
Boswell et al • A Systematic Review of Epidural Steroids 319
Pain Physician Vol. 6, No. 3, 2003
Pain Physician. 2003;6:319-334, ISSN 1533-3159
Epidural Steroids in the Management of Chronic Spinal Pain
and Radiculopathy
A Systematic Review
Mark V. Boswell, MD,PhD*, Hans C. Hansen, MD
#
, Andrea M. Trescot, MD**, and Joshua A. Hirsch, MD
##
From *Case Western Reserve University, Cleveland,
Ohio,
#
The Pain Relief Centers, Conover, North Caro-
lina, **The Pain Center, Orange Park, Florida, and
##
Harvard School of Medicine, Boston, Massachu-
setts. Address Correspondence: Mark V. Boswell,
MD, PhD, 11100 Euclid Avenue, Cleveland, Ohio
44106. E-mail: [email protected]
Funding: No external Support was received in
completion of this study
Epidural injections with or without
steroids are used extensively in the man-
agement of chronic spinal pain. However,
evidence is contradictory with continuing de-
bate about the value of epidural steroid in-
jections in chronic spinal syndromes.
The objective of this systematic re-
view is to determine the effectiveness of epi-
dural injections in the treatment of chronic
spinal pain. Data sources include relevant
literature identied through searchs of MED-
LINE, EMBASE (Jan 1966- Mar 2003), manual
searches of bibliographies of known primary
and review articles, and abstracts from sci-
entic meetings. Both randomized and non-
randomized studies were included in the re-
view based on the criteria established by the
Agency for Healthcare Research and Quality
(AHRQ). Studies were excluded from the anal-
ysis if they were simply review or descriptive
and failed to meet minimum criteria.
The results showed that there was
strong evidence to indicate effectiveness of
transforaminal epidural injections in manag-
ing lumbar nerve root pain. Further, evidence
was moderate for caudal epidural injections
in managing lumbar radicular pain. The ev-
idence in management of chronic neck pain,
chronic low back pain, cervical radiculopathy,
spinal stenosis, and post laminectomy syn-
drome was limited or inconclusive.
In conclusion, the evidence of effective-
ness of transforaminal epidural injections in
managing lumbar nerve root pain was strong,
whereas, effectiveness of caudal epidural in-
jections in managing lumbar radiculopathy
was moderate, while there was limited or in-
conclusive evidence of effectiveness of epi-
dural injections in managing chronic spinal
pain without radiculopathy, spinal stenosis,
post lumbar laminectomy syndrome, and cer-
vical radiculopathy.
Keywords: Low back pain, epidural ste-
roids, interlaminar, caudal, transforaminal,
radiculopathy
Lifetime prevalence of spinal pain
has been reported as 65% to 80% in the
neck and low back (1-5). After the initial
episode, modern evidence has shown that
the prevalence of persistent low back and
neck pain ranges from 26% to 75% (6-17).
Patho-anatomic evidence shows that discs
can produce pain in the neck and upper
extremities; thoracic spine, chest wall and
abdominal wall; and low back and lower
extremities. Disc related pain is caused by
disc degeneration, disc herniation, or by
biochemical effects including inflamma-
tion. Human intervertebral disc degen-
eration is a formidable clinical problem
and a leading cause of pain and disability,
resulting in significant healthcare-related
costs (18-22). The degenerative process
in intervertebral discs is associated with
a series of biochemical and morpholog-
ic changes that combine to alter the bio-
mechanical properties of the motion seg-
ment (18, 22-25). Disc degeneration with
or without disc herniation can cause low
back pain (26-30).
Traditionally, compression of nerve
roots or dorsal root ganglion by the her-
niated nucleus pulposus (HNP) has been
regarded as the cause of sciatica, but dur-
ing the past decade, the pivotal role of
multiple etiologies has been implicated.
Thus, proposed etiologies are not lim-
ited to neural compression (22, 26, 27),
but also include vascular compromise (22,
31), inflammation (32-35), biochemical
and neural mechanisms (18, 36-44), in-
ternal disc disruption (45), intraneural
and epidural fibrosis (46-50), dural irrita-
tion (51), spinal stenosis (52), and inflam-
mation and swelling of dorsal root gangli-
on (53-55).
Epidural injection of corticosteroids
is one of the commonly used interven-
tions in managing chronic spinal pain (56-
58). Several approaches are available to ac-
cess the lumbar epidural space: caudal, in-
terlaminar, and transforaminal. Epidural
administration of corticosteroids is one of
the subjects most studied in interventional
pain management with the most systemat-
ic reviews available, though highly contro-
versial (59-71). Bogduk et al (57) in 1994,
after extensive review, concluded that the
balance of the published evidence supports
the therapeutic use of caudal epidurals.
Bogduk (61) in 1999 supported the poten-
tial usefulness of transforaminal steroids
for disc prolapse. Bogduk and Govind
(72) in 1999 concluded that transforami-
nal injection of steroids can be entertained
with the prospect of achieving substantial
and lasting relief of the pain; but if facili-
ties for transforaminal injections are not
available, patients might be offered tempo-
rizing, palliative therapy by means of cau-
dal injection of steroid and local anesthetic
for patients with lumbar radicular pain un-
responsive to lesser, conservative measures,
and for whom surgery might be the only
other option. Bogduk (73) in 1999, in ref-
erence to cervical radicular pain concluded
that in the interest of helping patients avoid
surgery when this is the only other thera-
peutic option being entertained, a cervical
epidural injection of steroids might be of-
fered, or preferably, if facilities are available,
a periradicular injection of steroids might
be offered. However, both of these recom-
mendations (72, 73) apply to acute lumbar
and cervical radicular pain. Bogduk and
McGuirk (74) in reviewing monothera-
py for chronic low back pain (not radicu-

Boswell et al • A Systematic Review of Epidural Steroids320
Pain Physician Vol. 6, No. 3, 2003
Boswell et al • A Systematic Review of Epidural Steroids 321
Pain Physician Vol. 6, No. 3, 2003
lar pain) concluded that epidural steroids
may be indicated for radicular pain, but
they are not indicated for acute back pain
and there is no evidence that they are effec-
tive for chronic low back pain. Koes et al
(62, 63) in a systematic review of random-
ized clinical trials concluded that the effica-
cy of epidural steroid injections has not yet
been established and their benefit, if any,
seems to be of short duration only. van
Tulder et al (65, 75) in 1997 and 2000, con-
cluded that there was conflicting evidence
that epidural steroid injections provide
better short-term pain relief than placebo
for patients with radicular symptoms. Fur-
ther, they concluded that there was mod-
erate evidence that epidural steroid injec-
tions were not effective for chronic low
back pain without radicular symptoms.
Watts and Silagy (64) in a 1995 meta-anal-
ysis, concluded that epidural steroids were
effective based on the definition of effec-
tiveness in terms of pain relief (at least a
75% improvement) in the short-term (60
days) and in the long-term (1 year). Mc-
Quay and Moore (68) in 1998 concluded
that epidural corticosteroid injections were
effective for back pain and sciatica, provid-
ing substantial relief for up to 12 weeks,
but few patients with chronic spinal pain
reported complete relief with majority re-
turning for repeated epidural injections.
Nelemans et al (66) in 2001, in a Cochrane
review of injection therapy, concluded that
epidural steroid injections were not effec-
tive in management of chronic low back or
radicular pain. Vroomen et al (69) in 2000,
in a review of conservative treatment of sci-
atica, concluded that epidural steroids may
be beneficial for subgroups of nerve root
compression. Rozenberg et al (70) in 1999
were unable to determine whether epidural
steroids are effective in common low back
pain and sciatica based on their review. In
contrast, Manchikanti et al (56, 58) in re-
viewing the literature in 2001 and 2003, re-
viewed three types of epidurals separately
rather than in combination as the previous
reviews. They concluded that there was fa-
vorable evidence for caudal epidural ste-
roid injections and transforaminal epidu-
ral steroid injections in managing chronic
low back pain. There are no systematic re-
views available describing pain of cervical
or thoracic origin.
Mechanism of action of epidural in-
jections is not well understood. It is be-
lieved that neural blockade alters or in-
terrupts nociceptive input, reflex mecha-
nisms of the afferent limb, self-sustaining
activity of the neuron pools and neuraxis,
and the pattern of central neuronal activi-
ties (76). Explanations for improvements
are based in part on the pharmacological
and physical actions of local anesthetics,
corticosteroids, and other agents. It is be-
lieved that local anesthetics interrupt the
pain-spasm cycle and reverberating noci-
ceptor transmission, whereas corticoste-
roids reduce inflammation either by in-
hibiting the synthesis or release of a num-
ber of pro-inflammatory substances and
by causing a reversible local anesthetic ef-
fect (77-90), even though an inflamma-
tory basis for either cervical or radicular
pain has not been proven (72, 73).
This systematic review was under-
taken due to conflicting opinions and in-
conclusive evidence in the literature. Fur-
ther, authors strongly believe that due to
the inherent variations and differences
in the 3 techniques applied in delivery of
epidural steroids, previous reviews were
not only incomplete, but also inaccurate.
Thus, due to variations, differences, ad-
vantages, and disadvantages applicable to
each technique (including the effective-
ness and outcomes), caudal epidural in-
jections; interlaminar epidural injections
(cervical, thoracic, and lumbar epidural
injections); and transforaminal epidural
injections (cervical, thoracic, and lumbo-
sacral) are considered as separate entities
within epidural injections and are evalu-
ated as such.
METHODS
Literature Search
Our literature search included MED-
LINE, EMBASE (Jan 1966 – Mar 2003),
systematic reviews, narrative reviews,
cross-references to the reviews and vari-
ous published trials; and peer reviewed ab-
stracts from scientific meetings during the
past two years. The search strategy consist-
ed of diagnostic interventional techniques,
epidural injections and steroids, transfo-
raminal epidurals, nerve root blocks, and
caudal epidural steroids, with emphasis on
chronic pain/low back pain/neck pain/mid
back or thoracic pain or spinal pain.
Selection Criteria
The review focused on randomized
and non-randomized evaluations. The
population of interest was patients suf-
fering with chronic spinal pain for at least
3 months. Three types of epidural injec-
tions with local anesthetic, steroid, or oth-
er drugs, provided for management of
spinal pain were evaluated. All the studies
providing appropriate management with
outcome evaluations of 3 months and sta-
tistical evaluations were reviewed. The
primary outcome measure was pain relief
at various points. The secondary outcome
measures were functional status improve-
ment and complications.
For evaluating the quality of individ-
ual articles, we have used the criteria from
the Agency for Healthcare Research and
Quality (AHRQ) publication (91). This
document described important domains
and elements for randomized and non-
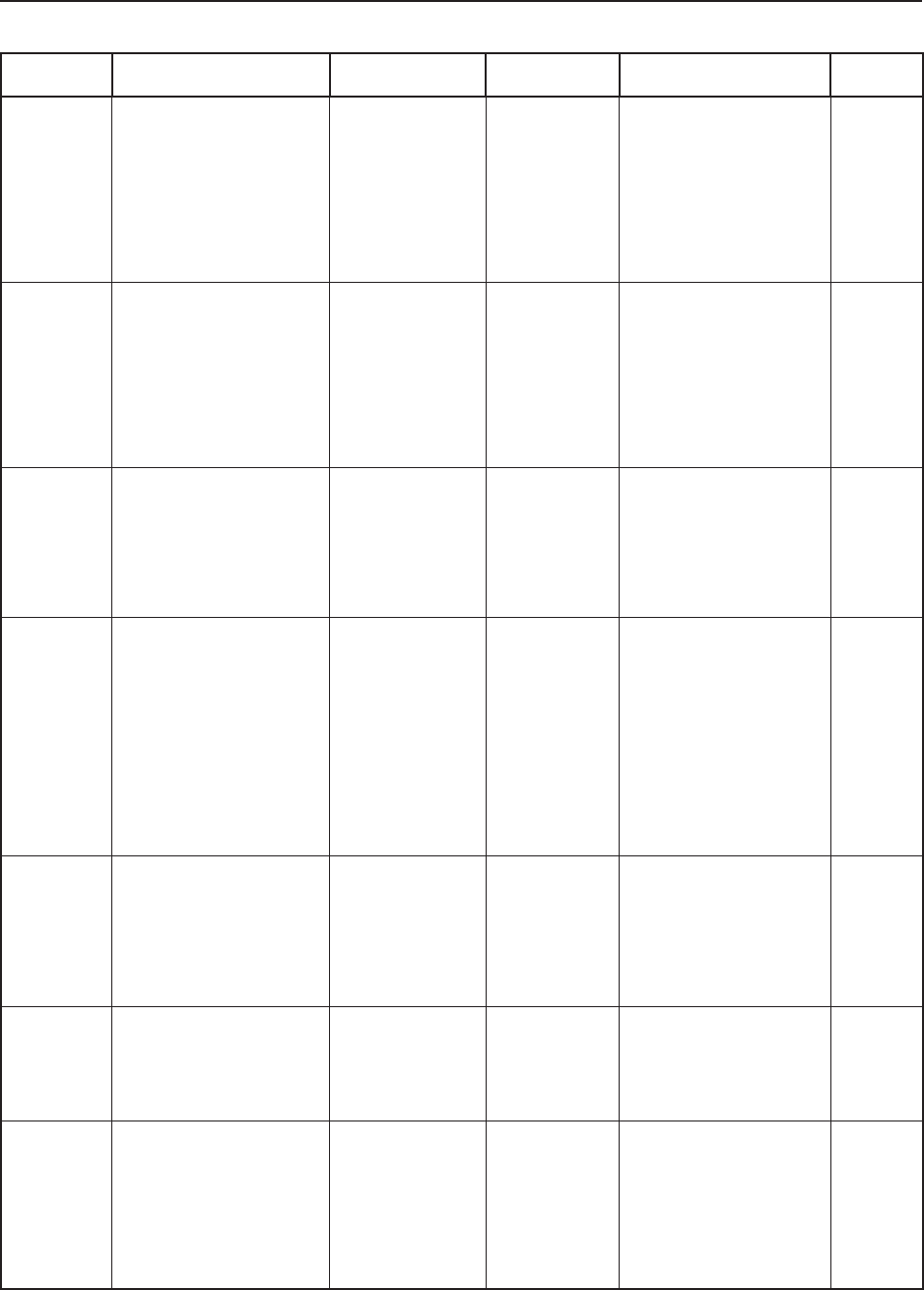
randomized trials as shown in Table 1.
Data Extraction
Study evaluation and inclusion and
exclusion algorithmic approach is shown
in Table 2. Methodologic quality assess-
ment was performed as described in Ta-
ble 1. A score of 4 or more of 7 for ran-
domized trials and a score of 3 or more
Randomized Clinical Trials Observational Studies
1. Study question Study question
2. Study population Study population
3. Randomization Comparability of subjects
4. Blinding
5. Interventions Exposure or intervention
6. Outcomes Outcome measurement
7. Statistical analysis Statistical analysis
8. Results Results
9. Discussion Discussion
10. Funding or sponsorship Funding or sponsorship
Table 1. AHRQ’s important domains and elements for systems to rate quality
of individual articles (91)
* Key domains in italics

Boswell et al • A Systematic Review of Epidural Steroids320
Pain Physician Vol. 6, No. 3, 2003
Boswell et al • A Systematic Review of Epidural Steroids 321
Pain Physician Vol. 6, No. 3, 2003
of 5 was required to meet inclusion crite-
ria. Studies were also eliminated if there
were no appropriate outcomes of at least
3 months or statistical analysis.
Modified quality abstraction forms
described by AHRQ were utilized. All the
potential studies were evaluated by the 3
authors. Any disagreements were resolved
by consensus.
Qualitative Analysis
Qualitative analysis was conduct-
ed, using five levels of evidence for effec-
tiveness of epidural steroids as illustrated
in Table 3. Pain relief was evaluated on
both a short-term (less than 3 months)
and long-term (3 months or longer) ba-
sis. A study was judged to be positive if
the authors concluded that the epidural
steroid injection therapy was more effec-
tive than the reference treatment in ran-
domized trials or simply concluded that it
was effective. All other conclusions were
considered negative. If in the opinion of
reviewers, there was conflict with the con-
clusion, the conclusions were changed
with appropriate explanation.
RESULTS
Caudal Epidural Injections
Multiple reports studying caudal epi-
dural injections included 8 randomized or
double blind trials (92-99), 4 prospective
trials (100-103), and multiple retrospec-
tive evaluations (104-107). The results of
published reports of the randomized tri-
als are described in Table 4, while Table 5
shows description of non-randomized tri-
als (prospective and retrospective).
Of the 8 randomized or double blind
trials, 2 trials were excluded. One study
was excluded (96), due to non-availability
of analyzable information. A second trial
(95) was excluded due to lack of data at 3
months. Of the remaining 6 trials, 4 were
positive for short-term pain relief (92,
93, 97, 98), and 4 were positive for long-
term relief (92, 94, 97, 98). Among the 4
prospective trials (100-103) and 4 retro-
spective trials (104-107) meeting inclu-
sion criteria, all were positive for short-
term and long-term relief with multiple
injections.
Among 6 randomized trials in-
cluded for analyses (92-94, 97-99), only
3 studied predominantly patients with
radiculopathy or sciatica (92-94), 2 stud-
ied post lumbar laminectomy syndrome
(98, 99), and 1 studied mixed population
(97). Of the 3 trials evaluating predomi-
nantly radiculopathy, 2 were positive (92,
93) and one study was negative (94) for
short-term relief, whereas 2 of 3 were pos-
itive for long-term relief (92, 94). Among
two studies with postlumbar laminec-
tomy syndrome (98, 99), only one study
(98) was positive in short-term and long-
term. None of the studies included only
the patients with chronic low back pain.
Among the non-randomized evalua-
tions, including retrospective studies, four
(102-104, 106) of eight (100-107) includ-
ed patients with radicular pain or sciatica,
all showing positive results. Three studies
essentially included patients with chronic
low back pain without demonstrated ra-
dicular pain (100, 101, 105). One study
(107) evaluated the patients with lumbar
canal stenosis.
Interlaminar Epidural Injections
Multiple studies evaluating the ef-
fectiveness of interlaminar epidural in-
jections, specifically the lumbar epidu-
ral injections included 16 randomized
or double blind trials (108-123), 8 non-
randomized prospective trials (124-131),
Table 2. Study evaluation (inclusion/exclusion) algorithm
Study Population
Specific inclusion/exclusion criteria
and
Appropriate diagnostic criteria
No
Yes
No
No
Yes
Yes
Study
Eliminated
Study
Included
Outcomes
Statistical Analysis
Level I -
Conclusive: Research-based evidence with multiple relevant and high-quality
scientic studies or consistent reviews of meta-analyses.
Level II - Strong: Research-based evidence from at least one properly designed randomized,
controlled trial of appropriate size (with at least 60 patients in smallest group); or
research-based evidence from multiple properly designed studies of smaller size; or
at least one randomized trial, supplemented by predominantly positive prospective
and/or retrospective evidence.
Level III – Moderate: Evidence from a well-designed small randomized trial or evidence from
well-designed trials without randomization, or quasi-randomized studies, single
group, pre-post cohort, time series, or matched case-controlled studies or positive
evidence from at least one meta-analysis.
Level IV – Limited: Evidence from well-designed nonexperimental studies from more than one
center or research group
Level V –
Indeterminate: Opinions of respected authorities, based on clinical evidence,
descriptive studies, or reports of expert committees.
Table 3. Designation of levels of evidence

Boswell et al • A Systematic Review of Epidural Steroids322
Pain Physician Vol. 6, No. 3, 2003
Boswell et al • A Systematic Review of Epidural Steroids 323
Pain Physician Vol. 6, No. 3, 2003
Study/Methods Participants Interventions Outcomes Results
Outcomes/
Conclusion
Breivik et al (92)
Randomized
double blind trial.
Randomization
according to a
list of random
numbers.
Parallel, cohort
design
35 patients with
incapacitating
chronic low back pain
and sciatica.
Diagnosis based
on radiculopathy:
arachnoiditis (n=8),
no abnormality
(n=11), inconclusive
ndings (n=5).
Duration: several
months to several
years.
Caudal epidural injection:
Experimental: 20 mL
bupivacaine 0.25% with 80
mg depomethylprednisone
(n=16)
Placebo: 20 mL bupivacaine
0.25% followed by 100 mL
saline (n=19).
Frequency: up to three
injections at weekly intervals.
Timing: not mentioned.
Outcome measures:
1. Pain relief:
signicant diminution of
pain and/or paresis to
a degree that enabled
return to work.
2. Objective
improvement: sensation,
Lasègue’s test, paresis,
spinal reexes, and
sphincter disorders.
56% of the patients
reported considerable
pain relief in experimental
group compared to 26% of
the patients in the placebo
group.
Positive
short-term
and long-
term relief
Bush and Hillier
(93)
Randomized double
blind trial.
28 patients were
randomized; only
23 patients were
entered into the
study.
23 patients with
lumbar nerve root
compromise.
Mean duration
(range) in
experimental group:
5.8 months (1-13
months) and in
control group 4.7
months (1-12).
Caudal epidural injections:
Experimental: 25 mL:
80 mg triamcinolone
acetonide + 0.5% procaine
hydrochloride (n=12)
Control: 25 mL normal saline
(n=11)
Frequency: two caudal
injections, the rst after
admission to the trial and a
second after 2 weeks
Timing: four weeks and
at one year.
Outcome measures:
1. Effect on lifestyle.
2. Back and leg pain
3. Angle of positive SLR.
Signicantly better results
with pain and straight leg
raising in experimental
group in short-term.
Pain not signicantly
different but straight leg
raise signicantly better
for long-term relief.
Positive
short-term
relief and
negative
long-term
relief
Matthews et al (94)
Double blind.
Stratication by
age and gender.
Survival curve
analyses based on
cumulative totals
recovered.
57 patients with
sciatica with a single
root compression
Experimental group:
male/female: 19/4,
median duration of
pain: 4 weeks (range:
8 days-3 months).
Control group:
male/female: 24/10,
median duration of
pain: 4 weeks (range:
3 days-9 weeks).
Caudal epidural injections:
Experimental: 20 mL
bupivacaine 0.125% + 2 mL
(80 mg) methylprednisolone
acetate (n=23).
Control: 2 mL lignocaine
(over the sacral hiatus or into
a tender spot) (n=34)
Frequency: fortnightly
intervals, up to three times
as needed
Timing: 2 weeks, 1, 3, 6,
and 12 months.
Outcome measures:
1. Pain (recovered vs not
recovered).
2. Range of movement
3. Straight leg raising
4. Neurologic
examination
There was no signicant
difference between
experimental and control
group with short-term
relief (67% vs 56%).
After 3 months, patients
in experimental group
reported signicantly more
pain-free than in control
group.
Negative
short-term
relief and
positive
long-term
relief
Helsa and Breivik
(97)
Double blind trial
with crossover
design
69 patients with
incapacitating
chronic low back pain
and sciatica.
36 of 69 previously
been operated on for
herniated disc.
Three caudal epidural
injections of either
bupivacaine with
depomethylprednisolone
80 mg or with bupivacaine
followed by normal saline.
If no improvement had
occurred after 3 injections, a
series of the alternative type
of injection was given.
Timing: not mentioned.
Outcome measures:
signicant improvement
to return to work or to
be retrained for another
occupation
i. 34 of the 58 patients
(59%) receiving caudal
epidural injections
of bupivacaine and
depomethylprednisolone
showed signicant
improvement.
ii. 12 of 49 patients (25%)
who received bupivacaine
followed by saline were
improved.
Positive
short-term
and long-
term relief
Revel et al (98)
Randomized trial.
60 post lumbar
laminectomy patients
with chronic low back
pain
Forceful caudal injection:
Experimental: 125 mg of
prednisolone acetate with
40 mL of normal saline in the
treatment group.
Control: 125 mg of
prednisolone in the control
group.
Timing: 6 months.
Outcome measures: pain
relief.
The proportion of patients
relieved of sciatica was
49% in the forceful
injection group compared
to 19% in the control group
with signicant difference.
Positive
short-term
and long-
term relief
Meadeb et al (99)
Randomized trial.
Parallel-group
study.
47 post lumbar
laminectomy
syndrome patients in
a multicenter study.
Experimental group: forceful
injection of 20 mL of normal
saline with or without 125
mg of epidural prednisolone
acetate.
Control group: 125 mg of
epidural prednisolone.
Frequency: each of the 3
treatments were provided
once a month for 3
consecutive months.
Timing: day 1, day 30
and day 120.
Outcome measures:
visual analog scores.
The VAS scores improved
steadily in the forceful
injection group, producing
a nonsignicant difference
on day 120 as compared to
the baseline (day 30=120
days).
Negative
short-term
and long-
term relief
Table 4. Characteristics of published randomized trials of caudal epidural injections

Boswell et al • A Systematic Review of Epidural Steroids322
Pain Physician Vol. 6, No. 3, 2003
Boswell et al • A Systematic Review of Epidural Steroids 323
Pain Physician Vol. 6, No. 3, 2003
Study/
Methods
Participants Interventions Outcomes Results Outcomes/
Conclusion
Yates (102)
Prospective
evaluation
20 patients with low
back pain and sciatica.
Group I: 60 mg of triamcinolone
(3 mL + 47 mL normal saline)
Group II: 60 mg of triamcinolone
(3 mL + 47 mL lignocaine 0.5%)
Group III: 50 mL saline
Group IV: 50 mL lignocaine
Injections were given at weekly
intervals in a random order
Timing not mentioned.
Subjective and objective
criteria of progress.
Study did not address
pain-relief.
Study focused on
improvement in straight
leg raising which seemed
to correlate with pain-
relief.
Greatest improvement
was noted after the
injection containing
steroid.
The results suggested
that the action of a
successful epidural
injection is primarily
anti-inammatory
and to a lesser extent,
hydrodynamic.
Positive
short-term
and long-
term relief.
Waldman
(103)
Prospective
evaluation
with
independent
observer
review.
53 patients meeting
stringent inclusion
criteria with radicular
pain distribution
anatomically
correlating with
documented disc
herniation and nerve
root impingement.
Treatment: 7.5 mL of 1%
lidocaine and 80 mg of
methylprednisolone with
the rst block and 40 mg of
methylprednisolone with
subsequent blocks.
Subsequent blocks were
repeated in 48 to 72 hour
intervals with the end point
being complete pain relief or 4
caudal epidural blocks.
Timing: 6 weeks, 3
months, 6 months.
Visual analog scale and
verbal analog scores.
Combined visual analog
scale and verbal analog
scores for all patients
were reduced 63% at 6
weeks, 67% at 3 months,
and 71% at 6 months.
Positive
short-term
and long-
term relief.
Manchikanti
et al (100)
A randomized
trial with
convenient
control
group.
70 patients after
failed conservative
management with
physical therapy,
chiropractic and
medication therapy.
All patients were
shown to be negative
for facet joint pain.
Caudal epidural injections:
Group I : no treatment
Group II: local anesthetic and
Sarapin total of 20 mL with 10
mL each.
Group III: 10 mL of local
anesthetic and 6 mg of
betamethasone
Timing: 2 weeks, 1
month, 3 months, 6
months and 1 year.
Outcome measures:
Average pain, physical
health, mental health,
and functional status
Average pain, physical
health, mental health,
functional status, narcotic
intake and employment
improved signicantly
in Group II and Group III
at 2 weeks, 1 month, 3
months, 6 months and
1 year.
Positive
short-term
and long-
term relief.
Manchikanti
et al (101)
Prospective
evaluation in
discogram-
positive and
discogram-
negative
chronic low
back pain
patients.
62 patients were
evaluated.
Negative provocative
discography: 45
patients
Positive provocative
discography: 17
patients
Caudal epidural injections (1-3)
with or without steroids.
Timing: 1 month, 3
months, and 6 months.
Average pain, physical
health, mental health,
functional status,
psychological status,
symptom magnication,
narcotic intake and
employment status.
69% of the patients in
the negative discography
group and 65% of the
patients in the positive
discography group were in
successful category.
Comparison of
overall health status,
psychological status,
narcotic intake and
return to work showed
signicant improvement in
successful category.
Positive
short-term
and long-
term relief.
Hauswirth
and Michot
(104)
Retrospective
evaluation
75 patients with
chronic low back pain
and sciatica
Caudal epidural injections of
local anesthetic and steroids
Timing: not mentioned
Outcome measures: pain
relief
Results were excellent in
60% and good in 24%.
16% of the patients
showed no improvement.
Positive
short-term
and long-
term relief.
Manchikanti
et al (105)
Retrospective
evaluation of
225 patients
with chronic
low back
pain.
Chronic pain
patients who have
failed to respond
to conservative
management with
physical therapy,
chiropractic and
medical therapy.
Group I: Blind lumbar epidural
steroid injections,
Group II: Caudal epidural steroid
injections under uoroscopy.
Group III: Transforaminal
epidural corticosteroid
injections under uoroscopic
visualization.
Duration of pain relief
with each injection.
Outcome measures:
relief ≥ 50%
Cumulative signicant
relief, was reported
following 3 procedures
for a mean of 10.3
+0.96 weeks in patients
receiving caudal
epidurals, in contrast
to 6.7 + 0.37 weeks in
patients receiving blind
lumbar epidural steroid
injections.
Positive
short-term
and long-
term relief.
Table 5. Characteristics and results of non-randomized studies of caudal epidural injections

Boswell et al • A Systematic Review of Epidural Steroids324
Pain Physician Vol. 6, No. 3, 2003
Boswell et al • A Systematic Review of Epidural Steroids 325
Pain Physician Vol. 6, No. 3, 2003
Study/
Methods
Participants Interventions Outcomes Results Outcomes/
Conclusion
Goebert et al
(106)
Retrospective
evaluation of
113 patients.
113 patients at a
tertiary care center
receiving 120
injections. 94 were
caudal epidural
injections
There were no
objective signs present
in the patients.
Epidural injections of 30 mL of
1% procaine combined with 125
mg of hydrocortisone acetate
usually for 3 consecutive or
alternate days.
Timing: 3 months
Pain relief:
Good result 60% relief for
3 months or longer
Failures: 40% to 60%
relief
Poor results: return
of pain in less than 3
months or less than 40%
of relief.
Overall good results in
72% of the patients with
poor results in 17%.
Positive
short-term
and long-
term relief.
Ciocon et al
(107)
Evaluation
of elderly
patients
30 patients with
various degrees of
degenerative lumbar
canal stenosis treated
with caudal epidural
steroid injections.
Mean age: 76 + 6.7 yrs
A total of 3 caudal epidural
steroid injections of 0.5%
lidocaine with 80 mg
of methylprednisolone
administered at weekly intervals
Timing: initial and at 2-
month intervals up to 10
months.
Outcome measures:
the Roland 5-point pain
rating scale.
Pain reduction and
walking capability.
The results showed
signicant pain reduction
for up to 10 months, with
satisfactory relief in 90%
of the patients.
Positive
short-term
and long-
term relief.
Table 5. Characteristics and results of non-randomized studies of caudal epidural injections (Continued)
and multiple other observational trials
(132-161).
Of the 16 studies, 8 studies were ex-
cluded and only 8 met inclusion crite-
ria. One study (112) was excluded as they
studied effects of subarachnoid and epi-
dural midazolam. Two studies (118, 119)
studied diabetic polyneuropathy and in-
tractable post herpetic neuralgia. One
study (123) evaluated only inpatients,
whereas 3 evaluations (113, 114, 120)
failed to evaluate long-term relief, and
finally, one study (121) was not includ-
ed due to lack of data for review. Table
6 illustrates various characteristics and re-
sults of published randomized or double
blind trials meeting inclusion criteria. Of
the 8 non-randomized prospective trials,
only 3 trials (124-126) met criteria for in-
clusion, whereas the remaining 5 studies
(127-131) were eliminated due to multi-
ple issues.
Of the 8 randomized trials included
in evaluation, 6 were positive for short-
term relief (108, 111, 115-117, 122),
whereas only 3 were positive for long-
term relief (111, 117, 122). Numerous
non-randomized trials, both prospective
and retrospective, reported good results
in 18% to 90% of patients receiving cer-
vical or lumbar interlaminar epidural ste-
roid injections, however, without specific
follow-up period. Among the 3 prospec-
tive trials included for evaluation (124-
126), only one was positive (125), one was
indeterminate (124), and one was nega-
tive (126).
Of the 2 randomized trials, which
were positive, Dilke et al (111) studied low
back pain and sciatica, whereas Cataneg-
ra (117) studied chronic cervical radicu-
lar pain. Cuckler et al (110) also included
post lumbar laminectomy syndrome pa-
tients with overall negative results. Due
to a multitude of randomized trials and
availability of double blind or random-
ized, and non-randomized prospective
trials in managing lumbar radicular pain,
evidence from retrospective trials was not
included. However, due to only one ran-
domized trial (117) and one prospective
study (122), in managing cervical radicu-
lar pain, multiple retrospective trials (132-
144) were included for review. Retrospec-
tive reports were also considered in man-
aging chronic low back pain with or with-
out radiculopathy (145-161).
Some studies evaluated the effec-
tiveness of cervical epidural steroid in-
jections in patients not only with cervi-
cal radicular pain, but also other cervical
pain problems (134, 137, 140, 142). One
study (138) studied patients with cervi-
cal radiculopathy. All these retrospective
studies show that there is probable bene-
fit in a significant number of patients in
short-term, however the benefits appear
to be limited in long-term. The results
for chronic low back pain also showed
positive results in short-term and nega-
tive results in long-term in chronic low
back pain.
Transforaminal Epidural Injections
Multiple reports evaluating the effec-
tiveness of transforaminal epidural injec-
tions included 7 randomized trials (120,
162-167); 8 prospective evaluations (124,
168-174); one prospective evaluation of
change in size and pattern of disc hernia-
tion (175); and multiple retrospective re-
ports (105, 176-187).
Among the 7 randomized controlled
trials, only 3 trials (120, 162, 164) met cri-
teria for inclusion. The trial by Kolsi et
al (166) was not included since the mea-
surements were only of short-term dura-
tion. Devulder et al (165) evaluated the
effectiveness of transforaminal epidurals
in post laminectomy syndrome. Karp-
pinen et al (163, 164) used two publi-
cations to report the results of one tri-
al. Buttermann (167) presented prelimi-
nary results at a scientific meeting in 1999
without subsequent publication. Details
of the randomized trials examining the
effectiveness of transforaminal epidural
steroid injections in the management of
spinal pain are illustrated in Table 7. All
3 studies showed effectiveness of trans-
foraminal epidural steroids in managing
nerve root pain. One study (164) showed
ineffectiveness of transforaminal epidur-
als for disc extrusions.
Among the prospective evaluations,
3 investigations, those of Vad et al (169),
Lutz et al (168), and Bush and Hilli-
er (124) met inclusion criteria. Others
were excluded because some were per-
formed under CT, long-term results were
not evaluated in some, and in others, mul-
tiple injections were performed in a short
period of time. As shown in Table 8, all
3 prospective trials (124, 168, 169) were
positive for short-term and long-term
relief. Among the retrospective evalu-
ations, 4 studies by Weiner and Fraser
Boswell et al • A Systematic Review of Epidural Steroids324
Pain Physician Vol. 6, No. 3, 2003
Boswell et al • A Systematic Review of Epidural Steroids 325
Pain Physician Vol. 6, No. 3, 2003
Study/
Methods
Participants Interventions Outcomes Results Outcomes/
Conclusion
Carette et al
(108)
Randomized
double blind
trial
158 patients with sciatica due to
a herniated nucleus pulposus.
78 patients in the treatment
group.
80 patients in the placebo
group.
50% of the patients had L4/5
disc herniation and 46% of
the patients had L5/S1 disc
herniation.
Experimental group:
methylprednisolone
acetate (80 mg and 8
mL of isotonic saline)
Control group: isotonic
saline 1 mL
Frequency: 3 epidural
injections 3 weeks
apart
Timing: 6 weeks, 3
months, 12 months
Outcome
measures:
Need for surgery
Oswestry Disability
scores
After 6 weeks, a signicant
difference was seen with
improvement in leg pain in the
methylprednisolone group.
After 3 months, there were no
signicant differences between
groups.
At 12 months, the cumulative
probability of back surgery was
equal in both groups.
Positive
short-term
Negative
long-term
relief
Snoek et al
(109)
Randomized
trial
51 patients with lumbar root
compression documented
by neurological decit and a
concordant abnormality noted
on myelography.
27 patients in experimental
group
24 patients in control group
Experimental
group: 80 mg of
methylprednisolone
(2 mL)
Control group: 2 mL of
normal saline
Frequency: single
injection
Timing: 3 days and
an average of 14
months
Outcome
measures:
Pain, sciatic nerve
stretch tolerance,
subjective
improvement,
surgical treatment.
No statistically signicant
differences were noted in
either group with regards to
low back pain, sciatic nerve
stretch tolerance, subjective
improvement, and surgical
treatment.
Negative
short-term
and long-
term relief
Cuckler et al
(110)
Randomized
double blind
trial
73 patients with back pain
due to either acute herniated
nucleus pulposus or spinal
stenosis.
Duration: greater than 6 months.
Experimental group = 42
patients, control group = 31
patients
Experimental group:
80 mg (2 mL) of
methylprednisolone +
5 mL of procaine 1%
Control group: 2
mL saline + 5 mL of
procaine 1%
Timing: 24 hours
and an average of
20 months
Outcome
measures:
subjective
improvement.
Need for surgery.
There was no signicant short-
term or long-term improvement
among both groups.
Negative
short-term
and long-
term relief
Dilke et al (111)
Randomized
trial
100 patients with low back pain
and sciatica of 1 week to more
than 2 yrs.
51 patients in experimental
group
48 patients in control group
Experimental
group: 10 mL of
saline + 80 mg of
methylprednisolone
Control group: 1 mL of
saline
Frequency: up to 2
injections separated
by 1 week
All patients received
physical therapy with
hydrotherapy and
exercise
Timing: 2 weeks
and 3 months
Outcome
measures: time of
bedrest, days of
hospitalization,
pain relief,
consumption of
analgesics and
resumption of
work 3 months
later
60% of the patients in the
treatment group and 31% of the
patients in the control group
improved immediately after the
injections.
A greater proportion of actively
treated patients had no pain at
3 months, took no analgesics,
resumed work and fewer of
them underwent subsequent
surgery or other non-surgical
treatment.
Positive
short-term
and long-
term relief
Ridley et al
(115)
Randomized
trial
35 patients with low back pain
and sciatica of mean duration
approximately 8 months
19 patients in experimental
group
16 patients in control group
Experimental
group: 10 mL of
saline + 80 mg of
methylprednisolone
(n=19)
Control group: saline
2 mL, interspinous
ligament (n=16)
Timing: 1 weeks, 2
weeks, 3 months
and 6 months
Outcome
measures:
pain control
improvement in
straight leg raising
90% of the patients in the
treated group compared to 19%
in the control group showed
improvement at 1 week, 2
weeks and 12 weeks.
By 24 weeks, the relief
deteriorated to pre-treatment
levels
Positive
short-term
relief
Negative
long-term
relief
Rogers et al
(116)
Randomized
single blind
sequential
analysis
30 patients with low back pain
15 patients in experimental
group
15 patients in control group
Experimental group:
local anesthetic +
steroid
Control group: local
anesthetic alone
Timing: 1 month
Outcome
measures: pain
relief
Nerve root tension
signs
Lumbar epidural injection
of steroid together with
local anesthetic produced
signicantly better results.
Long-term results were similar
for both.
Positive
short-term
relief
Negative
long-term
relief
Catanegra et al
(117)
Randomized
trial with
cervical
interlaminar
epidural
steroid
injections
24 patients with chronic cervical
radicular pain, however without
need of surgery, but suffering for
more than 12 months
i. 14 patients receiving local
anesthetic and steroid
ii. 10 patients receiving local
anesthetic, steroid + morphine
sulfate
i. 0.5% lidocaine
+ triamcinolone
acetonide
ii. Local anesthetic
+ steroid + 2.5 mg of
morphine sulfate
Timing: 1 month,
3 months, and 12
months
Outcome
measures: pain
relief
The success rate was 79% vs.
80% in group I and II.
Overall, initial success rate was
96%, 75% at 1 month, 79% at
3 months, 6 months, and 12
months.
Positive
short-term
and long-
term relief
Table 6. Characteristics of published randomized trials of interlaminar epidural injections

Boswell et al • A Systematic Review of Epidural Steroids326
Pain Physician Vol. 6, No. 3, 2003
Boswell et al • A Systematic Review of Epidural Steroids 327
Pain Physician Vol. 6, No. 3, 2003
Study/
Methods
Participants Interventions Outcomes Results Outcomes/
Conclusion
Stav et al (122)
Randomized
trial of cervical
epidural
steroid
injections
52 patients with chronic,
resistant cervical brachialgia
25 patients in experimental
group
17 patients in control group
Experimental group:
cervical epidural
steroid and lidocaine
injections
Control group:
steroid and lidocaine
injections into the
posterior neck
muscles
Frequency: 1 to 3
injections were
administered at 2
weeks intervals,
based on the clinical
response
All patients continued
pre-study treatment
with drugs and
physiotherapy
Timing: 1 week and
1 year
Outcome
measures: pain
relief, change
in deep tendon
reexes or sensory
loss, change in
range of motion
Reduction of daily
dose of analgesics
Return to work
After 1 week, 76% of the
patients in cervical epidural
group compared to 36% of the
patients in the neck injection
group showed improvement.
At 1 year, 68% of the cervical
epidural group continued to
have relief compared to 12% of
the control group.
Positive
short-term
and long-
term relief
Table 6. Characteristics of published randomized trials of interlaminar epidural injections (Continued)
Study/
Methods
Participants Interventions Outcomes Results Outcomes
/Conclusion
Riew et al (162)
Randomized
double blind
trial
55 patients with lumbar
disc herniations or spinal
stenosis referred for surgical
evaluation.
All subjects had clinical
indications for surgery, and
radiographic conrmation of
nerve root compression.
All patients had failed a
minimum of 6 weeks of
conservative care or had
unrelenting pain.
28 patients in experimental
group (71%)
27 patients in control group
(33%)
Experimental group:
transforaminal nerve root or
epidural steroid injection with
1 mL of 0.25% bupivacaine
and 6 mg of betamethasone
Control group: 1 mL of 0.25%
bupivacaine.
The patient was allowed to
choose to receive as many as
4 injections at any time during
the follow-up.
Timing: 1 year
Outcome measures:
Injections were
considered to have
failed if the patient
opted for operative
treatment.
Multiple injection
therapy was not
considered as
failure.
North American
Spine Society
questionnaire.
Of the 28 patients
in the experimental
group with
bupivacaine and
betamethasone, 20
decided not to have
the operation.
Of the 27 patients
in the control group
receiving bupivacaine
alone, 9 elected
not to have the
operation. They had
highly signicant pain
relief and functional
improvement.
Positive
short-term
and long-term
relief.
Kraemer et al
(120)
Randomized
double blind
study
49 patients with lumbar
radicular symptoms with 24
patients in the steroid group
and 25 patients in the normal
saline group.
Experimental group:
transforaminal epidural with
local anesthetic and 10 mg of
triamcinolone.
Control group: local
anesthetic only.
Normal saline group received
IM steroid injections to avoid
the systemic steroid effect.
Timing: not
mentioned
Outcome measures:
Pain relief
Single-short epidural
perineural injection
was effective it the
treatment of lumbar
radicular pain.
Positive
short-term
and long-term
relief.
Karppinen et al
(163, 164)
Randomized
double blind
trial
160 consecutive, eligible
patients with sciatica with
unilateral symptoms of 1 to 6
months duration.
None of the patients have
undergone surgery.
Experimental group:
local anesthetic and
methylprednisolone
Control group:
normal saline
Timing: 2 weeks, 3
months, 6 months
Outcome measures:
Pain relief, sick
leaves, medical
costs, and future
surgery
Nottingham Health
Prole
In the case of
contained herniations,
the steroid injection
produced signicant
treatment effects
and short-term in
leg pain, straight leg
raising, disability and
in Nottingham Health
Prole, emotional
reactions and cost
effectiveness.
Positive
short-term
and long-term
relief.
Table 7. Details of randomized trials studying the effectiveness of transforaminal epidural steroid injections for
low back pain

Boswell et al • A Systematic Review of Epidural Steroids326
Pain Physician Vol. 6, No. 3, 2003
Boswell et al • A Systematic Review of Epidural Steroids 327
Pain Physician Vol. 6, No. 3, 2003
Study/Methods Participants Interventions Outcomes Results Outcomes/
Conclusion
Vad et al (169)
A prospective
study randomized
by patient choice
from the private
practice of a single
physician.
Patients with leg pain, old-
er than 18 years, had been
symptomatic longer than
6 weeks, had undergone
a lumbar spine magnetic
resonance imaging scan
documenting herniated
nucleus pulposus or mani-
fested clinical signs such
as radicular pain and sen-
sory or xed motor de-
cits consistent with lum-
bar radiculopathy.
Experimental group: transforam-
inal epidural steroid injection.
1.5 mL each of betamethasone
acetate, 9 mg and 2% preserva-
tive-free Xylocaine per level.
Control group: trigger point in-
jections.
All patients received a self-di-
rected home lumbar stabiliza-
tion program consisting of four
simple exercises emphasizing
hip and hamstring exibility and
abdominal and lumbar paraspi-
nal strengthening.
Timing: 3 weeks, 6
weeks, 3 months,
6 months, and 12
months.
Outcome mea-
sures:
Roland-Morris
score, visual nu-
meric score, nger-
to-oor distance,
patient satisfaction
score.
Fluoroscopically guided
transforaminal epidural
steroid injections yielded
better results compared
to saline trigger point in-
jections.
The group receiving trans-
foraminal epidural steroid
injections had a success
rate of 84%, as compared
with the 48% for the group
receiving trigger point in-
jections.
Positive
short-term
and long-
term relief
Lutz et al (168)
A prospective case
series.
69 patients with lumbar
herniated nucleus pulpo-
sus and radiculopathy. 69
patients were recruited.
Every patient in the case
series had documented
magnetic resonance imag-
ing ndings that showed
disc herniation with nerve
root compression.
Transforaminal epidural steroid
injections with 1.5 cc of 2% Xy-
locaine and 9 mg of betametha-
sone acetate.
Timing: 28 to 144
weeks
Outcome mea-
sures: At least
±50% reduction in
pre-injection and
post-injection visu-
al numerical pain
scores.
A successful outcome
was reported by 52 of the
69 patients (75.4%) at
an average follow-up of
80 weeks (range 28-144
weeks).
Positive
short-term
and long-
term relief
Bush and Hillier
(124)
Prospective evalu-
ation of cervical
interlaminar and
transforaminal
epidural injections
68 patients with neck
pain and cervical
radiculopathy.
Following the rst blind cervical
epidural injection, if a signicant
improvement was not seen, a
repeat injection was performed
trans foraminally with uorosco-
py guidance within 1 month.
A third injection was also per-
formed if needed in the same
manner as the second injection.
Timing: 1 month to
1 year
Outcome mea-
sures: Pain relief
93% of the patients were
reported to have good pain
relief lasting for 7 months.
Positive
short-term
and long-
term relief
Weiner and Fraser
(183)
A retrospective
evaluation
30 patients with lateral
foraminal or extraforami-
nal herniation of a lumbar
disc were evaluated with
foraminal injection of local
anesthetic and steroids
for radiculopathy
Transforaminal injection of 2 mL
of 1% lidocaine combined with
11.4 mg of injectable betameth-
asone.
Timing: 1 to 10
years
Outcome mea-
sures:
Pain scale:
Use of analgesics,
work status, recre-
ational activities.
22 had lasting relief of
their symptoms.
14 had no pain allowing
them to participate freely
in their usual activities.
Of the 17 patients at work,
13 had returned to the
same job.
Positive
short-term
and long-
term relief
Manchikanti et al
(105)
Compared the 3
routes of epidural
steroid injections
in the manage-
ment of low back
in retrospective
manner
225 patients randomly de-
rived from a total sample
of 624 patients suffering
with low back pain from
a total of 972 patients re-
ferred for pain manage-
ment were evaluated.
Group I: interlaminar epidurals
with a midline approach without
uoroscopy.
Group II: caudal epidurals un-
der uoroscopy.
Group III: transforaminal epidu-
ral steroid injections.
Timing: 1, 3, 6, 12
months
Outcome mea-
sures: Pain relief
Group III reported +50%
relief per procedure of
7.69 + 1.20 weeks, which
was superior to blind inter-
laminar epidurals.
Positive
short-term
and long-
term relief
Rosenberg et al
(186)
Retrospective
evaluation
92 patients with radicu-
lopathic back pain due
to spinal stenosis, herni-
ated discs, spondylolis-
thesis, and degenerative
discs.
Group I: Previous back surgery
(16%)
Group II: Discogenic abnormali-
ties: herniations, bulges or de-
generation (42%)
Group III: spinal stenosis (32%)
Group IV: those without MRI
(11%)
Timing: 2, 6 and
12 months
Outcome mea-
sures:
Pain relief
The pain scores for all pa-
tients improved signi-
cantly at all three points.
Greater than 50% im-
provement after one year
was seen in 23% of Group
I; 59% in Group II; 35%
in Group III and 67% in
Group IV.
Positive
short-term
and long-
term relief
Wang et al (187)
Retrospective
evaluation
69 patients with lumbar
herniated discs
All patients were treated with 1-
6 epidural steroid injections
Timing: NA
Outcome mea-
sures: Pain relief
Avoidance of sur-
geon
77% of patients had sig-
nicant improvement and
refused surgery
Positive
short-term
and long-
term relief
Table 8. Details and results of non-randomized trials of transforaminal epidural injections

Boswell et al • A Systematic Review of Epidural Steroids328
Pain Physician Vol. 6, No. 3, 2003
Boswell et al • A Systematic Review of Epidural Steroids 329
Pain Physician Vol. 6, No. 3, 2003
(183), Rosenberg et al (186), Wang et al
(187) and Manchikanti et al (105) met
inclusion criteria. All retrospective eval-
uations showed positive short-term and
long-term relief.
Complications and Side Effects
The most common and worrisome
complications and side effects of caudal,
interlaminar, and transforaminal epidur-
al injections are of two types: those relat-
ed to the needle placement and those re-
lated to drug administration. Complica-
tions include dural puncture, spinal cord
trauma, infection, hematoma formation,
abscess formation, subdural injection, in-
tracranial injection, epidural lipomatosis,
pneumothorax, nerve damage, headache,
death, brain damage, increased intra-
cranial pressure, intravascular injection,
vascular injury, cerebral vascular or pul-
monary embolus, and effects of steroids
(188-239). No major complications or
side effects were reported in the trials pre-
sented in the review.
DISCUSSION
This systematic review evaluated the
effectiveness of epidural injections in pa-
tients with chronic spinal pain. The evi-
dence was evaluated for 3 types of epidu-
rals separately.
For the transforaminal epidural in-
jections, three (120, 162, 164) of the 7
randomized trials (120, 162-167), showed
positive short-term and long-term ef-
fectiveness for lumbar nerve root pain.
Three prospective evaluations (124, 168,
169) showed positive short and long-term
results. Four retrospective evaluations
(105, 183, 186, 187) were included which
showed positive results overall. Multiple
randomized and non-randomized tri-
als of transforaminal epidural injections
provided strong evidence for short-term
and long-term relief in managing lum-
bar nerve root pain. Their effectiveness
in post lumbar laminectomy syndrome
and disc extrusions is inconclusive. There
is no published evidence of effectiveness
of transforaminal epidural injections in
chronic neck or chronic low back pain,
post cervical or laminectomy syndrome,
and cervical or thoracic radicular pain.
The combined overall evidence of
caudal epidural steroid injections, based
on randomized trials and nonrandomized
trials (prospective and retrospective trials)
is strong for short-term relief and moder-
ate for long-term relief with two (92, 93)
of three (92-94) randomized trials, and
4 of 4 non-randomized trials (102-104-
106) demonstrating positive results in ra-
dicular pain. However, the evidence for
chronic low back pain and spinal stenosis
appears to be limited as there are no ran-
domized or double-blind trials evaluating
this effect. Non-randomized trials (100,
101, 105, 107) all showed positive results
in chronic low back pain after the facet
joint pain was excluded (100, 101, 105),
and also in spinal stenosis (107).
For interlaminar epidural injections,
of the 8 randomized trials included, 6 tri-
als (108, 111, 115-117, 122) showed posi-
tive evidence for short-term relief, and 3
of 8 (111, 117, 122) showed positive evi-
dence for long-term relief. The overall ef-
fectiveness of interlaminar epidural ste-
roid injections in managing chronic spi-
nal pain is moderate for short-term relief
and limited for long-term relief in man-
aging lumbar radicular pain. However,
there was no significant evidence based
on randomized trials of effectiveness of
interlaminar epidural steroids in manag-
ing cervical radicular pain. Further anal-
ysis combining one randomized trial, one
prospective trial and multiple retrospec-
tive evaluations (132-144), demonstrat-
ed moderate evidence for short-term,
and limited evidence for long-term re-
lief. The limited evidence for manage-
ment of chronic low back pain without
radiculopathy was based on all the retro-
spective studies.
The first systematic review of effec-
tiveness of epidural steroid injections was
performed by Kepes and Duncalf in 1985
(59). They concluded that the rationale
for epidural and systemic steroids was not
proven. However, in 1986 Benzon (60),
utilizing the same studies, concluded that
mechanical causes of low back pain, es-
pecially those accompanied by signs of
nerve root irritation, may respond to epi-
dural steroid injections. The difference in
the conclusion of Kepes and Duncalf (59)
and Benzon (60) may have been due to the
fact that Kepes and Duncalf (59) included
studies on systemic steroids whereas Ben-
zon (60) limited his analysis to studies on
epidural steroid injections only.
The debate concerning epidural ste-
roid injections is also illustrated by the
recommendations of the Australian Na-
tional Health and Medical Research
Council Advisory Committee on epidur-
al steroid injections (57). In this report,
Bogduk et al (57) extensively studied cau-
dal, interlaminar, and transforaminal epi-
dural injections, including all the litera-
ture available at the time, and concluded
that the balance of the published evidence
supports the therapeutic use of caudal
epidurals. They also concluded that the
results of lumbar interlaminar epidural
steroids strongly refute the utility of epi-
dural steroids in acute sciatica. Bogduk
(61) updated his recommendations in
1999, recommending against epidural ste-
roids by the lumbar route because effec-
tive treatment required too high a number
for successful treatment, but supporting
the potential usefulness of transforami-
nal steroids for disc prolapse. In 1995,
Koes et al (62) reviewed 12 trials of lum-
bar and caudal epidural steroid injections
and reported positive results from only six
studies. However, review of their analysis
showed that there were 5 studies for cau-
dal epidural steroid injections and 7 stud-
ies for lumbar epidural steroid injections.
Four of the five studies involving caudal
epidural steroid injections were positive,
whereas 5 of 7 studies were negative for
lumbar epidural steroid injections. Koes
et al (63) updated their review of epidu-
ral steroid injections for low back pain
and sciatica, including three more stud-
ies with a total of 15 trials which met the
inclusion criteria. In this study, they con-
cluded that of the 15 trials, eight reported
positive results of epidural steroid injec-
tions. Both reviews mostly reflected the
quality of studies, rather than any mean-
ingful conclusion.
Nelemans et al’s (66) Cochrane re-
view of injection therapy for subacute
and chronic benign low back pain includ-
ed 21 randomized trials. Of these, 9 were
of epidural steroids. They failed to sepa-
rate caudal from interlaminar epidural
injections, but still concluded that con-
vincing evidence is lacking regarding the
effects of injection therapy on low back
pain. Rozenberg et al (70), in a systematic
review, identified 13 trials of epidural ste-
roid therapy. They concluded that 5 tri-
als demonstrated greater pain relief with-
in the first month in the steroid group as
compared to the control group. Eight tri-
als found no measurable benefits. They
noticed many obstacles for meaningful
comparison of cross studies, which in-
cluded differences in the patient popula-
tions, steroid used, volume injected, and
number of injections. These authors
were unable to determine whether epidu-
ral steroids are effective in common low

Boswell et al • A Systematic Review of Epidural Steroids328
Pain Physician Vol. 6, No. 3, 2003
Boswell et al • A Systematic Review of Epidural Steroids 329
Pain Physician Vol. 6, No. 3, 2003
back pain and sciatica based on their re-
view. Rozenburg et al (70) concluded that
3 of the top 5 rated studies did not dem-
onstrate significant benefit of the steroid
over the non-steroid group. Hopayiank
and Mugford (71) expressed frustration
over the conflicting conclusions from two
systematic reviews of epidural steroid in-
jections for sciatica and asked which evi-
dence should general practitioners heed?
Multiple previous reviews have criticized
the studies evaluating the effectiveness
of epidural injections. Criticisms ranged
from methodology, small size of the study
populations, and other limitations, in-
cluding long-term follow-up and out-
come parameters. Many of these deficien-
cies were noted in our review also, in spite
of the fact that we have included non-ran-
domized trials.
With respect to complications and
side effects, only transient minor com-
plaints were reported in the trials present-
ed in this review. However, potential com-
plications also have been described. Spi-
nal cord trauma and spinal cord or epidu-
ral hematoma formation are catastroph-
ic complications. One of the suggestions
has been to perform interventional proce-
dures only in an awake patient and in the
cervical spine by limiting the midline in-
jection to be performed only at C7/T1 ex-
cept in rare circumstances. However, it
has also been reported that even an awake
patient may not be able to detect spinal
cord puncture (241). Thus, the recom-
mendation to limit the midline injection
only at C7/T1 is based neither on con-
sistent clinical nor anatomical evidence.
Three cases of paraplegia were reported
after lumbosacral nerve root block in post
lumbar laminectomy patients (229). In
each patient, paraplegia was reported sud-
denly. In each patient after injection of a
steroid solution, post procedure magnet-
ic resonance imaging (MRI) revealed spi-
nal cord edema in the low thoracic region.
The authors postulated that in these pa-
tients, the spinal needle penetrated or in-
jured an abnormally low dominant radic-
ulomedullary artery, a recognized ana-
tomical variant. This vessel, also known
as artery of Adamkiewicz, in 85% of indi-
viduals arises between T9 and L2, usually
from the left, but in a minority of people,
may arise from the lower lumbar spine
and rarely even from as low as S1 (229).
Others also have reported similar compli-
cations (234-236). Side effects related to
the administration of steroids are gener-
ally attributed either to the chemistry or
to the pharmacology of the steroids. The
major theoretical complications of corti-
costeroid administration include suppres-
sion of pituitary-adrenal access, hyper-
corticism, Cushing’s syndrome, osteopo-
rosis, avascular necrosis of bone, steroid
myopathy, epidural lipomatosis, weight
gain, fluid retention, and hyperglycemia.
One study (228) showed no significant
difference in patients undergoing various
types of interventional techniques with or
without steroids. Further, it has also been
shown that the most commonly used ste-
roids in the epidural steroids in the Unit-
ed States, methylprednisolone acetate, tri-
amcinolone acetonide, and betametha-
sone acetate, and phosphate mixture have
all been shown to be safe at epidural ther-
apeutic doses in both clinical and experi-
mental studies (242-250).
CONCLUSION
This systematic review, which includ-
ed not only randomized trials, but also all
available non-randomized trials, showed
variable effectiveness of epidural injections.
Strong evidence was provided for transfo-
raminal epidural steroid injections in man-
aging lumbar nerve root pain. Moderate
evidence was provided for caudal epidural
steroid injections in managing lumbar ra-
dicular pain. Evidence for other conditions
was either limited or inconclusive.
REFERENCES
1. Hellsing A, Bryngelsson I. Predictors of
musculoskeletal pain in men. A twenty-
year follow-up from examination at enlist-
ment. Spine 2000; 25:3080-3086.
2. Lawrence RC, Helmick CG, Arnett FC. Es-
timates of the prevalence of arthritis and
selected musculoskeletal disorders in the
United States. Arthritis Rheum 1998; 41:
778-799.
3. Bressler HB, Keyes WJ, Rochon PA et al.
The prevalence of low back pain in the el-
derly. A systemic review of the literature.
Spine 1999; 24:1813-1819.
4. Cassidy D, Carroll L, Cotê P: The Saskatch-
ewan Health and Back Pain Survey. The
prevalence of low back pain and related
disability in Saskatchewan Adults. Spine
1998; 23:1860-1867.
5. Côté DC, Cassidy JD, Carroll L. The Sas-
katchewan Health and Back Pain Survey.
The prevalence of neck pain and related
disability in Saskatchewan adults. Spine
1998; 23:1689-1698.
6. Elliott AM, Smith BH, Hannaford PC et al.
The course of chronic pain in the commu-
nity: Results of a 4-year follow-up study.
Pain 2002; 99:299-307.
7. van den Hoogen HJ, Koes BW, Deville W et
al. The prognosis of low back pain in gen-
eral practice. Spine 1997; 22:1515-1521.
8. Croft PR, Papageorgiou AC, Thomas E et
al. Short-term physical risk factors for
new episodes of low back pain. Prospec-
tive evidence from the South Manchester
Back Pain Study. Spine 1999; 24:1556-
1561.
9. Carey TS, Garrett JM, Jackman A et al. Re-
currence and care seeking after acute
back pain. Results of a long-term follow-
up study. Medical Care 1999; 37:157-164.
10. Miedema HS, Chorus AM, Wevers CW,
et al. Chronicity of back problems dur-
ing working life. Spine 1998; 23:2021-
2029.
11. Thomas E, Silman AJ, Croft PR et al. Pre-
dicting who develops chronic low back
pain in primary care. A prospective study.
Brit Med J 1999; 318:1662-1667.
12. Wahlgren DR, Atkinson JH, Epping-Jor-
dan JE et al. One-year follow up of first
onset low back pain. Pain 1997; 73:213-
221.
13. Schiottz-Christensen B, Nielsen GL, Han-
sen VK et al. Long-term prognosis of acute
low back pain in patients seen in general
practice: A 1-year prospective follow-up
Author Affiliation:
Mark V. Boswell, MD, PhD
Chief Division of Pain Medicine
Department of Anesthesiology
Case Western Reserve University
School of Medicine and University
Hospitals of Cleveland
11100 Euclid Avenue
Cleveland, Ohio, 44106
E-mail: [email protected]
Hans C. Hansen, MD
Medical Director
The Pain Relief Centers, PA
3451 Greystone Place SW
Conover, North Carolina 28613
E-mail: [email protected]
Andrea M. Trescot, MD
Medical Director
The Pain Center
1895 Kingsley Ave. Suite 903
Orange Park, Florida 32073
E-mail: [email protected]
Joshua A. Hirsch, MD
Harvard School of Medicine
Department of Interventional
Radiology
Massachusetts General Hospital
55 Blossom St. Gray 289
Boston, Massachusetts 02114
E-mail: [email protected]

Boswell et al • A Systematic Review of Epidural Steroids330
Pain Physician Vol. 6, No. 3, 2003
Boswell et al • A Systematic Review of Epidural Steroids 331
Pain Physician Vol. 6, No. 3, 2003
study. Fam Pract 1999; 16:223-232.
14. Ferguson SA, Marras WS, Gupta P. Lon-
gitudinal quantitative measures of the
natural course of low back pain recovery.
Spine 2000; 25:1950-1956.
15. Vingård E, Mortimer M, Wiktorin C et al.
Seeking care for low back pain in the
general population: A two-year follow-up
study: Results from the MUSIC-Norrtalje
Study. Spine 2002; 27:2159-2165.
16. Hildingsson C, Toolanen G. Outcome after
soft-tissue injury of the cervical spine: A
prospective study of 93 car accident vic-
tims. Acta Orthop Scand 1990; 61:357-
359.
17. Hodgson S, Grundy M. Whiplash injuries:
Their long-term prognosis and its relation-
ship to compensation. Neuro Orthopedics
1989; 7:88-91.
18. Paul R, Haydon RC, Cheng H et al. Poten-
tial use of sox9 gene therapy for interver-
tebral degenerative disc disease. Spine
2003; 28:755-763.
19. CDC. Prevalence of disabilities and asso-
ciated health conditions among adults –
United States, 1999. MMWR 2001; 50:120-
125.
20. Leigh JP, Markowitz S, Fahs M et al. Oc-
cupational injury and illness in the Unit-
ed States. Estimates of costs, morbidity,
and mortality. Arch Intern Med 1997; 157:
1557-1568.
21. Freedman VA, Martin LG, Schoeni RF. Re-
cent trends in disability and functioning
among older adults in the united states.
JAMA 2002; 288:3137-3146.
22. Wheeler AH, Murrey DB. Chronic lumbar
spine and radicular pain: Pathophysiolo-
gy and treatment. Curr Pain Headache Rep
2002; 6:97-105.
23. Antoniou J, Steffen T, Nelson F et al. The
human lumbar intervertebral disc: Evi-
dence for changes in the biosynthesis
and denaturation of the extracellular ma-
trix with growth, maturation, ageing, and
degeneration. J Clin Invest 1996; 98:996-
1003.
24. Buckwalter JA. Aging and degeneration of
the human intervertebral disc. Spine 1995;
20:1307-1314.
25. Guiot BH, Fessler RG. Molecular biology of
degenerative disc disease. Neurosurgery
2000; 47:1034-1040.
26. Mixter WJ, Ayers JB. Herniation or rupture
of the intervertebral disc into the spinal ca-
nal. N Engl J Med 1935; 213:385-395.
27. Mixter WJ, Barr JS. Rupture of the interver-
tebral disc with involvement of the spinal
canal. N Eng J Med 1934; 211:210-215.
28. Luoma K, Riihimaki H, Luukkonen R et al.
Low back pain in relation to lumbar disc
degeneration. Spine 2000; 25: 487-492.
29. Paajanen H, Erkintalo M, Parkkola R et al.
Age-dependent correlation of low back
pain and lumbar disc regeneration. Arch
Orthop Trauma Surg 1997; 116:106-107.
30. Salminen JJ, Erkintalo MO, Pentti J et al.
Recurrent low back pain and early disc de-
generation in the young. Spine 1999; 24:
1316-1321.
31. Olmarker K, Holm S, Rosenqvist AL et al.
Experimental nerve root compression.
Presentation of a model for acute, graded
compression of the porcine cauda equina,
with analysis of neural and vascular anat-
omy. Spine 1992; 16:61-69.
32. McCarron RF, Wimpee MW, Hudkins PG
et al. The inammatory effects of nucle-
us pulposus: A possible element in the
pathogenesis of low back pain. Spine
1987; 12:760-764.
33. Olmarker K, Blomquist J, Stromberg J et
al. Inammatogenic properties of nucleus
pulposus. Spine 1995; 20:665-669.
34. Saal JS, Franson RC, Dobrow R et al. High
levels of inammatory phospholipase A2
activity in lumbar disc herniations. Spine
1990; 15:674-678.
35. Chaoyang C, Cavanaugh JM, Ozaktay AC et
al. Effects of phospholipase A
2
on lumbar
nerve root structure and function. Spine
1997; 22:1057-1064.
36. Gertzbein SD. Degenerative disc disease
of the lumbar spine: Immunological impli-
cations. Clin Orthop Rel Res 1977; 190:68-
71.
37. Marshall LL, Trethewie ER, Curtain CC.
Chemical radiculitis: A clinical, physio-
logical, and immunological study. Clin Or-
thop Rel Res 1977; 190:61-67.
38. Miyamoto H, Saura R, Doita M et al. The
role of cyclooxygenase-2 in lumbar disc
herniation. Spine 2002; 27:2477-2483.
39. Kang JD, Georgescu HI, McIntyre-Larkin
L et al. Herniated lumbar intervertebral
discs spontaneously produce matrix me-
talloproteinases, nitric oxide, interleukin-
6, and prostaglandin E
2
. Spine 1996; 21:
271-277.
40. Takahashi H, Suguro T, Okazim Y et al. In-
ammatory cytokines in the herniated disc
of the lumbar spine. Spine 1996; 21:218-
221.
41. Cavanaugh JM. Neural mechanisms of
lumbar pain. Spine 1995; 20:1804-1809.
42. Weinstein JN. The role of neurogenic and
non-neurogenic mediators as they relate
to pain and the development of osteoar-
thritis. A clinical review. Spine 1992; 10:
S356-S361.
43. Karppinen J, Korhonen T, Malmivaara A et
al. Tumor necrosis factor- monoclonal an-
tibody, infliximab, used to manage severe
sciatica. Spine 2003; 28:751-754.
44. Igarashi T, Kikuchi S, Shubayev V et al.
Volvo Award Winner in Basic Science Stud-
ies. Exogenous tumor necrosis facto-al-
pha mimics nucleus pulposus-induced
neuropathology: Molecular, histologic,
and behavioral comparisons in rats. Spine
2000; 25:2975-2980.
45. Crock HV. Isolated lumbar disc resorption
as a cause of nerve root canal stenosis.
Clin Orthop 1976; 115:109-115.
46. Olmarker K, Rydevik B, Holm S. Edema for-
mation in spinal nerve roots induced by ex-
perimental, graded compression: An exper-
imental study on the pig cauda equina with
special reference to differences in effects
between rapid and slow onset of compres-
sion. Spine 1989; 14:569-573.
47. Law JD, Lehman RAW, Kirch WM. Reoper-
ation after lumbar intervertebral disc sur-
gery. J Neurosurg 1978; 48:259-263.
48. Fritsch EW, Heisel J, Rupp S. The failed
back surgery syndrome. Reasons, intraop-
erative ndings, and long-term results: A
report of 182 operative treatments. Spine
1996; 21:626-633.
49. Ross JS, Robertson JT, Frederickson RC et
al. Association between peridural scar
and recurrent radicular pain after lumbar
discectomy: Magnetic resonance evalua-
tion. Neurosurgery 1996; 38:855-863.
50. Nachemson AL. Failed back surgery syn-
drome is syndrome of failed back sur-
geons. Pain Clinic 1999; 11:271-284.
51. Spencer DL, Irwin GS, Miller JA. Anatomy
and signicance of xation of the lumbo-
sacral nerve roots in sciatica. Spine 1983;
8:672-679.
52. Amundsen T, Weber H, Nordal H et al.
Lumbar spinal stenosis: Conservative or
surgical management? Spine 2000; 25:
1424-1436.
53. Aota Y, Onari K, An HS et al. Dorsal root
ganglia morphologic features in patients
with herniation of the nucleus pulposus.
Assessment using magnetic resonance
myelography and clinical correlation.
Spine 2001; 26:2125-2132.
54. Rydevik BL, Myers RR, Powel HC. Pressure
increase in the dorsal root ganglion follow-
ing mechanical compression: Closed com-
partment syndrome in nerve roots. Spine
1989; 14:574-576.
55. Weinstein J. Mechanism of spinal pain:
The dorsal root ganglion and its role as
a pain mediator of low-back pain. Spine
1986; 11:999-1001.
56. Manchikanti L, Staats P, Singh V et al. Evi-
dence-based practice guidelines for inter-
ventional techniques in the management
of chronic spinal pain. Pain Physician
2003; 6:3-80.
57. Bogduk N, Christophidis N, Cherry D et al.
Epidural use of steroids in the manage-
ment of back pain. Report of working par-
ty on epidural use of steroids in the man-
agement of back pain. National Health
and Medical Research Council. Canber-
ra, Commonwealth of Australia, 1994, pp
1-76.
58. Manchikanti L, Singh V, Kloth D et al. Inter-
ventional techniques in the management
of chronic pain: Part 2.0. Pain Physician
2001; 4:24-98.
59. Kepes ER, Duncalf D. Treatment of back-
ache with spinal injections of local anes-
thetics, spinal and systemic steroids. Pain
1985; 22:33-47.
60. Benzon HT. Epidural steroid injections for
low back pain and lumbosacral radiculog-
raphy. Pain 1986; 24:277.

Boswell et al • A Systematic Review of Epidural Steroids330
Pain Physician Vol. 6, No. 3, 2003
Boswell et al • A Systematic Review of Epidural Steroids 331
Pain Physician Vol. 6, No. 3, 2003
61. Bogduk N. Epidural steroids for low back
pain and sciatica. Pain Digest 1999; 9:
226-7.
62. Koes BW, Scholten RJ, Mens JM et al. E-
cacy of epidural steroid injections for low
back pain and sciatica: A systematic re-
view of randomized clinical trials. Pain
1995; 63:279-288.
63. Koes BW, Scholten R, Mens JM et al. Epi-
dural steroid injections for low back pain
and sciatica. An updated systematic re-
view of randomized clinical trials. Pain Di-
gest 1999; 9:241-247.
64. Watts RW, Silagy CA. A meta-analysis on
the ecacy of epidural corticosteroids in
the treatment of sciatica. Anaesth Intens
Care 1995; 23:564-569.
65. van Tulder MW, Koes BW, Bouter LM. Con-
servative treatment of acute and chronic
nonspecic low back pain. A systematic
review of randomized controlled trials of
the most common interventions. Spine
1997; 22:2128-2156.
66. Nelemans PJ, deBie RA, deVet HC et al. In-
jection therapy for subacute and chronic
benign low back pain. Spine 2001; 26:501-
515.
67. Manchikanti L, Jasper J, Singh V. Letter to
the editor. Spine 2001; 26:2641-2642.
68. McQuay HJ, Moore RA. Epidural cortico-
steroids for sciatica. An Evidence-Based
Resource for Pain Relief. Oxford Univer-
sity Press, New York, 1998, pp 216-218.
69. Vroomen PC, de Krom MC, Slofstra PD et
al. Conservative treatment of sciatica: A
systematic reivew. J Spinal Disord 2000;
13:463-469.
70. Rozenberg S, Dubourg G, Khalifa P et al.
Ecacy of epidural steroids in low back
pain and sciatica: A critical appraisal by a
French task force of randomized trials. Re-
vue du Rhumatisme 1999; 66:79-85.
71. Hopayiank K, Mugford M. Conicting con-
clusions from two systematic reviews of
epidural steroid injections for sciatica:
Which evidence should general practitio-
ners heed? Br J Gen Pract 1999; 49:57-60.
72. Bogduk N, Govind J (eds). Epidural ste-
roids. In Medical Management of Acute
Lumbar Radicular Pain. 1
st
ed. University
of Newcastle, Newcastle Bone and Joint In-
stitute, Australia, 1999, pp 71-80.
73. Bogduk N (ed). Steroid injections. In
Medical Management of Acute Cervical
Radicular Pain. 1
st
ed. University of New-
castle, Newcastle Bone and Joint Institute,
Australia, 1999. pp 85-90.
74. Bogduk N, McGuirk B (eds). Monothera-
py. In Medical Management of Acute and
Chronic Low Back Pain. Vol 13. Elsevier
Science, Netherlands, 2002, pp 143-162.
75. van Tulder MW, Goossens M, Waddell G et
al. Conservative treatment of chronic low
back pain. In Neck and Back Pain. The
Scientific Evidence of Causes, Diagno-
sis, and Treatment. Lippincott Williams &
Wilkins, Philadelphia, pp 271-304.
76. Fox AJ, Melzack R. Transcutaneous electri-
cal stimulation to acupuncture. Compar-
ison of treatment of low back pain. Pain
1976; 2:141-148.
77. Byrod G, Otani K, Brisby H et al. Methyl-
prednisolone reduces the early vascular
permeability increase in spinal nerve roots
induced by epidural nucleus pulposus ap-
plication. J Orthop Res 2000; 18:983-987.
78. Fowler RJ, Blackwell GJ. Anti-inammato-
ry steroid induced biosynthesis of a phos-
pholipase A
2
inhibitor which prevents
prostaglandin generation. Nature 1979;
278:456-459.
79. Devor M, Govrin-Lippmann R, Raber P.
Corticosteroids suppress ectopic neural
discharges originating in experimental
neuromas. Pain 1985; 22:127-137.
80. Johansson A, Hao J, Sjolund B. Local corti-
costeroid application blocks transmission
in normal nociceptor C-bers. Acta Anaes-
thesiol Scand 1990; 34:335-338.
81. Olmarker K, Byrod G, Cornefjord M et al.
Effects of methylprednisolone on nucleus
pulposus-induced nerve root injury. Spine
1994; 19:1803-1808.
82. Hua SY, Chen YZ. Membrane receptor-me-
diated electrophysiological effects of glu-
cocorticoid on mammalian neurons. En-
docrinology 1989; 124:687-691.
83. Hayashi N, Weinstein JN, Meller ST et al.
The effect of epidural injection of beta-
methasone or bupivacaine in a rat model
of lumbar radiculopathy. Spine 1998; 23:
877-885.
84. Lee HM, Weinstein JN, Meller ST et al.
The role of steroids and their effects on
phospholipase A
2
. An animal model of
radiculopathy. Spine 1998; 23:1191-1196.
85. Minamide A, Tamaki T, Hashizume H et al.
Effects of steroids and lipopolysaccharide
on spontaneous resorption of herniated
intervertebral discs. An experience study
in the rabbit. Spine 1998; 23:870-876.
86. Kingery WS, Castellote JM, Maze M. Meth-
ylprednisolone prevents the development
of autotomy and neuropathic edema in
rats, but has no effect on nociceptive
thresholds. Pain 1999; 80:555-566.
87. Johansson A, Bennett GJ. Effect of local
methylprednisolone on pain in a nerve
injury model. A pilot study. Reg Anesth
1997; 22:59-65.
88. Merskey H, Thompson EN. Nerve blocks
and cognitive therapy: A benecial failure.
Pain Res Manage 2002; 7:175-176.
89. Li YM, Wingrove DE, Too HP et al. Local an-
esthetics inhibit substance P binding and
evoked increases in intracellular Ca
2+
.
Anesthesiology 1995:82:166-173.
90. Fink BR, Cairns AM. Differential use-de-
pendent (frequency-dependent) effects in
single mammalian axons: Data and clinical
considerations. Anesthesiology 1987; 67:
477-484.
91. Systems to rate the strength of scientic
evidence. Evidence Report/Technology
Assessment No. 47 University of North
Carolina: Agency for Healthcare Research
and Quality. AHRQ Publication No. 02-
E016; April 2002.
92. Breivik H, Hesla PE, Molnar I et al. Treat-
ment of chronic low back pain and sciat-
ica. Comparison of caudal epidural injec-
tions of bupivacaine and methylpredniso-
lone with bupivacaine followed by saline.
In Bonica JJ, Albe-Fesard D (eds). Advanc-
es in pain research and therapy. Vol. 1., Ra-
ven Press, New York, 1976, pp 927-932.
93. Bush K, Hillier S. A controlled study of
caudal epidural injections of triamcino-
lone plus procaine for the management of
intractable sciatica. Spine 1991; 16:572-
575.
94. Mathews JA, Mills SB, Jenkins VM et al.
Back pain and sciatica: Controlled trials
of manipulation, traction, sclerosant and
epidural injections. Brit J Rheumatol 1987;
26:416-423.
95. Beliveau P. A comparison between epidur-
al anesthesia with and without corticoste-
roids in the treatment of sciatica. Rheum
Phys Med 1971; 11:40-43.
96. Czarski Z. Leczenie rwy kulszowej
wstrzykiwaniem hydrokortyzonu inowo-
kainy do rozworu kryzowego. Przeglad
Kekarski 1965; 21:511-513.
97. Helsa PE, Breivik H. Epidural analgesia
and epidural steroid injection for treat-
ment of chronic low back pain and sciati-
ca. Tidsskr Nor Laegeforen 1979; 99:936-
939.
98. Revel M, Auleley GR, Alaoui S et al. Force-
ful epidural injections for the treatment
of lumbosciatic pain with post-operative
lumbar spinal brosis. Rev Rhum Engl Ed
1996; 63:270-277.
99. Meadeb J, Rozenberg S, Duquesnoy B et
al. Forceful sacrococcygeal injections in
the treatment of postdiscectomy sciatica.
A controlled study versus glucocorticoid
injections. Joint Bone Spine 2001; 68:43-
49.
100. Manchikanti L, Pampati V, Rivera JJ et al.
Caudal epidural injections with Sarapin
steroids in chronic low back pain. Pain
Physician 2001; 4:322-335.
101. Manchikanti L., Singh V, Rivera J et al. Ef-
fectiveness of caudal epidural injections
in discogram positive and negative chron-
ic low back pain. Pain Physician 2002; 5:
18-29.
102. Yates DW. A comparison of the types of
epidural injection commonly used in the
treatment of low back pain and sciatica.
Rheum Rehab 1978; 17:181-186.
103. Waldman SD. The caudal epidural admin-
istration of steroids in combination with
local anesthetics in the palliation of pain
secondary to radiographically document-
ed lumbar herniated disc: A prospective
outcome study with 6-months follow-up.
Pain Clinic 1998; 11:43-49.
104. Hauswirth R, Michot F. Caudal epidural in-
jection in the treatment of low back pain.
Ischweizerische Medizinische Wochen-
schrift 1982; 112:222-225.
105. Manchikanti L, Pakanati RR, Pampati V.
Comparison of three routes of epidural
steroid injections in low back pain. Pain

Boswell et al • A Systematic Review of Epidural Steroids332
Pain Physician Vol. 6, No. 3, 2003
Boswell et al • A Systematic Review of Epidural Steroids 333
Pain Physician Vol. 6, No. 3, 2003
Digest 1999; 9:277-285.
106. Goebert HW, Jallo SJ, Gardner WJ et al.
Painful radiculopathy treated with epidu-
ral injections of procaine and hydrocor-
tisone acetate: Results in 113 patients.
Anesth Analg 1961; 140:130-134.
107. Ciocon JO, Galindo-Clocon D, Amaranath
L et al. Caudal epidural blocks for elderly
patients with lumbar canal stenosis. J Am
Geriatr Soc 1994; 42:593-596.
108. Carette S, Leclaire R, Marcoux S et al. Epi-
dural corticosteroid injections for sciati-
ca due to herniated nucleus pulposus. N
Engl J Med 1997; 336:1634-1640.
109. Snoek W, Weber H, Jorgensen B. Double-
blind evaluation of extradural methylpred-
nisolone for herniated lumbar disc. Acta
Orthop Scand 1977; 48:635-641.
110. Cuckler JM, Bernini PA, Wiesel SW et al.
The use of epidural steroid in the treat-
ment of radicular pain. J Bone Joint Surg
1985; 67:63-66.
111. Dilke TF, Burry HC, Grahame R. Extradu-
ral corticosteroid injection in the manage-
ment of lumbar nerve root compression.
Br Med J 1973; 2:635-637.
112. Serrao JM, Marks RL, Morley SJ et al. In-
trathecal midazolam for the treatment of
chronic mechanical low back pain: A con-
trolled comparison with epidural steroid in
a pilot study. Pain 1992; 48:5-12.
113. Klenerman L, Greenwood R, Davenport
HT et al. Lumbar epidural injections in
the treatment of sciatica. Br J Rheumatol
1984; 23:35-38.
114. Rocco AG, Frank E, Kaul AF et al. Epidur-
al steroids, epidural morphine and epidur-
al steroids combined with morphine in the
treatment of post-laminectomy syndrome.
Pain 1989; 36:297-303.
115. Ridley MG, Kingsley GH, Gibson T et al.
Outpatient lumbar epidural corticosteroid
injection in the management of sciatica.
Br J Rheumatol 1988; 27:1003-1007.
116. Rogers P, Nash T, Schiller D et al. Epidur-
al steroids for sciatica. Pain Clinic 1992; 5:
67-72.
117. Castagnera L, Maurette P, Pointillart V et
al. Long-term results of cervical epidur-
al steroid injection with and without mor-
phine in chronic cervical radicular pain.
Pain 1994; 58:239-243.
118. Hernandez R, Lopez F. Assessment of pain
intensity in patients with diabetic poly-
neuropathy treated with peridural 2% li-
docaine methylprednisolone acetate vs
peridural 2% lidocaine. Anestesia en Mex-
ico 1999; 11:65-69.
119. Kikuchi A, Kotani N, Sato T et al. Compar-
ative therapeutic evaluation of intrathe-
cal versus epidural methylprednisolone
for long-term analgesia in patients with
intractable postherpetic neuralgia. Reg
Anesth Pain Med 1999; 24:287-293.
120. Kraemer J, Ludwig J, Bickert U et al. Lum-
bar epidural perineural injection: A new
technique. Eur Spine J 1997; 6:357-361.
121. Helliwell M, Robertson JC, Ellia RM. Out-
patient treatment of low back pain and sci-
atica by a single extradural corticosteroid
injection. Br J Clin Pract 1985; 39:228-31.
122. Stav A, Ovadia L, Sternberg A et al. Cer-
vical epidural steroid injection for cervi-
cobrachialgia. Acta Anaesthesiol Scand
1993; 37:562-566.
123. Buchner M, Zeifang F, Brocai DR et al. Epi-
dural corticosteroid injection in the con-
servative management of sciatica. Clin
Orth Rel Res 2000; 375:149-156.
124. Bush K, Hillier S. Outcome of cervical
radiculopathy treated with periradicular/
epidural corticosteroid injections: A pro-
spective study with independent clinical
review. Eur Spine J 1996; 5:319-325.
125. Rull BM, Miralles M, Aure S. Therapeutic
epidural inltrations in the lumbar nerve
roots. Revista de Ortopedia y Traumatolo-
gia 1996; 40:209-217.
126. Caglar S, Erdine S, Aldemir T. The results
of the epidural steroid injections in pa-
tients with radiculopathies due to lumbar
disc herniations. Fizik Tedavi Rehabilita-
syon Dergisi 1995; 19:186-190.
127. Rivest C, Katz JN, Ferrante FM et al. Effects
of epidural steroid injection on pain due to
lumbar spinal stenosis or herniated discs:
A prospective study. Arthritis Care Res
1998; 11:291-297.
128. Koning HM, Koning AJ, Bruinen TC et al.
The period of pain relief following a suc-
cessful epidural steroid injection for low
back pain. Pain Clinic 2002; 13:331-338.
129. Fukusaki M, Kobayashi I, Hara T et al.
Symptoms of spinal stenosis do not im-
prove after epidural steroid injection. Clin
J Pain 1998; 14:148-151.
130. Andersen KH, Mosdal C. Epidural appli-
cation of corticosteroids in low-back pain
and sciatica. Acta Neurochir 1987; 87:52-
53.
131. Wareld CA, Crews DA. Epidural steroid
injection as a predictor of surgical out-
come. Surg Gyn Obstet 1987; 164:457-
458.
132. Stav A, Ovadia L, Landau M et al. Epidural
steroid injection in the treatment of lum-
bar and cervical pain syndromes. A pre-
liminary retrospective comparison. Pain
Clinic 1991; 4:95-112.
134. Shulman M. Treatment of neck pain with
cervical epidural steroid injection. Reg
Anesth 1986; 11:92-94.
135. Catchlove RFH, Braha R. The use of cervi-
cal epidural nerve blocks in the manage-
ment of chronic head and neck pain. Can
Anaesth Soc J 1984; 31:188-191.
136. Berman AT, Garbarinbo JL Jr., Fisher SM et
al. The effects of epidural injection of lo-
cal anesthetics and corticosteroids in pa-
tients with lumbosciatic pain. Clin Orthop
1984; 188:144-151.
137. Purkis IE. Cervical epidural steroids. Pain
Clinic 1986; 1:3-7.
138. Rowlingson JC, Kirschenbaum LP. Epidural
analgesic techniques in the management
of cervical pain. Anesth Analg 1986; 65:
938-942.
139. Wareld CA, Biber MP, Crews DA et al. Epi-
dural steroid injection as a treatment for
cervical radiculitis. Clin J Pain 1988; 4:201-
204.
140. Cicala RS, Thoni K, Angel JJ. Long-term
results of cervical epidural steroid injec-
tions. Clin J Pain 1989; 5:143-145.
141. Pawl RP, Anderson W, Shulman M. Effect
of epidural steroids in the cervical and
lumbar region on surgical intervention for
discogenic spondylosis. Clin J Pain 1985;
1:181-185.
142. Ferrante FM, Wilson SP, Iacobo C et al.
Clinical classication as a predictor of
therapeutic outcome after cervical epidu-
ral steroid injection. Spine 1993; 18:730-
736.
143. Klein RG, Vaccaro AR, Cwik J et al. Eca-
cy of cervical epidural steroids in the treat-
ment of cervical spine disorders. Am J An-
esthesiol 2000; 9:547-552.
144. Ozyalcin S, Yucel A, Erdine S. Epidural ste-
roid injection in the treatment of cervical
pain syndromes: A retrospective follow up
study. Angri Dergisi 1996; 8:9-14.
145. Hickey RF. Outpatient epidural steroid in-
jections for low back pain and lumbosacral
radiculopathy. NZ Med J 1987; 100:54-59.
146. Heyse-Moore GH. A rational approach to
the use of epidural medication in the treat-
ment of sciatic pain. Acta Orthop Scand
1978; 49:366-370.
147. Harley C. Extradural corticosteroid inltra-
tion. A follow-up study of 50 cases. Ann
Phy Med 1966; 9:22-28.
148. Sharma S, Stedman R. Epidural steroids.
A retrospective analysis of the ecacy of
high and low dose therapy. Anesthesiol-
ogy 1998; 3A:A1135.
149. Rosen CD, Kahanovitz N, Berstein R et al.
A retrospective analysis of the ecacy of
epidural steroid injections. Clin Orthop
1988; 228:270-272.
150. Arnhoff FN, Triplett HB, Pokorney B. Fol-
low-up status of patients treated with
nerve blocks for low back pain. Anesthesi-
ology 1977; 46:170-178.
151. Jamison RN, VadeBoncouer T, Ferrante FM.
Low back pain patients unresponsive to
an epidural steroid injection: Identifying
predictive factors. Clin J Pain 1991; 7:311-
317.
152. Hopwood MB, Abram SE. Factors associ-
ated with failure of lumbar epidural ste-
roids. Reg Anesth 1993; 18:238-243.
153. Reale C, Turkiewicz AM, Reale CA et al.
Epidural steroids as a pharmacological
approach. Clin Exp Rheumatol 2000; 18:
S65-S66.
154. Bowman SJ, Wedderburn L, Whaley A et al.
Outcome assessment after epidural corti-
costeroid injection for low back pain and
sciatica. Spine 1993; 18:1345-1350.
155. Jurmand SH. Cortiotherapie peridurale
des lombalgies et des sciatiques d’origine
discale. Concours Medicale 1972; 94:
5061-5070.

Boswell et al • A Systematic Review of Epidural Steroids332
Pain Physician Vol. 6, No. 3, 2003
Boswell et al • A Systematic Review of Epidural Steroids 333
Pain Physician Vol. 6, No. 3, 2003
156. Ito R. The treatment of low back pain and
sciatica with epidural corticosteroids in-
jection and its pathophysiologic basis. J
Jpn Orthop Assoc 1971; 45:769-777.
157. Brown FW. Management of discogenic
pain using epidural and intrathecal ste-
roids. Clin Orthop 1977; 129:72-78.
158. Warr AC, Wilkinson JA, Burn JM et al.
Chronic lumbosciatica syndrome treated
by epidural injection and manipulation.
Practitioner 1977; 209:53-59.
159. Papagelopoulos PJ, Petrou HG, Triantafyl-
lidis PG et al. Treatment of lumbosacral
radicular pain with epidural steroid injec-
tions. Orthopedics 2001; 24:145-149.
160. Silva J, Costa AO, Simoes MT et al. Man-
agement of radicular pain from lumbar
herniated disc using betamethasone epi-
dural injection. Revista Brasileira de Orto-
pedia 1999; 34:165-168.
161. Mangar D, Thomas PB. Epidural steroid
injections in the treatment of cervical and
lumbar pain syndromes. Reg Anesth 1991;
16:246.
162. Riew KD, Yin Y, Gilula L et al. The effect of
nerve-root injections on the need for oper-
ative treatment of lumbar radicular pain. J
Bone Joint Surg 2000; 82A: 1589-1593.
163. Karppinen J, Malmivaara A, Kurunlahti M
et al. Periradicular inltration for sciatica.
Spine 2001; 26:1059-1067.
164. Karppinen J, Ohinmaa A, Malmivaara A et
al. Cost effectiveness of periradicular inl-
tration for sciatica. Spine 2001; 26:2587-
2595.
165. Devulder J, Deene P, De Laat M et al. Nerve
root sleeve injections in patients with
failed back surgery syndrome: A compari-
son of three solutions. Clin J Pain 1999; 15:
132-135.
166. Kolsi I, Delecrin J, Berthelot JM et al. Eca-
cy of nerve root versus interspinous injec-
tions of glucocorticoids in the treatment of
disc-related sciatica. A pilot, prospective,
randomized, double-blind study. Joint
Bone Spine 2000; 67:113-118.
167. Buttermann GR. Epidural steroid vs dis-
cectomy for lumbar disc herniation: A pro-
spective randomized study. Presented at
the 66
th
Annual Meeting, American Acad-
emy of Orthopaedic Surgeons, Anaheim,
CA, February 1999.
168. Lutz GE, Vad VB, Wisneski RJ. Fluoroscopic
transforaminal lumbar epidural steroids:
An outcome study. Arch Phys Med Reha-
bil 1998; 79:1362-1366.
169. Vad V, Bhat A, Lutz G, Camissa F. Transfo-
raminal epidural steroid injections in lum-
bosacral radiculopathy; A prospective
randomized study. Spine 2002; 27:11-16.
170. Berger O, Dousset V, Delmer O et al. Eval-
uation of the ecacy of foraminal infu-
sions of corticosteroids guided by com-
puted tomography in the treatment of ra-
dicular pain by foraminal injection. J Radi-
ol 1999; 80:917-925.
171. Melzer A, Seibel RM. Magnetic resonance
(MR)-guided percutaneous pain therapy
of degenerative spinal diseases. Semin
Interv Radiol 1999; 16:143-150.
172. Sequeiros RB, Ojala RO, Klemola R et al.
MRI-guided periradicular nerve root inl-
tration therapy in low-eld (0.23-T) MRI
system using optical instrument tracking.
Eur Radiol 2002; 12:1331-1337.
173. Zennaro H, Dousset V, Viaud B et al. Perig-
anglionic foraminal steroid injections per-
formed under CT control. Am J Neuroradiol
1998; 19:349-352.
174. Grönemeyer DH, Gevargez A, Schindler O
et al. CT-guided periradicular injections
of corticosteroids in the management of
lumbar radiculopathy associated with disk
herniation. J Radiol 2001; 1-12.
175. Buttermann GR. Lumbar disc herniation
regression after successful epidural ste-
roid injection. J Spin Dis Tech 2002; 15:
469-476.
176. Schmid G, Vetter S, Gottmann D et al. CT-
guided epidural/perineural injections in
painful disorders of the lumbar spine:
Short- and extended-term results. Cardio-
vasc Intervent Radiol 1999; 22:493-498.
177. Grönemeyer D, Seibel R, Schindler O et
al. Microinvasive CT guided periradicular
therapy for treatment of chronical func-
tional disorders of the spine. Weiner Med-
izinische Wochenschrift 1995; 145:129-
139.
178. Devulder J. Transforaminal nerve root
sleeve injection with corticosteroids, hy-
aluronidase, and local anesthetic in the
failed back surgery syndrome. J Spinal
Disord 1998; 11:151-154.
179. Slipman CW, Lipetz JS, Jackson HB et al.
Therapeutic selective nerve root block in
the nonsurgical treatment of atraumatic
cervical spondylotic radicular pain: A ret-
rospective analysis with independent clin-
ical review. Arch Phys Med Rehabil 2000;
81:741-746.
180. Lutze M, Stendel R, Vesper J et al. Perira-
dicular therapy in lumbar radicular syn-
dromes: Methodology and results. Acta
Neurochir 1997; 139:719-724.
181. Uhlenbrock D, Arlinghaus J. Results of CT-
guided periradicular pain therapy. Rofo
Fortschr Geb Rontgenstr Neuen Bildgeb
Verfahr 1997; 166:528-534.
182. Le Chevallier PL, Videgrain M, Roulleau P
et al. Injection of the sacrolumbar roots:
A complementary method of staging sci-
atica. 18 cases. Rev Rhum Mal Osteoartic
1978; 45:473-477.
183. Weiner BK, Fraser RD. Foraminal injection
for lateral lumbar disc herniation. J Bone
Joint Surg 1997; 79-B:804-807.
184. Narozny M, Zanetti M, Boos N. Therapeu-
tic ecacy of selective nerve root blocks in
the treatment of lumbar radicular leg pain.
Swiss Med Wkly 2001; 131:75-80.
185. Friedman R, Li V, Mehrotra D et al. Forami-
nal injection of a painful sacral nerve root
using an epidural catheter: Case report.
Reg Anesth Pain Med 2002; 27; 214-216.
186. Rosenberg SK, Grabinsky A, Kooser C et al.
Effectiveness of transforaminal epidural
steroid injections in low back pain: A one
year experience. Pain Physician 2002; 5:
266-270.
187. Wang JC, Lin E, Brodke DS et al. Epidural
injections for the treatment of symptomat-
ic lumbar herniated discs. J Spinal Disord
& Tech 2002; 15:269-272.
188. Waldman SD. Complications of cervical
epidural nerve blocks with steroids: A pro-
spective study of 790 consecutive blocks.
Reg Anesth 1989; 14:149-151.
189. Katz JA, Lukin R, Bridenbaugh PO et al.
Subdural intracranial air: An unusual
cause of headache after epidural steroid
injection. Anesthesiology 1991; 74:615.
190. Mateo E, Lopez-Alarcon MD, Moliner S et
al. Epidural and subarachnoid pneumo-
cephalus after epidural technique. Eur J
Anesthesiol 1999; 16:413-417.
191. MacLean CA, Bachman DT. Documented
arterial gas embolism after spinal epidural
injection. Ann Emerg Med 2001; 38:592-
595.
192. Williams KN, Jackowski A, Evans PJ. Epidu-
ral haematoma requiring surgical decom-
pression following repeated cervical epi-
dural steroid injections for chronic pain.
Pain 1990; 42:197-199.
193. Reitman CA, Watters W. Subdural hema-
toma after cervical epidural steroid injec-
tion. Spine 2002; 27:E174-E176.
194. Waldman SD. Cervical epidural abscess
after cervical epidural nerve block with
steroids (Letter). Anesth Anal 1991; 72:
717.
195. Mamourian AC, Dickman CA, Drayer BP et
al. Spinal epidural abscess: Three cases
following spinal epidural injection demon-
strated with magnetic resonance imaging.
Anesthesiology 1993; 78:204.
196. Knight JW, Cordingley JJ, Palazzo MG. Epi-
dural abscess following epidural steroid
and local anesthetic injection. Anaesthe-
sia 1997; 52:576-578.
197. Vijayan N, Dreyfus PM. Chemical epidural
abscess: Case report. J Neurol Neurosurg
Psychiatry 1971; 34:297-299.
198. Kaul S, Meena AK, Sundaram C et al. Spi-
nal extradural abscess following local ste-
roid injection. Neurol India 2000; 48:181-
183.
199. Elias M. Cervical epidural abscess follow-
ing trigger point injection. J Pain Symptom
Manage 1994; 9:71-72.
200. Chan ST, Leung S. Spinal epidural abscess
following steroid injection for sciatica:
Case report. Spine 1989; 14:106-108.
201. Goucke CR, Graziotti P. Extradural abscess
following local anaesthetic and steroid in-
jection for chronic low back pain. Brit J
Anesth 1990; 65:427-429.
202. Yamaguchi M, Kawakubo A, Ide R et al.
Epidural abscess associated with epidur-
al block in a patient with immunosuppres-
sive disease. Jpn J Anesthesiol 1999; 48:
506-508.
203. Sowter MC, Burgess NA, Woodsford PV et
al. Delayed presentation of an extradural
abscess complicating thoracic extradural

Boswell et al • A Systematic Review of Epidural Steroids334
Pain Physician Vol. 6, No. 3, 2003
analgesia. Br J Anaesth 1992; 68:103-105.
204. Vos PE, de Boer WA, Wurzer JA et al. Sub-
dural hematoma after lumbar puncture:
two case reports and review of the litera-
ture. Clin Neurol Neurosurg 1991; 93:127-
132.
205. Tekkok IH, Carter DA, Brinker R. Spinal
subdural hematoma as a complication of
immediate epidural blood patch. Can J An-
aesth 1996; 43:306-309.
206. Sabel M, Felsberg J, Neuen-Jacob E et al.
Enlargement of a chronic aseptic lum-
bar epidural abscess by intraspinal injec-
tions—a rare cause of progressive para-
paresis. Zentralbl Neurochir 2000; 61:111-
114.
207. Gutknecht DR. Chemical meningitis fol-
lowing epidural injections of corticoste-
roids (Letter). Am J Med 1987; 82:570.
208. Williamson JA. Inadvertent spinal subdu-
ral injection during attempted spinal epi-
dural steroid therapy. Anaesth Intens Care
1990; 18:406-408.
209. Lubenow T, Keh-Wong E, Kristof K et al. In-
advertent subdural injection: A complica-
tion of an epidural block. Anesth Analg
1988; 67:175-179.
210. Siegfried RN. Development of complex re-
gional pain syndrome after a cervical epi-
dural steroid injection. Anesthesiology
1997; 86:1394-1396.
211. Dreskin S, Bajwa ZH, Lehmann L et al.
Polymyoclonus resulting from possible ac-
cidental subdural injection of local anes-
thetic. Anesth Analg 1997; 84:692-693.
212. Kardash K, Morrow F, Béïque F. Seizures
after epidural blood patch with undiag-
nosed subdural hematoma. Reg Anesth
Pain Med 2002; 27:433-436.
213. Rovira E, Garcia-Escrig M, Catala J et al.
Chronic adhesive arachnoiditis following
epidural paramethasone. Revista de Neu-
rologia 1997; 25:2067-2068.
214. Ling C, Atkinson PL, Munton CF. Bilateral
retinal hemorrhages following epidural in-
jection. Br J Ophthalmol 1993; 77:316.
215. Young WF. Transient blindness after lum-
bar epidural steroid injection. Spine
2002; 27:E476-E477.
216. Kusher FH, Olson JC. Retinal hemorrhage
as a consequence of epidural steroid in-
jection. Arch Opthalmol 1995; 113:309-
313.
217. Purdy EP, Gurjit SA. Vision loss after lum-
bar epidural steroid injection. Anesth
Analg 1998; 86:119-122.
218. Kao LY. Bilateral serous retinal detach-
ment resembling central serious chorio-
retinopathy following epidural steroid in-
jection. Retina 1998; 18:479-481.
219. Slipman CW, Shin CH, Patel RK et al. Per-
sistent hiccup associated with thoracic
epidural injection. Am J Phys Med Rehabil
2001; 80:618-621.
220. Slipman CW, Chow DW, Lenrow DA. Dys-
phonia associated with epidural steroid
injection: A case report. Arch Phys Med
Rehabil 2002; 83:1309-1310.
221. Sandberg DI, Lavyne MH. Symptomat-
ic spinal epidural lipomatosis after local
epidural corticosteroid injections: Case re-
port. Neurosurgery 1999; 45:162-165.
222. Trattner A, Hodak E, David M et al. Kapo-
si’s sarcoma with visceral involvement af-
ter intraarticular and epidural injections of
corticosteroids. J Am Acad Dermatol 1993;
29:890-894.
223. Knight CL, Burnell JC. Systemic side-ef-
fects of extradural steroids. Anaesthesia
1980; 35:593-594.
224. Jacobs S, Pullan PT, Potter JM et al. Adre-
nal suppression following extradural ste-
roids. Anaesthesia 1983; 38:953-956.
225. Boonen S, Van Distel G, Westhovens R et
al. Steroid myopathy induced by epidural
triamcinolone injection. Brit J Rheumatol
1995; 34:385.
226. Maillefert JF, Aho S, Huguenin MC et al.
Systemic effects of epidural dexametha-
sone injections. Revue du Rhumatisme
1995; 62:429-432.
227. Ward A, Watson J, Wood P et al. Glucocor-
ticoid epidural for sciatica: Metabolic and
endocrine sequelae. Rheumatology 2002;
41:68-71.
228. Manchikanti L, Pampati V, Beyer C et al.
The effect of neuraxial steroids on weight
and bone mass density: A prospective
evaluation. Pain Physician 2000; 3:357-
366.
229. Houten JK, Errico TJ. Paraplegia after lum-
bosacral nerve root block: Report of three
cases. The Spine Journal 2002; 2:70-75.
230. Sullivan WJ, Willick SE, Chira-Adisai W et
al. Incidence of intravascular uptake in
lumbar spinal injection procedures. Spine
2000; 25:481-486.
231. Furman MB. Incidence of intravascular
uptake in transforaminal lumbar epidural
steroid injections. Spine 2000; 25:2628-
2632.
232. Botwin KP, Gruber RD, Bouchlas CG et al.
Complications of uoroscopically guid-
ed transforaminal lumbar epidural injec-
tions. Arch Phys Med Rehabil 2000; 81:
1045-1050.
233. Elias M. A rare cause of radiculopathy fol-
lowing transforaminal epidural steroid in-
jection. Pain Clinic 1998; 11:159-160.
234. Cousins MJ. An additional dimension to
the ecacy of epidural steroids. Anesthe-
siology 2000; 93:565.
235. Brouwers PJ, Kottink EJ, Simon MA et al.
A cervical anterior spinal artery syndrome
after diagnostic blockade of the right C6-
nerve root. Pain 2001; 91:397-399.
236. Nash TP. Comment on A cervical anterior
spinal artery syndrome after diagnostic
blockade of the right C6-nerve root. Pain
2001; 91:217-218.
237. Stohr M, Mayer K. Nerve-root damage
from local injections. Dtsch Med Wochen-
schr 1976; 101:1218-1220.
238. Milhaud D, Heroum C, Charif M et al. Dural
puncture and corticotherapy as risks fac-
tors for cerebral venous sinus thrombosis.
Eur J Neruol 2000; 7:123-124.
239. Bromage RP, Benumof JL. Paraplegia fol-
lowing intracord injection during attempt-
ed epidural anesthesia under general an-
esthesia. Reg Anesth Pain Med 1998; 23:
104-107.
240. Hodges SD, Castleberg RL, Miller T et al.
Cervical epidural steroid injection with in-
trinsic spinal cord damage. Two case re-
ports. Spine 1998; 23:2137-2142.
241. Pounder D, Elliott S. An awake patient
may not detect spinal cord puncture. An-
aesthesia 2000; 55:194.
242. Delaney TJ, Rowlingson JC, Carron H et al.
Epidural steroid effects on nerves and me-
ninges. Anesth Analg 1980; 58:610-614.
243. MacKinnon Se, Hudson AR, Gentilli R et al.
Peripheral nerve injection injury with ste-
roid agents. Plast Reconstr Surg 1982; 69:
482-489.
244. Chino N, Awad EA, Kottke FJ. Pathology
of propylene glycol administered by peri-
neural and intramuscular injection in rats.
Arch Phys Med Rehab 1974; 55:33-38.
245. Benzon HT, Gissen AJ, Strichartz GR et al.
The effect of polyethylene glycol on mam-
malian nerve impulses. Anesth Analg
1987; 66:553-559.
246. Abram SE, Marsala M, Yaksh TL. Analgesic
and neurotoxic effects of intrathecal corti-
costeroids in rats. Anesthesiology 1994;
81:1198-1205.
247. Latham JM, Fraser RD, Moore RJ et al. The
pathologic effects of intrathecal beta-
methasone. Spine 1997; 22:1558-1562.
248. Robustelli della Cuna FS, Mella M, Magis-
trali G et al. Stability and compatibility of
methylprednisolone acetate and ropiva-
caine hydrochloride in polypropylene sy-
ringes for epidural administration. Am J
Health Syst Pharm 2001; 58:1753-1756.
249. Swai EA, Rosen M. An attempt to develop a
model to study the effects of intrathecal ste-
roids. Eur J Anaesthesiol 1986; 3:127-136.
250. Slucky AV, Sacks MS, Pallares VS et al. Ef-
fects of epidural steroids on lumbar dura
material properties. J Spin Disord 1999;
12:331-340.
