
Aetna Student Health
SM
Plan Design and Benefits Summary
Preferred Provider Organization (PPO)
Illinois Institute of Technology
Policy Year: 2024 – 2025
Policy Number: 724532
https://www.aetnastudenthealth.com
(800) 841-3140

Illinois Institute of Technology 2024-2025 Page 2
This is a brief description of the Student Health Plan. The Plan is available for Illinois Institute of Technology students
and their eligible dependents. The Plan is underwritten by Aetna Life Insurance Company (Aetna). The exact provisions,
including definitions, governing this insurance are contained in the Policy issued to you and may be viewed online at
https://www.aetnastudenthealth.com
. If there is a difference between this Benefit Summary and the Master Policy,
the Policy will control.
Illinois Institute of Technology Health Services
The Student Health and Wellness Center is the University's on-campus health facility. Staffed by Nurse Practitioners,
Medical Assistants, Physician Assistants, a part-time Physician and Psychiatrist, Psychologist, LCPC’s, Psychology Externs
and a Post-Doctoral Fellow and Administrative Professionals
The Student Health and Wellness Center is open Monday - Friday from 8:30 -5pm. To view hours of operation, go online
to www.iit.edu/shwc
.
For more information about them, call the Student Health and Wellness Center at (312) 567-7550. In the event of an
emergency, call 911 or the Campus Police at (312) 808-6300.
Coverage Periods
Students: Coverage for all insured students enrolled for the Fall Semester will become effective at 12:01 AM on August
10, 2024 and will terminate at 11:59 PM on August 09, 2025.
New Spring Semester students: Coverage for all insured students enrolled for the Spring Semester will become effective
at 12:01 AM on January 6, 2025 and will terminate at 11:59 PM on August 09, 2025.
Insured dependents: Coverage will become effective on the same date the insured student's coverage becomes
effective, or the day after the postmarked date when the completed application and premium are sent, if later.
Coverage for insured dependents terminates in accordance with the Termination Provisions described in the Master
Policy. Examples include, but are not limited to:
The date the student’s coverage terminates, the date the dependent no longer meets the definition of a dependent.
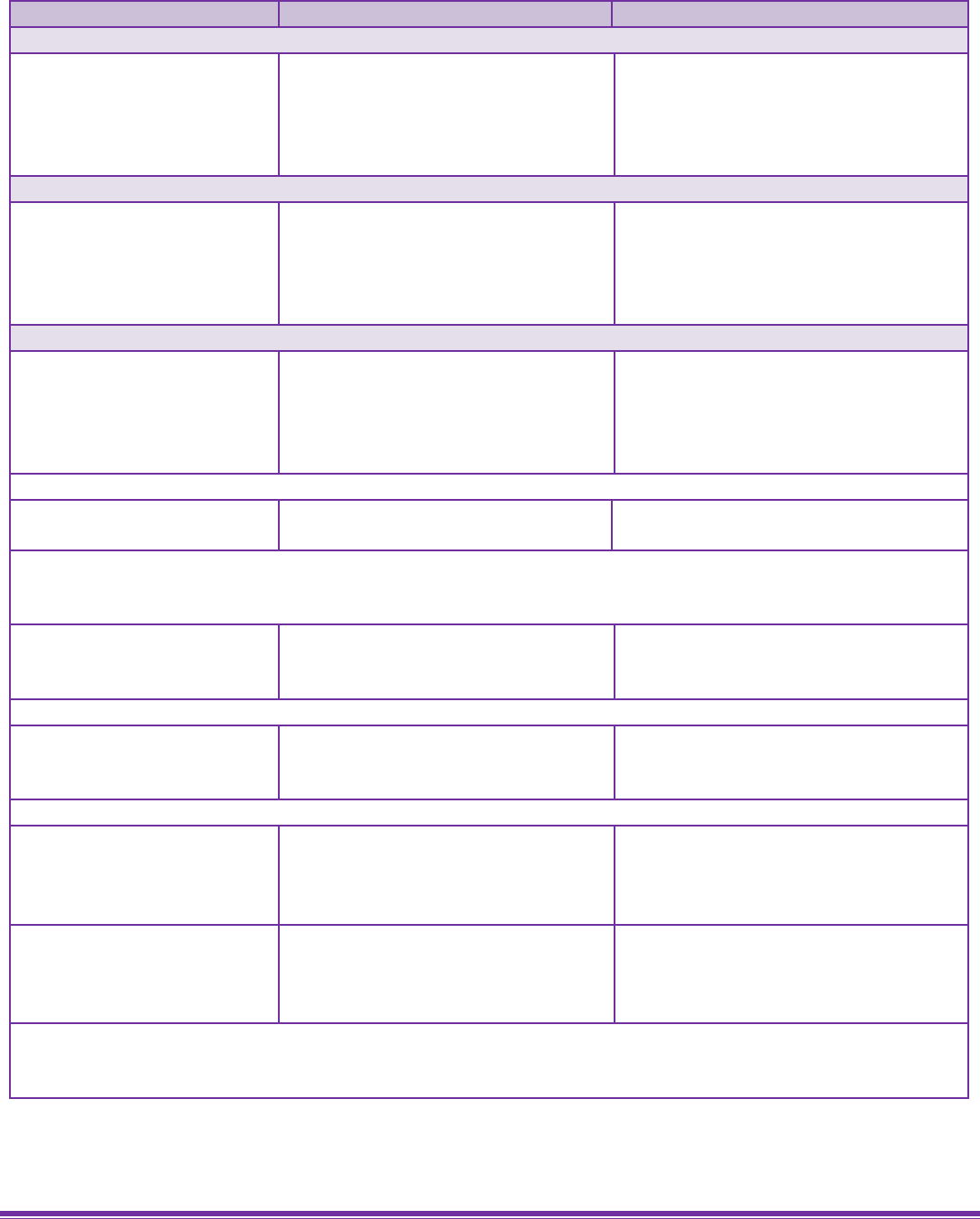
Coverage Period
Coverage Start Date
Coverage End Date
Enrollment/Waiver Deadline
Annual 08/10/2024 08/09/2025 09/01/2024
Fall 08/10/2024 01/05/2025 09/01/2024
Spring 01/06/2025 08/09/2025 01/26/2025
Summer 05/20/2025 08/09/2025 06/24/2025

Illinois Institute of Technology 2024-2025 Page 3
Eligible Dependents: Coverage will, will become effective at 12:01 AM on the Coverage Start Date indicated below
August 10, 2023, and will terminate at 11:59 PM on the Coverage End Date indicated August 09, 2024. Coverage for
insured dependents terminates in accordance with the Termination Provisions described in the Master Policy.
Coverage Period Coverage Start Date Coverage End Date Enrollment/Waiver Deadline
Annual 08/10/2024 08/09/2025 09/01/2024
Fall 08/10/2024 01/05/2025 09/01/2024
Spring 01/06/2025 08/09/2025 01/26/2025
Summer 05/20/2025 08/09/2025 06/24/2025
Rates
The rates below include both premiums for the Plan underwritten by Aetna Life Insurance Company (Aetna), as well as
the Illinois Institute of Technology administrative fee.
Annual
Spring
Summer
Student
$2,286 $1,344 $496
Spouse
$2,286 $1,344 $496
Child
$2,286 $1,344 $496
Children
$4,572 $2,688 $992
Student Coverage
Who is eligible?
You must purchase the IL Tech Student Health Insurance Plan if you are registered for" 1" or more academic credit hours
during the semester if you are not covered under another comparable plan.
Enrollment
Eligible students will be automatically enrolled in this plan, unless the electronic Waiver Form has been received and
approved by the Student Health and Wellness Center, by the specified enrollment deadline dates listed in the next
section of this brochure.
If you withdraw from school within the first 31 days of a coverage period, you will not be covered under the Policy and
the full premium will be refunded, less any claims paid. After 31 days, you will be covered for the full period that you
have paid the premium for, and no refund will be allowed. (This refund policy will not apply if you withdraw due to a
covered Accident or Sickness.)
Exception: A Covered Person entering the armed forces of any country will not be covered under the Policy as of the
date of such entry. A pro rata refund of premium will be made for such person, and any covered dependents, upon
written request received by Aetna within 90 days of withdrawal from school.

Illinois Institute of Technology 2024-2025 Page 4
Dependent Coverage
Eligibility
Covered students may also enroll their lawful spouse, civil union partner, and dependent children under age 26.
Overage dependents
If your plan includes dependent coverage, you can enroll unmarried dependents up to age 30 if they reside in Illinois,
have served in the US Armed Forces (AF) and were discharged from the AF other than dishonorable discharge.
Important note regarding coverage for a newborn infant or newly adopted child:
Newborn child
• Your newborn child is covered on your health plan for the first 31 days from the moment of birth.
• To keep your newborn covered, you must notify us (or our agent) of the birth and pay any required premium
contribution during that 31 day period.
• You must still enroll the child within 31 days of the moment of birth even when coverage does not require
payment of an additional premium contribution for the newborn.
• If you miss this deadline, your newborn will not have health benefits after the first 31 days from the moment of
birth.
• If your coverage ends during this 31 day period, then your newborn‘s coverage will end on the same date as
your coverage. This applies even if the 31 day period has not ended.
Adopted child or a child legally placed with you for adoption
A child that you, or you and your spouse, civil union partner or domestic partner adopt, or that is placed with you for
adoption is covered on your plan for the first 31 days after the adoption or the placement is complete.
• To keep your child covered, we must receive your completed enrollment information within 31 days after the
adoption or placement for adoption.
• You must still enroll the child within 31 days of the adoption or placement for adoption even when coverage
does not require payment of an additional premium contribution for the child.
• If you miss this deadline, your adopted child or child placed with you for adoption will not have health benefits
after the first 31 days.
• If your coverage ends during this 31 day period, then coverage for your adopted child or child placed with you
for adoption will end on the same date as your coverage. This applies even if the 31 day period has not ended.
Dependent coverage due to a court order
If you must provide coverage to a dependent because of a court order, your dependent is covered on your health plan
for the first 31 days from the court order.
• To keep your dependent covered, we must receive your completed enrollment information within 31 days of the
court order.
• You must still enroll the dependent within 31 days of the court order even when coverage does not require
payment of an additional premium contribution for the dependent.
• If you miss this deadline, your dependent will not have health benefits after the first 31 days.
• If your coverage ends during this 31 day period, then your dependent’s coverage will end on the same date as
your coverage. This applies even if the 31 day period has not ended.
Enrollment
If you are enrolled in the Student Health Insurance Plan, you may also purchase coverage for your eligible dependents by
completing the dependent enrollment form located under the navigation menu at www.universityhealthplans.com/iit

Illinois Institute of Technology 2024-2025 Page 5
Waiver Process/Procedure
Domestic students may waive this coverage if the student presents evidence of other health insurance coverage under a
plan, which provides benefits equivalent to the Plan. Students must complete the online Waiver Form by the Waiver
Deadline below. Waiver Forms are available at www.universityhealthplans.com/iit
To ensure all international students meet the Federal Visa Insurance Requirements, coverage is mandatory for all Full-
Time and Part-Time J-1 and F-1 international students.
Medicare Eligibility Notice
You are not eligible to enroll in the student health plan if you have Medicare at the time of enrollment in this student
plan. The plan does not provide coverage for people who have Medicare.
Termination and Refunds
Withdrawal from Classes – Leave of Absence:
If you withdraw from classes under a school-approved leave of absence, your coverage will remain in force through the
end of the period for which payment has been received and no premiums will be refunded.
Withdrawal from Classes – Other than Leave of Absence:
If you withdraw from classes other than under a school-approved leave of absence within 31 days after the policy
effective date, you will be considered ineligible for coverage, your coverage will be terminated retroactively and any
premiums collected will be refunded. If the withdrawal is more than 31 days after the policy effective date, your
coverage will remain in force through the end of the period for which payment has been received and no premiums will
be refunded. If you withdraw from classes to enter the armed forces of any country, coverage will terminate as of the
effective date of such entry and a pro rata refund of premiums will be made if you submit a written request within 90
days of withdrawal from classes.
In-network Provider Network
Aetna Student Health offers Aetna’s broad network of In-network Providers. You can save money by seeing In-network
Providers because Aetna has negotiated special rates with them, and because the Plan’s benefits are better.
If you need care that is covered under the Plan but not available from an In-network Provider, contact Member Services
for assistance at the toll-free number on the back of your ID card. In this situation, Aetna may issue a pre-approval for
you to receive the care from an Out-of-network Provider. When a pre-approval is issued by Aetna, the benefit level is
the same as for In-network Providers.

Illinois Institute of Technology 2024-2025 Page 6
Precertification
You need pre-approval from us for some eligible health services. Pre-approval is also called precertification. Your in-
network physician is responsible for obtaining any necessary precertification before you get the care. When you go to an
out-of-network provider, it is your responsibility to obtain precertification from us for any services and supplies on the
precertification list. For a current listing of the health services or prescription drugs that require precertification,
contact Member Services or go to www.aetna.com.
Precertification Call
Precertification should be secured within the timeframes specified below. To obtain precertification, call Member
Services at the toll-free number on your ID card. You, your physician or the facility must call us within these timelines:
Non-emergency admissions
Call at least 14 days before the date you are scheduled to be admitted.
Emergency admission
Call within 48 hours or as soon as reasonably possible after you have been
admitted.
Urgent admission
Call before you are scheduled to be admitted.
Outpatient non-emergency
medical services
Call at least 14 days before the care is provided, or the treatment is scheduled
An urgent admission is a hospital admission by a physician due to the onset of or change in an illness, the diagnosis of an
illness, or an injury.
We will provide a written notification to you and your physician of the precertification decision, where required by state
law. If your precertified services are approved, the approval is valid for 60 days as long as you remain enrolled in the
plan.
Coordination of Benefits (COB)
Some people have health coverage under more than one health plan. If you do, we will work together with your other
plan(s) to decide how much each plan pays. This is called coordination of benefits (COB). A complete description of the
Coordination of Benefits provision is contained in the certificate issued to you.

Illinois Institute of Technology 2024-2025 Page 7
Description of Benefits
The Plan excludes coverage for certain services and has limitations on the amounts it will pay. While this Plan Summary
document will tell you about some of the important features of the Plan, other features that may be important to you
are defined in the Certificate. To look at the full Plan description, which is contained in the Certificate issued to you, go
to https://www.aetnastudenthealth.com
.
This Plan will pay benefits in accordance with any applicable Illinois Insurance Law(s).
In-network coverage
Out-of-network coverage
Policy year deductibles
You have to meet your policy year deductible before this plan pays for benefits.
Student
$300 per policy year
$400 per policy year
Spouse
$300 per policy year
$400 per policy year
Each child
$300 per policy year
$400 per policy year
Family
None
None
Policy year deductible waiver
The policy year deductible is waived for all of the following eligible health services:
• In-network care for Preventive care and wellness, Pediatric Dental Care services, and Outpatient Prescription
Drugs
•
In-network care and out-of-network care for Pediatric Vision Care Services and Well newborn nursery care
Maximum out-of-pocket limits
In-network coverage
Out-of-network coverage
Student
$6,850 per policy year
None
Spouse
$6,850 per policy year
None
Each child
$6,850 per policy year
None
Family
$13,700 per policy year
None

Illinois Institute of Technology 2024-2025 Page 8
The coinsurance listed in the schedule of benefits below reflects the plan coinsurance percentage. This is the
coinsurance amount that the plan pays. You are responsible for paying any remaining coinsurance.
Eligible health services
In-network coverage
Out-of-network coverage
Preventive care and wellness
Routine physical exams
100% (of the negotiated charge) per
visit
No copayment or policy year
deductible applies
80% (of the recognized charge) per
visit
Covered persons through age 21
Maximum age and visit limits per
policy year
Subject to any age and visit limits provided for in the comprehensive guidelines
supported by the American Academy of Pediatrics/Bright Futures//Health
Resources and Services Administration guidelines for children and adolescents.
Preventive care immunizations
Performed in a facility or at a
physician's office
100% (of the negotiated charge) per
visit
No copayment or policy year
deductible applies
80% (of the recognized charge) per
visit
Maximums
Subject to any age limits provided for in the comprehensive guidelines
supported by Advisory Committee on Immunization Practices of the Centers
for Disease Control and Prevention
The following is not covered under this benefit:
• Any immunization that is not considered to be preventive care or recommended as preventive care, such as
those required due to employment or travel
Routine gynecological exams (including Pap smears and cytology tests)
Performed at a physician’s,
obstetrician (OB), gynecologist
(GYN) or OB/GYN office
100% (of the negotiated charge) per
visit
No copayment or policy year
deductible applies
80% (of the recognized charge) per
visit
Preventive screening and counseling services
Preventive screening and counseling
services for Obesity and/or healthy
diet counseling, Misuse of alcohol &
drugs, Tobacco Products, Sexually
transmitted infection counseling &
Genetic risk counseling for breast
and
ovarian cancer
100% (of the negotiated charge) per
visit
No copayment or policy year
deductible applies
80% (of the recognized charge) per
visit
Skin cancer behavioral counseling
office visits
100% (of the negotiated charge) per
visit
No copayment or policy year
deductible applies
80% (of the recognized charge) per
visit

Illinois Institute of Technology 2024-2025 Page 9
Eligible health services
In-network coverage
Out-of-network coverage
Falls prevention counseling office
visits
100% (of the negotiated charge) per
visit
No copayment or policy year
deductible applies
80% (of the recognized charge) per
visit
Routine cancer screenings
100% (of the negotiated charge) per
visit
No copayment or policy year
deductible applies
80% (of the recognized charge) per
visit
Maximum:
Subject to any age; family history; and frequency guidelines as set forth in the
most current:
• Evidence-based items that have in effect a rating of A or B in the current
recommendations of the United States Preventive Services Task Force; and
• The comprehensive guidelines supported by the Health Resources and
Services Administration.
Prenatal care services (Preventive
care services only)
100% (of the negotiated charge) per
visit
No copayment or policy year
deductible applies
80% (of the recognized charge) per
visit
Lactation counseling services
100% (of the negotiated charge) per
visit
No copayment or policy year
deductible applies
80% (of the recognized charge) per
visit
Breast pump supplies and
accessories
100% (of the negotiated charge) per
item
No copayment or policy year
deductible applies
80% (of the recognized charge) per
item
Family planning services – contraceptives
Contraceptive counseling services
office visit
100% (of the negotiated charge) per
visit
No copayment or policy year
deductible applies
80% (of the recognized charge) per
visit
Contraceptive prescription drugs
and devices provided, administered,
or removed, by a provider during an
office visit
100% (of the negotiated charge) per
item
No copayment or policy year
deductible applies
80% (of the recognized charge) per
item
Voluntary sterilization
Inpatient provider services
100% (of the negotiated charge) per
No copayment or policy year
deductible applies
80% (of the recognized charge)

Illinois Institute of Technology 2024-2025 Page 10
Eligible health services
In-network coverage
Out-of-network coverage
Outpatient provider services
100% (of the negotiated charge) per
No copayment or policy year
deductible applies
80% (of the recognized charge)
The following are not covered under this benefit:
• Services provided as a result of complications resulting from a voluntary sterilization procedure and related
follow-up care
•
Any contraceptive methods that are only "reviewed" by the FDA and not "approved" by the FDA
Physicians and other health professionals
Physician, specialist including
Consultants Office
visits (non-surgical/non-preventive
care by a physician and specialist)
includes telemedicine consultations)
80% (of the negotiated charge) per
visit
60% (of the recognized charge) per
visit
Allergy testing and treatment
Allergy testing performed at a
physician’s or specialist’s office
80% (of the negotiated charge) per
visit
60% (of the recognized charge) per
visit
Allergy injections treatment
performed at a physician or
specialist office
80% (of the negotiated charge) per
visit
60% (of the recognized charge) per
visit
The following are not covered under this benefit:
• Allergy sera and extracts administered via injection
Physician and specialist surgical services
Inpatient surgery performed during
your stay in a hospital or birthing
center by a surgeon
(includes anesthetist and surgical
assistant expenses)
80% (of the negotiated charge)
60% (of the recognized charge)
The following are not covered under this benefit:
• A stay in a hospital (Hospital stays are covered in the Eligible health services and exclusions – Hospital and
other facility care section)
•
Services of another physician for the administration of a local anesthetic
Outpatient surgery performed at a
physician’s or specialist’s office or
outpatient department of a hospital
or surgery center by a surgeon
(includes anesthetist and surgical
assistant expenses)
80% (of the negotiated charge) per
visit
60% (of the recognized charge) per
visit
The following are not covered under this benefit:
• A stay in a hospital (Hospital stays are covered in the Eligible health services and exclusions – Hospital and
other facility care section)
• A separate facility charge for surgery performed in a physician’s office
• Services of another physician for the administration of a local anesthetic

Illinois Institute of Technology 2024-2025 Page 11
Eligible health services
In-network coverage
Out-of-network coverage
Alternatives to physician office visits
Walk-in clinic visits
(non-emergency visit)
80% (of the negotiated charge) per
visit
60% (of the recognized charge) per
visit
Hospital and other facility care
Inpatient hospital (room and
board) and other miscellaneous
services and supplies)
Includes birthing center facility
charges
80% (of the negotiated charge) per
admission
60% (of the recognized charge) per
admission
In-hospital non-surgical physician
services
80% (of the negotiated charge) per
visit
60% (of the recognized charge) per
visit
Preadmission testing
Covered according to the type of
benefit and the place where the
service is received.
Covered according to the type of
benefit and the place where the
service is received.
Alternatives to hospital stays
Outpatient surgery (facility charges)
performed in the outpatient
department of a hospital or surgery
center
For physician charges, refer to the
Physician and specialist - outpatient
surgical services benefit
80% (of the negotiated charge)
60% (of the recognized charge)
The following are not covered under this benefit:
• A stay in a hospital (See the Hospital care – facility charges benefit in this section)
• A separate facility charge for surgery performed in a physician’s office
•
Services of another physician for the administration of a local anesthetic
Home health Care
80% (of the negotiated charge) per
visit
60% (of the recognized charge) per
visit
The following are not covered under this benefit:
• Nursing and home health aide services or therapeutic support services provided outside of the home (such as
in conjunction with school, vacation, work or recreational activities)
• Transportation
• Homemaker or housekeeper services
• Food or home delivered services
• Maintenance therapy
Hospice-Inpatient
(room and board and other
miscellaneous services and supplies)
80% (of the negotiated charge) per
admission
60% (of the recognized charge) per
admission
Hospice-Outpatient
80% (of the negotiated charge) per
visit
60% (of the recognized charge) per
visit
The following are not covered under this benefit:
• Funeral arrangements
• Pastoral counseling
• Bereavement counseling
• Financial or legal counseling which includes estate planning and the drafting of a will

Illinois Institute of Technology 2024-2025 Page 12
• Homemaker or caretaker services that are services which are not solely related to your care and may include:
- Sitter or companion services for either you or other family members
- Transportation
-
Maintenance of the house
Eligible health services
In-network coverage
Out-of-network coverage
Outpatient private duty nursing
80% (of the negotiated charge) per
visit
60% (of the recognized charge) per
visit
Skilled nursing facility-
Inpatient (room and board and
miscellaneous inpatient care
services and supplies)
Subject to semi-private room rate
unless intensive care unit is required
Room and board includes intensive
care
80% (of the negotiated charge) per
admission
60% (of the recognized charge) per
admission
Hospital emergency room
80% (of the negotiated charge) per
visit
Paid the same as in-network
coverage
Emergency services resulting from a
criminal sexual assault or abuse
100% (of the negotiated charge) per
visit
No policy year deductible applies
Paid the same as in-network
coverage
Important note:
• As out-of-network providers do not have a contract with us the provider may not accept payment of your cost
share, (copayment/coinsurance), as payment in full. You may receive a bill for the difference between the
amount billed by the provider and the amount paid by this plan. If the provider bills you for an amount above
your cost share, you are not responsible for paying that amount. You should send the bill to the address listed
on the back of your ID card, and we will resolve any payment dispute with the provider over that amount.
Make sure the ID card number is on the bill.
• A separate hospital emergency room copayment/coinsurance will apply for each visit to an emergency room.
If you are admitted to a hospital as an inpatient right after a visit to an emergency room, your emergency
room copayment/coinsurance will be waived and your inpatient copayment/coinsurance will apply.
• Covered benefits that are applied to the hospital emergency room copayment/coinsurance cannot be applied
to any other copayment/coinsurance under the plan. Likewise, a copayment/coinsurance that applies to
other covered benefits under the plan cannot be applied to the hospital emergency room
copayment/coinsurance.
• Separate copayment/coinsurance amounts may apply for certain services given to you in the hospital
emergency room that are not part of the hospital emergency room benefit. These copayment/coinsurance
amounts may be different from the hospital emergency room copayment/coinsurance. They are based on the
specific service given to you.
• Services given to you in the hospital emergency room that are not part of the hospital emergency room
benefit may be subject to copayment/coinsurance amounts that are different from the hospital emergency
room copayment/coinsurance amounts.

Illinois Institute of Technology 2024-2025 Page 13
Eligible health services
In-network coverage
Out-of-network coverage
Urgent medical care
80% (of the negotiated charge) per
visit
60% (of the recognized charge) per
visit
Pediatric dental care (Limited to covered persons through the end of the month in which the person turns age 19.
Type A services
100% (of the negotiated charge) per
visit
No copayment or deductible applies
70% (of the recognized charge) per
visit
Type B services
70% (of the negotiated charge) per
visit
No copayment or deductible applies
50% (of the recognized charge) per
visit
Type C services
50% (of the negotiated charge) per
visit
No copayment or deductible applies
50% (of the recognized charge) per
visit
Orthodontic services
50% (of the negotiated charge) per
visit
No copayment or deductible applies
50% (of the recognized charge) per
visit
Dental emergency services
Covered according to the type of
benefit and the place where the
service is received.
Covered according to the type of
benefit and the place where the
service is received.
The following are not covered under this benefit:
• Any instruction for diet, plaque control and oral hygiene
• Cosmetic services and supplies including:
- Plastic surgery, reconstructive surgery, cosmetic surgery, personalization or characterization of dentures
or other services and supplies which improve, alter or enhance appearance
- Augmentation and vestibuloplasty, and other substances to protect, clean, whiten, bleach or alter the
appearance of teeth, whether or not for psychological or emotional reasons, except to the extent
coverage is specifically provided in the Eligible health services and exclusions section
- Facings on molar crowns and pontics will always be considered cosmetic
• Crown, inlays, onlays, and veneers unless:
- It is treatment for decay or traumatic injury and teeth cannot be restored with a filling material
- The tooth is an abutment to a covered partial denture or fixed bridge
• Dental implants and braces (that are determined not to be medically necessary), mouth guards, and other
devices to protect, replace or reposition teeth
• Dentures, crowns, inlays, onlays, bridges, or other appliances or services used:
- For splinting
- To alter vertical dimension
- To restore occlusion
- For correcting attrition, abrasion, abfraction or erosion
• Treatment of any jaw joint disorder and treatments to alter bite or the alignment or operation of the jaw,
including temporomandibular joint dysfunction disorder (TMJ) and craniomandibular joint dysfunction
disorder (CMJ) treatment, orthognathic surgery, and treatment of malocclusion or devices to alter bite or
alignment, except as covered in the Eligible health services and exclusions – Specific conditions section
• General anesthesia and intravenous sedation, unless specifically covered and only when done in connection
with another eligible health service

Illinois Institute of Technology 2024-2025 Page 14
• Orthodontic treatment except as covered above and in the Pediatric dental care section of the schedule of
benefits
• Pontics, crowns, cast or processed restorations made with high noble metals (gold)
• Prescribed drugs, pre-medication
• Replacement of a device or appliance that is lost, missing or stolen, and for the replacement of appliances that
have been damaged due to abuse, misuse or neglect and for an extra set of dentures
• Routine dental exams and other preventive services and supplies, except as specifically provided in the
Pediatric dental care section of the schedule of benefits
• Services and supplies:
- Done where there is no evidence of pathology, dysfunction, or disease other than covered preventive
services
- Provided for your personal comfort or convenience or the convenience of another person, including a
provider
- Provided in connection with treatment or care that is not covered under your policy
• Surgical removal of impacted wisdom teeth only for orthodontic reasons
• Treatment by other than a dentist or dental provider that is legally qualified to furnish dental services or
supplies
Eligible health services
In-network coverage
Out-of-network coverage
Diabetic services and supplies
(including equipment and training)
Covered according to the type of
benefit and the place where the
service is received.
Covered according to the type of
benefit and the place where the
service is received.
Podiatric (foot care) treatment
Physician and specialist non-routine
foot care treatment
Covered according to the type of
benefit and the place where the
service is received.
Covered according to the type of
benefit and the place where the
service is received.
The following are not covered under this benefit:
• Services and supplies for:
- The treatment of calluses, bunions, toenails, flat feet, hammertoes, fallen arches
- The treatment of weak feet, chronic foot pain or conditions caused by routine activities, such as walking,
running, working or wearing shoes
- Supplies (including orthopedic shoes), foot orthotics, arch supports, shoe inserts, ankle braces, guards,
protectors, creams, ointments and other equipment, devices and supplies
- Routine pedicure services, such as cutting of nails, corns and calluses when there is no illness or injury of
the feet
Impacted wisdom teeth
80% (of the negotiated charge)
80% (of the recognized charge)
Accidental injury to sound natural
teeth
80% (of the negotiated charge)
80% (of the recognized charge)
The following are not covered under this benefit:
• The care, filling, removal or replacement of teeth and treatment of diseases of the teeth
• Dental services related to the gums
• Apicoectomy (dental root resection)
• Orthodontics
• Root canal treatment
• Soft tissue impactions
• Bony impacted teeth
• Alveolectomy
• Augmentation and vestibuloplasty treatment of periodontal disease
• False teeth
•
Prosthetic restoration of dental implants

Illinois Institute of Technology 2024-2025 Page 15
• Dental implants
Eligible health services
In-network coverage
Out-of-network coverage
Temporomandibular joint
dysfunction (TMJ) and
craniomandibular joint dysfunction
(CMJ) treatment
Covered according to the type of
benefit and the place where the
service is received.
Covered according to the type of
benefit and the place where the
service is received.
The following are not covered under this benefit:
• Dental implants
Clinical trial (routine patient
costs)
Covered according to the type of
benefit and the place where the
service is received.
Covered according to the type of
benefit and the place where the
service is received.
The following are not covered under this benefit:
• Services and supplies related to data collection and record-keeping that is solely needed due to the clinical
trial (i.e. protocol-induced costs)
• Services and supplies provided by the trial sponsor without charge to you
• The experimental intervention itself (except medically necessary Category B investigational devices and
promising experimental or investigational interventions for terminal illnesses in certain clinical trials in
accordance with Aetna’s claim policies)
Dermatological treatment
Covered according to the type of
benefit and the place where the
service is received.
Covered according to the type of
benefit and the place where the
service is received.
The following are not covered under this benefit:
•
Cosmetic treatment and procedures
Obesity bariatric Surgery and
services
Covered according to the type of
benefit and the place where the
service is received.
Covered according to the type of
benefit and the place where the
service is received.
The following are not covered services:
• Weight management treatment or drugs intended to decrease or increase body weight, control weight or
treat obesity, except as described in the certificate. This is regardless of whether there are other related
conditions. This includes:
- Drugs, stimulants, preparations, foods or diet supplements, dietary regimens and supplements, food
supplements, appetite suppressants and other medications
- Hypnosis or other forms of therapy
- Exercise programs, exercise equipment, membership to health or fitness clubs, recreational therapy or
other forms of activity or activity enhancement
Maternity care (includes
delivery and postpartum care
services in a hospital or
birthing center)
Covered according to the type of
benefit and the place where the
service is received.
Covered according to the type of
benefit and the place where the
service is received.
The following are not covered under this benefit:
• Any services and supplies related to births that take place in the home or in any other place not licensed to
perform deliveries

Illinois Institute of Technology 2024-2025 Page 16
Eligible health services
In-network coverage
Out-of-network coverage
Well newborn nursery
care in a hospital or
birthing center
80% (of the negotiated charge)
No policy year deductible applies
60% (of the recognized charge)
No policy year deductible applies
Abortion
Inpatient physician or
specialist surgical services
80% (of the negotiated charge)
60% (of the recognized charge)
Outpatient physician or
specialist surgical services
80% (of the negotiated charge)
60% (of the recognized charge)
Travel and lodging expenses
Travel and lodging reimbursement
100%
No policy year deductible applies
Limit per policy year
$3,000
The following are not covered under this benefit:
• Expenses for more than one travel companion [unless two parents are traveling with a minor child]
• Gasoline/fuel costs
• Car rentals
• Meals, groceries, hotel room service, alcohol/tobacco products
• Personal care/convenience items, (e.g. shampoo, clothing, deodorant)
• Entertainment/souvenir expenses
• Telephone calls
• Taxes
• Tips, gratuities
• Childcare expenses
• Lost wages
Abortion drugs (abortifacients)
Covered services include prescription drugs used for elective termination of pregnancy, including those prescribed or
ordered for off label use.
Gender affirming treatment
Surgical, hormone replacement
therapy, and counseling treatment
Covered according to the type of
benefit and the place where the
service is received.
Covered according to the type of
benefit and the place where the
service is received.
Autism spectrum disorder
Autism spectrum disorder
treatment, diagnosis and testing.
Includes Applied behavior analysis
and Physical, occupational, and
speech therapy associated with
diagnosis of autism spectrum
disorder
Covered according to the type of
benefit and the place where the
service is received.
Covered according to the type of
benefit and the place where the
service is received.

Illinois Institute of Technology 2024-2025 Page 17
Eligible health services
In-network coverage
Out-of-network coverage
Mental Health & Substance related disorders treatment
Inpatient hospital
(room and board and other miscellane
hospital
services and supplies)
80% (of the negotiated charge) per
admission
60% (of the recognized charge) per
admission
Outpatient office visits
(includes telemedicine
consultations)
80% (of the negotiated charge) per
visit
60% (of the recognized charge) per
visit
Other outpatient health disorders
treatment
(includes skilled behavioral health
services in the home)
(includes Partial hospitalization and
Intensive Outpatient Program)
80% (of the negotiated charge) per
visit
60% (of the recognized charge) per
visit
Eligible health services
In-network coverage (IOE facility)*
Out-of-network coverage*
(Includes providers who are
otherwise part of Aetna’s network
but are non-IOE providers)
Transplant services
Inpatient and outpatient transplant
facility services
Covered according to the type of
benefit and the place where the
service is received.
Covered according to the type of
benefit and the place where the
service is received.
Inpatient and outpatient transplant
physician and specialist services
Covered according to the type of
benefit and the place where the
service is received.
Covered according to the type of
benefit and the place where the
service is received.
Transplant services-travel and
lodging
Covered
Covered
Lifetime maximum payable for travel
and lodging expenses for any one
transplant, including tandem
transplants
$10,000
$10,000
Maximum payable for Lodging
Expenses per IOE patient
$50 per night
$50 per night
Maximum payable for Lodging
Expenses per companion
$50 per night
$50 per night
The following are not covered under this benefit:
• Services and supplies furnished to a donor when the recipient is not a covered person
• Harvesting and storage of organs, without intending to use them for immediate transplantation for your
existing illness
• Harvesting and/or storage of bone marrow, hematopoietic stem cells, or other blood cells without intending
to use them for transplantation within 12 months from harvesting, for an existing illness

Illinois Institute of Technology 2024-2025 Page 18
Eligible health services
In-network coverage
Out-of-network coverage
Infertility services
Treatment of basic infertility
Covered according to the type of
benefit and the place where the
service is received.
Covered according to the type of
benefit and the place where the
service is received.
Comprehensive infertility
services Inpatient and
outpatient care
Covered according to the type of
benefit and the place where the
service is received.
Covered according to the type of
benefit and the place where the
service is received.
Advanced reproductive technology
(ART) services
Covered according to the type of
benefit and the place where the
service is received.
Covered according to the type of
benefit and the place where the
service is received.
For treatment that includes an
oocyte retrieval, maximum number
of oocyte retrievals
4, however if a live birth follows a completed oocyte retrieval, 2 additional
oocyte retrievals will be covered.
The following are not covered under the infertility services benefit:
• All charges associated with or in support of surrogacy arrangements for you or the surrogate after discharge
to regular obstetrical care, non-medical expenses incurred to contract with the surrogate and any other
services provided to the surrogate that are not directly related to treatment of the covered individual's
infertility. A surrogate is a female carrying her own genetically related child with the intention of the child
being raised by someone else, including the biological father. If you choose to use a surrogate, this exclusion
does not apply to the cost for procedures to obtain the eggs, sperm or embryo from a covered individual.
• The purchase of donor embryos, donor eggs or donor sperm.
• Obtaining sperm from a person not covered under this plan.
• Infertility treatment when a successful pregnancy could have been obtained through less costly treatment.
• Infertility treatment when either partner has had voluntary sterilization surgery, with or without surgical
reversal, regardless of post reversal results. This includes tubal ligation, hysterectomy and vasectomy only if
obtained as a form of voluntary sterilization.
• Infertility treatment when infertility is due to a natural physiologic process such as age related ovarian
insufficiency (e.g., perimenopause, menopause) as measured by an unmedicated FSH level at or above 19 on
cycle day two or three of your menstrual period or other abnormal testing results as outlined in Aetna’s
infertility clinical policy..
• Treatment for dependent children, except for fertility preservation as described above.
Specific therapies and tests
Diagnostic complex imaging services
performed in the outpatient
department of a hospital or other
facility
No additional expense, such as a
copayment or deductible amount,
will be imposed for mammograms
80% (of the negotiated charge)
60% (of the recognized charge)
Diagnostic lab work performed in a
physician’s office, the outpatient
department of a hospital or other
facility
80% (of the negotiated charge)
60% (of the recognized charge)

Illinois Institute of Technology 2024-2025 Page 19
Eligible health services
In-network coverage
Out-of-network coverage
Diagnostic radiological services
performed in a physician’s office,
the outpatient department of a
hospital or other facility
No additional expense, such as a
copayment or deductible amount,
will be imposed for mammograms
80% (of the negotiated charge)
60% (of the recognized charge)
Outpatient infusion therapy
Covered according to the type of
benefit and the place where the
service is received.
Covered according to the type of
benefit and the place where the
service is received.
The following are not covered under this benefit:
• Drugs that are included on the list of specialty prescription drugs as covered under your outpatient
prescription drug plan
• Enteral nutrition
• Blood transfusions and blood products
• Dialysis
Outpatient Chemotherapy,
Radiation & Respiratory Therapy
80% (of the negotiated charge) per
visit
60% (of the recognized charge) per
visit
Outpatient physical, occupational,
speech, and cognitive therapies
(including Cardiac and Pulmonary
Therapy)
80% (of the negotiated charge) per
visit
60% (of the recognized charge) per
visit
Chiropractic services
80% (of the negotiated charge) per
visit
60% (of the recognized charge) per
visit
Specialty prescription drugs
purchased and injected or infused by
your provider in an outpatient
setting
Covered according to the type of
benefit or the place where the service
is received.
Covered according to the type of
benefit or the place where the
service is received.
Other services and supplies
Emergency ground, air, and water
ambulance
(includes non-emergency
ambulance)
80% (of the negotiated charge) per
trip
Paid the same as in-network
coverage
The following are not covered under this benefit:
• Ambulance services for routine transportation to receive outpatient or inpatient care
Durable medical and surgical
equipment
100% (of the negotiated charge) per
item
80% (of the recognized charge) per
item

Illinois Institute of Technology 2024-2025 Page 20
The following are not covered under this benefit:
• Whirlpools
• Portable whirlpool pumps
• Sauna baths
• Massage devices
• Over bed tables
• Elevators
• Communication aids
• Vision aids
• Telephone alert systems
• Personal hygiene and convenience items such as air conditioners, humidifiers, hot tubs, or physical exercise
equipment even if they are prescribed by a physician
Eligible health services
In-network coverage
Out-of-network coverage
Nutritional support
80% (of the negotiated charge) per
item
60% (of the recognized charge) per
item
The following are not covered under this benefit:
• Any food item, including infant formulas, nutritional supplements, vitamins, plus prescription vitamins,
medical foods and other nutritional items, even if it is the sole source of nutrition. except as described above
Orthotic devices
100% (of the negotiated charge) per
item
80% (of the recognized charge) per
item
All other prosthetic devices
100% (of the negotiated charge) per
item
80% (of the recognized charge) per
item
Prosthetic and customized orthotic
devices Includes Cranial prosthetics
(Medical wigs)
100% (of the negotiated charge) per
item
80% (of the recognized charge) per
item
The following are not covered under this benefit:
• Services covered under any other benefit
• Orthopedic shoes, therapeutic shoes, foot orthotics, or other devices to support the feet, unless required for
the treatment of or to prevent complications of diabetes, or if the orthopedic shoe is an integral part of a
covered leg brace
• Trusses, corsets, and other support items
• Repair and replacement due to loss, misuse, abuse or theft
•
Communication aids
Hearing aids for Minors
Hearing aids
Covered persons under age 18
80% (of the negotiated charge) per
visit
60% (of the recognized charge) per
visit
Hearing aids maximum per ear
One hearing aid per ear every 12 months
The following are not covered under this benefit:
• A replacement of:
– A hearing aid that is lost, stolen or broken
– A hearing aid installed within the prior 12 month period
• Replacement parts for a hearing aid
• Batteries or cords
• A hearing aid that does not meet the specifications prescribed for correction of hearing loss
• Any hearing aid prescribed by someone other than a hearing care professional

Illinois Institute of Technology 2024-2025 Page 21
• Any tests, appliances and devices to:
– Improve your hearing. This includes hearing aid batteries and auxiliary equipment.
– Enhance other forms of communication to make up for hearing loss or devices that simulate speech.
Eligible health services
In-network coverage
Out-of-network coverage
Hearing aids for Adults
80% (of the negotiated charge) per
item
60% (of the recognized charge) per
item
Hearing aids maximum per ear
One hearing aid per ear every 12 months
The following are not covered under this benefit:
• A replacement of:
- A hearing aid that is lost, stolen or broken
- A hearing aid installed within the prior 12 month period
• Replacement parts or repairs for a hearing aid
• Batteries or cords
• A hearing aid that does not meet the specifications prescribed for correction of hearing loss
• Any ear or hearing exam performed by a physician who is not certified as an otolaryngologist or otologist
Hearing exams
Covered persons over age 18
80% (of the negotiated charge) per
visit
60% (of the recognized charge) per
visit
The following are not covered under this benefit:
• Hearing exams given during a stay in a hospital or other facility, except those provided to newborns as part of
the overall hospital stay
Pediatric vision care (Limited to covered persons through the end of the month in which the person turns age 19)
Performed by a legally qualified
ophthalmologist or optometrist
(includes comprehensive low vision
evaluations)
100% (of the negotiated charge) per
visit
No policy year deductible applies
80% (of the recognized charge) per
visit
No policy year deductible applies
Office visit for fitting of contact
lenses
100% (of the negotiated charge) per
visit
No policy year deductible applies
80% (of the recognized charge) per
visit
No policy year deductible applies
Low vision Maximum
One comprehensive low vision evaluation every policy year
Pediatric vision care services &
supplies-Eyeglass frames,
prescription lenses or prescription
contact lenses
100% (of the negotiated charge) per
item
No policy year deductible applies
80% (of the recognized charge) per
item
No policy year deductible applies
Maximum number Per year:
Eyeglass frames
Prescription lenses
Contact lenses (includes non-
conventional prescription contact
lenses & aphakic lenses prescribed
after cataract surgery)
One set of eyeglass frames
One pair of prescription lenses
Daily disposables: up to 3 month supply
Extended wear disposable: up to 6 month supply
Non-disposable lenses: one set
Optical devices
Covered according to the type of
benefit and the place where the
service is received.
Covered according to the type of
benefit and the place where the
service is received.
Maximum number of optical devices
per policy year
One optical device

Illinois Institute of Technology 2024-2025 Page 22
*Important note: Refer to the Vision care section in the certificate of coverage for the explanation of these vision care
supplies.
As to coverage for prescription lenses in a policy year, this benefit will cover either prescription lenses for eyeglass
frames or prescription contact lenses, but not both.
Outpatient prescription drugs
Copayment/coinsurance waiver for risk reducing breast cancer
The prescription copayment/coinsurance will not apply to risk reducing breast cancer prescription drugs when
obtained at a retail in-network, pharmacy. This means that such risk reducing breast cancer prescription drugs are
paid at 100%.
Copayment waiver for tobacco cessation prescription and over-the-counter drugs
The outpatient prescription drug copayment will not apply to the first two 90-day treatment regimens per policy
year for tobacco cessation prescription drugs and OTC drugs when obtained at a in-network pharmacy. This
means that such prescription drugs and OTC drugs are paid at 100%.
Your prescription drug copayment will apply after those two regimens per policy year have been exhausted.
Copayment waiver for contraceptives
The prescription drug copayment will not apply to female contraceptive methods when obtained at a in-network
pharmacy.
This means that such contraceptive methods are paid at 100% for:
• Certain over-the-counter (OTC) and generic contraceptive prescription drugs and devices for each of the
methods identified by the FDA. Related services and supplies needed to administer covered devices will also
be paid at 100%.
• If a generic prescription drug or device is not available for a certain method, you may obtain certain brand-
name prescription drug or device for that method paid at 100%.
The outpatient prescription drug copayment continue to apply to prescription drugs
that have a generic equivalent,
biosimilar or generic alternative available within the same therapeutic drug class obtained at a in-network pharmacy
unless you are granted a medical exception. The certificate of coverage explains how to get a medical exception.
Eligible health services
In-network coverage
Out-of-network coverage
Preferred generic prescription drugs
For each fill up to a 30 day
supply filled at a retail
pharmacy
$12 copayment per supply then the
plan pays 100% (of the balance of the
negotiated charge)
No policy year deductible applies
Not Covered
Preferred brand-name prescription drugs
For each fill up to a 30 day
supply filled at a retail
pharmacy
$40 copayment per supply then the
plan pays 100% (of the balance of the
negotiated charge)
No policy year deductible applies
Not Covered
Illinois Institute of Technology 2024-2025 Page 23
Eligible health services
In-network coverage
Out-of-network coverage
Non-preferred generic prescription drugs
For each fill up to a 30 day
supply filled at a retail
pharmacy
$55 copayment per supply then the
plan pays 100% (of the balance of the
negotiated charge)
No policy year deductible applies
Not Covered
Non-preferred brand-name prescription drugs
For each fill up to a 30 day
supply filled at a retail
pharmacy
$55 copayment per supply then the
plan pays 100% (of the balance of the
negotiated charge)
No policy year deductible applies
Not Covered
Specialty prescription drugs
For each fill up to a 30 day
supply filled at a retail
pharmacy
Copayment is the greater of $150 or
20% (of the negotiated charge) but will
be no more than $250 per supply
No policy year deductible applies
Not Covered
Diabetic insulin
30 day supply at retail
pharmacy
Paid according to the type of drug per
the schedule of benefits above
Not Covered
Diabetic supplies, drugs, and insulin important note:
Your cost share will not exceed $100 per 30 day supply of a covered prescription insulin drug filled at an in-network
pharmacy. No policy year deductible applies for diabetic supplies and insulin.
Anti-cancer drugs taken by
mouth- For each fill up to a 30
day supply
100% (of the negotiated charge)
No policy year deductible applies
Not Covered
Infertility Drugs
For each fill up to a 30 day
supply filled at a retail
pharmacy
Paid according to the type of drug per
the schedule of benefits
Not Covered
Contraceptives (birth control)
For each fill up to a 12 month
supply of generic and OTC
drugs and devices filled at a
retail
100% (of the negotiated charge)
No policy year deductible applies
Not Covered
For each fill up to a 12 month
supply of brand name
prescription drugs and devices
filled at a retail
Paid according to the type of drug per
the schedule of benefits, above
Not Covered
Contraceptive prescription drugs
We may cover the dispensing of up to a 12 month supply worth of contraception at one time. The copayment per
supply is 1-12 times the 30 day copayment per supply

Illinois Institute of Technology 2024-2025 Page 24
Eligible health services
In-network coverage
Out-of-network coverage
Preventive care drugs and
supplements filled at a retail
or mail order pharmacy
For each 30 day supply
100% (of the negotiated charge per
prescription or refill
No copayment or policy year
deductible applies
Not Covered
Risk reducing breast cancer
prescription drugs filled at a
pharmacy
For each 30 day supply
100% (of the negotiated charge) per
prescription or refill
No copayment or policy year
deductible applies
Not Covered
Maximums:
Coverage will be subject to any sex, age, medical condition, family history, and
frequency guidelines in the recommendations of the United States Preventive
Services Task Force.
Tobacco cessation prescription
drugs and OTC drugs filled at a
pharmacy
For each 30 day supply
100% (of the negotiated charge per
prescription or refill
No copayment or policy year
deductible applies
Not Covered
Maximums:
Coverage is permitted for two 90-day treatment regimens only.
Coverage will be subject to any sex, age, medical condition, family history, and
frequency guidelines in the recommendations of the United States Preventive
Services Task Force.
Dispense As Written (DAW)
If a prescriber prescribes a covered brand-name prescription drug where a generic prescription drug equivalent is
available and specifies “Dispense As Written” (DAW), you will pay the cost sharing for the brand-name prescription
drug. If a prescriber does not specify DAW and you request a covered brand-name prescription drug where a
generic prescription drug equivalent is available, you will be responsible for the cost difference between the brand-
name prescription drug and the generic prescription drug, plus the cost sharing that applies to the brand-name
prescription drug. The cost difference related to a prescription drug that is not specified as DAW is not applied
towards your policy year deductible or maximum out-of-pocket limit.

Illinois Institute of Technology 2024-2025 Page 25
Outpatient prescription drug exclusions
The following are not eligible health services:
• Any services related to providing, injecting or application of a drug
• Compounded prescriptions containing bulk chemicals not approved by the FDA including compounded
bioidentical hormones
• Cosmetic drugs including medication and preparations used for cosmetic purposes
• Devices, products and appliances unless listed as an eligible health service
• Dietary supplements including medical foods
• Drugs or medications:
- Administered or entirely consumed at the time and place they are prescribed or provided
- Which do not require a prescription by law, even if a prescription is written, unless we have approved a
medical exception
- That are therapeutically the same or an alternative to a covered prescription drug, unless we approve a
medical exception
- Not approved by the FDA or not proven safe or effective
- Provided under your medical plan while inpatient at a healthcare facility
- Recently approved by the FDA but not reviewed by our Pharmacy and Therapeutics Committee
- That include vitamins and minerals unless recommended by the United States Preventive Services Task
Force (USPSTF)
- That are used to treat sexual dysfunction, enhance sexual performance or increase sexual desire,
including drugs, implants, devices or preparations to correct or enhance erectile function, enhance
sensitivity or alter the shape or appearance of a sex organ unless listed as an eligible health service
- That are used for the purpose of weight gain or loss including but not limited to stimulants,
preparations, foods or diet supplements, dietary regimens and supplements, food or food supplements,
appetite suppressants or other medications
- That are drugs or growth hormones used to stimulate growth and treat idiopathic short stature, unless
there is evidence that the covered person meets one or more clinical criteria detailed in our
precertification and clinical policies
• Duplicative drug therapy; for example, two antihistamines for the same condition
• Genetic care including:
- Any treatment, device, drug, service or supply to alter the body’s genes, genetic makeup or the
expression of the body’s genes unless listed as an eligible health service
• Immunizations related to travel or work
• Immunization or immunological agents except as specifically stated in the schedule of benefits or the
certificate
• Implantable drugs and associated devices except as specifically stated in the schedule of benefits or the
certificate
• Injectables including:
- Any charges for the administration or injection of prescription drugs
- Needles and syringes except for those used for insulin administration
- Any drug which, due to its characteristics must typically be administered or supervised by a qualified
provider or licensed certified health professional in an outpatient setting with the exception of Depo
Provera and other injectable drugs for contraception

Illinois Institute of Technology 2024-2025 Page 26
• Off-label drug use except for indications recognized through peer-reviewed medical literature or when
coverage is required by law for elective termination of pregnancy
• Prescription drugs:
- That are ordered by a dentist or prescribed by an oral surgeon in relation to the removal of teeth or
prescription drugs for the treatment of a dental condition
- That are considered oral dental preparations and fluoride rinses except pediatric fluoride tablets or
drops as specified on the plan’s drug guide
- That are used for the purpose of improving visual acuity or field of vision
- That are being used or abused in a manner that is determined to be furthering an addiction to a habit-
forming substance, or drugs obtained for use by anyone other than the person identified on the ID card
• Replacement of lost or stolen prescriptions
• Test agents except diabetic test agents
• Tobacco cessation drugs, unless recommended by the USPSTF
• We reserve the right to exclude:
- A manufacturer’s product when the same or similar drug (one with the same active ingredient or same
therapeutic effect), supply or equipment is on the plan’s drug guide
- Any dosage or form of a drug when the same drug is available in a different dosage or form on the
plan’s drug guide
A covered person, a covered person’s designee or a covered person’s prescriber may seek an expedited medical
exception process to obtain coverage for non-covered drugs in exigent circumstances. An “exigent circumstance” exists
when a covered person is suffering from a health condition that may seriously jeopardize a covered person’s life, health,
or ability to regain maximum function or when a covered person is undergoing a current course of treatment using a
non-formulary drug. The request for an expedited review of an exigent circumstance may be submitted by contacting
Aetna's Pre-certification Department at 1-855-240-0535, faxing the request to 1-877-269-9916, or submitting the
request in writing to:
CVS Health
ATTN: Aetna PA
1300 E Campbell Road
Richardson, TX 75081
Out of Country claims
Out of Country claims should be submitted with appropriate medical service and payment information from the
provider of service. Covered services received outside the United States will be considered at the Out-of-network level
of benefits.
General Exclusions
Acupuncture

Illinois Institute of Technology 2024-2025 Page 27
• Acupuncture
• Acupressure
Alternative health care
• Services and supplies given by a provider for alternative health care. This includes but is not limited to
aromatherapy, naturopathic medicine, herbal remedies, homeopathy, energy medicine, Christian faith-
healing medicine, Ayurvedic medicine, yoga, hypnotherapy, and traditional Chinese medicine.
Armed forces
• Services and supplies received from a provider as a result of an injury sustained, or illness contracted, while in
the service of the armed forces of any country. When you enter the armed forces of any country, we will refund
any unearned pro-rata premium to the policyholder.
Behavioral health treatment
• Services for the following based on categories, conditions, diagnoses or equivalent terms as listed in the most
recent version of the Diagnostic and Statistical Manual of Mental Disorders (DSM) of the American Psychiatric
Association:
- Stay in a facility for treatment for dementias and amnesia without a behavioral disturbance that
necessitates mental health treatment
- School and/or education service including special education, remedial education, wilderness treatment
programs, or any such related or similar programs
- Services provided in conjunction with school, vocation, work or recreational activities
- Transportation
- Sexual deviations and disorders except in the Eligible health services and exclusions section
- Tobacco use disorders except as described in the Eligible health services and exclusions – Preventive care
and wellness section
Beyond legal authority
• Services and supplies provided by a health professional or other provider that is acting beyond the scope of its
legal authority
Blood, blood plasma, synthetic blood, blood derivatives or substitutes
Examples of these are:
• The provision of donated blood to the hospital, other than blood derived clotting factors
• Any related services for donated blood including processing, storage or replacement expenses
• The service of blood donors, including yourself, apheresis or plasmapheresis
• The blood you donate for your own use, excluding administration and processing expenses and except where
described in the Eligible health services and exclusions – Transplant services section
Clinical trial therapies (experimental or investigational)
• Your plan does not cover clinical trial therapies (experimental or investigational), except as described in the
Eligible health services and exclusions- Clinical trial therapies (experimental or investigational) section in the
certificate
Cosmetic services and plastic surgery
• Any treatment, surgery (cosmetic or plastic), service or supply to alter, improve or enhance the shape or
appearance of the body except where described in the Eligible health services - Reconstructive surgery and

Illinois Institute of Technology 2024-2025 Page 28
supplies section.
This exclusion does not apply to:
• Surgery after an accidental injury when performed as soon as medically feasible. (Injuries that occur during
medical treatments are not considered accidental injuries even if unplanned or unexpected.)
• Coverage that may be provided under the Eligible health services and exclusions - Gender affirming treatment
section.
• The removal of breast implants due to an illness or injury
Court-ordered services and supplies
• Court-ordered testing or care unless medically necessary. This exclusion does not apply to court-ordered FDA-
approved prescription drugs for the treatment of substance use disorders and any associated counseling or
wraparound services.
Custodial care
Services and supplies meant to help you with activities of daily living or other personal needs.
Examples of these are:
• Routine patient care such as changing dressings, periodic turning and positioning in bed
• Administering oral medications
• Care of a stable tracheostomy (including intermittent suctioning)
• Care of a stable colostomy/ileostomy
• Care of stable gastrostomy/jejunostomy/nasogastric tube (intermittent or continuous) feedings
• Care of a bladder catheter (including emptying/changing containers and clamping tubing)
• Watching or protecting you
• Respite care except in connection with hospice care, adult (or child) day care, or convalescent care
• Institutional care. This includes room and board for rest cures, adult day care and convalescent care
• Help with walking, grooming, bathing, dressing, getting in or out of bed, toileting, eating or preparing foods
• Any other services that a person without medical or paramedical training could be trained to perform
• Any service that can be performed by a person without any medical or paramedical training
• For behavioral health (mental health treatment and substance related disorders treatment):
- Services provided when you have reached the greatest level of function expected with the current level of
care, for a specific diagnosis
- Services given mainly to:
o Maintain, not improve, a level of function
• Provide a place free from conditions that could make your physical or mental state worse

Illinois Institute of Technology 2024-2025 Page 29
Dental care for adults
• Dental services for adults including services related to:
- The care, filling, removal or replacement of teeth and treatment of injuries to or diseases of the teeth
- Dental services related to the gums
- Apicoectomy (dental root resection)
- Orthodontics
- Root canal treatment
- Soft tissue impactions
- Alveolectomy
- Augmentation and vestibuloplasty treatment of periodontal disease
- False teeth
- Prosthetic restoration of dental implants
- Dental implants
This exception does not include treatment of accidental injuries to sound natural teeth and treatment for
diseases of the teeth, removal of bony impacted teeth, bone fractures, removal of tumors, and odontogenic
cysts. . This exclusion also does not include tooth extraction surgery in preparation for radiation treatment of
neoplastic jaw or throat diseases.
Educational services
Examples of these services are:
• Any service or supply for education, training or retraining services or testing, except where described in the
Eligible health services and exclusions – Diabetic services and supplies (including equipment and training)
section. This includes:
- Special education
- Remedial education
- Wilderness treatment programs (whether or not the program is part of a residential treatment facility or
otherwise licensed institution)
- Job training
- Job hardening programs
Educational services, schooling or any such related or similar program, including therapeutic programs
within a school setting. However, covered services for autism spectrum disorders or habilitative services for
children will not be denied solely because of the location where clinically appropriate services of this type
are provided.
Examinations
Any health or dental examinations needed:
• Because a third party requires the exam. Examples are, examinations to get or keep a job, or
examinations required under a labor agreement or other contract
• Because a law requires it
• To buy insurance or to get or keep a license
• To travel
• To go to a school, camp, or sporting event, or to join in a sport or other recreational activity

Illinois Institute of Technology 2024-2025 Page 30
Experimental or investigational
• Experimental or investigational drugs, devices, treatments or procedures unless otherwise covered under clinical
trial therapies (experimental or investigational) or covered under clinical trials (routine patient costs). See the
Eligible health services and exclusions – Other services section . Note that this exclusion will not impact your
ability to obtain an external review of denial of coverage for a service or supply denied by us as experimental or
investigational.
Facility charges
For care, services or supplies provided in:
• Rest homes
• Assisted living facilities
• Similar institutions serving as a persons’ main residence or providing mainly custodial or rest care
• Health resorts
• Spas or sanitariums
• Infirmaries at schools, colleges, or camps
Gene-based, cellular and other innovative therapies (GCIT)
The following are not eligible health services unless you receive prior written approval from us:
• All associated services when GCIT services are not covered. Examples include infusion, laboratory, radiology,
anesthesia, and nursing services.
Please refer to the Medical necessity , referral and precertification requirements section.
Genetic care
• Any treatment, device, drug, service or supply to alter the body’s genes, genetic make-up, or the
expression of the body’s genes except for the correction of congenital birth defects
Growth/Height care
• A treatment, device, drug, service or supply with the primary purpose to increase or decrease height or
alter the rate of growth This does not include growth hormone therapy.
• Surgical procedures, devices and growth hormones to stimulate growth
Illegal Occupation
Services and supplies that you receive as a result of an injury due to your commission of a felony to which the
contributing cause was the engagement of an illegal occupation.
Incidental surgeries
• Charges made by a physician for incidental surgeries. These are non-medically necessary surgeries performed
during the same procedure as a medically necessary surgery.

Illinois Institute of Technology 2024-2025 Page 31
Jaw joint disorder
• Surgical treatment of jaw joint disorders
• Non-surgical treatment of jaw joint disorders
• Jaw joint disorders treatment performed by prosthesis placed directly on the teeth, surgical and non-
surgical medical and dental services, and diagnostic or therapeutics services related to jaw joint
disorders including associated myofascial pain
This exclusion does not apply to covered benefits for treatment of TMJ and CMJ as described in the Eligible
health services and exclusions –Temporomandibular joint dysfunction (TMJ) and craniomandibular joint
dysfunction (CMJ) treatment section in the certificate.
Judgment or settlement
• Services and supplies for the treatment of an injury or illness to the extent that payment is made as a judgment
or settlement by any person deemed responsible for the injury or illness (or their insurers)
Mandatory no-fault laws
• Treatment for an injury to the extent benefits are payable under any state no-fault automobile coverage.
Maintenance care
• Care made up of services and supplies that maintain, rather than improve, a level of physical or mental
function, except for habilitation therapy services. See the Eligible health services and exclusions –
Habilitation therapy services section in the certificate
Medical supplies – outpatient disposable
• Any outpatient disposable supply or device. Examples of these are:
- Sheaths
- Bags
- Elastic garments
- Support hose
- Bandages
- Bedpans
- Syringes
- Blood or urine testing supplies
- Other home test kits
- Splints
- Neck braces
- Compresses
- Other devices not intended for reuse by another patient
Medicare
• Services and supplies available under Medicare, if you are entitled to premium-free Medicare Part A or enrolled
in Medicare Part B, or if you are not entitled to premium-free Medicare Part A or enrolled in Medicare Part B
because you refused it, dropped it, or did not make a proper request for it
Non-U.S .citizen
• Services and supplies received by a covered person (who is not a United States citizen) within the covered
person’s home country but only if the home country has a socialized medicine program

Illinois Institute of Technology 2024-2025 Page 32
Other primary payer
• Payment for a portion of the charge that Medicare or another party is responsible for as the primary
payer
Outpatient prescription or non-prescription drugs and medicines
• Outpatient prescription drugs or non-prescription drugs and medicines provided by the policyholder
Personal care, comfort or convenience items
• Any service or supply primarily for your convenience and personal comfort or that of a third party
Riot
• Services and supplies that you receive from providers as a result of an injury from your “participation in
a riot”. This means when you take part in a riot in any way such as inciting, or conspiring to incite, the
riot. It does not include actions that you take in self-defense as long as they are not against people who
are trying to restore law and order.
Routine exams
• Routine physical exams, routine eye exams, routine dental exams, routine hearing exams and other preventive
services and supplies, except as specifically provided in the Eligible health services and exclusions section
School health services
• Services and supplies normally provided by the policyholder’s:
- School health services
- Infirmary
- Hospital
- Pharmacy or
by health professionals who
- Are employed by
- Are Affiliated with
- Have an agreement or arrangement with, or
- Are otherwise designated by
the policyholder.
Services not permitted by law
• Some laws restrict the range of health care services a provider may perform under certain circumstances or in a
particular state. When this happens, the services are not covered by the plan.
Services provided by a family member
• Services provided by a spouse, domestic partner, civil union partner parent, child, step-child, brother,
sister, in-law or any household member
Sexual dysfunction and enhancement
• Any treatment, prescription drug, service, or supply to treat sexual dysfunction, enhance sexual
performance or increase sexual desire, including:
- Surgery, prescription drugs, implants, devices or preparations to correct or enhance erectile
function, enhance sensitivity, or alter the shape or appearance of a sex organ
- Sex therapy, sex counseling, marriage counseling, or other counseling or advisory services
• Not eligible for coverage are prescription drugs in 60 day supplies

Illinois Institute of Technology 2024-2025 Page 33
This exclusion does not include surgery and prosthetic devices for erectile dysfunction resulting from:
• Natural causes
• Trauma
• Infection
• Congenital disease or defects
Strength and performance
• Services, , devices and supplies such as drugs or preparations designed primarily for enhancing your:
− Strength
− Physical condition
− Endurance
− Physical performance
Telemedicine
• Services given when you are not present at the same time as the provider
• Services including:
– Telemedicine kiosks
– Electronic vital signs monitoring or exchanges, (e.g. Tele-ICU, Tele-stroke)
Therapies and tests
• Full body CT scans
• Hair analysis
• Hypnosis and hypnotherapy
• Massage therapy, except when used as a physical therapy modality
• Sensory or auditory integration therapy
Tobacco cessation
• Any treatment, drug, service or supply to stop or reduce smoking or the use of other tobacco products
or to treat or reduce nicotine addiction, dependence or cravings, including, medications, nicotine
patches and gum unless recommended by the United States Preventive Services Task Force (USPSTF).
This also includes:
- Counseling, except as specifically provided in the Eligible health services and exclusions – Preventive
care and wellness section in the certificate
- Hypnosis and other therapies
- Medications, except as specifically provided in the Eligible health services and exclusions –
Outpatient prescription drugs section in the certificate
- Nicotine patches
- Gum
Treatment in a federal, state, or governmental entity
• Any care in a hospital or other facility owned or operated by any federal, state or other governmental entity,
except to the extent coverage is required by applicable laws
Vision care for adults
• Routine vision exam provided by an ophthalmologist or optometrist, including refraction and glaucoma testing
• Vision care services and supplies

Illinois Institute of Technology 2024-2025 Page 34
Voluntary sterilization
• Reversal of voluntary sterilization procedures, including related follow-up care
Wilderness treatment programs
See Educational services within this section
Work related illness or injuries
• Coverage available to you under worker’s compensation or under a similar program under local, state or
federal law for any illness or injury related to employment or self-employment.
• A source of coverage or reimbursement will be considered available to you even if you waived your right to
payment from that source. You may also be covered under a workers’ compensation law or similar law. If you
submit proof that you are not covered for a particular illness or injury under such law, then that illness or injury
will be considered “non-occupational” regardless of cause.
The Illinois Institute of Technology Student Health Insurance Plan is underwritten by Aetna Life Insurance Company.
Aetna Student Health
SM
is the brand name for products and services provided by Aetna Life Insurance Company Aetna
Health and Life Insurance Company and its applicable affiliated companies (Aetna).

Illinois Institute of Technology 2024-2025 Page 35
Sanctioned Countries
If coverage provided by this policy violates or will violate any economic or trade sanctions, the coverage is immediately
considered invalid. For example, Aetna companies cannot make payments for health care or other claims or services if it
violates a financial sanction regulation. This includes sanctions related to a blocked person or a country under sanction
by the United States, unless permitted under a written Office of Foreign Asset Control (OFAC) license. For more
information, visit http://www.treasury.gov/resource-center/sanctions/Pages/default.aspx
.
Assistive Technology
Persons using assistive technology may not be able to fully access the following information. For assistance, please call
1-877-480-4161.
Smartphone or Tablet
To view documents from your smartphone or tablet, the free WinZip app is required. It may be available from your App
Store.
Non-Discrimination
Aetna is committed to being an inclusive health care company. Aetna does not discriminate on the basis of ancestry, race,
ethnicity, color, religion, sex/gender (including pregnancy), national origin, sexual orientation, gender identity or
expression, physical or mental disability, medical condition, age, veteran status, military status, marital status, genetic
information, citizenship status, unemployment status, political affiliation, or on any other basis or characteristic prohibited
by applicable federal, state or local law.
Aetna provides free aids and services to people with disabilities and free language services to people whose primary
language is not English.
These aids and services include:
• Qualified language interpreters
• Written information in other formats (large print, audio, accessible electronic formats, other formats)
• Qualified interpreters
• Information written in other languages
If you need these services, contact the number on your ID card. Not an Aetna member? Call us at 1-877-480-4161.
If you have questions about our nondiscrimination policy or have a discrimination-related concern that you would like to
discuss, please call us at 1-877-480-4161.
Please note, Aetna covers health services in compliance with applicable federal and state laws. Not all health services are
covered. See plan documents for a complete description of benefits, exclusions, limitations, and conditions of coverage.
Language accessibility statement
Interpreter services are available for free.

Illinois Institute of Technology 2024-2025 Page 36
Attention: If you speak English, language assistance service, free of charge, are available to you. Call 1-877-480-
4161 (TTY: 711).
Español/Spanish
Atención: si habla español, tiene a su disposición servicios gratuitos de asistencia lingüística. Llame al
1-877-480-4161 (TTY: 711).
አማርኛ/Amharic
ልብ ይበሉ: ኣማርኛ ቋንቋ የሚናገሩ ከሆነ፥ የትርጉም ድጋፍ ሰጪ ድርጅቶች፣ ያለምንም ክፍያ እርስዎን ለማገልገል ተዘጋጅተዋል። የሚከተለው ቁጥር
ላይ
ይደውሉ 1-877-480-4161 (መስማት ለተሳናቸው: 711).
/Arabic
:
.
4161-480-877-1 )
:
711
.
(
Ɓàsɔ
̍
ɔ
̀
Wùɖù/Bassa
Dè d nìà k dy
k
dyi às
-wùù-po-ny
j n
, nì
à wuu kà kò ò po-po
gbo kp
a.
1-877-480-4161 (TTY: 711).
中文/Chinese
注意:如果您说中文,我们可为您提供免费的语言协助服务。请致电 1-877-480-4161 (TTY: 711)。
/Farsi
4161-480-877-1 )711TTY:
Français/French
Attention : Si vous parlez français, vous pouvez disposer d’une assistance gratuite dans votre langue en composant le 1-
877-480-4161 (TTY: 711).
/Gujarati
:
:
.
1-877-480-4161 (TTY: 711).
Kreyòl Ayisyen/Haitian Creole
Atansyon: Si w pale Kreyòl Ayisyen, gen sèvis èd pou lang ki disponib gratis pou ou. Rele 1-877-480-4161 (TTY: 711).
Igbo
Nrbama: br na na as Igbo, r enyemaka ass, n’efu, dr g. Kp 1-877-480-4161 (TTY: 711).

Illinois Institute of Technology 2024-2025 Page 37
한국어/Korean
주의: 한국어를 사용하시는 경우, 언어 지원 서비스가 무료로 제공됩니다. 1-877-480-4161(TTY: 711)번으로 전화해
주십시오.
Português/Portuguese
Atenção: a ajuda está disponível em português por meio do número 1-877-480-4161 (TTY: 711). Estes serviços são
oferecidos gratuitamente.
Русский/Russian
1-877-480-4161 (TTY: 711).
Tagalog
Paunawa: Kung nagsasalita ka ng Tagalog, maaari kang gumamit ng serbisyo ng tulong sa wika nang walang bayad
.
Tumawag sa 1-877-480-4161 (TTY: 711).
/Urdu
:
)711 (TTY: 4161-480-877-1 .
Tiếng Việt/Vietnamese
1-877-480-4161 (TTY: 711).
Yorùbá/Yoruba
Àkíyèsí: Bí o bá á, ìrànl
w
lórí èdè, lóf
, wà fú1-877-480-4161 (TTY: 711).
Aetna is the brand name used for products and services provided by one or more of the Aetna group of subsidiary
companies, including Aetna Life Insurance Company, Coventry Health Care plans and their affiliates (Aetna).
