 ppm equals 128 Hz
and 2 ppm equals 256 Hz. If the action limit for center frequency
is set at 2 ppm per week, then a 1.5T scanner should change
center frequency by no more than 128 Hz from one week to the
next, whereas a 3T scanner’s center frequency should change by
no more than 256 Hz from one week to the next.
32 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
IV. Technologist’s Weekly MRI Quality Control
If the recorded center frequency value exceeds the action level
established by the qualied medical physicist or MRI scientist,
the test should be repeated. If the center frequency change still
exceeds the action level following a repeat scan, the service
organization and the qualied medical physicist or MRI scientist
should be contacted.
Mobile MRI systems and resistive magnets should be reset to
consistent eld strength aer the magnet has been ramped down
and powered back up. Superconducting magnets may also have
their eld strengths adjusted on occasion. ese procedures
should be recorded in the service log and noted in the Data Form
for Weekly MRI Equipment Quality Control (Section VIII.A).
2. Transmitter Gain or Attenuation
Aer establishing the resonant frequency, the system acquires several
signals while varying the transmitter attenuation (or gain) level so that
imaging can proceed using the proper ip angles. Signicant uctuations
in the transmitter attenuation (or gain) levels suggest problems with the
RF chain.
Weekly
ACR MRI Phantom and Data Form for Weekly MRI Equipment Quality
Control (Section VIII.A)
1. Determine where the transmitter (TX) attenuation or gain is
displayed on the scanner console.
2. Record the value displayed in column 5 on the Data Form for
Weekly MRI Equipment Quality Control (Section VIII.A).
3. If the change in decibels (dB) exceeds the action limits, report the
problem to the qualied medical physicist or MRI scientist.
Transmitter (TX) attenuation or gain values are usually recorded in units
of dB. is engineering system takes advantage of a logarithmic scale so
that values over a large dynamic range can be easily related. However, a
small change in dB represents a large change in the transmitter attenuation
if displayed using a linear scale (volts or watts). Changes in the measured
TX attenuation or gain exceeding the action limits should be reported to
the qualied medical physicist/MRI scientist and the site service engineer.
C. Image Data Measurements
Weekly image quality measurements ensure accurate calibration of the
MRI system. ree specic measurements are to be performed weekly:
geometric accuracy, limiting spatial resolution, and LCD. Each of these
measurements is addressed specically below.
1. Geometric Accuracy Measurements
In MRI, the radiologist assumes that the geometric relationships are
accurate and concentrates on deciphering the tissue contrast relationships
OBJECTIVE
FREQUENCY
REQUIRED EQUIPMENT
TEST PROCEDURE
DATA INTERPRETATION
AND CORRECTIVE
ACTION
OBJECTIVE

Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 33
IV. Technologist’s Weekly MRI Quality Control
MRI
TECHNOLOGIST’S SECTION
for a variety of pulse sequences to make an accurate diagnosis. However,
the geometric relationships in the MR image can easily be in error by
a factor of 5%–10% if care is not taken to ensure the gradient-scaling
factors are properly calibrated and the magnet eld is very homogeneous.
e objective of the following tests is to verify that the image is
scaled in a manner reecting the true dimensions of the body part
under investigation.
Weekly
Geometric accuracy is checked with the ACR MRI accreditation phantoms
using the sagittal localizer image and image slice 5 from the T1-weighted
ACR axial series for the large phantom (or sagittal localizer image and
slice 3 for the small phantom). ese data are analyzed in the following
manner. Data are recorded on the Data Form for Weekly MRI Equipment
Quality Control (Section VIII.A).
e display window and level should be set so that the edges of the
phantom are approximately at the half-maximum value of the signal
intensity. To set the appropriate display values, follow this procedure:
1. Setting the Window and Level
a. Set the window width to a very narrow value (zero or one).
Adjust the window level until about one-half of the uid
within the phantom is white and the other half is black.
Note the window level value.
b. Change the window width value to the window level value
noted in step 1a.
c. Change the window level value to one-half of the window
width value that was set in step 1b.
2. Sagittal Image Measurement
a. Display the sagittal image of the phantom using the
procedure described above to set the display window width
and level.
b. Using the distance-measuring function, measure the length
from one end of the signal-producing region of the phantom
to the other (Figure 4).
c. Verify that the length is measured along a line that runs
vertically from one end of the phantom to the other and is
close to the center of the phantom.
d. Enter the resulting length (in millimeters) in column 6
(z-direction) of the Data Form for Weekly MRI Equipment
Quality Control (Section VIII.A).
FREQUENCY
REQUIRED EQUIPMENT
TEST PROCEDURE

34 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
IV. Technologist’s Weekly MRI Quality Control
Figure 4. Positioning of length measurement on ACR MR accreditation phantom.
3. Transaxial Image Measurements
a. Display slice 5 for the large phantom and slice 3 for the small
phantom in normal mode (Figure 5).
b. Since these distance measurements are dependent on the window
setting, use the standard routine for setting window width and
level routine described above in step 1.
c. Use the scanner’s distance-measuring function to determine the
diameter of the signal-producing circular phantom, measured
vertically through the center of the phantom.
d. Enter the resulting length (in millimeters) in column 7
(y-direction) of the Data Form for Weekly MRI Equipment
Quality Control (Section VIII.A).
e. Use the scanner’s distance-measuring function to determine the
diameter of the signal-producing circular phantom, measured
horizontally across the center of the phantom.
f. Enter the resulting length (in millimeters) in column 8
(x-direction) of the Data Form for Weekly MRI Equipment
Quality Control (Section VIII.A).

Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 35
IV. Technologist’s Weekly MRI Quality Control
MRI
TECHNOLOGIST’S SECTION
Figure 5. Position for x- and y-direction diameter measurements on ACR MRI
accreditation phantom in the large phantom, slice 5 (a) and small phantom,
slice 3 (b).
1. Geometric accuracy measurements on the ACR MRI accreditation
phantom, when measured over a 25-cm eld-of-view for the
large phantom and a 10-cm eld of view for the small phantom
are generally considered acceptable if they are within ±2 mm of
the true values. Depending on the mix of studies at a given site,
the qualied medical physicist or MRI scientist may determine
that a more strict action limit should be put in place.
2. If the length or either diameter measurement of the phantom
exceeds the action level established by the qualied medical
physicist or MRI scientist, the QC technologist should carefully
inspect the magnet bore or gap to verify that no ferromagnetic
material (hair pins, paper clips, etc.) has found its way near the
imaging volume.
3. e measurement should then be repeated.
DATA INTERPRETATION
AND CORRECTIVE ACTION

36 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
IV. Technologist’s Weekly MRI Quality Control
4. If the length or either diameter measurement of the phantom
exceeds the action level following a repeat measurement, the
service engineer and the qualied medical physicist or MRI
scientist should be contacted. e service engineer should be
able to correct improper gradient eld calibrations through a
vendor recommended procedure.
e most common cause of failure of this test is one or more miscalibrated
gradients. A miscalibrated gradient causes its associated dimension (x, y,
or z) in the images to appear longer or shorter than it really is. It will also
cause slice-position errors. It is normal for gradient calibration to dri
over time and to require recalibration by the service engineer.
Gradient ampliers need time to warm up and stabilize when they are
turned on. Some sites power o their scanner hardware, including gradient
ampliers, overnight. ose sites should make sure their hardware has
been on at least an hour before acquiring images of the phantom.
Another possible cause of failure is use of a very low MRI receiver
bandwidth. It is common practice on some scanners and at some
facilities to reduce receiver bandwidth to increase SNR. is strategy
can be pushed to the point that magnetic eld inhomogeneities manifest
themselves as large spatial distortions in the image. On most scanners
the default bandwidth for T1-weighted acquisitions is set high enough
to avoid this problem. If the geometric accuracy test exceeds the action
limits and the ACR T1-weighted series (described above) was acquired at
low bandwidth, one should try to acquire these images again at a larger
bandwidth to see if the problem is eliminated.
B
0
eld inhomogeneities could be caused by improper adjustment of
the gradient osets, improper adjustment of passive or active magnet
shims, or a ferromagnetic object such as a pocket knife or large hair clip
lodged in the magnet bore. Especially on open magnet systems, which
have relatively small volumes of gradient linearity and B
0
homogeneity,
it is possible that abnormally high B
0
eld inhomogeneities could
cause signicant dimensional errors in the phantom images. e
service engineer can easily measure the magnet homogeneity, and any
inhomogeneity large enough to cause failure of the geometric accuracy
test should be correctable.
2. High-Contrast Spatial Resolution
e high-contrast spatial resolution test assesses the scanner’s ability to
resolve small objects. is is sometimes called “limiting spatial resolution.”
A failure of this test means that for a given eld of view and acquisition
matrix size the scanner is not resolving small details as well as normal for
a properly functioning scanner.
Weekly
OBJECTIVE
FREQUENCY

Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 37
IV. Technologist’s Weekly MRI Quality Control
MRI
TECHNOLOGIST’S SECTION
High-contrast resolution is checked with the ACR MRI accreditation
phantom using image slice 1 from the T1-weighted ACR axial series.
ese data can be analyzed in the following manner.
For this test, one visually determines the number of individual small
bright spots in arrays of closely spaced uid-lled holes drilled in a small
block of plastic (called the resolution insert). e resolution insert is
located in slice 1 of the ACR T1-weighted axial image series (Figure 6).
Note that there are three pairs of not-quite-square arrays of holes in the
insert. e insert consists of an upper-le (UL) hole array and a lower-
right (LR) hole array, where right and le are the viewer’s right and le.
e UL and LR arrays share one hole in common at the corner where they
meet. e UL array is used to assess resolution in the right-le direction,
and the LR array is used to assess resolution in the top-bottom direction
(i.e., anterior-posterior if this phantom were a head).
e UL array comprises four rows of four holes each. e center-to-
center hole separation within a row is twice the hole diameter. e
center-to-center row separation is also twice the hole diameter. Each row
is staggered slightly to the right of the one above, which is why the array
is not quite square.
e LR array comprises four columns of four holes each. e center-
to-center hole separation within each column and the center-to-center
spacing between columns are twice the hole diameter. Each column is
staggered slightly downward from the one to its le.
e hole diameter for the large phantom diers between the array pairs:
for the le pair it is 1.1 mm; for the center pair it is 1.0 mm; and for the
right pair it is 0.9 mm. e hole diameter of the small phantom diers
between the array pairs: for the le pair it is 0.9 mm; for the center pair
it is 0.8 mm; and for the right pair it is 0.7 mm. us, using this insert,
one can determine whether or not resolution has been achieved at each
of these three hole sizes.
REQUIRED EQUIPMENT
TEST PROCEDURE

38 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
IV. Technologist’s Weekly MRI Quality Control
Figure 6. a) Large phantom high-contrast resolution insert from slice 1 of an axial
series shows three sets of two arrays of holes. Hole sizes and spacing: from left, 1.1
mm, 1.0 mm, and 0.9 mm. b) Small phantom high-contrast resolution insert from
slice 1. Hole sizes and spacing: from left, 0.9 mm, 0.8 mm, and 0.7 mm.
For this test, high-contrast spatial resolution in slice 1 of the ACR T1-
weighted axial series is evaluated. e following procedure is repeated for
each of those series:
1. Display the image of slice 1.
2. Magnify the image by a factor between two and four, keeping the
resolution insert visible in the display.
3. Set the window width to a small value (<10% of the entire range
of signal intensities for the image). Adjust the window level until
the holes in the resolution insert are individually displayed.
4. Begin with the lemost pair of hole arrays, which is the pair with
the largest hole size (large phantom: 1.1 mm; small phantom:
0.9 mm).
5. Look at the rows of holes in the UL array and adjust the display
window and level to best show the holes as distinct from
one another.
6. If all four holes in any single row are distinguishable from
one another, the image is considered resolved right-to-le
(horizontally) at this particular hole size.

Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 39
IV. Technologist’s Weekly MRI Quality Control
MRI
TECHNOLOGIST’S SECTION
7. Enter the smallest hole size (1.1, 1.0, or 0.9 mm for the large
phantom and 0.9, 0.8, or 0.7 mm for the small phantom) that
can be resolved horizontally in the UL array in column 9 of the
Data Form for Weekly MRI Equipment Quality Control (Section
VIII.A). at is the measured horizontal spatial resolution.
8. Look at the columns of holes in the LR array and adjust the
display window and level to best show the holes as distinct from
one another.
9. If all four holes in any single column are distinguishable from
one another, the image is considered resolved top-to-bottom
(vertically) at this particular hole size.
10. Enter the smallest hole size (1.1, 1.0, or 0.9 mm for the large
phantom and 0.9, 0.8, or 0.7 mm for the small phantom) that
can be resolved vertically in the LR array in column 10 of the
Data Form for Weekly MRI Equipment Quality Control (Section
VIII.A). at is the measured vertical spatial resolution.
One needs to be very clear about what is meant by the word “distinguishable.”
It is not required that image intensity drop to zero between the holes; that
is not normal. However, one must nd a single window and level setting
such that all four holes in at least one row are recognizable as points of
brighter signal intensity than the spaces between them.
When the hole size is comparable to the resolution in the image, there is
a tendency for groups of two or more holes in a row to blur together and
appear as a single irregularly shaped spot of signal. In this case the holes
in that row are considered unresolved.
Sometimes one or more holes, which are distinguishable from their
neighbors in their own row, blur together with their neighbors in adjacent
rows. is is acceptable and does not aect the scoring for the row.
For the large phantom, the eld of view and matrix size for the ACR
T1-weighted axial series are chosen to yield a nominal resolution of
1.0 mm in both directions. For both directions in the axial T1-weighted
ACR series, the measured resolution should be 1.0 mm or better. On
many scanners, one can distinguish the holes in the 0.9 mm arrays in one
or both directions. e resolution of the MRI system should not change.
For the small phantom, the eld of view and matrix size for the axial ACR
series are chosen to yield a resolution of 0.8 mm in both directions.
Changes in high-contrast spatial resolution can be due to the gradient eld
strength, the eddy current compensation, and/or the main (B
0
) magnetic
eld homogeneity being out of calibration. ese problems will oen
produce poor results in other QC tests described in this manual. Unstable
gradient ampliers also have been known to cause subtle decreases in
spatial resolution. Consult with the qualied medical physicist/MRI
scientist regarding any change in the measured resolution of the axial
ACR imaging series.
DATA INTERPRETATION
AND CORRECTIVE ACTION

40 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
IV. Technologist’s Weekly MRI Quality Control
3. Low-Contrast Detectability
e low-contrast detectability (LCD) test assesses the extent to which
objects of low contrast are discernible in the images. For this purpose
the ACR MRI accreditation phantom contains contrast objects of varying
size and contrast. e detection of a low-contrast object is primarily
determined by the contrast-to-noise ratio achieved in the image, and may
be degraded by the presence of artifacts such as ghosting.
e ACR MRI accreditation phantom contains low-contrast objects of
varying size and contrast that appear on four slices of the T1-weighted
axial multislice series (Figure 7): 8 through 11 for the large phantom
and 6 and 7 for the small phantom. In each slice the low-contrast objects
appear as rows of small disks, with the rows radiating from the center of
circle-like spokes in a wheel. Each spoke is made up of three disks, and
there are 10 spokes in each circle.
All of the spokes on a given slice have the same level of contrast. For
the large phantom and a 5-mm slice thickness, in order from slice 8 to
slice 11, the contrast values are 1.4%, 2.5%, 3.6%, and 5.1%. For the small
phantom and a 5-mm slice thickness, slices 6 and 7 have contrast values
of 3.6% and 5.1%, respectively. All disks in a given spoke have the same
diameter. Starting at the 12 o’clock position and moving clockwise, the
disk diameters decrease progressively from 7.0 mm at the rst spoke to
1.5 mm at the 10th spoke.
e low-contrast disks are actually holes drilled in thin sheets of plastic
mounted in the phantom at the locations of the four slices. e contrast
is derived from the displacement of solution from the slices by the
plastic sheets.
e measurement for this test consists of counting the number of
complete spokes seen in a designated axial slice. e specic slice
designated for this weekly QC test should be determined by the qualied
medical physicist or MRI scientist to be the most sensitive to deviations
in system performance. Scanners dier widely in their contrast-to-noise
ratio performance.
For instance in the large phantom, if a scanner depicts all of the disks in
all of the spokes in slices 9, 10, and 11 using the ACR T1-weighted axial
series, but only some of the spokes in slice 8, then slice 8 should be used
for this test. For the small phantom, if a scanner depicts all of the spokes
in slice 7 using the ACR T1-weighted axial series, then slice 6 should be
used for this test. Conversely for the large phantom, if a scanner typically
depicts none of the spokes in slices 8, 9, and 10, then slice 11 should be
used for this test. For the small phantom, if the MRI system typically
depicts none of the spokes in slice 6, then slice 7 should be used for this
test. e slice number will be entered in the rst row, column 11 of the
Data Form for Weekly MRI Equipment Quality Control (Section VIII.A).
OBJECTIVE
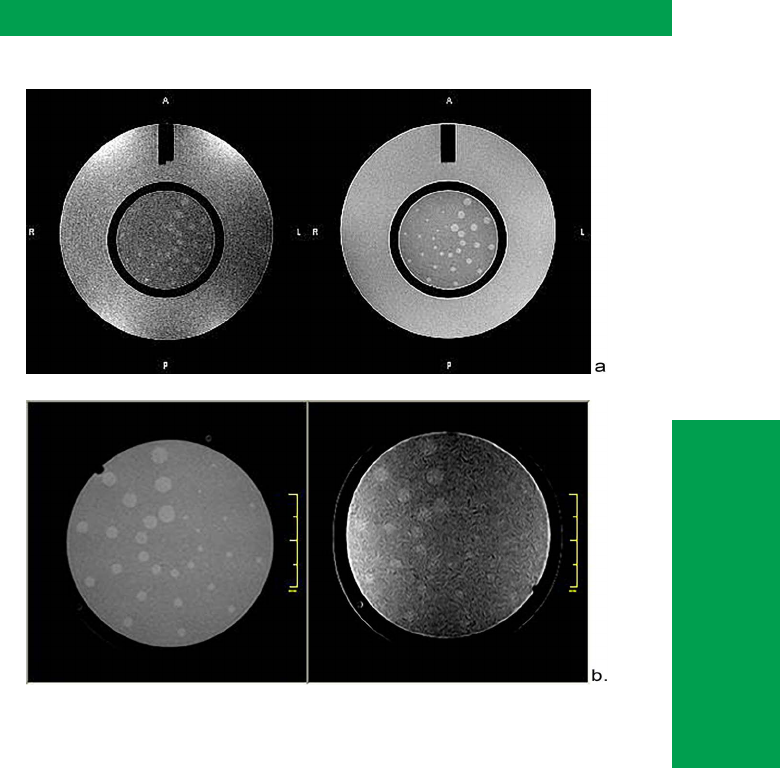
Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 41
IV. Technologist’s Weekly MRI Quality Control
MRI
TECHNOLOGIST’S SECTION
Figure 7. Phantom images of low-contrast detectability (LCD) inserts. a) Large
phantom LCD insert images. Slice 11 (5.1% contrast) acquired on two dierent
scanners, each with proper slice positioning. The left image is from a 1.5T scanner
where all 10 spokes (each spoke consisting of three test objects) are visible. Right
image is from slice 11 of a 0.3T scanner where only seven complete spokes are
visible. The qualied medical physicist or MRI scientist should designate the specic
ACR MRI phantom image slice that is most appropriate to assess for weekly QC. b)
Small phantom LCD insert images. The left image is slice 7 (5.1% contrast) from a 1T
scanner, where all 10 spokes are visible. The right image is also slice 7, but from a 0.3T
scanner, where 7 spokes are visible. One or two objects in the eighth spoke are seen,
but the outermost object is no more apparent than background noise, so the eighth
spoke is not counted, nor are any spokes beyond the eighth spoke.

42 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
IV. Technologist’s Weekly MRI Quality Control
Weekly
LCD is checked with the ACR MRI accreditation phantom using image
slices 8–11 for the large phantom and image slices 6–7 for the small
phantom from the T1-weighted ACR axial series. ese data should be
analyzed in the following manner.
Use the following procedure to score the number of complete spokes seen
in a slice:
1. Display the slice to be scored as prescribed by the qualied
medical physicist or MRI scientist and listed in the top cell of
column 11 on the Data Form for Weekly MRI Equipment Quality
Control (Section VIII.A).
2. Adjust the display window width and level settings for best
visibility of the low-contrast objects (Figure 7). is will require
a fairly narrow window width and careful adjustment of the
level to best distinguish the objects from the background. As
you move from slice to slice, the window and level may require
readjustment for best visualization of low-contrast objects. Once
obtained for a given scanner and slice number, the window and
level should remain the same from week to week.
3. Count the number of complete spokes seen. Begin counting
with the spoke having the largest diameter holes; this spoke is at
12 o’clock or slightly to the right of 12 o’clock (large phantom)
or slightly le of 12 o’clock (small phantom), and is referred to as
spoke 1 (see Figure 7). For the large phantom, count clockwise
from spoke 1 until a spoke is reached where one or more of the
holes are not discernible from the background. For the small
phantom, count counterclockwise from the largest spoke.
4. e number of complete spokes counted is the score for this slice.
Record the score in column 11 of the Data Form for Weekly MRI
Equipment Quality Control (Section VIII.A).
5. If the action criteria are exceeded (i.e., not enough rows of low-
contrast objects are detected), recheck the phantom positioning.
Tilting of the phantom in the head-foot direction can be
particularly troublesome (Figure 8). Verify that slices 8–11 for
the large phantom (or slices 6–7 for the small phantom) are
actually positioned over the thin plastic sheets in the phantom
that contain the holes (Figure 9). Acquire the axial series again.
6. If the LCD test still exceeds the action criteria, contact
the qualied medical physicist or MRI scientist and the
service engineer.
FREQUENCY
REQUIRED EQUIPMENT
TEST PROCEDURE
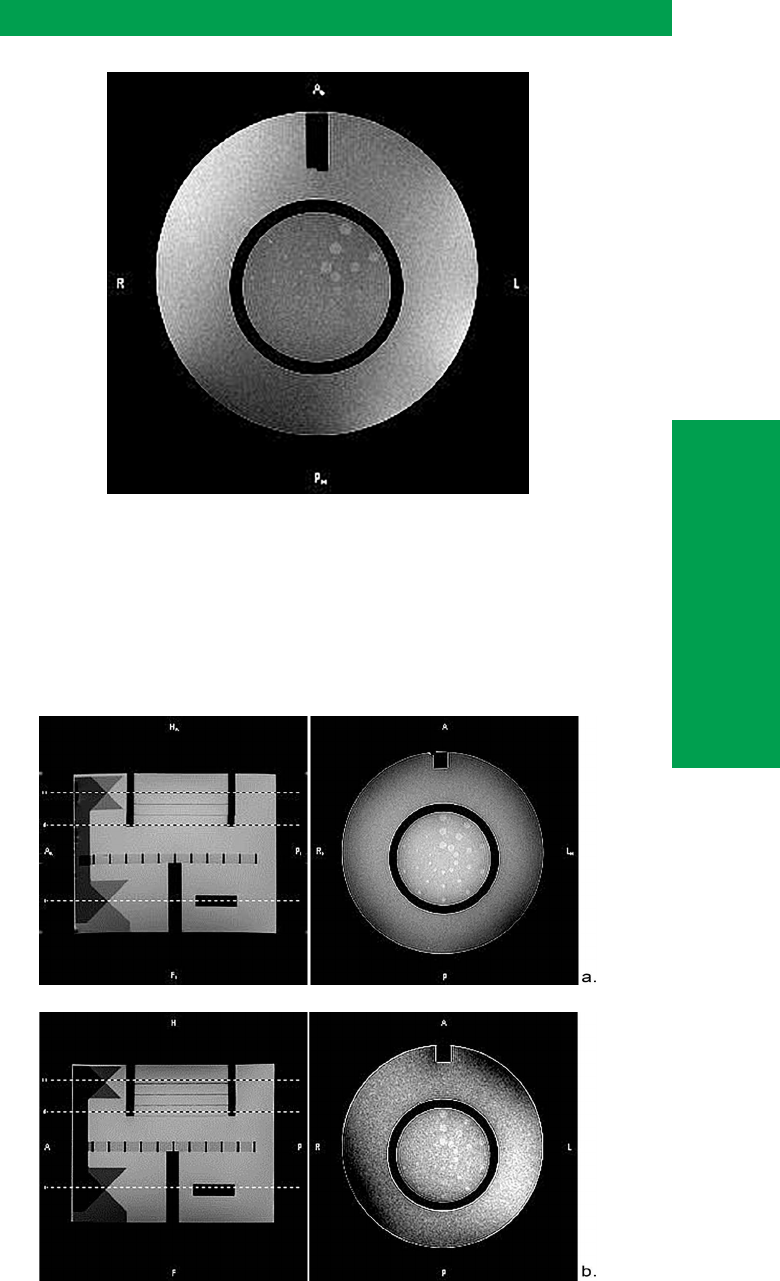
Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 43
IV. Technologist’s Weekly MRI Quality Control
MRI
TECHNOLOGIST’S SECTION
Figure 8. Slice 11 of a 1.5T scanner where the phantom is tilted from head to foot.
The upper portion of the LCD plate is within the selected slice, but the lower portion
of the plate is tilted out of the acquired slice plane, resulting in only 3 spokes being
fully detected before scoring is stopped. Note that spokes 8 and 9 are fully detected
but are not counted in the spoke score because not all 3 objects in spoke 4 (and in
spokes 5–7) are detected.
Figure 9. Sagittal localizer showing slice positioning (left) and slice 8 (right) from two
dierent 1.5T MRI systems. a) Proper slice positioning, shown by the overlaps of slices
1 and 11 on the intersection of the crossed wedges, slice 11 on the highest contrast
(5.1%) LCD plate, and slice 8 on the lowest contrast (1.4%) plate. All 10 spokes are
visible in slice 8. b) Misalignment of slices on the ACR phantom, resulting in only six
spokes being detected in slice 8.

44 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
IV. Technologist’s Weekly MRI Quality Control
LCD is related to the SNR of the MR image (Figure 10). However, other
factors can cause a degradation of the visibility of the spokes in the LCD
insert. Too low an acquisition matrix or excessive use of sharpening lters
can cause excessive truncation artifacts and result in poor depiction of
the outer holes in the spokes (Figure 11a). Excessive image-ghosting can
result in obscuration of some of the spokes (Figure 11b). e system’s
performance on this test is also sensitive to improper phantom and/or
slice positioning, so positioning should be the rst parameter checked if
there is a large decrease in the number of spokes perceived from week to
week (Figures 8 and 9).
Figure 10. Relationship between the total number of low-contrast spokes (in slices
8–11 combined) perceived on the ACR large phantom and the signal-to-noise ratio.
The shaded area represents +1 standard deviation in total spoke score. The number
of spokes visualized can also be degraded by poor positioning or image artifacts.
us, the issue of correspondence between the number of LCD spokes
and the SNR depends on proper positioning of the ACR phantom, proper
placement of acquired slices, and other factors such as image artifacts.
A spoke is complete only if all three of its holes are discernible. Count
complete spokes, not individual holes. Sometimes there will be one or
more complete spokes of smaller object size seen following a spoke that is
not complete, as in Figure 8. Do not count these additional spokes. Stop
counting prior to the rst incomplete spoke.
DATA INTERPRETATION
AND CORRECTIVE ACTION

Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 45
IV. Technologist’s Weekly MRI Quality Control
MRI
TECHNOLOGIST’S SECTION
Figure 11. Slice 8 from two dierent MRI systems. a) Truncation artifacts visible
as repeating light-dark bands near sharp interfaces in the ACR phantom tend to
obscure low-contrast objects. Air bubbles appearing as black-white dots can also
obscure test objects, as those at the innermost objects in spokes 7 and 8. b) Ghost
artifacts also obscure test objects. When this occurs, the source of ghosting should
be determined and eliminated by a qualied service engineer.
Holes on the threshold of perception can be dicult to score. ey may
appear ragged or misshapen; that is OK. e question is not whether each
test object is seen as perfectly round, but whether the object is suciently
distinct from the background that one can say with a reasonable degree
of condence that the object is present. In making this decision it can
be helpful to look at areas where there are no low-contrast objects to
gauge the uctuations in intensity from noise and artifacts that might
mimic a barely discernible test object. A test object that looks similar
to (or less distinct than) background noise uctuations would not be
deemed discernible.
In most cases it is not necessary to spend time pondering dicult
decisions on barely visible objects; just score the test conservatively
and revisit the scoring in the unlikely event the nal score is below the
action limit (i.e., several spokes below baseline). Typically, if the number
of detected spokes is reduced by more than three, then the qualied
medical physicist/MRI scientist and the service engineer should be
notied. However, the qualied medical physicist or MRI scientist should
determine the appropriate action limit for the MRI system and instruct
the QC technologist in the appropriate manner to evaluate the visibility
of low-contrast objects.
D. Artifact Evaluation
Various artifacts can occur during the weekly QC procedure that may be
early indicators of declining MRI system performance. e following is a
quick procedure for artifact analysis.
Weekly
Image artifacts are checked with the ACR MRI accreditation phantom
using the image slices from the T1-weighted ACR axial series. ese data
can be analyzed in the following manner.
OBJECTIVE
FREQUENCY
REQUIRED EQUIPMENT

46 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
IV. Technologist’s Weekly MRI Quality Control
1. On each slice, adjust the display window and level to show the
full range of pixel values in the image. is is dicult to do by eye
because the phantom image has mostly bright and dark regions
and very few intermediate gray regions to serve as a visual
reference for the adjustment.
2. e easiest way to get it right is to nd the approximate pixel
value for the bright areas, which can be done with a region-of-
interest (ROI) measurement of the mean value in a bright area.
en, set the window to that value and the level to half of that
value. e values don’t have to be exact, approximate ones will do
for this purpose.
3. Check that the following are true:
a.
e phantom appears circular, not elliptical or otherwise distorted.
b. ere are no ghost images of the phantom in the background
or overlying the phantom image.
c.
ere are no streaks or artifactual bright or dark spots in the image.
d. ere are no unusual or new features in the image.
4. If any of the foregoing items are false, then enter “Yes” in column
12 of the Data Form for Weekly MRI Equipment Quality Control
(Section VIII.A); otherwise enter “No.” If there is an artifact,
then enter a description as a note. Note that ghosting is a very
nonspecic symptom of a hardware problem. In general, it is
caused by instability of the measured signal from pulse cycle to
pulse cycle, which can have its origin in the receiver, transmitter,
or gradient subsystems. Motion of the phantom can also cause
ghosting. Make sure the phantom is stable in the RF coil and
not free to move or vibrate. Having ruled out phantom motion,
it will usually be necessary to ask the service engineer to track
down and correct the cause of the ghosting. More information
on ghosting is found in the Medical Physicist/MRI Scientist’s
Section IV.D. Radiofrequency Coil Checks.
TEST PROCEDURE

Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 47
V. Film Printer Quality Control
MRI
TECHNOLOGIST’S SECTION
FILM PRINTER
QUALITY CONTROL
To ensure artifact-free lms are produced with consistent gray levels that
match the image appearance on the lming console.
Operating levels should be established at the initiation of the QC program,
and whenever a signicant change is made in the lm system, e.g., change
of lm type, chemicals, or processing conditions.
Film printer QC is performed weekly if lm is used for primary
interpretation. If hardcopy images are not used for primary interpretation,
this test does not need to be performed. However, if the printer is used
infrequently (e.g., backup printers or ones used for occasional printing
for patients), this test should be performed prior to clinical use.
1. Densitometer
2. Film printer QC chart
About the SMPTE Test Pattern
e SMPTE test pattern (Figure 12) created by the Society of Motion
Picture and Television Engineers, is widely used for evaluating display
systems for medical diagnostic imaging [3,4]. It should be available on all
MRI scanners.
e SMPTE pattern has several components designed to test the quality
of the display. For the purposes of this procedure we are concerned only
with two of those components, which are indicated in Figure 12. e rst
component is a ring of square patches of dierent gray levels ranging
from 0 to 100% in increments of 10%.
e second component is a pair of square gray-level patches, each with a
smaller patch of slightly dierent gray level inside: one is a 0 patch with a
5% patch inside, and the other is a 100% patch with a 95% patch inside.
ese are referred to as the 0/5% patch and the 95/100% patch.
Figure 12. The central portion of the SMPTE test pattern with gray level steps, 0/5%
patch and 95/100% patch.
OBJECTIVE
FREQUENCY
REQUIRED EQUIPMENT

48 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
V. Film Printer Quality Control
Evaluation of the SMPTE pattern as printed in hard copy provides a
mechanism to verify that contrast levels observed on the system monitor
match those displayed on lm. For this reason the SMPTE pattern must
be printed from the MRI, not from SMPTE patterns that may exist on the
camera or on a PACS system.
e qualied medical physicist or MRI scientist is responsible for
establishing the correct operating levels for the lm printer. is procedure
will be carried out when the QC program is initiated and whenever a
signicant change is made in the lm system. e QC technologist then
compares lms against the established operating levels. is is done
weekly to ensure consistent lm quality.
1. Display the SMPTE test pattern on the lming console. Set the
display window and level to the manufacturer-specied values
for the SMPTE pattern. Do not set the window and level by eye;
doing so invalidates this procedure.
2. Examine the SMPTE pattern to conrm that the gray-level
display on the lming console is subjectively correct.
e visual impression should be that there is an even progression
of gray levels around the ring of gray-level patches. Verify that
the 5% patch can be distinguished in the 0/5% patch, the 95%
patch can be distinguished in the 95/100% patch, and that all the
gray level steps around the ring of gray levels are distinct from
adjacent steps.
If these conditions are not met, do not adjust the display window
and level in an eort to correct the problem. Corrective action
is needed. However, the rest of this procedure can be completed
prior to taking corrective action
3. Film the SMPTE pattern. Use a 6-on-1 format and capture the
pattern in all six frames to test the uniformity of response across
the full lm area.
4. Using a lm densitometer, measure the optical density of the 0,
10%, 40%, and 90% gray-level patches of the SMPTE pattern in
the upper le frame of the lm.
5. Plot these optical densities in the appropriate places on the Film
Printer QC chart. Circle any points that fall outside the control
limits. Optical density baseline values should already have been
established and entered on the chart when the operating levels
were set.
6. Put the lm on a light box and inspect it for streaks, uneven
densities and other artifacts.
e ambient lighting at the lming console should be kept very low. e
monitor should be positioned so that there is no glare from room lighting.
e lighting level should be kept the same whenever lming is done.
OPERATING LEVELS
WEEKLY FILM PRINTER
QUALITY CONTROL
PRECAUTIONS AND
CAVEATS

Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 49
V. Film Printer Quality Control
MRI
TECHNOLOGIST’S SECTION
If multiple modalities (such as CT or MRI) are connected to one lm
printer, similar initial setup and QC testing should be performed for each
printer input.
One common cause of variation beyond density control limits is changes
in lm emulsion batches. To reduce the need to recalibrate the lm
printer, do not mix emulsion batches. Instead, use up all of one emulsion
number before starting to use another batch.
Table 2 provides possible optical densities and control limits for selected
SMPTE gray-level patches. ese are oered as a starting point for setting
up the lm printer and can be adjusted according to the preferences
of the supervising radiologist or on the advice of the qualied medical
physicist or MRI scientist who might base the optical densities on Part
14 of the DICOM standard or on other published guidelines. If adopted,
the control limits in Table 2 should not be adjusted to larger values but,
in consultation with the qualied medical physicist or MRI scientist may
be adjusted to smaller values. Dry-lm printers, for example, might use
control limits of 0.10 instead of ±0.15.
Table 2. Optical Densities and Control Limits
SMPTE Patch Optical Density Control Limits
0 2.45 ±0.15
10% 2.10 ±0.15
40% 1.15 ±0.15
90% 0.30 ±0.08
It should be noted that many modern printers perform a self-calibration
each time a new package of lm is loaded. ese printers typically print a
calibrated step pattern that is used to calibrate the system. Even for such
self-calibrating printers, it is recommended that the optical densities for
a SMPTE or step density pattern be measured and recorded weekly to
verify consistent hardcopy performance.
Monitor Gray-Level Failure
In step 2, image display at the monitor is assessed by visual inspection of
the SMPTE pattern. A failure to meet the conditions described in step 2
means the monitor is providing an incorrect gray-scale representation
of the image data. is will lead the technologist to choose incorrect
window and level settings when lming patient studies.
Most oen the problem is caused by misadjustment of the monitor
brightness and contrast. Excessive ambient lighting can also cause the
problem and occasionally components of the display may need repair
or replacement.
Make sure the ambient light is low and comparable to the conditions
under which the data described in step 2 were acquired.
SUGGESTED
PERFORMANCE
CRITERIA

50 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
V. Film Printer Quality Control
Perform the manufacturer’s recommended procedure for contrast and
brightness adjustment of the monitor. If there is any doubt about the
correct procedure, or if the brightness and contrast controls are not
accessible, have the qualied medical physicist or MRI scientist or service
engineer make the adjustments.
e qualied medical physicist or MRI scientist can perform a more
complete set of tests of the monitor (Medical Physicist/MRI Scientist’s
Section IV.E). If there is still a problem, it will be necessary to have the
service engineer correct it.
If any optical densities fall outside the control limits, or artifacts are
found, corrective action should be taken.
e following is a general procedure to use for corrective action. It is
intended to provide guidance when the technologist is uncertain about
how to proceed. Oen the technologist will have information about
the circumstances in which the problem arose and experience with the
equipment that enables him or her to skip some of these steps and move
more directly to the cause of a problem:
1. Repeat the QC procedure to make sure the failure is real, not an
error in the measurements.
2. Check for easily corrected problems:
a. Has the lm been exposed to a light leak? is causes “fogging”
of the lm and shows up in the measurements as elevated
optical densities, with the 90% patch being most sensitive. If
this problem is suspected, check the dark room for light leaks,
then load a few sheets of lm from a new box having the same
emulsion run number, and repeat the measurements.
b. Is the correct type of lm in the cassette, and is it loaded in the
correct orientation?
c. Has there been a change in the type of lm being used? If so,
new action limits will have to be established.
e qualied medical physicist/MRI scientist responsible for lm QC
should be informed and asked to assist with troubleshooting the problem.
If the problem cannot be resolved quickly, consult with the supervising
radiologist to decide whether or not lming can continue while waiting
for the problem to be corrected.
CORRECTIVE ACTION

Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 51
VI. Visual Checklist
MRI
TECHNOLOGIST’S SECTION
To verify the MRI system patient bed transport, alignment and system
indicator lights, RF room integrity, emergency cart, safety lights, signage,
and monitors are present and working properly and are mechanically and
electrically stable.
is test should be performed at least weekly.
Visual checklist (Section VIII.B)
Some of the items on the checklist may not be present on all systems,
and some may be operator convenience features. However, many of the
items are essential for patient safety and high-quality diagnostic images.
It may be necessary to add additional items to the list that are specic
to particular equipment or procedures. ese should be included on the
checklist and in each evaluation.
Each of the items listed in the visual checklist should pass or receive a
checkmark. Items not passing the visual checklist should be replaced or
corrected immediately.
Items missing from the room should be replaced immediately.
Malfunctioning equipment should be reported to the MRI service
engineer for repair or replacement as soon as possible.
OBJECTIVE
FREQUENCY
REQUIRED EQUIPMENT
PRECAUTIONS AND
CAVEATS
SUGGESTED
PERFORMANCE CRITERIA
AND CORRECTIVE ACTION
VISUAL CHECKLIST

52 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
VII. References
1. ACR Practice Parameter for Performing and Interpreting Magnetic
Resonance Imaging (MRI)
2. ACR-AAPM Technical Standard for Diagnostic Medical Physics
Performance Monitoring of Magnetic Resonance Imaging (MRI) Equipment
3. Samei E, Badano A, Chakraborty D, et al. Assessment of display performance
for medical imaging systems, report of the American Association of Physicists
in Medicine (AAPM) Task Group 18. Madison, WI: Medical Physics
Publishing; 2005.
4. Kagadis GC, Walz-Flannigan A, Krupinski EA, et al. Medical imaging
displays and their use in image interpretation. RadioGraphics. 2013;33:
275–290.
REFERENCES

Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 53
VIII. Appendix
MRI
TECHNOLOGIST’S SECTION
Keeping orderly records of the QC tests is as important as doing them. If
there is no record or there is an unintelligible record of the QC test results,
then they might as well not have been done. e following datasheets
are formatted so that important information can appear in a compact,
readable space. e data forms cover the following three areas of the MRI
equipment quality control process:
• Weekly Technologists’ Quality Control
• Weekly System Visual Checklist
• Weekly Film Printer Quality Control
ese data sheets should be stored in a safe place near the scanners for
easy review. Copies of the qualied medical physicist’s or MRI scientist’s
quarterly or annual QC report should be stored in the same location to
facilitate data review and comparison.
All completed data forms should be reviewed and signed by the qualied
medical physicist or MRI scientist at the quarterly or annual equipment
review. At that time suggestions for improvement of the MRI equipment
quality control process should be considered.
A. Weekly Technologist’s Quality Control
Access the Small Phantom Weekly MR Equipment QC Form.
Access the Large Phantom Weekly MR Equipment QC Form.
B. Weekly System Visual Checklist
Access the Weekly System Visual Checklist.
C. Weekly Film Printer Quality Control
Access the Film Printer QC Form.
APPENDIX

Medical Physicist’s/MRI Scientist’s Section
2015
Magnetic Resonance Imaging
QUALITY CONTROL MANUAL

Magnetic Resonance Imaging Quality Control Manual 55
Contents
MEDICAL PHYSICIST’S/
MRI SCIENTIST’S SECTION
REVISIONS .....................................................................................................56
ROLE OF THE QUALIFIED MEDICAL PHYSICIST OR MRI SCIENTIST
IN THE IMAGE QC PROGRAM ..................................................................57
A. Changes Since 2004 Version ......................................................58
ESTABLISHING THE QUALITY CONTROL PROGRAM .......................60
A. Phantom Section ............................................................................ 60
B. Methods and Action Limits for Weekly Quality Control
Tests .....................................................................................................61
C. Establishing Action Limits for Weekly MR Image Quality
Control Tests .....................................................................................62
ANNUAL MRI SYSTEM PERFORMANCE EVALUATION .....................70
A. Magnetic Field Homogeneity ....................................................72
1. Spectral Peak Option ..............................................................74
2. Bandwidth-Dierence Option .............................................74
3. Phase Map Option ...................................................................77
4. Phase-Dierence Map Option .............................................80
B. Slice-Position Accuracy ................................................................87
C. Slice-Thickness Accuracy .............................................................88
D. Radiofrequency Coil Checks ......................................................90
1. Volume Coil Tests ...................................................................... 96
2. Surface Coil Tests ................................................................... 103
3. RF Array Coils .......................................................................... 105
E. Soft-Copy (Monitor) Quality Control .................................... 109
F. MR Safety Program Assessment ............................................. 111
REFERENCES .............................................................................................. 113
APPENDIX ................................................................................................... 116
A. MRI Equipment Evaluation Summary Form ......................116
B. MRI Safety Program Assessment Checklist ........................ 116
C. Hard-Copy (Film) Quality Control Operating Levels ....... 116

Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 57
II. Role of the Qualied Medical Physicist or MRI Scientist
MEDICAL PHYSICIST’S/
MRI SCIENTIST’S SECTION
e success of magnetic resonance imaging (MRI) depends on the
production of high-quality images. ese images must faithfully represent
the anatomy, pathology and physiologic function of patients imaged.
Production of such images is a dicult task.
Although equipment service engineers and technologists are oen
involved in MRI calibration and testing, they typically report how
well instrument values conform to some set of specications, which
are assumed to determine whether the MRI system is performing in
an adequate manner. e qualied medical physicist/MRI scientist
is uniquely qualied to perform tests and analyze data to determine
which sets of specications are relevant to a particular imaging problem.
Oen these tests allow the medical physicist/MRI scientist to recognize
equipment failures before they unacceptably degrade the clinical magnetic
resonance images. e medical physicist/MRI scientist can also perform
tests to determine if imaging irregularities can be attributed to procedural
or equipment errors. e tests performed by the medical physicist/MRI
scientist are also useful to help understand the design strategy used in
producing a particular MRI scanner and recommend the equipment
specications most appropriate for a given practice.
It is the responsibility of the qualied medical physicist/MRI scientist
conducting these tests to accurately convey test results in a written report,
to make recommendations for corrective actions according to the test
results, and to review the results with the radiologists and technologists
working with each scanner. In the written performance report, the
medical physicist/MR scientist should specically include the comparison
of current test results with the baseline values and report trends when
appropriate. is is particularly important in reporting coil performance.
Corrective action should not be limited to repair of MRI equipment by
a qualied service engineer, and should also include recommendations
concerning use of radiofrequency (RF) coils, appropriateness of pulse
sequences, image processing, viewing conditions and the quality control
(QC) process. e qualied medical physicist/MRI scientist must
periodically (at least annually) review the results of the routine QC tests
conducted by the technologist and make appropriate recommendations
regarding these tests. Furthermore, the qualied medical physicist/MRI
scientist must participate in periodic reviews of the MRI QC program as
a whole to ensure that the program is meeting its objectives. e periodic
review should specically include an evaluation of the site’s safety
guidelines, practices, and policies.
Note: If there is need for corrective action, the medical physicist
should instruct the facility to provide a copy of the medical
physicist’s annual system performance evaluation to the equipment
service engineer.
ROLE OF THE
QUALIFIED MEDICAL
PHYSICIST OR
MRI SCIENTIST IN
THE IMAGE QC
PROGRAM

58 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
II. Role of the Qualied Medical Physicist or MRI Scientist
e ACR-AAPM Technical Standard for Diagnostic Medical Physics
Performance Monitoring of Magnetic Resonance Imaging (MRI)
Equipment [1] sets a basic level of tests that should be performed. is
ACR Magnetic Resonance Quality Control Manual expands on those
tests, providing guidance on the conduct, analysis and interpretation
of results.
Both large and small ACR MRI accreditation phantoms may be used for
performing these measurements. In this manual, it is assumed that the
QC technologist typically performs these tests aer a qualied medical
physicist/MRI scientist has determined the range and sensitivity of these
tests for a particular MRI scanner and has set up action limits. ese
recommendations have been incorporated into the weekly QC routines,
which are specied in the MRI Technologist’s Section of this manual.
A. Changes Since 2004 Version
It should be noted that the list of tests and the following test descriptions
are somewhat dierent from the tests and descriptions of the 2004
ACR Magnetic Resonance Imaging Quality Control Manual. Specically,
the tests for interslice RF interference have been removed from the list
and signicant revisions to the recommended procedures for magnetic
homogeneity and percent image uniformity (PIU) assessments have
been made. e RF cross-talk assessment was removed in light of the
fact that essentially all modern systems were found to be capable of easily
meeting the guideline of maintaining at least 80% SNR when comparing
0-gap images to 100% slice-gap images. However, it is emphasized that
it is the responsibility of the qualied medical physicist/MRI scientist
to determine if this assumption is appropriate for each specic system
being evaluated and to add a cross-talk assessment when indicated.
Alternative approaches to the magnetic eld homogeneity assessment
were identied to assist the qualied medical physicist/MRI scientist
when evaluating systems that do not allow access to phase-angle images.
In addition, previously implemented changes in image uniformity, PIU
>87.5% for systems up to and including 1.5T and PIU >82% for 3T
systems have now been incorporated. We also have added criteria for
signal ghosting (<2.5%) and low-contrast detection (a total of at least
nine rows of test objects for 1.5T and below, and at least 37 rows of test
objects for 3T systems) to the manual to be consistent with the ACR MRI
Accreditation Program requirements. Other revisions have been made to
improve clarity.
e annual performance evaluation must also include an assessment of
the MRI safety program (Section IV.F) in addition to an inspection of the
mechanical integrity of the system. e annual performance evaluation
will comprise a protocol that the medical physicist/MRI scientist can use
to assess the functionality of an MRI scanner and to measure its reliability
by repeating these tests at regular intervals over time. Part III of this
section describes how the qualied medical physicist/MRI scientist can
set up tests for weekly QC and establish action limits. Part IV describes
tests that comprise an annual equipment evaluation by the qualied
medical physicist/MRI scientist. Part V is a list of references, and Part VI

Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 59
II. Role of the Qualied Medical Physicist or MRI Scientist
MEDICAL PHYSICIST’S/
MRI SCIENTIST’S SECTION
is an appendix, which contains an MRI Equipment Evaluation Summary
form and MR Safety checklist as well as a description of Hard Copy (Film)
Quality Control Operating Levels. e qualied medical physicist/MRI
scientist may use a data report format of his or her choice as long as the
required information is present.
e ACR has taken guidance from the test procedures outlined in the
National Electrical Manufacturers Association (NEMA) publications on
standards for MRI image quality and from the American Association of
Physicists in Medicine (AAPM) Report of MR Subcommittee Task Group
I. e documents most relevant to the writing of this manual include
the following:
• MS 1-2008: Determination of Signal-to-Noise Ratio in Diagnostic
Magnetic Resonance Images
• MS
2-2008: Determination of Two-Dimensional Geometric
Distortion in Diagnostic Magnetic Resonance Images
• MS 3-2008: Determination of Image Uniformity in Diagnostic
Magnetic Resonance Images
• MS
5-2010: Determination of Slice ickness in Diagnostic
Magnetic Resonance Imaging
• MS 6-2008: Determination of Signal-to-Noise Ratio and Image
Uniformity for Single-Channel, Non-Volume Coils in Diagnostic
Magnetic Resonance Imaging (MRI)
• MS 9-2008: Characterization of Phase Array Coils for Diagnostic
Magnetic Resonance Images
ese documents and other MR-related NEMA standards can be
obtained from the NEMA website (www.nema.org) [2,3,4,5,6,7].
• AAPM Report No. 100: Acceptance Testing and Quality
Assurance Procedures for Magnetic Resonance Imaging Facilities
is document and other MR-related reports can be obtained from the
AAPM website (www.aapm.org) [8].
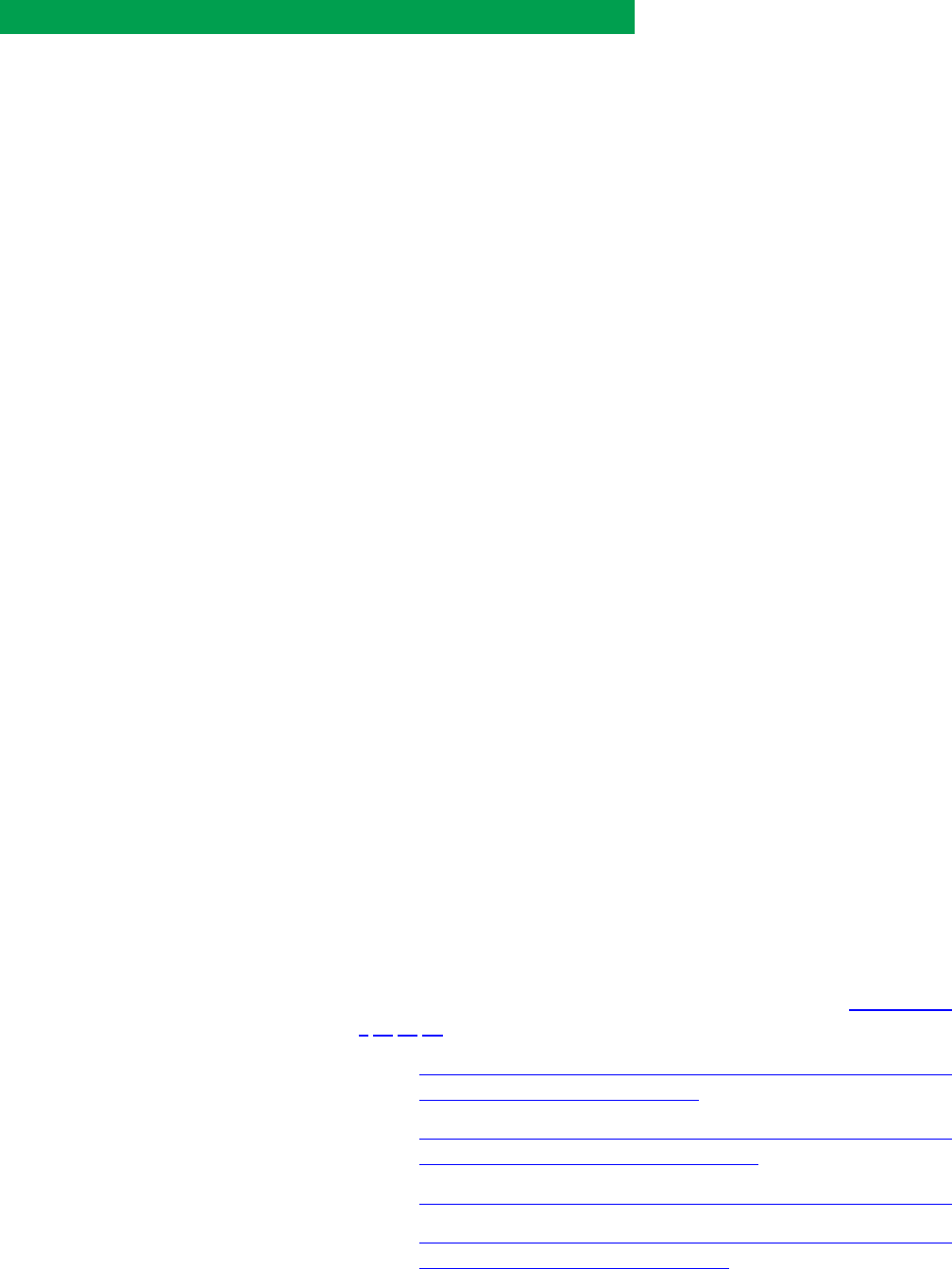
60 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
III. Establishing the Quality Control Program
A. Phantom Section
Currently, the ACR MRI Accreditation Program has two phantoms: large
and small. e large phantom is used for whole body magnets, and the
small phantom is used for extremity magnets. is manual describes the
use of both phantoms.
e ACR MRI accreditation large phantom is a short, hollow cylinder
of acrylic plastic closed at both ends. e inside length is 148 mm, and
the inside diameter is 190 mm. e phantom is lled with a solution of
nickel chloride and sodium chloride (10 mM NiCl
2
and 75 mM NaCl,
or 0.45% NaCl by weight). e outside of the phantom has the words
“NOSE” and “CHIN” etched into it as an aid when orienting the phantom
for the scanner as if it were a head.
e ACR MRI accreditation small phantom is a short, hollow cylinder of
acrylic plastic closed at both ends. e inside length is 100 mm, and the
inside diameter is 100 mm. It is lled with the same solution of nickel
chloride and sodium chloride as the large phantom: 10 mM NiCl
2
and 75
mM NaCl, or 0.45% aqueous NaCl by weight.
Both large and small ACR MRI phantoms contain a separate vial lled
with 20 mM NiCl2, but with no NaCl.
Inside the phantom are structures designed for performing the following
seven quantitative tests using measurements on the digital images:
1. Geometric accuracy
2. High-contrast spatial resolution
3. Slice-thickness accuracy
4. Slice-position accuracy
5. Image intensity uniformity
6. Percent signal ghosting
7. Low-contrast detectability
More detailed information on the ACR MRI accreditation phantom can
be found in the ACR documents and is downloadable from www.acr.org
[9,10,11,12]:
• Site Scanning Instructions for Use of the MR Phantom for the
ACR MRI Accreditation Program
• Site Scanning Instructions for the Use of the Small MR Phantom
for the ACR MRI Accreditation Program
• Phantom Test Guidance for the ACR MRI Accreditation Program
• Phantom Test Guidance for Use of the Small MRI Phantom for
the ACR MRI Accreditation Program
e ACR MRI accreditation phantoms are the recommended phantoms
for weekly QC. However, if the ACR phantom is incompatible with the
required test, another phantom can be used. First, the qualied medical
ESTABLISHING THE
QUALITY CONTROL
PROGRAM

Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 61
III. Establishing the Quality Control Program
MEDICAL PHYSICIST’S/
MRI SCIENTIST’S SECTION
physicist/MRI scientist should conrm that the proposed alternative
phantom meets the following criteria:
• It electrically loads the head coil approximately as much as a
typical patient.
• e T1 and T2 of the ller material are within the range of normal
so tissues (see NEMA MS 1-2008 [2]).
• It is about the same size as a typical adult head, and it ts in the
head coil.
• It can be easily and reliably positioned in the same location and
orientation every time it is used.
• ere is at least one location within the phantom that is free of
structures and presents an area of uniform signal suitable for
assessing percent image uniformity as described later.
In most clinical scans, the patient is the primary source of noise [13].
To best approximate the clinical situation, the coil should be electrically
loaded by using an appropriate ller material or by some other means,
so that the electrical properties of the body are simulated. e NEMA
standard for determining SNR in MRI (MS 1-2008) lists the coil loading
characteristics appropriate for such a phantom. Note that this criterion
contradicts the phantom specied in AAPM report No. 28 [14], in which
a phantom lled with nonconducting material is recommended
B. Methods and Action Limits for Weekly Quality
Control Tests
Eective equipment QC requires the regular assessment of system
performance. us, measurements should be taken at least weekly to
ensure that the scanner is operating eectively. e scope of these tests is
constrained by a desire to complete them expeditiously. e weekly tests,
which include measurement of center frequency and SNR, assessment of
image quality and a check for image artifacts, can all be performed using
the ACR MRI accreditation phantom. ese tests are described in detail
in the MRI Technologist’s Section of this manual.
MRI equipment manufacturers may have established daily methods
for measuring some or all of these parameters that will likely use pulse
sequences and phantoms dierent from those recommended by the
ACR. Not all manufacturer-supplied procedures, however, are suitable.
Due to economic constraints, the action levels set by vendors may be
more conservative or liberal than the level of scanner quality control
desired by the site. In addition, many vendors use phantoms that are
lled with paramagnetic solutions having T1 values that are sensitive to
changes in temperature and static magnetic eld (B
0
) strength [15]. Some
manufacturers encourage the collection of data; however, these data are
not analyzed until aer there is a clinical system failure, and are thus not
being used as a quality control tool.

62 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
III. Establishing the Quality Control Program
It is the task of the qualied medical physicist/MRI scientist to evaluate
the methods and eectiveness of the MRI equipment manufacturer’s
QC tests. e decision to use a procedure that is an alternative to the
recommended tests, using the ACR MRI accreditation phantom, should
only be implemented aer the facility obtains a recommendation and
justication from a qualied medical physicist or MRI scientist.
At a minimum, the procedure should satisfy the following criteria:
• Use the ACR phantom or an alternative phantom meeting the
criteria described above.
• Acquire and reconstruct images of the phantom. It is not sucient
to acquire only raw data.
• e pulse sequence and reconstruction soware should be the
same as those used for clinical imaging, with sequence parameters
typical of those used in clinical imaging.
• Produce and report to the user a numerical value for all test
measurements. Simply reporting “pass” or “fail” is not acceptable.
• SNR values are derived from images reconstructed in the normal
manner, not raw signals.
• Images produced are derived as if they were normal clinical
images and may be displayed and archived as desired.
• Report the center frequency for the image acquisition or ensure
that it is conveniently available to the user.
us, although it is important for a site to follow the vendor’s
recommendations, it is not always clear that the vendor’s methods are
adequate to ensure a high level of QC. e MRI Technologist’s Section
describes the recommended tests, using the ACR MRI accreditation
phantom. e qualied medical physicist/MRI scientist may determine
when it is necessary to deviate from these tests. If this decision is
made, the new procedures and their recommended action levels must
be documented in detail and made available in writing, as a part of
the facility’s MRI Quality Assurance Procedures Manual (Radiologist’s
Section IV.E).
C. Establishing Action Limits for Weekly MR Image
Quality Control Tests
It is the responsibility of the qualied medical physicist/MRI scientist
to set the action limits and to ensure that they are adequately sensitive
to detect MRI equipment problems. e suggested performance criteria
given in this document are liberal enough that all properly functioning
equipment should be able to meet them. erefore, it is not appropriate
to relax the recommended performance criteria. For MRI systems with
advanced technology, the qualied medical physicist/MRI scientist may
wish to tighten criteria. Failure to meet these criteria is an indication that
the equipment is functioning poorly and that corrective action is required.

Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 63
III. Establishing the Quality Control Program
MEDICAL PHYSICIST’S/
MRI SCIENTIST’S SECTION
e normal values of LCD and center frequency are dierent for each
scanner. LCD is strongly dependent on the sequence parameters and
choice of phantom. erefore it is necessary to begin a weekly QC
program by establishing action limits (control limits) for LCD and
center frequency that are appropriate to the scanner, phantom, and pulse
sequence parameters used in the QC program.
First, verify that the scanner is at peak performance levels.
If the scanner has just passed its acceptance test and a set of baseline
data has been established, that is sucient verication. Otherwise, do
the following:
1. Have the service engineer run the manufacturer’s diagnostic tests
to conrm that the scanner is performing well as measured by
those tests and that it meets all of the manufacturer’s performance
specications.
2. Review the results of the manufacturer’s diagnostic tests to
provide independent conrmation that appropriate and adequate
tests were run and that the test results meet manufacturer’s
specications.
3. Have the supervising radiologist examine several clinical images
and conrm that the image quality is as good as expected for this
make and model of scanner. For this purpose, it is better to assess
the image quality from the console or a diagnostic workstation
rather than from lm, since that eliminates any problems with
lm production from the assessment.
Collect QC data for 10 days following the procedures found in the
MRI Technologist’s Section of this manual. Use the MRI Equipment
Performance Evaluation Data Form (MRI Technologist’s Section,
Appendix VIII.A) provided in this manual to record the results. is data
form with the baseline measurements should be kept in the weekly QC
notebook (MRI Technologist’s Section III.C). Write the word “baseline”
on the data form prominently to distinguish it from ordinary QC data.
1. Center Frequency
e resonance frequency is dened as that RF frequency (f
0
) that matches
the B
0
(in Tesla) according to the Larmor equation:
f
0
= (
γ
2π
)B
0
Where γ is the gyromagnetic ratio for the nucleus under study. For
hydrogen nuclei, the quantity
(
γ
2π
)
is 42.58 MHz/T. For a 1.5T system,
the resonance frequency should be approximately 63.87 MHz.
e action limits for center frequency are expressed in terms of the
permissible weekly change. Typically for superconducting magnets the
change from week to week should be less than a few parts per million
(ppm). Permanent magnet systems will generally exhibit greater week-
to-week variation. Permissible action limits will depend upon the specic
system and should be set individually by the medical physicist. Enter the

64 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
III. Establishing the Quality Control Program
action limits in the space provided on the Data Form for Weekly MRI
Equipment Quality Control (MRI Technologist’s Section, VIII.A) with
the baseline data.
A more complete discussion of factors aecting magnetic eld dri can
be found in AAPM Report No. 100 [8].
Service-related center frequency change: In the case of a service-
related change in center frequency, accept the large, abrupt change in
center frequency and continue applying the center frequency action
criterion as before. Make an entry explaining what was done in the “QC
Incidents and Actions” section of the QC notebook (MRI Technologist’s
Section, III.C).
2. Transmitter Gain or Attenuation
Transmitter (TX) gain or attenuation is typically a measure of the power
needed to nutate the bulk magnetization by 90°. us, for the same coil
and phantom, TX gain should remain relatively constant if the MRI unit is
performing normally. A change in this parameter may indicate a problem
in some part of the RF transmitter and/or its associated coils.
Changes in TX gain are directly related to changes in SNR. is is a coarse
measure for two reasons. First, the TX gain or attenuation is generally
reported in decibels, a logarithmic unit. Second, these measurements
usually are made over the entire volume of the central slice. Nevertheless,
the RF transmitter gain measurement is a useful rst check of the system
and requires no extra scan time since it is measured with each prescan.
Any reduction in TX attenuation (or increase in transmitter gain)
required to perform the same study on a phantom should be taken as
an indication of potential MRI system problems. ese problems may
include impairment of the RF transmission eld, degradation of the B
0
magnetic eld homogeneity or noise added by the RF receiver chain.
Potential problems with the receiver chain electronics include noise
generated by active electronic components, such as PIN diodes, or
inadequate isolation between the TX and receiver (RX) channels of the
system. For more detailed information, including a detailed derivation of
the relationship between SNR and transmitter attenuation, the reader is
referred to Redpath and Wiggins [16].
3. Geometric Accuracy Measurements
Geometric accuracy is a term used to describe the degree of geometrical
distortion present in images produced by the MRI system. Geometric
distortion can refer to either displacement of displayed points within an
image relative to their known location or improper scaling of the distance
between points anywhere within the image. In terms of the weekly image
QC tests, the technologist is concerned only with the issue of proper
scaling. is is because measurements are made only along the central
axes of the ACR MRI phantom. However, the qualied medical physicist/
MRI scientist should also examine image displacement and distortion as

Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 65
III. Establishing the Quality Control Program
MEDICAL PHYSICIST’S/
MRI SCIENTIST’S SECTION
part of the annual review and should calculate and record the percent
geometric distortion (%GD).
%GD=
true dimension-observed dimension
true dimension
× 100
Geometric distortion may be measured between any two points within
the eld-of-view (FOV) provided that pixel resolution is not a signicant
source of error. Most modern MRI systems can achieve a %GD of less
than ±1%, which corresponds to a diameter measurement on the ACR
phantom of ±2 mm and a length measurement of ±1.5 mm. us,
geometric accuracy measurements on the ACR MRI accreditation
phantom, when measured over a 25-cm FOV (large phantom) and a
10-cm FOV (small phantom), are generally considered acceptable if they
are within ±2 mm of the true values.
Gradient ampliers need time to warm up and stabilize when they are
turned on. Some sites power o their scanner hardware, including gradient
ampliers, overnight. ose sites should ensure that their hardware has
been on at least an hour before images of the phantom are acquired.
Another factor leading to failure is the use of a very low MRI receiver
bandwidth. It is common practice on some scanners and at some facilities
to reduce receiver bandwidth to increase SNR. is strategy can be
pushed to the point that normal inhomogeneities in the magnetic eld
(B
0
) manifest themselves as large spatial distortions in the image. On
most scanners, the default bandwidth for T1-weighted acquisitions is set
high enough to avoid this problem. If the geometric accuracy test exceeds
the action limits and the ACR T1-weighted series (MRI Technologist’s
Section, IV.C) was acquired at low bandwidth, one should try to acquire
the images again at a larger bandwidth to see if the problem is eliminated.
B
0
eld inhomogeneities could be caused by improper adjustment of the
gradient osets, improper adjustment of passive and/or active magnet
shims, or ferromagnetic objects such as a pocket knife or large hair clip
lodged in the magnet bore. Especially on low-eld magnet systems, which
have relatively small volumes of gradient linearity and B
0
homogeneity,
it is possible that abnormally high B
0
eld inhomogeneities could cause
signicant dimensional errors in the phantom images. e service
engineer should measure the homogeneity of the magnet periodically,
and any inhomogeneity large enough to cause failure of the geometric
accuracy test should be corrected (see Section IV.A).
Depending on the mix of studies at a given site, the qualied medical
physicist/MRI scientist may determine that a more strict action limit
should be put in place. Geometric accuracy is of particular interest in the
following situations:
1. MRI images used for stereotactic surgical or radiation therapy
planning
2. Assessment of the geometrical reproducibility of pulse sequences
that use extremely high-gradient amplitudes and/or switching
rates (e.g., EPI)

66 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
III. Establishing the Quality Control Program
3. Co-registration of images acquired at various time points and/or
from multiple scanners
If these types of studies are performed regularly on a given system, the
qualied medical physicist/MRI scientist may decide that the volume
geometric linearity should be checked much more oen than annually. For
measurements pertinent to radiation oncology, the radiation oncology
physicist in charge of the procedure should be consulted to determine the
most appropriate frequency for this test (Moerland et al [17]).
Spatial linearity measurements should also be performed on lmed
images to provide combined performance information about the MR
imager as well as the video and lming systems. For more information on
volume geometric accuracy measurements, see Bakker et al [18].
4. High-Contrast Spatial Resolution
e origin of any detectable changes in high-contrast spatial resolution
should be determined. Inappropriate ltering of the MRI signal may
result in these types of changes. If high-contrast resolution is signicantly
degraded, check to make sure that any user-selectable spatial image
ltering is turned o.
Poor eddy current compensation can cause failure. e scanner’s service
engineer should check and adjust the eddy current compensation if this
problem is suspected. Geometric errors from gradient miscalibration,
B
0
inhomogeneity and low acquisition bandwidth also can cause failure
of this test. is problem also can arise if a gradient power supply
becomes unstable.
With a eld-of-view (FOV) of 250 mm using a 256 × 256 matrix size
for the large phantom and a FOV of 120 mm using a 152 × 192 matrix
size for the small phantom, scanners should be able to resolve the 1-mm
hole pattern for the large phantom and the 0.8-mm hole pattern for the
small phantom.
5. Low-Contrast Detectability (LCD)
Most scanners should be able to display at least nine spokes of holes out of
40 available spokes in slices 8–11 with the large phantom or at least nine
spokes out of 20 available spokes in slices 6–7 with the small phantom for
MRI systems with eld strengths less than 3T using the ACR T1-weighted
axial scanning protocol (see Phantom Test Guidance for the ACR MRI
Accreditation Program [10]). For MRI systems with eld strengths of 3T,
scanners should be able to display at least 37 spokes out of the 40 available
spokes in slices 8–11 for the large phantom. Typical LCD performance
as a function of eld strength is shown in Table 1. Slight changes in
the number of spokes detected may arise due to slice-positioning
errors, intermittent ghosting, or phantom tilting. e qualied medical
physicist/MRI scientist should determine the minimum number of
spokes perceived that constitute the action limit. Typically, a reduction of

Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 67
III. Establishing the Quality Control Program
MEDICAL PHYSICIST’S/
MRI SCIENTIST’S SECTION
more than three spokes perceived would be cause for concern, indicating
that the test should be repeated aer positioning is checked.
Table 1. Recommended slice of the ACR large MRI phantom to use for
weekly low-contrast detection QC and typical number of spokes visible
in the recommended slice and on all slices as a function of magnetic
eld strength.
Low-Contrast Detectability
Recommendations by Field Strength for
Large ACR Phantom for the ACR T1 Series
Field Strength Recommended
weekly QC slice #
Typical number of
spokes visible in
recommended QC slice
Total number of
spokes on all slices
0.2 11 4 12
0.3 11 5–7 21
0.5 10 6–9 27
0.7 10 6–8 31
1.0 9 7–8 34
1.5 8 6–9 36
2.0 8 9–10 38
3.0 8 10 40
e number of spokes visualized should be recorded weekly in a log
for trend analysis. e qualied medical physicist/MRI scientist sets
the action level based on a statistical analysis of a set of baseline data
obtained from the specic MRI system. It is important to ensure that the
technologist(s) are reproducibly positioning the phantom and prescribing
the slice locations.
If slice positioning is accurate, changes in the number of spokes visualized
may be due to a change in the SNR. If the SNR change is acceptable, then it
will be necessary to establish new action limits. Acquire weekly LCD data
and record them on a new Data Form for Weekly MRI Equipment Quality
Control (MRI Technologist’s Section, VIII.A). Make a note of the change
in the QC notebook (MRI Technologist’s Section, III.C) explaining the
problem and actions taken. Proceed with patient scanning, starting with
a fresh Data Form for Weekly MRI Equipment Quality Control (MRI
Technologist’s Section, VIII.A).
Use the Data Form for Weekly MRI Equipment Quality Control (MRI
Technologist’s Section, VIII.A) for the next 10 days as the baseline data
for the new LCD action criteria. During that time, before the new criteria
are set, monitor the SNR values (Section IV.D) and treat unusually
large uctuations or dri in the values as equivalent to a failure of the
action criteria.
If the problem cannot be corrected immediately, consult with the supervising
radiologist to determine whether patient scanning can proceed.

68 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
III. Establishing the Quality Control Program
6. Artifact Evaluation
Common image artifacts noted on phantom images include the following:
• Gross geometric distortion
• Ghost images
• Line or pixels with unusually high and/or low intensities
• Receiver saturation errors
• Inappropriate image blurring or enhanced truncation artifact
Gross geometric distortion can occur even on a system that passes the
geometric accuracy test because geometric accuracy measurements, as
prescribed in the MRI Technologist’s Section, are only along the primary
axes of the phantom. is problem is discussed in the MRI Technologist’s
Section IV.C geometric accuracy and the references cited therein.
Ghost images present as low signal intensity representations of structures
in the MR image that are shied in the phase-encoding direction. e
“ghosts” can be due to poor RF connections or motion. ey are discussed
in greater detail below in Section IV.D, Radiofrequency Coil Checks.
Lines or pixels with unusually high and/or low intensities can occur
through several processes:
1. Bright lines can result from DC osets on the MRI signal,
especially on images with no signal averaging. Typically view-to-
view phase alternation allows these artifacts to be located o to
the side of the image and do not aect the utility of the image. A
less frequent source of bright-line artifacts is an imperfect 180°
pulse in a spin-echo acquisition. e position of the resulting
artifactual line depends on the value of the read-out gradient
and therefore can aect clinical image quality. Interference from
external sources of RF can cause linear “single frequency” or
broadband artifacts.
2. Zipper artifacts can be caused in a spin-echo sequence due to
transverse magnetization being produced by imperfect slice
excitation of the 180° refocusing pulse. e signal is constant
from phase-encoding view to phase-encoding view so that
it presents as a single frequency line of alternating intensity
on the image.
3. DC-oset errors also can appear as a single bright pixel
(sometimes as a dark pixel if overow or image processing has
occurred) at the center of the image matrix. ey are due to
improper scaling of low-frequency components (typically DC)
in the Fourier transformation of the NMR time-domain signal.
4. Dotted-line artifacts across the image in the phase-encoding
direction may be due to RF interference. If such artifacts are
noted, one should check the integrity of the RF room shielding
or identify the source of the RF interference, such as equipment
or lighting within the MRI scan room.

Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 69
III. Establishing the Quality Control Program
MEDICAL PHYSICIST’S/
MRI SCIENTIST’S SECTION
If the RF attenuation (or gain) is not set correctly during the prescan,
the signals acquired during one or more phase-encoding steps during
image signal acquisition could be larger than the maximum allowable
digitization step. is “saturates” the receiver so that the signal is not
accurately digitized and the image is not properly displayed following
the inverse Fourier transform. is image appears to have a very bright
background that is smooth, not speckled like random noise. Spike signals
that can be caused by malfunctioning electronics also can produce this
type of artifact.
Inappropriate image blurring or enhanced truncation artifacts can be
caused by excessive ltration. Use of zero-ll interpolation or lters that
enhance spatial resolution tends to cause truncation artifacts to become
more apparent. In contrast, lters that enhance SNR tend to result in
increased image blurring.
e facility’s MRI Quality Assurance Procedures Manual (Radiologist’s
Section IV.E) should state that any noticeable artifacts need to be brought
to the attention of the service engineer and the qualied medical physicist
or MRI scientist. e qualied medical physicist/MRI scientist must
determine how oen and for what duration an image artifact must appear
in order for it to be signicant enough to be worthy of investigation.
Artifacts can be very transient phenomena. When artifacts are noted,
record any ancillary conditions that may be dierent from normal
procedures. ese data can be helpful to determine possible artifact
sources. It is also good policy for the technologist to save the raw data of
images in which artifacts occur. If the raw image data are accessible, they
can aid in the diagnosis of artifact sources by noting the characteristics
of the artifacts in k-space. For more detailed information on various MRI
artifacts see Vlaardingerbroek and den Boer [19] and Haacke et al [20].

70 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
IV. Annual MRI System Performance Evaluation
e annual MRI system performance evaluation must include the
previously described technologist QC measurements, scanning and
analyzing the ACR MRI phantom as submitted for accreditation, and
the measurements described below and listed in Table 2. e method
for performing these measurements may vary according to the needs
of the facility and the preference of the medical physicist/MRI scientist.
If the medical physicist/MR scientist is using other than ACR-specied
methods, the alternative methods should be fully documented for the
facility’s record. For some of these tests, the ACR MRI accreditation
phantom may not be the most appropriate tool. In addition, many of
these values will be system-specic, and baseline values will have to be
determined when the system is commissioned or when the qualied
medical physicist/MRI scientist rst undertakes a performance analysis.
In the written performance report, the medical physicist/MRI scientist
should specically include the comparison of current test results with
the baseline values and report trends when appropriate. At the time of
these tests, the qualied medical physicist/MRI scientist also reviews the
weekly QC records, service logs, and safety policies and procedures, and
recommends changes in QC program procedures indicated by these data.
ANNUAL
MRI SYSTEM
PERFORMANCE
EVALUATION

Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 71
IV.
Annual MRI System Performance Evaluation
MEDICAL PHYSICIST’S/
MRI SCIENTIST’S SECTION
Table 2. Specic Required Tests Required for Annual MRI System
Performance Evaluation
Performance Tests
(ose in italics
indicate tests that
can be performed by
scanning the ACR MRI
Phantom)
Technologist
QC (Weekly)
Medical Physicist/
MR Scientist
(Annually)
1 Setup and Table
Position Accuracy
X X
2 Center Frequency X X
3 Transmitter Gain or
Attenuation
X X
4 Geometric Accuracy
Measurements
X X
5 High-Contrast Spatial
Resolution
X X
6 Low-Contrast
Detectability
X X
7 Artifact Evaluation X X
8 Film Printer Quality
Control (if applicable)
X X
9 Visual Checklist X X
10 Magnetic Field
Homogeneity
X
11 Slice-Position Accuracy X
12 Slice-ickness Accuracy X
13 Radiofrequency Coil
Checks
X
a. SNR X
b. Percent Image
Uniformity (PIU)
X
c. Percent Signal
Ghosting (PSG)
X
14 So-Copy (Monitor)
Quality Control
X
15 MR Safety Program
Assessment
X

72 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
IV. Annual MRI System Performance Evaluation
A. Magnetic Field Homogeneity
Homogeneity refers to the uniformity of the main magnetic eld strength
B
0
over a designated volume. Magnetic eld inhomogeneity is usually
specied in parts per million (ppm) of the magnetic eld strength
over a spherical volume (DSV=diameter of spherical volume). e
actual homogeneity will be inuenced by a variety of factors, including
imperfections in the magnet manufacturing, the degree to which the B
0
magnetic eld is perturbed by external ferromagnetic structures or, in the
case of clinical scans, the presence of the patient within the eld and the
degree to which the above inuences can be compensated using magnetic
elds produced by shim and/or gradient coils. e most common problem
caused by magnet inhomogeneities at high eld strength is diculty in
obtaining uniform fat suppression. Inhomogeneities also can contribute
to geometrical distortion of images (particularly at low eld strengths),
adversely inuence image signal uniformity, increase the severity of wrap
artifacts, and compromise SNR in some fast imaging sequences.
is is sometimes a dicult test to perform independently. If the
magnetic eld homogeneity test cannot be performed, the physicist
should note this in the report, and the facility must arrange for the service
engineer to provide the medical physicist/MRI scientist with a copy of
the most recent eld map, which should be led as an attachment to the
report. Test results should demonstrate that magnetic eld homogeneity
is within manufacturer’s specications and was performed within the
last six months. If the medical physicist/MRI scientist has an alternate
method of accurately assessing magnetic eld uniformity, it is acceptable,
providing the report includes a description of the methodology used.
If a magnet is perfectly homogeneous over the imaging volume, all of
the water protons (also referred to as spins) will precess at the same
frequency, the magnet center frequency, which is directly proportional
to the strength of the magnet. Aer applying an RF excitation pulse, and
in the absence of any imaging gradients, a Fourier transform (FT) of the
resulting signal will exhibit a strong, narrow peak at that center frequency.
If the magnet were perfectly homogeneous, one would expect the FT to
have a peak at only one frequency (i.e., be a delta function). However,
random spin-spin interactions temporarily cause some protons to precess
a little faster than the center frequency, whereas others will temporarily
precess more slowly. is results in spreading of the peak with the
full-width half-maximum (FWHM) of the frequency peak related to the
average T2 time constant. A long T2 will have a narrow peak (little spin-
spin interaction), and a short T2 will have a very broad peak (substantial
spin-spin interaction). Along with these random spin-spin interactions,
anything that causes imperfections in the static magnetic eld will cause
this spectral peak to spread. e greater the imperfections and the more
inhomogeneous the magnetic eld, the wider the peak. Although it is
quick and easy to perform, monitoring the spread of the spectral peak is
a crude and insensitive method of assessing magnet homogeneity. is
measurement contains no information regarding spatial variations of the
magnetic eld.
OBJECTIVE
GENERAL THEORY

Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 73
IV.
Annual MRI System Performance Evaluation
MEDICAL PHYSICIST’S/
MRI SCIENTIST’S SECTION
Gradient-echo (GRE) imaging techniques can be used to obtain spatial
information about the magnetic eld. (Spin-echo techniques cannot
be used because the 180° pulse used to generate the spin-echo reverses
and eliminates any eect of magnetic eld inhomogeneities.) Ignoring
T2 eects, if a magnet is perfectly homogeneous, then at the time of a
gradient echo, all of the spins would be completely in phase with each
other. As stated above, spatial variations of the magnetic eld will cause
spins in dierent parts of the FOV to spin a little faster or a little slower,
causing the slower spins to lag behind the spins at the center frequency
and the faster ones to run ahead of the spins at the center frequency. e
greater the dierence in the magnetic eld across the phantom volume,
the greater the dierences in the spin frequencies and the greater the
spread of the phases of the spins at the echo time. e dierences in phases
of the spins measured by a gradient echo are linearly proportional to the
dierences in frequencies (hence, linearly proportional to the dierences
in magnetic eld) and linearly proportional to the echo time. An echo
time of 10 ms corresponds to a frequency of 100 Hz (1/0.010 seconds) per
phase cycle. A spin that precesses 25 Hz faster or slower than the center
frequency will be π/2 radians (90°) out of phase with the center frequency
spins. If a TE of 20 ms is used, the spins have twice as long to dephase, so
they will be π radians (180°) out of phase.
Reconstructing phase images, as opposed to the more common magnitude
images, provides a map of the dierences in precessional frequencies
relative to the center frequency and therefore a map of the changes in the
magnetic eld. e drawback of the phase map method is that dierences
in the magnetic eld are not the only causes of spatial variation of phase.
If the echo peak is not exactly at the center of the sample window, it will
cause a linear phase ramp across the FOV. At higher eld strengths, the
RF does not penetrate water-lled phantoms as well as at low elds. ese
RF penetration dierences, as well as magnetic susceptibility dierences,
result in changes in the phase of the received signal that vary by distance
from the surface of the phantom. Problems with the RF receiver chain
can also result in phase variations. Because of all of these other sources
of phase variation, phase map images only provide an upper limit on the
frequency or magnetic eld variation across the FOV; the true variation
will be lower.
With the exception of phase dierences caused by magnet eld
inhomogeneities, most of these other phase variations are not aected
by changes in echo time. ese other phase variations can be removed
by acquiring two GRE images, reconstructing phase maps, and then
subtracting the two phase-map images. e resulting phase dierences
will be proportional only to the magnetic eld variations and to the
dierence in echo times. For example, if echo times of 10 and 15 ms are
used, the resulting dierence of 5 ms corresponds to 200 Hz per phase
cycle. A phase shi of 90°, or one-quarter of a cycle, would mean there is a
50 Hz dierence in the resonance frequency. If this were the peak-to-peak
dierence across the DSV at 1.5T, then the magnetic eld inhomogeneity
would be reported as 50 Hz/64 MHz (the center frequency at 1.5T) or

74 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
IV. Annual MRI System Performance Evaluation
0.78 ppm. e phase-dierence method can be performed using either
2-D or 3-D GRE sequences and provides the most accurate measurement
of magnetic eld homogeneity.
Four dierent methods are presented: the spectral peak method, the
bandwidth-dierence method, the phase-map method (using GRE phase
maps acquired at a single TE value), and the phase-dierence method
(subtraction of GRE phase maps acquired at two dierent TE values).
1. Spectral Peak Option
1. Position a uniform, spherical phantom at the center of the magnet.
e phantom should have a spherical volume diameter similar to
that cited by the manufacturer’s homogeneity specications.
2. Obtain a spectrum from the sample. is can oen be
accomplished even without special spectroscopy soware by
going into manual tuning or prescan mode. Ensure that the
frequency resolution is much less than the expected peak width.
1. Measure the FWHM of the spectral peak. Convert the FWHM
from Hz to ppm of the B
0
eld strength (in Tesla) using the
Larmor equation:
FWHM(ppm) =
42.576B
0
(T)
FWHM(Hz)
e FWHM (ppm) denes the inhomogeneity over the phantom
volume.
2. Bandwidth-Dierence Option
An additional method for determining eld homogeneity has been
described by Chen et al [21]. is method is of particular value when
assessing systems that do not provide access to either phase images or
a detailed frequency plot. e bandwidth-dierence method makes use
of the fact that spatial distortions are a function of eld homogeneity
and gradient strength. Since for a given FOV in the frequency-encoding
direction (FOV
x
) the frequency-encoding gradient strength (G
x
) is
a function of receiver bandwidth (BW
x
), it is possible to estimate eld
homogeneity (ΔB
0
) by comparing the spatial distortion (d
1
- d
2
) observed
at the same FOV
x
for both small (BW
1
) and large (BW
2
) bandwidth
acquisitions (Figure 1).
e following equation is used for estimating the magnetic eld
inhomogeneity in ppm, using the bandwidth-dierence option:
∆B
0
(ppm) =
42.576MHz/T × B
0
(T) x FOV
x
× (BW
2
- BW
1
)
(BW
1
× BW
2
) x (d
1
- d
2
)
, where
BW
1
= smallest available receiver bandwidth (Hz)
BW
2
= largest available receiver bandwidth (Hz)
TEST PROCEDURE
DATA INTERPRETATION
AND ANALYSIS
TEST PROCEDURE

Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 75
IV.
Annual MRI System Performance Evaluation
MEDICAL PHYSICIST’S/
MRI SCIENTIST’S SECTION
(d
1
- d
2
) = spatial distortion (mm) measured as the distance dierence
of corresponding points in the phantom in the frequency-encoding
direction for a specied DSV
FOV
x
= FOV in the frequency-encoding direction (mm)
In the above equation, the receiver bandwidth must be expressed in units
of Hz across the full FOV. However, it should be noted that vendors may
express the receiver bandwidth in dierent ways. For example, some
vendors display receiver bandwidth as half the frequency shi across
the full FOV, which requires doubling the displayed receiver bandwidth.
Bandwidth may also be expressed as either Hz/pixel or as the fat-water-
shi (FWS) expressed in units of pixels.
To convert pixel bandwidth (Hz/pixel) to receiver bandwidth (Hz), it is
necessary to multiply the Hz/pixel value for the image by the number of
pixels in the frequency-encoding direction. Note that the displayed image
matrix may dier from the acquisition matrix when image interpolation
is used. Most manufacturers quote pixel bandwidth in the acquired image,
but at least one manufacturer quotes pixel bandwidth in Hz per displayed
pixel when image interpolation is used.
For example, if the image bandwidth per pixel is 125 Hz/pixel, and the
image matrix is 256 x 256, the receiver bandwidth (BW) for the full FOV
in Hz is calculated with the following formula:
BW (Hz) = 125
Hz
pixel
× 256 pixels = 32,000 Hz
To convert FWS expressed in units of pixels to Hz, it is necessary to rst
determine the static eld strength of the system being evaluated and then
determine the nominal frequency dierence between fat and water (FD)
for that eld strength. FD is commonly assumed to be approximately
3.5 ppm. Assuming resonant frequencies of 63 MHz and 127 MHz for
1.5T and 3T systems, respectively, the applicable FD values are estimated
as follows:
at 1.5T: FD(Hz) = 3.5 ppm × 63
Hz
pixel
= 220 Hz
at 3.0T: FD(Hz) = 3.5 ppm × 127
Hz
pixel
= 440 Hz
e BW is then determined by multiplying the applicable FD (in Hz) by
the number of acquired image pixels in the frequency-encoding direction
and then dividing by fat-water shi (in pixels).
For example, if the stated fat-water shi is 1.75 pixels for an image with
a 256 × 256 matrix and eld strength of 1.5T, the BW (Hz) would be
determined as follows:
BW(Hz) =
220Hz × 256 pixels
1.75 pixels
= 32,183Hz

76 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
IV. Annual MRI System Performance Evaluation
e bandwidth-dierence method assesses eld homogeneity only
in the direction of the frequency-encoding axis. us, to assess eld
homogeneity over the desired DSV, it will be necessary for separate
images to be acquired with the frequency-encoding direction along all
three orthogonal axes.
1. Position the phantom in the center of the RF coil. e size of
the phantom should be appropriate for the DSV to be assessed.
A spherical phantom with identiable reference points is
recommended. A right cylinder also can be used, but ideally
the cylinder should have a length that is greater than twice
the diameter, otherwise the measurements may be subject to
susceptibility artifacts. Employ a simple, eld-echo (spoiled
GRE) pulse sequence. A spin-echo sequence may also be used
for this test to increase SNR but will require longer acquisition
times. It should be noted that using a larger acquisition matrix
will increase precision of the measurement by reducing the
pixel size and thereby reducing the uncertainty in the distance
measurements. Ideally a large matrix value in the frequency-
encoding direction should be used (e.g., 512).
2. Acquire three separate series, each series consisting of a single
image through the center of the phantom, with receiver bandwidth
BW
1
, one with the frequency-encoding oriented along each of the
three orthogonal axes. Acquire three more separate series, each
consisting of a single image, with receiver bandwidth BW
2
, one
with frequency-encoding along each of the three orthogonal axes
while maintaining the phantom position and all other acquisition
parameters besides BW the same as used in Step 1 above.
3. If a right cylinder is used, it will be necessary to acquire BW
1
and
BW
2
images in each orthogonal plane before repositioning the
phantom to assess all three planes.
1. Images acquired with two dierent bandwidths but at
corresponding slice locations throughout the DSV will be
compared. First, display an image acquired at BW
1
. Choose two
reference points in the image that extend the full length of the
desired DSV to be assessed, e.g., points A and B in Figure 1.
Magnify the image on the monitor by a factor of two to four.
2. Adjust the display window using a narrow window width,
keeping the reference points to be measured in the image clearly
visible. e display level should then be set to a level roughly one-
half that of the signal in the bright portions of the phantom.
3. Use the viewer’s length measurement tool to determine the
distance between the two points. Record the measured length
(mm) as “d
1
.”
DATA INTERPRETATION
AND ANALYSIS

Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 77
IV.
Annual MRI System Performance Evaluation
MEDICAL PHYSICIST’S/
MRI SCIENTIST’S SECTION
4. Repeat Steps 1–3 for the same reference points and corresponding
slice position acquired with bandwidth BW
2
. Record the measured
length (mm) as “d
2
.” It should be noted that it is important to
identify the same physical reference points in each of the two
images. Otherwise, an additional unknown uncertainty in the
measurement will be introduced.
5. Record the distance dierence (d
1
- d
2
) for that plane and slice
location.
6. Repeat this procedure (Steps 1–5) to obtain the distance dierence
for the other planes and slice locations throughout the volume.
7. Using the maximum distance dierence measured above,
determine the greatest value of ∆B
0
using the equation above for
each orientation. is value is the inhomogeneity (in ppm) for
the specied diameter.
Figure 1. Images illustrate the bandwidth-dierence option; (left) axial magnitude
image acquired with the system’s smallest receiver bandwidth value (BW
1
= 6 Hz/
pixel); (right) image acquired with system’s largest receiver bandwidth value (BW
2
=
160 Hz/pixel). The frequency-encoding direction is vertical in the image.. The
frequency matrix was 256 pixels, 25-cm FOV and B
0
eld strength of 0.3T, resulting in
a magnetic eld inhomogeneity of 1.16 ppm.
3. Phase Map Option
is test provides an accurate upper bound measurement of B
0
inhomogeneity using a uniformity phantom (Figure 2). However, the test
requires features of the MRI system (i.e., display of phase images), which
may not be available on all units. If the MRI system can display phase-
contrast images, a pixel-by-pixel measurement of eld inhomogeneity
can be obtained.
Phase-contrast images may display phase wrap in those regions
where the total phase angle exceeds ±180° from the reference phase.
Although unwrapping algorithms can be employed to eliminate this
complication, this feature typically must be performed oine on an
independent workstation.
TEST PROCEDURE

78 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
IV. Annual MRI System Performance Evaluation
1. Position a uniform phantom in the center of the magnet. e
size of the phantom should be appropriate for the diameter to
be assessed and, in general, the larger the better. A spherical
phantom is preferable, if available. Employ a eld-echo (a spoiled
GRE, either 2-D or 3-D) pulse sequence with the appropriate
TE (see below). Do not use a spin-echo sequence because it will
result in rephasing of the phase dierences caused by magnetic
eld inhomogeneities.
2. In theory, nearly any echo time can be used, but some echo times
simplify processing. A TE of 10 ms corresponds to 100 Hz per
phase cycle, and 20 ms corresponds to 50 Hz per phase cycle. e
longer the TE, the greater the sensitivity, but this also potentially
results in a greater number of phase wraps that must be dealt
with and a reduction in the SNR. Another approach is to choose
a TE that corresponds to an integer value of ppm inhomogeneity.
At 1.5T, the center frequency is approximately 64 MHz. One ppm
per phase cycle would be 64 Hz, which corresponds to a TE of
15.6 ms.
3. Acquire a set of GRE images. A 3-D set acquired on a spherical
phantom is best, since it permits evaluation of the complete
volume from a single scan. If a 3-D scan is not possible, or if a
nonspherical phantom is being used, then multiple slices should
be obtained in each of the three orthogonal plane directions.
When using a 3-D GRE (or spoiled gradient-recalled [SPGR]) sequence,
typical scan parameters would be a TR of 40–50 ms, TE of 10–20 ms,
ip angle of 30–40°, and a 128 x 128 x 64 matrix. e FOV should be
10–25% larger than the diameter of the phantom, and the excited slab
should be roughly the same size as the FOV, allowing for easy multiplanar
reformatting.
When using a 2-D GRE (or SPGR), typical scan parameters would be a
TR of at least 200 ms and long enough to acquire all of the desired slices
in one TR period. e TE could be 10–30+ ms, as appropriate. Matrix size
is not critical; 128 × 128 or 128 × 64 is reasonable. Use a slice thickness of
5 mm (high eld) to 10 mm (low eld). e number of slices depends on
the size and shape of the phantom.
Data analysis involves assessing the maximum phase shi over the entire
phantom. As illustrated below, the maximum phase shi could occur
between any two points in the phantom (e.g., center-to-edge, edge-to-
edge, and not necessarily through the center of the image).
Each vendor has its own way of displaying and scaling phase images.
Some will display the pixel value as the phase in radians times 1000.
Others will scale from -2048 to +2048, or -5000 to +5000, or 0 to 4096;
there is no standard. e rst task of the physicist using this technique is
to determine how the images are scaled. Unfortunately, it is not always
easy to do. Figure 2a shows a phase map obtained from a 3T scanner
using a 32-cm diameter water-lled spherical phantom containing NiCl.
e gure shows the phase map of the center slice of a 3-D volume. ere
DATA INTERPRETATION
AND ANALYSIS

Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 79
IV.
Annual MRI System Performance Evaluation
MEDICAL PHYSICIST’S/
MRI SCIENTIST’S SECTION
is an obvious phase wrap at the point labeled B and all along that circular
border. By moving an ROI around that border it is possible to determine
the largest and smallest pixel values and assign those as ±π or ±180°.
In theory, this is reasonably straightforward. However, some vendors
will calculate the phase images and then apply lters that can round o
transitions or enhance edges, but this method should provide acceptable
results. See the phase-dierence method section for an alternative
method, IV.A.4.
Figure 2. Image data for axial phase map option obtained on a 3T scanner. CF = 127.7
MHz, TE 10 ms. a) Phase image. b) Phase prole along diagonal through the image. c)
Calculation of total phase change from point A to point C of 1.14 ppm.
e graph in Figure 2b depicts a prole of the phase values along the
diagonal line of Figure 2a. For clarity, values have been scaled to represent
the phase in degrees. is diagonal was chosen because from visual
inspection it appeared to encompass the largest changes in phase across
the image. e total phase change from point A to point C is calculated
as the sum of the phase change from A to B plus the change from B to C,
where the phase at point B can be ±180 as appropriate. In this case the total
phase change was 527°. Dividing this by 360° yields a total phase change
of 1.46 cycles. Since a TE of 10 ms was used, one cycle corresponds to 100
Hz; therefore, the total frequency change is 146 Hz. Finally, dividing this
by the center frequency of 127.7 MHz (for this 3T scanner) yields a peak-
to-peak magnetic eld inhomogeneity of 1.14 ppm.
e calculation above represents the inhomogeneity of the magnet in
that one axial slice. To properly evaluate magnet inhomogeneity, phase
maps in multiple slices in axial, sagittal, and coronal planes need to be
evaluated. Figure 3 shows a similar dataset and calculations in the coronal
plane, where the inhomogeneity is determined to be 0.98 ppm. An even
smaller inhomogeneity was found in the sagittal plane (not shown).
Comparing the results from all three planes, we report that the magnet
inhomogeneity does not exceed 1.14 ppm. In fact, the homogeneity of
this magnet is better than that, as shown below by the phase-dierence
method on the same scanner.

80 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
IV. Annual MRI System Performance Evaluation
Figure 3. Image data for coronal phase map option obtained on a 3T scanner. Center
frequency = 127.7 MHz, TE 10 ms. a) Phase image. b) Phase prole along horizontal
line through the image. c) Calculation of total phase change from point A to point C.
4. Phase-Dierence Map Option
e test procedure for the phase-dierence map option is identical to
the phase map option discussed above with the addition of a second set
of phase images obtained using a slightly longer TE, from 2.5 to 10 ms
longer. Greater TE dierences yield greater sensitivity, but with the need
to deal with a larger number of phase wraps.
Figure 4a is the phase map at TE=15 ms. Figure 4b is the corresponding
phase map with TE=10 ms, the same phase map shown in Figure 2a.
Figure 4d depicts the phase proles through both images. Note that the
total phase change of the TE=15 ms image corresponds to 0.89 ppm,
whereas the phase change of the TE=10 ms image is 1.14 ppm. Remember
that the total phase change is the net result of magnet inhomogeneity and
contributions from “other” sources, such as o-centering of the sample
window (fractional echo), nonuniform RF penetration, and magnetic
susceptibility dierences. Although these other sources do not change
with TE, the portion of the phase change caused by magnet inhomogeneity
increases with increasing TE. e phase-dierence method is more
accurate than the single phase map method because it removes the eects
of these other sources of inhomogeneity.
TEST PROCEDURE
DATA INTERPRETATION
AND ANALYSIS

Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 81
IV.
Annual MRI System Performance Evaluation
MEDICAL PHYSICIST’S/
MRI SCIENTIST’S SECTION
Figure 4. Image data for axial phase-dierence option obtained on the same 3T
scanner as Figure 2. Center frequency = 127.7 MHz. a) Phase image for TE = 15 ms.
b) Phase image for TE = 10 ms. c) Phase-dierence image. d) Phase prole along
diagonal through the images: image 4a (green) and image 4b (red). e) Phase prole
along the diagonal (blue) of the phase-dierence image and the calculation of the
total phase change from point C to point D within the phase-dierence image.
Figure 4c displays the result of subtracting the TE 10 ms phase image from
the TE 15 ms phase image. Note that the dark ring in the phase-dierence
(subtraction) image (Figure 4c) resulted because the phase wrap did not
occur at exactly the same location in the two images. In some cases, these
misalignments could complicate the nal analysis, but not in this case.
Figure 4e shows the diagonal prole through the dierence image. e
large discontinuities can be completely ignored and, in this case, have
no eect on the calculations. From the prole, we see that the net phase
change from point C to point A is 64°, whereas the change from C to D is
80°. e net dierence in the two echo times is 5 ms, which corresponds
to 200 Hz per phase cycle. e phase dierence of 80° divided by 360° per
cycle is multiplied by 200 Hz, yielding a 44 Hz peak-to-peak variation.
Dividing this by 127.7 MHz results in a magnetic eld inhomogeneity
of 0.34 ppm. is is a much smaller (and more accurate) value than is
calculated using either single phase image alone.
As stated in the phase map option above, it is necessary to examine the
phase shis in multiple planes. Figure 5a shows the phase-dierence
image (TE 15 ms - TE 10 ms) in the coronal plane. Note that the regions
of phase wrap misalignment show up as two irregular bands running top-
to-bottom in the image (head-to-foot in the scanner [H/F]). ese are
cross sections of the ring seen in the axial phase-dierence images. In
the phase map option above, we noted that the largest phase change went
from le to right. In this phase-dierence image and the corresponding
prole (red) in Figure 5d, we see that the largest phase change is in the H/F
direction. e calculations in Figure 5e show that the change from A to C
corresponds to 0.63 ppm, whereas the change from C to E corresponds to

82 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
IV. Annual MRI System Performance Evaluation
0.55 ppm. Combining these results with those obtained from the phase-
dierence image in the axial plane, we would report that the magnetic
eld inhomogeneity does not exceed 0.63 ppm.
Figure 5. Image data for phase-dierence option obtained on a 3T scanner in the
coronal plane. a) Dierence image obtained by simply subtracting the two coronal
phase maps (TE 15 ms - TE 10 ms). b) Dierence image obtained by multiplying the
complex (real and imaginary) version of the TE 15 image by the complex conjugate
of the TE 10 images. c) Contour plots of image 5b after phase unwrapping. d) Proles
through image 5a (red) and image 5b (blue). e) Calculation of the total phase change
from location A to location C and from location C to location E.
Note that the phase discontinuity at point D in Figure 5a does not equal
360° but equals 347°. When simply subtracting two phase images, the bands
at discontinuities can take on virtually any phase value depending on the
rate of change near the discontinuities in each original image. is makes
it very important to closely examine the actual values on both sides of the
discontinuity. Another method of calculating phase-dierence images
that is immune to these variations caused by the misalignment of phase
wrap is provided below. Although MR images are normally displayed as
magnitude images or sometimes phase images, the underlying data are
actually complex, with real and imaginary components. e relationship
between the magnitude and phase representation and the real and
imaginary parts is presented in equations below:
S
(complex)
= Ae
iθ
= S
(real)
+ i × S
(imaginary)
S
(real)
= A × cos (θ)
S
(imaginary)
= A × sin (θ)

Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 83
IV.
Annual MRI System Performance Evaluation
MEDICAL PHYSICIST’S/
MRI SCIENTIST’S SECTION
Where the complex pixel signal value S is represented in terms of its
magnitude (A) and phase (θ) or as its real and imaginary components;
i = the square root of -1. Assume we have two images, X
1
and X
2
, with
magnitudes and phases of A
1
, θ
1
and A
2
, θ
2
. For the phase-dierence
method we want the dierence θ
1
– θ
2
of each pixel in the image. is
phase dierence can be obtained by multiplying the complex version of
image 2 by the complex conjugate of image 1 as described below:
X
delta
= X
2
× conj(X
1
) = A
2
× e
i×θ
2
× A
1
× e
-i×θ
1
= A
2
× A
1
× e
i(θ
2
- θ
1
)
or
X
delta
= X
2
× conj(X
1
) = (R
2
+ i × I
2
) * (R
1
- i × I
1
) =
R
2
× R
1
+ I
2
× I
1
+ i × (I
2
× R
1
- R
2
× I
1
)
X
imaginary
= I
2
× R
1
- R
2
× I
1
X
real
= R
2
× R
1
+ I
2
× I
1
θ
2
- θ
1
= atan(X
imaginary
/X
real
)
Where “R” stands for real component, and “I” stands for imaginary
component. is image processing method is not available on any MRI
scanner but can be done if complex image data can be processed on an
independent workstation. is complex conjugate method was used to
generate the image in Figure 5b. e misalignment bands are eliminated,
and what remains are normal 360° phase wraps at the superior and
inferior edges of the phantom. As long as oine processing is being done,
from this image it is possible to unwrap the image and plot contours of
the phase map, as shown in Figure 5c. e red regions represent a positive
change in the frequency (and eld), and the blue regions represent a
negative change.
It was stated earlier in the phase map option section that some vendors
perform image processing that can adversely aect the determination of
the phase scaling. is problem is avoided when using real and imaginary
images since these images have no discontinuities, so their values
always change smoothly. By using the real and imaginary images, it is
straightforward to calculate true phase images with discontinuities that
are exactly 360°.
e nal value of 0.63 ppm as the inhomogeneity of the 3T image is
substantially dierent than that of 1.14 ppm found by using the phase map
option. A large part of this error can be avoided if an oil-lled phantom
is used, since oil does not suer from the same RF penetration problems
as water. Figure 6 below shows phase-dierence image calculations using
identical scan parameters, but with a 32-cm oil-lled phantom.

84 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
IV. Annual MRI System Performance Evaluation
Figure 6. Image data for axial phase-dierence option obtained on the same 3T
scanner with an oil-lled phantom. a) Phase image TE = 15 ms. b) Phase image TE
= 10 ms. c) Phase-dierence image. d) Phase proles along diagonals through the
images. e) Phase prole of dierence image and calculation of total phase change
from point C to point D.
Note that the two individual phase images result in estimates of
inhomogeneity of 0.45 ppm and 0.40 ppm as opposed to estimates of 1.14
ppm and 0.89 ppm obtained with the water-lled phantom. By eliminating
the phase changes caused by RF penetration dierences, accuracy of the
phase map option has been signicantly improved.
Some MRI vendors actually provide dual-echo imaging sequences that
provide a magnitude image and a phase-dierence image (or images).
is greatly simplies the analysis process. Figure 7 below shows an
example at 0.6T where the dual-echo image used TEs of 11.2 and 19.1 ms.
e dierence of 7.9 ms represents a frequency of 126.6 Hz; at 0.6T (25.5
MHz) this corresponds to 5 ppm per phase cycle.

Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 85
IV.
Annual MRI System Performance Evaluation
MEDICAL PHYSICIST’S/
MRI SCIENTIST’S SECTION
Figure 7. Image data for an axial phase-dierence option obtained on a 0.6T upright
scanner with a water-lled phantom. a) Phase-dierence image provided by scanner
software. b) Color contour plots obtained after oine phase unwrapping. c) Phase
prole from point A to E; d) Phase prole from point F to E.
In previous examples we looked at proles that went across the phantom
diagonally (Figures 2, 4, 6), horizontally (Figure 3), and vertically (Figure
5). Sometimes the path between the two points with the greatest phase
dierence is completely dierent. In Figure 7a the horizontal (blue) path
from A to E resulted in an estimate of 12.86 ppm. e shorter path (red)
at an angle between points F and E resulted in an estimate of 16.0 ppm.
Calculating both of these values required paying close attention to the
phase wraps. Although it is possible to estimate the magnet homogeneity
by simply counting the number of phase wraps in an image, it is best to
actually plot proles of various chords across the phantom.
It has been stated above that it is necessary to make homogeneity
measurements in all three planes. Obtaining only one image (or pair of
images) through the isocenter in each of the three planes, however, is not
adequate. Multiple slices in each plane (or 3-D volume data) are required
to ensure that small localized problems are not missed. Figure 8 shows a
series of phase map images in all three planes. e three images through
isocenter are outlined by red boxes. ese three images look completely
normal. On the le side, indicated by the arrows, is a well-dened region
of high magnetic eld inhomogeneity. is type of phase map arises when
metal is present in the bore of the scanner.
e site from which this 3-D phase map was acquired had reported
consistent problems with the fat saturation of right shoulder and le hip
images. Service engineers found nothing in the magnet bore and reported
FINAL COMMENT ON
PHASE MAPS AND
PHASE DIFFERENCE
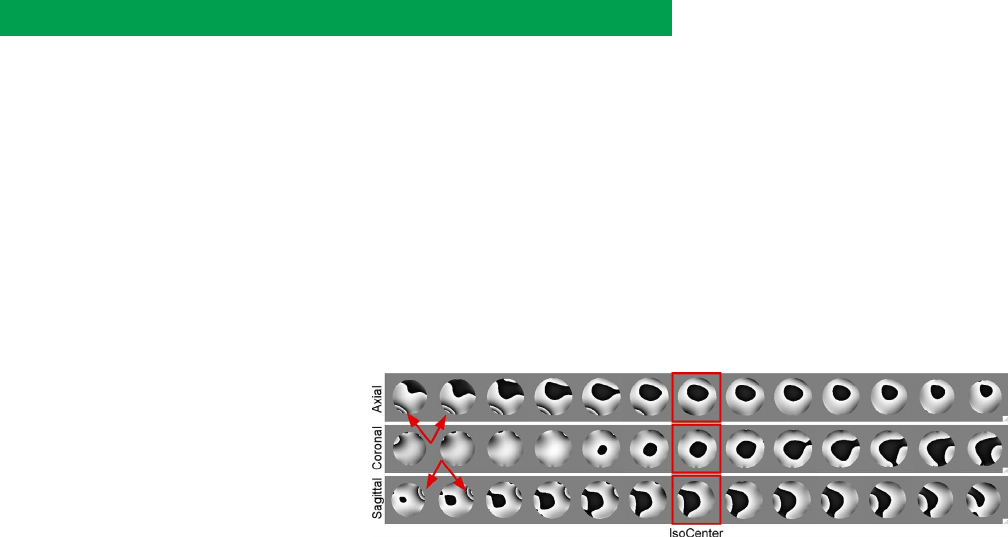
86 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
IV. Annual MRI System Performance Evaluation
that the magnet met magnetic eld homogeneity specications. Prior
to submitting for re-accreditation, the medical physicist/MRI scientist
performed an annual performance evaluation, obtained these images,
and failed the unit for excessive magnet inhomogeneity. In addressing the
physicist report, service engineers removed the cover from the magnet
bore and found a bobby pin underneath the covering in a location
corresponding to the region of high magnetic eld inhomogeneity. is
problem would not have been identied and corrected if only the spectral
peak method had been used or if phase maps had been obtained in each
of three orthogonal planes only through isocenter.
Figure 8. A series of multiplanar reformatted phase images from a 3-D GRE scan. The
slices through isocenter (red boxes) appear completely normal. The images on the far
left, indicated by the red arrows, show a well-dened region of eld inhomogeneity
that was caused by a bobby pin under the magnet bore cover.
Magnetic eld homogeneity data should be reported in the annual system
performance evaluation report. e homogeneity is specied by the MRI
system manufacturer. e values obtained should be compared to those
specied for the DSV equal to the phantom diameter.
Magnetic eld homogeneity requirements become more stringent for
systems used for ultrafast imaging, fat suppression, and/or spectroscopy.
Poor magnetic eld homogeneity can be due to ferromagnetic objects
contaminating the eld within the bore (or gap) of the magnet. Changes
in the location or arrangement of large ferromagnetic objects in the
exterior environment of the magnet can also cause magnetic eld
inhomogeneities.
Oen magnetic eld homogeneity problems can be corrected through
adjustment of the gradient osets. If the homogeneity is very poor,
the service engineer can measure it using a special jig that measures
resonant frequency in a small sample at various locations within the
magnet. ese measurements can be compared to those made at the
time of installation. In some extreme cases, superconducting shim
currents will have
to be adjusted.
SUGGESTED
PERFORMANCE
CRITERIA AND
CORRECTIVE ACTION

Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 87
IV.
Annual MRI System Performance Evaluation
MEDICAL PHYSICIST’S/
MRI SCIENTIST’S SECTION
B. Slice-Position Accuracy
e ACR slice-position accuracy test checks the accuracy with which
axial slices are positioned at specic locations utilizing a sagittal localizer
image. is test determines whether the actual locations of acquired
slices dier from their prescribed locations by substantially more than is
normal for a well-functioning scanner.
Dierences between the prescribed and actual positions of slices 1 and
11 for the large phantom and slice 1 for the small phantom for the ACR
T1 and T2 series are measured. ese measurements are typically made
using the ACR T1-weighted axial scanning series (MRI Technologist’s
Section IV.B and IV.C).
For the large phantom, slices 1 and 11 are originally positioned so that
they are aligned with the vertices of the crossed 45° wedges at the inferior
and superior ends of the phantom, respectively. e two crossed wedges
in slices 1 and 11 appear as parallel dark, vertical bars at the top (anterior
side) of the phantom. For both slice 1 and slice 11 the wedges will appear
as dark bars of equal length on the image if the slice is exactly aligned
with the vertex of the crossed wedges. If the slice is located superior to the
vertex, the right bar on the image (anatomical le) will be longer. If the
slice is displaced inferior to the vertex, the le bar will be longer.
For the small phantom, slice 1 in each ACR series is prescribed to align
with the center of the crossed 45˚ at the starting end of the phantom. e
crossed wedges appear as a pair of adjacent, dark, vertical bars at the top
(anterior side) of the phantom. If slice 1 is exactly aligned with the center
of the crossed wedges, then the wedges will appear as dark bars of equal
length on the image. If the slice is displayed superiorly with respect to the
center, the bar on the observer’s right (anatomical le) will be longer. If
the slice is displayed inferiorly with respect to the center, the bar on the
le will be longer.
Measurements are made for slices 1 and 11 of the ACR T1-weighted axial
series for the large phantom and for slice 1 of the ACR T1 and T2 series
for the small phantom.
Use the following procedure for each image:
1. Display the slice magnied on the monitor by a factor of two
to four. Keep the vertical bars of the crossed wedges within the
displayed portion of the magnied image.
2. Adjust the display window so that the ends of the vertical bars are
not fuzzy using a narrow window width. e display level should
be set to a level roughly one-half that of the signal in the bright
portions of the phantom.
3. Use the viewer’s length measurement tool to determine the
dierence in length between the le and right bars. If the le bar
is longer, then assign a minus sign to the length. For example, if
the bar-length dierence is 5.0 mm and the le bar is longer, then
record the measurement as -5.0 mm.
OBJECTIVE
TEST PROCEDURE

88 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
IV. Annual MRI System Performance Evaluation
4. Record the measured data in the annual system performance
evaluation report.
e action criteria are specied in terms of limits on the bar-length
dierence measurements, based on a series of baseline data compiled by
the qualied medical physicist/MRI scientist.
Since the crossed wedges have 45° slopes, the bar-length dierence is twice
the actual slice displacement error. For example, a bar-length dierence
of 5.0 mm implies the slice is displaced inferiorly by 2.5 mm from the
vertex of the crossed wedges.
e magnitude of each bar-length dierence should be less than or equal
to 5 mm. Note that a bar-length dierence of more than 4 mm for slice
11 for the large phantom will adversely aect the low-contrast object
detectability measurement. A bar-length dierence of more than 4 mm
for slice 1 for the small phantom may adversely aect the slice-thickness
measurements and the low-contrast object detectability.
e most common cause of failure likely is an error by the scanner
operator in the prescription of the slice locations. is type of error is
ruled out by examining the axial images, which are cross-referenced on
the localizer; slices 1 and 11 should be aligned with the crossed wedge
vertices on the localizer image. Slices should be prescribed as carefully as
possible because these errors in combination with other sources of error
can push an acceptable level of performance to an unacceptable level.
Many scanners automatically move the patient table position in the
inferior-superior direction to place the center of a prescribed imaging
volume at gradient isocenter. Aer the localizer is obtained, the table
position is adjusted so that an error in the table positioning mechanism
can lead to a slice-positioning error. If the bar-length dierence for slice 1
and slice 11 is the same in sign and similar in magnitude, this type of table
positioning error may be the cause.
Sometimes an unfortunate combination of two or three of the problems
(inaccurate slice prescription, error in the table-positioning mechanism
and poor gradient calibration or B
0
homogeneity) can lead to a failure
when no single problem would be suciently bad to cause a failure on
its own. erefore, if no one thing seems to be responsible for causing a
failure of this test, try having the service engineer shim B
0
, recalibrate the
gradients, and check the table positioning mechanism for excessive play.
en acquire a new image dataset aer prescribing the slices as carefully
as possible.
C. Slice-Thickness Accuracy
e slice-thickness test is used to determine the accuracy of a specied
slice thickness. e prescribed slice thickness is compared with the
measured slice thickness. Poor slice-thickness accuracy may not only
suggest that the slices are too thick or thin, but also can adversely aect
image contrast and SNR.
For this test, the lengths of two signal ramps in slice 1 of the ACR MRI
DATA INTERPRETATION
AND ANALYSIS
SUGGESTED
PERFORMANCE CRITERIA
AND CORRECTIVE ACTION
OBJECTIVE
TEST PROCEDURE

Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 89
IV.
Annual MRI System Performance Evaluation
MEDICAL PHYSICIST’S/
MRI SCIENTIST’S SECTION
accreditation phantom are measured for 5-mm thick slices for each of the
ACR imaging series.
e slice-thickness measurement performed with the ACR MRI phantoms
is similar to one of the methods described by NEMA (NEMA MS-5,
2009). Two thin, oppositely inclined ramps appear in a structure called
the slice-thickness insert. If the center of slice 1 is properly positioned
at the vertex of the crossed wedges, as shown in Figure 3 of the MRI
Technologist’s Section, and the phantom is not tilted, the two bright thick
lines representing the ramps will appear one above the other. e two
ramps are crossed: one has a negative slope and the other a positive slope
with respect to the plane of slice 1. e ramps are produced by cutting
1-mm wide slots in a block of plastic. e slots are open to the interior of
the phantom and are lled with the same solution that lls the bulk of the
phantom. e signal ramps have a slope of 10 to 1 with respect to the plane
of slice 1; i.e., they make an angle of about 5.71° with slice 1. erefore,
the signal ramps will appear in the image of slice 1 with a length that
is 10 times the thickness of the slice (as shown in Figure 6b of the MRI
Technologist’s Section for the small phantom). If the phantom is tilted in
the right-le direction, one ramp will appear longer than the other. Error
introduced by right-le tilt is corrected by averaging the measurements
from the two crossed ramps using the slice-thickness formula provided
in the next section.
For each ACR imaging series, length of the signal ramps in slice 1 is
measured according to the following procedure:
1. Display slice 1 magnied by a factor of two to four while keeping
the slice-thickness insert fully visible on the screen.
2. Adjust the display level so that the signal ramps are well visualized.
e ramp signal is much lower than that of the surrounding
water, so usually it will be necessary to lower the display level
substantially and narrow the window width.
3. Place a rectangular ROI at the middle of each ramp. Note the
mean signal values for each of the two ROI’s, then average the
values. is result is a number approximating the mean signal
at the middle of the ramps. Record this number as the RAMP
SIGNAL LEVEL. An elliptical ROI may be used if a rectangular
one is unavailable.
4. Be careful that the ROI’s cover the full widths of the ramps in the
top-bottom direction, but do not allow any portion of the ROI’s
to be located outside of the ramps. If there is a more than 20%
dierence between the signal values obtained for the two ROI’s it
is oen due to one or both of the ROI’s including regions outside
the ramps.
5. Lower the display level to one-half of the of the average ramp
signal calculated in step 3. Set the display window width to
its minimum.
DATA INTERPRETATION
AND ANALYSIS

90 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
IV. Annual MRI System Performance Evaluation
6. Use the on-screen length measurement tool of the display station
to measure the lengths of the top and bottom ramps. Record these
lengths. ey are the only measurements required for this test.
Record the values measured in the annual system performance
evaluation report.
Oen the ramps seem to be composed of stripes and the ends appear
scalloped or ragged. is striping pattern is due to truncation artifact and
is normal. One must estimate the average locations of the ends of the
ramps to measure the ramp lengths. A degree of inaccuracy arises from
estimating the ends of the ramps but a millimeter of error in the ramp
length measurement corresponds to only a tenth of a millimeter error in
the slice thickness and this turns out to be a small eect.
e slice thickness is calculated using the following formula:
Slice ickness = 0.2 ×
top+bottom
top × bottom
where “top” and “bottom” are the measured lengths of the top and bottom
signal ramps. For example, if the top signal ramp were 59.5 mm long and
the bottom ramp were 47.2 mm long, then the calculated slice thickness
would be
Slice thickness = 0.2 × (59.5 × 47.2) / (59.5 + 47.2) = 5.26 mm
Record the value calculated in the annual system performance evaluation
report. For the prescribed slice thickness of 5 mm, the ACR performance
criterion is that the measured slice thickness should be 5.0 mm ± 0.7 mm.
RF amplier nonlinearity can cause distorted RF pulse shapes and failure
of this test. On many scanners, the service engineer must empirically
calibrate the RF power amplier for linearity.
Malfunctions anywhere in the high-power RF portion of the scanner (RF
power amplier, coaxial cables, RF switch, or in the transmitter coil itself)
can produce distorted RF pulse shapes. Poor gradient calibration or poor
gradient switching performance also can cause failure of this test.
All of these possible causes for failure require corrective action by the
service engineer.
D. Radiofrequency Coil Checks
e design of RF MRI coils always represents a trade-o between
maximizing image uniformity and enhancing SNR. Coils that have been
designed to image body parts placed within their volumes (head coils,
body coils, and some neck and knee coils) will produce very uniform
excitation and reception of the MR signal.
Many procedures are now typically performed using surface coils that
improve SNR by combining, to various degrees, the following three
strategies: (1) placing the coil close to the volume of interest, (2) excluding
signal and noise from regions not under investigation and (3) maximizing
SUGGESTED
PERFORMANCE CRITERIA
AND CORRECTIVE ACTION
OBJECTIVE

Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 91
IV.
Annual MRI System Performance Evaluation
MEDICAL PHYSICIST’S/
MRI SCIENTIST’S SECTION
the sensitive region of the coil over the volume of interest. Typically, these
probes yield very non-uniform images. If the radiologist is aware of these
coils’ characteristics, however, this perception can be accommodated at
interpretation. RF coils, called phased-array coils, have been employed to
improve image uniformity from closely coupled RF coils.
At the present time, the following procedures for measuring SNR do not
apply to parallel imaging (pMRI) with acceleration factors. Until standard
methods for measuring SNR become available, it is recommended that all
images be acquired without pMRI acceleration.
e qualied medical physicist/MR scientist may use the QA procedures
and tools supplied by the vendor to test the coils.
Signal-to-Noise Ratio
SNR is a fundamental but very general parameter associated with MRI
system performance. e measurement of signal and noise in Fourier
MR imaging is a complex subject. Henkelman [22] described how signal
intensity measurements are determined in the setting of low SNRs for
magnitude reconstructed MR images obtained using linear RF coils.
Gudbjartsson and Patz [23] developed a theoretical analysis of the noise
statistical properties (Rayleigh distribution) in magnitude and phase
Fourier MR images. Constantinides et al [24] provided similar noise
distribution functions and correction factors for determining SNR for
phased-array RF coils.
e single-acquisition method used in this manual was proposed by
Kaufman et al [25]. However, care must be taken to ensure that the ROI
in which the “noise standard deviation” is measured is free of artifacts. In
addition, measurements in regions of nonuniformities due to bandwidth-
limiting ltering, truncation of the background signal data, and RF
ltering of the signal data at the edges of the frequency-encoding range
should be avoided.
An alternative method of SNR measurement, used by some MRI system
manufacturers (NEMA MS1-2008, Method 1), acquires two consecutive
scans with identical scan parameters. Sijbers et al [26] have compared
the single image acquisition method recommended in this manual with
NEMA Method 1 and determined that NEMA Method 1 yields acceptable
SNR measurements except in the presence of erratic ghosting or uid
motion. Data directly correlating the two methods, obtained by Firbank
et al [27], suggest that the single acquisition method is appropriate in
a QA program “since it is quicker and easier to perform and is a good
indicator of the more exact procedure.”
Whichever method is used to measure SNR, the single most important
concept is reproducibility. Tests must be performed the same way each
time, and analysis must be done the same way each time. To detect small
changes in SNR due to actual equipment failure one needs to ensure that
variations due to methodology are kept to a minimum. Because the noise
term is both small and in the denominator of the SNR, test design choices
that improve the accuracy of the noise measurement are more important
GENERAL THEORY

92 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
IV. Annual MRI System Performance Evaluation
than those that improve the mean signal measurement.
Note that the SNR data recorded in the annual system performance
evaluation report using the methods described below are estimates
and not rigorous measurements of the true SNR. However, for most
systems, this is a reproducible index that is quite adequate for routine
QC. For some low-eld systems where the background intensity may
be signicant relative to the signal, it may be necessary to correct the
signal by subtracting the background from the signal before calculating
the SNR.
Transmitter Gain Measurements
Transmitter gain (or attenuation) is automatically determined by the MRI
system during the prescan calibration routine. is value should be noted
in the annual system performance evaluation report so that it may be
compared when data are obtained at a later date.
Image Intensity Uniformity
e image intensity uniformity test measures the percent image
uniformity (PIU) of the image intensity over a large uniform region of
the phantom lying near the middle of the imaged volume and thus near
the middle of the sensitive region of the volume RF coil.
Head coils, body coils, and some extremity coils are designed for clinical
use to have a fairly uniform spatial sensitivity near the middle of the coil
when loaded as typical for human body parts. Poor signal uniformity
indicates that the coil has signicantly greater variation in image intensity
than is normal for a properly functioning system. Lack of image intensity
uniformity suggests a deciency in the scanner, oen a defective volume
coil or problem with the radiofrequency subsystems.
RF Phase Stability
e RF pulses used in MRI are generated using a stable radiofrequency
source (radiofrequency synthesizer), which usually works in the coherent
(phase locked) mode to assure stability of the generated signal. Multi-
slice imaging sequences require rapid switching of the radiofrequency
oset. Commonly, the coherence of the synthesized signal can be restored
within several microseconds aer switching. is feature, combined
with high stability of the generated frequency (commonly 10–8 ppm or
better) is more than sucient for most standard MRI applications. e
radiofrequency signal is then modulated (most oen in amplitude, but
frequency and/or phase modulations can be found as well) to generate
the appropriate pulses. Radiofrequency output, which is “decient” in
quality, can result in a variety of imaging artifacts depending on the
magnitude and type of the defect.
Phase related errors are dened in terms of inappropriate (either increased
or decreased) image signal at specied spatial locations. Generally, these
artifacts are characterized by increased signal intensity in areas known to

Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 93
IV.
Annual MRI System Performance Evaluation
MEDICAL PHYSICIST’S/
MRI SCIENTIST’S SECTION
contain no signal producing material. Errors in the application of phase-
encoding gradients for imaging and errors in both RF transmit and
receive quadrature phases result in unique ghost artifacts.
Phase-encoding ghosts will appear as multiple images (possibly smeared
into a column) originating at the true object position but displaced along
the phase-encoding axis of the image (perpendicular to the frequency-
encoding direction). e presence of these characteristic ghost images
will generally identify the two axes; however, the specic orientations
should not aect the outcome of the measurement described below.
Surface Coils and Volume Coils
In the following section, strategies that can be used to test all radiofrequency
coils used clinically on a particular MRI system are described. e tests
are described in two subsections: one for volume coils and the other for
surface coils. ey dier in the following essential approaches.
For volume coils, three measurements are performed: image uniformity,
SNR, and percent signal ghosting. Together, these three parameters can
be used to characterize a coil’s performance and track changes in RF coil
performance. e determination of image uniformity, SNR, and percent
signal ghosting may be obtained from a single image. In volume coils,
this image should be acquired at the center of the coil and oriented
perpendicular to the axis of the coil.
For surface coils, it was previously recommended that the maximum
SNR be measured because of the characteristic non-uniform sensitivity
patterns of these coils [6,28]. ough appropriate, considerable variations
in the maximum SNR will result if the phantom-to-coil positioning and
ROI placement for both signal and noise are not carefully recorded and
reproduced. Experience has shown that the mean SNR derived using large
ROIs for both signal and noise may be more easily reproduced and thus
be a more stable indicator of surface coil performance than maximum
SNR. For this reason, the revised manual includes both maximum SNR
and mean SNR as acceptable alternative performance parameters for
surface coils. In either case, images acquired with appropriate uniform
phantoms must be visually checked to ensure that there is not excessive
ghosting and that there are not uncharacteristic asymmetries in surface
coil performance. With surface coils, the appropriate position and
orientation must be determined based on the available phantom and
the type of clinical studies performed with the specic RF coil. e
determination of image orientations and positions is the rst task of
the qualied medical physicist/MRI scientist in the RF coil evaluation
process. A thorough description of each coil setup, the phantom used, and
scan parameters employed should be included in the annual performance
report. A photograph of the coil and phantom setup is helpful in ensuring
consistency from year to year.
For the purpose of this test, exible coils are considered to be surface
coils. For multi-channel coils, it is recommended to test individual
channel elements separately.

94 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
IV. Annual MRI System Performance Evaluation
Breast coils require testing to ensure that all coil elements function
properly, that signals are reasonably uniform within each breast, and that
signals are comparable between le and right breasts. Bilateral breast
coils can be tested using two identically-shaped phantoms containing the
same weak paramagnetic solution, each of which lls a large fraction of
the sensitive volume of each breast coil as shown in Figure 9.
Figure 9. Examples of a pair of identically-shaped and identically-lled cylindrical
phantoms imaged coronally in bilateral breast coils. a) Image showing ROIs that
indicate similar mean signal values in both coils. b) Example of a 4-channel bilateral
breast coil demonstrating signicantly lower signal in the medial portion of the
right breast coil, due to failure of a single channel of the 4-channel coil. Mean SNR in
the right breast coil measured approximately half of that in the left breast coil, with
signicant non-uniformity within the right coil. c) Identical acquisition to b., when
all 4-channels were functioning properly, but with some non-uniformity in the right
breast coil.
Phantom Characteristics
e phantom should be selected that best simulates the geometry of the
body part under investigation.
When imaging a small phantom in body coils, a large volume of conductive
solution inside a plastic annulus may have to be placed in the magnet to
ensure proper operation. is “body coil loader” simulates the electrical
PHANTOMS

Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 95
IV.
Annual MRI System Performance Evaluation
MEDICAL PHYSICIST’S/
MRI SCIENTIST’S SECTION
properties of a human body.
For imaging body parts with surface coils, the selection of phantom
geometry may be more dicult. Oen, MRI equipment manufacturers
provide appropriate phantoms with surface coils for purposes
of calibration.
e substance in the phantom should have a T1 value within the range
of those found in so tissues at the scanner’s eld strength. e phantom
should also be designed so that loading of the RF coil is similar to that
produced when the coil is in clinical use. e phantom should produce
a uniform signal in the region from which uniformity and SNR images
are obtained.
e ACR MRI accreditation phantom should be adequate for evaluating
head coils, if the images are acquired in an axial orientation. e ACR
phantom should be positioned so that the uniformity section, near the
center of the phantom, is in the center of the coil. Other phantoms will be
necessary for imaging with other volume coils. Breast coils can be tested
using an identical pair of 2-liter bottles, one inserted in each side, lled
with the same weak paramagnetic solution (e.g., 10 millimolar NiCl
2
or
CuSO
4
with 0.45% NaCl).
Scan Parameters
A T1-weighted scanning series is recommended since these typically do
not require a long scan times. e T1-weighted series used for the ACR
MRI Accreditation Program (a single spin-echo series, TR = 500 ms, TE
= 20 ms) is a good choice since it can be performed readily on almost
any scanner.
If the qualied medical physicist/MRI scientist is willing to spend some
time customizing the test procedure to the individual scanner, scan
times can be reduced. For instance, reducing TR may reduce scan times.
Whatever modications are performed, SNR should be maintained at a
value of 20 or greater for the region under investigation. e optimized
pulse timing and ip angle parameters should be recorded in the QC
procedures manual and used in subsequent measurements.
e FOV shall be chosen appropriately for the RF coil under investigation.
e FOV shall be selected so that regions outside the phantom are
displayed on the image for background noise measurements. To minimize
potential problems with ghosting wrapping around into the phantom, it
is preferable, where possible, to choose a FOV that is at least twice the
size of the phantom in the phase-encoding direction. When that is not
possible, select the largest FOV the magnet supports. e selected FOV
should be stated in the QC procedures manual.
e matrix size should be chosen to provide an adequate number of pixels
for good signal and noise measurements. A 256 × 256 matrix is typically
adequate. e matrix size and FOV shall be consistently applied for QC
testing with their value stated in the medical physicist’s report and the QC
procedures manual.

96 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
IV. Annual MRI System Performance Evaluation
For single slice measurements, the slice thickness should be chosen to
optimize the noise measurement while still providing adequate signal in
the phantom. is is typically between 1 mm and 5 mm depending on
the eld strength. inner slices should be used at higher eld strengths,
thicker slices at lower elds. e slice thickness chosen shall be used
consistently and its value stated in the medical physicist’s report and the
QC procedures manual.
1. Volume Coil Tests
Volume coils encompass the body part to obtain signals relatively
uniformly from the tissues within the coil. In superconducting magnets,
the axis of this type of coil is generally parallel to the axis of the magnet
(parallel to the B
0
magnetic eld). In low-eld open magnet systems,
the axis of the volume RF coil is generally oriented perpendicular
to the B
0
magnetic eld. Signal-to-noise ratio (SNR), percent image
uniformity (PIU), and percent signal ghosting (PSG) are complementary
measurements for volume RF coils.
1. Position the RF coil in its normal clinical orientation. Place
the phantom in an orientation that most closely represents the
position of the body part of interest in the clinical scan. Generally,
the center of the phantom should be positioned as close to the
center of the RF coil as possible.
2. Positioning aids, such as external references on both the coil
and the phantom, should be noted and described in the QC
procedures manual. e phantom should be marked with stickers
or other marks to indicate the position of the RF coil with respect
to the phantom. In cases of complex coil geometries, such as
shoulder coils, photographs, and/or diagrams may be necessary
to ensure that the relationship between the coil and the phantom
is reproducible from test to test.
3. Run the pulse sequence with a slice positioned near the center
of the RF coil and with the uniform signal-producing volume
positioned in the image plane most oen used in clinical practice
(axial, sagittal, coronal, or oblique).
4. Record all pulse sequence and hardware parameters in the annual
system performance evaluation report.
TEST PROCEDURES

Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 97
IV.
Annual MRI System Performance Evaluation
MEDICAL PHYSICIST’S/
MRI SCIENTIST’S SECTION
Intensity and gradient distortion correction algorithms can signicantly
alter image signal and noise. erefore, when possible it is recommended
that these corrections be turned o for SNR measurements even if they
are used clinically. A uniform homogeneous phantom should be used.
e choice of the specic SNR method is the decision of the qualied
medical physicist/MRI scientist; however, it is essential that the same
method be used for all measurement comparisons and trend assessments.
Below are acceptable methods for measuring SNR.
a. SNR
i. Single-Image SNR Method (SNR
ACR
or SNR
NEMA4
)
1. Select an image depicting the center of the phantom that is
along the central axis of the phantom and is free of any internal
structures (Figure 10).
2. Create a “mean signal region of interest” that covers at least 75%
of the cross-sectional area of the phantom, as viewed in the image
(Figure 10a). is “mean signal ROI” denes the region in which
measurements will be performed later for signal uniformity.
3. Record the mean signal, which is the average value of all the
pixels in the mean signal ROI, in the annual system performance
evaluation report.
4. Place a measurement ROI of as large a size as possible in a
position in the background area outside the phantom volume in
the frequency-encoding direction (Figure 10b), since regions in
the image corrupted by artifacts, such as those oen occurring in
the phase-encoding direction, should be avoided. is is the “air
ROI.” One should be careful not to position the air ROI in a region
where eects of the RF receiver lter or gradient nonlinearity
corrections are noticeable. One should evaluate the background
with a low window width and appropriate level setting to display
background signal and noise (Figure 10b) to avoid placing the air
ROI in an area containing RF leakage or an area where the values
have been zeroed by the system. e size of the air ROI should
be as large as possible to obtain the best statistics on background
signal and noise measurements within the constraints
mentioned above.
RECORDING SIGNAL
MEASUREMENTS

98 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
IV. Annual MRI System Performance Evaluation
Figure 10. a) ROI placement to determine mean signal in an axial image of a
cylindrical phantom in a single-channel knee coil. The phantom was 9 cm in
diameter, and the FOV was 20 cm x 20 cm. b) Illustration of appropriate windowing
to analyze background signal, determine ROI placement, and perceive signal
truncation in the same image as a. Note the thin region of signal truncation along
each outer edge of the image FOV where signal has been zeroed (gray arrows). This
image, where phase-encoding was left-to-right, shows uniform background signal
and noise in the air regions that exclude the truncation bands. Appropriate air ROIs
include as much background area as possible in the frequency-encoding directions
(above and below the phantom in this case), excluding signal truncation bands at the
edges of the image eld and signal bleed areas near the phantom, as shown.
e simplest method to assess image noise is to use the standard
deviation in the background air ROI. Accurate measurements of
image signal or noise require ROIs of at least 1,000 pixels (NEMA
MS-1, 2008). If a single background air ROI does not provide
an adequate number of pixels, multiple air ROIs, such as the
two background ROIs in Figure 10, can be combined. Standard
deviations from multiple ROIs can be combined in quadrature:
For n ROIs: σ
combined
= √(σ
1
2
+ σ
2
2
+
...
+ σ
n
2
)/n
It is important that each ROI included be of similar area, as
combining signal standard deviation ROIs in quadrature attributes
equal weight to each ROI, regardless of area. It is also important
that each background ROI included be free from artifacts, signal
ltering, and other confounding inuences, as described above.
is means that to get an accurate measurement of background
noise, all air ROIs should be placed in the frequency-encoding
direction and be free from artifacts and ltering eects.
5. SNR
ACR
is calculated by dividing the mean signal in the phantom
by the standard deviation in the air ROI:
SNR
ACR
= (Mean Signal in Phantom)/σ
air
Record this value in the annual system performance evaluation
report.

Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 99
IV.
Annual MRI System Performance Evaluation
MEDICAL PHYSICIST’S/
MRI SCIENTIST’S SECTION
6. For a single-channel coil, mean signal and standard deviation in
the air ROI should be related by the expression [22,24]:
S
air
= (1.913) σ
air
is relationship between S
air
and σ
air
applies for single-channel
coils when the air ROI has been placed appropriately in a region
in the frequency-encoding direction that is free from RF receiver
lter corrections, gradient nonlinearity corrections, artifacts,
and background signal truncation. Finding this approximate
relationship between background signal and standard deviation
can be used as a check that ROI placement is reasonable and that
the measurement is free from the eects mentioned above.
On some scanners, signal or noise ltering is beyond the control
of the medical physicist/MRI scientist, and this theoretical
relationship between signal and its standard deviation in the
background ROI will not apply. e relationship shown above
between S
air
and σ
air
applies only to single-channel coils. For
multichannel phased-array RF coils, the relationship between
background signal and background standard deviation depends
on the number of channels being combined [24].
In cases where σ
air
is very low (i.e., less than about 4), signal
truncation due to digitization can adversely aect the accuracy of
noise measurements. In such cases, more reliable measurements
of σ
air
can be made by increasing air standard deviation values
to greater than 4 so that a truncation error during signal
digitization does not adversely aect noise measurement. is
can be done by decreasing the voxel volume (either by decreasing
the slice thickness, increasing the matrix for the same FOV, or
both), by decreasing TR, by increasing the bandwidth, or with
some combination of these modications to the acquisition
pulse sequence. To avoid inducing signal nonuniformities,
TR values should not be decreased below about 200 ms for
spin-echo sequences.
7. For a single-channel coil, SNR
ACR
is related to SNR
NEMA4
by a
constant multiplicative factor:
SNR
NEMA4
=
Mean Signal
σ
air
2-
π
2
√
≈ 0.655 ×
Mean Signal
σ
air
= 0.655 × SNR
ACR
8. e factor of
π
2
= 0.655 corrects for the fact that the MR
background signal has a Rayleigh distribution, not a Gaussian
distribution [22]. e important issue is not the multiplicative
factor, but the fact that SNR is measured in a consistent,
repeatable, and reliable manner, with an adequately large FOV
and adequately large background ROIs placed in the frequency-
encoding direction each time SNR measurements are made.
Consistent image acquisition and measurement methods
are needed to ensure that SNR is a reliable metric of RF coil
performance over time.

100 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
IV. Annual MRI System Performance Evaluation
Record the SNR value in the annual system performance
evaluation report.
ii. Two-Image SNR Method (SNR
NEMA1
)
1. Acquire two identical images of a uniform homogeneous
phantom (Figure 11). e two images should be acquired during
the same imaging session with a minimal time interval between.
Figure 11. NEMA Method 1: two-image dierence method for measuring SNR.
2. In either one of the two images, create a “mean signal region of
interest” that covers at least 75% of the cross-sectional area of the
phantom as viewed in the image.
3. Record the mean signal, which is the average of all the pixels in the
mean signal ROI, in the annual system performance evaluation
report.
4. Create the “dierence image” by subtracting the two images.
Note that some scanners do not provide the operator with the
tool needed to produce the dierence image, thus the NEMA
Method 1 technique will not be practical unless the images are
taken to another workstation that permits image subtraction. If
the NEMA Method 1 approach is not practical, the single-image
method, described above, should be used.
5. In the dierence image, create similar ROIs as in step 2 to dene
the mean signal and determine the standard deviation of the
dierence image (σ
di
).
6. Record σ
di
, the standard deviation of the pixels in the dierence
image ROI, in the annual system performance evaluation report.
7. SNR
NEMA1
is calculated by multiplying the mean signal by the
factor
√
2
(to account for the noise in two subtracted images
adding in quadrature) and then dividing by the noise standard
deviation of the dierence image (σ
di
).
SNR
NEMA1
=
√
2
Mean Signal
σ
di

Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 101
IV.
Annual MRI System Performance Evaluation
MEDICAL PHYSICIST’S/
MRI SCIENTIST’S SECTION
8. Record the SNR value in the annual system performance
evaluation report.
b. Percent Image Uniformity (PIU)
1. Referring back to Figure 10a, set the window width to a small
value (e.g., 1). Adjust the window level so that the region of
greatest signal intensity is depicted with only a few bright pixels
within the large “mean signal ROI” as shown in Figure 12a.
2.
Create a “measurement ROI” that is approximately 0.15% of the
area of the FOV, e.g., approximately 1 cm
2
for a 25 cm
×
25 cm FOV.
Figure 12. Evaluation of percent image uniformity in the same knee coil and
phantom shown in Figure 10. a) Appropriate windowing and ROI placement for
determination of maximum signal within the large ROI using the small ROI centered
on the few bright pixels on the right. b) Appropriate windowing and ROI placement
for determination of minimum signal within the large ROI using the small ROI
centered on the dark pixels at the top.
3. Move the measurement ROI to the position of greatest signal
intensity that is within the mean signal ROI (i.e., covering the
largest number of bright pixels within the mean signal ROI).
4. Determine the mean signal value of all the pixels in the small
measurement ROI. is is the maximum signal (max ROI).
Record the value in the annual system performance evaluation
report.
5. In a similar manner as steps 1–3, lower the window level so that
only a few dark pixels are displayed within the large mean signal
ROI and create a similar sized small ROI over the lowest signal
intensity within the mean signal ROI, as shown in Figure 12b.
6. Record this minimum signal (min ROI) value in the annual
system performance evaluation report.

102 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
IV. Annual MRI System Performance Evaluation
7. e PIU is calculated by using the following formula with max
and min ROIs:
PIU = 100 ×
(1 -
Max ROI-Min ROI
Max ROI+Min ROI
)
8. Record this value in the annual system performance evaluation
report.
c. Percent Signal Ghosting (PSG)
1. Establish measurement ROIs in the four positions as shown in
Figure 13 outside of the phantom volume (le, right, top, and
bottom).
2. Record each of the four measured mean signal values (le, right,
top, and bottom) in the annual system performance evaluation
report.
3. e PSG) is calculated by using the following formula:
PSG = 100 ×
|
(Le+Right) - (Top+Bottom)
(2 × Mean Signal)
|
4. Record this value in the annual system performance evaluation
report.
Figure 13. Placement of ROIs inside and outside the phantom to determine percent
signal ghosting.

Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 103
IV.
Annual MRI System Performance Evaluation
MEDICAL PHYSICIST’S/
MRI SCIENTIST’S SECTION
2. Surface Coil Tests
Surface coils are generally designed to receive signals from dierent
regions of the body. us, in evaluating these devices, one should select a
uniform volume of a phantom to demonstrate variations in uniformity of
signal produced by a given coil. e volume of investigation should have
relaxation times and RF coil loading properties similar to living tissue.
Most manufacturers provide phantoms for testing complex surface coil
systems.
e phantom should be permanently marked so that the surface coil can
be accurately positioned for successive measurements. Use only phantoms
that will be permanently stored at the site. Allow about ve minutes for
the solution in the phantom to settle down before starting the SNR scan
(prescan routines can be performed during this time).
a. SNR Surface Coil (maxSNR)
1. Select an image depicting the center of the phantom that lies
along the central axis of the phantom and is free of any internal
structures (Figure 14a).
2. Set the window width to a small value so that signal variations
within the phantom are visible. Adjust the window level so that
the region of greatest signal intensity is depicted.
3. Create a “measurement ROI” with an area of at least 1cm
2
.
4. Move the measurement ROI to the position of greatest signal
intensity within the phantom.
5. Determine the mean signal value in the small measurement ROI.
e ROI should be positioned so that it does not include any
obvious artifacts. is is the maximum signal. Record the value
in the annual system performance evaluation report.
6. Place a large measurement ROI outside of and away from the
phantom in the frequency-encoding direction, since regions in
the images corrupted by artifacts should be avoided. is is the
“noise ROI.” e noise ROI should be carefully positioned in
a region where the eects of the RF receiver lter, ghosting or
other artifacts are avoided (see Figures 14a and 14b). e noise
ROI should be made as large as possible to improve sampling
statistics while minimizing the eect of artifacts.
7. Determine the noise as the standard deviation (i.e., the root
mean square signal value) in the noise ROI located in the
image background (σ
air
). Record the value in the annual system
performance evaluation report.
TEST PROCEDURE

104 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
IV. Annual MRI System Performance Evaluation
Figure 14. Axial image of a uniform phantom acquired with an 8-channel spine
coil. Noise ROI chosen in the background in the frequency-encoded axis. a) Image
illustrating ROI placement to be used when estimating the maximum SNR. b) Image
illustrating ROI placement when estimating the mean SNR.
8. e maximum SNR is calculated by dividing the maximum
signal within the phantom by the standard deviation measured
outside of the phantom, σ
air
:
maxSNR = (Max Signal in Phantom)/σ
air
Record this value in the annual system performance evaluation
report.
9. Observe the signal intensity distribution and note on the annual
system performance evaluation report whether it generally
appears the same as when previous measurements were
performed on this coil. Save a copy of the image and record the
window width and window level settings for future reference.

Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 105
IV.
Annual MRI System Performance Evaluation
MEDICAL PHYSICIST’S/
MRI SCIENTIST’S SECTION
10. Observe the image and note on the annual system performance
evaluation report whether image ghosting appears to be unusually
high. If ghosting does appear high, measure the PSG as described
above in Section IV.D.1.c (volume coil PSG measurements).
b. SNR Surface Coil (MeanSNR)
1. Select an image depicting the center of the phantom that lies
along the central axis of the phantom and is free of any internal
structures (Figure 14b).
2. Create a “mean signal region of interest” that covers as much of
the cross-sectional area of the phantom as possible, as shown in
Figure 14b.
3. Record the mean signal, which is the average value of all pixels
in the mean signal ROI, in the annual system performance
evaluation report.
4. Place a measurement ROI of as large a size as possible in a
position in the background area outside the phantom volume
in the frequency-encoding direction (Figure 14b), specically
avoiding regions in the image corrupted by artifacts, such as
those oen occurring in the phase-encoding direction. is is
the “air ROI.” e air ROI position should also avoid regions
where the eects of the RF receiver lter or gradient nonlinearity
corrections are noticeable. One should evaluate the background
with a low window width and appropriate level settings to display
background signal and noise to avoid placing the air ROI in an
area containing RF leakage or an area where the values have been
zeroed by the system. e size of the air ROI should be as large
as possible to obtain the best statistics on background signal and
noise measurements within the constraints mentioned above.
5. Image noise is dened to be the standard deviation in the
background air ROI.
6. e mean SNR for the surface coil is calculated by dividing the
mean signal in the phantom by the standard deviation in the air
ROI:
mean SNR = (Mean Signal in Phantom)/σ
air
Record this value in the annual system performance evaluation
report.
3. RF Array Coils
RF array coils are closely coupled coils that work together, each with
their own RF channel, to produce more uniform signal over an extended
or irregular body part. A spine array, for example, includes sections
that collectively can image the entire spine at once or sets of adjacent
individual elements that can be selected to acquire images over a more
restricted section of the spine, such as a cervical spine, thoracic spine,
TEST PROCEDURE

106 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
IV. Annual MRI System Performance Evaluation
or lumbar spine. It is recommended that the qualied medical physicist/
MRI scientist perform a more detailed assessment of coil performance
by measuring SNR for each element of an RF array coil in a manner
similar to the surface coil SNR assessment. is test may require special
settings prior to image acquisition or access to the service functions of
the system so that separate images of each independent RF channel can
be acquired and displayed. If assessment of individual coil elements is not
possible, the single-image method described below can be used to assess
multichannel array coils. For more details regarding RF array coils see
Glockner et al [29].
e single-image method of SNR determination described above for
single-channel coils can be extended to multichannel phased-array coils
based on the methods of Constantinides et al [24]. As for single-channel
coils, phase-array coils ideally should be imaged with a FOV at least
twice the size of the phantom used or, alternatively, with the largest FOV
permitted on the system.
1. Select an image depicting the center of the phantom that lies
along the central axis of the phantom and is free of any internal
structures (Figure 15).
2. Create a “mean signal region of interest” that covers as much of
the cross-sectional area of the phantom as possible, as shown in
Figure 15a.
Figure 15. Axial image of a uniform phantom of a near-rectangular cross-section to
test a 4-channel cardiac surface coil. a) Window width and level have been set to
display signal nonuniformities within the phantom and to place the large ROI for
mean signal measurement within the phantom. b) The same image with window
width narrowed and level adjusted to better display background signal and noise.
Air ROIs have been placed outside the phantom to measure mean and standard
deviation values in the background. Signal within the phantom and standard
deviation in air are used to determine mean SNR for this surface coil, as described
by method b. above. Consistency of such SNR measurements from survey to survey,
along with similar measurements of each coil channel individually, is the best way to
assess that the entire coil works properly.

Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 107
IV.
Annual MRI System Performance Evaluation
MEDICAL PHYSICIST’S/
MRI SCIENTIST’S SECTION
3. Record the mean signal, which is the average value of all the
pixels in the mean signal ROI, in the annual system performance
evaluation report.
4. Place a measurement ROI of as large a size as possible in position
in the background area outside the phantom volume in the
frequency-encoding direction (Figure 15b), since regions in
the image corrupted by artifacts should be avoided. is is the
“air ROI”. One should be careful not to position the air ROI
in a region where eects of the RF receiver lter or gradient
nonlinearity corrections are noticeable. One should evaluate
the background with a low window width and appropriate level
setting to display background signal and noise (Figure 15b) to
avoid placing the air ROI in a an area containing RF leakage or
an area where the values have been zeroed by the system. e
size of the air ROI should be as large as possible to obtain the
best statistics on background signal and noise measurements
within the constraints mentioned above. If a single air ROI does
not provide an adequate number of pixels (i.e., at least 1,000),
multiple ROIs, such as the two background ROIs in Figure 15,
can be combined. Standard deviations from multiple ROIs can be
combined in quadrature.
For n ROIs: σ
air
=
√
(σ
1
2
+ σ
2
2
+
...
+ σ
n
2
)/n)
It is important that each ROI included be of similar area, as
combining standard deviation ROIs in quadrature attributes
equal weight to each ROI, regardless of size. It is also important
that each background ROI included be free from artifacts, signal
ltering, and other confounding inuences.
As with single-channel coils, more reliable measurements of σ
air
can be made by taking steps to ensure that air standard deviation
values are above about 4, so that signal truncation during
digitization does not adversely aect noise measurements. is
can be done by decreasing the voxel volume (either by decreasing
the slice thickness or increasing the matrix for the same FOV,
or both), by decreasing TR, by increasing the bandwidth, or
with some combination of these adjustments. To avoid inducing
signal nonuniformities, TR values should not be decreased below
200 ms for spin-echo sequences.
SNR is calculated by dividing the mean signal in the phantom by
the true noise standard deviation, σ
true
:
SNR = (Mean Signal in Phantom)/σ
air
Note that this SNR diers from SNR
ACR
. For single-channel coils,
this denition of SNR is equal to SNR
NEMA4
.
Factors contributing to variations in SNR include (i) general system
calibration (resonance frequency, ip angles, etc.), (ii) gain, (iii) coil
tuning, (iv) RF shielding, (v) coil loading, (vi) image processing, (vii)
scan parameters, and (viii) phantom positioning.
SUGGESTED
PERFORMANCE CRITERIA
AND CORRECTIVE
ACTIONS – ALL COILS
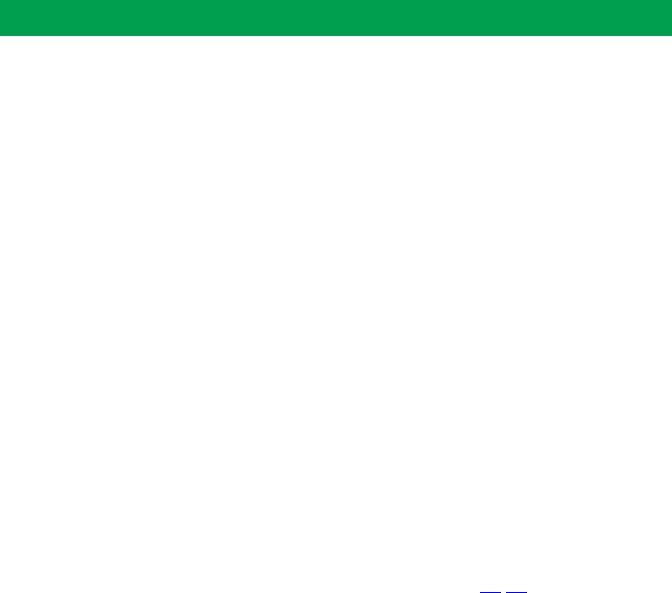
108 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
IV. Annual MRI System Performance Evaluation
A general lack of image intensity uniformity indicates a deciency in the
scanner, oen a defect in the RF subsystems. Sometimes pieces of metal
can get lost in the head coil or pieces of the RF coil can become dislodged
within the coil housing. ese can cause alterations of the distribution of
the RF magnetic eld.
Failure of coil components can aect coil impedance and may result in
degradation of image uniformity and SNR. Magnitude-reconstructed
images are commonly used in clinical MRI because they are relatively
immune to phase errors in the MR signals. When the phase errors
become large, they can result in ghosting and magnitude image. Ghosting
is a very nonspecic indication of a MRI system problem. In general, it is
caused by receiver, transmitter, or gradient uctuations.
Ghosting can also be caused by motion or vibration of the phantom
during the scan. Make sure that coils and phantoms are secured and are
not free to move during scanning.
Receivers on older systems that used analog components, particularly in
mixing and ltering stages, may have ghosts due to quadrature receiver
imbalance [30,31]. is ghosting is usually distinguished from other
ghosting since there will be one ghost, and it will be reected through
the origin of the volume of interest. us, an object in the upper right
corner of one slice will produce quadrature ghosts in the lower le corner
of another slice at an equal distance from the center of the image. e
service engineer recalibrating quadrature channels of the receiver coil can
eliminate quadrature ghosts.
Periodic amplitude inconsistencies can result in easily identiable types
of ghosting. A “half FOV ghost” or “N/2 ghost” is common in single-shot
EPI images and is dicult to eliminate entirely.
Action criteria should be determined by the qualied medical physicist/
MRI scientist taking into account the particular features of each piece of
equipment; however, simple guidelines should be followed.
Values of SNR vary greatly with MRI system type. e range of acceptable
measurements should be determined at the time of the acceptance testing
and/or by taking several baseline measurements and setting the action
limits at ± one standard deviation.
Head coils and other volume coils designed for clinical use have fairly
uniform spatial sensitivity near the middle of the coil when loaded as
typical for human tissue. In head coils, PIU values less than 90% are
uncommon for a properly functioning system. It should be noted that
for multielement array coils, application of an image intensity correction
algorithms may be necessary. e ACR MRI Accreditation Program
requires that PIU of the head coil be 87.5% or greater for systems of 1.5T
or below, and 82% or greater for 3T systems.
Ghosting ratios should be less than 2.5% using the head coil in
T1-weighted spin-echo scans.
ACTION CRITERIA
FOR ALL COILS
Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 109
IV.
Annual MRI System Performance Evaluation
MEDICAL PHYSICIST’S/
MRI SCIENTIST’S SECTION
is section has described a set of tests for monitoring RF coil
performance. It may be desirable to compare SNR and uniformity among
various RF coils. Note that the same imaging pulse sequence parameters
may be used for obtaining data on all RF coils. e data for these RF coils
also may have been obtained using various phantoms with dierent lling
solutions. Be careful to allow for the dierences among the relaxation
and loading properties of phantoms with dierent lling solutions. Using
phantoms with solutions that are identical in terms of relaxation times
and conductivity allows for the most direct comparison of performance
among various RF coils.
MRI service engineers have a set of diagnostic tests to determine whether
the RF coils are functioning properly. Oen, when a defect is detected the
RF coil cannot be repaired on-site and must be replaced with another coil
specic to the anatomy of interest.
E. Soft-Copy (Monitor) Quality Control
A so-copy QC program should be in place for all diagnostic
workstations. e specications for such a QC program are
outside the scope of this document. However, at a minimum,
the scanner console monitor and any on-site technologist
workstation, if applicable, should be included in the annual
system performance evaluation. For more information on so-
copy display QC, please refer to AAPM TG 18: Online report
N.03, Assessment of Display Performance for Medical Imaging
Systems.
At acceptance testing, display devices are tested to ensure that they
meet the manufacturer’s published specications for 1) maximum and
minimum luminance, 2) luminance uniformity, 3) resolution, and 4)
spatial accuracy. Measurements of the monitor’s performance should be
made at regular intervals thereaer using the techniques described below
or methods described in AAPM TG 18.
In general, so-copy display device quality control is dened in accordance
with DICOM Part 14. Currently, images are presented from the scanner
to the diagnostic workstation and scanner console monitors as raw pixel
values, but MRI system manufacturers do not provide the images with an
associated “presentation look-up table.”
Without full implementation of the DICOM Part 14 Standard, the
following limited set of tests is recommended. (In addition, the qualied
medical physicist/MRI scientist is referred to the report of Task Group 18
of the Diagnostic X-Ray Imaging Committee of the American Association
of Physicists in Medicine for more thorough and standardized so-copy
display tests [32]). If a scanner is fully DICOM Part 14 compliant, then
additional tests, such as luminance response can be carried out ([33,34]).
SUMMARY
OBJECTIVE
TEST PROCEDURE

110 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
IV. Annual MRI System Performance Evaluation
1. Maximum and Minimum Luminance
a. Measure monitor luminance using a precise luminance meter.
Record the data for the luminance meter in the annual system
performance evaluation report.
b. Measurements are performed on a monitor screen when the
image displays are at their brightest levels. Set the window width
and window level to their minimum values so that the monitor is
uniformly at its brightest value.
c. Measure the luminance in the center and at each of the four
corners of the image display area. Record these maximum
luminance values in the annual system performance evaluation
report.
d. Measurements are also performed in the same manner on the
monitor screen when the image display is at its darkest level. Set
the window width to its minimum value and window level so that
the monitor is uniformly at its darkest value. ese minimum
luminance values should also be recorded in the annual system
performance evaluation report.
2. Luminance Uniformity
Calculate the percent dierence of the brightest luminance values
measured in the image display area, using the following equation:
% dierence = 200 ×
L
max
- L
min
L
max
+ L
min
Where L
max
and L
min
are the maximum and minimum measured
luminance values, respectively, for the measurements taken with
the monitor at its brightest level (AAPM TG18: On-line report
No. 03, Assessment of Display Performance for Medical Imaging
Systems).
Record this value in the annual system performance evaluation
report.
3. Resolution, Linearity, Contrast, and Distortion
e qualied medical physicist/MRI scientist should view the “SMPTE”
pattern on the monitor while positioned directly in front of the image
display and at least 50 cm from the monitor surface. e SMPTE pattern
should be evaluated as follows:
a. e 0–5% contrast pattern should be visible.
b. e 95–100% contrast pattern should be visible.
c. Each gray-level step from 0% to 100% should be distinct from
adjacent steps.
d. e borders and lines of the SMPTE pattern should be straight.

Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 111
IV.
Annual MRI System Performance Evaluation
MEDICAL PHYSICIST’S/
MRI SCIENTIST’S SECTION
e. ere should be no distortion or misalignment using the grids
across the screen (linearity).
f. Alphanumeric characters should be sharp (in focus).
g. e high contrast line-pair images (each line in vertical and
horizontal stripes) in the squares at the center and in the corners
should be distinct without magnication.
h. ere should be no streaking in and around the white rectangles
and the black rectangles.
Record observations as “comments” in the annual system performance
evaluation report.
4. Spatial Accuracy
Typically, a SMPTE test pattern that displays a rectangular grid is displayed
with a magnication factor that allows it to ll the entire screen. A similar
grid pattern is laid over the screen and compared to the displayed image.
Record observations as “comments” in the annual system performance
evaluation report.
Maximum and minimum luminance: e maximum brightness of
diagnostic quality monitors should exceed 90 Cd/m
2
, and the minimum
brightness values should be less than 1.2 Cd/m
2
.
Luminance uniformity: e calculated % dierence in the maximum
luminance values should be ≤ 30%.
e resolution, linearity, contrast, and distortion criteria described above
should be met.
For more details regarding evaluation of the SMPTE test pattern, see
Medical Physicist/MRI Scientist’s Appendix, Section VI.C.
F. MR Safety Program Assessment
To minimize risks in the MR environment to patients, health care
professionals, and any others that may encounter the elds of the MR
scanner, each site must establish, implement, and maintain current safety
policies and procedures. Information regarding establishment of a quality
MR safety program can be found in the ACR Guidance Document for
Safe MR Practices: 2013 [35]. e hazards in the MRI suite maybe divided
into three categories: 1) facility design, 2) operational, and 3) clinical.
Facility design refers to the facility layout in which zones are identied
with appropriate signage and strategies for controlled access. Operational
refers to procedures for screening both personnel and objects that may
be introduced to the MR suite. Clinical refers to procedures that can be
used to determine the MR safety and compatibility of implants and other
medical devices.
SUGGESTED
PERFORMANCE CRITERIA
AND CORRECTIVE ACTION
OBJECTIVE

112 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
IV. Annual MRI System Performance Evaluation
At the time of the annual performance testing, the qualied medical
physicist/MRI scientist must review the site’s written safety policies and
determine that the written policies are readily accessible to facility sta.
e categories listed below should be addressed in the policies.
• Designated MR medical director
• Site access restrictions (MR zones)
• Documented MR safety education/training for all personnel
• Patient and non-MR personnel screening
• Pediatric patients
• Magnet quench
• Cryogen safety
• Acoustic noise
• Pregnant patients and sta
• Contrast agent safety
• Sedations
• ermal burns
• Emergency code procedures
• Device and object screening
• Designation of MR safe/MR conditional status
• Reporting of MR safety incidents or adverse incidents
• Patient communication
• Infection control and medical waste
1. Written policies and procedures are present and are being
reviewed and updated on a regular basis.
2. Facility has appropriate signage and methods of controlled
access.
3. Documentation of regular MR safety training for all
MR-designated personnel.
METHOD
CRITERIA FOR
COMPLIANCE

Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 113
V. References
MEDICAL PHYSICIST’S/
MRI SCIENTIST’S SECTION
1. American College of Radiology. ACR-AAPM technical standard for
diagnostic medical physics performance monitoring of magnetic resonance
imaging (MRI) equipment. Available at: http://www.acr.org/~/media/ACR/
Documents/PGTS/standards/MonitorMRIEquipment.pdf Published 2014.
Accessed March 1, 2015.
2. National Electrical Manufacturers Association. NEMA-MS-1. Determination
of SNR in Diagnostic Magnetic Resonance Images. Rosslyn, VA:
NEMA; 2008.
3. National Electrical Manufacturers Association. NEMA-MS-2. Determination
of Two-Dimensional Geometric Distortion in Diagnostic MR Images. Rosslyn,
VA: NEMA; 2008.
4. National Electrical Manufacturers Association. NEMA-MS-3. Determination
of Image Uniformity in Diagnostic Magnetic Resonance Images. Rosslyn, VA:
NEMA; 2008.
5. National Electrical Manufacturers Association. NEMA-MS-5. Determination
of Slice ickness in Diagnostic Magnetic Resonance Images. Rosslyn, VA:
NEMA; 2010.
6. National Electrical Manufacturers Association. NEMA-MS-6. Determination
of Signal-To-Noise Ratio and Image Unifomity for Single-channel, Non-
volume Coils in Diagnostic Magnetic Resonance Imaging (MRI). Rosslyn, VA:
NEMA; 2008.
7. National Electrical Manufacturers Association. NEMA-MS-9.
Characterization of Phase Array Coils For Diagnostic Magnetic Resonance
Images. Rosslyn, VA: NEMA; 2008.
8. American Association of Physicists in Medicine. AAPM Report No. 100:
Acceptance Testing and Quality Assurance Procedures for Magnetic Resonance
Imaging Facilities. College Park, MD: AAPM; 2010.
9. American College of Radiology. Site Scanning Instructions for Use of the MR
Phantom for the ACR MRI Accreditation Program. Reston, VA: ACR; 1997.
10. American College of Radiology. Phantom Test Guidance for the ACR MRI
Accreditation Program. Reston, VA: ACR; 1998.
11. American College of Radiology. Site Scanning Instructions for Use of the
Small MRI Phantom for the ACR MRI Accreditation Program. Reston, VA:
ACR; 2008.
12. American College of Radiology. Phantom Test Guidance for Use of the Small
MRI Phantom for the MRI Accreditation Program. Reston, VA: ACR; 2008.
13. Hoult DI, Lauterbur PC. e sensitivity of the zeugmatographic experiment
involving human samples. Journal of Magnetic Resonance. 1979;34:425-433.
14. Price RR, Axel L, Morgan T, et al. Quality assurance methods and phantoms
for magnetic resonance imaging: report of AAPM Nuclear Magnetic
Resonance Task Group No. 1. (AAPM Report No. 28). Medical Physics.
1990;17(2):287-295.
15. Kra KA, Fatouros PP, Clarke GD, Kishore PRS. An MRI phantom
material for quantitative relaxometry. Magnetic Resonance in Medicine.
1987;5:555-562.
REFERENCES

114 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
V. References
16. Redpath TW, Wiggins CJ. Estimating achievable signal-to-noise ratios of
MRI transmit-receive coils from radio-frequency power measurements:
applications in quality control. Physics in Medicine and Biology.
2000;45:217-227.
17. Moerland MA, Beersma R, Bhagwandien R, Wiljrdeman HK, Bakker CJG.
Analysis and correction of geometric distortions in 1.5T magnetic resonance
images for use in radiotherapy treatment planning. Physics in Medicine and
Biology. 1995;40:1651-1664.
18. Bakker CJG, Moreland MA, Bhagwandien R, Beersma R. Analysis of
machine-dependent and object-induced geometric distortion in 2DFT MR
imaging. Magnetic Resonance Imaging. 1992;10:597-608.
19. Vlaardingerbroek MT, den Boer JA. Magnetic Resonance Imaging. 2nd ed.
Berlin: Springer-Verlag; 1999.
20. Haacke EM, Brown RW, ompson MR, Venkatesan MR. Magnetic
Resonance Imaging: Physical Principles and Sequence Design. New York, NY:
Wiley-Liss; 1999.
21. Chen HH, Boykin RD, Clarke GD. Routine testing of magnetic eld
homogeneity on clinical MRI systems. Medical Physics. 2006;33:4299-4306.
22. Henkelman RM. Measurement of signal intensities in the presence of
noise in MR images [published correction appears in Medical Physics.
1986;13:544]. Medical Physics. 1984;12:232-233.
23. Gudbjartsson H, Patz S. e Rician noise distribution of noisy MRI data.
Magnetic Resonance in Medicine. 1995;34:910-914.
24. Constantinides CD, Atalar E, McVeigh ER. Signal-to-noise measurements
from magnitude images in NMR phased-arrays. Magnetic Resonance in
Medicine. 1997;38:852-857.
25. Kaufman L, Kramer DM, Crooks LE, Ortendahl DA. Measuring signal-to-
noise ratios in MR imaging. Radiology. 1989;173:265-267.
26. Sijbers J, den Dekker AJ, van Audekerke J, Verhoye M, van Dyck D.
Estimation of the noise in magnitude MR images. Magnetic Resonance
Imaging. 1998;16:87-90.
27. Firbank MJ, Coulthard A, Harrison RM, Williams ED. A comparison of two
methods for measuring the signal-to-noise ratio on MR images. Physics in
Medicine and Biology. 1999;44:N261-N264.
28. American College of Radiology. Magnetic Resonance Imaging Quality
Control Manual. Reston, VA: ACR; 2004.
29. Glockner JF, Hu HH, Stanley DW, et al. Parallel MR imaging: a user’s guide.
Radiographics. 2005;25:1279-1297.
30. Chen CN, Hoult DI. Biomedical Magnetic Resonance Technology. Boca
Raton, FL: CRC Press; 1989.
31. Holland GN, MacFall JR. An overview of digital spectrometers for MR
imaging. Journal of Magnetic Resonance Imaging. 1992;2:241-246.
32. Samei E, Badano A, Chakraborty D, et al. Assessment of Display Performance
For Medical Imaging Systems, Report of the American Association of
Physicists in Medicine (AAPM) Task Group 18. AAPM On-Line Report
No. 03. Madison, WI: Medical Physics Publishing; 2005.

Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 115
V. References
MEDICAL PHYSICIST’S/
MRI SCIENTIST’S SECTION
33. Shepard SJ. Calibration and quality control of digital hard and so copy
display devices on a PACS network. In: Quality Assurance for the ird
Millennium [CD-ROM]. Strakshall G, Jackson E, eds. College Park, MD:
Southwest Chapter AAPM; 2000.
34. Van Metter R, Zhao B, Kohn K. e sensitivity of visual targets for display
quality assessment. Proceedings of SPIE. 1999;3658:254.
35. Kanal E, Barkovich A, Bell C, et al. ACR guidance document on MR safe
practices: 2013. Journal of Magnetic Resonance Imaging. 2013;37(3):501-
530.

116 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
VI. Appendix
A. MRI Equipment Evaluation Summary Form
e MRI Equipment Evaluation Summary Form is provided to facilitate
the communication of test results to the facility managers. An Excel
version of this form, along with the MR Safety Checklist in another tab,
can be accessed here. MR Equipment Evaluation Summary Form.
e medical physicist/MR scientist may use any data report format as
long as the required information is present. Regardless of forms used,
the medical physicist’s report must include a pass-fail summary of tests
performed and a summary of recommendations to the facility.
B. MRI Safety Program Assessment Checklist
Access the MRI Safety Program Assessment Checklist.
C. Hard-Copy (Film) Quality Control Operating
Levels
e qualied medical physicist/MRI scientist should participate in
establishing the correct operating levels for the lm printer. is procedure
will be carried out when the QC program is initiated and whenever a
signicant change is made in the lm system. e QC technologist is
responsible for comparing lms against the established operating levels.
is is done weekly to ensure consistent lm quality (MRI Technologist’s
Section V).
e qualied medical physicist/MRI scientist should seek the participation
of the supervising radiologist and lm printer system service engineer.
1. Have the service engineer conrm that the lm printer is
performing within manufacturer’s specications. Running the
manufacturer’s diagnostic tests should do this.
2. If the lm system has a wet-process lm processor, make sure the
chemicals are fresh, it is operating at the correct temperature, and
it is operating with the correct developer and xer replenishment
rates. Correct temperature and replenishment rates are those
specied in the lm manufacturer’s written literature. e service
engineer should be asked to assist with this if needed.
3. At the lming console, adjust the monitor brightness and
contrast settings according to the manufacturer’s recommended
procedure.
4. Be sure there is low ambient light and that there is no glare on the
screen when making these adjustments. e lighting conditions
should be the same as that used for routine lming.
APPENDIX
ESTABLISHING
OPERATING LEVELS

Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 117
VI. Appendix
MEDICAL PHYSICIST’S/
MRI SCIENTIST’S SECTION
5. Oen the controls for monitor brightness and contrast are
hidden inside the console and not accessible to the user. If there
is any doubt about the correct procedure, or if the controls are
not accessible, have the service engineer make the adjustments.
6. Display the SMPTE test pattern (MRI Technologist’s Section
V) on the lming console. Set the display window and level to
the manufacturer-specied values for the SMPTE pattern on
this console.
7. It is important to nd out from the manufacturer’s documentation
or from the service engineer the correct window and level values
for the SMPTE pattern on the particular display being used.
Do not set the window and level by eye. Doing so invalidates
this procedure.
8. Examine the SMPTE pattern to conrm that the gray-level
display on the lming console is subjectively correct.
One should see an even progression of gray levels around the ring
of gray-level patches. e patch should appear fully black, and
the 100% patch should appear bright white. Verify that the 5%
patch can be distinguished in the 0/5% patch, the 95% patch can
be distinguished in the 95%/100% patch, and that all the patches
around the ring of gray levels are distinct from their neighbors.
On some displays, the 5% patch may be just barely discernible in
the 0/5% patch. at is acceptable. If it cannot be seen at all, that
is unacceptable. Normally the 95% patch is easy to discern in the
95%/100% patch.
If these conditions are not met, it is necessary to correct the
problem before continuing with this procedure. Most oen,
the problem is poor adjustment of the monitor brightness and
contrast. Excessive ambient lighting can also cause the problem
and occasionally, components of the display may need repair or
replacement. If so, seek assistance from the service engineer.
9. Film the SMTPE pattern. Use a 6-on-1 format and capture the
pattern into all six frames.
10. Visually compare the lmed SMPTE pattern grayscale densities
on a viewbox to the monitor displaying the same image with the
same window and level settings. Make necessary lm printer
adjustments to match the lm to the monitor appearance, using
the manufacturer’s recommended procedures. If you are unsure
how to do this, obtain assistance from the service engineer.

118 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
VI. Appendix
11. Film several patient images representative of the studies normally
done with this scanner. With the supervising radiologist,
compare these patient images printed on lm and displayed
on the monitor, being careful to display the images with the
same window width and level settings as used for their lming.
If necessary, make further adjustments to the lm printer to
match the patient lms to the monitor appearance, using the
manufacturer’s recommended procedures.
12. Repeat steps 6 through 8 until a lm printer adjustment is found
such that the lmed SMPTE pattern images and lmed patient
images are a good match to their appearance on the monitor.
Save the nal lms for future reference when troubleshooting
lm quality problems.
13. Using a lm densitometer, measure the optical density of the 0,
10%, 40%, and 90% gray-level patches of the SMPTE pattern.
Do this for the image in the upper-le frame of the lm, the
upper-right of the lm, and the lower-right of the lm. Note any
signicant variations from one location to another.
Record the measured optical density values on a new copy of
the Film Printer Control Chart. is will be the new chart for
the weekly lm QC measurements (MRI Technologist’s Section,
Appendix VIII.C).
At this point, the baseline data for the weekly lm printer QC
measurements have been acquired. e remaining three steps gather
some additional data, which are easy to obtain and are valuable when
troubleshooting lming problems.
1. Film printers can print test patterns that are generated internally
by the printer. If it is available, print an internally generated
SMPTE pattern; otherwise, print an internally generated
gray-level step pattern having at least eight steps. Consult the
manufacturer’s documentation or the service engineer for the
correct way to do this.
2. Using a lm densitometer, measure the optical densities of the 0,
10%, 40%, and 90% gray-level patches of the internally generated
SMPTE pattern.
3. If a gray-level step pattern was used instead of the SMPTE
pattern, nd and measure the steps with optical densities closest
to 2.45, 2.10, 1.15, and 0.30.
4. On a separate page for inclusion in the lm printer QC section of
the QC notebook, do the following:
a. Record the measured optical densities for the internally
generated test pattern.
b. Note which internally generated pattern was used and how it
was printed.
ADDITIONAL
BASELINE DATA

Magnetic Resonance Imaging Quality Control Manual Return to Table of Contents – 119
VI. Appendix
MEDICAL PHYSICIST’S/
MRI SCIENTIST’S SECTION
c. If a step pattern was used instead of the SMPTE pattern, note
which steps of the pattern were used for the optical density
measurements.
d. Put marks on the lm indicating which patches or steps were
measured. Save the lm for future reference.
When the qualied medical physicist/MRI scientist is called in to assess
problems with camera performance, the following steps should be
followed:
1. Determine whether the problem lies in the camera and/or
processor or if it lies in the part of the lm system chain between
the scanner and the camera.
Perform steps 1 and 2 listed under additional baseline data; that
is, print the internally generated test pattern from the lm printer
and measure the optical densities. Compare these measurements
with the baseline measurements previously recorded. Use the
same optical density ranges for the control limits on this data
as are used for the corresponding optical density values in the
weekly QC.
If the optical densities are outside the control limits, there is a
problem with the processor or the camera. If the optical densities
are within control limits, the problem lies in the part of the lm
chain from the scanner to the interface electronics in the camera.
2. If the problem is determined to lay in the camera or processor:
a. If the system has a wet-process lm processor, contact the
service engineer responsible for the processor. In systems
with a wet-process processor, it is the component most oen
responsible for lm quality problems.
b. If the system has a dry process camera, or it has a wet-process
processor that has been checked and found to be functioning
correctly, contact the service engineer responsible for the
camera.
3. If the problem is determined to lay in the part of the lm chain
between the scanner and the lm printer interface electronics:
Notify the service engineers responsible for the components
of this part of the lm chain and require them to cooperate in
identifying and correcting the problem. Normally this will
include the lm printer service engineer and the scanner service
engineer. If there is a PACS or digital imaging network between
the scanner and the camera, the service engineer for that system
must be involved as well.
CORRECTIVE ACTION

120 – Return to Table of Contents Magnetic Resonance Imaging Quality Control Manual
VI. Appendix
ere is, in general, no easy way to further localize the cause of
the problem. erefore, it is important to insist that the engineers
responsible for the various components of this part of the lm
chain work cooperatively to resolve the problem. e QC data
and data from step 1 above should be shown to the engineers so
they have a clear understanding of the nature of the problem and
the reasoning that led to identifying the problem within this part
of the lm chain.