School of Medicine
School of Medicine
Clinical Training Manual and
Teaching Hospital Affiliation
Agreement
February 2019

February 2019
School of Medicine, EUC/Clinical Training Manual …. 2
Table of Contents
Introduction .................................................................................................................... 5
Welcome Message ......................................................................................................... 7
PART I ............................................................................................................................. 8
Mission, Vision and Values
General Information.................................................................................................... 8
Roles and Responsibilities for Clinical Training ......................................................... 8
The Clinical Training Committee ............................................................................... 9
Clinical Training Advisors ....................................................................................... 11
Affiliated Hospitals ................................................................................................... 12
EUC Medical Students Clinical Training ................................................................. 13
Assignment of Students to Clinical Training Sites ................................................... 13
Involvement of Students with Patients ..................................................................... 14
Student Assessment ............................................................................................... 15
The Logbook ........................................................................................................... 16
Professional Conduct and Responsibility .............................................................. 17
Conduct Code ......................................................................................................... 17
Attendance and Time-off Policies ............................................................................ 19
Student Health and Safety ....................................................................................... 19
Immunization requirements ..................................................................................... 19
Hand hygiene and isolation precautions .................................................................. 19
Safe use and disposal of sharps ............................................................................. 20
Assessment of Training Sites ................................................................................. 20
Student Evaluations of Clinical Training ................................................................ 20
PART II .......................................................................................................................... 21
Clinical Training Curriculum .................................................................................... 21
EUC Curriculum ........................................................................................................ 21
Clinical Training Spiral ............................................................................................. 22
The Clinical Training Curriculum ............................................................................ 22
Competencies ......................................................................................................... 24
Entrustable Professional Activities .......................................................................... 24
Outcome Objectives ................................................................................................. 25
Medical Knowledge ................................................................................................. 25
Clinical Skills ........................................................................................................... 25

February 2019
School of Medicine, EUC/Clinical Training Manual …. 3
Professional Behavior ............................................................................................. 26
Assessment and Grading ........................................................................................ 26
Grading Policy for the clerkships ............................................................................. 26
Components of Assessment (in Addition to Written Examinations).................... 27
Clinical Performance ............................................................................................... 27
OSCEs .................................................................................................................... 28
Clinical Evaluation Exercise (MiniCEX) ................................................................... 29
Inadequate Performance ......................................................................................... 29
EUC Core Clinical Training Clerkships ................................................................... 30
Clinical Training I (MED407) Respiratory & Cardiovascular .................................... 30
Clinical Training II (MED417) - Digestive System & Hematology............................ 34
Clinical Training III (MED408) - Infectious Diseases and Clinical Microbiology ....... 37
Clinical Training IV - Endocrine system, Uro-Nephrological System & Male
Genital Tract ............................................................................................................ 40
Clinical Training V - Musculoskeletal System ......................................................... 45
Clinical Training VI (MED519) - Nervous System & Psychiatry .............................. 48
Clinical Training VII (MED510) - Pediatrics ............................................................. 51
Clinical Training VIII (MED520) - Dermatology ....................................................... 56
Clinical Training IX (MED611) - Obstetrics & Gynecology ...................................... 58
Diagnosis by Imaging (MED322) ............................................................................. 62
Clinical Bioethics & Legal Medicine (MED428) ........................................................ 63
Primary Care (MED631) ........................................................................................ 66
Clinical Training X (MED621) - Ophthalmology ....................................................... 70
Clinical Training XI (MED612) - Otorhinolaryngology .............................................. 74
Clinical Training XII (MED622) - ER, Toxicology, Oncology & Palliative Care ........ 78
Additional Requirements ......................................................................................... 82
Medical Therapeutics (MED530) ............................................................................. 82
Symptoms & Interpretation of Complementary Examination Procedures (MED661)
................................................................................................................................ 82
Electives .................................................................................................................... 83
Healthcare Management ......................................................................................... 83
Clinical Embryology ................................................................................................. 84
Rehabilitation Medicine ........................................................................................... 85
Research Methods & Scientific Writing .................................................................... 86

February 2019
School of Medicine, EUC/Clinical Training Manual …. 4
Interventional Radiology .......................................................................................... 87
PART III ......................................................................................................................... 89
Clinical Centers and Affiliated Hospitals ................................................................ 89
Affiliated Clinical Center or Hospital ....................................................................... 89
List of Appendices.................................................................................................... 90
APPENDIX I .............................................................................................................. 91
Clinical Training Organogram ................................................................................. 91
Appendix II ................................................................................................................ 95
Student Clerkship Evaluation Form – Final ............................................................ 95
Appendix III ............................................................................................................... 97
Individual Student Logbooks – Example Semester 8 ............................................ 97
Appendix IV ............................................................................................................. 124
Clinical Practice Incidence Report Form .............................................................. 124
Appendix V .............................................................................................................. 125
Health Requirements for Clinical Rotation ........................................................... 125
Appendix VI ............................................................................................................. 125
Confidential Student Feedback and Comments Form ........................................ 126
Appendix VII ............................................................................................................ 127
Clinical Competence Building Roadmap .............................................................. 127
Appendix VIII ........................................................................................................... 129
Student Confidence in Performing Practical and Clinical Skills Questionnaire129
Appendix IX ............................................................................................................. 134
Comprehensive Clinical Competency Assessment - OSCEs ............................. 134

February 2019
School of Medicine, EUC/Clinical Training Manual …. 5
Introduction
European University Cyprus (EUC), School of Medicine aims to assure quality in basic and
clinical medical education. In line with General Medical Council (GMC) and the Accreditation
Council for Graduate Medical Education (ACGME) requirements for clinical placements for
medical students, the EUC curriculum “includes practical experience of working with patients
throughout all years, increasing in duration and responsibility so that graduates are prepared
for their responsibilities as provisionally registered doctors.” According to these guidelines,
EUC aims to “provide enough structure in clinical placements to enable students to
demonstrate the “outcomes for graduates” across a range of clinical specialties.”
The Clinical Training Manual (CTM) serves as a reference guide for clinical placements and
training. The purpose of this manual is to explain how academic clinical training activities are
supported and organized at EUC, in order to assist both students and clinical instructors
throughout their clinical training activities. EUC Clinical Training Manual and Teaching Hospital
Affiliation Agreement also provides the framework for EUC to establish comprehensive
agreements with the individual organizations that provide clinical training for EUC medical
students. In order to be in agreement with changes in governmental policies and regulations,
as well as requirements outlined by the GMC and ACGME, the CTM is regularly reviewed and
revised, accordingly.
The aim of the EUC CTM and Teaching Hospital Affiliation Agreement is to:
1. Ensure that the affiliated hospitals are aware their responsibilities in relation to teaching
medical students
2. Ensure that the medical students are aware of their responsibilities in learning and in
relation to patients’ rights
3. Ensure that EUC medical students are effectively supervised during their clinical
placement
4. Indicate means that EUC will evaluate the effectiveness of clinical placements
5. Ensure compliance with national and EU accrediting agencies and licensing
requirements
To achieve these aims, the following have been specifically detailed in the CTM
The structure of EUC clinical program, including educational goals and learning
objectives
The roles and responsibilities of each participant in the EUC medical education program
with particular focus on the clinical affiliates
The learning environment and opportunities required for the medical students to achieve
competency
Process and responsibilities of organizing clinical placements within the medical school
and hospital
Internal Quality Assurance – evaluation of effectiveness of clinical placements
Selection process of those involved in clinical instruction
The curriculum of the School of Medicine, European University Cyprus (EUC) is of total duration
of 5685 hours and includes theoretical and clinical training, according to the European Directive
2013/55/EU of the European Council. Students’ clinical training is an integral part of their
education, of total duration of more than 2200 hours. Clinical training takes place in pre-
determined sites of the public and private sector, following appropriate planning. Clinical training

February 2019
School of Medicine, EUC/Clinical Training Manual …. 6
is continuously supervised by the academic staff of the School of Medicine of EUC, in close
collaboration with clinical teaching staff of the affiliated training sites, and is performed according
to the school clinical curriculum.
Clinical training at EUC:
Is mandatory for all students of the School of Medicine.
Takes place primarily during years 4 to 6 of medical studies
Has a duration according to the European and International guidelines that corresponds
to the year and course of study.
Vision, aim and objectives of clinical training
The overall objectives of the clinical training of medical students are:
To familiarize students with the structure, the function and the capacities of the healthcare
system
To familiarize and introduce the students to the various levels and institutions of the healthcare
system
To develop clinical skills and successfully combine them with their theoretical knowledge
To demonstrate and develop communication skills and teamwork
To apply practical skills in real-life healthcare environments
To develop professionalism in their daily clinical practice
To establish the concept of clinical training during medical undergraduate studies
To create an environment of mutual collaboration and develop ongoing relations between the
School of Medicine and the collaborating healthcare sites
Finally, to equip medical graduates with all necessary practical skills to pursue their
postgraduate endeavors

February 2019
School of Medicine, EUC/Clinical Training Manual …. 7
Welcome Message
On behalf of the European University Cyprus School of Medicine faculty, clinical teaching
personnel, staff and administration, welcome to the Clinical Training Core Program. Our
exceptional and diverse faculty and personnel are fully committed to the dissemination of medical
knowledge and the training of a new generation of competent physicians. We are dedicated to
the teaching process as we constantly aim to improve and embrace modern principles of medical
education. At EUC, we continuously strive towards providing an optimal learning environment by:
1) constantly improving our understanding of medical knowledge; 2) remaining innovative, both in
our curriculum and teaching practices; and 3) inspiring our student to be passionate about
providing their patients with the best possible care.
The Clinical Training Core at EUC is the last phase of the spiral, competency-based curriculum
designed to introduce students to the best practices in patient care, using innovative teaching
strategies, exposure to advanced simulation training, and much more. The horizontally integrated,
spiral program of the first three years of the Structure – Function curriculum, where students learn
clinical skills from their first year, was designed to ensure a smooth transition from basic to clinical
science applications.
As we enter the Era of Bioinformatics, medical educators are challenged to seek innovative
teaching methods that address the multitude and magnitude of scientific, technological and
demographic factors that have converged to revolutionize today’s approach to human health and
well-being. These advancements not only bring challenges and new demands to today’s
physicians, but also to today’s medical educators. EUC’s mission is to prepare our students to
excel in the art of healing, but also to become inspired innovators for the advancement of
knowledge and patient-centered healthcare.
Our affiliation with state-of the art clinics and hospitals affords our students with a unique clinical
learning experience. Each center is a foremost healthcare provider. With this exposure to an
incredible diversity of patients, our graduates emerge fully prepared to practice medicine in this
increasingly global society. Our aim is that our students experience a full spectrum of health care
environments.
EUC is stepping to the forefront of global medical and health education. We are dedicated to
preparing the healthcare leaders of tomorrow, with outstanding clinicians and scientists who will
contribute to the advancement of science and medicine across the globe.
Professor E. Johnson
Acting Dean

February 2019
School of Medicine, EUC/Clinical Training Manual …. 8
PART I
Mission, Vision and Values
The Mission of the School of Medicine is to educate medical students, graduate students, and
postdoctoral fellows in accordance with the highest professional standards; to train competent and
caring physicians to practice patient-centered medicine of the highest standard; and to identify and
answer fundamental questions in the mechanisms, prevention and treatment of disease, in health
care delivery and in the basic biomedical sciences.
The Vision of the undergraduate curriculum is to produce leaders in Medicine who will learn to
apply the foundation of a broad medical education to improve health at a National and International
level through patient care, research, and education.
The core Values of the EUC School of Medicine are
Excellence in the conduct of education, research, patient care and community engagement
Integrity Acting with honesty, accountability & social responsibility
Respect Demonstrated by civility and communication worthy of the trust given to us as
teachers, scholars and healers
Collaboration Fostering creative partnerships with open communication
Community Dedication to improve the quality of life of the community
Transparency Promoting an atmosphere of openness to promote quality in medical education,
research and clinical care
General Information
Clinical Training of medical students is the cornerstone of the EUC medical curriculum, where the
multiplicity of activities in clinics and hospitals affiliated with EUC are selected to constitute unique
learning environments for our medical students. Keeping in line with modern trends, Clinical
Training (Clerkships) at EUC takes place in a variety of health care sites, including primary,
secondary, and tertiary and community healthcare providers. As such, individualized joint
agreements between EUC and its affiliated hospitals and clinical centers are devised to facilitate
the clinical training program of our medical students.
While the healthcare providers of the hospital and clinic supervise the in-house educational
program, every affiliated hospital and clinic adheres to the precepts and standards established by
the EUC clinical curriculum, as outlined and detailed in the EUC CTM. Routine meetings between
the EUC course directors and the heads of the clinical health care departments, facilitates open
communication and clearly defined clinical educational goals.
The EUC School of Medicine has the ultimate and final right to evaluate the student’s overall
academic accomplishments within the clinical training program. The School of Medicine will
determine whether or not: 1) a student is able to advance to the next level within the medical
curriculum, 2) a student fails or passes, 3) remediation is required, whenever necessary, and 4)
the student has fulfilled all necessary requirements to be granted a Doctor of Medicine (MD)
February 2019
School of Medicine, EUC/Clinical Training Manual …. 9
degree. The University ensures that all students fulfill health care requirements required by
hospitals; and only assigns students to hospitals with academic qualifications consistent with the
demands of the clinical program provided by the hospital.
All hospitals have been carefully selected to ensure their facilities meet EUC’s standards. Each
affiliated hospital and clinic demonstrates a continuing commitment to medical education and
furnishes the necessary infrastructure to facilitate a successful clinical training program:
integrating medical students into the health care team, providing access to the library and other
ancillary facilities and supervising involvement with patients.
EUC follows the directives of the General Medical Council (GMC) publications The Doctor as
Teacher and Good Medical Practice, which outline what is expected of doctors with teaching
responsibilities, including those who supervise medical students. In alignment with the Principles
of Good Medical Education and Training, EUC adheres to the following principles:
Clinicians with responsibilities for teaching and training will be provided by EUC the
opportunity to improve and develop appropriate knowledge, skills, attitudes and behaviors
required for teaching medical students.
Medical students and clinical instructors will have appropriate teaching and learning
resources. These resources will be regularly reviewed and assessed.
Roles and Responsibilities for Clinical Training
EUC
EUC has a formal administrative and academic structure for facilitating the clinical training of its
medical students at its affiliated hospitals.
The Dean, in collaboration with the Deputy Dean and Chair, oversees and is responsible for the
Clinical Training (Clerkship) programs at EUC, School of Medicine. As such, they are not members
of any clinical training committee. The School council appoints a seven-member Clinical
Training Committee (CTC), who are all full-time faculty and Chairs of the Clinical Divisions (see
below) and the committee elects by majority a Chairman. (When available, senior faculty
members are selected as Chairs of the Clinical Divisions and the Chairman of the CTC). The
Chairs appoint by majority vote, two additional full-time faculty members (any rank). The Office
of the Dean can include additional full- or part-time faculty in the CTC, under special
circumstances.
The Clinical Training Committee
Oversees the planning of clinical training for all years of study
Assists the Dean in recruiting and assigning academic and clinical faculty in clinical training
Are the liaison between the clinical training sites and the faculty responsible for academic
program and course content (Hospital coordinators and Course Coordinators)
Ensures optimal cooperation between all affiliated persons and sites
Ensure appropriate training of scientific (clinical) collaborators and clinical instructors
Ensures optimal function of clinical training courses across all years of study
Ensures an environment of safe collaboration between the School and affiliated healthcare
sites
Assists the Dean in administrative, financial and other relevant obligations of the School of
Medicine related to the clinical training
Ensures that the learning objectives outlined for clinical training are achieved
Ensures accurate, complete and objective student evaluation

February 2019
School of Medicine, EUC/Clinical Training Manual …. 10
Works in collaboration with the academic and hospital coordinators, to solve any issues
that may arise up during clinical training
Oversees appropriate completion and evaluation of the logbooks
The medical program at EUC is comprised of 7 primary Divisions (5 of which are Clinical
Divisions), to which the courses and subjects are distributed. The Chairs of the Clinical
Divisions (Internal Medicine, Surgery, Child & Maternal Health, Social Medicine/Public
health/Primary Care, and Neuroscience/Mental Health/Sensory Systems) are full-time senior
faculty (Associate Professor or Professor) and are responsible for the overall academic content
and coordination of the courses taught in that Division. They oversee clinical program and
rotations at each affiliated hospital and ensure equality of training for EUC students across all
clinical training sites.
The Committee is comprised ex officio by the 5 Chairs / Directors of the Clinical Divisions. The
Chairs appoint by majority vote, two additional full-time faculty members (any rank). The CTC
reports to the Office of the Dean. The Chair of the Committee (Associate or Full Professor) is
determined by majority vote by the entire Committee.
1. Constantinos Tsioutis, Lecturer
2. Aris Angouridis, Lecturer
3. Theoklis Zaoutis, Professor
4. Gehardt Friehs, Professor
5. George Hadjigeorgiou, Lecturer
6. Anastasia Symeou, Special Scientist
7. Pantelis Trompoukis, Assistant Professor
8. Nikos Karpettas, Lecturer
February 2019
School of Medicine, EUC/Clinical Training Manual …. 11
Clinical training assistant
A clinical training assistant is appointed to assist the CTC in various matters regarding clinical
training coordination, including clinical training schedule preparation, communication with external
parties (including hospitals, clinical instructors and the Ministry of Health), student vaccination
forms, compensation of affiliated clinical sites and clinical instructors, on-site supervision of
student attendance, etc.
Clinical training Assistants: Mr. Charalambos Pittas
Ms. Ourania Antoniou
The Division Chairs work with heads of each course (Course Coordinators) taught in that
Division, who are also full-time faculty and coordinate the instruction of the course by full-time
faculty and scientific / clinical collaborators (part-time teaching faculty). Clinical Collaborators
are healthcare professionals who hold a medical specialization and a doctoral degree, as defined
by the EUC Charter. Posts of Scientific (Clinical) Collaborators are contractual for the duration of
one or two academic semesters, which may be renewed. The Council of School of Medicine
identifies the needs for positions, which are confirmed by the Dean in consultation with the Vice-
Rector of Academic Affairs and the Department of Human Resources. A Committee consisting
of Departmental Faculty members assesses the scientific qualifications and experience of each
candidate for each specific position/discipline and prepares a detailed report with supporting
documentation. Based on the Committee’s report, the final selection is made by the School
Council.
Clinical Divisions: Chairs & Chair Assistants
Internal Medicine
Chair: Constantinos Tsioutis, Lecturer
Chair Assistant: Aris Angouridis, Lecturer
Surgery
Chair: Adamantios Michalinos, Lecturer
Chair Assistant: Dimitris Ntourakis, Lecturer
Clinical Prof Pediatric Surgery, Andreas Neofytou
Child & Maternal Health
Chair: Theoklis Zaoutis, Professor
Chair Assistant: Zoi Pana, Lecturer (Child)
Chair Assistant: Clinical Assistant Prof. Andreas Stavroulis
Neuroscience, Mental Health & Sensory Systems
Chair: George Hadjigeorgiou, Lecturer
Chair Assistant: Prof. Gerhard Friehs
Social Medicine (Public Health & Primary Care)
Chair: Eirini Agapidaki, Lecturer
Chair Assistant: Anastasia Symeou, Special Scientist

February 2019
School of Medicine, EUC/Clinical Training Manual …. 12
Contact Information
Questions can be addressed to:
Eva Charalambous, Administrator
at E.Charalambous@euc.ac.cy
The clinical training organogram is shown in Appendix I.
Student Health and Safety Officer:
An Occupational medicine specialist, a General Physician or an Internist is appointed to oversee
health requirements and vaccinations of all students and keep record of any health issues that
might arise (eg.acute conditions that affect student attendance or performance). It is clear that the
Student Health and Safety Officer is not responsible for management of any acute or chronic
health conditions of the students of EUC.
Student Health & Safety Officer: Dr. Constantinos Tsioutis
Assistant Health & Safety Officer: Dr. Aris Angouridis
Nurse Assistant: Mr. Charalambos Pittas
Clinical Training Advisors
The Clinical Training Committee assigns full-time faculty members to serve as Clinical Training
Advisors to track each individual clinical student from year 4 through year 6 (semesters 7 – 12).
Each advisor ensures that all requirements are correct and complete, including: reviewing
evaluation, grades and graduation requirements and updating rotation schedules. Students must
maintain contact with their Clinical Training Advisor throughout their clinical terms until
graduation.
Clinical Training Advisors
1. Full-time faculty members, clinical doctors, assigned by Clinical Training Committee
2. Each advisor ensures that all requirements are correct and complete
3. Review evaluations, grades and graduation requirements and updating rotation schedules.
4. Students must maintain contact with their Clinical Training Advisor throughout their clinical
terms until graduation.

February 2019
School of Medicine, EUC/Clinical Training Manual …. 13
Affiliated Hospitals
The teaching cornerstone during the core clinical rotations is the close relationship between the
student and the attending physicians and/or residents who act as preceptors. Many hours are
spent in small group discussions involving students and their clinical teachers as during bedside
rounds. Together, they discuss the patient’s history, working diagnosis, management, progress,
etc. Students shadow their clinical instructors, to maximize their clinical exposure, while the clinical
teaching team at each site must ensure that all medical students are monitored at all times. The
roles and responsibilities of the affiliated hospital teaching staff and the clinical training
organogram are shown in Appendix I.
Hospital Coordinator of Clinical Education (HCCE)
Based on the qualifications, the provisions of the agreements signed between the hospitals and
the University and the recommendations of the hospital, EUC appoints for each affiliated hospital
/ clinic at least one local Hospital Coordinator of Clinical Education (HCCE) who is the hospital
administrator responsible for the EUC student program and is the liaison with the School of
Medicine. These designees may receive appointments to the School of Medicine’s faculty that are
commensurate with their qualifications and duties. A HCCE is on site at each clinical center and
affiliated teaching hospital, and is responsible for overseeing the EUC medical student program
at that health care site. Their principal role is to ensure quality and conformity with the EUC
guidelines as described in the CTM. This includes overseeing rotation schedules, and
determining the scope of student activities within the hospital / clinic. The HCCE reviews the
overall program with a Dean or Deputy Dean at the time of their visits to the hospital and has
continuous communication with the Clinical Training Committee and Department Clinical
Coordinator (see below).
Department Clinical Coordinator (DCC)
Each Clinical Department appoints a Department Clinical Coordinator (DCC), who works at
each respective hospital or clinic. The DCC is responsible administratively to the HCCE and
academically to the corresponding Division Chair and Course Coordinator at EUC, School of
Medicine. The DCC directly oversees the activities of the Clinical Instructors who teach students
at the bedside. The DCC is responsible for the optimal daily function of the clinical training of
students, completion of logbooks and student evaluation that take place in their department.
Clinical Instructors (CI)
The School of Medicine, in agreement with the HCCE and DCC, selects Clinical Instructors,
based on their academic and teaching credentials. The CI is directly responsible for the actual
bedside education of the medical students and for considering the student’s progress against
learning objectives set by the EUC clinical curriculum. The CI also determines the degree of
supervision required by each student. As such, CIs should provide such supervision personally
or arrange for its provision by one or more identified fully registered healthcare practitioners. While
the CI may determine that another doctor can oversee the student in certain context, the
responsibility for the student and their supervision ultimately remains with the CI. Following the
selection of clinical instructors, EUC organizes train-the-trainer programs aimed at familiarizing
CIs with the objectives and methods of clinical training.

February 2019
School of Medicine, EUC/Clinical Training Manual …. 14
EUC Medical Students Clinical Training
An essential feature of the clinical training consists of in-depth contact with patients. Students
take histories, examine the patient, propose diagnostic and therapeutic plans, record their
findings, present cases, perform minor procedures under supervision, attend all scheduled
lectures and conferences, participate in rounds with their peers and teachers, maintain a patient
log and study extensively about their patients’ diseases. In surgical departments, attendance in
the operating room is required. In special departments (eg. prenatal and postpartum clinics,
endoscopy units, etc.), attendance is mandatory; patients they are assigned to must be followed
through their different procedures.
A physician, nurse or other health care provider must be present in the room while students
examine patients. This is especially true for examinations of intimate body areas. Student orders
in the chart or electronic medical records must be authorized and countersigned by a physician.
Minor procedures may be performed on patients after adequate instruction has been given and
certification documented in the Student Logbook as permitted by hospital policy and governmental
regulations. Students working in hospitals are protected by liability insurance, which is carried by
EUC. Students must become familiar with the electronic medical record or patients’ charts and
know where to locate its individual components. Students are responsible for patient workups and
might also write daily progress notes as stipulated by the EUC clerkship curriculum and hospital
policy.
Students are expected to be on duty throughout the hospital workday, Monday through Friday.
Evening, weekend, and holiday on-call schedules may be the same or less than those for the
resident team to which the student is assigned, depending on the requirements of the EUC
curriculum. Student duty hours must take into account the effects of fatigue and sleep deprivation
on students’ education. Medical students are not required to work longer hours in patient care
than residents. Allowing for some modifications at different hospitals and for different cores, the
average workday or week should consist of approximately 50% patient care activities, 20%
conferences, lectures and/or preceptor sessions and about 30% academic time. . (Academic time
is used for students to prepare for case presentations, reports, etc.).
Students are given protected academic time for self-study and exam preparation before final
exams. While all clerkship directors must comply with this policy, they do have the option of
allowing additional time off for study.
Assignment of Students to Clinical Training Sites
The priority of EUC is to assure that all of our students are afforded an equal opportunity for high
quality clinical training. EUC considers all clinical training sites affiliated with the School of
Medicine equivalent in terms of the educational experiences they provide. Each student’s
placement in training sites and the rotation schedule is overseen by the Clinical Training
Committee, along with each student’s Clinical Advisor.
In order to start clinical training (clerkships) in years 4 - 6, students must:
1. Successfully complete all prerequisites according to the EUC School of Medicine
requirements.
2. Be in financial good standing.
February 2019
School of Medicine, EUC/Clinical Training Manual …. 15
3. Have cleared health requirements and immunizations (Y.Y.7.1.12 (12), Cyprus
Ministry of Health)
4. Be familiar with the Clinical Training Manual
Students are assigned to small groups (5-6 students) for their rotations. Within the department,
these groups may be further subdivided.
Exposure to both common conditions, as well as more complex cases is achieved by:
Evaluating the daily and weekly patient assignments
Encouraging resident shadowing
Rotation in inpatient, outpatient, special and emergency departments
The Clinical Training Committee in close collaboration with the Division Chairs and the Course
Coordinators devises a student allocation and schedule. The Clinical Training Committee
informs students of their hospital allocations and department rotation schedule. Students are also
advised on their obligations, rights, course objective and mode of evaluations. Required safety
measures are discussed and immunization records are examined.
The School is responsible for insurance coverage of the student against liability practice, as
required by the relative legislation, in all clinical training settings that are involved in the medical
studies of EUC.
Involvement of Students with Patients
Although the core of the student’s educational experience is with the patients that they are
assigned to, they will derive considerable benefit from exposure to other students’ patients and
by being present when attending’s or consultants see their own patients. Students must record
the patients they see into their logbook and have the encounter/procedure signed by the
supervising CI. The DCC reviews the patient encounter log continuously and when completing
the final clerkship evaluation form. The Office of the Dean and the EUC CTC also monitor the
logbooks to ensure that each student has fulfilled the minimum requirements during each
clerkship.
All students should be exposed to as many clinical situations as possible. Students shadow their
CI, assist them and prepare for the acquisition of the duties of a resident. Their CI should record
and sign student attendance and involvement in key clinical experiences. Students are expected
to follow up at least one patient every week from admission to discharge. Together with the
supervising doctor, they record admission data, perform physical examination, evaluate laboratory
and imaging findings, pose a diagnostic path, assess and prioritize the different problems of the
patient, discuss about further diagnostic and therapeutic choices, present the patient during
clinical rounds, update the daily report, and assist in the preparation of discharge documentations
(patient confidentiality at all times is preserved). Students should follow each patient daily on a
daily basis, be fully informed of the patients’ progress and actively participate with their team
members in the performance of various practical skills. It is important that all fields are completed
as requested, including skills or clinical conditions confirmation.
Students must remain compliant to guidelines by not using any patient identifiers, such as names,
initials, date of birth, medical record numbers, pictures and others. The rationale is that students
need to develop the clinical competencies required for graduation during their clinical years.
These competencies are assessed in various ways: by faculty observation during rotations, by
communication skills assessments, by completion of assignments and by clinical subject exams
(e.g. OSCEs). In order to develop many of these competencies and meet the objectives required
February 2019
School of Medicine, EUC/Clinical Training Manual …. 16
for graduation, the school needs to ensure that each student sees enough patients and an
appropriate mix of patients during their clinical terms.
One of the competencies that students must develop during their clinical training involves
documentation. Documentation is an essential and important feature of patient care and learning
how and what to document is an important part of medical education. Keeping an individual
student Logbook becomes a student training exercise in documentation. The seriousness and
accuracy with which students maintain and update their Logbook will be part of their assessment
during the core rotations. All of these features of documentation – seriousness, accuracy,
conscientiousness and honesty – are measures of professional behavior. Students should log
only encounters with real patients, and not simulated patients, case presentations, etc.
During their clinical training, all students are supervised by their clinical instructors, who note down
their observations in the individual student logbook. Student evaluation is described and
completed in the logbook, including student attendance, performance of clinical skills, and
essential course content observed and practiced. This is confirmed and signed by the clinical
instructor of the respective department. The Clinical Course coordinators inspect the Logbook
during and after each clinical training period.
Student Assessment
Students are assessed throughout their clinical training. Documentation of performance in
accordance with learning objectives and competencies, will be achieved with the application of
standardized assessment forms, such as mini-CEX, DOPS, etc. Logbooks document student
competence in mandatory clinical skills, in association with a defined clinical competency
roadmap.
1. Hospital Review
The Clinical Instructors and Department Clerkship Coordinators review and assess students’
logbooks as part of their mid-core and final assessment.
Clinical Faculty will be asked to evaluate students on the Student Clerkship Evaluation Form
(Appendix II).
2. EUC Review
The Clinical Training Committee and Clinical Advisors also review and assess students’
logbooks as part of the mid-core and final assessment. During the mid-core formative evaluation
they can comment on the completeness of the logbook and also ascertain whether students are
seeing a good mix of patients. Insufficient entries may impact the grade students receive. Students
are responsible to answer questions about the entries in their log. The clinical faculty and
departments can use data in the students’ logs to assess the quality of the program and the extent
to which it offers students an appropriate clinical experience.
By collecting, collating and analyzing logs from all students, EUC is able to:
a. To monitor and evaluate the clinical experience at different hospitals, so as to answer questions,
like “Have all of our students seen appendicitis? Have they all seen a patient with schizophrenia?
Do all our affiliated hospitals expose our students to end-of-life issues? Are all students involved
in communication with children and parents?” The ultimate aim is to document that all our
clinical training sites provide excellent and comparable clinical experiences.

February 2019
School of Medicine, EUC/Clinical Training Manual …. 17
b. To review the patient log of every clinical student, to identify those students that have gaps in
their clinical experience according to the criteria and objectives defined by the Division Chairs and
Course Coordinators for each course. The Clinical Training Committee and Clinical Advisors
will notify students identified and point out the deficiencies in their clinical experience. Students
will then be asked to remediate this deficiency.
The Logbook
The Logbook is a paper log used to document the competence of students in mandatory patient
encounters, clinical skills and procedures (Appendix III shows an example of a Clerkship Logbook
for Semester 8). Students must be certified in writing by a physician to perform these procedures.
The certification needs to be done only once and can be done on any service during any rotation.
Once certified, students can continue to perform these procedures without additional
documentation but always under supervision. As a requirement for promotion into the fifth and
sixth year, students must give their log with the appropriate signatures to their clinical coordinator.
All procedures performed by medical students must be done under faculty supervision.
At the end of each clinical training period, the student provides the School with a confidential
feedback form (see Appendix V). This aims to highlight the strengths of the clinical training
courses and to show areas in need of improvement.
Following completion of their clinical training and the logbook, the student submits the logbook to
the School Administration for evaluation by the academic clinical course coordinators. To confirm
completion of the clinical training, the logbook has to be sufficiently completed, the number of
absences for each course should be within allowed limits and the minimum successful grade
should be achieved in each respective course.
Clinical Instructors Role in Student Logbook Monitoring
The individual student logbook, as defined by each clinical training course, aims to provide brief
instructions on the learning objectives, expected outcomes and level of clinical exposure required.
Essential parts of the logbook include:
Patient assignment
Each student is expected to follow at least one patient every week from admission to discharge.
When you are satisfied that the student has reached a competent standard, you should complete
and sign the relevant entry.
History, Physical examination, Clinical skills, Essential course content
Students should be exposed to competencies and trained on clinical skills to a maximum possible
degree. In addition, students should exhibit competence level in situations commonly encountered
in the different clinical departments. Please rate student level according and sign.
Mini Clinical Evaluation Examination form (mini-CEX)
The miniCEX is a 15-minute snapshot of how students interact with patients. Students should
perform this at least once in each department of their rotation, under your supervision, which you
are kindly requested to complete and sign.
Student Attendance and Evaluation
Attendance is mandatory for students, unjustified absences are not allowed and the clinical
instructor signs the attendance sheet of every student logbook routinely. Students that are absent

February 2019
School of Medicine, EUC/Clinical Training Manual …. 18
systematically, violate occupational rules or misconduct should be reported to the hospital
coordinators.
Student training
Depending on the year of study and course content, students are expected to be exposed to
competencies and trained on clinical skills to a maximum possible degree. Individual student
logbooks provide a detailed description of learning objectives for each course of clinical training
and fields that require completion by the clinical instructors.
Following and observing
Actions performed by the student, such as obtaining medical history, following patients or
shadowing residents, performing various skills and being exposed to core clinical content, should
be completed in the respective entry and evaluated accordingly as described in the student
logbook. The clinical instructors need to confirm and sign all relevant entries.
Evaluating Students
The Role of the Clinical Instructor is also essential in the final assessment and evaluation of every
student that has rotated through the department. As such, it is imperative that they complete and
confirm all relevant entries.
Feedback
All clinical instructors are asked to provide feedback at the end of the clinical rotations period.
Professional Conduct and Responsibility
Conduct Code
Students are expected to demonstrate dedication to acquiring knowledge, skills, both cognitive
and non-cognitive, and attitudes necessary to provide competent medical care. Students are
expected to be responsible for their medical education and take an active role in the planning of
their medical education. A student shall be dedicated to providing competent medical service with
compassion and respect for human dignity. In all instances, the student must maintain the dignity
of the person, including respect for the patient’s modesty and privacy.
Nondiscrimination: It is unethical for a student to refuse to participate in the Care of a person
based on race, religion, ethnicity, socioeconomic status, gender, age, or sexual preference. It is
also unethical to refuse to participate in the care of a patient solely because of medical risk, or
perceived risk, to the student.
Confidentiality: The patient’s right to the confidentiality of his or her medical record is a
fundamental tenet of medical care. The discussion of problems or diagnoses of a patient by
professional staff/medical students in public violates patient confidentiality and is unethical. Under
no circumstances can any medical record be removed from the institution, nor is photocopying of
the record permitted. For presentations or rounds, students are permitted to extract information.
Professional Demeanor: The student should be thoughtful and professional when interacting
with patients and their families. Students should maintain a neat and clean appearance, and dress
in attire that is generally accepted as professional by the patient population served.
Misrepresentation: A student should accurately represent themselves to patients and others on
the medical team, and clearly indicated that they are medical students.
Honesty: Students are expected to demonstrate honesty and integrity in all aspects of their
education and in their interactions with patients, staff, faculty and colleagues. Cheating, plagiarism

February 2019
School of Medicine, EUC/Clinical Training Manual …. 19
or assisting others in these acts will not be tolerated by EUC. The student must assure the
accuracy and completeness of his or her part of the medical record. Each student is bound to
know, understand and preserve professional ethics and has a duty to report any breach of these
ethics by other students or health care providers through the appropriate channels.
Consultation: Students should seek consultation and supervision whenever they believe that
their care of a patient may be inadequate because of lack of knowledge and/or experience.
Conflict of Interests: When a conflict of interest arises the welfare of the patient must always be
of highest priority. Gifts, hospitality or subsidies offered by medical equipment, pharmaceutical or
other manufacturers or distributors should not be accepted if acceptance would influence the
objectivity of clinical judgment.
Sexual Misconduct: The student will not engage in romantic, sexual or other nonprofessional
relationships with a patient, while the student is involved with the patient’s care. The student is
not expected to tolerate inappropriate sexual behavior on the part of other medical personnel or
patients.
Impairment: The student will not use alcohol or drugs in a manner that could compromise patient
care. The student is obligated to report persons of the health care team whose behavior exhibits
impairment or lack of professional conduct or competence or who engage in fraud or deception.
Criticism of Colleagues: It is unethical for a student to disparage without evidence the
professional competence, knowledge, qualification or services of a colleague to a review (judicial)
body, staff, students or a patient. It is also unethical to imply by word, gesture or deed that a
patient has been poorly managed or mistreated by a colleague without tangible evidence.
Professional relations among all members of the medical community should be marked with
civility.
The medical student will deal with professional, staff and peer members of the health team in a
cooperative and considerate manner.
Evaluation: Students are expected to respond to constructive criticism by appropriate
modification of their behavior. When evaluating faculty performance, students may not include
disparaging remarks, offensive language or personal attacks, and should maintain the same
considerate, professional tone expected of faculty when they evaluate student performance.
Disclosure: The patient must be well informed to make health care decisions. Information that
the patient needs for decision-making should be presented in terms the patient can understand.
If the patient is unable to comprehend, for some reason, there should be full disclosure to the
patient’s authorized representative.
Informed Consent: Students are to understand the importance of obtaining informed consent
from patients. However, students are not responsible for obtaining informed consent; it is the
physician’s responsibility.
Medical students who fail to maintain the highest degree of personal and professional integrity or
whose behavior is not in keeping with achieving both cognitive and non-cognitive skills will be
subject to review, disciplinary action and possible dismissal.

February 2019
School of Medicine, EUC/Clinical Training Manual …. 20
Attendance and Time-off Policies
Clinical rotations require a full-time commitment by students. The educational component of the
4
th
-6
th
years of medical studies consist of involvement with patient care as part of the healthcare
team, attendance at all didactic activities, completion of assignments and self-directed learning.
Students must be at the hospital at least five days a week with daily hours and night and weekend
on call as scheduled by the clinical curriculum.
Each daily absence from clinical training activities is considered one absence and is noted in the
Logbook. Unjustified absences, violation of occupational rules, professional misconduct or student
engagement in activities other than those described in the curriculum, are to be inquired by the
academic coordinator of the School of Medicine, EUC. Students are entitled up to three (3) justified
absences for each course during the semester. In case of justified discontinuation of the clinical
training, the student is obliged to complete the remaining period of clinical training in a new
position.
If a student must be absent for a few hours or a day, permission must be obtained by the HCCE
and/or DCC before leaving. Longer absences from a rotation without permission from the clerkship
coordinator, DCC/HCCE and the Clinical Training Committee can be grounds for failure in that
rotation. Absenteeism and/or tardiness can result in an “F” in professional behavior and loss of
credit for any rotation.
Student Health and Safety
Compliance with health and safety measures is necessary for the proper function of clinical
training. These measures concern safety of students, of healthcare workers, of patients and their
chaperones.
When concerned over a safety issue or an incident, students should contact their CI, DCC and/or
HCCE. In case of personal safety issues, such as injury or exposure, students should also
immediately contact the CTC, either directly or through the Health and Safety Officer.
The student Logbook contains details on student safety matters. In addition, the Clinical Practice
Incidence Report Form (Appendix IV) should be completed and submitted to the School, in case
of any incidence concerning student safety.
Immunization requirements
Before entering the clinical training and in order to approve their entry in healthcare settings,
students should conform to the immunization requirements set by the Ministry of Health.
(Appendix V)
Hand hygiene and isolation precautions
Standard precautions and Hand hygiene are performed before and after contact with all
patients. Indications and technique for hand hygiene follow the World Health Organization
guidelines.

February 2019
School of Medicine, EUC/Clinical Training Manual …. 21
Isolation precautions, personal protective equipment are additional measures that depend
on the risk of transmission between patients and healthcare personnel (i.e. contact, droplet, and
airborne precautions).
Gloves are worn for invasive procedures, contact with non-intact skin, mucous
membranes, or sterile sites, and at all activities that carry risk of exposure to body fluids or
contaminated instruments.
Safe use and disposal of sharps
Incidents with sharps injuries can be prevented with basic practices:
Do not pass sharps directly from hand to hand
Always discard in appropriate sharps container immediately after use
Do not break or bend needle
Container should be kept within arms’ length during use
Do not attempt to replace cap
Assessment of Training Sites
Administrative and academic members of EUC perform site visits of each affiliated hospital or
clinic on a regular basis. The purpose of these visits is to ensure compliance with School of
Medicine standards, the clinical training curriculum and policies, to review the educational
program and to discuss any problems that arise on site. The coordinators document the important
features of the clerkship including the strengths and weaknesses of the program, feedback to the
Clinical Training Committee and suggestions for the future.
Student Evaluations of Clinical Training
The university uses a questionnaire to collect student feedback on the core rotations. These
questionnaires are in Appendix VI and will be sent to students automatically after the clerkship is
over. Each division may modify the questionnaire to measure the extent that a specific clerkship
rotation meet the departmental guidelines and objectives. Data from these questionnaires
provides documentation, enabling the Deans, Department Chairs, HCCEs, DCCs and CIs to
monitor and improve the educational program in each clerkship at each hospital based on student
experience and opinion.
An aspect of professional behavior requires a commitment to improve the medical school. Given
the importance of student feedback, the school of medicine only gives students credit for a core
rotation and access to their evaluation after completion and submission of the relevant
questionnaire. Answers are confidential. While our program can ascertain how many students
responded, it cannot match a response to an individual student.

February 2019
School of Medicine, EUC/Clinical Training Manual …. 22
PART II
Clinical Training Curriculum
EUC Curriculum
The innovative six-year curriculum at the European University of Cyprus is fully integrated both
horizontally (systems-based) and vertically (spiral-design) in three educational phases.
Phase I: Foundations of Medicine (years 1-2)
Phase II: Foundations of Clinical Practice (year 3)
Phase III: Clinical Medicine Core (years 4-6)
Horizontal integration brings together the various disciplines (e.g. Anatomy, Histology,
Embryology, Physiology, Biochemistry) for each module, whereas vertical integration is aimed at
bringing together basic and clinical sciences, to break the traditional divide between preclinical
and clinical studies. As such, the knowledge presented in the basic sciences is placed in clinical
context, as well as in context of professional practice. The overall aim is to enhance the
acquisition of knowledge, skills, attitude, values and professionalism in our students. The
interdisciplinary units in the Foundations of Medicine phase of the curriculum use a
multidisciplinary, systems-based, horizontally integrated approach to teach the normal structure
and function of the body, along the continuum from molecules-to-cell to entire functional systems.
During this process, students are also introduced to basic clinical skills, and abnormalities in
structure and function, when appropriate. The disciplines (Cell & Molecular Biology, Biochemistry)
and (Anatomy, Histology-Embryology, Physiology, Biochemistry) are integrated and organized
into modules based on foundational concepts or on organ systems. The teaching of
communication skills is also fully integrated alongside and introduction to the demands of
professional practice and care.
Vertical integration is achieved by the early introduction to clinical skills, thinking and clinical
reasoning. Each module is closed with a session designed to reinforce the basic knowledge
acquired and integrate that knowledge with its clinical significance. Clinicians present clinical
association lectures and interactive sessions. Students are introduced to clinical thinking by
applying their basic science knowledge to solve clinical problems and case-based sessions.
The reformed Structure and Function curriculum at EUC engages multiple active and
cooperative learning strategies. Innovated and web-based educational resources have
been tightly intercalated in the revised Structure & Function program. In the functional component,
interactive anatomy, histology and embryology programs are regularly applied to provide insight
into three-dimensional associations. In the structural component, virtual labs allow students to
gain the experience of practical experiment without bench work in an interactive platform. Digital
labs as a simulated model of the wet lab parallel our intensive integration of using high fidelity
simulators for the physiology, pathophysiology, semiology and surgery practical sessions, among
others. Simulation as one of the most prominent innovations in medical education over the last
decade is a pivotal component of the structure & functional practical sessions.
The EUC Medical Curriculum is designed to also facilitate the development of primary
competencies in our students, as defined by the Accreditation Council for Graduate Medical
Education (ACGME). The clinical years of the EUC curriculum aim to transform students who

February 2019
School of Medicine, EUC/Clinical Training Manual …. 23
have learned basic sciences into students who can deal with patients and their problems in a
hospital or outpatient milieu. To do this, numerous new clinical skills, professional behaviors and
considerable medical knowledge must be added to that which the student has previously acquired,
which is based on the learning objectives of their clinical courses and the clinical competencies
roadmap of the School of Medicine..
Clinical Training Spiral
1st year – Foundations of Medicine I are taught in modules that cover traditional synergies
related to understanding the Structure and Function of the human body from molecules to cells
(e.g. cell biology, biochemistry, genetics), as well as medical information (epidemiology,
biostatistics) in the first term and the basic structural components of the human body (anatomy,
physiology, histology, embryology, biochemistry) in the second term. Students are given their first
introduction to clinical practice in «Clinical Practicum».
2nd year – Foundations of Medicine II are taught in modules that cover traditional synergies
related to understanding the structure and function of the human body (anatomy, physiology,
histology, embryology, biochemistry) that is organized in primary body systems (cardiovascular,
pulmonary, renal reproductive and nervous). Instruction of basic clinical skills are promoted via
the course and practicum in «Introduction to Clinical Skills», as well as by the use of simulated
scenarios.
3rd year – Foundations of Clinical Practice focus is on pathophysiology, formation of differential
diagnoses, semiology, pathology and pharmacotherapy that is also organized in body systems
over the course of the year. Basic clinical skills are further promoted via simulation. Students are
also introduced to general surgery, immunology and microbiology.
4th-6th years – Clinical Medicine Core forms the final turn of curriculum spiral, with the
translation of knowledge and skills into practice, during clinical clerkships.
Themes such as medical ethics, family medicine, public health, etc. span all years and are
threaded throughout the basic modules and clinical clerkships.
The curriculum of the School of Medicine, European University Cyprus (EUC) is of total duration
of 5685 hours and includes theoretical and clinical training, according to the European Directive
2013/55/EU of the European Council. Students’ clinical training is an integral part of their
education, of total duration of more than 2200 hours. Clinical training takes place in pre-
determined sites of the public and private sector, following appropriate planning.
The overall objectives of the clinical training of medical students are:
To familiarize students with the structure, function and capacities of the healthcare system
To develop clinical skills and successfully combine them with their theoretical knowledge
To demonstrate and develop communication skills and teamwork
To apply practical skills in real-life healthcare environments
To develop professionalism in their daily clinical practice
To establish the concept of clinical training during medical undergraduate studies
To create an environment of mutual collaboration and develop ongoing relations between
the School of Medicine and the collaborating healthcare sites
Finally, to equip medical graduates with all necessary practical skills to pursue their
postgraduate endeavors
The Clinical Training Curriculum

February 2019
School of Medicine, EUC/Clinical Training Manual …. 24
This comprises Years of study 4-6 (Semesters 7-12) and consists of the following courses:
Core Rotations
ECTS
Weeks
Clinical Training I
(Respiratory & Cardiovascular)
15
6
Clinical Training II
(Digestive System & Hematology)
15
6
Clinical Training III
(Infectious Diseases and Clinical Microbiology)
9
3
Clinical Training IV
(Endocrine system, Uro-Nephrological System & Male
Genital Tract)
14
6
Clinical Training V
(Musculoskeletal System)
7
6
Clinical Training VI
(Nervous System & Psychiatry)
15
6
Clinical Training VII
(Pediatrics)
12
5
Clinical Training VIII
(Dermatology)
6
2.5
Clinical Training IX
(Obstetrics & Gynecology)
8
3
Clinical Training X
(Ophthalmology)
6
2.5
Clinical Training XI
(Otorhinolaryngology)
5
2.5
Clinical Training XII
(ER, Toxicology, Oncology & Palliative Care)
14
5
Additional Requirements
Diagnosis by Imaging
7
2
Clinical Bioethics & Legal Medicine
6
2
Medical Therapeutics
6
1.5
Symptoms & Interpretation Of Complementary Examination
Procedures
5
1.5
Primary Care
6
3
Electives
Healthcare Management
Clinical Embryology
Rehabilitation Medicine

February 2019
School of Medicine, EUC/Clinical Training Manual …. 25
Research Methods & Scientific Writing
Interventional Radiology
Competencies
The US Accreditation Council on Graduate Medical Education (ACGME) defines six domains
thought to be useful in defining “competency”; these are called the core competencies -
patient care, medical knowledge, practice-based learning and improvement, professionalism,
systems-based practice, and interpersonal skills and communication. While these were initially
developed for residency programs, today competencies are used at many levels of professional
practice to define and measure an individual’s ability and capability. EUC has devised a
Clinical Competence Building Roadmap to guide both instructors and students during their
clerkships. (Appendix VII)
The American Association of Medical Colleges (AAMC) has grouped competencies into the
following 13 Entrustable Professional Activities (EPAs) as a basis for starting postgraduate
training in the US.
Entrustable Professional Activities
1. Gather a History and Perform a Physical Examination
2. Prioritize a Differential Diagnosis Following a Clinical Encounter
3. Recommend and Interpret Common Diagnostic and Screening Test
4. Enter and Discuss Orders/Prescriptions
5. Document a Clinical Encounter in the Patient Record
6. Provide an Oral Presentation of a Clinical Encounter
7. Form Clinical Questions and Retrieve Evidence to Advance Patient Care
8. Give or Receive a Patient Handover to Transition Care Responsibility
9. Collaborate as a member of an Interprofessional Team
10. Recognize a Patient Requiring Urgent or Emergent Care, & Initiate Evaluation & management.
11. Obtain Informed Consent for Tests and/or Procedures
12. Perform General Procedures of a Physician
13. Identify System Failures and Contribute to a Culture of Safety and Improvement.
The emphasis of the EUC curriculum is on achieving and demonstrating competency. Student
confidence in performing practical and clinical skills in different levels of their studies, is assessed
by using a student questionnaire (Appendix VIII).

February 2019
School of Medicine, EUC/Clinical Training Manual …. 26
Outcome Objectives
Medical Knowledge
1. Apply the multidisciplinary body of basic sciences to clinical analysis and problem solving using:
The knowledge of normal structure, function, physiology and metabolism at the levels of
the whole body, organ systems, cells, organelles and specific biomolecules including
embryology, aging, growth and development.
The principles of normal homeostasis including molecular and cellular mechanisms.
The etiology, pathogenesis, structural and molecular alterations as they relate to the signs,
symptoms, laboratory results imaging investigations and causes of common and important
diseases.
2. Incorporate the impact of factors including aging, psychological, cultural, environmental, genetic,
nutritional, social, economic, religious and developmental on health and disease of patients as
well as their impact on families and caregivers.
3. Utilize the important pharmacological and non-pharmacological therapies available for the
prevention and treatment of disease based on cellular and molecular mechanisms of action and
clinical effects. Identify and explain factors that govern therapeutic interventions such as clinical
and legal risks, benefits, cost assessments, age and gender.
4. Apply the theories and principles that govern ethical decision making in the management of
patients. v. Evaluate and apply clinical and translational research to the care of patient
populations.
Clinical Skills
1. Communicate effectively with patients, their families and members of the health care team.
2. Obtain a comprehensive and/or focused medical history on patients of all categories.
3. Perform physical and mental status examinations on patients of all categories appropriate to the
patient’s condition.
4. Document pertinent patient health information in a concise, complete and responsible way.
5. Select appropriate investigations and interpret the results for common and important diseases
and conditions.
6. Recognize and communicate common and important abnormal clinical findings.
7. Develop a problem list and differential diagnosis based on the history, physical findings and initial
investigations.
8. Apply effective problem solving strategies to patient care.
9. Perform routine and basic medical procedures.
10. Provide patient education for all ages regarding health problems and health maintenance.
11. Identify individuals at risk for disease and select appropriate preventive measures.
12. Recognize life threatening emergencies and initiate appropriate primary intervention.
13. Outline the management plan for patients under the following categories of care: preventive,
acute, chronic, emergency, end of life, continuing and rehabilitative.
14. Continually reevaluate management plans based on the progress of the patient’s
condition and appraisal of current scientific evidence and medical information.

February 2019
School of Medicine, EUC/Clinical Training Manual …. 27
Professional Behavior
1. Establish rapport and exhibit compassion for patients and families and respect their privacy,
dignity and confidentiality.
2. Demonstrate honesty, respect and integrity in interacting with patients and their families,
colleagues, faculty and other members of the health care team.
3. Be responsible in tasks dealing with patient care, faculty and colleagues including health- care
documentation.
4. Demonstrate sensitivity to issues related to culture, race, age, gender, religion, sexual orientation
and disability in the delivery of health care.
5. Demonstrate a commitment to high professional and ethical standards.
6. React appropriately to difficult situations involving conflicts, nonadherence and ethical dilemmas.
7. Demonstrate a commitment to independent and lifelong learning including evaluating research in
healthcare.
8. Demonstrate the willingness to be an effective team member and team leader in the delivery of
health care.
9. Recognize one’s own limitations in knowledge, skills and attitudes and the need for asking for
additional consultation.
10. Participate in activities to improve the quality of medical education, including evaluations of
courses and clerkships.
Assessment and Grading
The Course Coordinator must arrange for formative mid-core assessments of all students in order
to discuss the student’s performance including a review the Patient Encounter Logbook. These
consist of individualized face-to-face meetings with each student. This assessment may entail
consultations with the DCC and CIs at each respective clinical training site. The purpose of this
assessment is to verbally provide students with qualitative feedback early enough in the clerkship
to allow time for remediation of deficiencies. This meeting gives the Course Coordinator an
opportunity to help students recognize their strengths. This discussion should include
encouragement if the student is doing well or a warning with constructive criticism if the student
is doing poorly. The mid-core assessment also gives medical students the opportunity to measure
their progress in learning. Comments in the mid-core might be integrated in to the final evaluation.
Grading Policy for the clerkships
The Course Coordinator completes a final assessment form for each student in a core clerkship.
The form requires narrative comments, grades in individual components and a final summative
grade. The narrative comments summarize the student’s clinical performance and,
importantly, professional behavior. This includes attendance, rapport with patients and staff and
the extent to which the students developed the required competencies for that core. This narrative
section offers the faculty the opportunity to provide additional personalized evaluative
information beyond the letter grade.
An additional section allows for constructive comments. Students should make every effort to
review these comments as soon as possible after completion of a rotation. The opinions of the
physicians who have worked with a student are critical for self-improvement by the student. In
particular, constructive criticisms can help a student develop into a more competent physician.
The final grade in the clerkship represents a semi-quantitative average of following components:
February 2019
School of Medicine, EUC/Clinical Training Manual …. 28
1. Medical knowledge
50%
4. Clinical & Communication skills
40%
5. Attendance & Professional behavior
10%
Grading System:
Letter Grade Grade Meaning
Grade Points
Percentage Grade
A Excellent
4.0
90 and above
B+ Very Good
3.5
85-89
B Good
3.0
80-84
C+ Above Average
2.5
75-79
C Average
2.0
70-74
D+ Below Average
1.5
65-69
D Poor
1.0
60-64
F Failure
0
I Incomplete
0
W Withdrawal
0
P Pass
0
AU Audit
0
Components of Assessment (in Addition to Written Examinations)
Clinical Performance
The teaching physicians who work with the student during the rotation assess the student’s clinical
performance in three areas, which carry 20% of the grade. The more feedback the CC gets from
different members of the medical staff that instructed the student, the more objective grades can
be. The faculty assesses the extent to which the student has developed the competencies
required for that rotation. These specific competencies appear in Section II of this manual in
the curriculum for each of the core clerkships. The following general goals form the basis of all
assessments.
Medical Knowledge includes the knowledge of basic, clinical and social sciences; the
pathophysiology of disease; the clinical signs, symptoms and abnormal laboratory findings
associated with diseases and the mechanism of action of pharmaceuticals.
Clinical Skills includes diagnostic decision making, oral and written case presentations, history
and physical examination, test interpretation and therapeutic decision-making. Students must be
observed and evaluated at the bedside.
Professional Behavior include the interaction with staff and patients, integrity, sensitivity to
diversity, attendance and a commitment to lifelong learning and independent study.
Communication Skills “as they relate to physician responsibilities, including communication with
patients, families, colleagues, other health professionals and resolution of conflicts.”

February 2019
School of Medicine, EUC/Clinical Training Manual …. 29
OSCEs
An objective structured clinical examination (OSCE) is designed to test clinical skill performance
and competence in skills such as communication, clinical examination, medical procedures /
prescription, exercise prescription / joint mobilization / manipulation techniques / radiographic
image evaluation / interpretation of results, etc. It is a hands-on, real-world approach to learning
that keeps examinees engaged, allows them to understand the key factors that drive the medical
decision-making process, and challenges the professional to be innovative and reveals their errors
in case-handling and provides an open space for improved decision-making, based on evidence-
based practice for real-world responsibilities.
An OSCE usually comprises a circuit of short (the usual is 5–10 minutes although some use up
to 15 minute) stations, in which each candidate is examined on a one-to-one basis with one or
two impartial examiner(s) and either real or simulated patients (actors or electronic patient
simulators). Each station has a different examiner, as opposed to the traditional method of clinical
examinations where a candidate would be assigned to an examiner for the entire examination.
Candidates rotate through the stations, completing all the stations on their circuit. In this way, all
candidates take the same stations. It is considered to be an improvement over traditional
examination methods because the stations can be standardized enabling fairer peer comparison
and complex procedures can be assessed without endangering the patient’s health.
As the name suggests, an OSCE is designed to be objective – all candidates are assessed using
exactly the same stations (although if real patients are used, their signs may vary slightly) with the
same marking scheme. In an OSCE, candidates get marks for each step on the mark scheme
that they perform correctly, which therefore makes the assessment of clinical skills more objective,
rather than subjective, structured – stations in OSCEs have a very specific task. Where simulated
patients are used, detailed scripts are provided to ensure that the information that they give is the
same to all candidates, including the emotions that the patient should use during the consultation.
Instructions are carefully written to ensure that the candidate is given a very specific task to
complete. The OSCE is carefully structured to include parts from all elements of the curriculum
as well as a wide range of skills. A clinical examination - the OSCE is designed to apply clinical
and theoretical knowledge. Where theoretical knowledge is required, for example, answering
questions from the examiner at the end of the station, then the questions are standardized and
the candidate is only asked questions that are on the mark sheet and if the candidate is asked
any others then there will be no marks for them. Grading in OSCEs is done by the examiner.
Occasionally written stations, for example, writing a prescription chart, are used and these are
marked like written examinations, again usually using a standardized mark sheet. One of the ways
an OSCE is made objective is by having a detailed mark scheme and standard set of questions.
For example, a station concerning the demonstration to a simulated patient on how to use a
metered dose inhaler [MDI] would award points for specific action, which are performed safely
and accurately. The examiner can often vary the marks depending on how well the candidate
performed the step. At the end of the mark sheet, the examiner often has a small number of marks
that they can use to weight the station depending on performance and if a simulated patient is
used, then they are often asked to add marks depending on the candidates approach. At the end,
the examiner is often asked to give a "global score". This is usually used as a subjective score
based on the candidates overall performance, not taking into account how many marks the
candidate scored. The examiner is usually asked to rate the candidate as pass/borderline/fail or
sometimes as excellent/good/pass/borderline/fail. This is then used to determine the individual
pass mark for the station. (Appendix IX)
February 2019
School of Medicine, EUC/Clinical Training Manual …. 30
Clinical Evaluation Exercise (MiniCEX)
EUC incorporates the Clinical Evaluation Exercise (miniCEX) with the Logbook framework in order
to assess clinical skills, attitudes and behaviors in the secondary care setting. By providing a
short snapshot of how students interact with patients in a secondary care setting, it is used as an
effect tool to collect evidence on competency attainment. The miniCEX is overseen by the clinical
supervisor and may be observed by a staff doctor, nurse practitioner, consultant or other.
The MiniCEX is intended to facilitate formative assessment of core clinical skills in 10- to 20-
minute direct observation assessment of student-patient interactions. The observations are
documented in the Logbook. The aim, ultimately, is to guide learning and improve performance
through structured feedback from the clinical instructors. Particular emphasis is place in areas
such as communication, history taking, physical examination and professional practice.
Each mini-CEX focuses on specific aspects of the clinical encounter, including:
History taking
Medical interviewing skills
Physical examination skills
Professional qualities
Counseling skills
Clinical judgment
Organization and efficiency
Inadequate Performance
An F in any area requires a discussion between the student and the clinical coordinator, Division
Chair, Course Coordinator, Chair and/or a Dean. Students who fail the entire year, not just a
course/rotation, will be recommended for dismissal. In addition, the University reserves the right
in the absence of due process or under ambiguous circumstances to put an I Grade (incomplete)
notation on the transcript. In this case, the student must repeat the course/rotation.
A student can be given credit for a rotation if there is an F in any one area as long as the final
grade is passing. The university will not approve this student for graduation until the successful
completion of remediation. An F in any area requires a discussion between the student and the
clinical coordinator, Division Chair, Course Coordinator, Chair and/or a Dean. Students who fail
the entire year, not just a course/rotation, will be recommended for dismissal. In addition, the
University reserves the right in the absence of due process or under ambiguous circumstances to
put an I Grade (incomplete) notation on the transcript. In this case, the student must repeat the
course/rotation.
A formal mechanism exists for identifying and helping a student whose achievement is not up to
standard. If CI or DCC judge a student to be marginal, the Course coordinator is notified. The
student shall be informed as early as possible during the clerkship and given assistance and
counseling. Depending on the seriousness of the problem, the division coordinator, and Dean
may be involved.
Thus, a three-tiered system for dealing with student problems exists at all clinical sites. Initially a
student’s CI and/or DCC discuss a student’s behavior or attitude with the student. This is done at
the time of the mid-core assessment or at any other time that is appropriate. Many times
counseling the student is sufficient. If the problem recurs, a pattern develops or a single problem
appears serious, the HCCE is notified. The HCCE might meet with and counsel the student. If
the problem is serious enough, the HCCE notifies the Clinical Training Committee and Deans’
office. The Dean of the School of Medicine has the ultimate responsibility for dealing with
students’ problems.

February 2019
School of Medicine, EUC/Clinical Training Manual …. 31
EUC Core Clinical Training Clerkships
Clinical Training I (MED407) Respiratory & Cardiovascular
Description
Students shadow residents and consultants in departments of pulmonology, cardiology,
thoracic surgery and vascular surgery. They are assigned to patients, whom they follow
from admission to discharge and act as attending physicians, under the supervision of
their clinical instructors. The overall objective of this rotation is for students to familiarize
with the responsibilities of physicians, including obtaining history, performing physical
examination, performing differential diagnoses, proposing investigation and management
plans, observing patients’ daily progress, completing medical charts and discharging.
The objective of the course is to familiarize students with
The clinical manifestations, diagnosis, medical and surgical management and
prevention of the diseases of the cardiovascular and respiratory system
Course Content
Most frequently encountered pathologies of the immune system
Inflammatory reactions, hypersensitivity reactions, autoimmune diseases and other
pathologies relevant to the immune system..
Most frequently encountered pathologies of the respiratory system.
Respiratory insufficiency, obstructive and restrictive syndromes, lung tumors, pleural
pathology, mediastinal pathology and other pathologies that are relevant to the
respiratory system
Most frequently encountered pathologies of the cardiovascular system
Cardiac arrhythmias, thoracic pain, acute coronary syndrome, cardiac insufficiency,
syncope, shock, valvulopathies, ischemic syndromes, venous alterations and arterial
hypertension, edematous syndromes, pericardial pathologies and other relevant
cardiovascular pathologies.
Methods of diagnosis (history, physical examination and laboratory tests) of the above
diseases and conditions
Medical and surgical treatment and prevention of the above diseases and conditions
Guidelines
Length: 4 weeks
Site: cardiology department, respiratory department, outpatient clinic, bronchoscopy unit,
spirometry, interventional cardiology unit, echo unit, ambulatory care unit, emergency
department, cardiology/cardiosurgery ICU, medical ICU, private office practice, additional
sites, as available.
Orientation: At the start of the clerkship an orientation is given. The clerkship director or
designee discusses the program’s goals and objectives, the responsibilities of the student,
the schedule and assignments to preceptors and residents. The student is introduced to
the key preceptors and staff members in the department.
Schedule: The student must attend scheduled clinical conferences, grand rounds,
morning visits, classes, subspecialty conferences, learning sessions.
Attending Rounds: The student is involved in all patient care activities in the outpatient
facility and inpatient unit.
Preceptor sessions: A preceptor meets with students daily. The preceptor sessions will
include clinical discussions that focus on problem solving, decision making and adherence
to bioethical principals.

February 2019
School of Medicine, EUC/Clinical Training Manual …. 32
Assessment
Grade Components
Medical knowledge 50%
Clinical & Communication skills 40%
Attendance & Professional behavior 10%
Educational Objectives
Upon successful completion of this course students should be able to:
Identify the most frequent pathologies of the immune system
Diagnose the most frequent pathologies of the immune system: obtaining a clinical history
and carrying out a physical examination focused on the pathology of the immune system,
indications and interpretation of the principal complementary diagnostic tests (basic
analytical immunology, cutaneous tests, histocompatibility studies, imaging and
anatomopathological tests, etc).
Manage the clinical treatment of most frequently encountered pathologies of the immune
system.
Identify the most frequently encountered pathologies of the respiratory system.
Diagnose the most frequently encountered diseases of the respiratory system by
obtaining a past clinical history with focus on the respiratory pathology, physical
respiratory examination (respiratory auscultation, percussion, inspection, palpation, etc),
indications for and interpretation of the principal complementary tests for diagnosis
(spirometry, gasometry, arterial blood gasses) clinical laboratory tests, imaging,
anatomopathological tests, etc.
Manage the medical-surgical treatment of the most frequent diseases of the respiratory
system.
Identify the most frequent cardiocirculatory pathologies
Diagnose the most frequent cardiocirculatory pathologies by obtaining a past clinical
history with focus on cardiovascular pathology, physical cardiovascular examination
(cardiac auscultation, taking pulses and arterial pressure, assessment of edemas, etc),
indications and interpretation of the principal complementary tests for diagnosis
(electrocardiograms, stress tests, clinical laboratory tests, imaging, anatomopathological
tests, etc).
Manage the medical-surgical treatment of the most frequently encountered diseases of
the cardiovascular system.
Medical Knowledge
Demonstrate knowledge of the principal syndromes and illnesses, their underlying causes
both medically and socially and the various diagnostic and therapeutic options available
to physicians in the care of their patients.
Demonstrate knowledge of the indications for and the ability to interpret standard
diagnostic tests, e.g.; CBC, chemistries, chest x-rays, urinalysis, EKGs, as well as other
relevant specialized tests.
Recognize unusual presentations of disease in elderly patients and demonstrate
understanding of the complexity of providing care for the chronically ill with multiple
medical problems. This should include an understanding of end of life issues, as well as
bioethical, public health and economic considerations, which arise in our health care
system.
Demonstrate knowledge of the indications for various levels of care post-discharge, e.g.,
short and long term rehabilitation, long-term skilled nursing facility care, hospice, home
care, etc.

February 2019
School of Medicine, EUC/Clinical Training Manual …. 33
Clinical Skills
Take a comprehensive history and perform a complete physical exam. Formulate a
comprehensive problem list, differential diagnosis; and articulate a basic therapeutic plan,
employing concern for risks, benefits, and costs.
Analyze additional clinical information, lab tests and changes in patients’ clinical status;
note changes in the differential diagnosis or in the diagnostic or therapeutic plans as
circumstances and test results change. Begin to develop proficiency in basic procedures,
such as venipuncture, arterial puncture, nasogastric tube insertion, insertion of intravenous
lines, urinary bladder catheterization, etc.
Clinical examination, including recognition of common signs of cardiovascular
diseases: skin and mucosa, murmurs, lung auscultation, assessment of volume status
and peripheral vasculature
Common cardiovascular disorders (see Part D): recognition, evaluation, diagnosis,
management
Differentiation between respiratory and heart disorders
ECG performance and interpretation
History taking and focus on pulmonary risk factors, family history, social and
occupational history
History taking and focus on cardiovascular risk factors, family history, and social history
Arterial blood gases and acid-base balance: obtaining and evaluation
Clinical examination, including recognition of common signs of respiratory diseases:
skin and mucosa, lung auscultation findings, lymphadenopathy
Common respiratory disorders (see Part D): recognition, evaluation, diagnosis,
management
Differentiation between respiratory and heart disorders
Spirometry evaluation
Arterial blood gases
Blood culture
Blood glucose examination using finger stick
Blood transfusion
Hand washing (including surgical scrubbing)
Intramuscular injection
Intravenous injection
Nasogastric tube placement
Oxygen supplementation
Peripheral venous catheter placement
Rectal examination
Respiratory secretions culture
Setting up syringe driver
Skin suturing
Skin swabs for culture
Subcutaneous injections
Suction of respiratory secretions
Swabs from nose, throat and skin
Urinary catheter insertion, female
Urinary catheter insertion, male
Urinary catheter removal
Urinalysis using urine stick
Vein puncture and blood drawing
Wound care and basic wound dressing

February 2019
School of Medicine, EUC/Clinical Training Manual …. 34
Communication Skills
Verbal:
Basic competence in comprehensive case presentation
Basic competence in focused case presentation
Basic competence in explaining to a patient a simple diagnostic and therapeutic plan
Basic informed consent scenario for a procedure
Written:
Competence in comprehensive case write-ups
Competence in brief case write-ups
Professional Behavior
Demonstrate a regimen of independent learning through the reading of suggested basic
texts, research via the Internet and through other electronic resources, maintenance of the
patient encounter log and completion of the web-based educational program
requirements.
Demonstrate a commitment to quality, patient safety and self-directed improvement.
Demonstrate competency and comfort in dealing with people of varying racial, cultural
and religious backgrounds
Demonstrate a commitment to treating all patients, families and other caregivers with
respect.
Participate fully with the patient care team and fulfill all responsibilities in a timely fashion.
Maintain a professional appearance and demeanor.
Demonstrate facility in working in concert with other caregivers, nutritionists and
social workers / discharge planners to obtain optimal, seamless multidisciplinary care
for their patients, both during the hospitalization and after discharge.
Core Topics & Patients
Students should make every effort to see patients with conditions listed below. This list is based
on “Training Problems “published by the Clerkship Directors of Internal Medicine.
A. The healthy patient: health promotion and education, disease prevention and screening.
B. Patients with a symptom, sign, abnormal laboratory value or known medical condition
1. Acute coronary syndrome
2. Acute pulmonary edema
3. Angina - Chest pain
4. Arrhythmia (eg. atrial fibrillation)
5. Heart Failure
6. Heart murmur
7. Hepatojugular sign
8. Hypertension
9. Orthopnoea
10. Pericardial effusion
11. Pericarditis/Myocarditis/Endocarditis
12. Peripheral edema
13. Valve disorders
14. Bronchial Asthma
15. COPD
16. COPD exacerbation
17. Hemoptysis
18. Interstitial Lung Disease
19. Pleural effusion
20. Pleural effusion
21. Pneumonia (CAP, HAP, immune compromise)
22. Pulmonary embolism
23. Rales
February 2019
School of Medicine, EUC/Clinical Training Manual …. 35
24. Stridor
25. Wheezing
Clinical Training II (MED417) - Digestive System & Hematology
Description
Students shadow residents and consultants in departments of gastroenterology, general
abdominal surgery, and hematology. They are assigned to patients, whom they follow from
admission to discharge and act as attending physicians, under the supervision of their
clinical instructors. The overall objective of this rotation is for students to familiarize with
the responsibilities of physicians, including obtaining history, performing physical
examination, performing differential diagnoses, proposing investigation and management
plans, observing patients’ daily progress, completing medical charts and discharging.
The objective of the course is to familiarize students with
The clinical manifestations, diagnosis, medical and surgical management and
prevention of the diseases of
The digestive system and the blood and blood forming organs
Course Content
Most frequently encountered pathologies of the digestive system.
Functional abnormalities, gastrointestinal bleeding, ulcerative syndromes, acute
abdomen, pathologies of the biliary pathway, jaundice, liver failure, portal
hypertension, ascites, pathology of the pancreas, gastrointestinal cancer,
malabsorption syndromes, diarrhoea, constipation and other relevant pathologies of
the digestive system.
Most frequently encountered pathologies of the hematopoietic system.
Hyperglobulinemia, anemia syndromes, leucocyte abnormalities, bleeding and
thrombotic diathesis, pathology of the lymphatic system, hemotalogical neoplasias
and other relevant hematological pathologies
Methods of diagnosis (history, physical examination and laboratory tests) of above
diseases and conditions
Medical and surgical treatment and prevention of above diseases and conditions
Educational Objectives
Upon successful completion of this course students should be able to:
Identify the most frequently encountered pathologies of the digestive system:
Diagnose the most frequently encountered pathologies of the digestive system by
obtaining a past clinical history and carrying out physical examination with focus on
digestive pathologies, indications and interpretation of the principal complementary
tests for diagnosis (clinical laboratory and imaging tests, anatomopathological studies,
etc).
Carry out the medical-surgical management of the most frequently encountered
pathologies of the digestive system.
Identify the most frequently encountered pathologies of the hematopoietic system.
Diagnose the most frequently encountered pathologies of the hematopoietic system
by obtaining a past clinical history and carrying out a physical examination with focus
on the hematopoietic system, indications and interpretation of the principal
complementary tests for diagnosis (hemogram, peripheral blood smear,
proteinogram, hemostasis tests, iron metabolism values, other laboratory, imaging
and anatomopathological tests, etc).

February 2019
School of Medicine, EUC/Clinical Training Manual …. 36
Manage the medical-surgical treatment of the most frequent diseases of the
hematopoietic system.
Guidelines
Length: 4 weeks
Site: gastroenterology department, hematology department, outpatient clinics,
endoscopy unit, chemotherapy unit, ambulatory care unit, emergency department,
medical ICU, private office practice, additional sites, as available.
Orientation: At the start of the clerkship an orientation is given. The clerkship director
or designee discusses the program’s goals and objectives, the responsibilities of the
student, the schedule and assignments to preceptors and residents. The student is
introduced to the key preceptors and staff members in the department.
Schedule: The student must attend scheduled clinical conferences, grand rounds,
morning visits, classes, subspecialty conferences, learning sessions.
Attending Rounds: The student is involved in all patient care activities in the
outpatient facility and inpatient unit.
Preceptor sessions: A preceptor meets with students daily. The preceptor sessions
will include clinical discussions that focus on problem solving, decision making and
adherence to bioethical principals.
Grade Components
Medical knowledge 50%
Clinical & Communication skills 40%
Attendance & Professional behavior 10%
Medical Knowledge
Demonstrate knowledge of the principal syndromes and illnesses, their underlying causes
both medically and socially and the various diagnostic and therapeutic options available
to physicians in the care of their patients.
Demonstrate knowledge of the indications for and the ability to interpret standard
diagnostic tests, e.g.; CBC, chemistries, chest x-rays, urinalysis, EKGs, as well as other
relevant specialized tests.
Recognize unusual presentations of disease in elderly patients and demonstrate
understanding of the complexity of providing care for the chronically ill with multiple
medical problems. This should include an understanding of end of life issues, as well as
bioethical, public health and economic considerations, which arise in our health care
system.
Demonstrate knowledge of the indications for various levels of care post-discharge, e.g.,
short and long term rehabilitation, long-term skilled nursing facility care, hospice, home
care, etc.
Clinical Skills
Take a comprehensive history and perform a complete physical exam. Formulate a
comprehensive problem list, differential diagnosis; and articulate a basic therapeutic plan,
employing concern for risks, benefits, and costs.
Analyze additional clinical information, lab tests and changes in patients’ clinical status;
note changes in the differential diagnosis or in the diagnostic or therapeutic plans as
circumstances and test results change. Begin to develop proficiency in basic procedures,
such as venipuncture, arterial puncture, nasogastric tube insertion, insertion of intravenous
lines, urinary bladder catheterization, etc.

February 2019
School of Medicine, EUC/Clinical Training Manual …. 37
Clinical examination, including recognition of common signs of gastrointestinal
diseases: abdominal examination and findings, skin and mucosa, liver and spleen
evaluation, volume status assessment
Common gastrointestinal disorders (see Part D): recognition, evaluation, diagnosis,
management
Evaluation of endoscopy findings
History taking and focus on risk factors for digestive diseases, family history, social
and occupational history
Clinical examination, including recognition of common signs of hematological
diseases: skin and mucosa, lymph nodes, liver and spleen evaluation, immune status
Common hematological disorders (see Part D): recognition, evaluation, diagnosis,
management
History taking and focus on risk factors for hematological diseases, family history,
social and occupational history
Peripheral blood findings and smear evaluation
Arterial blood gases
Blood culture
Blood glucose examination using finger stick
Blood transfusion
Hand washing (including surgical scrubbing)
Intramuscular injection
Intravenous injection
Nasogastric tube placement
Oxygen supplementation
Peripheral venous catheter placement
Rectal examination
Respiratory secretions culture
Setting up syringe driver
Skin suturing
Skin swabs for culture
Subcutaneous injections
Suction of respiratory secretions
Swabs from nose, throat and skin
Urinary catheter insertion, female
Urinary catheter insertion, male
Urinary catheter removal
Urinalysis using urine stick
Vein puncture and blood drawing
Wound care and basic wound dressing
Communication Skills
Verbal:
Basic competence in comprehensive case presentation
Basic competence in focused case presentation
Basic competence in explaining to a patient a simple diagnostic and therapeutic plan Basic
informed consent scenario for a procedure
Written:
Competence in comprehensive case write-ups
Competence in brief case write-ups
Professional Behavior
Demonstrate a regimen of independent learning through the reading of suggested basic
texts, research via the Internet and through other electronic resources, maintenance of the

February 2019
School of Medicine, EUC/Clinical Training Manual …. 38
patient encounter log and completion of the web-based educational program
requirements.
Demonstrate a commitment to quality, patient safety and self-directed improvement.
Demonstrate competency and comfort in dealing with people of varying racial, cultural
and religious backgrounds
Demonstrate a commitment to treating all patients, families and other caregivers with
respect.
Participate fully with the patient care team and fulfill all responsibilities in a timely fashion.
Maintain a professional appearance and demeanor.
Demonstrate facility in working in concert with other caregivers, nutritionists and
social workers / discharge planners to obtain optimal, seamless multidisciplinary care
for their patients, both during the hospitalization and after discharge.
Core Topics & Patients
A. The healthy patient: health promotion and education, disease prevention and screening.
B. Patients with a symptom, sign, abnormal laboratory value or known medical condition
1. Acute abdominal pain
2. Ascites
3. Colostomy
4. Diarrhea
5. Functional disorder (irritable bowel syndrome, constipation, diarrhea)
6. Gastroesophageal reflux disease (GERD)
7. Hematemesis
8. Hematochezia
9. Hepatitis - Elevated liver enzymes (acute liver damage)
10. Inflammatory bowel disease (Crohn’s disease, Ulcerative colitis)
11. Liver cirrhosis
12. Pancreatitis
13. Peptic ulcer disease
14. Upper gastrointestinal bleeding
15. Vomiting
16. Anemia
17. “B” symptomatology
18. Bone marrow biopsy
19. Idiopathic thrombopenic purpura / Thrombotic thrombopenic purpura
20. Leukemia (AML, ALL, CML, CLL)
21. Lymphadenopathy
22. Multiple myeloma
23. Myelodysplastic syndromes (MDS)
24. Splenomegaly
25. Thalassemia syndromes
26. Abdominal pain
27. Anemia
28. Dyspepsia
29. GI bleeding
30. Irritable bowel
31. Jaundice
32. Weight loss
Clinical Training III (MED408) - Infectious Diseases and Clinical Microbiology
Description

February 2019
School of Medicine, EUC/Clinical Training Manual …. 39
Students shadow residents and consultants in departments of internal medicine /
infectious diseases, intensive care units and microbiology. They are assigned to patients
whom they follow from admission to discharge and act as attending physicians, under the
supervision of their clinical instructors. In clinical microbiology, they familiarize with the
daily functions of the department of microbiology and with the basic principles of infection
control in healthcare settings.
The objective of the course is to familiarize students with
The clinical manifestations, diagnosis, medical and surgical management and
prevention of the infectious diseases
Course Content
Infectious Pathologies of the Various Organs and Systems
Bacterial, viral and fungal diseases
Parasitic diseases and zoonoses
Diseases due to intestinal bacteria (Enterobacteriaceae, vibrios, Campylobacter,
Helicobacter).
Prevention of infectious diseases and immunizations
Methods of diagnosis (history, physical examination and laboratory tests) of above
diseases and conditions
Medical and surgical treatment and prevention of above diseases and conditions
Educational Objectives
Upon successful completion of this course students should be able to:
Identify the most frequently encountered infectious pathologies in the various organs
and systems.
Diagnose the most frequently encountered infectious pathologies in the various
organs and systems by obtaining a past clinical history and carrying out physical
examination with focus on infectious pathologies, indications and interpretation of the
principal complementary studies of infectious pathologies, obtaining and processing
the various biological samples in the clinical microbiology laboratory.
Manage the medical-surgical treatment of the most frequently encountered infectious
diseases in the various organs and systems.
Guidelines
Length: 2 weeks
Site: internal medicine department, outpatient clinics, ambulatory care unit,
specialized units (eg.HIV), emergency department, medical or ID ICU, private office
practice, additional sites, as available.
Orientation: At the start of the clerkship an orientation is given. The clerkship director
or designee discusses the program’s goals and objectives, the responsibilities of the
student, the schedule and assignments to preceptors and residents. The student is
introduced to the key preceptors and staff members in the department.
Schedule: The student must attend scheduled clinical conferences, grand rounds,
morning visits, classes, subspecialty conferences, learning sessions.
Attending Rounds: The student is involved in all patient care activities in the
outpatient facility and inpatient unit.
Preceptor sessions: A preceptor meets with students daily. The preceptor sessions
will include clinical discussions that focus on problem solving, decision making and
adherence to bioethical principals.
Grade Components
Medical knowledge 50%
Clinical & Communication skills 40%

February 2019
School of Medicine, EUC/Clinical Training Manual …. 40
Attendance & Professional behavior 10%
Medical Knowledge
Demonstrate knowledge of the principal syndromes and illnesses, their underlying causes
both medically and socially and the various diagnostic and therapeutic options available
to physicians in the care of their patients.
Demonstrate knowledge of the indications for and the ability to interpret standard
diagnostic tests, e.g.; CBC, chemistries, chest x-rays, urinalysis, EKGs, as well as other
relevant specialized tests.
Recognize unusual presentations of disease in elderly patients and demonstrate
understanding of the complexity of providing care for the chronically ill with multiple
medical problems. This should include an understanding of end of life issues, as well as
bioethical, public health and economic considerations, which arise in our health care
system.
Demonstrate knowledge of the indications for various levels of care post-discharge, e.g.,
short and long term rehabilitation, long-term skilled nursing facility care, hospice, home
care, etc.
Clinical Skills
Take a comprehensive history and perform a complete physical exam. Formulate a
comprehensive problem list, differential diagnosis; and articulate a basic therapeutic plan,
employing concern for risks, benefits, and costs.
Analyze additional clinical information, lab tests and changes in patients’ clinical status;
note changes in the differential diagnosis or in the diagnostic or therapeutic plans as
circumstances and test results change. Begin to develop proficiency in basic procedures,
such as venipuncture, arterial puncture, nasogastric tube insertion, insertion of intravenous
lines, urinary bladder catheterization, etc.
Arterial blood gases
Blood culture
Blood glucose examination using finger stick
Blood transfusion
Hand washing (including surgical scrubbing)
Intramuscular injection
Intravenous injection
Nasogastric tube placement
Oxygen supplementation
Peripheral venous catheter placement
Rectal examination
Respiratory secretions culture
Setting up syringe driver
Skin suturing
Skin swabs for culture
Subcutaneous injections
Suction of respiratory secretions
Swabs from nose, throat and skin
Urinary catheter insertion, female
Urinary catheter insertion, male
Urinary catheter removal
Urinalysis using urine stick
Vein puncture and blood drawing
Wound care and basic wound dressing

February 2019
School of Medicine, EUC/Clinical Training Manual …. 41
Communication Skills
Verbal:
Basic competence in comprehensive case presentation
Basic competence in focused case presentation
Basic competence in explaining to a patient a simple diagnostic and therapeutic plan
Basic informed consent scenario for a procedure
Written:
Competence in comprehensive case write-ups
Competence in brief case write-ups
Professional Behavior
Demonstrate a regimen of independent learning through the reading of suggested
basic texts, research via the Internet and through other electronic resources,
maintenance of the patient encounter log and completion of the web-based
educational program requirements.
Demonstrate a commitment to quality, patient safety and self-directed improvement.
Demonstrate competency and comfort in dealing with people of varying racial,
cultural and religious backgrounds
Demonstrate a commitment to treating all patients, families and other caregivers with
respect.
Participate fully with the patient care team and fulfill all responsibilities in a timely
fashion.
Maintain a professional appearance and demeanor.
Demonstrate facility in working in concert with other caregivers, nutritionists and
social workers / discharge planners to obtain optimal, seamless multidisciplinary
care for their patients, both during the hospitalization and after discharge.
Core Topics & Patients
A. The healthy patient: health promotion and education, disease prevention and
screening.
B. Patients with a symptom, sign, abnormal laboratory value or known medical condition.
1. Antibiogram interpretation
2. Antimicrobial stewardship principles
3. Bloodstream infection
4. Community-acquired infections
5. Cultures follow-up and their correlation to the patient’s condition
6. Diagnostic tests: Sampling, transfer & preparation of specimens, culture,
Gram-stain, microscopy
7. Immunosuppression and infection
8. Infection prevention & control measures
9. Methods to detect resistance
10. Nosocomial infection definitions
11. Pneumonia
12. Skin & soft tissue infection
13. Surgical site infection
Clinical Training IV - Endocrine system, Uro-Nephrological System & Male Genital Tract
Description
Students shadow residents and consultants in departments of endocrinology, urology, and
nephrology (including transplant units and hemodialysis units). They are assigned to
patients, whom they follow from admission to discharge and act as attending physicians,

February 2019
School of Medicine, EUC/Clinical Training Manual …. 42
under the supervision of their clinical instructors. The overall objective of this rotation is for
students to familiarize with the responsibilities of physicians, including obtaining history,
performing physical examination, performing differential diagnoses, proposing
investigation and management plans, following patients’ daily progress, completing
medical charts and discharging.
The objective of the course is to familiarize students with
The clinical manifestations, diagnosis, medical and surgical management and
prevention of the diseases of
The endocrine and uro-nephrological system and the male genital tract
Course Content
Most frequently encountered pathologies of the endocrine system and the
metabolism.
Diabetes mellitus, dislipidemias, endocrine syndromes due to glandular hyperfunction
and hypofunction (pituitary, thyroid, parathyroids, adrenals), growth disorders,
nutritional and eating disorders, storage diseases and other relevant endocrine and
metabolic pathologies
Most frequently encountered pathologies of the uretero-nephroglogical systems and
the male genital tract.
Hydroelectrolytic changes, acute and chronic renal insufficiency, nephrotic and
nephritic syndrome, neoplasias, obstructive uropathy, pathology of the prostate,
erectile dysfunction and other relevant uro-nephrological pathologies and pathologies
of the male genital tract.
Methods of diagnosis (history, physical examination and laboratory tests) of the above
described diseases and conditions
Medical and surgical treatment and prevention of the above described diseases and
conditions
Educational Objectives
Upon successful completion of this course students should be able to:
Identify the most frequently encountered pathologies of the endocrine system and the
metabolism.
Diagnose the most frequently encountered pathologies of the endocrine system by
obtaining a past clinical history and carrying out a physical examination with focus on
the endocrine system, indications and interpretation of the principal complementary
diagnostic tests (laboratory, imaging, anatomopathological tests, etc).
Manage the medical-surgical treatment of the most frequently encountered diseases
of the endocrine system and the metabolism.
Identify the most frequently encountered uro-nephrological pathologies
Diagnose the most frequently encountered uro-nephrological pathologies by obtaining
a past clinical history and physical examination with focus on uro-nephrological
pathologies and on pathologies of the male genital tract, indications and interpretation
of the basic blood serum and urine analysis related to the renal function and the
electrolyte balance including acid/base abnormalities, other clinical laboratory tests,
imaging, and anatomopathological tests, etc.
Manage the medical-surgical treatment of the most frequently encountered diseases
of the uro-nephrological system.
Guidelines
Length: 6 weeks
Site: endocrinology department, diabetes clinic, obesity clinic, nephrology/renal
department, hemodialysis, peritoneal dialysis, outpatient clinics, urology department,

February 2019
School of Medicine, EUC/Clinical Training Manual …. 43
andrology clinic, lithotropsy unit, urological operation room, ambulatory care units,
private office practice, additional sites, as available.
Orientation: At the start of the clerkship an orientation is given. The clerkship director
or designee discusses the program’s goals and objectives, the responsibilities of the
student, the schedule and assignments to preceptors and residents. The student is
introduced to the key preceptors and staff members in the department.
Schedule: The student must attend scheduled clinical conferences, grand rounds,
morning visits, classes, subspecialty conferences, learning sessions, surgeries.
Attending Rounds: The student is involved in all patient care activities in the
outpatient facility and inpatient unit.
Preceptor sessions: A preceptor meets with students daily. The preceptor sessions
will include clinical discussions that focus on problem solving, decision making and
adherence to bioethical principals.
Assessment
Medical knowledge 50%
Clinical & Communication skills 40%
Attendance & Professional behavior 10%
Medical Knowledge
Demonstrate knowledge of the principal syndromes and illnesses, their underlying causes
both medically and socially and the various diagnostic and therapeutic options available
to physicians in the care of their patients.
Demonstrate knowledge of the indications for and the ability to interpret standard
diagnostic tests, e.g.; CBC, chemistries, chest x-rays, urinalysis, EKGs, as well as other
relevant specialized tests.
Recognize unusual presentations of disease in elderly patients and demonstrate
understanding of the complexity of providing care for the chronically ill with multiple
medical problems. This should include an understanding of end of life issues, as well as
bioethical, public health and economic considerations, which arise in our health care
system.
Demonstrate knowledge of the indications for various levels of care post-discharge, e.g.,
short and long term rehabilitation, long-term skilled nursing facility care, hospice, home
care, etc.
Clinical Skills
Take a comprehensive history and perform a complete physical exam. Formulate a
comprehensive problem list, differential diagnosis; and articulate a basic therapeutic plan,
employing concern for risks, benefits, and costs.
Analyze additional clinical information, lab tests and changes in patients’ clinical status; note
changes in the differential diagnosis or in the diagnostic or therapeutic plans as circumstances
and test results change. Begin to develop proficiency in basic procedures, such as venipuncture,
arterial puncture, nasogastric tube insertion, insertion of intravenous lines, urinary bladder
catheterization, etc.
Arterial blood gases
Blood culture
Blood glucose examination using finger stick
Blood transfusion
Hand washing (including surgical scrubbing)
Intramuscular injection
Intravenous injection
Nasogastric tube placement

February 2019
School of Medicine, EUC/Clinical Training Manual …. 44
Oxygen supplementation
Peripheral venous catheter placement
Rectal examination
Respiratory secretions culture
Setting up syringe driver
Skin suturing
Skin swabs for culture
Subcutaneous injections
Suction of respiratory secretions
Swabs from nose, throat and skin
Urinary catheter insertion, female
Urinary catheter insertion, male
Urinary catheter removal
Urinalysis using urine stick
Vein puncture and blood drawing
Wound care and basic wound dressing
Communication Skills
Verbal:
Basic competence in comprehensive case presentation
Basic competence in focused case presentation
Basic competence in explaining to a patient a simple diagnostic and therapeutic
plan Basic informed consent scenario for a procedure
Written:
Competence in comprehensive case write-ups
Competence in brief case write-ups
Professional Behavior
Demonstrate a regimen of independent learning through the reading of suggested basic
texts, research via the Internet and through other electronic resources, maintenance of the
patient encounter log and completion of the web-based educational program
requirements.
Demonstrate a commitment to quality, patient safety and self-directed improvement.
Demonstrate competency and comfort in dealing with people of varying racial, cultural
and religious backgrounds
Demonstrate a commitment to treating all patients, families and other caregivers with
respect.
Participate fully with the patient care team and fulfill all responsibilities in a timely fashion.
Maintain a professional appearance and demeanor.
Demonstrate facility in working in concert with other caregivers, nutritionists and
social workers / discharge planners to obtain optimal, seamless multidisciplinary care
for their patients, both during the hospitalization and after discharge.
Core Topics & Patients
A. The healthy patient: health promotion and education, disease prevention and screening.
B. Patients with a symptom, sign, abnormal laboratory value or known medical condition
1. Blood sugar obtaining and interpretation
2. Bone densitometry test (eg.DEXA) interpretation
3. Diabetes mellitus
4. Dyslipidemia interpretation
5. Hyperthyroidism
6. Hypothyroidism
7. Lipid disorders

February 2019
School of Medicine, EUC/Clinical Training Manual …. 45
8. Oral glucose tolerance test interpretation
9. Osteoporosis / Metabolic bone disease
10. Surgical treatment of thyroid disease
11. Thyroid tests interpretation
12. Kidney stone disease
13. Lithotripsy
14. Male subfertility
15. Obstructive uropathy
16. Prostate biopsy
17. Prostate cancer
18. Prostate examination
19. Prostate hypertrophy
20. Urethral catheterization (male)
21. Urethral catheterization (female)
22. Urinary colic
23. Urine retention
24. Acute renal failure
25. Creatinine clearance calculation and interpretation
26. Glomerulonephritis (any)
27. Hemodialysis
28. Kidney biopsy
29. Kidney transplantation
30. Kidney vasculitis (any)
31. Patient with fistula
32. Urine sediment microscopy

February 2019
School of Medicine, EUC/Clinical Training Manual …. 46
Clinical Training V - Musculoskeletal System
Description
Students shadow residents and consultants in departments of orthopedics and trauma,
and rheumatology. They are assigned to patients, whom they follow from admission to
discharge and act as attending physicians, under the supervision of their clinical
instructors. The overall objective of this rotation is for students to familiarize with the
responsibilities of physicians, including obtaining history, performing physical examination,
performing differential diagnoses, proposing investigation and management plans,
following patients’ daily progress, participating in surgery, completing medical charts and
discharging.
The objective of the course is to familiarize students with
The clinical manifestations, diagnosis, medical and surgical management and
prevention of the diseases of the Musculoskeletal System
Course Content
Most frequently encountered pathologies of the musculoskeletal system
Principal pain syndromes of the musculoskeletal system, inflammatory and
degenerative processes, autoimmune diseases affecting the musculoskeletal
system, traumas and fractures, tumors and other pathologies relevant to the
musculoskeletal system.
Methods of diagnosis (history, physical examination and laboratory tests) of above
diseases and conditions
Medical and surgical treatment and prevention of above diseases and conditions
Educational Objectives
Upon successful completion of this course students should be able to:
Identify the most frequently encountered pathologies of the musculoskeletal system.
Diagnose the most frequently encountered pathologies of the musculoskeletal
system by obtaining a past clinical history and physical examination with focus on
the pathology of the musculoskeletal system, indications and interpretation of the
principal complementary analytical tests, imaging, anatomopathological studies, etc.
Manage the medical-surgical treatment of the most frequently encountered
pathologies of the musculoskeletal system.
Guidelines
Length: 4 weeks
Site: orthopedics department, paraplegics department, rheumatology department,
outpatient clinics, orthopedics/trauma operation room, acute trauma unit, ambulatory
care unit, emergency department, surgical ICU, private office practice, additional
sites, as available.
Orientation: At the start of the clerkship an orientation is given. The clerkship
director or designee discusses the program’s goals and objectives, the
responsibilities of the student, the schedule and assignments to preceptors and
residents. The student is introduced to the key preceptors and staff members in the
department.
Schedule: The student must attend scheduled clinical conferences, grand rounds,
morning visits, classes, subspecialty conferences, learning sessions, operations.
Attending Rounds: The student is involved in all patient care activities in the
outpatient facility and inpatient unit.

February 2019
School of Medicine, EUC/Clinical Training Manual …. 47
Preceptor sessions: A preceptor meets with students daily. The preceptor sessions
will include clinical discussions that focus on problem solving, decision making and
adherence to bioethical principals.
Assessment
Medical knowledge 50%
Clinical & Communication skills 40%
Attendance & Professional behavior 10%
Medical Knowledge
Demonstrate knowledge of the principal syndromes and illnesses, their underlying causes
both medically and socially and the various diagnostic and therapeutic options available
to physicians in the care of their patients.
Demonstrate knowledge of the indications for and the ability to interpret standard
diagnostic tests, e.g.; CBC, chemistries, chest x-rays, urinalysis, EKGs, as well as other
relevant specialized tests.
Recognize unusual presentations of disease in elderly patients and demonstrate
understanding of the complexity of providing care for the chronically ill with multiple
medical problems. This should include an understanding of end of life issues, as well as
bioethical, public health and economic considerations, which arise in our health care
system.
Demonstrate knowledge of the indications for various levels of care post-discharge, e.g.,
short and long term rehabilitation, long-term skilled nursing facility care, hospice, home
care, etc.
Clinical Skills
Take a comprehensive history and perform a complete physical exam. Formulate a
comprehensive problem list, differential diagnosis; and articulate a basic therapeutic plan,
employing concern for risks, benefits, and costs.
Analyze additional clinical information, lab tests and changes in patients’ clinical status;
note changes in the differential diagnosis or in the diagnostic or therapeutic plans as
circumstances and test results change. Begin to develop proficiency in basic procedures,
such as venipuncture, arterial puncture, nasogastric tube insertion, insertion of intravenous
lines, urinary bladder catheterization, etc.
Arterial blood gases
Blood culture
Blood glucose examination using finger stick
Blood transfusion
Hand washing (including surgical scrubbing)
Intramuscular injection
Intravenous injection
Nasogastric tube placement
Oxygen supplementation
Peripheral venous catheter placement
Rectal examination
Respiratory secretions culture
Setting up syringe driver
Skin suturing
Skin swabs for culture
Subcutaneous injections
Suction of respiratory secretions
Swabs from nose, throat and skin
Urinary catheter insertion, female

February 2019
School of Medicine, EUC/Clinical Training Manual …. 48
Urinary catheter insertion, male
Urinary catheter removal
Urinalysis using urine stick
Vein puncture and blood drawing
Wound care and basic wound dressing
Communication Skills
Verbal:
Basic competence in comprehensive case presentation
Basic competence in focused case presentation
Basic competence in explaining to a patient a simple diagnostic and therapeutic
plan Basic informed consent scenario for a procedure
Written:
Competence in comprehensive case write-ups
Competence in brief case write-ups
Professional Behavior
Demonstrate a regimen of independent learning through the reading of suggested
basic texts, research via the Internet and through other electronic resources,
maintenance of the patient encounter log and completion of the web-based
educational program requirements.
Demonstrate a commitment to quality, patient safety and self-directed improvement.
Demonstrate competency and comfort in dealing with people of varying racial,
cultural and religious backgrounds
Demonstrate a commitment to treating all patients, families and other caregivers with
respect.
Participate fully with the patient care team and fulfill all responsibilities in a timely
fashion.
Maintain a professional appearance and demeanor.
Demonstrate facility in working in concert with other caregivers, nutritionists and
social workers / discharge planners to obtain optimal, seamless multidisciplinary
care for their patients, both during the hospitalization and after discharge.
Core Topics & Patients
A. The healthy patient: health promotion and education, disease prevention and screening.
B. Patients with a symptom, sign, abnormal laboratory value, or known medical condition
Back pain
Chronic pain
Osteoporosis
Falls, gait and balance problems
Arthritis examination
Arthritis differential diagnosis
Gait assessment
GALS examination
Knee aspiration
Muscle strength
Plaster placement
Plaster removal
Acute trauma
Arthritis, inflammatory
Arthritis, non-inflammatory
Arthroplasty

February 2019
School of Medicine, EUC/Clinical Training Manual …. 49
Osteoporosis
Rheumatoid arthritis
Sacroiliitis
Clinical Training VI (MED519) - Nervous System & Psychiatry
Description
Students shadow residents and consultants in departments of neurology, neurosurgery
and psychiatry. They are assigned to patients, whom they follow from admission to
discharge and act as attending physicians, under the supervision of their clinical
instructors. The overall objective of this rotation is for students to familiarize with the
responsibilities of physicians, including obtaining history, performing physical examination,
performing differential diagnoses, proposing investigation and management plans,
following patients’ daily progress, participating in surgery, completing medical charts and
discharging.
The objective of the course is to familiarize students with
The clinical manifestations, diagnosis, medical and surgical management and
prevention of the diseases of
The nervous system and of psychiatric disorders
Course Content
Most frequently encountered pathologies of the central and peripheral nervous system.
Intracraneal hypertension syndrome, cephalalgeas, vertiginous syndromes, cerebelar
syndromes, meningeal syndromes, convulsive syndromes, encephalopathies,
cranioencephalic trauma, peripheral neuropathies and neuropathies of the
autonomous nervous system, myopathies and other pathologies relevant to the
central and peripheral nervous system.
Psychiatric disorders.
Anxiety disorders, related food intake disorders, syndromes associated with the use
of drugs, delirium, psychosis, dementia, affective disorders, phobias, obsessive-
compulsive disorders, post-traumatic stress, psychopathological reactions in
situations of illness and death, somatization disorders, dissociative disorders, sleep
disorders, impulse control disorders and personality disorders
Methods of diagnosis (history, physical examination and laboratory tests) of above diseases
and conditions
Medical and surgical treatment and prevention of the above described diseases and
conditions
Educational Objectives
Upon successful completion of this course students should be able to:
Identify the most frequently encountered pathologies of the central and peripheral
nervous system
Diagnose the most prevalent diseases of the central and peripheral nervous system
by obtaining a past clinical history and physical examination with focus on the
pathologies of the central and peripheral nervous system, indications and
interpretation of the principal complementary studies in neurology, laboratory,
imaging, anatomopathological tests, etc.
Manage the medical-surgical treatment of the most frequently encountered
pathologies of the central and peripheral nervous system.

February 2019
School of Medicine, EUC/Clinical Training Manual …. 50
Identify the principal psychiatric disorders.
Diagnose psychiatric disorders by obtaining a past clinical history and physical
examination with focus on psychiatric pathologies, indications and interpretation of
the principal complementary studies in psychiatry.
Manage the treatment of the principal psychiatric disorders (anxiety, depression,
delirium, agitation, insomnia, etc).
Guidelines
Length 4 weeks
Site: neurology department, stroke unit, dementia clinic, psychiatry department,
outpatient clinics, substance abuse unit, neurological/neurosurgery ICU, ambulatory
care unit, emergency department, private office practice, additional sites, as available.
Orientation: At the start of the clerkship an orientation is given. The clerkship director
or designee discusses the program’s goals and objectives, the responsibilities of the
student, the schedule and assignments to preceptors and residents. The student is
introduced to the key preceptors and staff members in the department.
Schedule: The student must attend scheduled clinical conferences, grand rounds,
morning visits, classes, subspecialty conferences, learning sessions.
Attending Rounds: The student is involved in all patient care activities in the outpatient
facility and inpatient unit.
Preceptor sessions: A preceptor meets with students daily. The preceptor sessions
will include clinical discussions that focus on problem solving, decision making and
adherence to bioethical principals.
Assessment
Medical knowledge 50%
Clinical & Communication skills 40%
Attendance & Professional behavior 10%
Medical Knowledge
Demonstrate knowledge of the principal syndromes and illnesses, their underlying causes
both medically and socially and the various diagnostic and therapeutic options available
to physicians in the care of their patients.
Demonstrate knowledge of the indications for and the ability to interpret standard
diagnostic tests, e.g.; CBC, chemistries, chest x-rays, urinalysis, EKGs, as well as other
relevant specialized tests.
Recognize unusual presentations of disease in elderly patients and demonstrate
understanding of the complexity of providing care for the chronically ill with multiple
medical problems. This should include an understanding of end of life issues, as well as
bioethical, public health and economic considerations which arise in our health care
system.
Demonstrate knowledge of the indications for various levels of care post-discharge, e.g.,
short and long term rehabilitation, long-term skilled nursing facility care, hospice, home
care, etc.
Clinical Skills
Take a comprehensive history and perform a complete physical exam. Formulate a
comprehensive problem list, differential diagnosis; and articulate a basic therapeutic plan,
employing concern for risks, benefits, and costs.

February 2019
School of Medicine, EUC/Clinical Training Manual …. 51
Analyze additional clinical information, lab tests and changes in patients’ clinical status;
note changes in the differential diagnosis or in the diagnostic or therapeutic plans as
circumstances and test results change. Begin to develop proficiency in basic procedures,
such as venipuncture, arterial puncture, nasogastric tube insertion, insertion of intravenous
lines, urinary bladder catheterization, etc.
Clinical examination, including recognition of common signs of neurological diseases:
cognitive status assessment, muscle tone and power, reflexes, sensation, motor
function and coordination, localizing neurology
Common neurological and psychiatric disorders (see Part D): recognition, evaluation,
diagnosis, management
History taking and focus on neurological and psychiatric diseases: risk factors, family
history, social history
History taking and patient evaluation in psychiatry, including use of screening tools
Evaluation and management of substance and alcohol use and abuse
Arterial blood gases
Blood culture
Blood glucose examination using finger stick
Blood transfusion
Hand washing (including surgical scrubbing)
Intramuscular injection
Intravenous injection
Nasogastric tube placement
Oxygen supplementation
Peripheral venous catheter placement
Rectal examination
Respiratory secretions culture
Setting up syringe driver
Skin suturing
Skin swabs for culture
Subcutaneous injections
Suction of respiratory secretions
Swabs from nose, throat and skin
Urinary catheter insertion, female
Urinary catheter insertion, male
Urinary catheter removal
Urinalysis using urine stick
Vein puncture and blood drawing
Wound care and basic wound dressing
Communication Skills
Verbal:
Basic competence in comprehensive case presentation
Basic competence in focused case presentation
Basic competence in explaining to a patient a simple diagnostic and therapeutic
plan Basic informed consent scenario for a procedure
Written:
Competence in comprehensive case write-ups
Competence in brief case write-ups
Professional Behavior
Demonstrate a regimen of independent learning through the reading of suggested
basic texts, research via the Internet and through other electronic resources,

February 2019
School of Medicine, EUC/Clinical Training Manual …. 52
maintenance of the patient encounter log and completion of the web-based
educational program requirements.
Demonstrate a commitment to quality, patient safety and self-directed improvement.
Demonstrate competency and comfort in dealing with people of varying racial,
cultural and religious backgrounds
Demonstrate a commitment to treating all patients, families and other caregivers with
respect.
Participate fully with the patient care team and fulfill all responsibilities in a timely
fashion.
Maintain a professional appearance and demeanor.
Demonstrate facility in working in concert with other caregivers, nutritionists and
social workers / discharge planners to obtain optimal, seamless multidisciplinary
care for their patients, both during the hospitalization and after discharge.
Core Topics & Patients
A. The healthy patient: health promotion and education, disease prevention and screening.
B. Patients with a symptom, sign, abnormal laboratory value or known medical condition
Cranial nerve examination
Cerebellar tests
Cerebrovascular event (stroke)
Huntington’s disease
Intracranial hemorrhage
Lower motor neuron disease
Lumbar puncture
Motor system examination
Multiple sclerosis
Neurological examination
Parkinson’s disease
Peripheral neuropathy
Sensory system examination
Tendon reflexes
Upper motor neuron disease
Alcohol misuse screening
Alcohol misuse / withdrawal
Anxiety disorder
Cognitive status assessment
Dementia
Depression
Psychiatric history
Psychosis
Substance abuse
Altered mental status
Geriatric Issues
Cognitive Impairment
Falls, gait and balance problems
Sensory impairments
Sleep disorders
Clinical Training VII (MED510) - Pediatrics

February 2019
School of Medicine, EUC/Clinical Training Manual …. 53
Description
Students shadow residents and consultants in departments of pediatrics and pediatric
surgery. They are assigned to patients, whom they follow from admission to discharge and
act as attending physicians, under the supervision of their clinical instructors. The overall
objective of this rotation is for students to familiarize with the responsibilities of physicians,
including obtaining history, performing physical examination, performing differential
diagnoses, proposing investigation and management plans, following patients’ daily
progress, participating in surgery, completing medical charts and discharging.
The objective of the course is to familiarize students with
The process of normal growth of children from birth to adolescence and of growth
abnormalities
The development of the cognitive and mental functions of children
The clinical manifestations, management and counselling of genetic disorders
The clinical manifestations, diagnosis, medical and surgical management and
prevention of the diseases of children
Course Content
Normal growth and development of the newly-born, infant, child and adolescent.
Cognitive, emotional and psychosocial development in childhood and adolescence
Fundamentals of child nutrition.
Premature newly-born and its comprehensive care and neonatal care.
Childhood immunizations, prevention of disease and health promotion
Most frequently encountered paediatric pathologies.
Immune system and infections
Disorders of the metabolic, respiratory, circulatory, hematological, digestive, nephro-
urological, endocrine, nervous, dermatological & musculoskeletal systems and of the
eye and ear;
Hematological and solid malignancies;
Methods of diagnosis (history, physical examination and laboratory tests) of the
above described diseases and conditions
Medical and surgical treatment and prevention of the above described diseases and
conditions
Educational Objectives
Upon successful completion of this course students should be able to:
Recall the morphological and functional characteristics of the newly-born, the child
and the adolescent.
Describe the normal process of growth of the child and the adolescent.
Explain the cognitive, emotional and psychosocial development in childhood and
adolescence.
Discuss the fundamentals of nutrition in the child.
Demonstrate that they know the characteristics of the premature new-born and their
comprehensive care.
Discuss the fundamentals of diagnosis and genetic counselling.
Identify the most frequently encountered pediatric pathologies.
Diagnose the most frequently encountered pediatric pathologies by obtaining a past
clinical history of the child, physical examination of the newly-born, infant, child and
adolescent, indications and interpretation of the principal complementary studies used
in pediatrics.
Manage the medical-surgical treatment of the most frequently encountered pediatric
pathologies.

February 2019
School of Medicine, EUC/Clinical Training Manual …. 54
Guidelines
Length: 6 weeks
Site: general pediatric unit, ambulatory care unit, pediatric emergency department,
nursery, NICU, PICU, private office practice, additional sites, as available.
Orientation: At the start of the clerkship an orientation is given. The clerkship director
or designee discusses the program’s goals and objectives, the responsibilities of the
student, the schedule and assignments to preceptors and residents. The student is
introduced to the key preceptors and staff members in the department.
Schedule: The student must attend scheduled clinical conferences, grand rounds,
morning visits, classes, subspecialty conferences, learning sessions.
Attending Rounds: The student is involved in all patient care activities in the outpatient
facility and inpatient unit.
Preceptor sessions: A preceptor meets with students daily. The preceptor sessions
will include clinical discussions that focus on problem solving, decision making and
adherence to bioethical principals.
Assessment
Grade Components
Medical knowledge 50%
Clinical & Communication skills 40%
Attendance & Professional behavior 10%
Medical Knowledge
Gain knowledge in the core topics of the curriculum.
Gain supplementary information and data from journals, texts, research, the internet and
other resources.
Demonstrate knowledge regarding the major illnesses and conditions that affect
newborns.
Demonstrate knowledge of health maintenance and preventive pediatrics, including:
immunization schedules, newborn screening, lead testing, TB testing, vision and hearing
screening.
Demonstrate knowledge of growth and development with special emphasis on puberty.
(Tanner Stages)
Compare and contrast the feeding and nutritional requirements of each age and stage of
childhood.
Demonstrate knowledge of fluid and electrolyte balance.
Learn the principles of bioethics and understand how they apply to clinical practice.
Clinical Skills
Demonstrate the ability to approach the patient and family in an empathic and focused
manner to form a positive and informative relationship.
Demonstrate the ability to perform an accurate and organized diagnostic interview and
record the information precisely and concisely.
Perform both comprehensive and focused histories and physical examinations on
newborns, infants, toddlers, children and adolescents.
Participate in the selection of relevant laboratory and radiological tests.
Interpret results to support or rule out diagnoses and arrive at a working diagnosis.
Actively participate in formulating a management plan and participate in carrying out that
patient care plan.
Communicate orally and/or in writing the information necessary to inform and educate all
persons involved in the care of the patient: the patient, family/guardians, nurses and all
members of the multidisciplinary health care team. Communication should avoid jargon
and vagueness.

February 2019
School of Medicine, EUC/Clinical Training Manual …. 55
Participate in making decisions regarding management, discharge and follow-up plans.
Interpret laboratory values according to age-related norms.
Accompany and observe senior staff in the delivery room for high risk births.
Communicate with families regarding education and anticipatory guidance during
outpatient visits.
Evaluate common infections and acute illness of children of all ages in the urgent care or
emergency setting.
Evaluate children with serious illness in the inpatient setting.
Evaluate children with chronic and rare illnesses in the outpatient and sub-specialty
centers.
Prepare management plans that consider the patient’s identity, culture and ability to
adhere to the recommendations.
Demonstrate your ability to research topics and apply clinical research to your
understanding of patient issues.
Participate in clinical research when possible, either by participating in an ongoing project
or initiating a new line of inquiry.
Learn to self-assess your own unique learning needs.
Learn how to devise and enact a plan to remediate your deficiencies relevant to learning
gaps.
Learn to assess the credibility of information sources.
Professional Behavior
Establish rapport with patients and families that demonstrates respect and compassion.
Appreciate and acknowledge their identity and culture.
Demonstrate honesty, integrity and respect in dealing with patients, families and
colleagues.
Adhere to the principals of confidentiality, privacy and informed consent.
Demonstrate that you are a responsible team member and carry out all of your assigned
duties in a timely manner.
Offer assistance when and where it is needed.
Demonstrate that you are an effective member of the team by fully participating in
discussions and contributing to learning endeavors.
Demonstrate sensitivity to issues related to culture, race, age, gender, religion, sexual
orientation and disabilities.
React appropriately to conflicts and ethical dilemmas by working toward solutions.
Demonstrate a commitment to professionalism and adherence to the principals of
Bioethics.
Demonstrate responsibility in completing assignments.
Share insights and information with your peers.
Learn to recognize your personal biases and how they lead to diagnostic error.
Learn to recognize when there is a need for consultation.
Prepare for and commit to life-long learning.
Clinical Skills
Take a comprehensive history and perform a complete physical exam. Formulate a
comprehensive problem list, differential diagnosis; and articulate a basic therapeutic plan,
employing concern for risks, benefits, and costs.
Analyze additional clinical information, lab tests and changes in patients’ clinical status;
note changes in the differential diagnosis or in the diagnostic or therapeutic plans as

February 2019
School of Medicine, EUC/Clinical Training Manual …. 56
circumstances and test results change. Begin to develop proficiency in basic procedures,
such as venipuncture, arterial puncture, nasogastric tube insertion, insertion of intravenous
lines, urinary bladder catheterization, etc.
Communication Skills
Verbal:
Basic competence in comprehensive case presentation
Basic competence in focused case presentation
Basic competence in explaining to a patient a simple diagnostic and therapeutic
plan Basic informed consent scenario for a procedure
Written:
Competence in comprehensive case write-ups
Competence in brief case write-ups
Professional Behavior
Demonstrate a regimen of independent learning through the reading of suggested
basic texts, research via the Internet and through other electronic resources,
maintenance of the patient encounter log and completion of the web-based
educational program requirements.
Demonstrate a commitment to quality, patient safety and self-directed improvement.
Demonstrate competency and comfort in dealing with people of varying racial,
cultural and religious backgrounds
Demonstrate a commitment to treating all patients, families and other caregivers
with respect.
Participate fully with the patient care team and fulfill all responsibilities in a timely
fashion.
Maintain a professional appearance and demeanor.
Demonstrate facility in working in concert with other caregivers, nutritionists
and social workers / discharge planners to obtain optimal, seamless
multidisciplinary care for their patients, both during the hospitalization and after
discharge.
Core Topics & Patients
A. The healthy patient: health promotion and education, disease prevention and screening.
B. Patients with a symptom, sign, abnormal laboratory value or known medical condition
Communication skills with children, adolescence and parents.
Vaccines
Developmental milestones in children
Infant and child nutrition
Breast feeding
Fever and fever phobia
Clinical examination of newborn and neonatal resuscitation
Neonatal jaundice
Skin rash in children
Pediatric emergencies
Seizures
Dehydration – Acid base balance
Urinary Tract Infection
Acute gastroenteritis
Gastrointestinal bleeding and Idiopathic inflammatory bowel disease
Upper and lower respiratory tract Infections
CNS Infections
Antimicrobial drugs

February 2019
School of Medicine, EUC/Clinical Training Manual …. 57
Tuberculosis
Evaluation of full blood count and Iron deficiency anaemia
Thalassemia, sickle cell anaemia and rare forms of anaemia
Asthma
Common kidney conditions
Type I diabetes mellitus
Short stature and hypothyroidism
Arthritis in children
Cervical lymphadenitis
Malignant tumors
Cardiology
Common surgical problems
Common ENT and eye problems
Common orthopedic problems
Behavioral disorders
Genetics
Cushing syndrome
Adrenal Deficiency
Clinical Training VIII (MED520) - Dermatology
Description
Students shadow residents and consultants in departments of dermatology (including
outpatient offices and clinics). They are assigned to patients, whom they follow from
admission to discharge and act as attending physicians, under the supervision of their
clinical instructors. The overall objective of this rotation is for students to familiarize with
the responsibilities of physicians, including obtaining history, performing physical
examination, performing differential diagnoses, proposing investigation and management
plans, observing dermatological surgery, following patients’ daily progress, completing
medical charts and discharging.
The objective of the course is to familiarize students with
The clinical manifestations, diagnosis, medical and surgical management and
prevention of the diseases of
The skin and dermatological system
Course Content
Most frequently encountered skin pathologies.
By obtaining a past clinical history with focus on dermatological pathologies,
identification and expertise to describe the principal cutaneous lesions by means of
identifying the correct symptomatology (basic lesions), indications and interpretation
of the complementary studies used for the diagnosis of dermatological diseases,
especially in the anatomopathological study
Methods of diagnosis (history, physical examination and laboratory tests) of the above
described diseases and conditions
Medical and surgical treatment and prevention of the above described diseases and
conditions
Educational Objectives
Upon successful completion of this course students should be able to:

February 2019
School of Medicine, EUC/Clinical Training Manual …. 58
Identify the most frequently encountered skin pathologies.
Diagnose the most frequently encountered skin pathologies.
Manage the medical-surgical treatment of the most frequently encountered skin
pathologies.
Guidelines
Length: 2 weeks
Site: dermatology department, outpatient clinics, plastic/reconstructive surgery,
ambulatory care unit, burn ICU, private office practice, additional sites, as available.
Orientation: At the start of the clerkship an orientation is given. The clerkship director
or designee discusses the program’s goals and objectives, the responsibilities of the
student, the schedule and assignments to preceptors and residents. The student is
introduced to the key preceptors and staff members in the department.
Schedule: The student must attend scheduled clinical conferences, grand rounds,
morning visits, classes, subspecialty conferences, learning sessions.
Attending Rounds: The student is involved in all patient care activities in the
outpatient facility and inpatient unit.
Preceptor sessions: A preceptor meets with students daily. The preceptor sessions
will include clinical discussions that focus on problem solving, decision making and
adherence to bioethical principals.
Assessment
Grade Components
Medical knowledge 50%
Clinical & Communication skills 40%
Attendance & Professional behavior 10%
Medical Knowledge
Demonstrate knowledge of the principal syndromes and illnesses, their underlying causes
both medically and socially and the various diagnostic and therapeutic options available
to physicians in the care of their patients.
Demonstrate knowledge of the indications for and the ability to interpret standard
diagnostic tests, e.g.; CBC, chemistries, chest x-rays, urinalysis, EKGs, as well as other
relevant specialized tests.
Recognize unusual presentations of disease in elderly patients and demonstrate
understanding of the complexity of providing care for the chronically ill with multiple
medical problems. This should include an understanding of end of life issues, as well as
bioethical, public health and economic considerations which arise in our health care
system.
Demonstrate knowledge of the indications for various levels of care post-discharge, e.g.,
short and long term rehabilitation, long-term skilled nursing facility care, hospice, home
care, etc.
Clinical Skills
Take a comprehensive history and perform a complete physical exam. Formulate a
comprehensive problem list, differential diagnosis; and articulate a basic therapeutic plan,
employing concern for risks, benefits, and costs.
Analyze additional clinical information, lab tests and changes in patients’ clinical status;
note changes in the differential diagnosis or in the diagnostic or therapeutic plans as
circumstances and test results change. Begin to develop proficiency in basic procedures,
such as venipuncture, arterial puncture, nasogastric tube insertion, insertion of intravenous
lines, urinary bladder catheterization, etc.

February 2019
School of Medicine, EUC/Clinical Training Manual …. 59
Communication Skills
Verbal:
Basic competence in comprehensive case presentation
Basic competence in focused case presentation
Basic competence in explaining to a patient a simple diagnostic and therapeutic
plan Basic informed consent scenario for a procedure
Written:
Competence in comprehensive case write-ups
Competence in brief case write-ups
Professional Behavior
Demonstrate a regimen of independent learning through the reading of suggested
basic texts, research via the Internet and through other electronic resources,
maintenance of the patient encounter log and completion of the web-based
educational program requirements.
Demonstrate a commitment to quality, patient safety and self-directed improvement.
Demonstrate competency and comfort in dealing with people of varying racial,
cultural and religious backgrounds
Demonstrate a commitment to treating all patients, families and other caregivers
with respect.
Participate fully with the patient care team and fulfill all responsibilities in a timely
fashion.
Maintain a professional appearance and demeanor.
Demonstrate facility in working in concert with other caregivers, nutritionists
and social workers / discharge planners to obtain optimal, seamless
multidisciplinary care for their patients, both during the hospitalization and after
discharge.
Core Topics & Patients
A. The healthy patient: health promotion and education, disease prevention and screening.
B. Patients with a symptom, sign, abnormal laboratory value or known medical condition
Acne
Rosacea
Hidradenitis suppurativa
Psoriasis
Papulosquamous and inflammatory disorders
Severe cutaneous eruptions
Sexually transmitted diseases
Bacterial, Viral, Fungal, Parasitic infections of the skin
Bullous diseases
Skin lesion description
Skin cancers and precancerous lesions
Eczema-Dermatitis
Major Pediatric Dermatologic diseases
Genetic skin diseases
Scalp, Hair, Nail disorders
Clinical Training IX (MED611) - Obstetrics & Gynecology
Description

February 2019
School of Medicine, EUC/Clinical Training Manual …. 60
Students shadow residents and consultants in departments of obstetrics and gynecology
(including outpatient offices and clinics and maternity departments). They are assigned to
patients, whom they follow from admission to discharge and act as attending physicians,
under the supervision of their clinical instructors. The overall objective of this rotation is for
students to familiarize with the responsibilities of physicians, including obtaining history,
performing physical examination, delivery, proposing investigation and management
plans, following patients’ daily progress, completing medical charts and discharging.
The objective of the course is to familiarize students with
The concepts and practices of obstetrics, including pregnancy, birth and puerperium,
and contraceptive methods
The clinical manifestations, diagnosis, medical and surgical management and
prevention of the diseases of the gynaecological system
Course Content
Pregnancy, birth and puerperium.
Contraception and fertilization methods.
Most frequently encountered gynecological pathologies
o Gynecological cancer and tumors of the genital tract, disturbances of the
menopause, contraception, adolescent gynecology, inflammatory diseases of the
pelvic area, endometriosis, other gynecological diseases, tumors and cancer of
the breast.
Methods of diagnosis (history, physical examination and laboratory tests) of the above
described diseases and conditions
Medical and surgical treatment and prevention of the above described diseases and
conditions
Guidelines
Length: 4 weeks
Site: gastroenterology department, hematology department, outpatient clinics,
endoscopy unit, chemotherapy unit, ambulatory care unit, emergency department,
medical ICU, private office practice, additional sites, as available.
Orientation: At the start of the clerkship an orientation is given. The clerkship
director or designee discusses the program’s goals and objectives, the
responsibilities of the student, the schedule and assignments to preceptors and
residents. The student is introduced to the key preceptors and staff members in
the department.
Schedule: The student must attend scheduled clinical conferences, grand rounds,
morning visits, classes, subspecialty conferences, learning sessions.
Attending Rounds: The student is involved in all patient care activities in the
outpatient facility and inpatient unit.
Preceptor sessions: A preceptor meets with students daily. The preceptor
sessions will include clinical discussions that focus on problem solving, decision
making and adherence to bioethical principals.
Assessment
Grade Components
Medical knowledge 50%
Clinical & Communication skills 40%
Attendance & Professional behavior 10%
Educational Objectives
Upon successful completion of this course students should be able to:
Discuss the characteristics of pregnancy, birth and puerperium.

February 2019
School of Medicine, EUC/Clinical Training Manual …. 61
Carry out a physical examination of pregnant women and supervision of
pregnancy.
Describe the basis of contraception and fertilization methods.
Identify the most frequently encountered gynecological pathologies.
Diagnose the most frequently encountered gynecological pathologies by obtaining
a past medical history and carry out a physical examination with focus on
gynecological pathologies, to indications and interpretations of the complementary
studies used for the diagnosis of gynecological diseases and the changes
occurring in pregnancy, laboratory, imaging, anatomopathological tests.
Manage the medical-surgical treatment of the most frequently encountered
gynecological pathologies.
Medical Knowledge: The student will learn:
Health maintenance and preventive care for women, including age-related issues
in cancer screening, screening for other common adult-onset illnesses,
nutrition, sexual health, vaccination and risk factor identification and
modification.
Acute and chronic conditions common in women’s general and reproductive
health, including their diagnosis and treatment.
Principles of physiology and pharmacology applicable to women from puberty
through their reproductive life and menopause, especially pregnancy and age-
related changes.
Prenatal, intra-partum and post-partum care of normal pregnancy and
common pregnancy-related complications as well as the care of women
with acute or chronic illness throughout pregnancy.
Clinical Skills: The student will demonstrate competence in:
Communication skills: Interacting effectively and sensitively with patients, families,
and with health care teams in verbal and written presentations. Recognize the
important role of patient education in prevention and treatment of disease.
Verbal Presentations: Organize a case presentation to accurately reflect the reason for
the evaluation, the chronology of the history, the details of physical findings,
the differential diagnosis and the suggested initial evaluation. Include age
specific information and precise description of physical findings. Justify the
thought process that led to the diagnostic and therapeutic plan.
Written Documentation: Document the independent clinical thinking of the student.
When using templates, or their own prior documentation, students should carefully
adjust the note to reflect newly completed work and to ensure the note is a
useful addition to the medical record. In settings where students are not
permitted to document in the EMR, an alternative form of documentation needs to
be established and evaluated by a preceptor.
History Taking: patients in more complex situations such as in the emergency and labor
setting, collecting complete and accurate information and focusing appropriately.
Describe how to modify the interview depending on the clinical situation—
inpatient, outpatient, acute and routine settings including Physical Exams which
are complete and focused depending on the indication and condition.
Clinical Problem Solving: Using data from history, physical, labs and studies to
define problems, develop a differential diagnosis, and identify associated risks.
Clinical Decision Making: Incorporating patient data with patient needs and desires when
formulating diagnostic and therapeutic plans incorporating cultural and ethical
issues.

February 2019
School of Medicine, EUC/Clinical Training Manual …. 62
Evidence - Based Medicine Ability to conduct an evidence-based search surrounding
a specific clinical question and to appropriately evaluate the literature to
answer such question.
Self - Education: Recognizing knowledge deficits and learning needs through a
reflective self-assessment process, plan or seek assistance in remediation of
knowledge deficits, develop key critical thinking and problem solving skills. Seek
feedback.
Professional Behavior: The student will be expected to:
Demonstrate compassion, empathy and respect toward patients, including respect
for the patient’s modesty, privacy, confidentiality and cultural beliefs.
Demonstrate communication skills with patients that convey respect, integrity,
flexibility, sensitivity and compassion.
Demonstrate respect for patient attitudes, behaviors and lifestyle, paying
particular attention to cultural, ethnic and socioeconomic influences and values.
Function as an effective member of the health care team, demonstrating
collegiality and respect for all members of the health care team.
Demonstrate a positive attitude and regard for education by demonstrating
intellectual curiosity, initiative, honesty, responsibility, dedication to being
prepared, maturity in soliciting, accepting and acting on feedback, flexibility
when differences of opinion arise and reliability.
Identify and explore personal strengths, weaknesses and goals.
Core Topics
General
Obstetrics
History
Physical exam
Patient write up
Differential Diagnosis and management plan
Preventive care
Professional behavior and communication skills
Domestic violence and sexual assault
Maternal-fetal physiology
Preconception care
Antepartum care - ntrapartum care
Care of Newborn in labor and delivery
Postpartum care
Breastfeeding
h. Abortion (spontaneous, threatened, incomplete, missed)
Hypertensive disorders of pregnancy
Isoimmunization
Multifetal gestation
Normal and abnormal labor m. Preterm labor
Preterm rupture of membranes
Third trimester bleeding
Postpartum hemorrhage
Postdates pregnancy
Fetal growth restriction
Antepartum and intrapartum fetal surveillance
Gynecology
Ectopic pregnancy
February 2019
School of Medicine, EUC/Clinical Training Manual …. 63
Contraception
Sterilization
Abortion
Sexually transmitted diseases
Endometriosis
Chronic pelvic pain
Urinary incontinence
Breast disease
Vulvar disease and neoplasm
Cervical disease and neoplasm
Uterine and ovarian disease and neoplasm
Endocrinology and Infertility
Menarche - Menopause
Amenorrhea - Normal and abnormal uterine bleeding
Infertility
Hirsutism and Virilization
Diagnosis by Imaging (MED322)
Description
Students familiarize with the basic concepts of imaging methods and with their use in
everyday clinical practice.
The objective of the course is to familiarize students with
The fundamentals of diagnostic image interpretation and clinical indications for
imaging examinations and special procedures
The principles of protection from ionizing radiation
Course Content
Fundamentals of the interaction of radiation and the human organism.
Indications and contra-indications of the various imaging diagnostic procedures.
Techniques used to obtain diagnostic images.
Interpretation of the diagnostic images.
Criteria for radiological protection.
Principles of digital technology.
Educational Objectives
Upon successful completion of this course students should be able to:
Describe the fundamentals of the interaction of radiation with the human organism.
Assess and define the indications and contra-indications of the various diagnostic
imaging procedures.
Describe the diagnostic imaging techniques.
Describe the basic semiology used in the various diagnostic procedures involving
imaging techniques.
Evaluate the radiographic images obtained.
Apply the recommendations for radiological protection against ionizing radiation
utilized in diagnostic and therapeutic procedures.
Discuss the principles of digital technology as applied to diagnostic imaging.
Guidelines

February 2019
School of Medicine, EUC/Clinical Training Manual …. 64
Length: 1 week
Site: imaging/radiology units including CT, MRI, radiography, PET-CT, nuclear
medicine, interventional radiology, additional sites, as available.
Orientation: At the start of the clerkship an orientation is given. The clerkship director
or designee discusses the program’s goals and objectives, the responsibilities of the
student, the schedule and assignments to preceptors and residents. The student is
introduced to the key preceptors and staff members in the department.
Schedule: The student must attend scheduled classes learning sessions.
Preceptor sessions: A preceptor meets with students daily. The preceptor sessions
will include clinical discussions that focus on problem solving, decision making and
adherence to bioethical principals.
Assessment
Grade Components
Medical knowledge 50%
Clinical & Communication skills 40%
Attendance & Professional behavior 10%
Core topics & Medical Knowledge
Abdominal Ultrasound
Basic interpretation of abdominal ultrasound
Basic interpretation of abdominal CT
Basic interpretation of chest CT
Basic view box images – normal and abnormal
Breast imaging
Chest imaging
Interpretation of chest x-ray
Interventional Radiology
Radiological radiation, exposure & safety
Professional Behavior
Demonstrate a regimen of independent learning through the reading of suggested
basic texts, research via the Internet and through other electronic resources,
maintenance of the patient encounter log and completion of the web-based
educational program requirements.
Demonstrate a commitment to quality, patient safety and self-directed improvement.
Demonstrate competency and comfort in dealing with people of varying racial,
cultural and religious backgrounds
Demonstrate a commitment to treating all patients, families and other caregivers with
respect.
Participate fully with the patient care team and fulfill all responsibilities in a timely
fashion.
Maintain a professional appearance and demeanor.
Demonstrate facility in working in concert with other caregivers, nutritionists and
social workers / discharge planners to obtain optimal, seamless multidisciplinary
care for their patients, both during the hospitalization and after discharge.
Clinical Bioethics & Legal Medicine (MED428)
The objective of the course is to familiarize students with

February 2019
School of Medicine, EUC/Clinical Training Manual …. 65
The essential values and other elements of the medical profession, including the
principal ethics and legal responsibilities.
The application of the principles of social justice to professional practice and the
respect to the autonomy, privacy, beliefs and culture of the patient.
The methods and applications of forensic medicine and medical jurisprudence
Course Content
Legal foundations of the practice of the medical profession.
Ethical aspects of informed consent and confidentiality.
Social and legal implications of death.
Normal evolution of changes in the cadaver and postmortem diagnostic techniques.
Basic aspects of the medical criminal investigation.
Medical-legal documents.
Professional values. Professional competences.
Fundamentals of medical ethics.
Ethical conflicts.
Educational Objectives
Upon successful completion of this course students should be able to:
Describe the legal fundamentals applied to the practice of the medical profession.
Adhere to and apply the professional values of excellence, altruism, the sense of duty,
responsibility, integrity and honesty to the practice of the medical profession.
Identify the need to maintain professional competences.
Demonstrate that their approach to medical professional practice respects the
autonomy, the beliefs and culture of the patient.
Discuss the ethical aspects of informed consent and confidentiality.
Demonstrate that they recognize, analyze and can advise on ethical conflicts.
Demonstrate that they analyze the ethical/legal aspects of biomedical research.
Identify, diagnose and give advice on the management of physical and mental injury.
Discuss and analyze the social and legal implications of death.
Describe and identify the normal evolution of the cadaver and the techniques used for
postmortem diagnosis.
Identify the basic aspects of medical criminal investigation.
Draw up medical-legal documents.
Demonstrate that they comprehend and describe the fundamentals and principles of
bioethics.
Guidelines
Length: 1 week
Site: pathology labs, mortuary, private office practice, additional sites, as available.
Orientation: At the start of the clerkship an orientation is given. The clerkship director
or designee discusses the program’s goals and objectives, the responsibilities of the
student, the schedule and assignments to preceptors and residents. The student is
introduced to the key preceptors and staff members in the department.
Schedule: The student must attend scheduled clinical conferences, grand rounds,
classes, subspecialty conferences, learning sessions.
Preceptor sessions: A preceptor meets with students daily. The preceptor sessions
will include clinical discussions that focus on problem solving, decision making and
adherence to bioethical principals.
Assessment

February 2019
School of Medicine, EUC/Clinical Training Manual …. 66
Grade Components
Medical Knowledge –(Subjective assessment by preceptors, attending, etc & OSCE)
Core topics & Medical Knowledge
Fundamentals of medical ethics.
Decisions at the Start and End of Life.
Consent.
Confidentiality and Disclosure/ Medical Negligence.
Diagnosing death; signs and changes after death
The scene of crime: Role of the forensic pathologist and clinical forensic practitioner
The autopsy
The Coroner’s system: Death certificates; Inquest; Disposal of the dead.
Sudden and unexpected natural deaths
Identification
Mass disasters
Exhumations (single and multiple graves)
Human Rights and torture investigations
Assessment of trauma
Asphyxia and drowning
Deaths and the environment
Fires and explosions
Clinical and pathological aspects of alcohol and drug abuse
Preparation of reports and giving evidence in court
Paediatric forensic pathology
Communication Skills
Verbal:
Basic competence in comprehensive case presentation
Basic competence in focused case presentation
Basic competence in explaining to a patient a simple diagnostic and therapeutic
plan Basic informed consent scenario for a procedure
Written:
Competence in comprehensive case write-ups
Competence in brief case write-ups
Professional Behavior
Demonstrate a regimen of independent learning through the reading of suggested
basic texts, research via the Internet and through other electronic resources,
maintenance of the patient encounter log and completion of the web-based
educational program requirements.
Demonstrate a commitment to quality, patient safety and self-directed
improvement.
Demonstrate competency and comfort in dealing with people of varying racial,
cultural and religious backgrounds
Demonstrate a commitment to treating all patients, families and other caregivers
with respect.
Participate fully with the patient care team and fulfill all responsibilities in a timely
fashion.
Maintain a professional appearance and demeanor.
Demonstrate facility in working in concert with other caregivers, nutritionists
and social workers / discharge planners to obtain optimal, seamless

February 2019
School of Medicine, EUC/Clinical Training Manual …. 67
multidisciplinary care for their patients, both during the hospitalization and after
discharge.
Primary Care (MED631)
Description
Students familiarize with the essentials of primary care and its various levels of care,
including primary prevention of illness, managing the patient and the healthy person,
cooperation with other health and welfare services and with other specialists, visiting home
care, long-term care, nursing homes.
The objective of the course is to familiarize students with
The diagnosis, management and prevention of the most common diseases
encountered in primary care
The special features of the doctor-patient relationship in primary care
The functions and services provided by primary care
Course Content
Primary care and its relationships with the various levels of care.
Promotion of health and prevention of illness during the various stages of life.
Management of the patient and the healthy person, taking into account their
psychological, personal, family, occupational and social circumstances
The family and the interaction of the familial environment with health promotion and
the natural history of disease in the community
Community oriented primary care (COPC): health needs assessment and outreach
programmes in the catchment area of primary care
Cooperation with other health and welfare services delivering care to the population
Most frequently encountered reasons for consultations in the community.
o Chronic conditions, acute & life threatening conditions, home care
Educational Objectives
Upon successful completion of this course students should be able to:
Discuss the structure and function of Primary Care and its relationship to the various
levels of care.
Describe the vital environment of the sick persons and the interaction of education
and culture in medical care.
Explain the principal means used to promote health and prevent illness during the
different stages of life.
Identify the most frequent reasons claimed for consultation in the community.
Establish an action plan focusing on the individual needs of the patient, his/her family
and social environment.
Guidelines
Length: 4 weeks
Site: gastroenterology department, hematology department, outpatient clinics,
endoscopy unit, chemotherapy unit, ambulatory care unit, emergency department,
medical ICU, private office practice, additional sites, as available.
Orientation: At the start of the clerkship an orientation is given. The clerkship director
or designee discusses the program’s goals and objectives, the responsibilities of the

February 2019
School of Medicine, EUC/Clinical Training Manual …. 68
student, the schedule and assignments to preceptors and residents. The student is
introduced to the key preceptors and staff members in the department.
Schedule: The student must attend scheduled clinical conferences, grand rounds,
morning visits, classes, subspecialty conferences, learning sessions.
Attending Rounds: The student is involved in all patient care activities in the outpatient
facility and inpatient unit.
Preceptor sessions: A preceptor meets with students daily. The preceptor sessions
will include clinical discussions that focus on problem solving, decision making and
adherence to bioethical principals.
Assessment
Grade Components
Medical knowledge 50%
Clinical & Communication skills 40%
Attendance & Professional behavior 10%
Medical Knowledge
Demonstrate knowledge of the principal syndromes and illnesses, their underlying causes
both medically and socially and the various diagnostic and therapeutic options available
to physicians in the care of their patients.
Demonstrate knowledge of the indications for and the ability to interpret standard
diagnostic tests, e.g.; CBC, chemistries, chest x-rays, urinalysis, EKGs, as well as other
relevant specialized tests.
Recognize unusual presentations of disease in elderly patients and demonstrate
understanding of the complexity of providing care for the chronically ill with multiple
medical problems. This should include an understanding of end of life issues, as well as
bioethical, public health and economic considerations, which arise in our health care
system.
Demonstrate knowledge of the indications for various levels of care post-discharge, e.g.,
short and long term rehabilitation, long-term skilled nursing facility care, hospice, home
care, etc.

February 2019
School of Medicine, EUC/Clinical Training Manual …. 69
Clinical Skills
Take a comprehensive history and perform a complete physical exam. Formulate a
comprehensive problem list, differential diagnosis; and articulate a basic therapeutic plan,
employing concern for risks, benefits, and costs.
Analyze additional clinical information, lab tests and changes in patients’ clinical status;
note changes in the differential diagnosis or in the diagnostic or therapeutic plans as
circumstances and test results change. Begin to develop proficiency in basic procedures,
such as venipuncture, arterial puncture, nasogastric tube insertion, insertion of intravenous
lines, urinary bladder catheterization, etc.
Clinical examination, including recognition of common signs of gastrointestinal
diseases: abdominal examination and findings, skin and mucosa, liver and spleen
evaluation, volume status assessment
Common gastrointestinal disorders (see Part D): recognition, evaluation, diagnosis,
management
Evaluation of endoscopy findings
History taking and focus on risk factors for digestive diseases, family history, social
and occupational history
Clinical examination, including recognition of common signs of hematological
diseases: skin and mucosa, lymph nodes, liver and spleen evaluation, immune status
Common hematological disorders (see Part D): recognition, evaluation, diagnosis,
management
History taking and focus on risk factors for hematological diseases, family history,
social and occupational history
Peripheral blood findings and smear evaluation
Arterial blood gases
Blood culture
Blood glucose examination using finger stick
Blood transfusion
Hand washing (including surgical scrubbing)
Intramuscular injection
Intravenous injection
Nasogastric tube placement
Oxygen supplementation
Peripheral venous catheter placement
Rectal examination
Respiratory secretions culture
Setting up syringe driver
Skin suturing
Skin swabs for culture
Subcutaneous injections
Suction of respiratory secretions
Swabs from nose, throat and skin
Urinary catheter insertion, female
Urinary catheter insertion, male
Urinary catheter removal
Urinalysis using urine stick
Vein puncture and blood drawing
Wound care and basic wound dressing

February 2019
School of Medicine, EUC/Clinical Training Manual …. 70
Communication Skills
Verbal:
Basic competence in comprehensive case presentation
Basic competence in focused case presentation
Basic competence in explaining to a patient a simple diagnostic and therapeutic
plan Basic informed consent scenario for a procedure
Written:
Competence in comprehensive case write-ups
Competence in brief case write-ups
Professional Behavior
Demonstrate a regimen of independent learning through the reading of suggested
basic texts, research via the Internet and through other electronic resources,
maintenance of the patient encounter log and completion of the web-based
educational program requirements.
Demonstrate a commitment to quality, patient safety and self-directed improvement.
Demonstrate competency and comfort in dealing with people of varying racial,
cultural and religious backgrounds
Demonstrate a commitment to treating all patients, families and other caregivers with
respect.
Participate fully with the patient care team and fulfill all responsibilities in a timely
fashion.
Maintain a professional appearance and demeanor.
Demonstrate facility in working in concert with other caregivers, nutritionists and
social workers / discharge planners to obtain optimal, seamless multidisciplinary
care for their patients, both during the hospitalization and after discharge.
Core Topics & Patients
A. The healthy patient: health promotion and education, disease prevention and screening.
B. Patients with a symptom, sign, abnormal laboratory value or known medical condition
Acute abdominal pain
Ascites
Colostomy
Diarrhea
Functional disorder (irritable bowel syndrome, constipation, diarrhea)
Gastroesophageal reflux disease (GERD)
Hematemesis
Hematochezia
Hepatitis - Elevated liver enzymes (acute liver damage)
Inflammatory bowel disease (Crohn’s disease, Ulcerative colitis)
Liver cirrhosis
Pancreatitis
Peptic ulcer disease
Upper gastrointestinal bleeding
Vomiting
Anemia
“B” symptomatology
Bone marrow biopsy
Idiopathic thrombopenic purpura / Thrombotic thrombopenic purpura
Leukemia (AML, ALL, CML, CLL)
Lymphadenopathy
Multiple myeloma
Myelodysplastic syndromes (MDS)

February 2019
School of Medicine, EUC/Clinical Training Manual …. 71
Splenomegaly
Thalassemia syndromes
Abdominal pain
Anemia
Dyspepsia
GI bleeding
Irritable bowel
Jaundice
Weight loss
Clinical Training X (MED621) - Ophthalmology
Description
Students shadow residents and consultants in departments of ophthalmology (including
outpatient offices and clinics and maternity departments). They are assigned to patients,
whom they follow from admission to discharge and act as attending physicians, under the
supervision of their clinical instructors. The overall objective of this rotation is for students
to familiarize with the responsibilities of physicians, including obtaining history, performing
physical examination, observing specialized diagnostic and invasive methods in
ophthalmology, proposing investigation and management plans, following patients’ daily
progress, completing medical charts and discharging.
The objective of the course is to familiarize students with
The clinical manifestations, diagnosis, medical and surgical management and
prevention of the diseases of the ophthalmologic system
Course Content
Most frequently encountered ophthalmological pathologies.
Palpebral and lacrimal pathologies, pathologies of the cornea, the lens, the retina,
the sclera, the visual pathways and other related ophthalmological pathologies.
Methods of diagnosis (history, physical examination and laboratory tests) of the
above described diseases and conditions
Medical and surgical treatment and prevention of the above described diseases
and conditions
Educational Objectives
Upon successful completion of this course students should be able to:
Identify the most frequently encountered ophthalmological pathologies
Diagnose the most frequently encountered ophthalmological pathologies by
obtaining a past clinical history and carrying out physical examination (ocular
fundus, visual acuity, campimetry, etc) with focus on ophthalmological pathologies.
Manage the medical-surgical treatment of the most frequently encountered
ophthalmological pathologies.
Guidelines
Length: 4 weeks
Site: gastroenterology department, hematology department, outpatient clinics,
endoscopy unit, chemotherapy unit, ambulatory care unit, emergency department,
medical ICU, private office practice, additional sites, as available.

February 2019
School of Medicine, EUC/Clinical Training Manual …. 72
Orientation: At the start of the clerkship an orientation is given. The clerkship
director or designee discusses the program’s goals and objectives, the
responsibilities of the student, the schedule and assignments to preceptors and
residents. The student is introduced to the key preceptors and staff members in
the department.
Schedule: The student must attend scheduled clinical conferences, grand rounds,
morning visits, classes, subspecialty conferences, learning sessions.
Attending Rounds: The student is involved in all patient care activities in the
outpatient facility and inpatient unit.
Preceptor sessions: A preceptor meets with students daily. The preceptor
sessions will include clinical discussions that focus on problem solving, decision
making and adherence to bioethical principals.
Assessment
Grade Components
Medical knowledge 50%
Clinical & Communication skills 40%
Attendance & Professional behavior 10%
Medical Knowledge
Demonstrate knowledge of the principal syndromes and illnesses, their underlying
causes both medically and socially and the various diagnostic and therapeutic options
available to physicians in the care of their patients.
Demonstrate knowledge of the indications for and the ability to interpret standard
diagnostic tests, e.g.; CBC, chemistries, chest x-rays, urinalysis, EKGs, as well as
other relevant specialized tests.
Recognize unusual presentations of disease in elderly patients and demonstrate
understanding of the complexity of providing care for the chronically ill with multiple
medical problems. This should include an understanding of end of life issues, as well
as bioethical, public health and economic considerations which arise in our health care
system.
Demonstrate knowledge of the indications for various levels of care post-discharge,
e.g., short and long term rehabilitation, long-term skilled nursing facility care, hospice,
home care, etc.
Clinical Skills
Take a comprehensive history and perform a complete physical exam. Formulate a
comprehensive problem list, differential diagnosis; and articulate a basic therapeutic plan,
employing concern for risks, benefits, and costs.
Analyze additional clinical information, lab tests and changes in patients’ clinical status;
note changes in the differential diagnosis or in the diagnostic or therapeutic plans as
circumstances and test results change. Begin to develop proficiency in basic procedures,
such as venipuncture, arterial puncture, nasogastric tube insertion, insertion of intravenous
lines, urinary bladder catheterization, etc.
Arterial blood gases
Blood culture
Blood glucose examination using finger stick
Blood transfusion
Hand washing (including surgical scrubbing)
Intramuscular injection
Intravenous injection
Nasogastric tube placement

February 2019
School of Medicine, EUC/Clinical Training Manual …. 73
Oxygen supplementation
Peripheral venous catheter placement
Rectal examination
Respiratory secretions culture
Setting up syringe driver
Skin suturing
Skin swabs for culture
Subcutaneous injections
Suction of respiratory secretions
Swabs from nose, throat and skin
Urinary catheter insertion, female
Urinary catheter insertion, male
Urinary catheter removal
Urinalysis using urine stick
Vein puncture and blood drawing
Wound care and basic wound dressing
Communication Skills
Verbal:
Basic competence in comprehensive case presentation
Basic competence in focused case presentation
Basic competence in explaining to a patient a simple diagnostic and therapeutic
plan Basic informed consent scenario for a procedure
Written:
Competence in comprehensive case write-ups
Competence in brief case write-ups
Professional Behavior
Demonstrate a regimen of independent learning through the reading of suggested
basic texts, research via the Internet and through other electronic resources,
maintenance of the patient encounter log and completion of the web-based
educational program requirements.
Demonstrate a commitment to quality, patient safety and self-directed
improvement.
Demonstrate competency and comfort in dealing with people of varying racial,
cultural and religious backgrounds
Demonstrate a commitment to treating all patients, families and other caregivers
with respect.
Participate fully with the patient care team and fulfill all responsibilities in a timely
fashion.
Maintain a professional appearance and demeanor.
Demonstrate facility in working in concert with other caregivers, nutritionists
and social workers / discharge planners to obtain optimal, seamless
multidisciplinary care for their patients, both during the hospitalization and after
discharge.

February 2019
School of Medicine, EUC/Clinical Training Manual …. 74
Core Topics & Patients
A. The healthy patient: health promotion and education, disease prevention and screening.
B. Patients with a symptom, sign or abnormal laboratory value
Abdominal pain
Altered mental status
Anemia
Back pain
Chest pain
Cough
Chronic pain
Dyspepsia
Dyspnea
Dysuria
Fever
Fluid, electrolyte, and acid-base disorders
GI bleeding
Hemoptysis
Irritable bowel
Jaundice
Knee pain
Rash
Upper respiratory complaints
Weight loss
C. Patients presenting with a known medical condition.
Acute MI
Acute renal failure and chronic kidney disease
Asthma
Common cancers
COPD
Diabetes mellitus
Dyslipidemia
CHF
HIV
Hypertension
Inflammatory bowel disease
Liver disease
Nosocomial infection
Obesity
Peptic ulcer disease
Pneumonia
Skin and soft tissue infections
Substance abuse
Thyroid disease
Venous thromboembolism
Geriatric Issues
Cognitive Impairment
Osteoporosis
Polypharmacy
Incontinence
Falls, gait and balance problems

February 2019
School of Medicine, EUC/Clinical Training Manual …. 75
Failure to thrive
Pressure ulcers
Sensory impairments
Sleep disorders
Depression
Pain
Elder abuse and neglect
End-of-life
Clinical Training XI (MED612) - Otorhinolaryngology
Description
Students shadow residents and consultants in departments of ENT (including outpatient
offices and clinics). They are assigned to patients, whom they follow from admission to
discharge and act as attending physicians, under the supervision of their clinical
instructors. The overall objective of this rotation is for students to familiarize with the
responsibilities of physicians, including obtaining history, performing physical examination,
observing specialized diagnostic and invasive methods in otorhinolaryngology including
surgery, proposing investigation and management plans, following patients’ daily
progress, completing medical charts and discharging.
The objective of the course is to familiarize students with
The clinical manifestations, diagnosis, medical and surgical management and
prevention of the diseases of the Ear, Nose and Throat
Course Content
Most frequently encountered pathologies of the ear, nose and throat.
Diseases of external, middle and inner ear, hearing loss, vertigo, tinnitus, facial nerve
disorders, inflammations and tumors of the nose, epistaxis, injuries, deformities,
inflammatory diseases and neoplastic lesions of the pharynx and larynx , voice
disorders and dysphagia
Methods of diagnosis (history, physical examination and laboratory tests) of the above
described diseases and conditions
Medical and surgical treatment and prevention of the above described diseases and
conditions
Educational Objectives
Upon successful completion of this course students should be able to:
Identify the most frequently encountered pathologies affecting the ear, nose and
throat.
Diagnose the most frequently encountered pathologies of the ear, nose and throat
by obtaining a past clinical history and carrying out physical examinations with
focus on the otorrhinolaryngological pathologies, indications and interpretation of
the principal complementary studies in otorrhinolaryngology, audiometry,
otoscopy, rhinoscopy, etc.
Manage the medical-surgical treatment of the most frequently encountered
pathologies of the ear, nose and throat.
Guidelines
Length: 4 weeks

February 2019
School of Medicine, EUC/Clinical Training Manual …. 76
Site: gastroenterology department, hematology department, outpatient clinics,
endoscopy unit, chemotherapy unit, ambulatory care unit, emergency department,
medical ICU, private office practice, additional sites, as available.
Orientation: At the start of the clerkship an orientation is given. The clerkship director
or designee discusses the program’s goals and objectives, the responsibilities of
the student, the schedule and assignments to preceptors and residents. The student
is introduced to the key preceptors and staff members in the department.
Schedule: The student must attend scheduled clinical conferences, grand rounds,
morning visits, classes, subspecialty conferences, learning sessions.
Attending Rounds: The student is involved in all patient care activities in the
outpatient facility and inpatient unit.
Preceptor sessions: A preceptor meets with students daily. The preceptor sessions
will include clinical discussions that focus on problem solving, decision making and
adherence to bioethical principals.
Assessment
Grade Components
Medical knowledge 50%
Clinical & Communication skills 40%
Attendance & Professional behavior 10%
Medical Knowledge
Demonstrate knowledge of the principal syndromes and illnesses, their underlying causes
both medically and socially and the various diagnostic and therapeutic options available
to physicians in the care of their patients.
Demonstrate knowledge of the indications for and the ability to interpret standard
diagnostic tests, e.g.; CBC, chemistries, chest x-rays, urinalysis, EKGs, as well as other
relevant specialized tests.
Recognize unusual presentations of disease in elderly patients and demonstrate
understanding of the complexity of providing care for the chronically ill with multiple
medical problems. This should include an understanding of end of life issues, as well as
bioethical, public health and economic considerations which arise in our health care
system.
Demonstrate knowledge of the indications for various levels of care post-discharge, e.g.,
short and long term rehabilitation, long-term skilled nursing facility care, hospice, home
care, etc.
Clinical Skills
Take a comprehensive history and perform a complete physical exam. Formulate a
comprehensive problem list, differential diagnosis; and articulate a basic therapeutic plan,
employing concern for risks, benefits, and costs.
Analyze additional clinical information, lab tests and changes in patients’ clinical status;
note changes in the differential diagnosis or in the diagnostic or therapeutic plans as
circumstances and test results change. Begin to develop proficiency in basic procedures,
such as venipuncture, arterial puncture, nasogastric tube insertion, insertion of intravenous
lines, urinary bladder catheterization, etc.
Arterial blood gases
Blood culture
Blood glucose examination using finger stick
Blood transfusion
Hand washing (including surgical scrubbing)
Intramuscular injection

February 2019
School of Medicine, EUC/Clinical Training Manual …. 77
Intravenous injection
Nasogastric tube placement
Oxygen supplementation
Peripheral venous catheter placement
Rectal examination
Respiratory secretions culture
Setting up syringe driver
Skin suturing
Skin swabs for culture
Subcutaneous injections
Suction of respiratory secretions
Swabs from nose, throat and skin
Urinary catheter insertion, female
Urinary catheter insertion, male
Urinary catheter removal
Urinalysis using urine stick
Vein puncture and blood drawing
Wound care and basic wound dressing
Communication Skills
Verbal:
Basic competence in comprehensive case presentation
Basic competence in focused case presentation
Basic competence in explaining to a patient a simple diagnostic and therapeutic
plan Basic informed consent scenario for a procedure
Written:
Competence in comprehensive case write-ups
Competence in brief case write-ups
Professional Behavior
Demonstrate a regimen of independent learning through the reading of suggested
basic texts, research via the Internet and through other electronic resources,
maintenance of the patient encounter log and completion of the web-based
educational program requirements.
Demonstrate a commitment to quality, patient safety and self-directed
improvement.
Demonstrate competency and comfort in dealing with people of varying racial,
cultural and religious backgrounds
Demonstrate a commitment to treating all patients, families and other caregivers
with respect.
Participate fully with the patient care team and fulfill all responsibilities in a timely
fashion.
Maintain a professional appearance and demeanor.
Demonstrate facility in working in concert with other caregivers, nutritionists
and social workers / discharge planners to obtain optimal, seamless
multidisciplinary care for their patients, both during the hospitalization and after
discharge.
Core Topics & Patients
A. The healthy patient: health promotion and education, disease prevention and screening.
B. Patients with a symptom, sign or abnormal laboratory value
Abdominal pain
Altered mental status

February 2019
School of Medicine, EUC/Clinical Training Manual …. 78
Anemia
Back pain
Chest pain
Cough
Chronic pain
Dyspepsia
Dyspnea
Dysuria
Fever
Fluid, electrolyte, and acid-base disorders
GI bleeding
Hemoptysis
Irritable bowel
Jaundice
Knee pain
Rash
Upper respiratory complaints
Weight loss
C. Patients presenting with a known medical condition.
Acute MI
Acute renal failure and chronic kidney disease
Asthma
Common cancers
COPD
Diabetes mellitus
Dyslipidemia
CHF
HIV
Hypertension
Inflammatory bowel disease
Liver disease
Nosocomial infection
Obesity
Peptic ulcer disease
Pneumonia
Skin and soft tissue infections
Substance abuse
Thyroid disease
Venous thromboembolism
Geriatric Issues
Cognitive Impairment
Osteoporosis
Polypharmacy
Incontinence
Falls, gait and balance problems
Failure to thrive
Pressure ulcers
Sensory impairments
Sleep disorders
Depression
Pain

February 2019
School of Medicine, EUC/Clinical Training Manual …. 79
Elder abuse and neglect
End-of-life
Clinical Training XII (MED622) - ER, Toxicology, Oncology & Palliative Care
Description
Students shadow residents and consultants in departments of accidents & emergency and
oncology (including outpatient offices and clinics) and also visit palliative care settings. The overall
objective of this rotation is for students to familiarize with the various structures involved and with
the responsibilities of physicians, including practical and theoretical matters.
The objective of the course is to familiarize students with
The clinical manifestations, diagnosis, medical and surgical management and
prevention of the neoplastic diseases, including palliative care
The management of medical emergencies and acute intoxications
Course Content
Oncological diseases.
Cancer of the respiratory, digestive, nervous, endocrine, musculoskeletal,
urinary, gynecological systems, the skin, and other systems
Leukaemia and other hematologic malignancies.
Toxicology (different toxicological agents, poisoning and its management,
environmental pollutants, including pesticides, forensic toxicology).
Medical-surgical emergencies
Acute emergencies and life-threatening conditions
Management of the injured in major accidents and natural disasters
Palliative medicine and treatment of chronic pain
Methods of diagnosis (history, physical examination and laboratory tests) of above
diseases and conditions
Medical and surgical treatment and prevention of above diseases and conditions
Educational Objectives
Upon successful completion of this course students should be able to:
Identify, diagnose and manage the treatment of oncological diseases.
Identify, diagnose and manage the treatment of the principal intoxications.
Identify, diagnose and manage the treatment of conditions associated with
threatening life situations.
To acquire the expertise to diagnose a cardiorespiratory arrest and to carry out the
basic techniques for cardiopulmonary resuscitation. To gain knowledge about the
techniques for advanced vital support.
Identify the principles and basics of palliative medicine, and manage palliative care
cases including basic aspects of home care.
Guidelines
Length: 4 weeks
Site: gastroenterology department, hematology department, outpatient clinics,
endoscopy unit, chemotherapy unit, ambulatory care unit, emergency department,
medical ICU, private office practice, additional sites, as available.
Orientation: At the start of the clerkship an orientation is given. The clerkship
director or designee discusses the program’s goals and objectives, the

February 2019
School of Medicine, EUC/Clinical Training Manual …. 80
responsibilities of the student, the schedule and assignments to preceptors and
residents. The student is introduced to the key preceptors and staff members in the
department.
Schedule: The student must attend scheduled clinical conferences, grand rounds,
morning visits, classes, subspecialty conferences, learning sessions.
Attending Rounds: The student is involved in all patient care activities in the
outpatient facility and inpatient unit.
Preceptor sessions: A preceptor meets with students daily. The preceptor
sessions will include clinical discussions that focus on problem solving, decision
making and adherence to bioethical principals.
Assessment
Grade Components
Medical knowledge 50%
Clinical & Communication skills 40%
Attendance & Professional behavior 10%
Medical Knowledge
Demonstrate knowledge of the principal syndromes and illnesses, their underlying causes
both medically and socially and the various diagnostic and therapeutic options available
to physicians in the care of their patients.
Demonstrate knowledge of the indications for and the ability to interpret standard
diagnostic tests, e.g.; CBC, chemistries, chest x-rays, urinalysis, EKGs, as well as other
relevant specialized tests.
Recognize unusual presentations of disease in elderly patients and demonstrate
understanding of the complexity of providing care for the chronically ill with multiple
medical problems. This should include an understanding of end of life issues, as well as
bioethical, public health and economic considerations which arise in our health care
system.
Demonstrate knowledge of the indications for various levels of care post-discharge, e.g.,
short and long term rehabilitation, long-term skilled nursing facility care, hospice, home
care, etc.
Clinical Skills
Take a comprehensive history and perform a complete physical exam. Formulate a
comprehensive problem list, differential diagnosis; and articulate a basic therapeutic plan,
employing concern for risks, benefits, and costs.
Analyze additional clinical information, lab tests and changes in patients’ clinical status;
note changes in the differential diagnosis or in the diagnostic or therapeutic plans as
circumstances and test results change. Begin to develop proficiency in basic procedures,
such as venipuncture, arterial puncture, nasogastric tube insertion, insertion of intravenous
lines, urinary bladder catheterization, etc.
Arterial blood gases
Blood culture
Blood glucose examination using finger stick
Blood transfusion
Hand washing (including surgical scrubbing)
Intramuscular injection
Intravenous injection
Nasogastric tube placement
Oxygen supplementation
Peripheral venous catheter placement

February 2019
School of Medicine, EUC/Clinical Training Manual …. 81
Rectal examination
Respiratory secretions culture
Setting up syringe driver
Skin suturing
Skin swabs for culture
Subcutaneous injections
Suction of respiratory secretions
Swabs from nose, throat and skin
Urinary catheter insertion, female
Urinary catheter insertion, male
Urinary catheter removal
Urinalysis using urine stick
Vein puncture and blood drawing
Wound care and basic wound dressing
Communication Skills
Verbal:
Basic competence in comprehensive case presentation
Basic competence in focused case presentation
Basic competence in explaining to a patient a simple diagnostic and therapeutic
plan Basic informed consent scenario for a procedure
Written:
Competence in comprehensive case write-ups
Competence in brief case write-ups
Professional Behavior
Demonstrate a regimen of independent learning through the reading of suggested
basic texts, research via the Internet and through other electronic resources,
maintenance of the patient encounter log and completion of the web-based
educational program requirements.
Demonstrate a commitment to quality, patient safety and self-directed
improvement.
Demonstrate competency and comfort in dealing with people of varying racial,
cultural and religious backgrounds
Demonstrate a commitment to treating all patients, families and other caregivers
with respect.
Participate fully with the patient care team and fulfill all responsibilities in a timely
fashion.
Maintain a professional appearance and demeanor.
Demonstrate facility in working in concert with other caregivers, nutritionists
and social workers / discharge planners to obtain optimal, seamless
multidisciplinary care for their patients, both during the hospitalization and after
discharge.
Core Topics & Patients
A. The healthy patient: health promotion and education, disease prevention and screening.
B. Patients with a symptom, sign or abnormal laboratory value
Abdominal pain
Altered mental status
Anemia
Back pain
Chest pain
Cough

February 2019
School of Medicine, EUC/Clinical Training Manual …. 82
Chronic pain
Dyspepsia
Dyspnea
Dysuria
Fever
Fluid, electrolyte, and acid-base disorders
GI bleeding
Hemoptysis
Irritable bowel
Jaundice
Knee pain
Rash
Upper respiratory complaints
Weight loss
Patients presenting with a known medical condition.
Acute MI
Acute renal failure and chronic kidney disease
Asthma
Common cancers
COPD
Diabetes mellitus
Dyslipidemia
CHF
HIV
Hypertension
Inflammatory bowel disease
Liver disease
Nosocomial infection
Obesity
Peptic ulcer disease
Pneumonia
Skin and soft tissue infections
Substance abuse
Thyroid disease
Venous thromboembolism
Geriatric Issues
Cognitive Impairment
Osteoporosis
Polypharmacy
Incontinence
Falls, gait and balance problems
Failure to thrive
Pressure ulcers
Sensory impairments
Sleep disorders
Depression
Pain
Elder abuse and neglect
End-of-life

February 2019
School of Medicine, EUC/Clinical Training Manual …. 83
Additional Requirements
Medical Therapeutics (MED530)
The objective of the course is to familiarize students with
The methods of administering medical treatments, the safe prescription of
pharmaceutical agents and the process of pharmacovigilance
Course Content
Prescription and administration of the principal pharmacological groups
Anti-inflammatory-drugs, analgesics, opioids and CNS stimulants, drugs acting on
nervous system, anxiolytics and hypnotics, neuroleptics, anti-depressants, anti-
epileptics, drugs used in anesthesia.
Therapeutic supervision of drugs.
Adherence to treatment.
Pharmacovigilance and pharmacoeconomics.
Clinical trials: fundamentals of design, implementation and evaluation of the outcomes
Educational Objectives
Upon successful completion of this course students should be able to:
Prescribe and appropriately administer the principal groups of pharmacological
agents.
Explain the fundamentals applied in the therapeutic supervision of drugs.
Describe the concepts of adherence to treatment, its indications, implications and
complications/adverse effects related to administrations.
Discuss the current systems of pharmacovigilance.
Explain the fundamentals of pharmacoeconomics.
Outline the development of procedures used in clinical trials.
Symptoms & Interpretation of Complementary Examination Procedures (MED661)
The objective of the course is to familiarize students with
The methods, applications and interpretation of diagnostic techniques
Course Content
Relationship between risk/benefit and cost/effectiveness of the diagnostic and therapeutic
procedures.
Integration of knowledge on:
o Indications and limitations of the various complementary examinations.
o Procedures and means required to carry out diagnostic explorations.
o Interpretation of the results obtained by the diagnostic tests.
Educational Objectives
Upon successful completion of this course students should be able to:
Accurately assess the risk/benefit and cost/effectiveness ratios of diagnostic
procedures.

February 2019
School of Medicine, EUC/Clinical Training Manual …. 84
Integrate and correlate the expertise acquired from other study courses to the
indications of the various complementary examinations used in medicine:
biochemical, hematological, immunological, microbiological, anatomopathological,
imaging, electrophysiological and other tests and examinations.
Demonstrate that they can integrate and correlate the knowledge acquired from other
study courses encompassed in this curriculum to the procedures and methods
required to carry out the various diagnostic techniques.
Interpret and correlate in an integrated collective fashion the results of various
diagnostic tests and demonstrate that they are cognizant in respect of their
limitations.
Electives
Healthcare Management
The objective of the course is to familiarize students with:
The organization, functions and management of health care systems and the impact
of health care in improving the health of populations.
The tools, methods and processes used for strategic planning, decision making and
quality assurance / control in healthcare
Course Content
Health system structure at a global, European, national and regional level.
Planning, programming and assessment of health programs.
Core functions and competencies of leaders and managers in healthcare.
Essentials of health economics.
Principles of quality management, audit and clinical governance.
Managing crisis, stress, time, conflict and change.
Educational Objectives
Upon successful completion of this course students should be able to:
Define the role of managers and leaders in healthcare, identify their core competencies
and associate these with the structure of healthcare organizations and healthcare
systems.
Demonstrate that they comprehend healthcare planning and administration on a global,
European, national and regional level.
Demonstrate that they comprehend the economic and social implications that medical
practice entails, taking into account valid effectiveness and efficiency criteria.
Describe the principles of Occupational Health.

February 2019
School of Medicine, EUC/Clinical Training Manual …. 85
Clinical Embryology
Description
This course is aiming to acquaint Medical students to a broad and concrete overview of the
mechanisms causing major and minor birth defects after drug and environmental causative factors
during pregnancy and neonatal life, to types of their prevention and to the clinical problems which
arise for their repair and rehabilitation. Genetic Counseling methods and international Guidelines
for birth defects prevention and their early diagnosis in pregnancy will be taught. The role of folic
acid and healthy and enhanced nutrition before and during pregnancy will be analyzed. Viruses,
bacteria, toxic substances, chemicals, endocrine disrupters, drugs, particulate matters and toxic
nanoparticles bio-distribution throughout the embryonic/fetal and neonatal body which can have
consequences to the developing human organism via their placenta blood barrier permeability will
be taught. Incidence of genetic syndromes and epigenetic disturbances will be emphasized. Thus,
the course is going to serve as a connective foundation upon which, clinical orientated problems
and their prevention and repair in Clinical Embryology and Neonatology in Medical sciences will
be based.
Course Content
In that regard, students will familiarize themselves with the following Modules:
Genetic Counseling for Birth Defects.
Endocrine disrupters and Birth Defects.
Birth Defects caused by drugs, viruses, bacteria, toxic substances and multiple teratogenic
environmental causative factors during pregnancy and neonatal life.
Epigenetics and Clinical Embryology.
Congenital Anomalies due to Genetic disorders. Clinical expression of Parental Diseases
and Syndromes.
Clinical expression of birth defects at the Craniofacial area.
Clinical expression of birth defects at the Cardiovascular and the Respiratory System.
Clinical expression of birth defects at the Gastrointestinal System.
Clinical expression of birth defects at the Renal System.
Clinical expression of birth defects at the Male and Female Reproductive System.
Clinical expression of birth defects at the Neural System and the Sensory organs.
Clinical expression of birth defects at the Skin, Muscular and Skeletal System and at the
Upper and Lower extremities.
Clinical expression of birth defects at the Umbilical Cord and the Placenta.
Clinical and modern imaging modalities' methods for prenatal diagnosis of Birth defects.
Laboratory exercises:
Observations of normal and pathological clinical embryonic cases from the systems
described.
Drawing methods for understanding the clinical expression of birth defects of the organs
and systems described above and observations of various types of high fidelity 3D
embryological models
Clinical Seminars and Discussions of pathological clinical cases of birth defects in
comparison with normal clinical appearance from the organs and systems described.
Clinical Seminars and Discussions with videos for clinical cases of congenital
malformations and birth defects from the modules described using videos and Computer
Assisting Learning-CAL.
February 2019
School of Medicine, EUC/Clinical Training Manual …. 86
Educational Objectives
Upon successful completion of this course students should be able to:
Demonstrate an understanding of clinical orientated problems in embryology influencing
the developing of the human embryo and of each of its organs and systems.
Illustrate, recognize, identify and describe the normal and abnormal embryonic
development in comparison with the clinical problems raised after the influence of
causative teratogenic and genetic factors.
Understand the role of Clinical evaluation in Embryology for accurate diagnosis of birth
defects.
Understand the role of Clinical Genetic Counseling for birth defects prevention.
Understand the role of Clinical rehabilitation and surgical repair of birth defects.
Understand the role of Networking with diverse types of physicians and clinics for
information of birth defects prevention.
Describe and explain diagnostic methods as :the prenatal ultrasound 2D and 3D
diagnosis, amniocentesis and other modern prenatal examination methods for diagnostic
purposes of birth defects.
All the above will acquaint Medical students to demonstrate effective self-assessment
skills, communicative and collaborative skills, communication with peers, discussions in
small groups with clinicians and presentation of Problem Based Learning and Clinical
Discussions in human clinical cases of birth defects.
Laboratory skills
Describe and explain prenatal diagnostic methods in collaboration with clinicians.
Describe and identify clinical cases of birth defects into the human embryonic body.
Understand the role of Genetic Counselling and Clinical Embryology for accurate
diagnosis in diverse diseases demonstrating skills in critical thinking via Problem Based
Learning and Clinical Discussions.
Describe and identify stages of embryological and fetal normal and defective
differentiation of organs and systems from implantation of the blastocyst to the full term
pregnancy.
Identify tissue and organs' normal and defective embryological structure , from 3-D high
fidelity embryological models, videos and Computer Assisting Learning-CAL.
Rehabilitation Medicine
Description
This course is intended to give the student a broad overview of Rehabilitation Medicine. It is
designed to acquaint students with the fundamental terms, concepts, and principles used in
Rehabilitation Medicine, especially for disability and to serve as a foundation upon which the
Rehabilitation plans for individual patients can be applied.
Course Content
The students will familiarize themselves with:
The use of the International Classification of functionality, disability and health (ICF) of the
WHO.
The use of several assessment tools in Rehabilitation Medicine.
The design of a Rehabilitation plan for acute musculoskeletal disorders of adult age.
The design of a Rehabilitation plan for acute nervous system disorders of adult age.
February 2019
School of Medicine, EUC/Clinical Training Manual …. 87
The design of a Rehabilitation plan for acute cardiopulmonary disorders of adult age.
The design of a Rehabilitation plan for progressive musculoskeletal disorders.
The design of a Rehabilitation plan for progressive nervous system disorders.
The design of a Rehabilitation plan for progressive cardiopulmonary disorders.
The design of a Rehabilitation plan for disorders in the developmental age (scoliosis,
congenital disorders, cerebral palsy etc).
The design of a Rehabilitation plan for injuries or disorders which will need the use of
prosthesis.
Educational Objectives
Upon successful completion of this course students should be able to:
Describe the concepts of functioning, disability and health (the WHO-ICF).
Understand the epidemiology of disability, the principles of functional recovery and motor
learning.
Understand the disabling consequences of injury and diseases in the adult age,
concerning acute and progressive musculoskeletal and neurological disorders, balance
troubles in the elderly and the risk for falls, chronic obstructive pulmonary diseases, heart
diseases and cancer diseases.
Describe the disabling consequences of injury and diseases in the developmental age
(e.g. scoliosis, congenital disorders, cerebral palsy).
Understand essential methods of assessing patient’s needs, including electromyography
and diagnostic ultrasounds.
Define the discharge planning and the concept of the interdisciplinary care.
Describe the effectiveness of the several rehabilitation interventions (e.g. medications,
exercise, physical modalities, manual therapy, cognitive rehabilitation, prosthetics and
orthotics).
Understand the ethical implications of working with people with disabilities, including the
role of physician as advocate and the guardianship responsibilities, the economic
implications of disability management and medicolegal issues.
Laboratory skills
Explain the use of the International Classification of Functioning, Disability and Health
(ICF)
Use of several assessment tools.
Analyse clinical cases and setting up the rehabilitation plan for possibly disabling
disorders of the musculoskeletal, nervous and cardiopulmonary system
Visit Physical and Rehabilitation Medicine Departments for developing clinical awareness
of the main areas presented during the training lectures.
Research Methods & Scientific Writing
Description
This is a basic introductory course in research methodology that will also include statistical
analyses and covers a comprehensive range of topics for students that will allow them to apply
quantitative/qualitative research using a critical thinking approach. Moreover, examples of clinical
trial studies, protocols and international guidelines for that purposes will also be discussed. This
is a theory-based course along with exercising on research proposition and with plenty of
opportunities to apply the concepts via practical and interactive activities integrated throughout
the course.

February 2019
School of Medicine, EUC/Clinical Training Manual …. 88
Course Content
Students will familiarize themselves with the following:
Introduction to quantitative research
Research question development
Study design, sampling and confounding
Types of data and displays of data and results
Summarizing numeric and categorical data
Numeric and categorical differences between groups
Hypothesis testing and confidence intervals and p-values
Parametric statistical tests and Non-Parametric tests
Reliability and Validity of research data\
Clinical trials/protocols/guidelines
Educational Objectives
Upon successful completion of this course students should be able to
Analyze clinical data and be able to discuss and interpretate as a research team in a
seminal manner
The use of complex research data and use statistical anlysis to evaluate results
Identify ethical matters on the use of animal and human samples for research
Clinical Trials and protocols
Formats and guidelines
Interventional Radiology
Description
Modern imaging modalities (CT, MRI, Ultrasound, PET/CT and x-rays) have become the mainstay
of diagnosis. In addition, these modalities offer guidance for novel minimally-invasive treatment
options. The objective of this course is to provide an introductory but comprehensive review of
the imaging findings of the most common anatomic pathologies in an organ based approach and
describe the minimally-invasive treatment options.
Course Content
The course will begin with an introduction to the fundamentals of imaging physics, and will include
references to plain x-ray films, computed tomography, magnetic resonance imaging, ultrasound
and nuclear imaging. Emphasis will be given to aspects that will enable the students to improve
their image interpretation skills.
The course will continue with a series of topics during which the normal anatomy/physiology will
be presented. Relevant pathophysiology will then be taught to the students, followed by
presentation of the available minimally invasive treatment option, as well as comparison with
traditional treatment options.
Topics will include:
Liver cancer. During this section we shall present normal hepatic anatomy and function,
the pathophysiology of hepatocellular carcinoma and the option of transarterial
chemoembolization.
Gastrointestinal hemorrhage. We shall review the causes of GI hemorrhage, present the
medical, surgical and minimally invasive options to address such hemorrhage and
showcase the tools of the trade (catheters, coils, microspheres etc)

February 2019
School of Medicine, EUC/Clinical Training Manual …. 89
Liver cirrhosis: The students will learn the pathophysiology of liver cirrhosis, its
consequences (hepatocellular carcinoma, portal hypertension) and treatment options for
the latter (i.e. TIPSS)
A similar structure will followed for other topics and will include aortic/arterial disease,
cerebrovascular disease, renal cancer, hepatico-pancreatico-biliary disease and other specialty
interventions.
In addition to the above, the students will be given a basic introduction to medical research and
relevant statistical methodology; they will develop the basic critical skill of judging scientific papers
and present a paper of their choice.
Educational Objectives
Upon successful completion of this course students should be able to:
Define the basic biophysics of imaging modalities (MRI, CT, Ultrasound, PET/CT and X-
ray systems), as they apply to every-day clinical practice.
Recognize and describe the relevant imaging findings, formulate a differential diagnosis
and specify an investigational approach towards the final diagnosis.
Describe the diagnosis, epidemiology, pathophysiology, and treatment options of each
disease covered.
Describe the novel, minimally-invasive treatment options available for each disease.

February 2019
School of Medicine, EUC/Clinical Training Manual …. 90
PART III
Clinical Centers and Affiliated Hospitals
EUC is committed to providing our students with a rich variety of experiences and opportunities
for training. We have an outstanding and diverse group of affiliated clinical training sites, including
Medical Centers and Hospitals, in Cyprus, Greece and Germany.
EUC Affiliation Agreements follow the guidelines established by the Cypriot Ministry of Health,
European Union accreditation policy and the Association of American Medical Colleges affiliation
agreement project.
The aim of the uniform agreement of EUC with each affiliated Medical Center is to provide
consistency and standardized expectations for both parties, and ensure clinical training of EUC
students at the highest level.
The Clinical Training Affiliation Agreement is shown in Appendix X.
Affiliated Clinical Center or Hospital
Location
Description
Link to web-site
Teaching Staff (Curriculum Vitae) (Appendix XI)

February 2019
School of Medicine, EUC/Clinical Training Manual …. 91
PART IV
List of Appendices
Appendix I
Clinical Training Organogram
Roles and Responsibilities EUC and Affiliated Hospital Teaching Staff
Appendix II
Student Clerkship Evaluation Form
Appendix III
Clerkship Logbooks
Appendix IV
Clinical Practice Incidence Report
Appendix V
Student Health Requirements for Clinical Rotations
Appendix VI
Confidential Student Feedback and Comments Form for Clinical Training
Appendix VII
EUC Clinical Competence Building Roadmap
Appendix VIII
Student Confidence in Performing Practical and Clinical Skills Questionnaire
Appendix IX
Comprehensive Clinical Competency Assessment – OSCEs

Chair Division
Surgery
Chair Division
Child
/
Maternal
Health
DCC
Social
Med/Public
Course
Coordinator
Course
Coordinator
DCC
Surgery
DCC
Internal
Medicine
Ch Division
Social Med/ Public
Health/ Primary Care
Course
Coordinator
Chair Division
Neurosci/Mental
Health & Sensory
DCC
Neurosci/Mental
Health &
Sensory
Course
Coordinator
DCC
Child /
Maternal
Health
Chair Division
Internal Medicine
Course
Coordinator
HCCE
Clinical Training
Committee
Vice Chair
Affiliated Hospital
Chair
Vice Dean
Strategy & Institutional Advisor
Dean
Curriculum
Coordinator
Course
Heads
Chair Division
Functional Sciences
APPENDIX I
Clinical Training Organogram
February 2019 School of Medicine, EUC/Clinical Training Manual …. 91
S&F
Coordinator
&
Committee
Chair Division
Structural Sciences
Course
Heads
Clinical Instructors
92
Roles & Responsibilities for Clinical Training
Responsibilities EUC
Clinical Training Committee (CTC)
1. 7-member Committee comprising the 5 Division Chairs and 2 voted members
2. Oversees the planning of clinical training for all years of study
3. Assists the Dean in recruiting and assigning academic and clinical faculty in
clinical training
4. Are the liaison between the clinical training sites and the faculty responsible for
academic program and course content (Chairs of Clinical Divisions and Course
Coordinators)
5. Ensures optimal cooperation between all affiliated persons and sites
6. Ensure appropriate training of scientific (clinical) collaborators and clinical
instructors
7. Ensures optimal function of clinical training courses across all years of study
8. Ensures an environment of safe collaboration between the School and affiliated
healthcare sites
9. Assists the Dean in administrative, financial and other relevant obligations of
the School of Medicine related to the clinical training
10. Ensures that the learning objectives outlined for clinical training are achieved
11. Ensures accurate, complete and objective student evaluation
12. Works in collaboration with the academic and hospital coordinators, to solve
any issues that may arise up during clinical training
13. Oversees appropriate completion and evaluation of the logbooks
Clinical Training Advisors
1. Full-time faculty members assigned by Clinical Training Committee
2. Each advisor ensures that all requirements are correct and complete
3. Review evaluations, grades and graduation requirements and updating rotation
schedules.
4. Students must maintain contact with their Clinical Training Advisor
throughout their clinical terms until graduation.
Chairs of Clinical Divisions
1. Full-time senior faculty members (Associate or Full Professor) chair each
clinical Division:
Internal Medicine
Surgery
Child & Maternal Health
Social Medicine
Neuroscience & Sensory Systems
2. Responsible for overall academic content and coordination of the courses
taught in that division.
3. Work with head of each course (Course Coordinators) taught in that division
4. Oversee clinical program and rotations at each affiliated hospital
5. Ensure equality of training for EUC students across all clinical training sites.
93
Course Coordinators (CC)
1. Full- or Part- time faculty
2. Head of course taught in Division
3. Coordinate the instruction of individual courses by themselves and other full-
time faculty and scientific / clinical collaborators (part-time teaching faculty)
4. Responsible for outlining teaching objectives and competencies for the course
5. Prepare Syllabi, Course Plans, Session Plans and relevant academic
documentation
6. Prepare and oversee course exams and submit course grades
94
Responsibilities of Affiliated Hospital Teaching Staff
Hospital Coordinator of Clinical Education (HCCE)
1. Is the hospital administrator responsible for the EUC student program
(including scheduling rotations, delineating holidays and vacation time,
determining the scope of student activities, dealing with student concerns and
being responsible for acute medical problems that students might develop)
2. Is the liaison with the School of Medicine
3. May receive formal appointments to the School of Medicine’s faculty that are
commensurate with their qualifications and duties
4. Is to supervise the clinical program and ensure its quality and its conformity
with the University’s guidelines as described in the CTMAA and the Faculty
Handbook
5. Reviews the overall program with a Dean or Deputy Dean at the time of their
visits to the hospital
6. Is a member of the Clinical Training Committee, the main advisory body to the
Dean for the clinical terms
Department Clerkship Coordinator (DCC)
1. Is appointed for each core rotation in which EUC students participate at each
affiliated hospital.
2. Is responsible administratively to the HCCE and academically to the
appropriate Departmental chair and Division coordinator of EUC
3. Is responsible for checking that the students; logbooks are kept updated daily.
4. Grants permission for absences
5. Arranges for formative mid-core assessments of all students
Clinical Instructors (CI)
1. Teach students at the bedside
2. Assess students medical knowledge, clinical and communication skills and
professional behavior
3. Serve as a role model
4. Notify CC if student is marginal

95
Appendix II
Student Clerkship Evaluation Form – Final
Students Name:
Clerkship:
Rotation Dates:
Course Name:
Submitted by:
Department Clerkship Coordinator (DCC):
Hospital Name:
Confirmed by HCCE:
Review of Logbook by DCC
Evaluator:
Satisfactory Unsatisfactory
Medical Knowledge
Clinical Skills
Communication Skills
Professional Behavior
Logbook Check
MiniCEX
Feedback
FINAL GRADE
GUIDELINES FOR EVALUATING STUDENTS
Required Narrative Summary: This section enables the faculty to provide evaluative
information qualifying the letter grade.
GRADES
Policy
The final grade in the clerkship represents a semi-quantitative average of five
components. The first four reflect subjective faculty evaluations. Students should be
evaluated based on the following:

96
1. Medical Knowledge (50%) – knowledge of basic, clinical and social sciences;
the pathophysiology of disease; clinical signs, symptoms and abnormal
laboratory findings associated with diseases and the mechanism of action of
pharmaceuticals.
2. Clinical & Communication Skills (40%) – diagnostic decision making, case
presentation, history and physical examination, communication and
relationships with patients and colleagues, test interpretation and therapeutic
decision making. Students must be observed and evaluated at the bedside.
Communication skills as they relate to physician responsibilities, including
communication with patients, families, colleagues, other health professionals
and resolution of conflicts.”
3. Attendance & Professional Behavior (10%) – their interaction with staff and
patients, integrity, sensitivity to diversity and attendance.
Grading System:
Letter Grade
A
Grade Meaning
Excellent
Grade Points
4.0
Percentage Grade
90 and above
B+
Very Good
3.5
85-89
B
Good
3.0
80-84
C+
Above Average
2.5
75-79
C
Average
2.0
70-74
D+
Below Average
1.5
65-69
D
Poor
1.0
60-64
F
Failure
0
I
Incomplete
0
W
Withdrawal
0
P
Pass
0
AU
Audit
0

97
Appendix III
Individual Student Logbooks – Example Semester 8
Student name: Student’s Reg. No:
COVER PAGE
SCHOOL OF MEDICINE
CLINICAL TRAINING LOGBOOK
MED408: Clinical Training III (Infectious Diseases and Clinical Microbiology)
MED418: Clinical Training IV (Endocrine System, Uro- Nephrological System and Male
Genital Tract)
MED322: Diagnosis by Imaging
CLASS 2014/20: 4
th
YEAR MEDICAL STUDENTS
Academic Year 2017-18: Spring Semester 2018
© European University Cyprus, 2018
98
OBJECTIVES
The clinical training program for MED408: Clinical Training III (Infectious Diseases and Clinical
Microbiology), MED418: Clinical Training IV (Endocrine System, Uro- Nephrological System and
Male Genital Tract) and MED322: Diagnosis by Imaging, is intended to provide essential
knowledge, for medical students of EUC at the affiliated private and public training healthcare
centers.
The overall objective is to enrich students with theoretical knowledge, practical skills and
safety information about the relevant departments, including inpatient wards, interventional units,
outpatient clinics and accidents & emergency departments, and to identify the roles and
responsibilities of medical doctors, as well as the professional and clinical conduct in these
settings.
Students must observe and develop different clinical and communication skills and apply
knowledge gained from previous years in real-life clinical settings.
EVALUATION CRITERIA
All Clinical Training Courses in the EUC Medical School are evaluated based on a combination of
examinations performed in the EUC campus and clinical performance in the clinical area. For joint
clinical training fields, a minimum 50% performance is required in each subject area before the
overall final degree can be calculated.
The examination carries 70% of all grade assigned by each instructor of the theoretical
component (collaborator), of which 30% is during a formal midterm exam and 40% is assigned in
a final exam, including OSCE assessment. The clinical performance carries 30% of all grade,
of which 10% is assigned based on the attendance reports and 20% is based on logbook recording
of each student’s clinical merit throughout the semester.
Note. you are required to submit the completed logbook upon conclusion of your clinical
rotations at the end of the semester. Any delay or lack of compliance will lead to grade deduction
and/or course failure.
99
GUIDE FOR STUDENTS
This logbook is a comprehensive training guide for your clinical rotation. Attendance is mandatory
at all assigned clinical departments times and within the designated timeframe. Accurate
completion is required, to provide sufficient evidence regarding the extent of your training and
achieved level of competence.
For academic matters, please contact the Academic Contact Person of the respective hospital. In
case of clinical issues, please contact the Hospital Coordinator of the respective hospital, as
designated in page 3.
Professional Standards
During your clinical rotation, you should at all times:
Demonstrate respectful and courteous behavior towards patients, chaperons and
colleagues.
Maintain patient confidentiality.
Comply with hospital policy and procedure and adhere to the School’s Code of Conduct.
Work with enthusiasm and take advantage of all learning opportunities.
Professional Appearance
Students must wear the school dress and the school ID badge must be worn and remain visible
at all times. Footwear must enclose the foot with heels < 5cm. Single piercing jewelry limited to
the ears and one small stud in the nose are permitted. Rings or other jewelry are strongly
discouraged (wedding bands are acceptable). Hair longer than shoulder length should be tied
back or contained in net. Facial makeup should be subtle and kept to a minimum. No artificial
nails. Fingernails should be kept short (<0.5 cm long). No caps/hats, unless part of required
uniform or for religious purposes.
Signatures
The School of Medicine of EUC considers falsification of signatures to be an unprofessional act
of forgery. Any suspicion of falsification of signatures within the logbooks will be further
investigated. If you experience difficulty in obtaining needed signatures, please discuss the issue
with the hospital coordinator at the site of your placement, and also complete the self-reflection
diary accordingly. The faculty of the School of Medicine is always willing to provide support.
Parts B, C & D. Patient assignment, History, Physical examination, Clinical skills, Essential
course content
All students should be exposed to as many clinical situations as possible. Students assist doctors
and prepare for the acquisition of the duties of a resident. You should record your attendance and
involvement (as determined by the clinical instructor) in key clinical experiences, and ask the
clinical instructor to sign the entry. You are expected to follow up at least one patient every week
from admission to discharge. Together with the supervising doctor, you record admission data,
perform physical examination, evaluate laboratory and imaging findings, pose a diagnostic path,
assess and prioritize the different problems of the patient, discuss about further diagnostic and
therapeutic choices, present the patient during clinical rounds, update the daily report, and assist
in the preparation of discharge documentations (patient confidentiality at all times is preserved).
You follow your patients daily, are fully informed of the patients’ progress and actively participate
with your team members in the performance of various practical skills.
Please note the following:
grades will be not be assigned if the fields are not completed as requested.
signing any of the skills or clinical conditions confirms that you have gained sufficient
theoretical and/or practical knowledge for official evaluation.
Part E. Mini Clinical Evaluation Examination form (mini-CEX)
The miniCEX is a 15-minute snapshot of how you interact with patients. You are requested to
perform this procedure at least once in each discipline, under the supervision of your clinical
100
instructor. Request from one of the supervising clinical Instructors to complete and sign
accordingly.
Part F. Self-reflection diary
You must ensure that feedback is completed for all weeks and departments of clinical rotation.

101
GUIDE FOR CLINICAL INSTRUCTORS AND LEARNING PRIORITIES
Student Attendance and Evaluation
Attendance is mandatory for students and the clinical instructor signs the attendance sheet (Part
A) of every student routinely. Actions performed by the student, as described below, are also
signed by the clinical instructor. The role of the clinical instructor is also essential in the final
assessment and evaluation of every student that has rotated through their department.
Part B. Patient assignment
Each student is expected to follow at least one patient every week from admission to discharge,
as presented in Part B. Patient assignment/Resident shadowing. When you are satisfied that the
student has reached a competent standard, you should complete and sign the relevant entry.
Parts C & D. History, Physical examination, Clinical skills, Essential course content
Students should be exposed to competencies and trained on clinical skills to a maximum possible
degree, as described in Part C. History, Physical examination, Clinical skills. In addition, students
should exhibit competence level in situations commonly encountered in the different clinical
departments, as described in Part D. Essential course content. Please rate student level according
to the following scale and sign: O:observed (not performed), 1.exceptional, 2.satisfactory,
3.average, 4.needs improvement, 5.unsatisfactory.
Part E. Mini Clinical Evaluation Examination form (mini-CEX)
The miniCEX is a 15-minute snapshot of how students interact with patients. Students should
perform this at least once in each clinical discipline, under your supervision, which you are kindly
requested to complete and sign.
Feedback
You will be asked to complete a prepared feedback form at the end of the clinical rotations period.

102
LEARNING PRIORITIES OF MED408, MED418 & MED322
Based on the theoretical and practical background of our students and according to the school
syllabus, clinical training should focus on the following skills and clinical content:
Infectious diseases and Clinical microbiology:
Clinical examination, including recognition of common signs of infectious diseases: fever,
systematic symptoms, SIRS criteria and the sepsis continuum, upper and lower respiratory
tract symptoms, diarrhea, arthritis, rash
Common infectious disorders (see Part D): recognition, evaluation, diagnosis, management
Common community-acquired and healthcare-associated infections
History taking and focus on infection characteristics, risk factors, travel, social, occupational
history
Systematic inflammatory response assessment and management
Endocrinology:
Clinical examination, including recognition of common signs of endocrine diseases: weight
changes, mood changes, hypotension/hypertension, skin disorders, organ dysfunction, etc
Common endocrine disorders (see Part D): screening, recognition, evaluation, diagnosis,
management
History taking and focus on endocrine diseases and metabolism: risk factors, family history,
social history
Investigation, evaluation and management of common endocrine/metabolic disorders
Nephrology:
Clinical examination, including recognition of common signs of renal diseases: edema,
hypotension/hypertension, mental status changes, rash, weight loss, etc
Common renal disorders (see Part D): recognition, evaluation, diagnosis, management
History taking and focus on renal diseases, inflammatory disorders and electrolyte
imbalances: past medical history, risk factors, exposures, family history, social history
Investigation, evaluation and management of common renal disorders
Evaluation and management of the patient with end-stage renal disease
Urology/Male genital system:
Clinical examination, including recognition of common signs of urological diseases: urinary
colic, urine retention, hematuria, erectile dysfunction etc
Common urological disorders (see Part D): recognition, evaluation, diagnosis, surgical &
medical management
History taking and focus on diseases of the male genital tract: past medical history, risk factors,
exposures, family history, social history
Investigation, evaluation and management of common disorders of the male genital tract
Evaluation and management of the patient with urological disease
Medical imaging:
Familiarization with basic imaging practices (see Part D): abdominal ultrasound, breast
imaging, chest imaging, interventional Radiology, radiological radiation exposure & safety
Basic interpretation of common imaging modalities: chest x-ray, abdominal ultrasound,
abdominal CT, chest CT

103
SAFETY MEASURES FOR MEDICAL STUDENTS
It is important to follow indicated measures for personal and patient safety at all times during your
clinical rotations. When concerned over a safety issue or an incident, contact immediately your
clinical instructor or supervisor. In cases of personal safety issues, such as injury or exposure,
you should also contact immediately the Faculty of the School of Medicine.
Vaccination
Students should be immunized according to the University immunization agreement.
Hand hygiene and isolation precautions
1. Standard precautions and Hand hygiene are performed before and after contact with all
patients. Indications and technique for hand hygiene follow the World Health Organization
guidelines.
2. Isolation precautions, personal protective equipment are additional measures that depend on
the risk of transmission between patients and healthcare personnel (i.e. contact, droplet, and
airborne precautions).
3. Gloves are worn for invasive procedures, contact with non-intact skin, mucous membranes, or
sterile sites, and at all activities that carry risk of exposure to body fluids or contaminated
instruments.
Safe use and disposal of sharps
Incidents with sharps injuries can be prevented with basic practices:
Do not pass sharps directly from hand to hand.
Do not break or bend needle.
Do not attempt to replace cap.
Always discard in appropriate sharps container immediately after use. Container should be
kept within arms’ length during use.
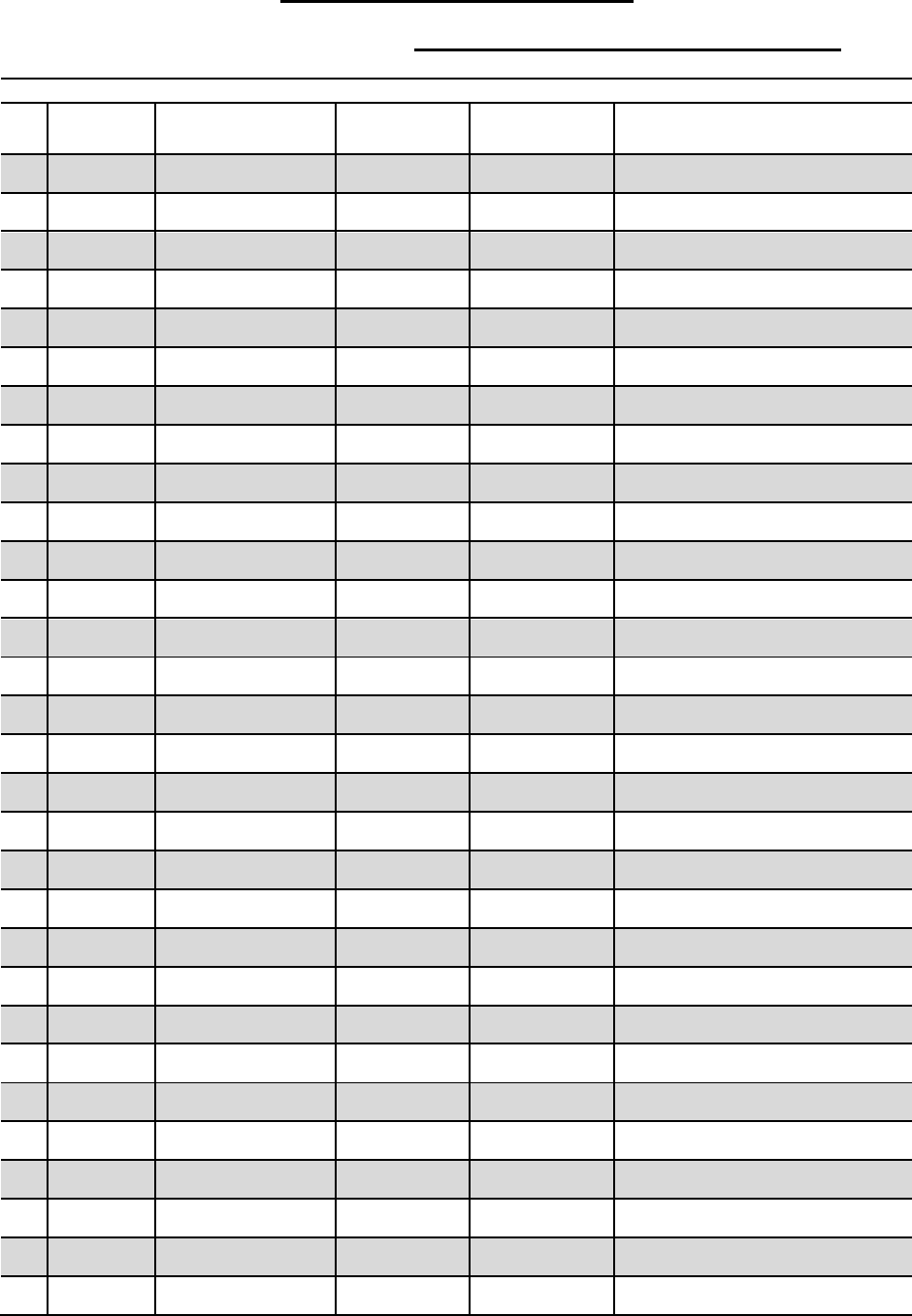
104
PART A. ATTENDANCE REGISTRY
For each day of clinical training, please record your arrival and departure time and request from
one of the supervising Clinical Instructors to sign your logbook at the end of each day.
Clinical Instructors are requested sign your attendance at the end of each day
DATE
WARD
Arrival
Time
Depart.Time
C.I Stamp & Signature
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
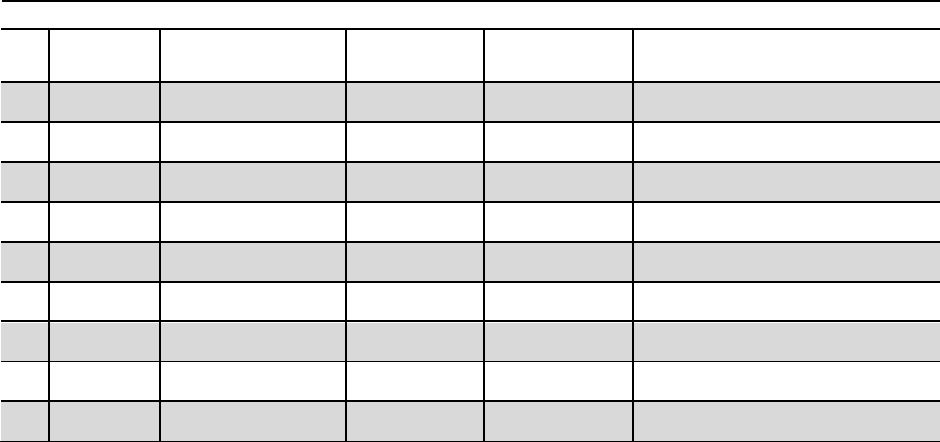
105
Clinical Instructors are requested sign your attendance at the end of each day
DATE
WARD
Arrival
Time
Depart.Time
C.I Stamp & Signature
31
32
33
34
35
36
37
38
39
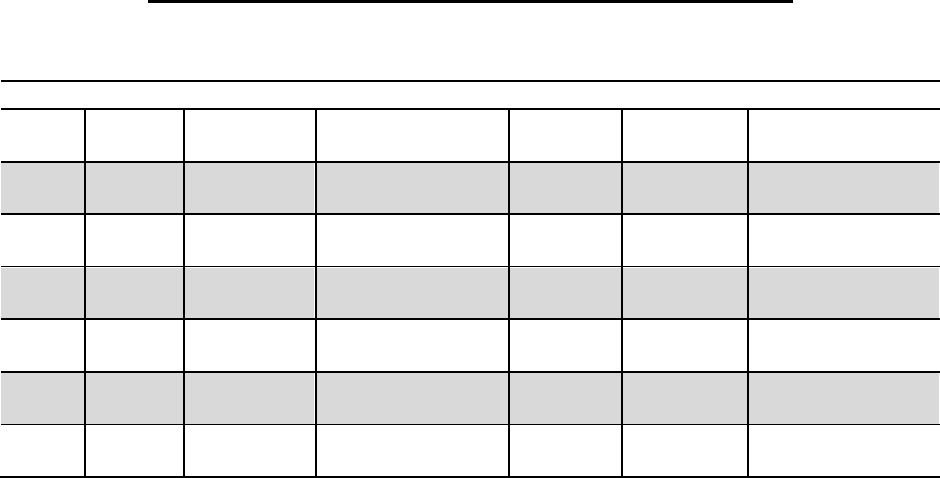
106
ACCIDENTS & EMERGENCY SHIFT ATTENDANCE REGISTRY
For each day of A&E practice, please record your arrival and departure time and request from one
of the supervising Clinical Instructors to sign your logbook at the end of each day.
Clinical Instructors are requested sign your attendance at the end of each day
DATE
A&E
Placement
C.I. Name
Arrival
Time
Departure
Time
C.I Stamp &
Signature
1
2
3
4
5
6
107
PART B. PATIENT ASSIGNMENT / RESIDENT SHADOWING (at least 1 case/week)
DATES
WARD
Assigned Patient Code and Condition
C.I Stamp
& Signature
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17

108
DATES
WARD
Assigned Patient Code and Condition
C.I Stamp
& Signature
18
19
20
21
22
23

109
PART C. HISTORY, PHYSICAL EXAMINATION, CLINICAL SKILLS
For each field below, the C.I. must confirm the performance of each of the following skills, using
the following scale:
O: observed (not performed), 1.exceptional, 2.satisfactory, 3.average, 4.needs
improvement, 5.unsatisfactory.
Note 1: grades will be not be assigned if the fields are not completed as requested.
Note 2: signing any of the clinical conditions below confirms that the respective student has
gained sufficient theoretical and/or practical knowledge for official evaluation.
Clinical Skill
Performance
& CI initials I
Performance
& CI initials
II
Performance
& CI initials
III
Performance
& CI initials
IV
Performance
& CI initials
V
History, patient file and physical examination
History taking
Perform differential diagnosis
Present case orally
Evaluate laboratory findings
Write a referral to another
specialty
Write a discharge note
Complete blood test form
Perform and interpret
electrocardiogram
Perform full physical
examination
Perform
Head/Eyes/Ear/Nose/Throat
examination
Perform neurological
examination
Endocrine system
Obtain and interpret blood
sugar
Interpret an oral glucose
tolerance test
Interpret abnormal thyroid
tests
Patient with dyslipidemia
(any)
Interpret a bone
densitometry test (eg.DEXA)
Infectious Diseases / Clinical Microbiology
Diagnostic tests: Sampling,
transfer & preparation of
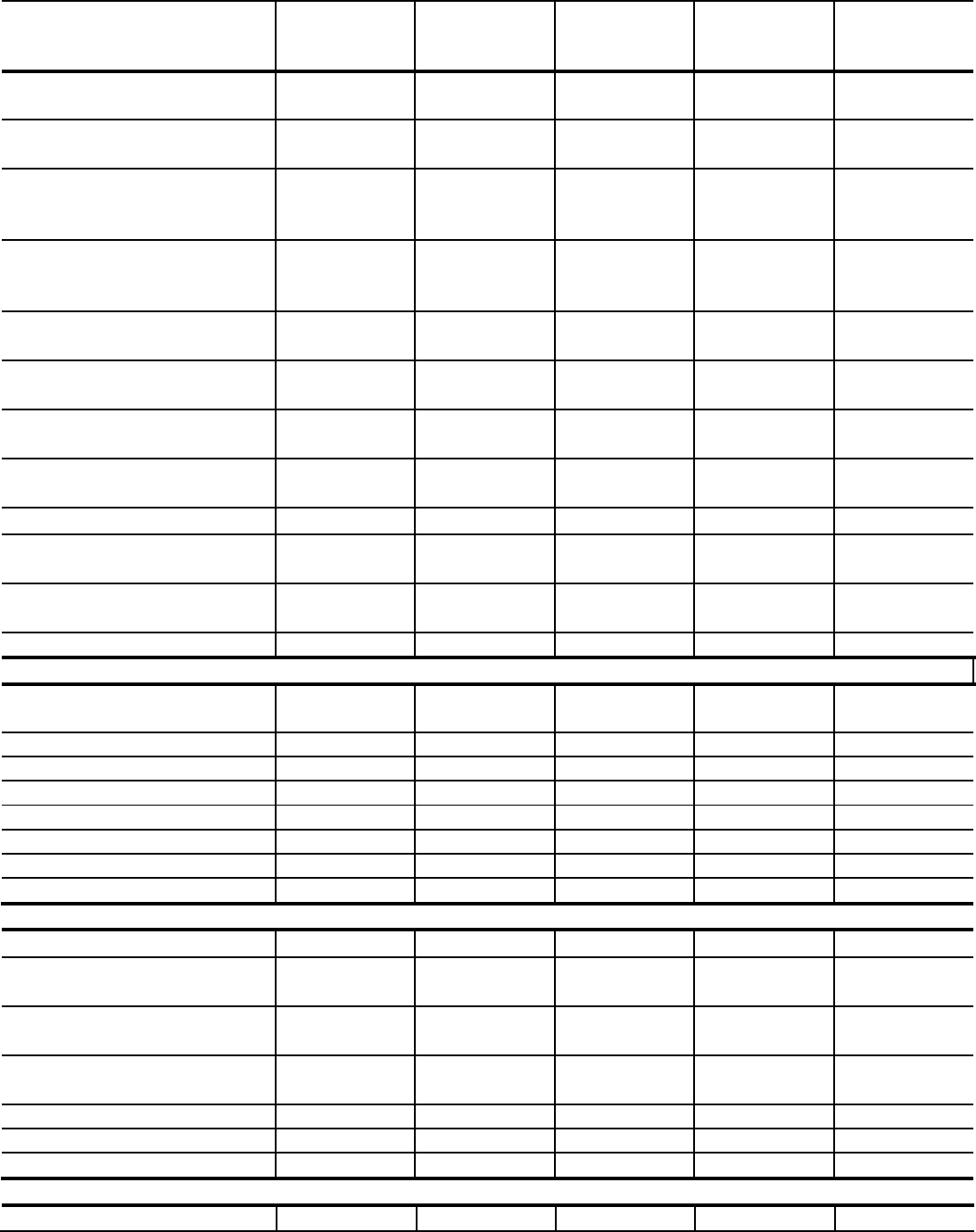
110
Clinical Skill
Performance
& CI initials I
Performance
& CI initials
II
Performance
& CI initials
III
Performance
& CI initials
IV
Performance
& CI initials
V
specimens, Microbial culture,
Gram-stain, Microscopy
Recognize and interpret
different antibiograms
Recognize methods applied
to detect resistance
mechanisms
Follow-up on cultures and
their correlation to the
patient’s condition
Basic infection prevention &
control measures
Patient with upper
respiratory tract infection
Patient with lower respiratory
tract infection
Immunosuppressed patient
with infection
Urinary tract infection
Central nervous system
infection
Nosocomial infection
definitions
Nephrology
Calculate and interpret
creatinine clearance
Urine sediment microscopy
Patient in hemodialysis
Kidney biopsy
Patient with fistula
Radiology
Interpretation of chest x-ray
Basic interpretation of
abdominal ultrasound
Basic interpretation of
abdominal CT
Basic interpretation of chest
CT
Urology
Patient with urinary colic

111
Clinical Skill
Performance
& CI initials I
Performance
& CI initials
II
Performance
& CI initials
III
Performance
& CI initials
IV
Performance
& CI initials
V
Patient with kidney stone
disease
Lithotripsy
Prostate examination
Prostate biopsy
Urine retention
Urethral catheterization
(male & female)
Performance of procedures (alphabetical order)
Arterial blood gases
Blood culture
Blood glucose examination
using finger stick
Hand washing (including
surgical scrubbing)
Injection of intramuscular
drug
Injection of intravenous drug
Nasogastric tube placement
Oxygen supplementation
Peripheral venous catheter
placement
Rectal examination
Respiratory secretions
culture
Setting up syringe driver
Skin suturing
Skin swabs for bacterial,
fungi and viral culture
Subcutaneous injections
Suction of respiratory
secretions
Swabs from nose, throat and
skin
Urinary catheter insertion,
female
Urinary catheter insertion,
male
Urinary catheter removal
Urine assessment. Mid-
stream urine
Urinalysis using urine stick
Vein puncture and blood
drawing
Wound care and basic wound
dressing

112
Clinical Skill
Performance
& CI initials I
Performance
& CI initials
II
Performance
& CI initials
III
Performance
& CI initials
IV
Performance
& CI initials
V
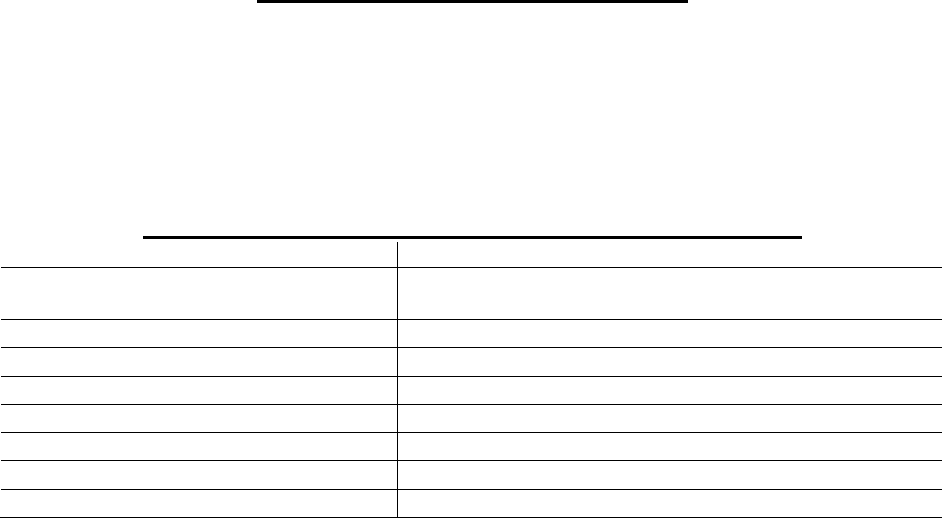
113
PART D. ESSENTIAL COURSE CONTENT
For each section, the clinical instructors must confirm the maximum competence level reached
by assigning the following indication using the following scale and sign:
O: observed (not performed), 1.exceptional, 2.satisfactory, 3.average, 4.needs
improvement, 5.unsatisfactory.
Note 1: grades will be not be assigned if the fields are not completed as requested.
Note 2: signing any of the clinical conditions below confirms that the respective student has
gained sufficient theoretical and/or practical knowledge for official evaluation.
INFECTIOUS DISEASES / CLINICAL MICROBIOLOGY (MED408)
CORE AREA
PERFORMANCE & COMMENTS
Applied antimicrobial stewardship
principles
Bloodstream infection
Community-acquired infection (any)
Immunosuppression and infection
Pneumonia
Skin & soft tissue infection
Surgical site infection
Clinical Instructor 1 (sign): Clinical Instructor 2 (sign):
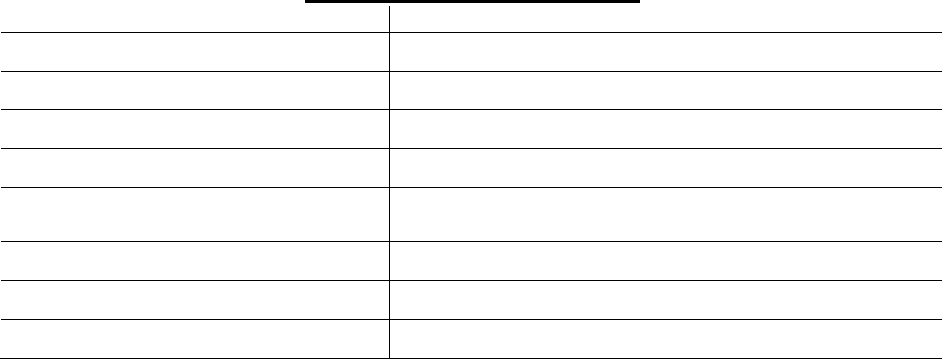
114
ENDOCRINE SYSTEM (MED418)
CORE AREA
PERFORMANCE & COMMENTS
Diabetes mellitus
Hyperthyroidism
Hypothyroidism
Lipid disorders
Osteoporosis / Metabolic bone
disease
Surgical treatment of thyroid disease
Clinical Instructor 1 (sign): Clinical Instructor 2 (sign):
115
UROLOGICAL SYSTEM AND MALE GENITAL TRACT (MED418)
CORE AREA
PERFORMANCE & COMMENTS
Kidney stone disease
Male subfertility
Obstructive uropathy
Prostate cancer
Prostate hypertrophy
Clinical Instructor 1 (sign): Clinical Instructor 2 (sign):
116
NEPHROLOGICAL SYSTEM (MED418)
CORE AREA
PERFORMANCE & COMMENTS
Acute renal failure
Glomerulonephritis (any)
Hemodialysis
Kidney transplantation
Kidney vasculitis (any)
Clinical Instructor 1 (sign): Clinical Instructor 2 (sign):
117
RADIOLOGY (MED322)
CORE AREA
PERFORMANCE & COMMENTS
Abdominal Ultrasound
Basic view box images – normal and
abnormal
Breast imaging
Chest imaging
Interventional Radiology
Radiological radiation, exposure &
safety
Clinical Instructor 1 (sign): Clinical Instructor 2 (sign):
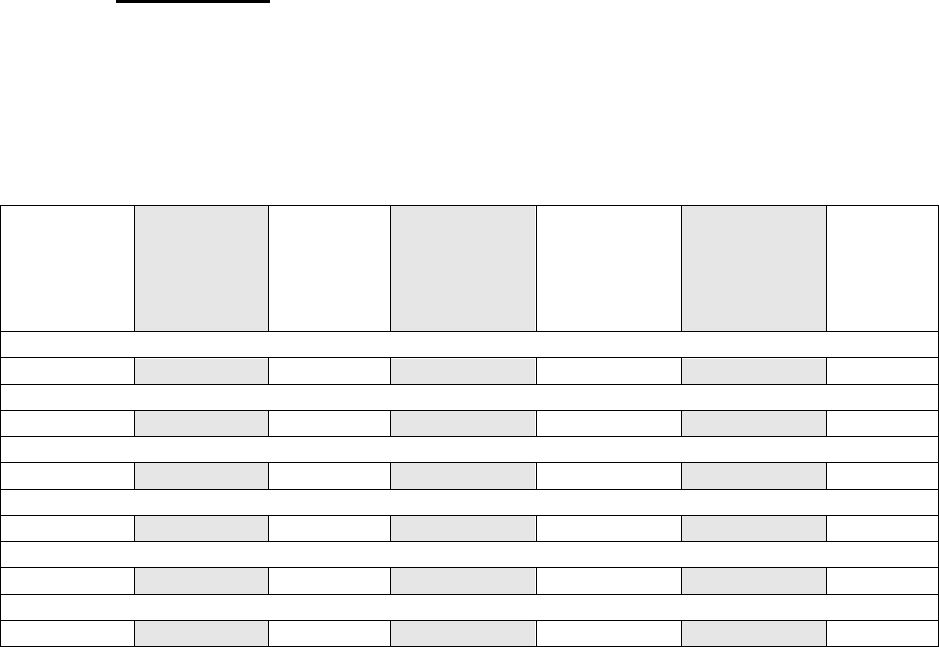
118
PART E1. mini-Clinical evaluation exercise (mini-CEX)
The miniCEX is a 15-minute snapshot of how you interact with patients. You are requested to
perform this procedure at least once in each discipline, under the supervision of your clinical
instructor. Request from one of the supervising clinical Instructors to complete and sign
accordingly.
Discipline: Endocrinology
Clinical department: Date: Clinical instructor Stamp:
Brief summary of case:
Please score the student on the scale shown. Note that your scoring should reflect the
performance of the trainee against that which you would reasonably expect at their year of
training and level of experience.
Well below
expectation
for stage of
training
Below
expectation
for stage of
training
Borderlin
e for
stage of
training
Meets
expectation
s for stage of
training
Above
expectation
s for stage of
training
Well above
expectation
s for stage of
training
Unable
to
commen
t
Medical Interviewing Skills:
Physical Examination Skills:
Counselling and Communications Skills:
Clinical Judgement:
Consideration for Patient/Professionalism:
Organisation/Efficiency:
Based on the above, rate the level of overall competence the student has shown:
…………… Below level expected for stage of training (Basic consultation skills resulting in
complete history and/or examination findings. Limited clinical judgement following encounter)
…………… Performed at the level expected for stage of training (Sound consultation skills
resulting in adequate history and/or examination findings. Basic clinical judgement following
encounter)
…………… Performed above the level expected for stage of training (Good consultation skills
resulting in a sound history, and/or examination findings. Solid clinical judgement following
encounter consistent stage of training)
…………… Performed at the level expected of a graduate (Excellent and timely consultation skills
resulting in a comprehensive history and/or examination findings in a complex or difficult situation.
Good clinical judgement following encounter)
Which aspects of the encounter were done well:
Suggestions for development:
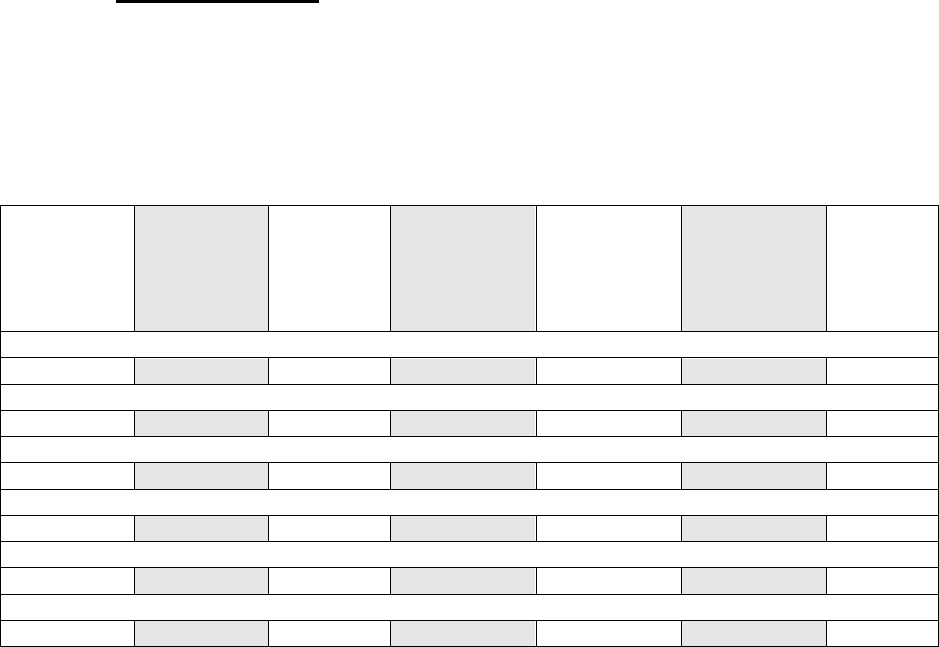
119
PART E2. mini-Clinical evaluation exercise (mini-CEX)
The miniCEX is a 15-minute snapshot of how you interact with patients. You are requested to
perform this procedure at least once in each discipline, under the supervision of your clinical
instructor. Request from one of the supervising clinical Instructors to complete and sign
accordingly.
Discipline: Infectious diseases
Clinical department: Date: Clinical instructor Stamp:
Brief summary of case:
Please score the student on the scale shown. Note that your scoring should reflect the
performance of the trainee against that which you would reasonably expect at their year of
training and level of experience.
Well below
expectation
for stage of
training
Below
expectation
for stage of
training
Borderlin
e for
stage of
training
Meets
expectation
s for stage of
training
Above
expectation
s for stage of
training
Well above
expectation
s for stage of
training
Unable
to
commen
t
Medical Interviewing Skills:
Physical Examination Skills:
Counselling and Communications Skills:
Clinical Judgement:
Consideration for Patient/Professionalism:
Organisation/Efficiency:
Based on the above, rate the level of overall competence the student has shown:
…………… Below level expected for stage of training (Basic consultation skills resulting in
complete history and/or examination findings. Limited clinical judgement following encounter)
…………… Performed at the level expected for stage of training (Sound consultation skills
resulting in adequate history and/or examination findings. Basic clinical judgement following
encounter)
…………… Performed above the level expected for stage of training (Good consultation skills
resulting in a sound history, and/or examination findings. Solid clinical judgement following
encounter consistent stage of training)
…………… Performed at the level expected of a graduate (Excellent and timely consultation skills
resulting in a comprehensive history and/or examination findings in a complex or difficult situation.
Good clinical judgement following encounter)
Which aspects of the encounter were done well:
Suggestions for development:
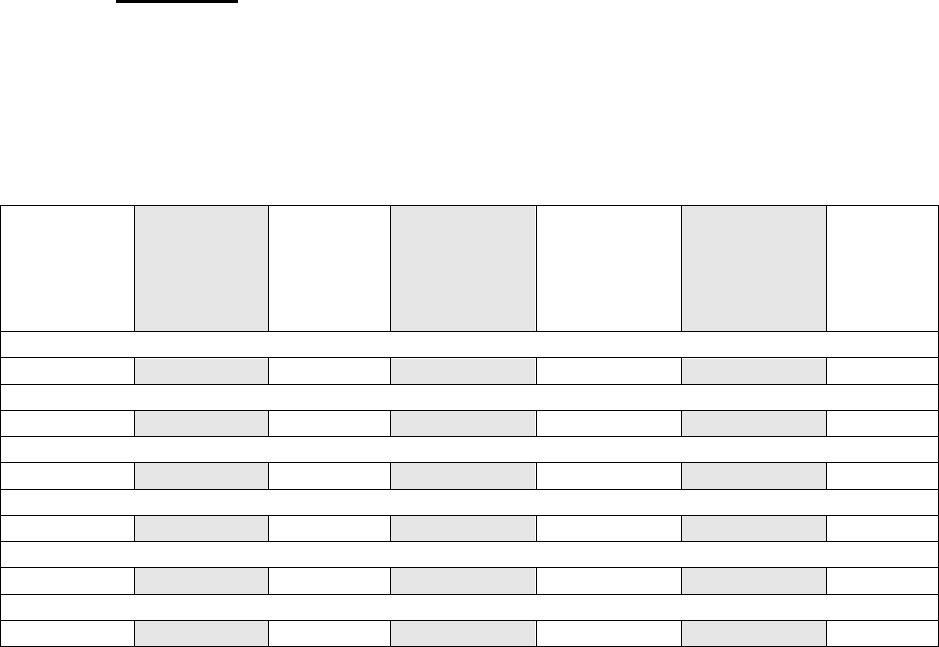
120
PART E3. mini-Clinical evaluation exercise (mini-CEX)
The miniCEX is a 15-minute snapshot of how you interact with patients. You are requested to
perform this procedure at least once in each discipline, under the supervision of your clinical
instructor. Request from one of the supervising clinical Instructors to complete and sign
accordingly.
Discipline: Nephrology
Clinical department: Date: Clinical instructor Stamp:
Brief summary of case:
Please score the student on the scale shown. Note that your scoring should reflect the
performance of the trainee against that which you would reasonably expect at their year of
training and level of experience.
Well below
expectation
for stage of
training
Below
expectation
for stage of
training
Borderlin
e for
stage of
training
Meets
expectation
s for stage of
training
Above
expectation
s for stage of
training
Well above
expectation
s for stage of
training
Unable
to
commen
t
Medical Interviewing Skills:
Physical Examination Skills:
Counselling and Communications Skills:
Clinical Judgement:
Consideration for Patient/Professionalism:
Organisation/Efficiency:
Based on the above, rate the level of overall competence the student has shown:
…………… Below level expected for stage of training (Basic consultation skills resulting in
complete history and/or examination findings. Limited clinical judgement following encounter)
…………… Performed at the level expected for stage of training (Sound consultation skills
resulting in adequate history and/or examination findings. Basic clinical judgement following
encounter)
…………… Performed above the level expected for stage of training (Good consultation skills
resulting in a sound history, and/or examination findings. Solid clinical judgement following
encounter consistent stage of training)
…………… Performed at the level expected of a graduate (Excellent and timely consultation skills
resulting in a comprehensive history and/or examination findings in a complex or difficult situation.
Good clinical judgement following encounter)
Which aspects of the encounter were done well:
Suggestions for development:
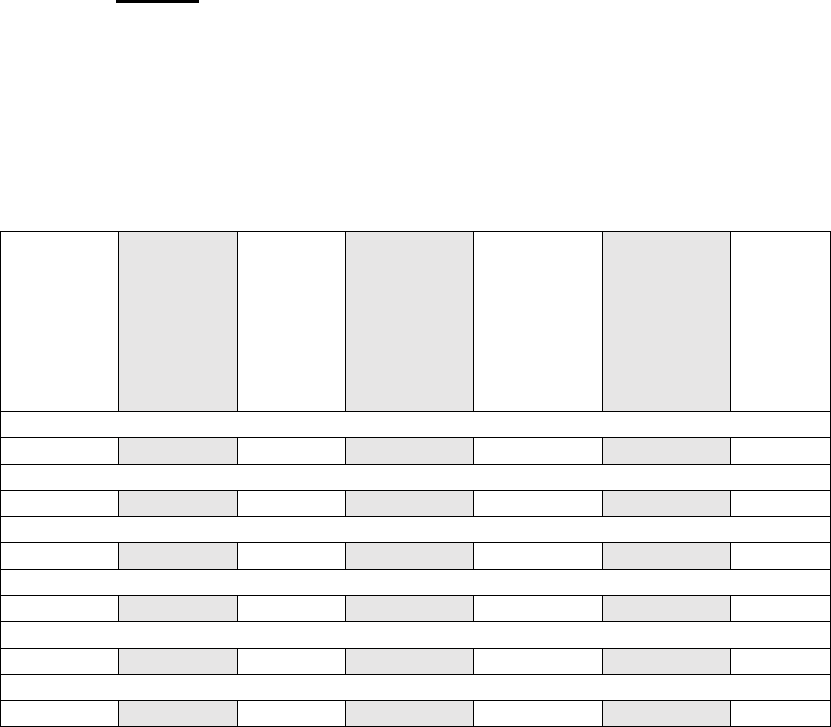
121
PART E4. mini-Clinical evaluation exercise (mini-CEX)
The miniCEX is a 15-minute snapshot of how you interact with patients. You are
requested to perform this procedure at least once in each discipline, under the
supervision of your clinical instructor. Request from one of the supervising clinical
Instructors to complete and sign accordingly.
Discipline: Urology
Clinical department: Date: Clinical
instructor Stamp:
Brief summary of case:
Please score the student on the scale shown. Note that your scoring should
reflect the performance of the trainee against that which you would reasonably
expect at their year of training and level of experience.
Well
below
expectati
on for
stage of
training
Below
expectati
on for
stage of
training
Borderli
ne for
stage of
training
Meets
expectatio
ns for
stage of
training
Above
expectatio
ns for
stage of
training
Well
above
expectatio
ns for
stage of
training
Unable
to
comme
nt
Medical Interviewing Skills:
Physical Examination Skills:
Counselling and Communications Skills:
Clinical Judgement:
Consideration for Patient/Professionalism:
Organisation/Efficiency:
Based on the above, rate the level of overall competence the student has shown:
…………… Below level expected for stage of training (Basic consultation skills
resulting in complete history and/or examination findings. Limited clinical judgement
following encounter)
…………… Performed at the level expected for stage of training (Sound consultation
skills resulting in adequate history and/or examination findings. Basic clinical
judgement following encounter)
…………… Performed above the level expected for stage of training (Good
consultation skills resulting in a sound history, and/or examination findings. Solid
clinical judgement following encounter consistent stage of training)
…………… Performed at the level expected of a graduate (Excellent and timely
consultation skills resulting in a comprehensive history and/or examination findings in
a complex or difficult situation. Good clinical judgement following encounter)
Which aspects of the encounter were done well:
Suggestions for development:
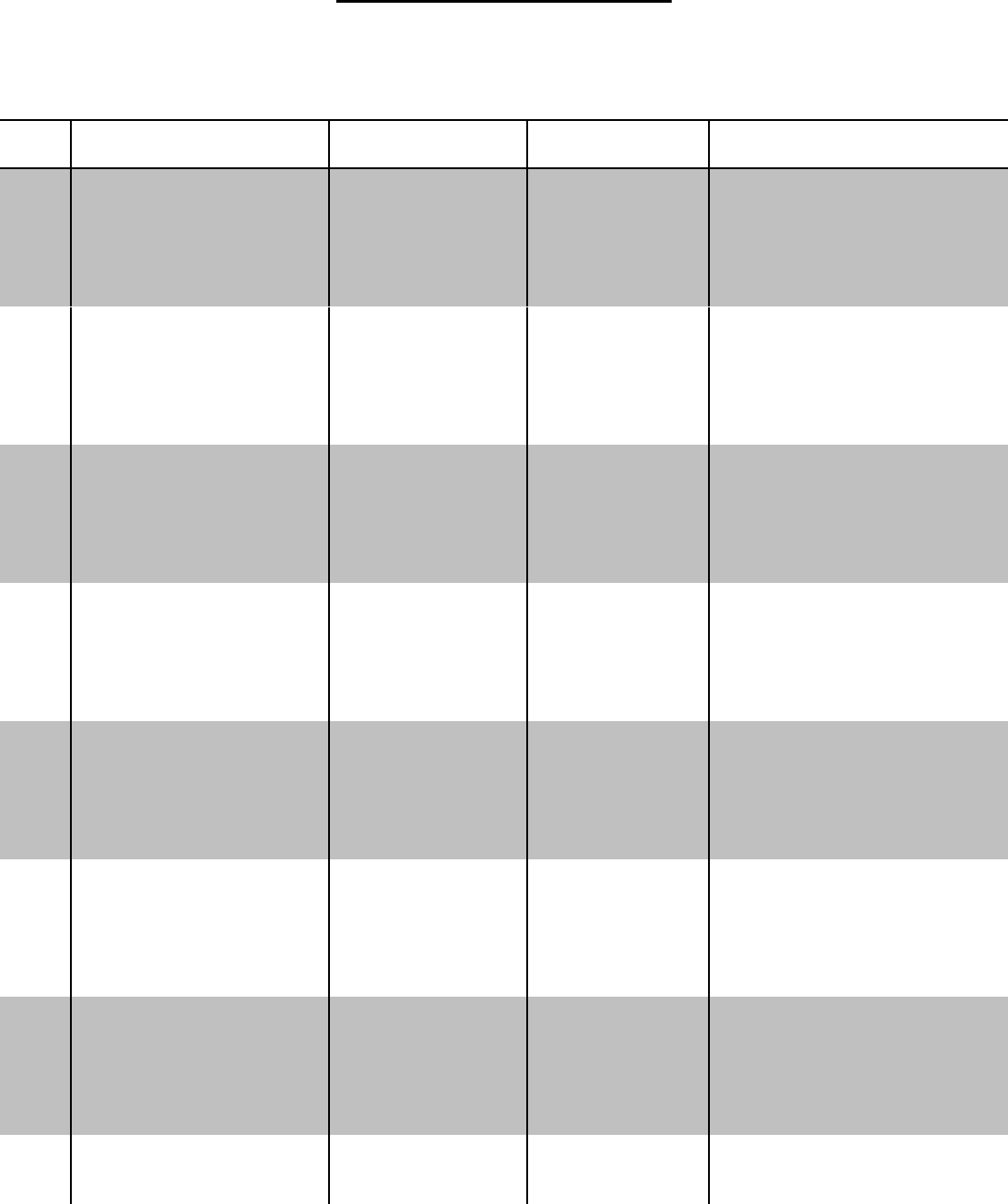
122
PART F. SELF REFLECTION DIARY
You are encouraged to record your concerns and suggestions. Please provide any
positive or negative remarks regarding your clinical training. Your feedback is valuable
to help improve the clinical teaching, but it will not affect your grading. In addition to
this diary, you will be requested to complete a confidential feedback form upon
conclusion of your rotations.
WARD
Strengths
Weaknesses
Suggestions for
Improvement
123
WARD
Strengths
Weaknesses
Suggestions for
Improvement
124
Appendix IV
Clinical Practice Incidence Report Form
Any incident regarding breach of safety issues, health and safety exposure of a student
of EUC, professional misconduct or violation of occupational rules should be directly
communicated to the Clinical instructor, Department Clinical Coordinator and/or
Hospital Coordinator of Clinical Education (HCCE), as well as to the Clinical Training
Committee (CTC) either directly or through the EUC Health and Safety Officer.
The following form should be completed by involved students and submitted to
the CTC of the School of Medicine, EUC.
Date: Department / Placement:
Involved student/s:
Other involved individuals:
Event description:
Actions taken – Persons informed:
Student/s signature:
For administration use (CTC response):

125
Appendix V
Health Requirements for Clinical Rotation
Students need to have all mandatory health requirements completed, documented and
cleared, before they can start their clinical rotation. Students must send all documents
to the office of the Clinical Training Committee, Eva Charalambous, Administrator at
E.Charalambous@euc.ac.cy.
EUC health requirements include:
TB SCREENING AND IMMUNIZATION RECORD
A. TUBERCULOSIS SCREENING
Screening consists of a 2-step skin PPD test or an interferon gamma release assay
blood test, e.g. QuantiFERON - TB Gold within 1 year prior to the start of their rotation.
B. MANDATORY IMMUNIZATIONS
1. Measles, mumps, rubella
Students are required to submit either a history of 2 doses of MMR
(measles, mumps, rubella) vaccination or laboratory copies of sufficient
serum IgG titers for measles, mumps, and rubella. If any of the serum
IgG titers indicated non- immunity, students must submit evidence of a
MMR vaccination obtained after the non-immune titer date.
2. Hepatitis B
Completion of the hepatitis B series (3 vaccinations) is a mandatory
requirement. Students need to submit the dates of vaccination and the
results of a serum hepatitis B surface antibody test obtained after the series
was completed. If the hepatitis B titer result indicates non-immunity, students
should submit proof of one additional vaccine after the titer result date.
Students should also check with their personal physician who may advise
further vaccines and titers.
3. Tdap vaccination within ten years is mandatory
C. ADDITIONAL VACCINATIONS
Depending on the clinical training site, students might also need to review the health
form recommendations for other vaccinations (eg. polio, hepatitis A, varicella zoster,
influenza).
D. ANNUAL REQUIREMENTS
After starting clinical training, and to continue, students will be required to submit the
following on an annual basis:
1. Tuberculosis screening (as described above)
2. Any changes in their immunization history.
Appendix VI
126
Confidential Student Feedback and Comments Form
CLINICALTRAINING
STUDENT CONFIDENTIAL FEEDBACK AND COMMENTS
Course code
Semester - Year
Dear colleague,
We would like to thank you for your time to complete this feedback form. This is an
anonymous and confidential form and will only be used by the Faculty of the School of
Medicine, European University Cyprus. We ask from you to add any comments that
you believe might be of significance, concerning each department of your rotation.
Your contribution will help us improve the content and quality of the clinical rotations
program.
This feedback form has two parts. The first is a table that we ask from you to complete;
the second part concerns comments and suggestions that you may have.
In the following table, please complete each parameter using a scale from 1-5 for each
department:
1. Strongly agree. 2.Agree. 3.Neutral. 4.Disagree. 5.Strongly disagree.
Department
Clinical
Clinical
Duration of rotation
content was
instructors
instructors’
was longer than
educational
showed
use of English
necessary / Number
interest in
was sufficient
of visits were more
student training
than necessary
Department A
Department B
Department C
Comments: Please add any comments that you may have and believe that will
help us improve the clinical training during the upcoming semesters. These
comments may concern the clinical rotations program in general, or specific
departments.
127
Appendix VII
Clinical Competence Building Roadmap
Year
Knowledge
Attitude
Skills
Milestone
Deliverables
1
Structure and function –
Introduction to patient-
Hand hygiene
Graded mpr101 course –
-year 1 logbook
human body in health
doctor relationship
Glove use/disposal
first clinical orientation
-recorded video sessions on
Health and safety
Initiating medical interview
visit plus ward simulation
interdisciplinary
Vital signs
workshops
communication
Multicultural and interdiscplinary
-written assessment on
communication
clinical communication
problems
2
Structure and function –
Dealing with conflict/anger
Nutritional screening
First clinical placement
-year 2 logbook
human body in health
Working with teams
History taking
in primary care in
-recorded video sessions on
and structured approach
Recognizing opportunities
Ecg recording
semester 3 /
team work and history taking
to the patient (transition
for prevention and health
Physical examination of a healthy
First formative osce in
-10 completed history and
year)
promotion
patient
semester 4
examination sets
Venous blood sampling
Iv catheterization
Abgs
Sc/im injections
Mantoux test
3
Structure and function –
Breaking the news
Suturing
Formative and
-year 3 logbook
human body in disease
Passing information
Wound care
summative osce in each
-recorded video sessions on
Iv/io placement
semester
complete primary/secondary
Ngt/peg insertion
Optional certification in
assessment stations
U/c placement
bls
Intubation/airway management
Recognizing abnormal signs/symptoms
Performing basic differential diagnosis
128
4
Core clinical
competences – adults
Triage / assessing patient
severity
Conducting a structured
clinical approach (from
history to treatment)
Managing intimate
examinations
Using decision support
algorithms and scores
Diagnosis and treatment: cardiovascular
/ respiratory / gi / blood and lymphatics /
urinary and endocrine system
Obtaining cultures
Appropriate choice and interpretation of
common imaging modalities
Opportunity for elective
clinical rotations in
coooperating hospitals
abroad
-year 4 logbook
-use of mini cex and dops as
assessment tools in the
clinics (wpba)
5
Core clinical
competences – mental
and child services
Clinical approach to non
cooperative patients
(minors, mental disability)
Bioethical considerations
Diagnosis and treatment:
musculoskeletal / nervous system and
skin, mental and children’s health
-year 5 logbook
-use of mini cex and dops as
assessment tools in the
clinics (wpba)
6
Core clinical
competences – mother
health and emergencies
Multicultural approach to
care
Dealing with disability
(sensory/motor/cognitive)
Breaking the news (death
/ cancer / toxic agent use /
abortion / stillbirth)
Working in teams in
stressful conditions (crisis
management)
Diagnosis and treament:
Reproductive system, eye and ent
conditions, poisonings and emergencies
Observation of advanced skills (lp, cvc,
chest tube, biopsy)
Clinical elective
Free electives in both
semesters with a
potential research
direction
Eligibility for als/ atls /
phtls accreditation
Usmle exam (to practice
in usa)
-year 6 logbook
-lpa assessment
-use of mini cex and dops as
assessment tools in the
clinics (wpba)
-completion of individual
portfolio for residency
applications
-graduation / issue of
medical license

129
Appendix VIII
Student Confidence in Performing Practical and Clinical Skills Questionnaire
Understanding student confidence in performing
practical and clinical skills. 4th Year students, May 2017.
This is an anonymous questionnaire prepared by the clinical training coordinators of the School of
Medicine of EUC.
Our aim is to understand your confidence in performing practical and clinical skills and to improve the
quality of your training. All personal information will be kept confidential. Results of this questionnaire won’t
be used for personal or promotional purposes.
Completion of this questionnaire requires less than 5 minutes.
Thank you in advance for your contribution.
*Required
1. Gender *
Mark only one oval.
Male
Female
Please answer the following questions based on "How confident
do you feel..." performing the following actions, on a scale from 1
to 5, where:
1 = Not confident at all
2 = Mostly Not confident
3 = Not sure - Average confident
4 = Mostly confident
5 = Totally confident

130
2.
1 ...Communicating with a patient who presents acutely with a complaint *
Mark only one oval.
Not confident at all
Mostly Not confident
Not sure - Average confident
Mostly confident
Totally confident
3.
2 ...Obtaining a full medical history of a patient who presents acutely with a complaint. *
Mark only one oval.
Not confident at all
Mostly Not confident
Not sure - Average confident
Mostly confident
Totally confident
4.
3 ...Performing a full respiratory examination on a patient with a respiratory problem. *
Mark only one oval.
Not confident at all
Mostly Not confident
Not sure - Average confident
Mostly confident
Totally confident
5.
4 ...Performing a full cardiovascular examination on a patient with a cardiovascular problem. *
Mark only one oval.
Not confident at all
Mostly Not confident
Not sure - Average confident
Mostly confident
Totally confident

131
6. 5 ...Performing a full neurological examination on a patient with a neurological problem. *
Mark only one oval.
Not confident at all
Mostly Not confident
Not sure - Average confident
Mostly confident
Totally confident
7. 6 ...Performing differential diagnosis in a patient who presents with one or more symptoms. *
Mark only one oval.
Not confident at all
Mostly Not confident
Not sure - Average confident
Mostly confident
Totally confident
8. 7 ...Proposing an investigation plan in a patient who presents with one or more symptoms. *
Mark only one oval.
Not confident at all
Mostly Not confident
Not sure - Average confident
Mostly confident
Totally confident
9. 8 ...Successfully placing a peripheral vein catheter in a patient. *
Mark only one oval.
Not confident at all
Mostly Not confident
Not sure - Average confident
Mostly confident
Totally confident

132
10.
9 ...Successfully placing a urinary catheter in a patient. *
Mark only one oval.
Not confident at all
Mostly Not confident
Not sure - Average confident
Mostly confident
Totally confident
11.
10 ...Successfully obtaining arterial blood gases from a patient. *
Mark only one oval.
Not confident at all
Mostly Not confident
Not sure - Average confident
Mostly confident
Totally confident
133
134
Appendix IX
Comprehensive Clinical Competency Assessment - OSCEs
EUC School of Medicine approves all students for graduation who have successfully completed
the curriculum. Students who have not who have not developed clinical skill competencies
required for graduation are required to undergo remediation and pass a comprehensive clinical
skill examination.
A comprehensive clinical competency assessment is designed for graduation purposes and
includes a rigorous assessment of the clinical skills of senior medical students. It assesses the
candidate’s capacity to take a history, conduct a physical examination, select and interpret
investigational data, formulate diagnostic and management plans, communicate effectively with
patients, relatives and other health workers, and prescribe medicines safely and accurately.
Structure
The exam is a 12-station OSCE examination in clinical skills, which is administered by a team of
examiners at each site, over a period of three hours and thus requires a single morning or
afternoon for every 12 applicants. Details of the OSCE examination will be provided by EUC
coordinators.
Format
The OSCE stations are designed to assess the proficiency of candidates in the fundamental skills
acquired during their five core clinical rotations;
taking a history in Medicine, Psychiatry, Pediatrics, Obstetrics & Gynecology
performing a physical examination of the cardiovascular, respiratory, abdominal and
neurological systems
performing a physical assessment of a surgical patient
completing an exercise in physical diagnosis by interpreting the history, examination
and investigational data findings in an integrated case
communicating a specific issue to a patient or relative against the background of an
ethical dilemma
ordering or prescribing medicines accurately and safely in a defined clinical scenario
Attributes and attitudes The aim of undergraduate medical education is to develop postgraduate
trainees who possess attributes and attitudes that will ensure they are initially competent to
practice safely and effectively and have the basis for further training in any branch of medicine
and for lifelong learning. Attributes should be developed to an appropriate level for the graduate’s
stage of training.
Clinical skills and professional behavior
In terms of clinical skills assessment the attributes and attitudes defined as outcome objectives in
the MD Program are listed below:
Assessment in the exam
In light of the outcome objectives outlined above each station is utilized to assess candidates and
allocate marks according to the following criteria:
History taking
-
interpersonal and communications skills
-
ability to direct and adjust questioning
-
ability to obtain pertinent facts
-
clinical reasoning in relation to diagnosis and management

135
Physical examination
- interpersonal skills
- examination technique
- ability to elicit and demonstrate physical signs
- ability to interpret the examination findings and form a differential diagnosis and
management plan
Communication skills
- initiating the consultation and information gathering
- providing information that is understandable and appropriate
- ability to direct, negotiate and adjust the consultation
- ability to build a relationship and show empathy
Integrated case
- ability to identify key issues in the history
- ability to seek for specific examination findings
- ability to interpret electrocardiograms, radiological images, functional data, hematology
and biochemical results with appropriate management
Safe prescribing
- ability to complete all aspects of a drug chart accurately and legibly
- ability to prescribe correct dose, timing, route and duration of medication appropriately
- ability to adjust medication correctly according to defined clinical scenarios
- ability to maintain patient safety at all times
Characteristics and structure of an OSCE:
An OSCE usually consists of a circuit of short stations (usually 5–10 minutes duration), during
which candidates are examined on real or simulated patients (actors or electronic simulators).
Candidates rotate through the stations, completing all the stations on their circuit. In this way, all
candidates take the same stations.
Objective: candidates get marks for each step that they perform correctly (a preformed checklist
is used).
Structured: stations have very specific tasks and instructions given to the candidate, to the
assessors and to the actors/simulators are very specific
Clinical examination: the OSCE is designed to apply clinical and theoretical knowledge.
When theoretical knowledge is examined, answering questions from the assessor requires that
the questions are standardized and the candidate is only asked questions that are on the mark
sheet; if for example, the candidate is asked any others then there will be no marks for them.
Preparation for OSCE
The OSCE will take place in two given time periods for each discipline: 1.mock OSCEs during the
semester, which are not graded but serve the purpose of preparing for the finals, and 2. the final
OSCE in January, which are graded. For your convenience, you may assign an OSCE coordinator
in your course, to be directly implicated in preparations and OSCE sessions.
1. Mock OSCE: each scenario should last 10-12 minutes. They can include both a clinical
scenario and one clinical skill. For the mock OSCE, students can rotate in groups of 4-6 persons
and not necessarily individually. However, for the clinical skills (separate lab), it is advisable that
students rotate individually, so that they all have the opportunity to practice.

136
2. Final OSCE: these will be performed one-to-one (no group rotations) and each station should
last no more than 6 minutes. Their content is much briefer compared to the mock OSCE and
therefore should focus to evaluate fewer abilities/skills.
How OSCE stations are scored
A detailed mark scheme/checklist is available with a standard set of questions. Each item
on the checklist carries a grading coefficient.
During observation, a preformed checklist is completed by the assessor for each student.
The assessor can often vary the marks depending on how well the candidate performed
the step.
At the end of the mark sheet, the assessor often has a small number of marks that they
can use to weight the station depending on total student performance.
Each station is worth the same as every other station. Total score is the average of all
station scores.
